Abstract
Serratia marcescens is a bacterial pathogen that tends to cause opportunistic infections, mainly in immune-compromised patients. In this case, we present a 69-year-old female who presented to the emergency department (ED) at Mount Sinai Hospital in Chicago on February 11th, 2022, after a mechanical fall. She had a medical history of metastatic lung cancer treated with chemotherapy, hypertension, pulmonary embolism, polysubstance abuse, and chronic obstructive pulmonary disease (COPD). The patient was found to be positive for systemic inflammatory response syndrome (SIRS). The patient was then started on broad-spectrum antibiotics, including vancomycin and cefepime. Blood cultures were ordered and came back positive for Serratia marcescens. This patient had multiple factors for immune suppression, including metastatic lung cancer, chemotherapy, and polysubstance abuse. The infectious disease department was consulted for the blood culture results, and ceftriaxone was recommended. Later on, levofloxacin was recommended. Blood cultures were negative two days after being positive. Afterward, the patient was kept for monitoring until discharge. Serratia marcescens is found in several reservoirs in nature. Therefore, preventing contact with this pathogen in immune-compromised patients can be difficult. It is important to have a degree of clinical suspicion for opportunistic pathogens like Serratia marcescens whenever a patient with factors for immune compromise presents for any condition.
Keywords: susceptibility, immune compromise, opportunistic bacterial infection, sirs criteria, serratia marcescens
Introduction
Serratia marcescens is a relatively rare bacterial infection. It mostly presents as an opportunistic infection [1-7]. Therefore, it more commonly causes infection in some form of the immune-compromised setting. Although multiple Serratia species can cause opportunistic infections, Serratia marcescens tends to be the most common one [2]. In addition, Serratia species are known to have resistance to multiple antibiotics [3,8-10]. In particular, Serratia species have intrinsic resistance to ampicillin, amoxicillin, ampicillin-sulbactam, amoxicillin-clavulanate, narrow-spectrum cephalosporins (including cefazolin, cefotaxime, and ceftazidime), cephamycins, cefuroxime, macrolides, tetracycline, and nitrofurantoin, and colistin [3,6]. Furthermore, resistant strains can transfer resistance to strains that are not intrinsically resistant; this can be done through the transfer of R-factors, which are certain kinds of plasmids [4]. This resistance can result in difficulty treating Serratia infections. Nevertheless, treatment options are available and based on susceptibility. Sometimes, multiple antibiotics need to be part of the treatment regimen in order to be effective. In this case, we present a 69-year-old female who was brought in for a mechanical fall and found to have a blood infection with Serratia marcescens.
Case presentation
A 69-year-old female with a history of metastatic lung cancer being treated with chemotherapy using erlotinib and complicated by metastases to the brain and bone, hypertension, pulmonary embolism, smoking, IV heroin abuse, and chronic obstructive pulmonary disease (COPD) was brought to the emergency department (ED) at Mount Sinai Hospital in Chicago on February 11th, 2022. She was brought for a mechanical fall while tripping over an oxygen tank at the oncology clinic. The patient was on erlotinib for her chemotherapy. In addition, the patient had a history of heroin and cocaine abuse. Upon arrival at the ED, her vitals were significant for having a temperature of 37, a heart rate of 137, and a respiratory rate of 28. As a result, the patient tested positive for systemic inflammatory response system (SIRS), and thus blood cultures were taken.
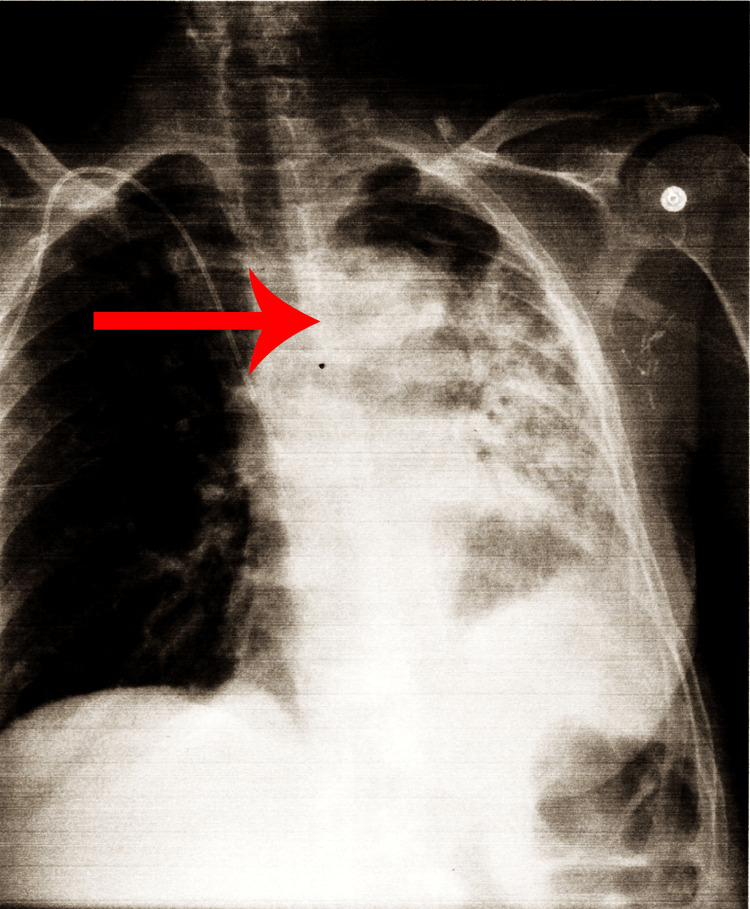
Furthermore, she was started on empiric vancomycin and cefepime. The patient was given IV fluids and potassium in the ED. In addition, the patient was found to have hypomagnesemia. Imaging, including chest X-ray, head CT, and echocardiogram (ECHO), were performed. Her brain CT showed no acute processes due to her fall. ECHO did not show any findings concerning endocarditis. Chest X-ray showed changes in the third left rib (Figure 1).
Figure 1. Chest X-ray showing changes near left third rib.
Blood cultures came back positive for Serratia marcescens. On the second day of admission, a chest ultrasound showed a small left effusion with atelectasis/consolidation. Repeat blood cultures on February 13th, 2022, came back negative. However, the patient was continued on antibiotics.
Furthermore, the patient endorsed left rib pain. The patient was given pain management via acetaminophen and morphine sulfate, which controlled the pain. Further, the patient complained of abdominal pain. Therefore, an abdominal CT scan was done, which showed no abscesses.
The infectious disease department was also consulted and recommended switching the patient to ceftriaxone. The patient was then switched to ceftriaxone on February 15th, 2022. Afterward, she was switched to levofloxacin on February 16th, 2022, which was last given on February 18th, 2022. All in all, the patient was on antibiotics for one week. The patient was then kept for monitoring for a few more days. The patient was finally discharged on February 21st, 2022. The patient's course summary is included in Table 1.
Table 1. Summary of the patient admission.
| Day of admission | Events |
| 1 | The patient was admitted to the emergency room for a mechanical fall; image studies did not reveal acute injuries. |
| 1 | The patient developed fever, tachycardia, hypotension, and leukocytosis concerning sepsis. The provider decided to pan-culture, including blood culture, urine culture, and sputum culture, to search for an infection source. However, a sputum culture was not sent as the patient did not have sputum. Meanwhile, the patient was given empirical antibiotics, vancomycin and cefepime, and fluid resuscitation, which improved the patient's vital signs. |
| 4 | Blood culture came positive for Serratia marcescens. She was susceptible to all the antibiotics. Urine culture was negative. The infection disease physician recommended switching antibiotics to ceftriaxone per sensitive test results. |
| 5 | The patient's general condition normalized after antibiotics therapy; a repeat blood culture from 02/13/2022 remained negative for three days. |
| 5 | The infection disease physician recommended switching to levofloxacin po 500mg, Q24hrs (02/16-02/18) for better compliance when the patient is discharged home. |
| 10 | The patient's general condition is good, and she is discharged home. |
Discussion
Serratia marcescens is an opportunistic pathogen with several reservoirs. It can be found in water, soil, plants, and animals [3,4,8]. In addition, Serratia marcescens can colonize patients' gastrointestinal or respiratory tract [11]. Colonized individuals may or may not experience symptoms [11]. Nevertheless, it rarely is a cause of primary infection. Rather, it tends to cause opportunistic infections in immune-compromised individuals [1,3-5]. Its abundance in the environment can make transmission difficult to avoid in immune-compromised patients. In this case, transmission can lead to infections such as bacteremia [12]. This patient had several factors contributing to immune suppression. One factor was that this patient had metastatic cancer and was treated with chemotherapy using erlotinib. Chemotherapy can cause immune suppression by inhibiting the production and proliferation of immune cells. This makes chemotherapy patients particularly prone to infection by pathogens that would not affect regular individuals.
Furthermore, cancer can affect an individual's ability to fight infection. Cancer disrupts the body's natural processes, especially when it metastasizes. Cancer cells take up vital nutrients, which deprives healthy cells. In addition, metastases can disrupt surrounding tissues, thus inhibiting them from carrying out their function. Furthermore, many tumors cause cachexia via factors they secrete [13]. This can also decrease a patient's ability to fight infection.
Another factor for immune suppression this patient had was polysubstance abuse. Substance abuse increases the risk of infection [14]. This occurs by contaminating substance delivery sites, especially IV drug injection sites. This allows pathogens to bypass barriers like the skin and enter more vulnerable sites like the blood. Moreover, another risk factor this patient had was old age, which has been associated with an increased risk for Serratia infections [15].
Furthermore, there are many other factors which may cause immune suppression. Factors such as diabetes, chronic kidney disease, malnutrition, autoimmune disease medications, steroids, organ transplant rejection prevention medications, hyposplenia, asplenia, human immunodeficiency virus (HIV), and some genetic disorders can all contribute to an immune-compromised state [16]. Scores of patients worldwide suffer from one or more of these conditions. Therefore, they are all at increased risk for opportunistic pathogens such as Serratia marcescens. Other examples of opportunistic pathogens are in the table below (Table 2).
Table 2. Opportunistic pathogens.
| Organism | Source | Presentation(s) |
| Candida albicans [10] | Oral cavity and genital organs [10] | Endocarditis, oral thrush, urinary tract infection, endophthalmitis [11] |
| Staphylococcus aureus | Skin [10] | Sepsis [10] |
| Pseudomonas aeruginosa | Medical devices [10] | Otitis externa, burn infections, pneumonia [10] |
| Clostridium difficile | Gastrointestinal tract [10] | Diarrhea, colitis [12] |
| Legionella pneumophila | Water [13] | Pneumonia [10] |
| Serratia marcescens | Water, soil, plants, and animals [3] | Urinary tract infections, bloodstream infections, and bloodstream infections [13] |
Antibiotic treatments for Serratia often depend on the infection's severity and sensitivities. Uncomplicated infections, including uncomplicated bacteremia, can be treated with fluoroquinolones, trimethoprim-sulfamethoxazole, piperacillin-tazobactam, third- and fourth-generation cephalosporins, and carbapenems as long as the strain is susceptible [3]. Even in panresistant strains, combining antibiotics can synergistically control Serratia marcescens infections [17]. In this case, the ID department recommended cefepime initially despite the patient having sepsis. The patient's condition quickly improved, and she had no evidence of severe hypoxia, acute organ failure, altered mental status, or central nervous system (CNS) infection.
Moreover, her blood culture showed susceptibility to all antibiotics. That is why we narrowed the antibiotics to ceftriaxone per culture results. The patient's general condition improved. Furthermore, repeated blood cultures remained negative, and the patient would be discharged home soon. Therefore, ID recommended switching to the oral antibiotic levofloxacin.
Conclusions
Taking care of patients with factors for immune suppression can be a complex task. They are at risk for infection with various opportunistic pathogens. In addition, there is great overlap in the clinical presentations of opportunistic infections. Due to their immune-compromised state, infection with these pathogens can have dire consequences for these patients. Therefore, it is important to have some degree of clinical suspicion for opportunistic infections, such as Serratia marcescens, whenever a patient with immune compromising factors presents, even if the chief complaint is not related to infection as in this case.
Case report was presented as an oral presentation on April 19th 2022 at Resident Research Day.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Herra Herra, Celine Celine, and Frederick R Falkiner. Serratia marcescens. [ Jul; 2022 ]. 2017. http://www.antimicrobe.org/b26.asp http://www.antimicrobe.org/b26.asp
- 2.Payal K Patel, MD MD, MPH MPH. Serratia. Medscape. [ Jul; 2022 ]. 2021. https://emedicine.medscape.com/article/228495 https://emedicine.medscape.com/article/228495
- 3.Moehring Moehring, Rebekah Rebekah, and Stephen Mahlen. UpToDate. Philadelphia, PA: Wolters Kluwer Health; [ Oct; 2020 ]. 2023. Infections due to Serratia species. [Google Scholar]
- 4.Serratia marcescens. [ Oct; 2022 ]. 2011. https://microbewiki.kenyon.edu/index.php/Serratia_marcescens https://microbewiki.kenyon.edu/index.php/Serratia_marcescens
- 5.Serratia marcescens - a rare opportunistic nosocomial pathogen and measures to limit its spread in hospitalized patients. Khanna A, Khanna M, Aggarwal A. J Clin Diagn Res. 2013;7:243–246. doi: 10.7860/JCDR/2013/5010.2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ceftazidime-avibactam activity when tested against ceftazidime-nonsusceptible Citrobacter spp., Enterobacter spp., Serratia marcescens, and Pseudomonas aeruginosa from Unites States medical centers (2011-2014) Sader HS, Castanheira M, Farrell DJ, Flamm RK, Jones RN. Diagn Microbiol Infect Dis. 2015;83:389–394. doi: 10.1016/j.diagmicrobio.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Marvelous but morbid: Infective endocarditis due to Serratia marcescens. Phadke VK, Jacob JT. Infect Dis Clin Pract. 2016;24:143–150. doi: 10.1097/IPC.0000000000000360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.RssAB-FlhDC-ShlBA as a major pathogenesis pathway in Serratia marcescens. Lin CS, Horng JT, Yang CH, et al. Infect Immun. 2010;78:4870–4881. doi: 10.1128/IAI.00661-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serratia infections: from military experiments to current practice. Mahlen SD. Clin Microbiol Rev. 2011;24:755–791. doi: 10.1128/CMR.00017-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serratia bacteremia in a large university hospital: trends in antibiotic resistance during 10 years and implications for antibiotic use. Choi SH, Kim YS, Chung JW, et al. Infect Control Hosp Epidemiol. 2002;23:740–747. doi: 10.1086/502004. [DOI] [PubMed] [Google Scholar]
- 11.Serratia marcescens colonization in preterm neonates during their neonatal intensive care unit stay. Moles L, Gómez M, Moroder E, et al. Antimicrob Resist Infect Control. 2019;8:135. doi: 10.1186/s13756-019-0584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Serratia marcescens siderophore serratiochelin is necessary for full virulence during bloodstream infection. Weakland DR, Smith SN, Bell B, Tripathi A, Mobley HL. Infect Immun. 2020;88:0–20. doi: 10.1128/IAI.00117-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Understanding cachexia as a cancer metabolism syndrome. Porporato PE. Oncogenesis. 2016;5:0. doi: 10.1038/oncsis.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Acute infections in intravenous drug users. Lavender TW, McCarron B. Clin Med. 2013;13:511–513. doi: 10.7861/clinmedicine.13-5-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Population-based laboratory surveillance for Serratia species isolates in a large Canadian health region. Laupland KB, Parkins MD, Gregson DB, Church DL, Ross T, Pitout JD. Eur J Clin Microbiol Infect Dis. 2008;27:89–95. doi: 10.1007/s10096-007-0400-7. [DOI] [PubMed] [Google Scholar]
- 16.Tidy Tidy, Dr Colin. Immunosuppression. Patient.info, 24 May. [ Jul; 2022 ]. 2023. https://patient.info/allergies-blood-immune/immune-system-diseases/immune-suppression https://patient.info/allergies-blood-immune/immune-system-diseases/immune-suppression
- 17.Synergistic effect of ceftazidime-avibactam with meropenem against panresistant, carbapenemase-harboring acinetobacter Baumannii and Serratia marcescens investigated using time-kill and disk approximation assays. Gaudereto JJ, Perdigão Neto LV, Leite GC, et al. Antimicrob Agents Chemother. 2019;63:0–18. doi: 10.1128/AAC.02367-18. [DOI] [PMC free article] [PubMed] [Google Scholar]