Abstract
Introduction
COVID pandemic shifted healthcare-related education to digital platforms. With the widespread availability of learning management systems like MOODLE, many opportunities exist to create innovative e-modules. Its success depends on the interactive multimedia resources and structural framework. The present study aims to create two patient-centric e-modules on Diabetes and Alcoholic liver disease in Pathology by a medical undergraduate facilitated by faculty and to assess its impact on learning outcomes and learners’ perceptions in relation to student seminars.
Methodology
This mixed-method intervention study combines quantitative and qualitative research methods to gain deeper insight into learners’ experiences. By random allocation, half of the second-year medical undergraduates (n = 60) attended an e-module, and the other half listened to a student seminar on the same topic with the same specific learning objectives. Pre- and post-test scores and feedback questionnaires were quantitatively analysed. Student-led focus group discussions (FGD) for learners’ experiences underwent thematic analysis.
Results
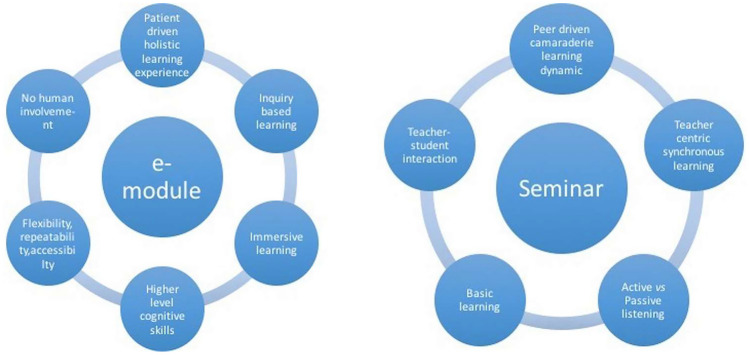
Pre- and post-tests for both learning techniques were statistically significant, while the feedback questionnaire’s responses favoured e-module. Four focus group discussions yielded six themes for the e-module: Patient-driven holistic learning experience, Inquiry-based learning, Immersive learning, Higher level cognitive skills, Flexibility, repeatability and accessibility, and No human involvement. The five themes for the seminar were: Peer-driven camaraderie learning dynamic, Teacher-centric synchronous learning, Active vs passive listening, Basic learning, and Teacher-student interaction.
Conclusion
While both learning techniques had comparable effects on test scores, they have merits and demerits. Hence, blending both techniques where seminars impart basic knowledge and e-module for deeper reinforcement will benefit the students.
Keywords: Patient-centric e-module, MOODLE, Seminar, Student-led focus group discussion, Mixed-method study
Introduction
COVID-19 pandemic led to an accelerated shift in medical and healthcare-related education to digital platforms [1]. The tech-savvy medical students quickly became accustomed to e-learning during lockdowns. However, a considerable gap exists between the student's demand and the availability of authentic e-learning resources [2]. Most available digital tools, especially in preclinical disciplines, are replicas of the traditional teaching–learning method. Thus, many educational institutes worldwide introduced Learning Management Systems (LMS) for better access to learning material, in addition to administrative announcements, attendance, assessments, and keeping track of learners’ academic performance. Some commonly used LMS include MOODLE, Blackboard, Canvas, Google Classroom and Osmosis [3, 4]. Though medical students have a positive attitude towards e-learning, some require extra motivation and encouragement to learn [3, 5]. Hence, embedding interactive tools and multimedia resources in the teaching module via LMS keeps the learner engaged [3]. While routine lecture-based approaches are teacher-directed and compartmentalised with no active involvement of students, e-learning tools can provide an innovative, interactive learning environment with the student’s active participation. One of the important shortcomings of LMS in the literature includes a lack of developing clinical reasoning skills due to a lack of interaction with patients [3]. The delivery of case-based e-learning modules could overcome this problem [6]. Most of the e-modules in the literature were created for postgraduate students, health professionals, and allied sciences and only a few for undergraduate medical students in the preclinical discipline. At the University of New South Wales, Australia, case-based e-modules on pathology topics like leukaemia, glomerulonephritis, and lymphoma with theoretical concepts administered to medical students resulted in significantly higher post-test scores when compared to control groups who underwent e-learning resources. Students also reported reduced perceived difficulty levels. Well-structured modules that are case-based with the conceptual framework and interactive multimedia resources with supporting quizzes were effective learning tools in e-modules in multiple studies. Feedback from the students revealed improved understanding and increased confidence regarding the topic [7, 8]. We used actual patients in this study to build a patient-based e-learning module in Pathology with relevant clinical data through multi-disciplinary integration. This also helps to understand the significance of Pathology in patient care and clinical decision-making [6]. Patient-centred learning provides realistic exposure to clinical scenarios and helps acquire contextualised knowledge through tailored information and targeted data. A literature review shows better knowledge retention when the learning material is proximal to patient data [9, 10]. Some challenges mentioned in e-learning studies include technical difficulties, internet connectivity, eye strain, distractions and lack of human interaction.
In the current learning climate, e-learning through a learning management system (LMS) is one of the effective ways to deliver ‘Competence-based medical education (CBME)’-prescribed clinically oriented integrated learning content interactively. Of many LMS available, MOODLE is a free, open-source learning platform used in many educational institutions worldwide. MOODLE stands for Modular Object-oriented Dynamic Learning Environment that helps in designing interactive instructional module catering to adult learning principles [6]. The wide range of options in MOODLE enables the integration of various clinical and laboratory-related videos and images with interactivity [11–14]. However, most medical teachers do not explore various MOODLE options due to technology resistance despite millennials and Gen Z medical students being digitally receptive. Studies show that teachers used to traditional teaching methods find it a burden to move towards e-learning modalities and have low technology skills [3, 15–17]. Involving students in creating e-learning content can overcome technical difficulties and make learning learner-centric [18]. Literature is sparse in evaluating the impact of student-generated material [18]. Adrian et al. evaluated a student-generated question bank which improved the depth and interactivity of learning [19]. A student-led web-based learning modality in Pediatrics posting empowered students with active, self-directed learning [20]. Virginia and Smith in their study noticed active participation in the laboratory following the conduct of student-generated comprehensive reviews in histology [21]. Incorporating learning resources from multiple disciplines can further enrich e-learning content. The clinical relevance of basic science knowledge can enhance the learning experience [13, 14, 18]. Using actual patients to build e-learning content in preclinical discipline is a step towards holistic learning with multi-disciplinary integration essential for clinical practice in the real world.
With the above conceptual ideas, the present study aims to create two patient-centric e-learning modules in pathology via MOODLE in integration with various disciplines by a second-year (preclinical) medical undergraduate, facilitated by faculty. The secondary objective is to assess the impact of the modules on learning outcomes (test scores), learners’ perceptions and satisfaction in relation to student-led seminars. Since seminars are one of the standard learner-centric traditional teaching–learning tools in many medical institutes worldwide, they are chosen for comparison. The student-led seminar is a small group teaching where the participants discuss with their fellow students under the guidance of a teacher. Clinical-based approach, quiz and interactivity were included to make the learning engaging and active [29, 30].
As pragmatists, we the researchers embrace newer, technologically innovative teaching–learning tools. We believe in the need for the digitalisation of medical education and assume that e-learning can grab the attention of young medical students. Before analysing the data from this study, we believed that interactive e-learning through MOODLE would enhance students’ knowledge of the topic. We expected a deeper understanding and better learning experience with a clinically integrated e-module using actual patients.
Methodology
Design
This mixed-method (educational) intervention study combines quantitative and qualitative research methods to get more insight into learners’ perspectives on the learning process and outcome and to understand the barriers and facilitators of e-learning and seminar experience. Figure 1 shows the overview of the interventions and the research design.
Fig. 1.
Overview of the research plan with corresponding research designs
We used the ‘Interpretative phenomenological approach’ for the qualitative part of the study. While participants present their perspectives on their learning experience, we, the researchers, interpret their views. The focus was to collect and analyse the undergraduates’ experiences with e-module and seminar learning. We believe in the constructivist paradigm that everyone individually constructs ideas as they interact with people, places, objects or situations. A constructivist believes that there is no one fixed reality but interactions, backgrounds and experiences give unique world views to people [31].
Context
Our institute’s medical school program spans five and a half years, with initial two and half years of preclinical subjects and the later 2 years of clinical disciplines followed by a year of internship. The majority of theory classes are discipline-specific and predominantly lecture-based. Student seminars are usually conducted once or twice a year in each department, where selected students present an assigned topic under the faculty’s guidance in their classroom. During the Covid pandemic, most medical colleges across India switched to online classes. As medical teachers, we explored a lot of e-learning platforms, viz. Google Classroom, Google Forms, and Kahoot, including MOODLE LMS. With the current CBME curriculum encouraging multiple innovative integrated learning approaches, we intend to create interactive e-modules in Pathology with multi-disciplinary integration. Since students were exposed to MOODLE platform for the first time in this study, we organised a brief sensitisation before the intervention. We chose Diabetes Mellitus and Alcoholic liver disease for the intervention due to the common geographical prevalence of the disease.
The research team includes a second-year medical undergraduate (first author) and four Pathology faculty with a common interest in undergraduate medical education and teaching experience ranging from 8 to 26 years. The second and third authors have 2 years of experience in qualitative research, with a few projects related to undergraduate medical education. Both have completed an introductory online course in MOODLE LMS.
Procedure
The study was conducted in the Pathology department at a reputed medical college in South India between August and October 2022 among second-year medical students (n = 60) who were divided randomly into two-halves by generating random numbers with MS Excel. One-half underwent Moodle-based e-module, and the other half attended the student-led seminar for an hour with the same ‘Specific learning objectives (SLOs)’. For the second intervention after 3 weeks, the group that attended the seminar previously underwent the e-module and vice-versa. Each learning technique had a participation of 25 to 27 students. Students who absented themselves during the interventions were excluded from the study. Attendance to e-module or seminars was purely voluntary and not made mandatory, and we did not intend to compare it with students’ scores on the final exams.
Two e-modules on ‘Diabetes Mellitus’ and ‘Alcoholic liver disease’ was designed with the key criteria of ‘Integration, Patient-based learning and Interactivity’ in a story format. Two patients admitted to the hospital ward with the above diagnosis exhibiting typical signs and symptoms of the disease during the study period were selected for the study after consultation with the concerned department in charge. These e-modules featured the patient’s clinical history, examination, laboratory investigations, pathogenesis, morphology, treatment and prognosis as subsections. The learning content was created by integrating multiple disciplines like General Medicine, Surgery, Ophthalmology and Pharmacology. The first author (student researcher) created the e-modules under the guidance of the second author through the varying stages of preparation. Six students prepared for two seminars, three each, under the guidance of another faculty. The seminar topic was divided into three subtopics, and each student was allotted 15 to 20 min. The same specific learning objectives as that of the e-module were used to prepare the seminar content. The structural framework of the seminar was clinical-based and included clinical features, pathological concepts, investigation and treatment. To make the seminar more interactive, students were also asked to prepare three questions (MCQs) related to their assigned subtopics that a faculty validated. Students presented their learning material as PowerPoint in an interactive way; at the end, they questioned their peers and discussed the answers. Seminar was conducted simultaneously with the e-module for the same duration of one hour. Two faculty members independently validated the structure and content of e-modules and seminars.
After consent, the first author recorded patients’ medical details as short audio in the patient’s voice. Clinical examinations conducted by the faculty and simple investigations done by the technician were captured as videos with subtitles (Fig. 2). The student researcher explained the pathogenesis of the disease as a voice-over by ‘concept map’ in PowerPoint. ‘You tube’ videos related to the subtopic were added to the module, with interactive questions embedded. Gross, microscopic slides and clinical features were displayed as H5P interactive images with explanations as ‘hotspot buttons’. H5P is the abbreviation for the HTML 5 package that allows interactive content creation with available images and videos. ‘Hotspot buttons’ allows you to place an overlay of a hotspot on the image; when a user presses the button, he/she gets the explanation of the spot in text or audio as designed. These plugins can be easily embedded in the module through MOODLE. Quizzes containing different question patterns, like MCQs, drag and drop, and matching, were designed with interactivity (Fig. 3). For every wrong response, hints were given, and multiple attempts were allowed until the learner reached the correct response. Only by answering the quiz can the student navigate to the next subsections. To encourage collaborative learning, ‘A discussion forum’ to raise/answer queries (Fig. 4), ‘Wiki’ to contribute learning points and ‘Workshop assignment’ for learners to answer a few short questions and evaluate their peer’s answers to assignment questions by random allocation were designed and were made mandatory to complete the module. Wiki in MOODLE is a common web page allowing students to create, add and change content. The student researcher and the second author were present during the e-learning session for guidance.
Fig. 2.
Interactive video of patient’s examination findings with labels
Fig. 3.
Example of an interactive quiz with a hint for a wrong response. Multiple tries are allowed
Fig. 4.
Response to query raised in the discussion forum
After the first intervention on Diabetes, we collected feedback questionnaires from all the students who attended either the seminar or e-module. We conducted focus group discussion (FGD) to explore learners’ experience after the second intervention on Alcoholic liver disease. From the researchers’ previous experience of FGD on medical students, inhibition to share their opinion to the faculty facilitator posed a significant hurdle. To overcome this problem, we opted for student-led FGD under the faculty’s supervision [17]. The second and fourth authors trained the student volunteers (2 males; 2 females) for a week to moderate FGD, which included a mock FGD session. A total of four focus group discussions (with 30 students), two each for seminar and e-learning experiences, were moderated by students under the guidance of four faculty members. Each session lasted an hour, with 7–8 students participating by random sampling. Faculty also took the role of ‘observers’ by taking notes (Fig. 1). Debriefing sessions were conducted after FGD among all the researchers and student moderators.
Ethics
The current study proposal was selected under the ‘Indian council for medical research-Short-term studentship’ (ICMR STS) project. The study was undertaken after the institute’s review board’s ethical clearance (Protocol number: JIP/IEC-OS/2022/256) and written consent from patients and students. In the ‘patient-centric e-module’, the patient’s identity was anonymised using photographs of the only affected body part (diabetic foot, ascites) and facial details were obscured in the videos. Students’ data was anonymised by reversible coding, and confidentiality was maintained.
Data Collection Instruments
Pre- and post-tests with ten multiple choice questions (MCQs) were prepared for each intervention in ‘Google Forms’ by faculty who were not facilitating e-module or seminars for that session. Of the 10 MCQs, seven were related to Pathology subjects and the remaining three were taken from the other clinical disciplines, with one MCQ per each specific learning objective framed. Five questions were designed to check the simple recall memory, while the other five MCQs were to examine application knowledge with considerable difficulty level. The same MCQs were used for pre- and post-test, e-module, and seminar intervention. Feedback questionnaires containing closed-ended questions with a 5-point Likert scale where 1 implies strongly disagree (2—disagree; 3—neither agree nor disagree; 4—agree) and 5 means strongly agree. The Likert scale measures the degree of respondents’ attitude allowing them to express how much they agree or disagree with a given statement. The three open-ended questions for the seminar and e-module were as follows: (1) Mention a few factors that enabled your learning?; (2) Mention a few factors that hindered your learning?; (3) Give your suggestions for us to improve. The items for the feedback questionnaire were generated after an exhaustive literature review. The pooled questions were peer-reviewed with other faculty members (authors), and the selected questions underwent expert validation. The experts include the Chief of our institute’s medical education unit and the Head of the Pathology department, with vast experience in medical education. They helped us at all project stages, from concept development to the item generation stage to content validation. They checked each item for its accuracy, representativeness, significance to the construct, and logical sequence of items and scored for degree of relevance and clarity. Ultimately, the questionnaires were pilot tested with a few medical undergraduates. The questionnaire responses were collected from all students anonymously in Google Forms after the first intervention on Diabetes Mellitus and analysed. Feedback responses of the three open-ended questions on e-learning and seminar revealed few learning barriers. Time was a significant concern in both groups, which was addressed in the subsequent module by making clear and crisp Specific learning objectives. A few suggestions, like making more interactive content, and explanations for histopathology images, were addressed in the intervention.
For focus group discussion (FGD) after the second intervention, an interview guide was prepared for the seminar and e-learning by brainstorming among the authors. The semistructured ‘interview guide’ contained an ice-breaking task to get everyone to talk; focusing exercises on orienting the group to the topic of discussion; transitioning questions to move the conversation into the main questions, and nine open-ended key questions that drive this discussion. For focussing exercises, we gave ten cards containing different learning methods/resources, and the students ranked them from one to ten in order of priority after group discussion. The key questions focused on the content’s structure, learning process, learning tools, presentation pattern, interactivity, level of learning achieved, type of execution, comparison to other methods, and suggestions for the future. The main objective behind these key questions is to understand the meaning of the learner’s experience, perception and satisfaction with the intervention. The discussion was audio recorded after written consent.
Data Analysis
Paired t-test was performed to compare pre- and post-interventional test scores for each group. While unpaired t-test was done to compare post-test scores between the seminar and e-module. Feedback questions’ Likert’s score (closed-ended) for the seminar and e-learning group were analysed by unpaired t-test. Statistical tests were done using SPSS software, and a p-value less than 0.05 was taken as statistically significant.
Four students who moderated the FGD prepared verbal transcripts in a Word document after hearing the audio, and the second author verified the transcripts’ integrity. There was a total of 56 pages of transcripts. The open-ended feedback questions from the first intervention were also included for analysis. The FGD analysis began with creating ‘anchor codes’ for the nine key questions in the FGD interview guide. Anchor codes are labels to represent each key question in the study for organisational purposes. After reading and re-reading the transcript, we highlighted relevant sentences and words that helped address the research questions. These highlighted sentences or words are called ‘empirical indicators’. Based on the research questions, ‘empirical indicators’ were ‘coded’. Codes are concepts or labels given to highlighted data in the transcript called empirical indicators. There are two main strategies for coding used in this study, the ‘descriptive’ and the ‘interpretative’ method. The ‘descriptive code’ summarises the basic description of the empirical indicator in the sentence. It includes ‘in-vivo coding’ where codes are taken directly from the text of the transcript. While ‘interpretative coding’ is when the researcher codes the implied meaning. We then compiled the codes according to how they answered the research question or anchor codes. This step aligned the ‘codes’ with the ‘anchor codes’. The second author manually coded the transcript and reached consensus codes with the other researchers. We also noted the number of times each code (code numbers) was assigned to the empirical indicators. The coding researcher bracketed her preconceptions and biases about e-learning and seminar by brainstorming & reflecting on them and then deliberately setting them aside. The next step in the data analysis is to create ‘Categories’ by assessing the characteristics of each code and grouping them based on the shared characteristics. So clusters of codes are called categories. We tabulated 17 ‘categories’ for e-module and seminar by constantly reviewing and comparing the final codes. By further iterating the codes and categories back and forth, the commonality among the codes in the related categories was assembled to derive ‘themes’. Themes emerge as a result of deeper examination of the categories to reduce them to concepts that represent sets of codes. The level of abstraction increases as we move from codes to categories to themes. We shared the ‘thematic analysis’ results with student moderators and participants of the Focus group discussion (FGD) (called ‘member checking’) for their validation. After four FGDs, we stopped as the data reached saturation (theoretical sampling) with no new topics emerging. The credibility of the present study was strengthened by the triangulation process done through multiple researchers using both quantitative and qualitative methods with multisource data collected from test scores, feedback questionnaires and focus group discussions.
Results
The students’ average age was 19 years, with a male-to-female ratio of 1:1. For the first intervention on ‘Diabetes’, one-half of the students (n = 25) attended the seminar, and the other half (n = 25) were assigned an e-module. For the second intervention on ‘Alcoholic liver disease’, the group that participated previously in the seminar took e-learning (n = 25) and vice-versa (n = 27). Pre- and post-tests for the seminar and e-learning group were statistically significant for each learning technique (Table 1). However, comparing the seminar and e-learning groups’ post-test scores, the p-value was insignificant. But the feedback questionnaires’ responses after the first intervention favoured the e-module (Table 2).
Table 1.
Pre-test vs post-test score for seminar vs e-module
| Learning interventions (score) | Average seminar score | p-value | Average E-module score | p-value | ||
|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | |||
| Diabetes (out of 10) |
4.8 (n = 25) |
6.3 (n = 25) |
0.002 |
4.5 (n = 25) |
6.6 (n = 25) |
0.0001 |
| Alcoholic liver disease (out of 10) |
4.5 (n = 27) |
6.2 (n = 27) |
0.0002 |
4.8 (n = 25) |
6.8 (n = 25) |
0.0001 |
Table 2.
List of statistically significant response to questions for seminar vs e-module after the first intervention (Diabetes)
| S. No. | Questions | Average Likert’s score (1 to 5) | Significant p-value |
|---|---|---|---|
| 1 | Seminar: Engaging | 3.5 | 0.0005 |
| E-learning: Engaging | 4.5 | ||
| 2 | Seminar: Objectives was clear | 3.5 | 0.00005 |
| E-learning: Objectives was clear | 4.4 | ||
| 3 | Seminar: Provided me an insight into holistic learning | 3.3 | 0.0007 |
| E-learning: Provided me an insight into holistic learning | 4.2 | ||
| 4 | Seminar: Well organised and interlinked | 3.6 | 0.0004 |
| E-learning: Well organised and interlinked | 4.5 | ||
| 5 | Seminar: Utilisation of digital & multimedia resources | 3.4 | 0.0002 |
| E-learning: Utilisation of digital & multimedia resources | 4.4 | ||
| 6 | Seminar: In-depth understanding | 3.1 | 0.00004 |
| E-learning: In-depth understanding | 4.1 | ||
| 7 | Seminar: No difference between ‘Seminar’ & traditional method | 3.0 | 0.0042 |
| E-learning: No difference between ‘e-learning’ & traditional method | 2.1 |
After the second intervention, four student-led FGDs for the seminar and e-learning (two each) were conducted. The transcripts were coded manually through an ‘inductive approach’ by a single researcher and reviewed by others. E-module generated 42 codes, and seminar FGD led to 40 codes of either descriptive or interpretative types. Further reviewing the codes for similarities and dissimilarities for both learning techniques, we grouped them into 17 ‘categories’. Table 3 shows an example for a category on ‘differences between seminar & e-learning’ obtained from all four FGDs with ten codes and their illustrations. In total, we brought about 102 codes grouped into 17 categories. By clustering and reviewing these codes and categories, we derived 11 ‘themes’ (Fig. 5). Thematic analysis of qualitative data underwent researcher, data and method triangulation, including member checking for further validation and credibility.
Table 3.
Differences between e-module and seminar
| Codes (number of times coded) with illustrations |
|---|
|
1. Repeatability vs One-time event (9) ‘E-learning can be used anytime. Lectures are only available at a certain time during the day’ |
|
2. Reinforcement tool vs Primary learning tool (6) ‘I prefer seminars as a first-time learning tool and e-learning as a concept strengthening tool’ |
|
3. Active learning vs Passive learning (7) ‘It [seminar] is just listening, no active participation is needed, and everyone has their own way of presenting things. In the e-learning everything was covered and we had the quizzes and all, so we test what we learned’ |
|
4. Computer-based interactivity vs Live human interactivity (6) ‘…in moodle…we will be skipping videos, but in seminar, some questions will be asked and we should answer, so atleast we try to contribute…’ |
|
5. Less scope to clarify doubts vs Easy-to-clarify doubts (2) ‘…if we have doubts we can ask the person [in seminar] but in moodle it is not possible’ |
|
6. Learner-controlled learning vs Teacher-controlled learning environment (2) ‘In e-learning we can go back and review our work and progress, try to understand well but in seminar we cannot’ |
|
7. Relaxed learning at own pace vs Pressure of missing the flow (2) ‘…in seminar if a person talks to you and if you miss any keywords, the flow will go, but in a e-learning you can go back and see whatever you have understood and whether we missed out anything, so it is very relaxed’ |
|
8. Patient-oriented learning vs theoretical understanding (2) ‘….somethings [patient’s images, videos] you cannot see in the hospital, we can see live in our screens…its very useful for us and when lecturer is taking a theory class we cannot see the patient, but in e-learning, we saw the diabetic foot and all, so thats better’ |
|
9. Engrossed in learning vs Chance of spacing out (2) ‘In moodle, we have to do something so we will not sleep, but lecture is a one-way interaction so we may feel sleepy’ |
|
10. Personalised experience vs Shared experience (2) ‘E-learning is one to one. You and the computer only know what is happening during the session….while seminars are more interactive…’ ‘…. in a lecture class, teachers will be telling their experience, what they did….they will be sharing things, which will stay in our mind’ |
Fig. 5.
Derived ‘Themes’ for e-module and seminar
The following ‘themes’ derived from FGD on the e-module with a short description and the participants’ illustrations are shown below:
-
Flexibility, repeatability and accessibility
The e-module is flexible to time and place and easily accessible via mobile or laptop. The students can repeatedly learn the e-content at their own pace..we could learn at our own pace, and we could use it whenever we want. -
Inquiry-based learning
The progressive disclosure of patients’ data with the inbuilt question design of the e-module makes the learners curious. The quiz segment challenges the learner’s prior knowledge, demands a response to questions at each step and guides them by giving clues. The learners can also self-assess the gained knowledge.After completing every topic, we can attempt the quiz, even if we commit any mistake, hint will be given, it is very helpful. Also, we can reattempt the quiz anytime. -
Immersive learning
E-module designed using a variety of audio-visual aids with interactive learning content in a personalised learning environment make the learners engaged and engrossed.Everything [e-learning content] was in order, from [patient’s]history it went into the subject and then, in between, videos were added from youtube, that was also very helpful so that we can know the content very nicely, like we will go deep into that… -
Patient-driven holistic learning experience
E-module built on actual patients gives near to real-life experience to the learners. Integrating multi-disciplinary content built around a patient provides a holistic approach to learning.… it’s [e-learning] like a mini virtual experience. We can see a patient in all stages of progression of the disease and how they [doctors] manage them. -
Higher level cognitive skill
The patient-based, clinically oriented e-module design and content helps learners to reach a higher order learning of Bloom’s taxonomy, such as ‘applying, analysing and evaluating’.…if a real live scenario happens, i feel like i can somewhat correlate and act accordingly after an e-learning session. -
No human involvement
E-learning does not involve face-to-face human interaction. It has little scope to clarify the doubts.
The following ‘themes’ emerged from the seminar FGD with a short description and illustrations from the participants:
-
Active vs passive listening
Listening to the seminar depends on the learners’ receptiveness. When a learner pays attention to what the presenter is saying, it is called active listening. While only hearing what the presenter is presenting is passive listening.….it [seminar] is just listening, no active participation is needed… -
Teacher/presenter and student interaction
The teacher’s presence and interaction between the learner and presenter, depending on the tutor’s skill and the student’s participation, promote the learning atmosphere.You [teacher/ presenter] ask questions first, and you know what the student knows about the topic and this way we can explain the topic. -
Basic learning
Conventional method helps to introduce a new topic in the classroom. It can be a useful primary mode for learning basic information.I prefer seminars as a first-time learning tool… -
Peer-driven camaraderie learning dynamic
Peer teaching instills a positive attitude and a motivation to learn. The learner can easily relate to their peer’s teaching.…with our friends [teaching], we feel comfortable and can ask doubt when needed. -
Teacher-centric synchronous learning
The teacher/instructor presents the information to the classroom while students listen and learn in real time.…we need a real teacher in front of us to make us understand things better.…we may miss some slides when we take lecture notes, and we will not have a continuation to the topic.
Discussion
Most medical colleges during the pandemic organised online classes, and students gained a fair amount of knowledge [22]. However, these e-classes were limited to traditional methods like lectures, practicals, and assessments [13, 14]. Some institutes shifted their online teaching to one of the learning management systems (LMS) like MOODLE to share their learning resources in an organised manner and to keep track of the student’s attendance and grades. Few institutes created online courses which encouraged active student participation [23]. MOODLE’s user-friendly interface and multiple options to create interactive content help in creating a student-centred education [12, 14, 23]. Few educators have designed e-modules in their respective disciplines, and others have designed case-based modules to improve the understanding among undergraduates [6–8, 14, 23]. We built the e-module around actual patients with a conceptual framework that includes multi-disciplinary integration and interactive multimedia resources to give a holistic approach to learning. Only a few studies have used actual patients in their e-learning platform [13, 24]. Using real patients in the teaching modules encourages situational learning for the students, which improves clinical decision-making skills. It encourages students to approach the clinical problems of the patients in their entirety [9, 10]. When students generate learning materials, its increases the depth and interactivity among learners. Studies have shown improved students performance with a positive attitude towards learning [18–21, 25, 26]. Students can address the baseline knowledge deficiencies more appropriately than faculty members [18].
Quantitative analysis between pre- and post-intervention tests proved the impact of learning by seminars and e-learning (Table 1). However, post-test scores between e-learning and seminar did not prove statistical significance. Hence, both interventions might result in comparable learning outcomes based on test scores. One of the limitations of this quantitative analysis is its low sample number (n = 60) which might have affected the statistical results. The other quantitative data on the responses to the feedback questionnaire after the first intervention, however, favoured e-module (Table 2). While the intervention test results proved the effectiveness of both learning techniques individually, they did not favour either e-module or seminar. However, the response to the e-module from the questionnaire reflects the learner’s perception and satisfaction towards e-learning. To further explore the learner’s thought process and explanation of the response, a Focus group discussion (FGD) was conducted after the second intervention. The qualitative research intended to understand the meaning behind the learner’s experience and factors that impacted the learning and to explain the variations in outcome responses of the two learning interventions.
We organised peer-led Fous group discussions to improve student participation in the discussion and to overcome teacher-student autonomy. On observing student-led FGD, the participants seemed relaxed (much giggling noticed) and shared their views honestly with their peers (e.g. ‘I just want to sleep during lectures’). However, some student moderators misinterpreted a few questions in the interview guide (e.g. asking e-learning-related questions in the seminar group) and could not explore a few questions in depth. Conducting more mock FGD sessions and detailed structuring of the ‘interview guide’ may improve the outcome.
A literature review on undergraduate e-learning highlighted its flexibility, easy accessibility, repetition and engagement. Cognitively, students attributed more knowledge and better understanding to e-learning content. However, the commonly perceived drawbacks were the lack of teacher interaction and internet connectivity issues [2, 11, 13, 18, 22]. Studies related to students’ seminars showed a positive effect on information acquisition, interaction, active learning and improved teaching effects [24–27]. The themes derived from the e-module and seminar in the present study also reiterate the same features. In addition, a patient-centric approach and interactive inquisitive quiz design engender the learners in e-module. Peer-driven learning and human interaction were the strengths of the student seminar. Though most data favoured e-module, students needed them as a reinforcement tool, while seminars were preferred as a learning tool to introduce new topics. Blending both techniques at the right time would benefit more students. A study by Popovic et al., too, arrived at the same conclusion [12].
Combining multiple methods (future and qualitative) and the data sources (test score, questionnaire, FGD), called ‘method & data triangulation’, were the strengths of the present study. The study’s limitations include a small sample size and fewer modules for analysis. In future, we will implement more such modules with added suggestions generated in this study. Though student-led FGD has its merits, the depth of the discussion necessary for a phenomenological study may not be adequate. Necessary FGD training and peer-led participatory FGD, where a student moderator also participates in discussion, may be tried in the future as they can explore different and deeper perspectives [28].
The structural framework of patient-centredness embedded with multimedia interactivity built in this e-module would help medical educators to design better engaging e-learning content in the future. Using actual patients in the e-learning platform generates interest and gives clinical context to solve real-world problems for the students [9, 10]. Learning material created by the students gives them ownership and motivates them to active, self-directed learning. As students encounter patients in their clinical posting, they can create patient-centric e-learning contents, which can later be validated by faculty. Such e-learning modules can supplement bedside teaching in future [10]. Clinically significant topics can be assigned to groups of students who can collaboratively work on the e-modules with their digitally native minds under a faculty’s guidance. This would save time where clinically experienced faculty can hold hands with the technically rich students to create a resourceful e-content to bridge the knowledge gap. However, periodic student and faculty development program for technical training in chosen e-platforms is necessary for the successful implementation of e-learning content. More research comparing various conceptual frameworks and multimedia tools in digital platforms is the way forward.
Conclusion
Students perceived ‘Patient-centric e-learning’ as an immersive learning experience of real-life scenarios with inquisitive, interactive and integrated content resulting in higher cognitive skills. Peer teaching in seminars created an interactive and friendly learning environment for basic subject learning. However, e-module and student seminars lack human interactivity and learners’ active participation, respectively. While both interventions have merits and demerits, they produce a significant learning outcome.‘The blended learning approach’ would benefit the students by utilising the best of both practices. Student involvement in creating learning content gives them ownership and encourages a learner-centred approach. Faculty supervision blended with students’ participation in designing educational tools can bridge the teacher’s experience and the learner’s engagement. In the future, student seminars can be used to impart basic knowledge blended with e-module for deeper enforcement.
Acknowledgements
This project was conducted under ‘ICMR-STS’, 2022. Dr Zayapragassarazan Z, Professor and Head of Medical Education Unit, JIPMER, for expert validation of feedback questionnaire. Dr Prabhakar, Dr Kalaimani, Dr Divyashanthi, Dr Janani, faculty and SR, JIPMER Karaikal — for the guidance with clinical content of the e-module. Sujey Gopalakrishnan, Keerthana Dharavath, Sreelakshmi Unnikrishnan, Vanshi Pahuja, Jaya Krishna Subramanian, Bindu Pranitha Vegesna, second-year MBBS students, JIPMER Karaikal — for seminar presentation, moderating FGD and helping with transcript preparation
Declarations
Ethics Approval and Consent to Participate
The study was undertaken after approval from the institutional ethical committee, and written consent was obtained from both the students and patients who participated in the study.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Karunaratne D, Karunaratne N, Wilmot J, Vincent T, Wright J, Mahmood N, Tang A, Sam AH, Reed M, Howlett D. An online teaching resource to support UK medical student education during the COVID-19 pandemic: a descriptive account. Adv Med Educ Pract. 2021;12:1317–1327. doi: 10.2147/AMEP.S337544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stoehr F, Müller L, Brady A, Trilla A, Mähringer-Kunz A, Hahn F, Düber C, Becker N, Wörns MA, Chapiro J, Hinrichs JB, Akata D, Ellmann S, Huisman M, Koff D, Brinkmann S, Bamberg F, Zimmermann O, Traikova NI, Marquardt JU, Chang DH, Rengier F, Auer TA, Emrich T, Muehler F, Schmidberger H, Baeßler B, Dos Santos DP, Kloeckner R. How COVID-19 kick-started online learning in medical education-The DigiMed study. PLoS ONE. 2021;16(9):e0257394. [DOI] [PMC free article] [PubMed]
- 3.John KJ. Learning management system and its role in the effective delivery of medical education. SBV Journal of Basic, Clinical and Applied Health Science [Internet]. 2022;5(4):105–6.
- 4.Dash S. Google classroom as a learning management system to teach biochemistry in a medical school. Biochem Mol Biol Educ. 2019;47(4):404–407. doi: 10.1002/bmb.21246. [DOI] [PubMed] [Google Scholar]
- 5.Zakaria N, Jamal A, Bisht S, Koppel C. Embedding a learning management system into an undergraduate medical informatics course in Saudi Arabia: lessons learned. Med 2 0. 2013;2(2):e13. [DOI] [PMC free article] [PubMed]
- 6.Villatoro T, Lackritz K, Chan JSY. Case-based asynchronous interactive modules in undergraduate medical education. Acad Pathol. 2019;6:2374289519884715. doi: 10.1177/2374289519884715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morgulis Y, Kumar RK, Lindeman R, Velan GM. Impact on learning of an e-learning module on leukaemia: a randomised controlled trial. BMC Med Educ. 2012;12:36. doi: 10.1186/1472-6920-12-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Velan GM, Killen MT, Dziegielewski M, Kumar RK. Development and evaluation of a computer-assisted learning module on glomerulonephritis for medical students. Med Teach. 2002;24(4):412–416. doi: 10.1080/01421590220145806. [DOI] [PubMed] [Google Scholar]
- 9.Peacock JG, Grande JP. Patient exposure in the basic science classroom enhances differential diagnosis formation and clinical decision-making. PeerJ. 2015;3:e809. [DOI] [PMC free article] [PubMed]
- 10.Selzer R, Tallentire VR, Foley F. The effects of utilizing a near-patient e-learning tool on medical student learning. Med Teach. 2015;37(6):558–565. doi: 10.3109/0142159X.2014.955842. [DOI] [PubMed] [Google Scholar]
- 11.Dhir SK, Verma D, Batta M, Mishra D. E-learning in medical education in India. Indian Pediatr. 2017;54(10):871–877. doi: 10.1007/s13312-017-1152-9. [DOI] [PubMed] [Google Scholar]
- 12.Popovic N, Popovic T, Rovcanin Dragovic I, Cmiljanic O. A MOODLE-based blended learning solution for physiology education in Montenegro: a case study. Adv Physiol Educ. 2018;42(1):111–117. doi: 10.1152/advan.00155.2017. [DOI] [PubMed] [Google Scholar]
- 13.Mukherjee M. E-learning in pathology education: A narrative review and Personal Perspective. EMJ Innov. 2020;4(1):48–56. doi: 10.33590/emjinnov/18-00093. [DOI] [Google Scholar]
- 14.Back DA, Behringer F, Haberstroh N, Ehlers JP, Sostmann K, Peters H. Learning management system and e-learning tools: an experience of medical students' usage and expectations. Int J Med Educ. 2016;20(7):267–273. doi: 10.5116/ijme.57a5.f0f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hulke SM, Wakode SL, Thakare AE, Parashar R, Bharshnakar RN, Joshi A, Vaidya YP. Perception of e-learning in medical students and faculty during COVID time: A study based on a questionnaire-based survey. J Educ Health Promot. 2022;11:139. doi: 10.4103/jehp.jehp_655_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delungahawatta T, Dunne SS, Hyde S, Halpenny L, McGrath D, O'Regan A, Dunne CP. Advances in e-learning in undergraduate clinical medicine: a systematic review. BMC Med Educ. 2022;22:711. doi: 10.1186/s12909-022-03773-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prabu Kumar A, Omprakash A, Chokkalingam Mani PK, Kuppusamy M, Wael D, Sathiyasekaran BWC, Vijayaraghavan PV, Ramasamy P. E-learning and E-modules in medical education-A SOAR analysis using perception of undergraduate students. PLoS ONE. 2023;18(5):e0284882. [DOI] [PMC free article] [PubMed]
- 18.Isaacs AN, Nisly S, Walton A. Student-generated e-learning for clinical education. Clin Teach. 2017;14(2):129–133. doi: 10.1111/tct.12526. [DOI] [PubMed] [Google Scholar]
- 19.Gooi AC, Sommerfeld CS. Medical school 2.0: How we developed a student-generated question bank using small group learning. Med Teach. 2015;37(10):892–6. [DOI] [PubMed]
- 20.Gill P, Kitney L, Kozan D, Lewis M. Online learning in paediatrics: a student-led web-based learning modality. Clin Teach. 2010;7(1):53–57. doi: 10.1111/j.1743-498X.2009.00337.x. [DOI] [PubMed] [Google Scholar]
- 21.Black VH, Smith PR. Increasing active student participation in histology. Anat Rec B New Anat. 2004;278(1):14–17. doi: 10.1002/ar.b.20017. [DOI] [PubMed] [Google Scholar]
- 22.Tashkandi E. E-Learning for Undergraduate Medical Students. Adv Med Educ Pract. 2021;12:665–674. doi: 10.2147/AMEP.S314509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasan HF, Nat M, Vanduhe VZ. Gamified collaborative environment in MOODLE. IEEE Access. 2019;7:89833–89844. doi: 10.1109/ACCESS.2019.2926622. [DOI] [Google Scholar]
- 24.Yeni K, Tülek Z, Çavuşoğlu A, Bebek N, Gürses C, Baykan B, Gökyiğit A. The effect of a seminar on medical students’ information acquisition of and attitudes toward epilepsy. Epilepsy Behav. 2021;116:107720. [DOI] [PubMed]
- 25.Vij V, Chitnis P, Mendhurwar S. Summative program evaluation of a Student-Led Seminar Series in the subject of physiology: an outcome-based study. Korean J Med Educ. 2022;34(1):41–48. doi: 10.3946/kjme.2022.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeng HL, Chen DX, Li Q, Wang XY. Effects of seminar teaching method versus lecture-based learning in medical education: A meta-analysis of randomized controlled trials. Med Teach. 2020;42(12):1343–1349. doi: 10.1080/0142159X.2020.1805100. [DOI] [PubMed] [Google Scholar]
- 27.Asghar S, Rahman S, Shaikh S, Aslam S, Karania T. Medical students' perspective on 'effects of seminar teaching method versus lecture-based learning in medical education: A meta-analysis of randomized controlled trials'. Med Teach. 2021;43(9):1100–1101. doi: 10.1080/0142159X.2021.1873928. [DOI] [PubMed] [Google Scholar]
- 28.Djohari N, Higham R. Peer-led focus groups as ‘dialogic spaces’ for exploring young people’s evolving values. Camb J Educ. 2020;50(5):657–672. doi: 10.1080/0305764X.2020.1754763. [DOI] [Google Scholar]
- 29.Palappallil DS, Sushama J, Ramnath SN. Effectiveness of modified seminars as a teaching-learning method in pharmacology. Int J Appl Basic Med Res. 2016;6(3):195–200. doi: 10.4103/2229-516X.186971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iqbal SP, Rafi S, Rahman M. Student seminar on smoking: A novel way to introduce different perspectives on smoking to medical students. J Res Med Sci. 2013;18(3):245–251. [PMC free article] [PubMed] [Google Scholar]
- 31.Tenny S, Brannan JM, Brannan GD. Qualitative Study. 2022 Sep 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.