Abstract
Women with either breast cancer (BC) or ovarian cancer (OC) have a 1.5–2 times higher risk of developing the other. Discerning discrete primaries versus metastases from either can be challenging. Clinico-pathological and outcome details of patients diagnosed with both BC and OC from December 1994 to August 2018 were retrospectively evaluated at a single tertiary cancer centre. We report the pattern of presentation and recurrences with case-based illustrations. Out of 139 patients, presentation was BC-first in 66.2%, OC-first in 24.5% and synchronous cancers (SC) in 9.3% of women. The median age at diagnosis in BC-first, OC-first and SC was 42 years, 48 years and 49 years, respectively. The most common histological subtype was invasive breast carcinoma-no special type (74.8%) in BC and serous cystadenocarcinoma (81.3%) in OC. BC presented at an early stage in 67.6% while OC presented at an advanced stage in 48.2% of patients. Germline mutation results were available in 82% with 61.4% of the cohort exhibiting a mutation- BRCA1 mutation being the most common. The median time to development of second cancer was 77.4 months and 39.4 months in BC-first and OC-first, respectively. At a median follow-up of 9.47 years, disease-free survival was 32.6%, 32.4% and 30.8% in BC-first, OC-first and SC, respectively (p < 0.001). In hereditary breast and ovarian cancer, BC-first patients have a better prognosis while synchronous malignancies have worse oncological outcomes. Deaths are mainly due to OC progression. Appropriate surveillance and prophylactic intervention in young patients with breast cancer may improve overall outcomes.
Keywords: Hereditary breast and ovarian cancers, Survival outcomes, Germline profiling, Synchronous and metachronous breast and ovarian cancer
Synopsis
We report the findings of 139 women of metachronous (second primary tumours detected > 6 months after index cancer) and synchronous (second primary cancers detected within 6 months of primary tumour) breast and ovarian cancers. Breast cancer-first was the most common presentation. Germline mutation was identified in 61% of tested patients, and BRCA1 was the most common mutation. The prognosis was better in the BC-first group as compared to OC-first group or synchronous presentation. Ovarian cancer was diagnosed at an advanced stage in majority of cases, and most deaths were due to ovarian cancer progression. A high index of clinical suspicion, serum tumour markers, imaging and pathological assessment help clinch the diagnosis of metastases versus discrete primaries.
Background
The most common cancer among women globally and in India is breast cancer (BC) [1, 2]. Epithelial ovarian cancer (OC) accounts for 47% of all female genital tract cancer deaths and is also the most common second primary in patients with primary BC [3, 4]. Studies worldwide have reported that even in the absence of family history, 10% of women with BC and 15–20% of women with OC have a possible germline mutation [5, 6]. This estimate rises to as high as 80% in the presence of significant family history [7]. Classically, synchronous tumours are defined as second primary cancers detected within 6 months of primary tumour detection while metachronous tumours have been defined as second primary tumours detected more than 6 months after diagnosis of the index cancer. Women with BC have a twofold higher risk of developing subsequent OC while women with OC have a 1.5 times higher risk of developing a subsequent BC [8–10]. Age < 50 years at the time of BC diagnosis is the factor associated with the highest risk of metachronous OC [11]. The most common genetic mutation associated with hereditary breast and ovarian cancer (HBOC) is in the BRCA1 gene [12]. BC and OC presenting as a synchronous or metachronous tumour often pose a diagnostic dilemma with respect to diagnosing a second primary versus a metastatic deposit from the other [13]. Differentiating between the two clinical scenarios is important for planning further management. Reaching a pertinent diagnosis requires a high index of clinical suspicion, use of appropriate tumour markers, radiological imaging, as well as biopsies with histomorphological and immunohistochemical (IHC) evaluation. In the background of this impediment, we aimed to study the patterns of presentation and oncological outcomes of women diagnosed with both BC and OC, with an emphasis on case-based illustrations for diagnostic workflow.
Materials and Methods
This study reviewed a database of patients who presented with both BC and OC in either a synchronous or metachronous manner at a single high-volume oncology institution, Tata Memorial Centre, Mumbai, between 1994 and 2018. Following Institutional Ethics Committee approval, demographic data, clinico-pathological characteristics and disease-related outcomes were obtained from hospital electronic medical records. BC staging followed the 8th edition American Joint Committee on Cancer staging system while OC staging followed the 2018 International Federation of Gynecology and Obstetrics staging system. Germline mutation results were obtained from the clinical genetics laboratory at the Advanced Centre for Treatment, Research and Education in Cancer, Navi Mumbai. Patients were divided into three groups based on the sequence of diagnosis: group 1, BC-first (BC predated OC); group 2, OC-first (OC predated BC); and group 3, SC (synchronous BC and OC).
Pathology
Diagnostic samples were commonly obtained from biopsies of either breast lesions or image-guided or open biopsies, as applicable, from abdomino-pelvic disease as well as fluid cytology and cell blocks of ascitic and/or pleural fluid. Synchronous, metachronous or metastatic disease was further confirmed using a panel of IHC markers, PAX8 and WT1 for OC, and oestrogen receptor (ER), progesterone receptor (PR), HER2 and GATA3 for BC. Additional markers such as CK7, CK20, TTF1 and CDX2 were performed to rule out metastatic disease from the lung or GI tract as and when required.
Germline Mutation Testing
All patients with synchronous or metachronous OC and BC were referred to the clinical cancer genetics unit for genetic counselling and germline profiling. Germline BRCA1/2 hot spot mutations were tested using Sanger sequencing of exons harbouring common geo-ethnic specific mutations. When hot spot mutations were negative, full gene testing of all coding exons of BRCA1/2 was performed by Sanger sequencing or by next-generation sequencing on the Illumina platform.
Statistical Analysis
Data on demographics and treatment were reported as numbers and percentages. Study outcomes including overall survival (OS) and disease-free survival (DFS), were each measured from the time of diagnosis. OS was the interval between diagnosis and death while DFS was the interval between diagnosis and first progression of disease. DFS and OS were estimated using Kaplan–Meier curves and log-rank test. Data was analysed using SPSS version 25.0 for Windows (SPSS, Chicago, IL).
Results
Clinico-pathological Characteristics
A total of 139 patients were included in the study, and the median age at diagnosis was 45 years (23–77 years). The presentation was BC-first in 92 women (66.2%), OC-first in 34 women (24.5%) and SC in 13 women (9.3%). The median age at diagnosis was 42 years, 48 years and 49 years in women who presented with BC-first, OC-first and SC, respectively. Table 1 details the demographic and disease characteristics of patients in this study.
Table 1.
Clinico-pathological characteristics and management details of 139 patients
| Clinico-pathological feature | BC first, N = 92 (%) | OC first, N = 34 (%) | Synchronous presentation, N = 13 (%) | Overall, N = 139 (%) |
|---|---|---|---|---|
| Age (median) years | 42 (23–76) | 48 (30–69) | 49 (38–66) | 45 (23–77) |
| Stage at presentation of BC | ||||
| EBC | 69 (75) | 20 (58.7) | 5 (38.5) | 94 (67.6) |
| LABC | 9 (9.8) | 8 (23.5) | 6 (46.2) | 23 (16.6) |
| MBC | 0 (0) | 3 (8.8) | 1 (7.6) | 4 (2.9) |
| NK | 14 (15.2) | 3 | 1 (7.7) | 18 (12.9) |
| Histological type of BC | ||||
| IBC-NOS | 73 (79.3) | 24 (70.6) | 7 (53.9) | 104 (74.8) |
| DCIS | 2 (2.2) | 3 (8.8) | 0 | 5 (3.6) |
| Other subtypes | 1 (1) | 1 (3) | 0 | 2 (1.4) |
| NK | 16 (17.5) | 6 (17.6) | 6 (46.1) | 28 (20.2) |
| Histological grade of BC | ||||
| Grades 1–2 | 8 (8.8) | 3 (8.8) | 0 | 11 (7.9) |
| Grade 3 | 58 (63) | 22 (64.7) | 11 (84.6) | 88 (63.3) |
| NK | 26 (28.2) | 9 (26.5) | 2 (15.4) | 40 (28.8) |
| Nodal stage of BC | ||||
| Node negative | 41 (44.6) | 14 (41.2) | 6 (46.2) | 61 (43.9) |
| Node positive | 23 (25) | 10 (29.4) | 3 (23.1) | 36 (25.9) |
| NK/NA | 28 (30.4) | 10 (29.4) | 4 (30.7) | 42 (30.2) |
| Molecular subtype of BC | ||||
| HR + /HER2 + | 1 (1.1) | 1 (2.9) | 0 | 2 (1.3) |
| HR + /HER2 equivocal | 2 (2.1) | 2 (5.9) | 0 | 4 (2.8) |
| HR + /HER2 − | 11 (12) | 15 (44.1) | 4 (30.8) | 30 (21.6) |
| HR − /HER2 + | 2 (2.1) | 1 (2.9) | 0 | 3 (2.2) |
| TNBC | 39 (42.4) | 13 (38.2) | 8 (61.5) | 60 (43.2) |
| NK | 37 (40.1) | 2 | 1 (7.7) | 40 (28.8) |
| Type of surgery for BC | ||||
| MRM | 41 (44.6) | 13 (38.2) | 7 (53.8) | 61 (43.9) |
| BCS | 48 (52.2) | 13 (38.2) | 2 (15.4) | 63 (45.3) |
| NK/NA (surgery not done) | 3 (3.2) | 8 (23.6) | 4 (30.8) | 15 (10.8) |
| Chemotherapy for BC | ||||
| Neoadjuvant | 8 (8.7) | 6 (17.6) | 2 (15.4) | 16 (11.6) |
| Adjuvant | 53 (57.6) | 9 (26.5) | 2 (15.4) | 64 (46) |
| Both neoadjuvant and adjuvant | 11 (11.9) | 6 (17.6) | 6 (46.2) | 23 (16.6) |
| Palliative | 0 | 0 | 2 (15.4) | 2 (1.4) |
| NK/NA | 20 (21.8) | 13 (38.2) | 1 (7.6) | 34 (24.4) |
| Radiation therapy for BC | ||||
| Received | 55 (59.8) | 15 (44.2) | 7 (53.8) | 77 (55.4) |
| Not received | 20 (21.7) | 11 (32.3) | 1 (7.7) | 32 (23) |
| NK/NA | 17 (18.5) | 8 (23.5) | 5 (38.5) | 30 (21.6) |
| Stage at presentation of OC | ||||
| Early (FIGO 1, 2) | 11 (11.9) | 8 (23.5) | 5 (38.5) | 24 (17.3) |
| Late (FIGO 3 and 4) | 47 (51.1) | 15 (44.1) | 5 (38.5) | 67 (48.2) |
| NK/NA | 34 (37) | 11 (32.4) | 3 (23) | 48 (34.5) |
| Histological type of OC | ||||
| Serous | 76 (85.9) | 28 (82.5) | 9 (69.2) | 113 (81.3) |
| Mucinous | 0 | 1 (2.9) | 0 | 1 (0.7) |
| Clear cell | 1 (1) | 0 | 0 | 1 (0.7) |
| Endometrioid | 5 (5.4) | 2 (5.9) | 0 | 7 (5) |
| Poorly differentiated | 3 (3.2) | 1 (2.9) | 1 (7.7) | 5 (3.6) |
| Benign | 3 (3.2) | 1 (2.9) | 0 | 4 (2.9) |
| NK | 4 (4.3) | 1 (2.9) | 3 (23.1) | 8 (5.8) |
| Histological grade of OC | ||||
| Low grade (p53 low) | 6 (6.5) | 5 (14.7) | 1 (7.7) | 12 (8.6) |
| High grade (p53 high) | 68 (74) | 25 (73.5) | 9 (69.3) | 102 (73.4) |
| NK | 19 (20.5) | 3 ((8.8) | 3 (23) | 25 (18) |
| CA-125, U/mL | ||||
| Median | 1369 | 205 | 305 | 882 |
| Mean | 2540 | 1186 | 645 | 2027 |
| IQR | 8.9–24,275 | 5–7222 | 3.5–3541 | 3.5–24,275 |
| Type of surgery for OC | ||||
| Primary cytoreduction | 13 (14.1) | 11 (32.3) | 1 (7.7) | 25 (18) |
| Interval cytoreduction | 67 (72.8) | 19 (55.9) | 8 (61.5) | 94 (67.6) |
| NK/NA | 12 (13.1) | 3 (8.8) | 7 (53.8) | 20 (14.4) |
| Chemotherapy for OC | ||||
| Neoadjuvant or adjuvant chemotherapy | 69 (75.1) | 25 (73.5) | 9 (69.2) | 103 (74.1) |
| Palliative | 4 (4.3) | 0 | 3 (23.1) | 7 (5.1) |
| NK/NA | 19 (20.6) | 9 (26.5) | 1 (7.7) | 29 (20.8) |
| Contralateral BC | ||||
| Yes | 17 (18.5) | 2 (5.9) | 1 (7.7) | 20 (14.3) |
| No | 68 (74) | 29 (85.3) | 11 (84.6) | 108 (77.7) |
| NK | 7 (7.5) | 3 (8.8) | 1 (7.7) | 11 (8) |
BC breast cancer, OC ovarian cancer, IBC-NOS invasive breast carcinoma-not otherwise specified, DCIS ductal carcinoma in situ, EBC early breast cancer, LABC locally advanced breast cancer, MBC metastatic breast cancer, TNBC triple-negative breast cancer, MRM modified radical mastectomy, BCS breast conservation surgery, NK not known, NA not applicable
The most common histological subtype of BC was invasive breast carcinoma-not otherwise specified (NST) in 74.8% patients followed by ductal carcinoma in situ (DCIS) in 3.5% and other rarer subtypes (such as papillary carcinoma) in 1.4% of patients. The most common molecular subtype was triple-negative breast cancer (TNBC) in 43.2% followed by hormone receptor–positive BC in 21.6%, and the majority (63.3%) had grade 3 tumours. BC was diagnosed at an early stage (tumours < 5 cm and without regional lymphadenopathy) in 67.6%, locally advanced (tumours > 5 cm with regional lymphadenopathy) in 16.5% and metastatic in 2.8%.
The most common histological subtype of OC was serous cystadenocarcinoma (81.3%) followed by endometrioid type (5%) with 73.4% of women harbouring high-grade disease. OC was diagnosed at stages 1–2 in 17.2% and stages 3–4 in 48.2%. At the time of diagnosis of OC, the median serum CA-125 levels were 1369 U/mL (8.9–24,275 U/mL), 205 U/mL (5–7222 U/mL) and 308 U/mL (3.5–3541 U/mL) in the cohort of patients with BC-first, OC-first and SC, respectively.
All patients were treated following discussion in a multidisciplinary team. Surgery for BC comprised breast conservation surgery (BCS) in 45.3% and mastectomy in 43.8% followed by chemo-endocrine therapy and radiotherapy as per institutional protocols. For patients with OC, optimal cytoreduction was attained in all patients; 18% underwent primary debulking surgery, and 67.6% had interval debulking surgery (IDS); 74.1% of patients received platinum-based chemotherapy in the adjuvant and/or neoadjuvant setting. Treatment details are provided in Table 1.
Germline Mutation Profiling
Of the 139 patients, 53 (38.1%) had a first-degree relative with a history of cancer while 7 (5%) had a second-degree relative with a history of cancer. The most common family history was either BC or OC. Forty-nine patients (35.3%) had no family history of cancer while 30 patients (21.6%) had no family history available. Germline mutations were tested for in 114 (82%) patients, and a mutation was identified in 70 patients (61.4%). BRCA1 mutation was identified in 88.6% and BRCA2 in 5.7%. Universal geo-ethnic specific hotspot mutation testing was the most common method of testing used in 61.4% (70/114) of patients. The results of genetic mutation profiling are summarized in Table 2.
Table 2.
Genetic mutation profiling data of 139 patients
| BC first, N = 92 | OC first, N = 34 | Synchronous presentation, N = 13 | Overall, N = 139 | |
|---|---|---|---|---|
| Family history (N = 139) | ||||
| First-degree relative | 35 (38) | 12 (35.3) | 6 (46.2) | 53 (38.1) |
| Second-degree relative | 6 (6.5) | 1 (2.9) | 0 | 7 (5) |
| No family history | 28 (30.5) | 14 (38.2) | 7 (53.8) | 49 (35.3) |
| NK | 23 (25) | 7 (20.6) | 0 | 30 (21.6) |
| Genetic testing done (N = 114) | ||||
| Yes | 79 (85.9) | 27 (79.4) | 8 (61.5) | 114 (82) |
| No | 13 (14.1) | 7 (20.6) | 5 (38.5) | 25 (18) |
| Mutation identified (N = 114) | ||||
| Yes | 55 (59.8) | 11 (32.4) | 4 (30) | 70 (61.4) |
| No | 24 (26) | 15 (44) | 5 (38.5) | 44 (38.6) |
| Not done | 13 (14.1) | 7 (20.6) | 5 (38.5) | 25 (18) |
| Type of genetic testing (N = 114) | ||||
| Hot spot mutation alone | 47 (51.1) | 16 (47.1) | 7 (53.8) | 70 (61.4) |
| Full gene ± MLPA | 20 (21.8) | 3 (8.8) | 1 (7.7) | 24 (21) |
| Hereditary cancer panel | 12 (11.9) | 8 (23.5) | 0 | 20 (17.6) |
| Mutation type (N = 70) | ||||
| BRCA1 | 52 (94.6) | 6 (54.5) | 4 (100) | 62 (88.6) |
| BRCA2 | 1 (1.8) | 3 (27.3) | 0 | 4 (5.7) |
| Others (Tp53, MSH, RAD51) | 2 (3.6) | 2 (18.2) | 0 | 4 (5.7) |
Long-Term Outcome
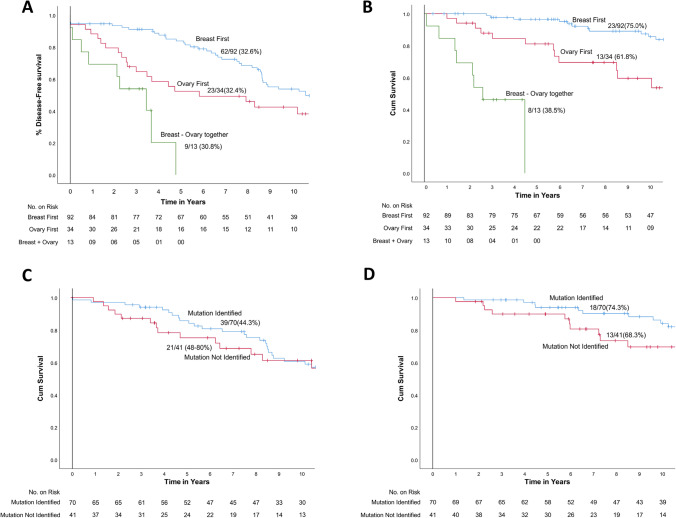
The median DFS was 10.4 years, 5.7 years and 3.4 years, and the median OS was 21 years, 10.6 years and 2.6 years in BC-first, OC-first and SC, respectively. The median time to development of second cancer was 77.4 months in those with BC-first and 39.4 months in those with OC-first. At a median follow-up of 9.47 years, DFS was 32.6%, 32.4% and 30.8% in BC-first, OC-first and SC, respectively (p < 0.001). The corresponding OS was 69.6%, 58.8% and 38.5% in BC-first, OC-first and SC, respectively (p < 0.01) (Fig. 1A, B). At 5 years, the DFS and OS were 88.1% and 95.2% in the BC-first cohort, and 58.2% and 78.5% in the OC-first cohort respectively (Table 3).
Fig. 1.
Survival outcome. A Disease-free survival and B overall survival with respect to BC-first, OC-first and synchronous presentation (139 patients) and C disease-free survival and D overall survival with respect to the presence or absence of germline mutation (111 patients)
Table 3.
Disease-related outcome of 139 patients
| BC first | OC first | Synchronous presentation | |
|---|---|---|---|
| DFS (%) | 32.6 | 32.4 | 32 |
| OS (%) | 69.6 | 58.8 | 38.5 |
| Median time to development of second cancer (months) | 77.4 | 39.4 | – |
| 3-year DFS, % | 91.1 (85.22–96.98) | 64.6 (48.53–80.67) | 53.8 (26.75–80.65) |
| 5-year DFS, % | 88.1 (81.24–94.96) | 58.2 (41.54–74.86) | – |
| 3-year OS, % | 97.7 (94.56–1.01) | 85.0 (72.85–97.15) | 46.2 (19.15–73.25) |
| 5-year OS, % | 95.2 (90.69–99.71) | 78.5 (64.39–92.61) | – |
In the entire study group, 50 deaths were recorded; 41 patients died due to progression of OC, six died due to progression of BC and two died from unknown causes (Table 4). During the follow-up period, 14.4% of women developed contralateral BC. Of the 111 patients who underwent germline mutation testing, the presence or absence of an identified mutation revealed no difference in DFS (44.3% and 44.8%, p = 0.21) or OS (74.3% and 68.3%, p = 0.08) (Fig. 1C, D).
Table 4.
Cause of death
| BC first, N = 92 | OC first, N = 34 | Synchronous presentation, N = 13 | Total, N = 139 | |
|---|---|---|---|---|
| Died due to BC | 1 | 4 | 1 | 6 |
| Died due to OC | 25 | 9 | 7 | 41 |
| Died due to other cause | 2 | 1 | 0 | 3 |
| Total number of deaths | 28 | 14 | 8 | 50 |
On univariate Cox regression analysis, advanced stage at presentation of BC (HR 2.10, p < 0.005), absence of germline mutation (HR 1.64, p = 0.035), clinical presentation with OC-first (HR-1.8 [p = 0.02]) and presentation with synchronous cancers (HR − 6.4 [p < 0.001]), resulted in a significantly worse DFS. However, on multivariate Cox regression analysis, none of the factors were significantly associated with DFS (Table 5).
Table 5.
Cox regression univariate and multivariate analyses of prognostic factors affecting DFS in HBOC
| Category | Univariate | Cox regression, multivariate | |||||
|---|---|---|---|---|---|---|---|
| No. of events | Survival | HR | p value | HR | 95% CI | p value | |
| Age | – | – | – | – | 1.02 | 0.99–1.05 | 0.29 |
| Stage of ovarian cancer | |||||||
| Early | 9/24 | 62.5 | 1 | ||||
| Advanced | 49/67 | 26.9 | 1.93 | 0.06 | |||
| Stage of breast cancer | |||||||
| Early | 60/94 | 36.2 | 1 | 1 | |||
| Advanced | 21/27 | 22.2 | 2.10 | 0.005 | 1.57 | 0.84–2.99 | 0.17 |
| Grade of ovarian cancer | |||||||
| Low | 8/12 | 33.3 | 1 | ||||
| High | 69/102 | 32.4 | 0.77 | 0.48 | |||
| Grade of breast cancer | |||||||
| Low | 9/11 | 18.2 | 1 | ||||
| High | 56/88 | 36.4 | 0.90 | 0.76 | |||
| Mutation status | |||||||
| Present | 47/70 | 32.9 | 1 | ||||
| Absent | 31/43 | 27.9 | 1.64 | 0.035 | 1.20 | 0.71–2.04 | 0.51 |
| Sequence of malignancies | |||||||
| BC-first | 62/92 | 32.6 | 1 | 1 | |||
| OC-first | 23/34 | 32.4 | 1.8 | 0.02 | 1.32 | 0.70–2.51 | 0.40 |
| Synchronous malignancies | 9/13 | 30.8 | 6.4 | < 0.001 | 2.84 | 0.89–9.10 | 0.08 |
We describe a few clinical case scenarios here where diagnostic dilemmas were resolved by appropriate pathological evaluation.
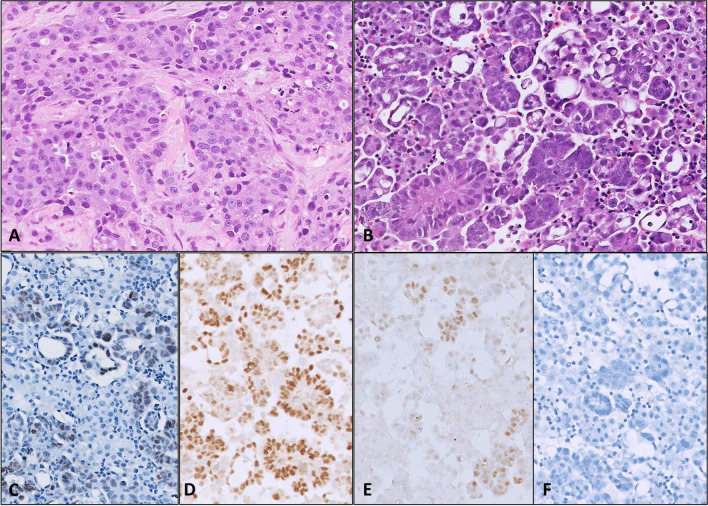
Diagnosis of OC After BC (Fig. 2)
Fig. 2.
Microphotographs of case scenario 1, with initial diagnosis of BC (A, HE × 200). Ascitic fluid cell block 6 years later showed a metastatic papillary adenocarcinoma (B, HE × 200), which was positive for PAX8 (C, × 200), WT1 (D, × 200) and ER (E, × 200), while negative for GATA3 (F), confirming ovarian origin
A 52-year-old postmenopausal lady was diagnosed with TNBC. Her mother had died of an unknown cancer at a young age. She was treated with anthracycline-based neoadjuvant chemotherapy (NACT) followed by surgery and radiotherapy. Six years later, she had an ascitic fluid cell block which revealed a high-grade serous ovarian adenocarcinoma. She received platinum-based NACT followed by IDS and adjuvant chemotherapy. She had a pathogenic BRCA1 mutation.
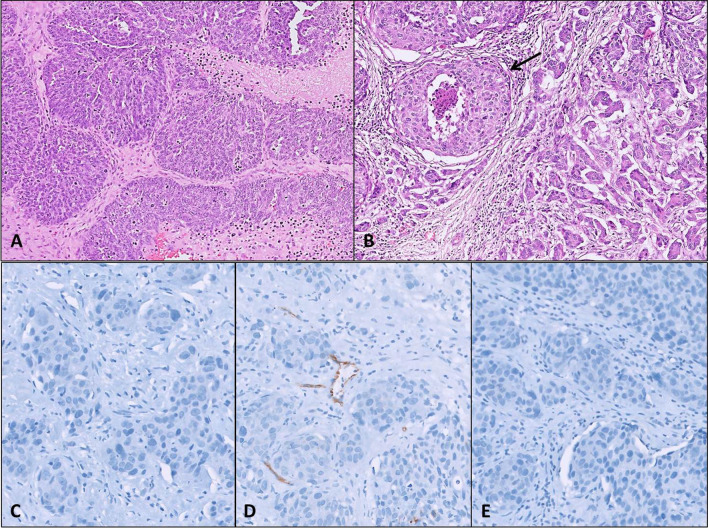
Diagnosis of BC After OC (Fig. 3)
Fig. 3.
Microphotographs of case scenario 2, showing a section from the initial high-grade papillary adenocarcinoma of ovary (A, HE × 200). Subsequent breast biopsy 3 years later showed a BC (B, HE × 200) which was triple negative (not shown), negative for PAX8 (C, × 200) and WT1 (D, × 200) and negative for GATA3 (E, × 200). Difference in morphology between initial OC and BC, along with the presence of DCIS in BC (B, arrow) helped confirm the second breast primary
A 51-year-old premenopausal lady with no significant family history was diagnosed with advanced serous ovarian adenocarcinoma. She underwent a primary debulking surgery followed by platinum-based adjuvant chemotherapy. After 2 years, she was diagnosed with a locally advanced TNBC. She received anthracycline and taxane–based NACT, followed by a left mastectomy and adjuvant radiotherapy. Her germline test revealed a BRCA1 mutation.
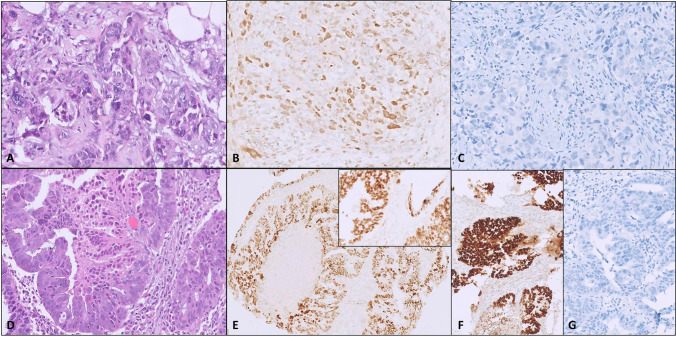
Synchronous Diagnoses of BC and OC (Fig. 4)
Fig. 4.
Microphotographs of case scenario 3 with synchronous presentation of BC (A, HE × 200), which was triple negative (not shown), and positive for GATA3 (B, × 200), while negative for PAX8 (C, × 200), along with high-grade serous OC diagnosed on pelvic biopsy (D, HE × 200), which was positive for PAX8 (E, × 100) and WT1 (E, inset, × 200), as well as p53 (F, × 100), while negative for GATA3 (G, × 200)
A 59-year-old postmenopausal lady was diagnosed with bilateral TNBC and an adnexal mass. A biopsy from the adnexal mass revealed a high-grade serous ovarian adenocarcinoma (p53 positive). She received platinum-based NACT followed by bilateral BCS and simultaneous IDS. She received further adjuvant chemotherapy and radiation therapy. Since the adnexal tumour was strongly ER + , the patient was started on an aromatase inhibitor. She had a pathogenic BRCA1 mutation.
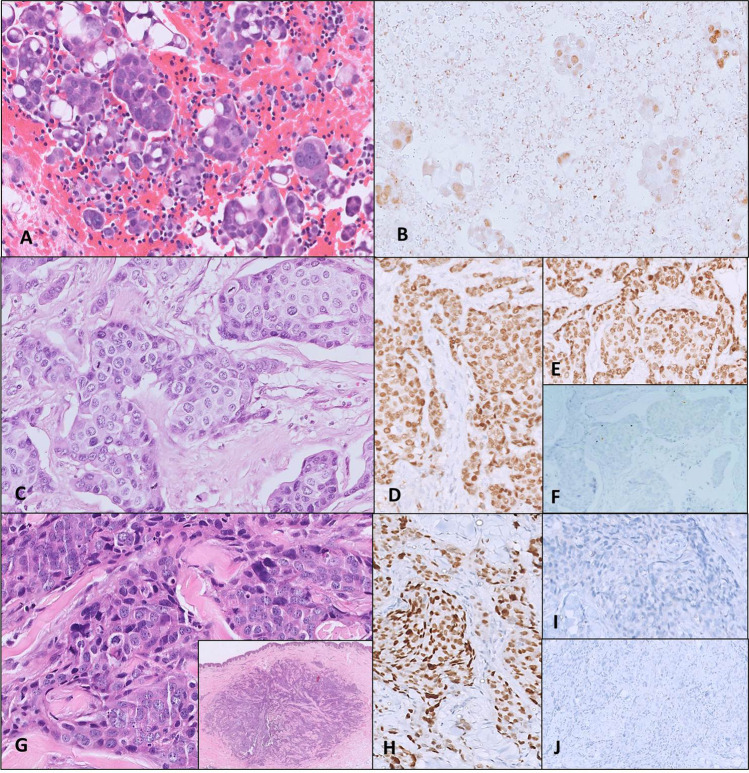
Metachronous BC and OC with Progression of Ovarian Metastasis to Breast (Fig. 5)
Fig. 5.
Microphotographs of case scenario 4 with initial presentation of serous OC diagnosed on ascitic fluid cell block (A, HE, × 200), which was positive for PAX8 (B, × 200). Right breast biopsy a year later showed a BC (C, × 200), which was positive for GATA3 (D, × 200) and ER (E, × 200), while negative for PAX8 (F, × 200). Two years later, biopsy of a new right breast nodule showed a dermal tumour deposit (G, inset, HE × 50), with a poorly differentiated high-grade morphology (G, HE, × 200), which was positive for PAX8 (H, × 200) and negative for GATA3 (I, × 200) and ER (J, × 200), confirming metastasis of OC to breast
A 47-year-old premenopausal lady with a strong family history was diagnosed with advanced high-grade serous ovarian adenocarcinoma. She received NACT, underwent IDS and was treated with adjuvant chemotherapy. A year later, she developed a right breast lump and was diagnosed with BC. Following BCS, she had anthracycline-based adjuvant chemotherapy, adjuvant radiation therapy and maintenance hormonal therapy. Two years later, she presented with recurrent ovarian malignancy and was rechallenged with platinum-based chemotherapy. A few months later, the patient presented with a breast nodule which was found to be of ovarian origin (negative for GATA-3 and ER and positive for PAX-8) and was treated with additional chemotherapy. Her genetic test did not reveal any mutation.
Discussion
HBOC is a well-known entity with paucity of literature describing disease presentation, diagnoses and patterns of failure. In metachronous setting, our series found BC-first (66.2%) to be the commonest presentation with 9% presenting as SC. An Italian study documented the same trend with 75% BC-first and 9% synchronous presentations [14]. The age at diagnosis of BC is usually a decade younger than age at diagnosis of OC. In the HBOC cohort similarly, the age at diagnosis of BC predates that of OC [15]. Metachronous or synchronous presentations of HBOC pose diagnostic challenge with respect to discerning two discrete primaries versus metastatic disease. In turn, a pertinent diagnosis is necessary to guide treatment intent [16, 17]. Krukenberg tumours of ovary from a breast primary are common; however, ovarian metastases to the breast have been described in the literature, albeit less frequently [18, 19]. Isolated Krukenberg tumours cause a diagnostic dilemma, especially when associated with early breast cancer. While primary OC tends to present with an ovarian mass, ascites, omental deposits, pleural effusion and markedly raised CA-125 levels, metastases from BC to the ovary tend to be smaller in size, bilateral and often devoid of peritoneal disease. Isolated metastasis from OC to the breast parenchyma, axilla and supraclavicular fossa is known to occur but is uncommon [20–22].
Our data showed a higher prevalence of TNBC and serous cystadenocarcinoma of the ovary in HBOC patients like most prior published series [14]. We employed a complete IHC panel with morphological analysis to prove the presence of two separate primaries [23, 24]. BC is positive for GATA-3 and mammaglobin while serous OC is positive for PAX8 and WT1 [25]. Hormone receptors (ER and PR) can be positive in both OC and BC depending on tumour subtype. GATA3, although a highly sensitive and specific marker for BC, requires careful interpretation as it may be positive in a variety of other tumours, although unusually in epithelial ovarian tumours [25–27]. In addition, mammaglobin, and less frequently GATA3, may be negative in TNBC [28]. The IHC work-up should include a panel, rather than isolated markers, as many BCs in HBOC are TNBC. Identification of an associated DCIS in a breast biopsy favours diagnosis of BC. The majority of OC and BC show similar cytokeratin expression—strong CK7 and a lack of CK20 immunoreactivity. This limits CK7/20 diagnostic utility to differentiate between OC and BC, but is useful to substantiate the diagnosis of a breast primary in GATA3-negative TNBC, concomitant with negative PAX8 and WT1 immunoreactivity. In lymph node or pleural/peritoneal biopsies/fluid cell blocks, immunoreactivity of other relevant markers (such as TTF1 and Napsin A to exclude lung origin tumours, and CDX2 and SATB2 to exclude GI origin tumours) helps exclude metastases from other organ. Ultimately, correlating patterns of clinical presentation with radiological findings, tumour markers, histopathology, IHC and multidisciplinary team meeting discussion are key to increasing diagnostic accuracy.
BRCA mutations account for approximately half of all inherited HBOC [14]. We observed an overall 50.4% germline mutation positive rate (61% in tested patients), with BRCA1 followed by BRCA2 being the commonest mutations. These mutations confer a relative risk of BC 10–30 times that of women in the general population. BRCA1 and BRCA2 confer a 60–85% and 15–40% lifetime risk of developing BC and OC, respectively [29, 30]. BRCA1-related BC has more aggressive features and characteristically has an absence of ER, PR and HER2 [4, 31]. In India, the incidence of BRCA mutation in women with BC is reported by Saxena et al. [32] and Mittal et al. [33] to be around 2.9 and 18.6% respectively. Another study reported that the incidence is as high as 16% if a high-risk cohort is selected (young age, positive family history and personal history of related cancers) [34]. This emphasizes the need for germline testing in patients with both BC and OC [35, 36].
Breast cancer patients have better survival outcomes as compared to patients with OC as women with OC often present with advanced-stage disease. The cause of death in most patients was attributable to a recurrence of OC irrespective of presentation with BC-first or OC-first. Tasca et al. [14] and Liou et al. [37] also reported a detriment to OS in patients who had BC-first who received a subsequent diagnosis of OC. Survival is dominated by the stage of disease at presentation as well as synchronicity. A case series from Memorial Sloan Kettering Cancer Center determined the lifetime risk of developing OC in BRCA mutation carriers as 20–50%, with the 10-year actuarial risk of OC after BC being 12.7% for BRCA1 carriers and 6.8% for BRCA2 carriers [38].
Stage, age, disease-free interval and interval between presentation of metachronous malignancies are factors that can be useful in designing an algorithm aimed at prevention or early detection during surveillance in HBOC. Appropriate surveillance and prophylactic oophorectomy are recommended for young BC survivors with or without germline mutation [39]. In the case of BC-first patients with a BRCA mutation, our data makes a case for risk reducing salpingo-oophorectomy, since subsequent OC was the main threat to survival. This is particularly relevant in the era of improved BC outcomes [40]. With respect to optimal timing of prophylactic oophorectomy, our data supports timing prophylactic oophorectomy 5–6 years after diagnosis of first BC based on the median time interval before development of second cancer to be 77 months after diagnosis of OC. This is similar to what is recommended in other series of healthy BRCA carriers [41, 42].
Correspondingly, counselling patients with BRCA-associated OC is complex as it should address the subsequent risk of BC and the risk of OC recurrence. In our study, the rate of BRCA mutation detection was the lowest in the OC-first group. Other studies have outlined a similar observation with one study reporting metachronous BC in BRCA carriers with previous OC as infrequently as in 10% patients. Moreover, the same studies also confirmed that the survival of these patients is dominated by OC [43, 44]. McGee et al. [45] also showed that in patients carrying a BRCA mutation diagnosed with stage 3/4 OC, the cause of death was most likely from OC progression. We did not note a better survival in patients with germline mutations contrary to some published series. However, survival of the BC-first group compared to OC-first and synchronous groups was better and is consistent with the published literature [14]. The incidence of contralateral BC was 14.3% in our series. The time lag between the occurrence of BC, OC and contralateral BC provides an opportunity to improve awareness, provide counselling and implement screening strategies for the prevention and early detection of OC and contralateral BC.
Our study has the shortcomings of a retrospective analysis with some loss of information on disease stage, grade and germline mutations in the early part of the study. Also, detailed multigene panel testing was not employed for all women, especially in the early cohort. The strength is that it is the largest HBOC series published from the Indian subcontinent and thus generates relevant real-world data in this cohort. As patients in the current study had not undergone prophylactic surgery based on prevailing guidelines, the study also provides insight into the natural history of second cancers in the HBOC group. This information sheds light on various lead time and length time biases for HBOC management in relation to screening, downstaging and prophylactic interventions in young patients presenting with either of the two cancers. Going forwards, the development of nomograms incorporating variables such as age, disease characteristics, mutation type, intervention, surveillance and prophylactic surgery can aid patients in the treatment decision-making process.
Conclusion
In patients presenting with metachronous or synchronous BC and OC, BC-first is the commonest presentation. A high index of suspicion, appropriate imaging, adequate biopsies, pathological testing and multidisciplinary management are necessary. Since the prognosis is dominated by OC stage, young women with BC should undergo germline mutation profiling and appropriately timed risk-reducing oophorectomy should be insisted upon.
Acknowledgements
The names of the institutions at which the work was performed were Tata Memorial Centre and Homi Bhabha National Institute, Mumbai, India, and Advanced Centre for Treatment, Research and Education in Cancer (ACTREC), Navi Mumbai, India.
Author Contribution
Conception and design: Shalaka Joshi and TS Shylasree; administrative support: Rajiv Sarin, Pradnya Kotwal, Rohini Hawaldar and R. A. Badwe; provision of the study materials or patients: Shalaka Joshi, TS Shylasree, Nita Nair, Vani Parmar, Rajiv Sarin; collection and assembly of the data: Shalaka Joshi, Sridevi Murali-Nanavati, Anand Thomas, Urvashi Jain, Ayushi Sahay, Vaibhav Vanmali and Sagar Tripathi; data analysis and interpretation: Shalaka Joshi, TS Shylasree, Sridevi Murali-Nanavati, Rohini Hawaldar and Urvashi Jain; manuscript writing: Shalaka Joshi, Sridevi Murali-Nanavati, Ayushi Sahay and TS Shylasree; final approval of the manuscript: all authors.
Declarations
Ethics Approval
The study was approved by Institutional Ethics Committee.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shalaka Joshi and Sridevi Murali-Nanavati contributed equally to this work.
Contributor Information
Shalaka Joshi, Email: drjoshishalaka@gmail.com.
Rajiv Sarin, Email: drrajivsarin@gmail.com.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Dhillon PK, Mathur P, Nandakumar A, et al. The burden of cancers and their variations across the States of India: the global burden of disease study 1990–2016. Lancet Oncol. 2018;19(10):1289–1306. doi: 10.1016/S1470-2045(18)30447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Disaia P (2002) Epithelial ovarian cancer. Clin Gynecol Oncol 289–350
- 4.Mavaddat N, Barrowdale D, Andrulis IL, et al. Pathology of breast and ovarian cancers among BRCA1 and BRCA2 mutation carriers: results from the consortium of investigators of modifiers of BRCA1/2 (CIMBA) Cancer Epidemiol Biomark Prev. 2011;21(1):134–147. doi: 10.1158/1055-9965.EPI-11-0775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Network CGA. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70. doi: 10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engel C, Rhiem K, Hahnen E, et al. Prevalence of pathogenic BRCA1/2 germline mutations among 802 women with unilateral triple-negative breast cancer without family cancer history. BMC Cancer. 2018;18(1):265. doi: 10.1186/s12885-018-4029-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singer CF, Tan YY, Muhr D, et al. Association between family history, mutation locations, and prevalence of BRCA1 or 2 mutations in ovarian cancer patients. Cancer Med. 2019;8(4):1875–1881. doi: 10.1002/cam4.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prior P, Waterhouse JA. Multiple primary cancers of the breast and ovary. British Journal of Cancer. 1981;44(5):628–36. doi: 10.1038/bjc.1981.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King M-C, Marks JH, Mandell JB (2003) Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302(5645):643–6 [DOI] [PubMed]
- 10.Shah S, Evans DG, Blair V, et al. Assessment of relative risk of second primary tumors after ovarian cancer and of the usefulness of double primary cases as a source of material for genetic studies with a cancer registry. Cancer. 1993;72(3):819–827. doi: 10.1002/1097-0142(19930801)72:3<819::AID-CNCR2820720330>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 11.Gronwald J, Byrski T, Huzarski T et al (2008) Hereditary breast and ovarian cancer. Hered Cancer Clin Pract 88(6). 10.1186/1897-4287-6-2-88 [DOI] [PMC free article] [PubMed]
- 12.Szabo CI, King MC. Population genetics of BRCA1 and BRCA2. Am J Hum Genet. 1997;60(5):1013–1020. [PMC free article] [PubMed] [Google Scholar]
- 13.Lee MI, Jung YJ, Kim DI et al (2021) Metastasis to breast from ovarian cancer and primary ovarian cancer concurrently diagnosis. Gland Surg 10(5):1806–1811. 10.21037/gs-20-640 [DOI] [PMC free article] [PubMed]
- 14.Tasca G, Dieci MV, Baretta Z et al (2020) Synchronous and metachronous breast and ovarian cancer: experience from two large cancer center. Front Oncol 10:608783 [DOI] [PMC free article] [PubMed]
- 15.Agarwal G, Pradeep PV, Aggarwal V, Yip CH, Cheung PS (2007) Spectrum of breast cancer in Asian women. World J Surg 31(5):1031–1040. 10.1007/s00268-005-0585-9 [DOI] [PubMed]
- 16.Kriplani D, Patel MM (2013) Immunohistochemistry: A diagnostic aid in differentiating primary epithelial ovarian tumors and tumors metastatic to the ovary. South Asian Journal of Cancer 02(04):254–258 [DOI] [PMC free article] [PubMed]
- 17.Lotan TL, Ye H, Melamed J et al (2009) Immunohistochemical panel to identify the primary site of invasive micropapillary carcinoma. Am J Surg Pathol 33(7):1037–1041 [DOI] [PMC free article] [PubMed]
- 18.Bennett JA, Young RH, Chuang A-Y et al (2018) Ovarian metastases of breast cancers with signet ring cells. Int J Gynecol Pathol 37(6):507–515 [DOI] [PubMed]
- 19.Al-Agha OM, Nicastri AD (2006) An in-depth look at Krukenberg Tumor: an overview. Arch Pathol Lab Med 130(11):1725–1730 [DOI] [PubMed]
- 20.Caruso G, Musacchio L, Santangelo G et al (2020) Ovarian Cancer Metastasis to the Breast: a Case Report and Review of the Literature. Case Rep Oncol 31(3):1317–1324. 10.1159/000509770 [DOI] [PMC free article] [PubMed]
- 21.Phung, H.T, Q.P.T, Van Nguyen T et al (2022) Recurrent ovarian cancer presenting with isolated axillary lymph node metastasis: a rare case report. Annals of Medicine and Surgery 77. 10.1016/j.amsu.2022.103640 [DOI] [PMC free article] [PubMed]
- 22.López F, Rodrigo JP, Silver CE et al (2016) Cervical lymph node metastases from remote primary tumor sites. Head Neck 38. 10.1002/hed.24344 [DOI] [PMC free article] [PubMed]
- 23.Zuhdy M, Alghandour R, Abdelazeem G et al (2019) Axillary nodal metastasis in ovarian cancer: A report of three cases and review of literature. J Egypt Natl Canc Inst 31(1) [DOI] [PubMed]
- 24.Caruso G, Musacchio L, Santangelo G et al (2020) Ovarian cancer metastasis to the breast: A case report and review of the literature. Case Reports in Oncology 13(3):1317–1324 [DOI] [PMC free article] [PubMed]
- 25.Espinosa I, Gallardo A, D’Angelo E et al (2015) Simultaneous carcinomas of the breast and ovary. Int J Gynecol Pathol 34(3):257–265 [DOI] [PubMed]
- 26.Liu H, Shi J, Prichard JW et al (2014) Immunohistochemical evaluation of GATA-3 expression in ER-negative breast carcinomas. Am J Clin Pathol 141(5):648–655 [DOI] [PubMed]
- 27.Cimino-Mathews A. Novel uses of immunohistochemistry in breast pathology: Interpretation and pitfalls. Modern Pathology. 2020;34(S1):62–77. doi: 10.1038/s41379-020-00697-3. [DOI] [PubMed] [Google Scholar]
- 28.Peng Y, Butt YM, Chen B et al (2017) Update on immunohistochemical analysis in breast lesions. Archives of Pathology & Laboratory Medicine 141(8):1033–1051 [DOI] [PubMed]
- 29.Antoniou A, Pharoah PDP, Narod S, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for Family history: a combined analysis of 22 studies. The American Journal of Human Genetics. 2003;72(5):1117–30. doi: 10.1086/375033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foulkes WD. Inherited susceptibility to common cancers. New England Journal of Medicine. 2008;359(20):2143–2153. doi: 10.1056/NEJMra0802968. [DOI] [PubMed] [Google Scholar]
- 31.Peshkin BN, Alabek ML, Isaacs C et al (2011) BRCA1/2 mutations and triple negative breast cancers. Breast Dis 32(1–1):25–33 [DOI] [PMC free article] [PubMed]
- 32.Saxena S, Chakraborty A, Kaushal M et al (2006) Contribution of germline BRCA1 and BRCA2sequence alterations to breast cancer in Northern India. BMC Med Genet 7(1) [DOI] [PMC free article] [PubMed]
- 33.Mittal A, Deo SVS, Gogia A et al (2022) Profile of Pathogenic Mutations and Evaluation of Germline Genetic Testing Criteria in Consecutive Breast Cancer Patients Treated at a North Indian Tertiary Care Center. Ann Surg Oncol 29(2):1423–1432. 10.1245/s10434-021-10870-w [DOI] [PMC free article] [PubMed]
- 34.Soumittra N, Meenakumari B, Parija T et al (2009) Molecular genetics analysis of hereditary breast and ovarian cancer patients in India. Hereditary Cancer in Clinical Practice 7(1) [DOI] [PMC free article] [PubMed]
- 35.Daly MB, Pal T, Berry MP et al (2021) Genetic/familial high-risk assessment: Breast, ovarian, and pancreatic, version 2.2021 NCCN clinical practice guidelines in oncology. Journal of the National Comprehensive Cancer Network 19(1):77–102 [DOI] [PubMed]
- 36.Daly MB, Pilarski R, Berry M et al (2016) NCCN guidelines insights: Genetic/familial high-risk assessment: Breast and ovarian, version 2.2017. Natl Compr Cancer Netw 15(1):9–20 [DOI] [PubMed]
- 37.Liou W-S, Hamilton CA, Cheung MK et al (2006) Outcomes of women with metachronous breast and ovarian carcinomas. Gynecol Oncol 103(1):190–194 [DOI] [PubMed]
- 38.Metcalfe KA, Lynch HT, Ghadirian P et al (2005) The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol 96(1):222–226 [DOI] [PubMed]
- 39.Rebbeck TR, Kauff ND, Domchek SM (2009) Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. JNCI Journal of the National Cancer Institute 101(2):80–87 [DOI] [PMC free article] [PubMed]
- 40.Domchek SM, Jhaveri K, Patil S, et al. Risk of metachronous breast cancer after brca mutation-associated ovarian cancer. Cancer. 2012;119(7):1344–1348. doi: 10.1002/cncr.27842. [DOI] [PubMed] [Google Scholar]
- 41.Heemskerk-Gerritsen BA, Seynaeve C, van Asperen CJ et al (2015) Breast cancer risk after salpingo-oophorectomy in healthy BRCA1/2 mutation carriers: Revisiting the evidence for risk reduction. JNCI: Journal of the National Cancer Institute 107(5) [DOI] [PubMed]
- 42.Kotsopoulos J, Huzarski T, Gronwald J et al (2016) Bilateral oophorectomy and breast cancer risk in brca 1 and brca 2 mutation carriers. JNCI: Journal of the National Cancer Institute 109(1) [DOI] [PMC free article] [PubMed]
- 43.Cvelbar M, Hocevar M, Vidmar G, et al. BRCA1/2 status and clinicopathologic characteristics of patients with double primary breast and ovarian cancer. Neoplasma. 2011;58(3):198–204. doi: 10.4149/neo_2011_03_198. [DOI] [PubMed] [Google Scholar]
- 44.Fishman A, Dekel E, Chetrit A et al (2000) Patients with double primary tumors in the breast and ovary— clinical characteristics and BRCA1–2 mutations status. Gynecol Oncol 79(1):74–78 [DOI] [PubMed]
- 45.McGee J, Giannakeas v, Karlan B et al (2017) Risk of breast cancer after a diagnosis of ovarian cancer in BRCA mutation carriers: Is preventive mastectomy warranted? Gynecol Oncol 145(2):346–351 [DOI] [PubMed]