Abstract
Xanthogranulomatous cholecystitis (XGC) is one of the rare variants of chronic cholecystitis which is characterized by inflammation of gall bladder along with infiltration by acute and chronic inflammatory cells. Intramural accumulation of lipid laden macrophages in GB wall is the hallmark of the disease. XGC results in dense adhesion of gall bladder (GB) to surrounding structures, like duodenum, colon, and stomach. The intense GB inflammation results in gall bladder perforation and development of fistulous communication between gall bladder and surrounding structures. This may also lead to formation of inflammatory mass which closely mimic gall bladder malignancy. Often differentiation from carcinoma of GB (Ca GB) on the basis of clinical presentation and even on intra-operative and radiological findings is difficult, and the issue could only be resolved on final Histopathology (HPE). We review presentation and investigation of a patient, discuss our approach in managing dilemma in treating such cases of XGC, and review the literature.
Keywords: Xanthogranulomatous cholecystitis, Gall bladder cancer, Radical cholecystectomy, Cholecystitis
Introduction
Xanthogranulomatous cholecystitis (XGC) is an uncommon variant of cholecystitis characterized by focal or diffuse destructive inflammatory process leading to marked proliferative fibrosis along with infiltration by macrophages and foamy cells [1, 2]. The inflammatory process can involve adjacent organs like liver, colon, and duodenum, leading to mass formation, which mimic gall bladder (GB) carcinoma. Incidence ranges from 0.7 to 10% of all the cholecystectomy specimen [1]. It is observed in the elderly age group of 60 to 70 years with, male to female ratio of 2:1. The clinical presentation, imaging, and intra-operative findings closely resemble GB carcinoma leading to misdiagnosis as GB cancer. Here, we report a case to focus on management dilemmas.
Case Presentation
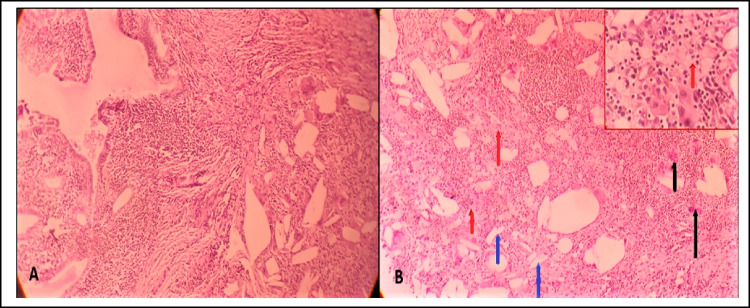
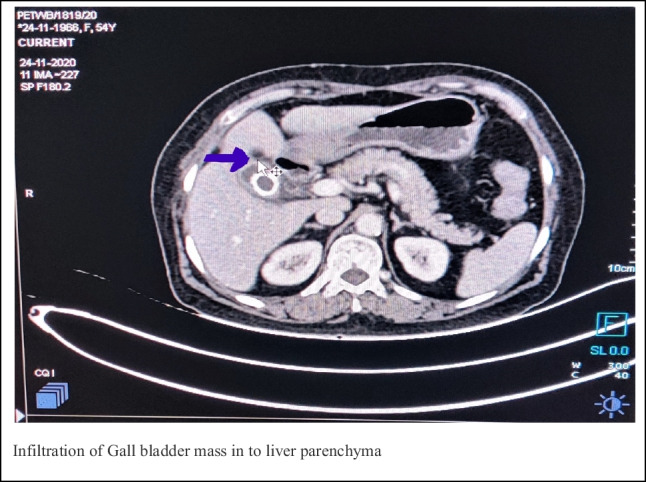
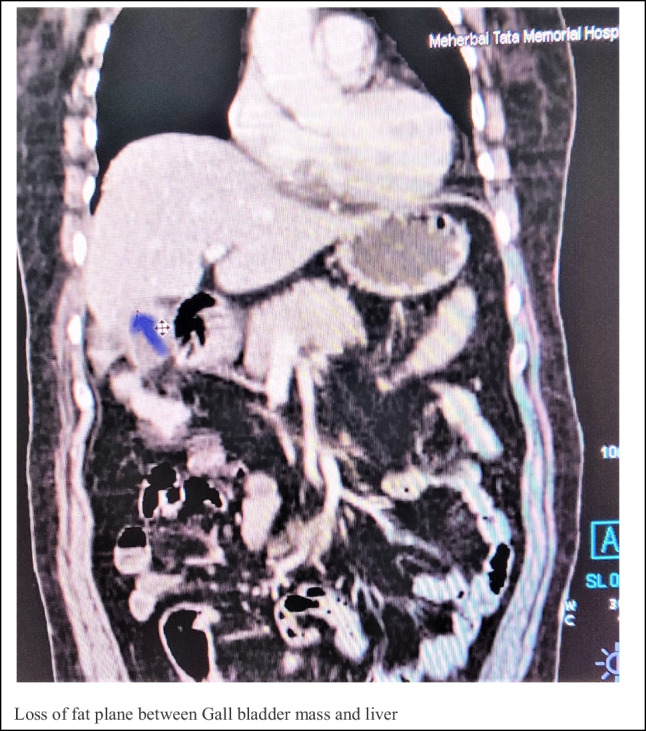
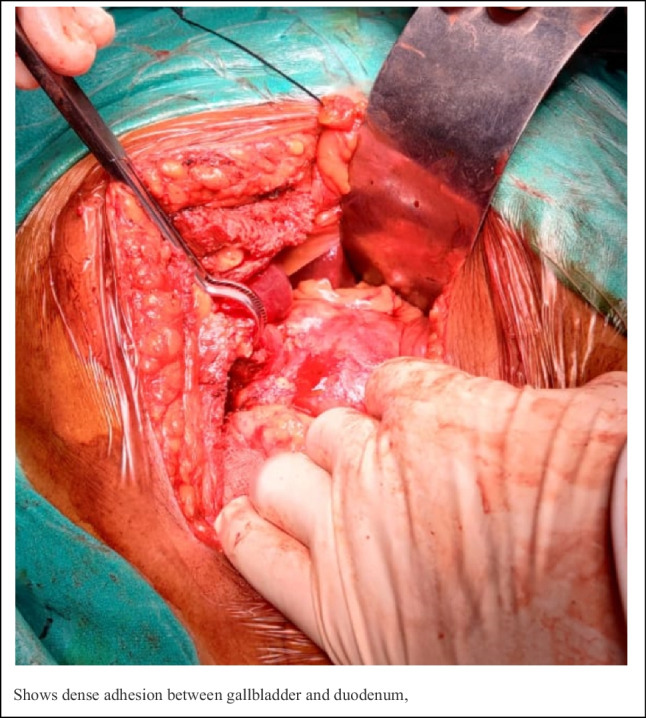
A 65-year-old female presented with the complaints of abdominal discomfort and pain in the past 4 months. Pain was insidious in onset, non-radiating with no aggravating factors. Ultrasonography of abdomen showed calculus chronic cholecystitis. She was taken up for laparoscopic cholecystectomy. Intra-operatively mass in GB fossa was found, giving an impression of malignancy. Consequently, surgery was aborted and biopsy taken from GB fossa mass. Biopsy suggested xanthogranulomatous cholecystitis (XGC). Patient self-referred to TMH Jamshedpur, where computed tomography of abdomen revealed contracted GB with inhomogenously enhancing wall thickening in fundus of gall bladder, pericholecystic fat stranding with gall stones. There was involvement of adjacent segment V liver with formation of mass lesion, measuring 40 × 44 × 40 mm, giving impression of gall bladder malignancy (Fig. 1 and Fig. 2). CEA was 6.09 ng/mL( normal < 5 ng/mL), and CA19.9 was 7.70 U/mL. Based on the radiological investigation, diagnosis of GB mass suspicious of malignancy was made and patient planed for extended cholecystectomy with intra-operative frozen section. Intra-operatively hard shrunken GB mass densely adherent to the duodenum and colon with loss of interface between gall bladder and liver suggestive of invasion was seen (Fig. 3). During the dissection of gall bladder mass, cholecysto-duodenal fistula was found (Fig. 4), which was divided. In view of strong possibility of Ca GB, we proceeded with cholecystectomy with 2 cm adjoining liver margin excision. Cystic duct stump was sent for frozen section, which was negative for malignancy. Final histopathology confirmed XGC (Fig. 5). Patient recovered well and was discharged on 5th postoperative day.
Fig. 1.
Infiltration of gall bladder mass in to liver parenchyma
Fig. 2.
Loss of fat plane between gall bladder mass and liver
Fig. 3.
Dense adhesion between gallbladder and duodenum
Fig. 4.

Cholecystoduodenal fistula
Fig. 5.
Hematoxylin and eosin–stained microphotographs of the cholecystectomy specimen: A (40 ×) Intact benign mucosal epithelium with dense chronic inflammation and deeper foamy macrophages accompanied by cholesterol clefts and giant cell response. B (200 ×) Red arrows pointing to foamy macrophage aggregates, blue arrows pointing to cholesterol clefts, and black arrows pointing to the giant cells
Discussion
Xanthogranulomatosis is an uncommon condition, which is characterized by infiltration by lipid laden histocytes in different parts of body such as the skin, retroperitoneum, genitals, brain, and gastrointestinal organ such as gallbladder [3]. Xanthogranulomatous cholecystitis (XGC) is chronic inflammatory disease of gall bladder characterized with obliterate fibrosis and the presence of foam cell. This condition was first described by Christensen et.al in 1970, and the nomenclature was given by Mc coy et al. in 1976 [4]. The exact etiology of XGC is still unknown, but it is usually associated with gallbladder stone. The etiopathogenesis suggest obstruction to bile flow by gall stones. Cholestasis results in xtravasations of bile into GB wall. This starts an inflammatory process, with the involvement of Rokitansky–Aschoff sinuses, leading to formation of sub mucosal abscesses or xanthogranulomas [5]. Finally, fibrous reaction and dense scarring results from healing of the inflammatory reaction. The inflammatory reaction may be associated with development of fistulous communication between GB and adjoining structures, chronic cholecystoenteric fistula may be a significant risk factor in the development of gallbladder carcinoma, and the incidence of gallbladder carcinoma associated with a cholecystoduodenal fistula is 15%. XGC patients can present with the features of acute cholecystitis in 22%, while chronic cholecystitis results in 88%. Pain occurs in 95%, while cholangitis is seen in 2%, and palpable GB mass is seen in (5%) of cases [6]. There is no definite biochemical marker for XGC. Yu et al. found that elevation of tumor biomarkers CA19-9 is frequent in XGC, which creates further confusion in differentiating the disease from carcinoma of gallbladder [7]. Ultrasonography may show contracted GB with cholelithiasis with diffuse and even focal thickening of gall bladder wall. The presence of characteristic hypoechoic nodules or bands in thickened gallbladder is seen in only 19% of cases [4]. Computed tomography and magnetic resonance imaging of abdomen may show diffuse or focal gall bladder wall thickening with intact luminal mucosal lining in XGC, while the presence of asymmetric GB focal thickening with discontinuity in luminal lining is more commonly seen in carcinoma GB [4]. FNAC may pre-operatively differentiate carcinoma of GB and XGC, with overall sensitivity and specificity is approx. 90% and 94% in detecting malignancy [8]. However in 20%, XGC may co-exist with adenocarcinoma. Hence, FNAC is avoided in operable suspected Ca GB, due to risk of tumor spillage and false negativity. Intra-operatively, XGC may resemble GB cancer due to formation of GB mass and inflammatory reaction; sensitivity of intra-operative naked eye gross assessment by surgeon to differentiate between XGC and carcinoma is only about 50 percentage [9]. In 2019, Anshuman Pandu et al. described the standard protocol for management of patients with asymmetric gall bladder wall thickness. According to it following cholecystectomy, the GB is opened and examined. Any suspicious lesion from the specimen is sent for frozen section [FS] to rule out malignancy. Completion radical cholecystectomy is done if malignancy is proved on FS [10]. Mistaking XGC as simple chronic cholecystitis can trap surgeon, since cholecystectomy is often a difficult operation in XGC, due to intense inflammation. Differentiating XGC from Ca GB may be difficult preoperatively, and current guidelines suggest that all suspicious GB masses [on cross-sectional radiological imaging] should be presumed to be malignant and subjected to cholecystectomy with excision of 2 cm liver margin and FS examination in high volume centers. This way the opportunity to cure operable Ca GB is not lost by choosing inappropriate lesser operation of cholecystectomy. In our study, we had done open surgery in all cases of suspicious or inconclusive gall bladder lesions, where the malignancy is possible. But however, currently, laparoscopic radical cholecystectomy (LRC) is an accepted modality and can be done in high-volume tertiary centers by expert hepatobiliary surgeons [11, 12].
Conclusion
Xanthogranulomatous cholecystitis is a rare destructive inflammatory benign disease associated with cholelithiasis which closely mimics malignancy. Difficulty to differentiate XGC from Ca GB, preoperatively or intra-operatively, causes dilemma. If diagnosed preoperatively XGC, then management is laproscopic/open cholecystectomy by experienced surgeon. If there is suspicion of malignancy either on radiological or intra-operatively, then cholecystectomy with 2 cm liver margin in high volume center should be done. Frozen section examination of resected GB specimen and of cystic duct stump is done to decide on extent of surgery should it be positive for malignancy.
Declarations
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rammohan A, Cherukuri SD, Sathyanesan J, Palaniappan R, Govindan M. Xanthogranulomatous cholecystitis masquerading as gallbladder cancer: can it be diagnosed preoperatively? Gastroenterol Res Practice. 2014;2014:253645. doi: 10.1155/2014/253645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bolukbasi H, Kara Y. An important gallbladder pathology mimicking gallbladder carcinoma: xanthogranulomatous cholecystitis: a single tertiary center experience. Surg Laparosc Endosc Percutaneous Tech. 2020;30(3):285–289. doi: 10.1097/SLE.0000000000000781. [DOI] [PubMed] [Google Scholar]
- 3.Yang T, Zhang BH, Zhang J, Zhang YJ, Jiang XQ, Wu MC. Surgical treatment of xanthogranulomatous cholecystitis: experience in 33 cases. Hepatobiliary Pancreat Dis Int: HBPD INT. 2007;6(5):504–508. [PubMed] [Google Scholar]
- 4.Singh VP, Rajesh S, Bihari C, Desai SN, Pargewar SS, Arora A. Xanthogranulomatous cholecystitis: what every radiologist should know. World J Radiol. 2016;8(2):183. doi: 10.4329/wjr.v8.i2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yabanoglu H, Aydogan C, Karakayali F, Moray G, Haberal M. Diagnosis and treatment of xanthogranulomatous cholecystitis. Eur Rev Med Pharmacol Sci. 2014;18(8):1170–1175. [PubMed] [Google Scholar]
- 6.Guzmán-Valdivia G. Xanthogranulomatous cholecystitis in laparoscopic surgery. J Gastrointest Surg. 2005;9(4):494–7. doi: 10.1016/j.gassur.2004.09.036. [DOI] [PubMed] [Google Scholar]
- 7.Hong YU, Yu TN, Cai XJ. Tumor biomarkers: help or mislead in the diagnosis of Xanthogranulomatous cholecystitis? –Analysis of serum CA 19–9, carcinoembryonic antigen, and CA 12–5. Chin Med J. 2013;126(16):3044–3047. doi: 10.3760/cma.j.issn.0366-6999,20120341. [DOI] [PubMed] [Google Scholar]
- 8.Hijioka S, Mekky MM, Sawaki A, Mizuno N, Hara K, Imamura H, et al. “T1460: diagnosis utility of endoscopic ultrasound-guided fine needle aspiration for diagnosis of gallbladder mass lesions. Gastrointest Endosc. 2010;71(5):AB282–83. doi: 10.1016/j.gie.2010.03.673. [DOI] [Google Scholar]
- 9.Deng YL, Cheng NS, Zhang SJ, Ma WJ, Shrestha A, Li FY, et al. Xanthogranulomatous cholecystitis mimicking gallbladder carcinoma: an analysis of 42 cases. World J Gastroenterol. 2015;21:12653–12659. doi: 10.3748/wjg.v21.i44.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandey A, Kumar D, Masood S, Chauhan S, Kumar S. Is final histopathological examination the only diagnostic criteria for xanthogranulomatous Cholecystitis? Niger J Surg. 2019;25(2):177–182. doi: 10.4103/njs.NJS_1_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoon YS, Han HS, Agarwal A, et al. Survey results of the expert meeting on laparoscopic surgery for gallbladder cancer and a review of relevant literature. Dig Surg. 2019;36:7–12. doi: 10.1159/000486208. [DOI] [PubMed] [Google Scholar]
- 12.Navarro JG, Kang I, Hwang HK, Yoon DS, Lee WJ, Kang CM. Oncologic safety of laparoscopic radical cholecystectomy in pT2 gallbladder cancer: a propensity score matching analysis compared to open approach. Medicine (Baltimore) 2020;99(20):e20039. doi: 10.1097/MD.0000000000020039. [DOI] [PMC free article] [PubMed] [Google Scholar]