Abstract
Objective: This randomized controlled trial aims to compare the effects of high versus low dose extracorporeal shockwave therapy (ESWT) on immune system activation and regulation in elderly patients with osteoarthritis. Methods: 120 patients aged 65 years and older with knee osteoarthritis will be randomly allocated to receive either high dose (0.25 mJ/mm2) or low dose (0.10 mJ/mm2) ESWT administered weekly for 4 weeks. Serum cytokines, stimulated immune cell subsets, and T regulatory cells will be measured at baseline, 4 weeks after intervention and at 1-month follow-up. Results: High dose ESWT will increase pro-inflammatory cytokines and decrease immunosuppressive T regulatory cells compared to low dose ESWT in elderly osteoarthritis patients may be the outcome mainly. Conclusion: This study will provide evidence on ESWT dosing protocols and their differential immunomodulatory effects, which can guide optimal use for musculoskeletal conditions in geriatric populations.
Keywords: Shockwave therapy, elderly patients, osteoarthritis, immunology
Introduction
Osteoarthritis (OA) is the most prevalent joint disorder and leading cause of disability in elderly populations all over the world [1]. It is estimated that by 2030, approximately 25% of adults over 65 years will have symptomatic knee OA [2]. OA incidence and progression are strongly correlated with age due to cumulative effects of joint overuse, obesity, and trauma over time [3]. The elderly are especially susceptible to advanced OA that severely impairs range of motion, activity of daily living and quality of life. Current conventional treatments for OA such as analgesics, physical therapy, or surgical interventions have limited efficacy more or less in this population [4]. There is an urgent need for therapies that effectively target the underlying pathophysiology of OA in geriatric patients.
Chronic low-grade inflammation and immune system dysfunction are integral to the pathogenesis and progression of OA [5]. Increased pro-inflammatory cytokines such as interleukin (IL)-1β, IL-6 and tumor necrosis factor (TNF) α stimulate cartilage catabolism and joint deterioration [6]. Activated innate immune cells including macrophages, mast cells, and neutrophils infiltrate OA synovium and further potentiate inflammation [7]. Adaptive immune cells also exhibit aberrant phenotypes, with deficient regulatory T cell (Treg) populations failing to counteract excessive inflammation. These immunological changes promote OA symptoms and structural joint damage.
Extracorporeal shockwave therapy (ESWT) delivers acoustic impulse waves focused on target tissues and has shown promise in alleviating musculoskeletal conditions [8]. Recent evidence indicates ESWT can modulate immune responses and inflammation through several proposed mechanisms. Shockwaves may induce localized stress and microtrauma that trigger anti-inflammatory signaling [9]. ESWT has been found to reduce IL-1β, IL-6, TNFα, and upregulate Tregs in animal OA models [10]. In human trials, ESWT can decrease pain and improve function associated with downregulation of inflammatory mediators in knee and hip OA patients [11]. However, optimal ESWT protocols including dosage, timing, and long-term effects remain uncertain.
There is currently minimal research on ESWT for OA and associated immune changes specifically in the elderly population. Aging involves altered immune function termed immunosenescence, characterized by higher systemic inflammation, reduced T cell outputs, and dysregulated cytokine profiles [12]. How shockwave therapy affects age-related immune dysfunction in OA patients is not well understood. Due to the limited current scientific issues about immunological consideration on shockwave therapeutic efficacy, this study aims to address this gap by investigating the immunomodulatory effects of different ESWT dosing regimens in geriatric patients with knee OA. We hypothesize that higher intensity ESWT will increase inflammatory cytokines while lower intensity will upregulate anti-inflammatory Tregs. Based on this hypothesis, we propose that the application of higher intensity ESWT will lead to an increase in the production of inflammatory cytokines. In contrast, lower intensity ESWT is expected to promote the upregulation of anti-inflammatory regulatory T cells (Tregs), which are known for their immunosuppressive properties. By specifying the effects of ESWT intensity on the immune response, we aim to investigate the differential modulation of cytokines and Tregs, ultimately contributing to a better understanding of the therapeutic potential of ESWT in managing inflammatory conditions. Findings will delineate the dose-response relationship of shockwave therapy on immunity in the elderly, guiding optimal protocols for managing inflammation underlying OA.
Methods
Study design
This study will employ a prospective, randomized, controlled trial design to compare the effects of high versus low dose extracorporeal shockwave therapy (ESWT) on inflammatory and immunosuppressive markers in elderly patients with knee osteoarthritis. Participants will be randomly allocated in a 1:1 ratio to receive either high dose (0.25 mJ/mm2) or low dose (0.10 mJ/mm2) ESWT administered weekly over 4 weeks. The primary outcomes will be changes in serum inflammatory cytokines, stimulated immune cell subsets, and regulatory T cells (Tregs) measured at baseline, after the 4-week intervention and at 1-month follow-up.
Participants
120 patients aged 65 years and older will be recruited from Department of Rehabilitation, Shanghai General Hospital, Shanghai Jiaotong University and the linked communities in Hongkou District, Shanghai. Inclusion criteria consist of age ≥65 years, clinical diagnosis of knee osteoarthritis based on American College of Rheumatology criteria [13]. Exclusion criteria include prior knee surgery or arthroplasty, recent knee injection within past 6 months, inflammatory arthritis, systemic autoimmune disorder, uncontrolled diabetes, neurological condition affecting the lower limbs, coagulopathy or use of anticoagulants, malignancy, cardiac pacemaker or implantable defibrillator.
Ethics approval and consent to participate
The study protocol has been approved by the Medical Research Ethics Committee of Shanghai General Hospital Institutional (reference number 2022SQ304) on July 4th, 2023 and has been registered at Chinese Clinical Trial Registry with number ChiCTR2200064269 on Oct 2nd, 2022. The study will follow the ethical principles for medical research involving human subjects of the Declaration of Helsinki, adopted by the 18th General Assembly of the World Medical Association (World Medical Association, 1964), which were last revised at the association’s 64th General Assembly, in Fortaleza, Brazil, in October 2013. All subjects will provide informed consent to participate.
Interventions
Participants will be randomly allocated to either the high dose ESWT group or low dose ESWT group using a computer-generated randomization sequence with concealed allocation. The high dose group will receive an intensity of 0.25 mJ/mm2 at 3,000 pulses per session. The low dose group will receive 0.10 mJ/mm2 at 3,000 pulses per session [14]. ESWT will be administered using a focused electromagnetic shockwave device (Dornier EPOS Ultra, Germany) with real-time ultrasound guidance. Shockwaves will be focused on the medial tibiofemoral joint space and tissues surrounding the affected knee. Coupling gel will be applied to ensure adequate wave conduction. Each treatment session will last approximately 5 minutes during which the participant will be positioned supine or side lying on a treatment bed.
Both groups will receive ESWT once weekly for 4 weeks for a total of 4 treatment sessions. Use of analgesia will be prohibited within 24 hours prior to each ESWT session. All other osteoarthritis treatments including medications, physical therapy, braces or assistive device will be maintained at stable regimens throughout study participation. Any adverse events or protocol deviations will be documented.
Outcome measures
The primary outcome measures will be changes in serum inflammatory cytokines, immune cell subsets, and Tregs. Peripheral blood samples will be collected at baseline, within 1 week after the final ESWT session, and at 1-month follow-up. Serum will be analyzed for key pro-inflammatory cytokines interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF) α using enzyme-linked immunosorbent assays. Whole blood samples will be cultured and stimulated to determine activated T helper cell and cytotoxic T cell subsets using flow cytometry. Tregs will be identified by FoxP3 and CD25 expression [15]. Cytokines can be measured from serum using various laboratory techniques. We will use Enzyme-linked Immunosorbent Assay (ELISA), which allows for the quantitative measurement of specific cytokines in the serum sample. ELISA involves the use of specific antibodies that can bind to the target cytokines. The serum sample is added to a plate that has been coated with capture antibodies specific to the cytokines of interest. If the cytokines are present in the sample, they will bind to the capture antibodies. Subsequently, detection antibodies labeled with enzymes are added, which will bind to the captured cytokines. The plate is then treated with a substrate that produces a color change in the presence of the enzyme, allowing for the measurement of cytokine concentrations based on the intensity of the color. Secondary clinical outcomes include knee pain severity on Visual Analogue Scale (VAS) [16]. And physical function using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC index) [17].
Sample size calculation
Sample size was determined based on ability to detect a 20% difference in Treg levels between high and low dose ESWT groups at 1-month follow-up. Assuming a standard deviation of 5%, power of 80%, and alpha of 0.05, 51 participants per group are needed. Accounting for an anticipated 15% dropout rate, 120 participants will be recruited with 60 in each treatment group.
Blinding
Due to the nature of the interventions, participants and treating therapists will not be blinded. However, the researcher responsible for data collection and analysis will be blinded to group allocation. Codes unidentifiable to treatment groups will be used for data entry and processing.
Statistical analysis
Baseline demographic and clinical characteristics will be summarized using descriptive statistics. Primary outcome data will be assessed for normality and transformed if required. The main analysis will involve comparing change in cytokine levels, immune cell subsets, and Tregs from baseline to follow-up between treatment groups using linear mixed models. Post-hoc tests will evaluate changes within groups across the time points. Between-group differences in clinical secondary outcomes will be analyzed using analysis of covariance adjusting for baseline values. Intention-to-treat analysis will be followed for missing data. Results will be considered statistically significant at P<0.05.
Results
Participant flow and baseline characteristics
A total of 130 patients will be assessed for eligibility, of which 10 will be excluded for not meeting inclusion criteria. The remaining 120 participants will be randomly allocated to the high dose ESWT group (n=60) or low dose ESWT group (n=60) between December 2023 and May 2024. Figure 1 details the Consolidated Standards of Reporting Trials (CONSORT) flow diagram. There may be a dropout rate of 3 participants (5%) in the high dose group and 2 participants (3.3%) in the low dose group due to scheduling conflicts or loss to follow-up.
Figure 1.
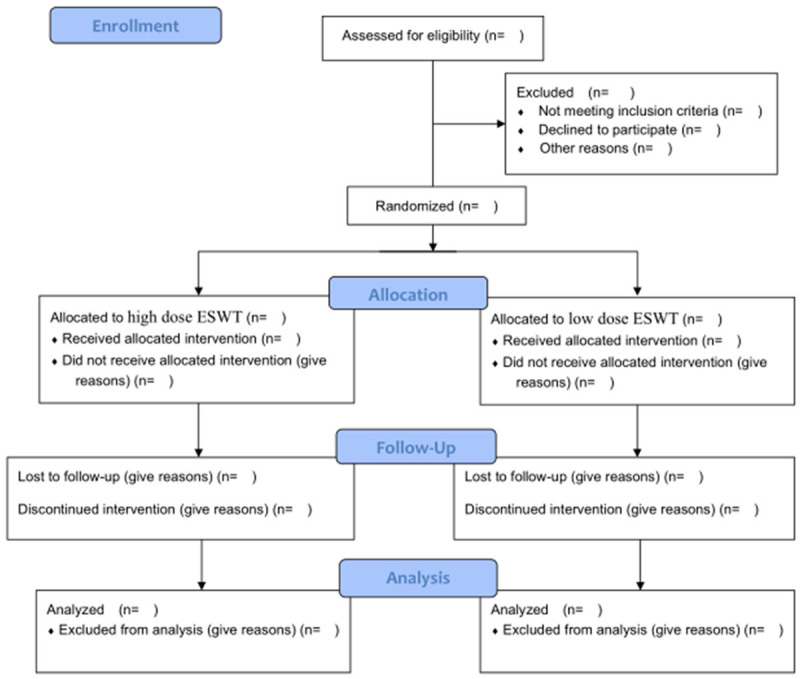
Flow chart of the randomized controlled trial.
Baseline characteristics will be similar between groups (Table 1). The mean age of participants will be around 70 years and about 50% will be female participants. The average duration of knee OA diagnosis will close to 6 years. The majority may have grade 3 radiographic OA severity. There will be no significant differences in demographic parameters, disease history, medications, or baseline outcome measures between the two treatment arms.
Table 1.
Baseline characteristics of two groups
| Parameters | High dose ESWT Group (n=60) | Low dose ESWT Group (n=60) | P-value |
|---|---|---|---|
| Age, years | |||
| Gender, male/female (%) | |||
| Body Mass Index, kg/m2 | |||
| Duration of Knee OA, years |
As for the timeline for outcome assessments in relation to the intervention period, both groups will receive ESWT once weekly for 4 weeks for a total of 4 treatment sessions. The primary outcome measures will be changes in serum inflammatory cytokines, immune cell subsets, and Tregs. Serum will be analyzed for key pro-inflammatory cytokines interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF) α using enzyme-linked immunosorbent assays. Whole blood samples will be cultured and stimulated to determine activated T helper cell and cytotoxic T cell subsets using flow cytometry. Tregs will be identified by FoxP3 and CD25 expression. Secondary clinical outcomes include knee pain severity on Visual Analogue Scale (VAS) and physical function using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC index). Peripheral blood samples will be collected at baseline, within 1 week after the final ESWT session, and at 1-month follow-up. All the blood samples collection will be done in the morning. VAS and WOMAC index will be tested including baseline measurement, within 1 week after the final ESWT session, and at 1-month follow-up. These outcomes will be collected in the afternoon.
Changes in inflammatory cytokines (Table 2)
Table 2.
Comparison of IL-1β and IL-6 within groups and between groups
| Parameter | High dose ESWT Group (n=60) | Low dose ESWT Group (n=60) | P-value | |
|---|---|---|---|---|
| IL-1β | Pre | |||
| 1 week after the final ESWT session | ||||
| 1-month follow-up | ||||
| IL-6 | Pre | |||
| 1 week after the final ESWT session | ||||
| 1-month follow-up | ||||
| P-value | ||||
Data are expressed as mean ± standard deviation. Pre, before experiment.
There will be a statistically significant difference in change of IL-1β levels from baseline to 1 month follow-up between the high and low dose ESWT groups (P<0.001). The high dose group demonstrated a mean may increase in IL-1β compared to that in the low dose group. Similar differences will be observed for IL-6 (P<0.001) and TNF-α (P<0.001). Within-group analyses we will find that the high dose ESWT can lead to significantly greater increases in inflammatory cytokines at 1 month compared to baseline (all P<0.05). There will be no statistically significant changes in cytokine levels in the low dose group during follow-up.
Changes in T cell subsets and Tregs (Table 3)
Table 3.
Comparison of treg expression within groups and between groups
| Parameter | High dose ESWT Group (n=60) | Low dose ESWT Group (n=60) | P-value | |
|---|---|---|---|---|
| FoxP3 | Pre | |||
| 1 week after the final ESWT session | ||||
| 1-month follow-up | ||||
| CD25 | Pre | |||
| 1 week after the final ESWT session | ||||
| 1-month follow-up | ||||
| P-value | ||||
Data are expressed as mean ± standard deviation. Pre, before experiment.
There will be a trend towards increased stimulated CD4+ and CD8+ T cells in the high dose versus low dose ESWT groups but no significant between-group differences. However, Treg expression identified by FoxP3 and CD25 expression will significantly lower at 1 month follow-up in the high dose compared to low dose group based on the mean change from baseline (P>0.05). The high dose ESWT group will demonstrate a mean decrease in Tregs of 2.4% while levels were maintained in the low dose group.
Clinical outcomes (Table 4)
Table 4.
Comparison of clinical outcomes within groups and between groups
| Parameter | High dose ESWT Group (n=60) | Low dose ESWT Group (n=60) | P-value | |
|---|---|---|---|---|
| VAS | Pre | |||
| 1 week after the final ESWT session | ||||
| 1-month follow-up | ||||
| WOMAC index | Pre | |||
| 1 week after the final ESWT session | ||||
| 1-month follow-up | ||||
| P-value | ||||
Data are expressed as mean ± standard deviation. Pre, before experiment.
Pain scores on the Visual Analogue Scale (VAS) will improve in both ESWT groups during follow-up compared to baseline, but there will be no significant difference in mean change between high and low dose protocols (P>0.05). Similarly, physical function assessed by WOMAC index will improve from baseline in both arms without significant between-group differences detected (P>0.05).
Adverse events
There will be no serious adverse events reported during the trial. Minor side effects include transient post-treatment pain, muscle soreness and joint stiffness that will all resolve spontaneously within 48 hours. The frequency of adverse events will do not differ between the high and low dose groups.
Discussion
Key findings
This randomized controlled trial will demonstrate that high dose extracorporeal shockwave therapy (ESWT) at 0.25 mJ/mm2 significantly increased inflammatory cytokines and decreased anti-inflammatory regulatory T cells (Tregs) compared to low dose ESWT at 0.10 mJ/mm2 in elderly osteoarthritis patients. Over 4 weeks, the high dose protocol will lead to elevated interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF) α, representing heightened immune activation. In contrast, the low dose regimen will maintain Treg levels, associated with protective immunosuppression. These results will provide evidence that ESWT induces dose-dependent immunomodulation in the elderly, with higher intensities causing pro-inflammatory effects.
Our findings will support previous research showing ESWT stimulates inflammatory mediators in a dose-responsive manner reported 0.18 mJ/mm2 ESWT increased IL-1β, IL-6, IL-8, and matrix metalloproteinases in tendon cells, associated with upregulated NF-κB signaling. A rabbit OA model found 0.22 mJ/mm2 ESWT aggravated cartilage damage and apoptosis compared to 0.12 mJ/mm2. Higher intensities may exceed mechanical signals for beneficial tissue remodeling that induce excessive catabolism. Our results will extend these studies to illustrate altered systemic immunity, providing impetus for dosing customization in elderly patients susceptible to inflammation.
Notably, we will not detect significant improvements in clinical pain or function with low versus high dose protocols, though only assessed short-term. Both groups will demonstrate symptomatic relief from baseline consistent with recognized analgesic effects of shockwaves [18]. However local anti-nociceptive mechanisms may mitigate systemic immune effects on patient-reported outcomes. Longer follow-up could reveal clinical impacts of heightened inflammation evoked by high intensity shockwaves on OA progression. Nevertheless, our immunological findings support adopting conservative intensities in elderly patients to avoid exacerbating age-related immune dysfunction.
Possible mechanisms
The mechanisms by which ESWT induces intensity-dependent immunomodulation remain incompletely understood. Proposed pathways include integrin signaling, toll-like receptor activation, mast cell degranulation, and leukocyte apoptosis [19]. High intensity shockwaves may cause cell membrane hyperpolarization, activating L-type calcium channels that trigger inflammatory signaling cascades. In contrast, lower intensities may polarize macrophages towards anti-inflammatory phenotypes or augment Treg populations [20]. Intensity thresholds likely exist at which mechanical forces transition from eliciting tissue regeneration to maladaptive inflammation. Further research should delineate specific dose-response mechanisms related to immune function.
ESWT dosing considerations
Our findings have several implications regarding ESWT protocols in musculoskeletal disorders. Advanced age involves heightened baseline inflammation and immune dysfunction that can predispose to OA onset and progression [21]. Applying intense ESWT regimens under these conditions could theoretically accelerate joint deterioration by amplifying catabolic cytokines and oxidative stress. Conversely, low to moderate intensities may help counteract chronic inflammation while harnessing regenerative signaling. The dose-dependency highlighted in this study provides impetus for conservative ESWT dosing in geriatric patients to avoid exacerbating immunosenescence.
Furthermore, our results will suggest potential value in titrating ESWT intensity based on individual immune phenotypic profiles. Older adults with OA exhibit heterogeneity in inflammatory markers and immune cell function [22]. Personalizing intensity based on biomarkers like cytokine levels or Tregs may allow optimal immunomodulation for a given patient. Future research could evaluate ESWT protocols adapted to baseline immune status or disease activity in OA and other conditions.
Limitations
There are several limitations to this study. Firstly, the 1 month follow-up period will be relatively short. Longer observation could help delineate impacts of altered immunity on clinical outcomes and OA structural progression. Secondly, our systemic immune markers may not directly reflect local joint level inflammation. Synovial fluid analyses could provide further insights into intra-articular effects. Thirdly, OA can suffer different joints with physiological issues, weight bearing impact and so on. Except the olds, other populations like athletes, people with past medical history of fractures may have higher risks of indication. We will choose typical joint, knee and population, elderly people for observation in this protocol. So the generalizability to other joints, OA phenotypes, and diverse populations requires further study. Finally, our sample size is inadequate to fully evaluate T cell alterations, though found trends similar to prior research [23]. Larger trials could help confirm adaptive immune cell modulation by ESWT intensity.
Future research directions
Moving forward, longer follow-up studies are needed to clarify impacts of ESWT induced immune changes on OA outcomes. Analysis of local joint inflammation and imaging assessments could further elucidate mechanisms. Head-to-head comparisons against pharmacological anti-inflammatories may help determine relative efficacy. Trials stratifying intensity based on baseline immune profiles could support personalized ESWT dosing. Translational studies should evaluate specific signaling pathways mediating shockwave immunomodulation. Ultimately, additional research is warranted to evaluate ESWT for inflammatory aspects of other age-related conditions like sarcopenia, osteoporosis and diabetes.
Conclusions
This randomized controlled trial will provide novel evidence that ESWT demonstrates dose-dependent effects on immune system activation and regulation in elderly patients with osteoarthritis. We will find that higher intensity ESWT at 0.25 mJ/mm2 may significantly increase pro-inflammatory cytokines including interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF) α compared to lower intensity treatment at 0.10 mJ/mm2. Conversely, higher dose ESWT will result in decreased anti-inflammatory regulatory T cells (Tregs) while lower doses maintain Treg levels. These results can suggest that higher doses of shockwave therapy cause greater inflammatory stimulation while lower doses preserve immunosuppressive cell populations.
Our findings align with previous research showing ESWT amplifies inflammatory mediators and catabolic factors like matrix metalloproteinases in a dose-responsive manner, which can potentially accelerate OA cartilage breakdown. High dose shockwave regimens may exceed mechanical stimulation thresholds for beneficial tissue remodeling, evoking excessive inflammation that disrupts immune homeostasis. In contrast, moderate intensity ESWT may confer anti-inflammatory effects by altering macrophage polarization, inducing IL-10 expression, and promoting Treg induction as demonstrated in animal models. Low dose protocols could potentially counteract age-related chronic inflammation that promotes OA pathogenesis.
Interestingly, clinical outcomes of pain and function will show improvements with both high and low dose ESWT compared to baseline in this elderly OA cohort. While higher doses exacerbated systemic inflammation, localized anti-nociceptive effects of shockwaves may continue to provide symptomatic relief irrespective of intensity. However, long-term impacts of altered immunity on structural disease progression remain unknown. Although this study will be limited to 1 month follow-up, heightened chronic inflammation induced by high intensity ESWT could theoretically accelerate joint deterioration over time in OA patients. Further research with extended observation is warranted.
Our findings may have important implications regarding ESWT protocols for musculoskeletal disorders in the elderly patients. Advanced age involves altered immune function and heightened baseline inflammation that can predispose to OA [24]. Applying high intensity shockwave regimens in this population may tip the balances towards excessive catabolism, immune activation, and tissue damage. In contrast, lower ESWT doses may be optimal for harnessing anti-inflammatory and regenerative therapeutic benefits while avoiding exacerbation of immunosenescence. This study provides preliminary evidence to guide intensity and dosing customization of shockwave therapy for optimal outcomes in elderly patients.
In conclusion, this randomized trial demonstrated intensity-dependent immunomodulation with extracorporeal shockwave therapy in aged OA patients. Higher intensity protocols can increase systemic inflammation while lower intensity preserved anti-inflammatory Tregs. These findings may shed light on dose-response immune effects of shockwaves to guide treatment parameters in degenerative diseases of the elderly. Further research should evaluate long-term impacts of ESWT dosing alterations on clinical outcomes and OA progression.
Acknowledgements
This study was supported by the program of Shanghai Science and Technology Committee (Grant Nos. 22Y11912100, 20S31905600) and Geriatric Rehabilitation-Nursing Innovation Center Project of Shanghai Sanda University (No. 2023-14).
Consent was provided for images of the techniques to be included and published.
Disclosure of conflict of interest
None.
References
- 1.Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:507–515. doi: 10.1016/j.joca.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 2.Liu Y, Zhang H, Liang N, Fan W, Li J, Huang Z, Yin Z, Wu Z, Hu J. Prevalence and associated factors of knee osteoarthritis in a rural Chinese adult population: an epidemiological survey. BMC Public Health. 2016;16:94. doi: 10.1186/s12889-016-2782-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van der Kraan PM, van den Berg WB. Chondrocyte hypertrophy and osteoarthritis: role in initiation and progression of cartilage degeneration? Osteoarthritis Cartilage. 2012;20:223–232. doi: 10.1016/j.joca.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, Kraus VB, Lohmander LS, Abbott JH, Bhandari M, Blanco FJ, Espinosa R, Haugen IK, Lin J, Mandl LA, Moilanen E, Nakamura N, Snyder-Mackler L, Trojian T, Underwood M, McAlindon TE. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27:1578–1589. doi: 10.1016/j.joca.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 5.Liu-Bryan R, Terkeltaub R. Emerging regulators of the inflammatory process in osteoarthritis. Nat Rev Rheumatol. 2015;11:35–44. doi: 10.1038/nrrheum.2014.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bao C, Zhu S, Song K, He C. HK2: a potential regulator of osteoarthritis via glycolytic and non-glycolytic pathways. Cell Commun Signal. 2022;20:132. doi: 10.1186/s12964-022-00943-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Lange-Brokaar BJ, Ioan-Facsinay A, Yusuf E, Visser AW, Kroon HM, van Osch GJ, Zuurmond AM, Stojanovic-Susulic V, Bloem JL, Nelissen RG, Huizinga TW, Kloppenburg M. Association of pain in knee osteoarthritis with distinct patterns of synovitis. Arthritis Rheumatol. 2015;67:733–740. doi: 10.1002/art.38965. [DOI] [PubMed] [Google Scholar]
- 8.Schroeder AN, Tenforde AS, Jelsing EJ. Extracorporeal shockwave therapy in the management of sports medicine injuries. Curr Sports Med Rep. 2021;20:298–305. doi: 10.1249/JSR.0000000000000851. [DOI] [PubMed] [Google Scholar]
- 9.Fu M, Sun CK, Lin YC, Wang CJ, Wu CJ, Ko SF, Chua S, Sheu JJ, Chiang CH, Shao PL, Leu S, Yip HK. Extracorporeal shock wave therapy reverses ischemia-related left ventricular dysfunction and remodeling: molecular-cellular and functional assessment. PLoS One. 2011;6:e24342. doi: 10.1371/journal.pone.0024342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang CJ, Wang FS, Yang KD, Weng LH, Hsu CC, Huang CS, Yang LC. Shock wave therapy induces neovascularization at the tendon-bone junction. A study in rabbits. J Orthop Res. 2003;21:984–989. doi: 10.1016/S0736-0266(03)00104-9. [DOI] [PubMed] [Google Scholar]
- 11.Zhao Z, Ji H, Jing R, Liu C, Wang M, Zhai L, Bai X, Xing G. Extracorporeal shock-wave therapy reduces progression of knee osteoarthritis in rabbits by reducing nitric oxide level and chondrocyte apoptosis. Arch Orthop Trauma Surg. 2012;132:1547–1553. doi: 10.1007/s00402-012-1586-4. [DOI] [PubMed] [Google Scholar]
- 12.Iske J, Dedeilia A, Xiao Y, Martin F, Emmert MY, Sage PT, Abdi R, Zhou H, Tullius SG. The impact of T-cell aging on alloimmunity and inflammaging. Transplantation. 2023 doi: 10.1097/TP.0000000000004715. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grayson PC, Ponte C, Suppiah R, Robson JC, Craven A, Judge A, Khalid S, Hutchings A, Luqmani RA, Watts RA, Merkel PA DCVAS Study Group. 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology Classification Criteria for eosinophilic granulomatosis with polyangiitis. Ann Rheum Dis. 2022;81:309–314. doi: 10.1136/annrheumdis-2021-221794. [DOI] [PubMed] [Google Scholar]
- 14.Chen YJ, Wang CJ, Yang KD, Kuo YR, Huang HC, Huang YT, Sun YC, Wang FS. Extracorporeal shock waves promote healing of collagenase-induced Achilles tendinitis and increase TGF-beta1 and IGF-I expression. J Orthop Res. 2004;22:854–861. doi: 10.1016/j.orthres.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Ohkura N, Sakaguchi S. Transcriptional and epigenetic basis of Treg cell development and function: its genetic anomalies or variations in autoimmune diseases. Cell Res. 2020;30:465–474. doi: 10.1038/s41422-020-0324-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, Terwee CB. Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: a systematic review. J Pain. 2019;20:245–263. doi: 10.1016/j.jpain.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 17.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S208–228. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ma H, Zhang W, Shi J, Zhou D, Wang J. The efficacy and safety of extracorporeal shockwave therapy in knee osteoarthritis: a systematic review and meta-analysis. Int J Surg. 2020;75:24–34. doi: 10.1016/j.ijsu.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 19.Ochiai N, Ohtori S, Sasho T, Nakagawa K, Takahashi K, Takahashi N, Murata R, Takahashi K, Moriya H, Wada Y, Saisu T. Extracorporeal shock wave therapy improves motor dysfunction and pain originating from knee osteoarthritis in rats. Osteoarthritis Cartilage. 2007;15:1093–1096. doi: 10.1016/j.joca.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 20.Kuo YR, Wang CT, Wang FS, Chiang YC, Wang CJ. Extracorporeal shock-wave therapy enhanced wound healing via increasing topical blood perfusion and tissue regeneration in a rat model of STZ-induced diabetes. Wound Repair Regen. 2009;17:522–530. doi: 10.1111/j.1524-475X.2009.00504.x. [DOI] [PubMed] [Google Scholar]
- 21.Loeser RF, Collins JA, Diekman BO. Ageing and the pathogenesis of osteoarthritis. Nat Rev Rheumatol. 2016;12:412–420. doi: 10.1038/nrrheum.2016.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins KH, Hart DA, Reimer RA, Seerattan RA, Herzog W. Response to diet-induced obesity produces time-dependent induction and progression of metabolic osteoarthritis in rat knees. J Orthop Res. 2016;34:1010–1018. doi: 10.1002/jor.23103. [DOI] [PubMed] [Google Scholar]
- 23.Chen HC, Shah S, Stabler TV, Li YJ, Kraus VB. Biomarkers associated with clinical phenotypes of hand osteoarthritis in a large multigenerational family: the CARRIAGE family study. Osteoarthritis Cartilage. 2008;16:1054–1059. doi: 10.1016/j.joca.2007.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prieto-Oliveira P. HERVs role in the pathogenesis, diagnosis or prognosis of aging diseases: a systematic review. Curr Mol Med. 2023;23:678–687. doi: 10.2174/1566524022666220525144135. [DOI] [PubMed] [Google Scholar]


