Abstract
Objective
To examine the association between the mobilization level during intensive care unit (ICU) admission and independence in activity of daily living (ADL), defined as Barthel Index (BI)≥70.
Methods
This was a post-hoc analysis of the EMPICS study involving nine hospitals. Consecutive patients who spend >48 hours in the ICU were eligible for inclusion. Mobilization was performed at each hospital according to the shared protocol and the highest ICU mobility score (IMS) during the ICU stay, baseline characteristics, and BI at hospital discharge. Multiple logistic regression analysis, adjusted for baseline characteristics, was used to deter-mine the association between the highest IMS (using the receiver operating characteristic [ROC]) and ADL.
Results
Of the 203 patients, 143 were assigned to the ADL independence group and 60 to the ADL dependence group. The highest IMS score was significantly higher in the ADL independence group than in the dependence group and was a predictor of ADL independence at hospital discharge (odds ratio, 1.22; 95% confidence interval, 1.07–1.38; adjusted p=0.002). The ROC cutoff value for the highest IMS was 6 (specificity, 0.67; sensitivity, 0.70; area under the curve, 0.69).
Conclusion
These results indicate that, in patients who were in the ICU for more than 48 hours, that patients with good function in the ICU also exhibit good function upon discharge. However, prospective, multicenter trials are needed to confirm this conclusion.
Keywords: Intensive care units, Rehabilitation, Activities of daily living, Postintensive care syndrome
GRAPHICAL ABSTRACT
INTRODUCTION
Although the short-term prognosis of intensive care unit (ICU) patients has improved recently, long-term dysfunction has become increasingly important [1]. Physical dysfunction after ICU discharge results in the weakening of limbs and limitation of ADL, and it has been reported that 50%–70% of ICU patients develop physical dysfunction [2]. Therefore, improving the functional prognosis of ICU patients has been recognized as an important problem in intensive care medicine [3].
Physical dysfunction after ICU discharge can occur in all patients, but immobility is considered a major risk factor [4,5]. Therefore, early rehabilitation for physical dysfunction should begin immediately after admission to the ICU [6]. The effects of early rehabilitation are widely reported, including the prevention of delirium [7], shortening the length of mechanical ventilation [8] and shortening the length of stay in the ICU [9,10]. Although relatively short-term results have been increasingly reported recently, data on the relationship between the mobilization level in critically ill patients and activity of daily living (ADL) independence at hospital discharge are still lacking [11-13]. Previous studies examined the mobilization level of ICU patients and reported that patients discharged home had higher ICU mobility score (IMS) scores at discharge from the ICU than patients discharged to the facility. However, an analysis of cutoff scores to predict ADL independence in Japan has not yet been performed [14].
Insight into what mobilization level should be targeted during ICU stay for early recovery may help avoid increasing dependence on ADLs during the hospital discharge of critically ill patients. However, the targeted mobilization level during ICU stay for critically ill patients remains unclear. Therefore, this study investigated the relationship between the mobilization level during ICU admission and independence in ADL at hospital discharge. A post-hoc analysis of the EMPICS study [11], a multicenter prospective study of psychiatric symptoms in ICU patients three months after hospital discharge, was performed to investigate the association between the mobilization level during the ICU stay and ADL independence at hospital discharge.
METHODS
Study design, setting, and patients
This was a post-hoc analysis of the EMPICS study (Association between the achievement of Early Mobilization and Psychiatric symptoms in Japanese Intensive Care Survivors, UMIN ID; 000036503) [11]. This EMPICS study was approved by the Ethics Committee of Nagoya Medical Center (No. 2018093) and eight other participating hospitals. We followed the STROBE guidelines and all methods in this study were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all patients. Consecutive patients, up to 25 in each participating hospital, who stayed in the ICU for more than 48 hours between June and December in 2019, were eligible for enrollment. Patients under 18 years of age, unable to walk independently before admission, with neurological complications, lack of communication skills due to preexisting mental diseases, or in a terminal state were excluded.
Early mobilization protocol
In this study, we sought to mobilize all patients equally and daily under the five-level protocol (level 1, passive range of motion and respiratory physical therapy; level 2, active range of motion; level 3, sitting exercise; level 4, standing exercise; and level 5, walking exercise) tailored to each participating hospital [11,15,16]. At each participating site, ICU physicians or physiotherapists referred to the protocol and decided each patient’s rehabilitation level based on the patient’s condition. To increase the mobilization level above level 3, it was necessary for the patient to meet the stability criteria listed in Supplementary Table S1. All participating hospitals followed the evidence based expert consensus for early rehabilitation in the ICU of the Japanese society of intensive care medicine regarding the criteria for conducting each mobilization stage of the other five-level protocol [3]. All patients received at least one rehabilitation session per week for 20 minutes. In addition, after ICU discharge, physical or occupational therapists provided rehabilitation, such as muscle strengthening, balance, walking, and stair exercises, for more than 20 minutes on weekdays to each patient according to the rehabilitation policy in the general ward of each hospital. Therefore, in this study, it is difficult to confirm the relationship between the mobilization level after ICU discharge and ADL independence at hospital discharge. Detailed characteristics of the institutions are listed in Supplementary Table S2.
Data collection
The mobilization level during the ICU stay was assessed daily by a physio-therapist using IMS. The IMS is a quick and easy method to measure bedside mobility in a critically ill patient. As a functional endpoint in ICU rehabilitation studies, the IMS provides a sensitive 11-point ordinal scale, ranging from nothing (lying/passive exercises in bed, score 0), sitting in bed, exercises in bed (any activity in bed, score 1), passively moved to chair (score 2), sitting over edge of bed (score 3), standing (score 4), transferring bed to chair (score 5), marching on spot (at bedside, score 6), walking with assistance of 2 or more people (score 7), walking with assistance of 1 person (score 8), walking independently with a gait aid (score 9), and independent ambulation (score 10) [17]. At the time of ICU admission, the following basic patient information was recorded: age, sex, body mass index (BMI), Acute Physiology and Chronic Health Evaluation II score, Sequential Organ Failure Assessment (SOFA) score, Charlson Comorbidity Index (CCI), Barthel Index (BI) before hospitalization, ICU admission diagnosis, ICU and hospital length of stay, the incidence of ICU-acquired weakness (ICU-AW) at ICU discharge, EuroQol-5 Dimensions-5 Levels (EQ-5D-5L) at hospital discharge, [18] and in-hospital mortality.
Additionally, BI was measured at discharge. As in previous studies, ADL dependence was defined as BI<70 points [7,11,12,19], and mobilization was defined as being able to sit on the edge of the bed or a higher degree of mobility [9,11,12,19,20]. In this study, early rehabilitation was defined as within the first 72 hours after ICU admission [3]. BI pre-hospitalization was assessed at the time of admission to the ICU based on information from the family or patients if they were conscious. ICU-AW was defined as a Medical Research Council sum score (evaluated by a physical therapist)<48 at ICU discharge [21].
Statistical analysis
We compared patient characteristics by ADL independence at hospital discharge expressed as median (interquartile range) or the number of cases (%) in the data of both groups. For the analysis of continuous variable, the Mann–Whitney U-test was used for nominal variables, the χ2 test or Fisher’s exact test, as appropriate. Before using a non-parametric test, the distribution of each parameter was assessed with the Shapiro–Wilk test. Deaths were excluded from the analysis of ICU and hospital length of stays, as using the ICU and hospital length of stays for early deaths may incorrectly shorten the hospital days in the ADL dependent group.
To assess the association between the highest IMS and independence in ADL at hospital discharge, multivariable logistic regression was performed, adjusting for covariates such as age, BMI, CCI, BI before hospitalization, ICU admission diagnosis (sepsis of non-pulmonary origin status), and SOFA score at ICU admission. These variables were selected based on the results of previous studies and our clinical interest [9,11,12,15,16]. Results are reported as odds ratio (OR) and 95% confidence interval (95% CI). Receiver operating characteristic (ROC) were constructed for ADL independence at hospital discharge and highest IMS during ICU stay and the area under the curve (AUC) was calculated. To further look for associations between highest IMS during ICU stay and other outcomes, we performed logistic regression analysis with length of ICU (>7 days) and hospital (>28 days) and EQ-5D-5L (>0.5) at discharge as objective variables. Variables were modeled as continuous data when appropriate or were dichotomized using clinically relevant cutoff values.
Next, the patients were divided into two groups for a sensitivity analysis based on changes in the SOFA score, to assess the progress in mobilization. In one group, the SOFA score improved or did not change from the time of ICU admission to the next day (unchanged SOFA score), whereas in the other group, the SOFA score had worsened (worse SOFA score). For sensitivity analysis, we restricted the number of covariates to four: age, BMI, CCI, and BI before hospitalization to prevent model over fitting. Variables in the model with p<0.05 from the lack-of-fit test were excluded from the results of this study considering non-fitting [22].
We then performed one subanalysis. We excluded those who died in hospital because the association between ADL independence and mortality is assumed to be bidirectional: ADL dependence may be a consequence of mortality. Covariates in the multivariate analysis included age, BMI, CCI, and prehospital BI.
All analyses were performed using the JMP software (version 13.0; SAS Institute Inc.). Statistical tests were two-sided, and statistical significance was defined as p<0.05.
RESULTS
Baseline characteristics
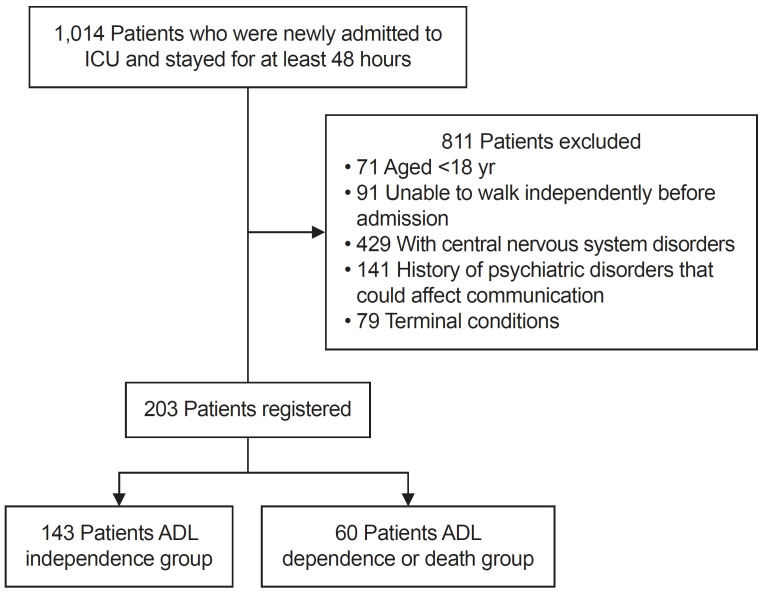
A total of 1,014 patients were admitted to the ICU. After the exclusion of patients younger than 18 years, unable to walk independently before admission, patients with neurological complications, lacking communication skills due to preexisting mental ill-ness, and terminal patients, 203 patients remained. In all patients, the mobilization level activity was assessed by a full-time physiotherapist (Fig. 1). Independent ADL hospital discharge was observed in 143 patients (ADL independence group) but not in 60 patients (ADL dependence group, including death in the hospital.
Fig. 1.
Flow chart of the patient selection process. ICU, intensive care unit; ADL, activity of daily living.
Table 1 shows the baseline characteristics of patients in the entire study cohort and in the ADL independence and ADL dependence groups. Intergroup comparisons revealed significant differences (Table 1) in age (p<0.001), BMI (p=0.004), BI before hospitalization (p=0.040), SOFA score at ICU admission (p=0.001), highest IMS during ICU admission (p<0.001), ICU length of stay (p<0.001), incidence of ICU-AW (p<0.001) and EQ-5D-5L score at hospital discharge (p<0.001). In this study, 25 patients (12.3%) died during hospitalization and were included in the analysis as an ADL dependency group.
Table 1.
Comparison of patient characteristics based the ADL independence at hospital discharge
| Variable | All patients (n=203) | ADL independence (n=143) | ADL dependence (n=60) | p-value |
|---|---|---|---|---|
| Age (yr) | 71 (61–79) | 69 (57–76) | 78 (70–85) | <0.001 |
| Sex, male | 131 (64.5) | 96 (67.1) | 35 (58.3) | 0.262 |
| Body mass index (kg/m2) | 23 (20–26) | 23 (21–26) | 22 (19–24) | 0.004 |
| Charlson Comorbidity Index | 2 (1–3) | 2 (1–3) | 2 (0–3) | 0.783 |
| Barthel Index before hospitalizationa) | 100 | 100 | 100 | 0.040 |
| (100–100) | (100–100) | (100–100) | ||
| ICU admission diagnosis | ||||
| Acute respiratory failure | 43 (21.2) | 30 (21.0) | 22 (36.7) | 0.074 |
| Cardiovascular disease | 74 (36.5) | 48 (33.6) | 10 (16.7) | |
| Gastric or colonic surgery | 31 (15.3) | 23 (16.1) | 8 (13.3) | |
| Sepsis, non-pulmonary origin status | 32 (15.8) | 22 (15.4) | 12 (20.0) | |
| Other diagnoses | 23 (11.3) | 20 (14.0) | 8 (13.3) | |
| APACHE II score | 20 (14–25) | 18 (13–24) | 21 (16–28) | - |
| SOFA at ICU admission | 7 (4–10) | 6 (3–9) | 8 (6–10) | 0.001 |
| Highest IMS during ICU stay | 6 (3–8) | 7 (4–9) | 4 (2–7) | <0.001 |
| ICU length of stayb) | 5 (4–9) | 5 (3–7) | 8 (4–14) | 0.001 |
| Incidence of ICU-acquired weakness | 42 (20.7) | 20 (14.0) | 22 (36.7) | <0.001 |
| Hospital length of stayb) | 18 (10–25) | 25 (19–44) | 32 (21–67) | 0.104 |
| EQ-5D-5L at hospital dischargeb) | 0.7 (0.4–0.9) | 0.8 (0.7–0.9) | 0.4 (0.2–0.6) | <0.001 |
| In-hospital mortality | 25 (12.3) | 0 (0) | 25 (41.7) | - |
Values are presented as median (IQR) or number (%).
ADL, activity of daily living; ICU, intensive care unit; APACHE II, Acute Physiology and Chronic Health Evaluation II; SOFA, Sequential Organ Failure Assessment; IMS, ICU mobility scale; EQ-5D-5L, EuroQol-5 Dimensions-5 Levels.
a)Barthel Index before hospitalization was scored at the time of ICU admission based on the information from the family or the patients if they were conscious.
b)Excluding fatal case.
Relationship between ADL independence and the highest IMS in the ICU
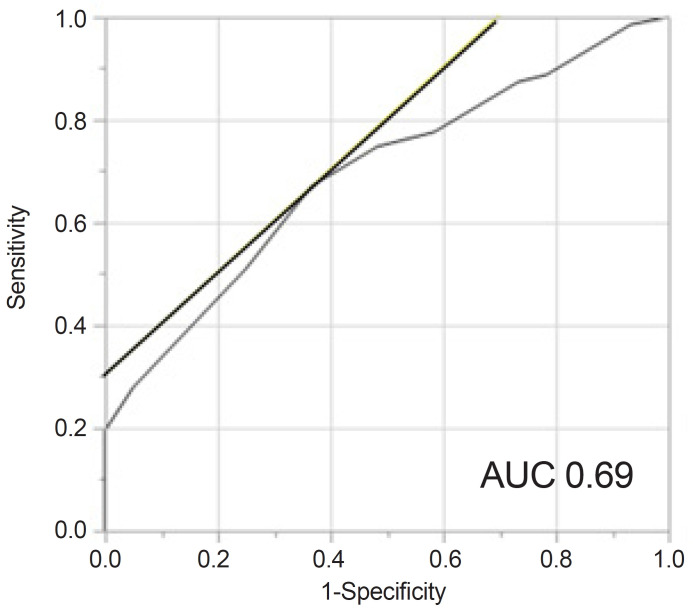
No multicollinearity was found between the variables highest IMS, age, BMI, BI before hospitalization, sepsis, non-pulmonary status, and SOFA score at ICU admission. Performing multivariable logistic regression analysis using these variables, revealed that the highest IMS (OR, 1.22; 95% CI, 1.07–1.38; p=0.002), age (OR, 0.93; 95% CI, 0.89–0.96; p<0.001), and SOFA score (OR, 0.91; 95% CI, 0.83–1.01; p=0.069) were independent factors for independence in ADL at hospital discharge (Table 2). On performing multivariable logistic regression analysis with ICU (>7 days) and hospital length of stay (>28 days) and EQ-5D-5L (>0.5 point) at discharge as objective variables, we found that EQ-5D-5L at discharge (OR, 1.14; 95% CI, 1.01–1.31; p=0.039) was significantly associated with the highest IMS (Table 3). Fig. 2 shows the ROC curve for the highest IMS during ICU stay as a predictor of ADL at discharge. The cutoff value was IMS 6 (specificity, 0.67; sensitivity, 0.70; AUC, 0.69).
Table 2.
Multivariable logistic regression analysis of independent variables for the activity of daily living independence at hospital discharge
| Variable | Activity of daily living independence | ||
|---|---|---|---|
| Odds ratio | 95% CI | p-value | |
| Highest ICU mobility scale | 1.22 | 1.07–1.38 | 0.002 |
| Age | 0.93 | 0.89–0.96 | <0.001 |
| Body mass index | 1.04 | 0.96–1.14 | 0.296 |
| Charlson Comorbidity Index | 1.11 | 0.92–1.34 | 0.264 |
| Barthel Index before hospitalization | 1.01 | 0.97–1.04 | 0.574 |
| Sepsis, non-pulmonary origin status | 0.88 | 0.34–2.24 | 0.785 |
| SOFA at ICU admission | 0.91 | 0.83–1.01 | 0.069 |
Model χ2-test p<0.01; AUC, 0.81.
95% CI, 95% confidence interval; ICU, intensive care unit; SOFA, Sequential Organ Failure Assessment.
Table 3.
Association between highest ICU mobility scale and other outcomes, excluding fatal case
| Unadjusted odds ratio (95% CI) | p-value | Adjusted odds ratioa) (95% CI) | p-value | |
|---|---|---|---|---|
| ICU length of stay (>7 day) | 0.94 (0.84–1.05) | 0.271 | 1.01 (0.89–1.15) | 0.837 |
| Hospital length of stay (>28 day) | 0.91 (0.82–1.01) | 0.068 | 0.96 (0.86–1.08) | 0.526 |
| EQ-5D-5L at hospital discharge (>0.5 point) | 1.20 (1.07–1.36) | 0.002 | 1.14 (1.01–1.31) | 0.039 |
ICU, intensive care unit; 95% CI, confidence interval; EQ-5D-5L, Euro Qol-5 Dimensionss-5 Levels.
a)The covariates in the multivariable analysis included age, body mass index, Charlson Comorbidity Index, Barthel Index before hospitalization, sepsis, non-pulmonary origin status, Sequential Organ Failure Assessment score at ICU admission.
Fig. 2.
Receiver operating characteristic curve for highest intensive care unit mobility scale and independence of activity daily living. AUC, area under the curve.
Maximum level of activity from day 1 to 7
All patients in this study started rehabilitation within 48 hours. A total of 164 patients (80.8%) were mobilized (sit on the edge of the bed or a higher degree of mobility) within the first seven days of their ICU stay. On day 1 of ICU admission, 128 out of 203 patient (63.1%) underwent rehabilitation at the IMS 0 level, 51 patients (25.1%) at IMS 1–2, 8 patients (3.9%) at IMS 3, 11 patients (5.4%) at IMS 4–6, and 5 patient (2.5%) at IMS 7–10.
The number of patients who underwent rehabilitation with an IMS of zero decreased from 63% to 19% on day 3, and to 7% on day 7. The fraction of patients with IMS 1–2 did not change within seven days of ICU admission. The fraction of patients with IMS or more is low on ICU days 1 (12%) and 2 (26%), increased from day 3 (47%) to 5 (57%), and remained at the same level on ICU days 6 (56%) and 7 (64%) (Supplementary Table S3). All rehabilitation sessions were performed for 20 minutes regardless of intensity.
Sensitivity and subanalysis
Supplementary Fig. S1 and Table 4 show the results of the analysis of the relationship between independence in ADL at hospital discharge and the highest IMS in the ICU in the two groups of SOFA scores. Logistic regression analysis showed that the highest IMS was significantly correlated with ADL independence at hospital discharge (OR, 1.23; 95% CI, 1.03–1.46; adjusted p=0.016) when the SOFA score remained unchanged. In the ROC curve, the cutoff value was IMS 7 (specificity, 0.85; sensitivity, 0.63; AUC, 0.76).
Table 4.
Multivariate logistic regression analysis of independent variables for activity of daily living independence at hospital discharge with unchanged and worse SOFA score
| ADL independence group with unchanged SOFA score (n=104) | ADL independent group with worse SOFA score (n=39) | |||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Highest IMS | 1.43 | 1.16–1.76 | <0.001 | 1.17 | 1.02–1.34 | 0.020 |
| Odds ratio adjusted with covariatesa) | 1.23 | 1.03–1.46 | 0.016 | 1.14 | 0.95–1.41 | 0.095 |
SOFA, Sequential Organ Failure Assessment; ADL, activity of daily living; 95% CI, 95% confidence intervals; IMS, intensive care unit mobility scale.
a)The covariates in the multivariable analysis included age, body mass index, Charlson Comorbidity Index, Barthel Index before hospitalization.
In contact, logistic regression analysis showed that the highest IMS in the worse SOFA score group was not significantly correlated with ADL independence at hospital discharge (OR, 1.14; 95% CI, 0.95–1.41; adjusted p=0.095). In the ROC curve, the cutoff value was IMS 5 (specificity, 0.53; sensitivity, 0.63; AUC, 0.65). In the subanalysis, our results remained unchanged even upon excluding those who died in the hospital (Supplementary Table S4).
DISCUSSION
This study examined the association between ADL independence at the hospital discharge of critically ill patients admitted to the ICU and the mobilization level during their stay in the ICU. The highest IMS during ICU stay was significantly higher in the group with ADL independence at hospital discharge. Multivariate analysis also showed a significant association between ADL independence at hospital discharge and the highest IMS during ICU stay. To our knowledge, this is the first report of the association between independence in ADL at hospital discharge and mobilization level during an ICU stay.
Multivariable analysis showed that the highest IMS score during ICU stay was strongly associated with independence in ADL at hospital discharge. A previous study also reported that IMS during ICU admission was a predictor of home discharge, and our study had similar results [13]. The primary results of this study suggest that good functioning during ICU stay may be significantly related to ADL independence at discharge. The Katz and Barthel Indices used in conventional rehabilitation assessment, do not change significantly in the ICU, and it is difficult to make a difference [3]. On the other hand, recently, the IMS has been widely used early rehabilitation in the ICU because it can assess baseline function in more detail. Other measures of physical function that have been developed for use in the ICU include the Functional Status Score for the ICU [23], physical function in the ICU test [24], and medical research council scores [25]. However, there are limitations to the generalization in the ICU, such as the lack of reliability or validity evaluation in the ICU, and time-consuming measurements in these evaluation scales [26,27]. IMS has the advantage of being easy to assess, reliable when performed by a nurse or physiotherapist, takes less than a minute, and requires no special equipment. The IMS have demonstrated adequate levels of reliability when applied to diverse patient populations hospitalized in the ICU [13,28]. The advantages of IMS support its use in the ICU to measure a patient's daily mobility level. Furthermore, in this study, highest IMS during ICU stay was significantly associated with EQ-5D-5L at hospital discharge. The EQ-5D-5L primarily measures quality of life, with 3 out of 5 items related to ADL. Therefore, IMS may show an association not only with physical function, but also with physical quality of life at hospital discharge, suggesting that future studies should examine the relationship between mobilization level and other outcomes.
The area under the ROC curve showed similar results to previous studies on home discharge outcomes with 70% sensitivity, 67% specificity, and 69% accuracy [29]. Patients in this study were age older, tended to be more severe than in previous studies, and may have been influenced by the patient's condition (i.e., sedation or hemodynamic instability) in their degree of mobility in the ICU [13,23]. The IMS showed considerable accuracy in predicting independence in ADL with an AUC of 0.76 in the group worse SOFA score had not worsened since the ICU admission (unchanged SOFA group). In the study by Tipping et al. [29], the ROC curve for IMS was not determined. However, the higher the IMS at the time of ICU discharge, the better the discharge prediction by the logistic regression model. This seems logical from a clinical viewpoint, as more functional patients tend to perform ADL independently after the acute phase.
The IMS rating, which provided the highest accuracy for early determination of whether a patient was independent of ADL at hospital discharge had a strength of six or higher. A Japanese multicenter study investigating the safety of early mobilization reported that the incidence of adverse events increased with the mobilization level be-yond standing [15]. Delayed mobilization due to adverse events occurring while the patient is standing may be associated with independence in ADL at hospital discharge. Furthermore, the results of the subanalysis of this study showed that the highest IMS during the ICU stay was not associated with ADL independence at hospital discharge in patients who could not achieve the rehabilitation of IMS≥6 or worse SOFA score worsened during the ICU stay. Our study suggests that if the rehabilitation of IMS 6 or higher cannot be achieved in the ICU, the time to the first IMS of 6 or higher, including the total length of hospital stay, may predict ADL independence at hospital discharge. In this study, the incidence of ICU-AW was significantly higher in the ADL dependent group. There is a possibility that ICU-AW had a direct impact on the highest mobility level, and future investigation may be necessary the relationship between the incidence of ICU-AW and the highest IMS.
This study had some limitations. First, confounding factors that could not be adjusted for may have had a relatively large impact on the results. Second, the results were limited to short-term follow-up. Third, whether patients could receive rehabilitation at the bedside level or higher depended on the rehabilitation policy of each participating hospital. Fourth, the IMS is itself an assessment tool, consisting of classifications based on functional activity. Factors such as muscle strength, degree of ventilator support, and oxygen demand can cause patients to perceive different intensities during the same mobilization phase. This study may have lacked objectivity as a method for expressing exercise intensity. Future studies should use the variable “amount of rehabilitation” instead of focusing solely on mobilization level. A multicenter randomized controlled trial with more patients is needed to further validate these findings and investigate causality.
For the above reason, good function during ICU stay is significantly related to independence in ADL at hospital discharge. This finding argues with future prospective multicenter trials. In patients whose SOFA score do not show deterioration, the mobilization level achieved during ICU admission could be an important parameter for maximizing the beneficial effect on patient outcomes.
Acknowledgments
The authors would like to thank the study coordinators Dr Tetsuo Ikai, PT Gen Kudo, Ns Masako Shimada, PT Syouhei Yokota, PT Naoko Shima, Dr Maiko Mori, Ns Yayoi Honjo, Ns Ohno Mika, ST Takahiro Kanaya, Ns Yasuko Muranaka, Dr Hiromasa Harada, Dr Masahiro Tamashiro, PT Shohei Miyazato, PT Shogo Sakihama, Ns Ryo Nagato, Ns Shuhei Ike-guchi, PT Yoshiyuki Teranobu, PT Tsubasa Watanabe, PT Yuuiichi Miyagi, PT Hiroyuki Touyama, Ns Moromizato, Ns Ayako Kawasaki, Ns Noriyo Suzuki, Ns Sayaka Hosoi, PT Takahiro Fujita, PT Syohei Hachisu, Dr Hidehiko Nakano, Dr Hiromu Naraba, PT Hajime Katsukawa. The authors would also like to thank the entire ICU staff at all the participating hospital. The authors thank Akiko Kada, a biostatistician at Nagoya Medical Center, for providing assistance in reviewing the manuscript.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING INFORMATION
None.
AUTHOR CONTRIBUTION
Conceptualization: Watanabe S, Liu K. Methodology: Watanabe S, Liu K. Formal analysis: Watanabe S. Project administration: Morita Y. Visualization: Katsukawa H. Writing – original draft: Watanabe S. Writing – review and editing: Watanabe S, Liu K, Kozu R, Yasumura D, Yamauchi K, Katsukawa H, Suzuki K, Koike T, Morita Y. Approval of final manuscript: all authors.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.5535/arm.23056.
Criteria for physiological stability
The background information of the participating ICUs and the patients
Maximum level of activity from day 1 to 7
Multivariate logistic regression analysis of independent variables for activity of daily living independence at discharge, excluding fatal case
Receiver operating characteristic curve for highest intensive care unit mobility scale and independence of activity daily living with (A) unchanged and (B) worse Sequential Organ Failure Assessment (SOFA) score. AUC, area under the curve.
REFERENCES
- 1.Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40:502–9. doi: 10.1097/CCM.0b013e318232da75. [DOI] [PubMed] [Google Scholar]
- 2.Myers EA, Smith DA, Allen SR, Kaplan LJ. Post-ICU syndrome: rescuing the undiagnosed. JAAPA. 2016;29:34–7. doi: 10.1097/01.JAA.0000481401.21841.32. [DOI] [PubMed] [Google Scholar]
- 3.Ad Hoc Committee for Early Rehabilitation. The Japanese Society of Intensive Care Medicine [Evidence based expert consensus for early rehabilitation in the intensive care unit] J Jpn Soc Intensive Care Med. 2017;24:255–303. Japanese. [Google Scholar]
- 4.Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017;43:171–83. doi: 10.1007/s00134-016-4612-0. [DOI] [PubMed] [Google Scholar]
- 5.Watanabe S, Iida Y, Ito T, Mizutani M, Morita Y, Suzuki S, et al. Effect of early rehabilitation activity time on critically ill patients with intensive care unit-acquired weakness: a Japanese retrospective multicenter study. Prog Rehabil Med. 2018;3:20180003. doi: 10.2490/prm.20180003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nishida O, Ogura H, Egi M, Fujishima S, Hayashi Y, Iba T, et al. The Japanese Clinical Practice Guidelines for Management of Sepsis and Septic Shock 2016 (J-SSCG 2016) Acute Med Surg. 2018;5:3–89. doi: 10.1002/ams2.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–82. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. 2013;41:1543–54. doi: 10.1097/CCM.0b013e31827ca637. [DOI] [PubMed] [Google Scholar]
- 9.Watanabe S, Liu K, Morita Y, Kanaya T, Naito Y, Suzuki S, et al. Effects of mobilization among critically ill patients in the intensive care unit: a single-center retrospective study. Prog Rehabil Med. 2022;7:20220013. doi: 10.2490/prm.20220013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36:2238–43. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 11.Watanabe S, Liu K, Nakamura K, Kozu R, Horibe T, Ishii K, et al. Association between early mobilization in the ICU and psychiatric symptoms after surviving a critical illness: a multi-center prospective cohort study. J Clin Med. 2022;11:2587. doi: 10.3390/jcm11092587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watanabe S, Morita Y, Suzuki S, Kochi K, Ohno M, Liu K, et al. Effects of the intensity and activity time of early rehabilitation on activities of daily living dependence in mechanically ventilated patients. Prog Rehabil Med. 2021;6:20210054. doi: 10.2490/prm.20210054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tymkew H, Norris T, Arroyo C, Schallom M. the use of physical therapy ICU assessments to predict discharge home. Crit Care Med. 2020;48:1312–8. doi: 10.1097/CCM.0000000000004467. [DOI] [PubMed] [Google Scholar]
- 14.Denehy L, Lanphere J, Needham DM. Ten reasons why ICU patients should be mobilized early. Intensive Care Med. 2017;43:86–90. doi: 10.1007/s00134-016-4513-2. [DOI] [PubMed] [Google Scholar]
- 15.Katsukawa H, Ota K, Liu K, Morita Y, Watanabe S, Sato K, et al. Risk factors of patient-related safety events during active mobilization for intubated patients in intensive care units-a multi-center retrospective observational study. J Clin Med. 2021;10:2607. doi: 10.3390/jcm10122607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watanabe S, Kotani T, Taito S, Ota K, Ishii K, Ono M, et al. Determinants of gait independence after mechanical ventilation in the intensive care unit: a Japanese multicenter retrospective exploratory cohort study. J Intensive Care. 2019;7:53. doi: 10.1186/s40560-019-0404-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hodgson C, Needham D, Haines K, Bailey M, Ward A, Harrold M, et al. Feasibility and inter-rater reliability of the ICU Mobility Scale. Heart Lung. 2014;43:19–24. doi: 10.1016/j.hrtlng.2013.11.003. Erratum in: Heart Lung 2014;43:388. [DOI] [PubMed] [Google Scholar]
- 18.Shiroiwa T, Ikeda S, Noto S, Igarashi A, Fukuda T, Saito S, et al. Comparison of value set based on DCE and/or TTO data: scoring for EQ-5D-5L health states in Japan. Value Health. 2016;19:648–54. doi: 10.1016/j.jval.2016.03.1834. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe S, Liu K, Morita Y, Kanaya T, Naito Y, Arakawa R, et al. Changes in barriers to implementing early mobilization in the intensive care unit: a single center retrospective cohort study. Nagoya J Med Sci. 2021;83:443–64. doi: 10.18999/nagjms.83.3.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrold ME, Salisbury LG, Webb SA, Allison GT, Australia and Scotland ICU Physiotherapy Collaboration Early mobilisation in intensive care units in Australia and Scotland: a prospective, observational cohort study examining mobilisation practises and barriers. Crit Car. 2015;19:336. doi: 10.1186/s13054-015-1033-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel BK, Pohlman AS, Hall JB, Kress JP. Impact of early mobilization on glycemic control and ICU-acquired weakness in critically ill patients who are mechanically ventilated. Chest. 2014;146:583–9. doi: 10.1378/chest.13-2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stephens MA. EDF statistics for goodness of fit and some comparisons. J Am Stat Assoc. 1974;69:730–7. [Google Scholar]
- 23.Huang M, Chan KS, Zanni JM, Parry SM, Neto SG, Neto JA, et al. Functional Status Score for the ICU: an international clinimetric analysis of validity, responsiveness, and minimal important difference. Crit Care Med. 2016;44:e1155–64. doi: 10.1097/CCM.0000000000001949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Denehy L, de Morton NA, Skinner EH, Edbrooke L, Haines K, Warrillow S, et al. A physical function test for use in the intensive care unit: validity, responsiveness, and predictive utility of the physical function ICU test (scored) Phys Ther. 2013;93:1636–45. doi: 10.2522/ptj.20120310. [DOI] [PubMed] [Google Scholar]
- 25.Hermans G, Clerckx B, Vanhullebusch T, Segers J, Vanpee G, Robbeets C, et al. Interobserver agreement of Medical Research Council sum-score and handgrip strength in the intensive care unit. Muscle Nerve. 2012;45:18–25. doi: 10.1002/mus.22219. [DOI] [PubMed] [Google Scholar]
- 26.Thrush A, Rozek M, Dekerlegand JL. The clinical utility of the functional status score for the intensive care unit (FSS-ICU) at a long-term acute care hospital: a prospective cohort study. Phys Ther. 2012;92:1536–45. doi: 10.2522/ptj.20110412. Erratum in: Phys Ther 2013;93:282. [DOI] [PubMed] [Google Scholar]
- 27.Skinner EH, Berney S, Warrillow S, Denehy L. Development of a physical function outcome measure (PFIT) and a pilot exercise training protocol for use in intensive care. Crit Care Resusc. 2009;11:110–5. [PubMed] [Google Scholar]
- 28.Nydahl P, Wilkens S, Glase S, Mohr LM, Richter P, Klarmann S, et al. The German translation of the Perme Intensive Care Unit Mobility Score and inter-rater reliability between physiotherapists and nurses. Eur J Physiother. 2017;20:109–15. [Google Scholar]
- 29.Tipping CJ, Bailey MJ, Bellomo R, Berney S, Buhr H, Denehy L, et al. The ICU mobility scale has construct and predictive validity and is responsive. A multicenter observational study. Ann Am Thorac Soc. 2016;13:887–93. doi: 10.1513/AnnalsATS.201510-717OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Criteria for physiological stability
The background information of the participating ICUs and the patients
Maximum level of activity from day 1 to 7
Multivariate logistic regression analysis of independent variables for activity of daily living independence at discharge, excluding fatal case
Receiver operating characteristic curve for highest intensive care unit mobility scale and independence of activity daily living with (A) unchanged and (B) worse Sequential Organ Failure Assessment (SOFA) score. AUC, area under the curve.