Abstract
Purpose: This study aimed to show the outcomes of isolated tricuspid valve replacement (ITVR) after left-sided valve surgery (LSVS).
Methods: Patients who underwent ITVR after LSVS were divided into bioprosthetic tricuspid valve (BTV) and mechanical tricuspid valve (MTV) groups. Clinical data were collected and analyzed between groups.
Results: 101 patients were divided into BTV (n = 46) and MTV (n = 55) groups. The mean ages of the BTV and MTV groups were 63.4 ± 8.9 and 52.4 ± 7.6 years, respectively (P <0.01). There was no significant difference in 30-day mortality (BTV 10.9% vs. MTV 5.5%), early postoperative complications, and long-term tricuspid valve (TV)-related adverse events between these two groups. New-onset renal insufficiency was an independent risk factor for early mortality. Survival rates in the BTV group were 94.8% ± 3.6%, 86.5% ± 6.5%, and 54.2% ± 17.6% and in the MTV group were 96.0% ± 2.8%, 79.0% ± 7.4%, and 59.4% ± 14.8% at 1, 5, and 10 years, respectively (P = 0.826).
Conclusion: The TV prosthesis selection in ITVR after LSVS seems to not affect 30-day mortality and early postoperative complications. Long-term survival and the occurrence of TV-related events were also comparable between these two groups.
Keywords: isolated tricuspid valve replacement, left-sided valve surgery, bioprosthetic tricuspid valve, mechanical tricuspid valve, long-term outcome
Introduction
Tricuspid regurgitation (TR) is a common condition that has been overlooked compared to left-sided valve diseases. A large-scale investigation study in China showed that moderate and severe TR rates were 2.22% and 1.39%, respectively.1) Long-term severe TR seriously affects the quality of patients’ life and is an independent risk factor associated with worse survival.2) A considerable proportion of moderate to severe TR occurs after left-sided valve surgery (LSVS) for various reasons,3) especially in those with rheumatic valvular heart disease.4) When conservative treatment or tricuspid valve (TV) repair fails, isolated tricuspid valve replacement (ITVR) may be the only effective approach. However, ITVR after LSVS is rarely performed due to its high operative mortality and poor prognosis.5) Data from Guangdong Provincial People’s Hospital show that in the past 20 years, more than 15000 TV surgery were performed, whereas isolated TV surgery after LSVS accounted for only 1.1%.6)
The optimal type of TV prosthesis is a subject of ongoing debate. The limited durability of bioprosthetic tricuspid valves (BTVs) and the higher rate of thrombotic events in mechanical tricuspid valves (MTVs) have always been a controversy for both the doctors and patients to make an appropriate decision. The conclusive evidence on the better choice of TV prosthetic is lacking.
Patients undergoing ITVR after LSVS are at greater risk than those undergoing initial ITVR,6,7) and few studies are reported on the optimal selection of TV prosthesis for these patients. Therefore, the present study was conducted to analyze the short-term and long-term outcomes of patients who underwent bioprosthetic and mechanical ITVR after LSVS, focusing on operative mortality, early postoperative complications, long-term survival, and TV-related events.
Materials and Methods
This study was approved by the Ethics Committee of Changhai Hospital affiliated to Naval Medical University (NO.CHEC2018-136), and individual consent for this retrospective analysis was waived.
Study population
This study reviewed patients who underwent ITVR at Shanghai Changhai Hospital from 2009 to 2020. Of these patients, those who underwent transcatheter TV replacement or initial TV replacement were excluded. A total of 101 patients who underwent ITVR were enrolled in the present study; all patients had undergone LSVS before. These patients were divided into two groups, 46 in the BTV group and 55 in the MTV group as shown in Supplementary Fig. 1. (The supplementary figures are available online.) The primary outcome was defined as the all-cause death during the perioperative period and follow-up. The secondary outcomes were adverse events at the early postoperative stage and long-term TV-related events during follow-up.
Operative strategy
The anterolateral mini-thoracotomy incision approach was adopted, and femoral arteriovenous cannulation was used to establish cardiopulmonary bypass. Right atrium incision was adopted after blocking of the upper and lower vena cava. ITVR was performed under mild hypothermia conditions on a beating heart with the assistant of parallel extracorporeal circulation. The TV prosthesis selection was decided by the surgeon in combination with a preoperative comprehensive evaluation and post-thoracotomy exploration results.
Follow-up
The data of patients during hospitalization were collected from the electronic medical record system of Shanghai Changhai Hospital. The patients were arranged for follow-up at outpatient at 3 and 6 months after discharge. After that, patients’ condition was mainly obtained through phone contact with patients or their relatives. The follow-up period depended on the patient’s condition but at least once a year. Follow-up data included descriptions of death, reintervention of TV, and other adverse events. The end points were defined as all-cause death and reintervention for TV. Completeness of follow-up was 96.8% (90 of 93 cases).
Statistical analysis
Normally distributed continuous variables and continuous variables without normal distribution are stated as mean ± standard deviation and median (first quartile, third quartile), respectively. Categorical variables are depicted as absolute numbers (proportions). For quantitative data, Student’s t-test or Mann–Whitney U test was used to identify difference between the two groups. For categorical data, the chi-squared test was used to evaluate the differences in percentage. Significant variables associated with 30-day mortality in the univariate analysis (P <0.1) were analyzed by the logistic regression model for multivariable analysis. Kaplan–Meier analysis was used for the evaluation of survival and freedom from reoperation, and the log-rank test was used to test for significance. The statistical analysis was performed by SPSS-V26.0 software. In all analyses, P <0.05 was considered statistically significant.
Results
Patient characteristics
In all, 101 patients were enrolled in this study. They were divided into the BTV group (n = 46) and the MTV group (n = 55) according to the type of TV prosthesis. The preoperative characteristics of patients are listed in Table 1. Patients in the BTV group were significantly older than those in the MTV group (63.4 ± 8.9 vs. 52.4 ± 7.6 years; P <0.01). There were no significant differences in preoperative comorbidities such as hypertension, diabetes mellitus, chronic obstructive pulmonary disease, chronic renal insufficiency, atrial fibrillation, and stroke history between the two groups. Among the main preoperative laboratory examination, albumin in the BTV group (40.9 ± 3.6) was higher than that in the MTV group (39.3 ± 3.6) with a statistically significant difference (P <0.01). Other preoperative results such as hemoglobin, creatinine, and total bilirubin were not significantly different between the two groups. Echocardiography results showed no significant difference in the TR volume between the two groups. The median right atrial volume were 169 mL and 207 mL in the BTV and MTV groups, respectively. The difference between the two groups was statistically significant (P = 0.035). Of note, the etiology of TR was not statistically different in the two groups.
Table 1. Preoperative characteristics.
| Preoperative | BTV group (n = 46) | MTV group (n = 55) | P |
| Age (years) | 63.4 ± 8.9 | 52.4 ± 7.6 | <0.01** |
| Sex (female) | 33 (71.7) | 37 (67.3) | 0.628 |
| BMI (kg/m2) | 23.1 ± 6.2 | 21.7 ± 3.4 | 0.140 |
| Diabetes mellitus (%) | 5 (10.9) | 3 (5.5) | 0.526 |
| Hypertension (%) | 5 (10.9) | 1 (1.8) | 0.135 |
| Smoking (%) | 3 (6.5) | 3 (5.5) | 1.000 |
| COPD (%) | 1 (2.2) | 4 (7.3) | 0.474 |
| Chronic kidney disease (%) | 0 (0) | 1 (1.8) | 1.000 |
| History of stroke (%) | 1 (2.2) | 2 (3.6) | 1.000 |
| NYHA class ≥3 (%) | 34 (73.9) | 35 (63.6) | 0.269 |
| LVEF (%) | 61.4 ± 8.3 | 62.5 ± 7.8 | 0.496 |
| Atrial fibrillation (%) | 36 (78.3) | 42 (76.4) | 1.000 |
| Hemoglobin (g/L) | 116.0 ± 20.9 | 115.7 ± 23.2 | 0.944 |
| Albumin (g/L) | 40.9 ± 3.6 | 39.3 ± 3.6 | 0.026 |
| Creatinine (μmoI/L) | 70.0 ± 23.9 | 70.6 ± 17.6 | 0.885 |
| Total bilirubin (μmoI/L) | 23.4 ± 14.2 | 24.1 ± 12.1 | 0.804 |
| Hepatomegaly (%) | 20 (43.5) | 34 (61.8) | 0.066 |
| TR (mL) | 55 (30.8, 70.7) | 56 (35, 84) | 0.449 |
| Right atrial volume (mL) | 169.0 (118.8, 244.3) | 207.0 (146.5, 321.5) | 0.035 * |
| Aetiology of TR (%) | 0.316 | ||
| Rheumatic | 31 (67.4) | 42 (76.4) | |
| Non rheumatic | 15 (32.6) | 13 (23.6) |
*P <0.05, **P <0.01. BTV: bioprosthetic tricuspid valve; MTV: mechanical tricuspid valve; BMI: body mass index; COPD: chronic obstructive pulmonary disease; NYHA: New York Heart Association; LVEF: left ventricular ejection fraction; TR: tricuspid regurgitation
Previous cardiac surgery
The previous surgical history of the patients is shown in Table 2. All patients had undergone LSVS. In all, 25 patients (54.3%) in the BTV group and 36 patients (65.4%) in the MTV group had undergone mitral valve replacement with or without TV surgery. A total of 18 patients (39.2%) in the BTV group and 17 patients (30.9%) in the MTV group had undergone double valve replacement with or without TV surgery. Fewer patients had undergone aortic valve replacement. There was no significant difference in previous surgical history between the two groups.
Table 2. Previous surgery.
| Previous cardiac surgery (%) | BTV group (n = 46) | MTV group (n = 55) | P |
| MVR | 18 (39.1) | 23 (41.8) | 0.840 |
| MVR + TV surgery | 7 (15.2) | 13 (23.6) | 0.326 |
| AVR | 3 (6.5) | 0 (0) | 0.182 |
| AVR + TV surgery | 0 (0) | 2 (3.6) | 0.556 |
| DVR | 13 (28.3) | 13 (23.6) | 0.652 |
| DVR + TV surgery | 5 (10.9) | 4 (7.3) | 0.779 |
MVR: mitral valve replacement; AVR: aortic valve replacement; DVR: double valve replacement; TV: tricuspid valve; BTV: bioprosthetic tricuspid valve; MTV: mechanical tricuspid valve
Intraoperative data and postoperative characteristics
Operative details and postoperative characteristics are presented in Table 3. The cardiac pulmonary bypass time in the BTV group and the MTV group was 62.0 (49.0, 82.3) minutes and 56.0 (46.0, 84.0) minutes, respectively. There was no significant difference between the two groups. The intraoperative mean arterial pressure and minimum nasopharyngeal temperature were not statistically different in the two groups. It is worth mentioning that TV prosthesis size differed between the two groups. Although the 31 mm TV prosthesis was in the predominant position in both two groups (BTV group 50.0% vs. MTV group 78.2%), the proportion of 29 mm TV prosthesis in the BTV group (47.8%) was higher than that in the MTV group (18.2%); the difference between the two groups is statistically significant (P <0.01).
Table 3. Operative details and postoperative characteristics.
| Operative data | BTV group (n = 46) | MTV group (n = 55) | P |
| CPB time (min) | 62.0 (49.0, 82.3) | 56.0 (46.0, 84.0) | 0.226 |
| Minimum nasopharyngeal temperature (°C) | 33.7 ± 1.0 | 34.0 ± 1.0 | 0.312 |
| Mean arterial pressure (mmHg) | 85.1 ± 12.0 | 84.6 ± 14.2 | 0.825 |
| Prosthetic valve size (%) | <0.01** | ||
| 31 mm | 23 (50.0) | 43 (78.2) | |
| 29 mm | 22 (47.8) | 10 (18.2) | |
| 27 mm | 1 (2.2) | 2 (3.6) | |
| In-hospital (early) events | |||
| Early postoperative drainage (24 h) | 390.0 (152.5, 572.5) | 300.0 (125.0, 560.0) | 0.635 |
| Ventilator support (h) | 19.5 (11.5, 27.5) | 17.0 (10.0, 22.0) | 0.165 |
| ICU stay (h) | 65.0 (42.0, 128.0) | 58.0 (43.0, 73.5) | 0.497 |
| Hospital stay (days) | 20.0 (15.5, 28.5) | 18.0 (15.0, 22.0) | 0.223 |
| Tracheotomy (%) | 4 (8.7) | 1 (1.8) | 0.260 |
| Reoperation for bleed (%) | 3 (6.5) | 1 (1.8) | 0.487 |
| Pericardial effusion (%) | 3 (6.5) | 4 (7.3) | 1.000 |
| Pleural effusion (%) | 35 (76.1) | 34 (61.8) | 0.139 |
| Lung infection (%) | 10 (21.7) | 5 (9.1) | 0.134 |
| New onset renal failure (%) | 4 (8.7) | 3 (5.5) | 0.806 |
| Sepsis (%) | 2 (4.3) | 0 (0) | 0.398 |
| Stroke (%) | 1 (2.2) | 0 (0) | 0.928 |
| Operative mortality | 5 (10.9) | 3 (5.5) | 0.526 |
**P <0.01. CPB: cardiac pulmonary bypass; BTV: bioprosthetic tricuspid valve; MTV: mechanical tricuspid valve; ICU: intensive care unit
A total of 8 patients died within 30 days after surgery; the 30-day mortality was 7.9%. In all, 5 patients (10.9%) died in the BTV group and 3 patients (5.5%) died in the MTV group (P = 0.526). The postoperative ventilator support time in the BTV group (19.5 hours) was longer than that in the MTV group (17.0 hours) but without significance. In addition, the intensive care unit duration and total length of hospital stay in the BTV group were higher than those in the MTV group without statistical significance. There were also no significant differences between the two groups in the incidence of other postoperative adverse events such as reoperation for hemostasis, pericardial or pleural effusion, tracheotomy, lung infection, new onset renal insufficiency (defined as postoperative acute renal failure requiring dialysis), sepsis, and stroke.
Multivariable logistic regression analysis
The univariate analysis was performed to identify risk factors for 30-day mortality. All the 101 patients were divided into survival group and non-survival group. The perioperative data of 93 patients (92.1%) in the survival group and 8 patients (7.9%) in the non-survival group were compared. The results are shown in Supplementary Tables 1–3. All the factors (P <0.1) were enrolled in the multivariable logistic analysis; the results are presented in Table 4. The logistic regression analysis results showed that new onset renal insufficiency was an independent risk factor for 30-day mortality (OR = 25.70, P = 0.020).
Table 4. Logistic regression of in-hospital mortality.
| Variable | OR | 95% CI | P |
| Age (years) | 1.09 | 0.95–1.25 | 0.203 |
| Creatinine (μmoI/L) | 1.01 | 0.97–1.06 | 0.592 |
| Mean arterial pressure (mmHg) | 0.98 | 0.90–1.06 | 0.558 |
| Ventilator support (h) | 1.00 | 1.00–1.01 | 0.486 |
| Lung infection (%) | 5.53 | 0.55–55.64 | 0.147 |
| New onset renal failure (%) | 25.70 | 1.65–399.66 | 0.020 * |
*P <0.05. OR: odds ratio; CI: confidence interval
Long-term outcomes
The average follow-up time was 61.5 ± 37.8 months, and a total of 90 (96.8%) patients completed the follow-up. In all, 16 patients died after discharge during the follow-up. The causes of death were cardiac death in 13 patients, cancer in 2 patients, and accidents in 1 patient. Among the 16 deaths, 7 cases were in the BTV group and 9 cases were in the MTV group. There was no significant difference between the two groups. Kaplan–Meyer survival analysis was used to evaluate the long-term survival of two groups. Survival rates in the BTV group were 94.8% ± 3.6%, 86.5% ± 6.5%, and 54.2% ± 17.6% and in the MTV group were 96.0% ± 2.8%, 79.0% ± 7.4%, and 59.4% ± 14.8% at 1, 5, and 10 years, respectively (P = 0.826, Fig. 1A).
Fig. 1. Long-term survival (A) and freedom from TV-related reoperation (B). BTV: bioprosthetic tricuspid valve; MTV: mechanical tricuspid valve; TV: tricuspid valve.
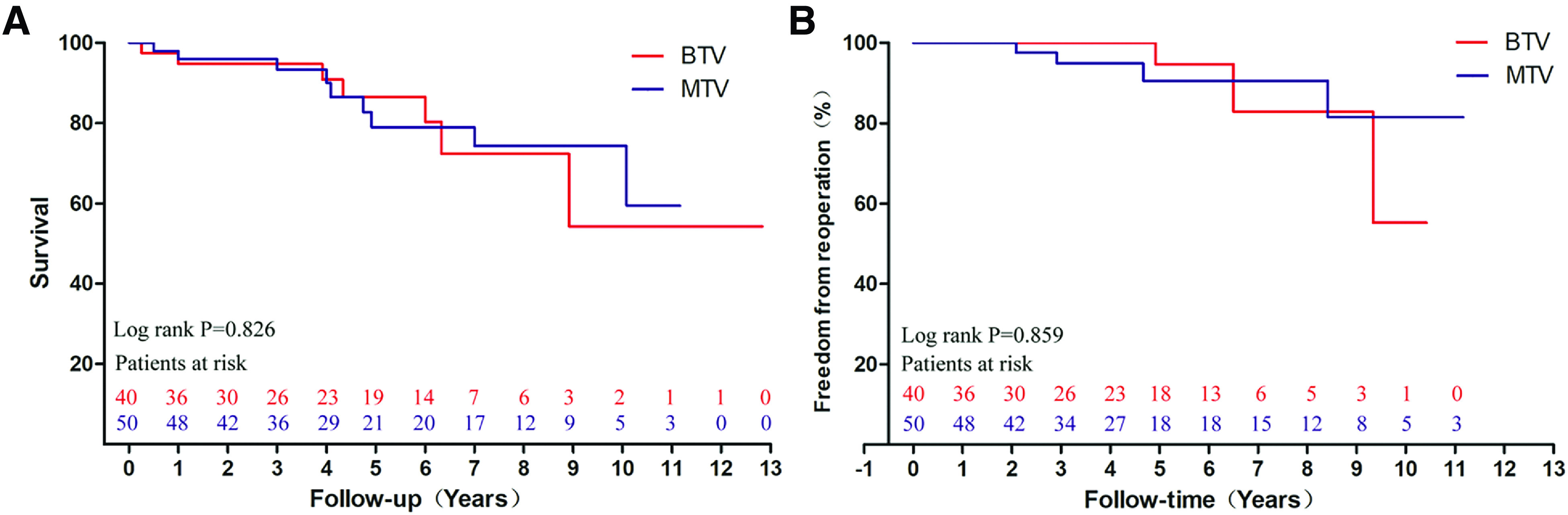
During follow-up, 8 patients underwent cardiac reoperation intervention, including 7 cases for TV surgery and 1 case for aortic valve surgery. In the BTV group, the indication for 2 patients was TV failure and 1 patient was tricuspid paravalvular leakage, and in the MTV group, 2 patients for thrombosis and 2 patients for TV dysfunction. Additionally, 1 patient diagnosed with aortic valve regurgitation underwent aortic valve replacement during follow-up. There was no significant difference in the reoperation between the two groups. Freedom from TV reoperation in the BTV group was 94.7% ± 5.1% and 55.3% ± 23.9% at 5 and 10 years, respectively. Freedom from TV reoperation in the MTV group was 90.6% ± 5.4% and 81.5 ± 9.9% at 5 and 10 years, respectively (P = 0.868, Fig. 1B).
A total of 3 patients underwent stroke during the follow-up: 2 cases were in the BTV group and 1 case was in the MTV group. In addition, 1 patient in the MTV group underwent TV thrombosis; the clinical symptoms were relieved after thrombolytic therapy.
Discussion
Isolated TV surgery remains relatively infrequent due to significant comorbidities in patients and poor long-term outcomes.8) Zack and associates reported 5005 isolated TV operations from 2004 to 2014, with an overall operative mortality of 8.8%, which did not vary across the study period.9) However, most of the TR patients are in poor clinical condition with a terrible quality of life; 31%–97% of them are in New York Heart Association functional class III or IV.10) The patients with TR tend to be asymptomatic for a long period. The majority of them are initially treated with a conservative strategy and are only referred for surgical treatment when they reach a clinically advanced stage. Surgical intervention is an important method to alleviate the clinical symptoms of patients. However, there are no specific criteria for the indications for surgery, the appropriate time of intervention, and the method of surgery. TV surgery is often performed concomitantly with other cardiac surgery. A review of the Society of Thoracic Surgeons database shows that 86% of TV surgery was performed in conjunction with another major cardiac procedure, usually LSVS.11) Current guidelines strongly recommend concomitant repair of moderate to severe TR at the time of LSVS.12) However, TR caused by various reasons after LSVS is not uncommon. When conservative treatment or TV repair is invalid, a considerable number of patients with moderate to severe TR have to undergo TV replacement surgery.5)
Our study retrospectively analyzed 101 patients who underwent ITVR after LSVS, and focused on short-term and long-term outcomes between different types of TV prostheses. By comparing the 30-day postoperative mortality, early complications, long-term survival, and occurrence of adverse TV events between the BTV group and MTV group, we found that the type of TV prosthesis did not affect 30-day mortality and the occurrence of major complications in the early postoperative period, as well as long-term survival. These results were consistent with the meta-analysis by Rizzoli et al. who compared 646 bioprosthetic valves and 514 mechanical prostheses from 11 studies and found no difference in the early and long-term survival.13) We also found that there was no significant difference between the two groups in the risk of TV reoperation and occurrence of TV-related adverse events during follow-up, suggesting that the choice of TV prosthesis did not have an influence on the clinical outcome of ITVR patients with the history of LSVS. Moreover, Fang et al. demonstrated that the Kaplan–Meier survival rates at 1 year and 5 years were 97.7% and 90.0%, respectively, after analyzing the mid-term results and risks of ITVR following LSVS, which enrolled 91 cases. In addition, the valve-type selection had no significant effect on the survival of TR patients who underwent ITVR.14)
The 2021 ESC/EACTS Guidelines for Valvular Heart Disease recommend prosthetic valve selection based on the patient’s lifestyle and personal preferences, as well as their age-related risks and benefits.15) However, the choice of the TV prosthesis remains controversial, and there is no clear evidence to show which prosthesis is the better choice. In most cases, the TV prosthesis selection is based on the surgeon’s comprehensive evaluation and the patients’ preference. BTV was considered a better option in the past16); however, it remains unclear whether BTV replacement has better survival and fewer TV-related complications.
Bioprostheses take the advantage of being free from permanent anticoagulation therapy and have a lower risk of valve thrombosis compared with mechanical valves.17) Péterffy et al. supposed that the higher rate of mechanical valve thrombosis in the tricuspid position is a result of lower pressure on the right side of the heart system and low prostacyclin concentration of venous blood to a great extent.18) Some researchers also pointed out that the low pressure in the right side of the heart may be also associated with the longer durability of bioprosthetic valves at the tricuspid position.19) Kang and colleagues even advocated that BTV should be used aggressively in younger patients because of the poor life expectancy of patients with TR requiring surgical intervention.20) In our study, the mean age of patients in the BTV group was more than that in the MTV group. However, in the long term, the use of bioprostheses in younger patients may facilitate later interventional procedures due to the boom of transcatheter TV replacement.
On the contrary, advocates of MTV insisted that reoperation for the TV is an important consideration for prosthetic valve selection. They believed that with the continuous development of mechanical valves, the new generations of bileaflet mechanical valves functioned well with low gradient, low turbulence, and optimal durability.21) Whereas the failure of bioprostheses is unavoidable, reoperation seems inevitable, especially for younger patients. Spampinato et al. figured out that although bioprostheses in the tricuspid position have a lower degeneration risk than those in the left-sided position, they are still limited by fibro calcifications and fatigue-related disruption.22) Furthermore, selective patients undergoing ITVR require long-term anticoagulation therapy since a majority of them undergo mechanical valve replacement previously or are with atrial fibrillation.23) In our study, most patients underwent ITVR based on existing mechanical valves of the left-sided heart system and 78 (77.2%) patients suffered from atrial fibrillation. For these patients, the advantage of weaning from long-term anticoagulation therapy after BTV replacement seems not to be well represented.
Taken together, the present study demonstrates that no difference between MTV and BTV in short-term and long-term outcomes was identified. The decision-making should be based on the patients’ situation. We also suppose that all patients who undergo ITVR after LSVS should be carefully evaluated with periodic echocardiograms, and strict anticoagulation is necessary for all the MTV patients and some of the BTV patients with atrial fibrillation or prior mechanical valve replacement surgery in the left-sided heart system.
The main limitation of this study is that it is a retrospective study conducted in a single center. Results are prone to selection and recall bias. Moreover, the number of patients enrolled in our study is limited and hence the conclusion may be unreliable. In addition, this study covered a long time span; the surgical strategy, perioperative management, and the surgical technique of the surgeon may also potentially influence the results. A larger number of patients and extended follow-up are required to establish solid conclusions.
Conclusions
In conclusion, our study identifies that no significant difference exists between MTV and BTV in patients undergoing ITVR after LSVS in terms of short-term and long-term outcomes. We suppose that age is a crucial factor for TV prosthesis selection in ITVR; patients’ underlying disease, lifestyle, and previous surgical history should also be taken into account to make an appropriate decision.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82100383) and National Key Research and Development Program of China (Grant No. 2016YFC1100900).
Disclosure Statement
None declared.
Supplementary Material
References
- 1).Yang L, Chen H, Pan W, et al. Analyses for prevalence and outcome of tricuspid regurgitation in China: an echocardiography study of 134,874 patients. Cardiology 2019; 142: 40–6. [DOI] [PubMed] [Google Scholar]
- 2).Benfari G, Antoine C, Miller WL, et al. Excess mortality associated with functional tricuspid regurgitation complicating heart failure with reduced ejection fraction. Circulation 2019; 140: 196–206. [DOI] [PubMed] [Google Scholar]
- 3).Shiran A, Sagie A. Tricuspid regurgitation in mitral valve disease incidence, prognostic implications, mechanism, and management. J Am Coll Cardiol 2009; 53: 401–8. [DOI] [PubMed] [Google Scholar]
- 4).Izumi C, Miyake M, Takahashi S, et al. Progression of isolated tricuspid regurgitation late after left-sided valve surgery. Clinical features and mechanisms. Circ J 2011; 75: 2902–7. [DOI] [PubMed] [Google Scholar]
- 5).Park CK, Park PW, Sung K, et al. Early and midterm outcomes for tricuspid valve surgery after left-sided valve surgery. Ann Thorac Surg 2009; 88: 1216–23. [DOI] [PubMed] [Google Scholar]
- 6).Chen J, Hu K, Ma W, et al. Isolated reoperation for tricuspid regurgitation after left-sided valve surgery: technique evolution. Eur J Cardiothorac Surg 2020; 57: 142–50. [DOI] [PubMed] [Google Scholar]
- 7).Yang L, Zhou K, Yang YC, et al. Outcomes of redo-isolated tricuspid valve surgery after left-sided valve surgery. J Card Surg 2021; 36: 3060–9. [DOI] [PubMed] [Google Scholar]
- 8).Ejiofor JI, Neely RC, Yammine M, et al. Surgical outcomes of isolated tricuspid valve procedures: repair versus replacement. Ann Cardiothorac Surg 2017; 6: 214–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Zack CJ, Fender EA, Chandrashekar P, et al. National trends and outcomes in isolated tricuspid valve surgery. J Am Coll Cardiol 2017; 70: 2953–60. [DOI] [PubMed] [Google Scholar]
- 10).Guenther T, Noebauer C, Mazzitelli D, et al. Tricuspid valve surgery: a thirty-year assessment of early and late outcome. Eur J Cardiothorac Surg 2008; 34: 402–9; discussion, 409. [DOI] [PubMed] [Google Scholar]
- 11).Kilic A, Saha-Chaudhuri P, Rankin JS, et al. Trends and outcomes of tricuspid valve surgery in North America: an analysis of more than 50,000 patients from the Society of Thoracic Surgeons database. Ann Thorac Surg 2013; 96: 1546–52; discussion, 1552. [DOI] [PubMed] [Google Scholar]
- 12).Stephens EH, Borger MA. “Forgotten” valve or “enigmatic” valve? Further insights into the tricuspid valve in patients undergoing mitral valve surgery. J Thorac Cardiovasc Surg 2014; 148: 1962–4. [DOI] [PubMed] [Google Scholar]
- 13).Rizzoli G, Vendramin I, Nesseris G, et al. Biological or mechanical prostheses in tricuspid position? A meta-analysis of intra-institutional results. Ann Thorac Surg 2004; 77: 1607–14. [DOI] [PubMed] [Google Scholar]
- 14).Fang L Li W Zhang W et al. Mid-term results and risks of isolated tricuspid valve reoperation following left-sided valve surgery. Eur J Cardiothorac Surg 2018; 53: 1034–9. [DOI] [PubMed] [Google Scholar]
- 15).Vahanian A. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. 2021.
- 16).Hornick P, Harris PA, Taylor KM. Tricuspid valve replacement subsequent to previous open heart surgery. J Heart Valve Dis 1996; 5: 20–5. [PubMed] [Google Scholar]
- 17).Cheng Z, Fang T, Wang D, et al. Tricuspid valve replacement: mechanical or biological prostheses? A systematic review and meta-analysis. Heart Surg Forum 2021; 24: E209–14. [DOI] [PubMed] [Google Scholar]
- 18).Péterffy A, Szentkiralyi I. Mechanical valves in tricuspid position: cause of thrombosis and prevention. Eur J Cardiothorac Surg 2001; 19: 735–6. [DOI] [PubMed] [Google Scholar]
- 19).Carrier M, Hebert Y, Pellerin M, et al. Tricuspid valve replacement: an analysis of 25 years of experience at a single center. Ann Thorac Surg 2003; 75: 47–50. [DOI] [PubMed] [Google Scholar]
- 20).Kang Y, Hwang HY, Sohn SH, et al. Fifteen-year outcomes after bioprosthetic and mechanical tricuspid valve replacement. Ann Thorac Surg 2020; 110: 1564–71. [DOI] [PubMed] [Google Scholar]
- 21).Negm S, Arafat AA, Elatafy EE, et al. Mechanical versus bioprosthetic valve replacement in the tricuspid valve position: a systematic review and meta-analysis. Heart Lung Circ 2021; 30: 362–71. [DOI] [PubMed] [Google Scholar]
- 22).Spampinato N, Gagliardi C, Pantaleo D, et al. Bioprosthetic replacement after bioprosthesis failure: a hazardous choice? Ann Thorac Surg 1998; 66(6 Suppl): S68–72. [DOI] [PubMed] [Google Scholar]
- 23).Redondo Palacios A, Lopez Menendez J, Miguelena Hycka J, et al. Which type of valve should we use in tricuspid position? Long-term comparison between mechanical and biological valves. J Cardiovasc Surg (Torino) 2017; 58: 739–46. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


