Abstract
Background:
Disparities in the global availability of operating theatres, essential surgical equipment and surgically trained providers are profound. Although efforts are ongoing to increase surgical care and training, little is known about the surgical capacity in developing countries. The aim of this study was to create a baseline for surgical development planning at a national level.
Methods:
A locally adapted World Health Organization survey was conducted in November 2010 to assess emergency and essential surgical capacity and volumes, with on-site interviews at 44 district and referral hospitals in Rwanda. Results were compiled for education and capacity development discussions with the Rwandan Ministry of Health and the Rwanda Surgical Society.
Results:
Among 10·1 million people, there were 44 hospitals and 124 operating rooms (1·2 operatingrooms per 100 000 persons). There was a total of 50 surgeons practising full- or part-time in Rwanda (0·49 total surgeons per 100 000 persons). The majority of consultant surgeons worked in the capital (covering 10 per cent of the population). Anaesthesia was performed primarily by anaesthesia technicians, and six of 44 hospitals had no trained anaesthesia provider. Continuous availability of electricity, running water and generators was lacking in eight hospitals, and 19 reported an absence or shortage in the availability of pulse oximetry. Equipment for life-saving surgical airway procedures, particularly in children, was lacking. A dedicated emergency area was available in only 19 hospitals. In 2009 and 2010 over 80 000 surgical procedures (major and minor) were recorded annually in Rwanda.
Conclusion:
A comprehensive countrywide assessment of surgical capacity in resource-limited settings found severe shortages in available resources. Immediate local feedback is a useful tool for creating a baseline of surgical capacity to inform country-specific surgical development.
Introduction
Access to surgical care and the burden of surgical disease have historically been neglected by the global health community. Surgical disease contributes to at least 11 per cent of the global burden of disease and more than 25 million disability-adjusted life-years1,2. Disparities in the availability of operating theatres and essential surgical equipment are profound, with more than two billion people in low-income countries estimated to lack access to basic, lifesaving surgical care3.
In 2005, the World Health Organization (WHO) Global Initiative for Emergency and Essential Surgical Care (GIEESC) was established, encouraging collaborations aimed at reducing mortality and morbidity from surgically treatable conditions4,5. The GIEESC has published a situational analysis tool to characterize surgical capacity in low- and middle-income countries. The purpose of this survey is to evaluate facility, materials and personnel capacity rather than surgical outcomes and the impact of treating surgical disease6. This survey has been used previously to characterize surgical capacity in over 25 countries and is the most widely used survey assessment of surgical capacity in resource-limited settings7–10.
Rwanda is a land-locked, densely populated country in East Africa, with over 67 per cent of the population aged less than 20 years11,12. The economic and political capital is Kigali, with a population of nearly one million, approximately 10 per cent of the nation’s population of 10·1 million12. The economy of the country is primarily agrarian, with coffee and tea as the major exports; 2009 gross national income per capita was US $460, classifying Rwanda as a low-income country13. The Rwandan health system was devastated following the genocide of 1994. Despite tremendous progress in the health sector since then, including a national community-based health insurance plan with greater than 94 per cent enrolment and a better percentage of human immunodeficiency virus-positive patients on antiretroviral therapy than in the USA, there is still a severe shortage of physicians, with approximately 5·5 doctors per 100 000 population14. The need to increase access to surgical care is increasingly being recognized by the governance as a health priority, but neither the unmet need nor the extent of existing capacity has been evaluated systematically.
The aim of this study was to assess the resources available and current surgical capacity of Rwandan hospitals, to identify gaps in the availability of emergency and essential surgical care as defined by international standards, and to provide a baseline for quality improvement of surgical services by the Rwandan Ministry of Health (MOH). Capacity and perceived gaps in personnel and training, infrastructure, supplies, surgical volumes and referral systems were evaluated in order to develop a national plan to improve the quality and availability of surgical services in Rwanda. This survey is presented to the international community as an indication of the importance of both defining the problem comprehensively at a local level, and collaborating with local researchers and health officials to utilize the information for creating change.
Methods
Ethical approval for this study was obtained from the University Teaching Hospital – Kigali, in Rwanda. Formal institutional review board approval was not required at the University of Virginia.
Survey
In consultation with surgeons at the National University of Rwanda and MOH, the WHO Tool for Situational Analysis to Assess Emergency and Essential Surgical Care was adapted for use in Rwanda. The WHO survey instrument itself is available in the public domain; it consists of four sections that collect a combination of quantitative and qualitative data related to infrastructure, human resources, interventions, and emergency equipment and supplies6. For adaptation in Rwanda, exact numbers of types of equipment were obtained where possible, with additional questions related to the availability of pulse oximetry, chest tube, self-contained/water-seal suction apparatus, and materials for emergency surgical airway. A fifth section evaluating compliance with personal protective equipment was new to the survey.
Procedures and volume
Data on types and volume of procedures performed in district hospitals were extracted from the central MOH statistical system; volume data from referral hospitals were reported separately from operative registers or annual reports. District data were analysed regionally to provide some indication of the strength and weaknesses of referral systems, a key concern of the MOH. Population values for district hospitals were self-reported by each hospital based on the population at health centres designated by the MOH to refer to that hospital. For the referral hospitals, national population statistics and projections from the MOH were used to estimate the populations served by the relevant centres based on which district hospitals are designated for that referral centre. For all national calculations, the most recent population statistics from the National Institute of Statistics of Rwanda (NISR) of 10 117 029 persons was used12.
Site visits
In November 2010, one investigator performed on-site surveys of 44 hospitals, including 41 district hospitals, two university referral hospitals and one tertiary referral hospital. Staff at the individual hospitals provided data through interviews to complete the surveys. In nearly all hospitals, a data manager and at least two other informed individuals were questioned. Usually the other individuals interviewed had one of the following local roles: hospital director or administrator, theatre nurse, anaesthetist and/or physician. Only operating rooms and pieces of equipment that were functional at the time of interview were tabulated. Total on-ground costs for conducting the survey, including transportation, lodging, meals and administrative costs, were less than US $5000.
Presentation of data
A written report of the survey results was submitted to the MOH and the Rwanda Surgical Society in March 2011. The results were presented to the Strengthening Rwanda Surgery Workshop in Kigali, Rwanda, in March 2011; MOH and National University of Rwanda leadership, Rwandan surgeons, anaesthetists and trainees, and surgical partners from five countries participated in the ensuing dialogue, which focused on the development of a national plan for improving surgical care and training in Rwanda.
Descriptive data are reported; no formal statistical analyses were attempted.
Results
Rwanda is divided into five provinces: North, South, East, West and Kigali City. All 44 government-supported district and referral hospitals were surveyed. Referral hospitals include two university teaching hospitals, one in Butare in the Southern Province (Centre Hospitalier Universitaire Butare, CHUB) and one in the capital of Kigali (Centre Hospitalier Universitaire Kigali, CHUK), and a tertiary hospital in Kigali (King Faisal Hospital, KFH). The map in Fig. 1 show the provinces and hospital locations in Rwanda.
Fig. 1.

Map showing Rwandan hospitals
Operating rooms
In all, there were 124 major and minor operating rooms functional in November 2010, equating to 1·2 per 100 000 persons; 81·5 per cent of the operating rooms were located in district hospitals. Table 1 shows a profile of district hospital, stratified by province, and referral hospital demographics. Furthest health centre is listed as a marker of distance as patients must present first to a health centre to be referred to a district hospital for surgical care.
Table 1.
Rwandan government hospital profile
| n | Mean distance to furthest health centre (km) | Population served | Hospital beds | Operating rooms | Operating rooms per 100 000 | |
|---|---|---|---|---|---|---|
| District hospitals | 41 | 44 | 9710 108* | 6534 | 101 | 1·04 |
| Kigali City | 4 | 27 | 882 011 | 640 | 15 | 1·70 |
| Northern Province | 6 | 54 | 1 852 517 | 1129 | 16 | 0·86 |
| Southern Province | 10 | 39 | 2 355 891 | 1576 | 25 | 1·06 |
| Eastern Province | 9 | 48 | 2 168 518 | 1250 | 17 | 0·78 |
| Western Province | 12 | 50 | 2 451 171 | 1939 | 28 | 1·14 |
| Referral hospitals | 10 117 029† | 1063 | 23 | 0·22 | ||
| CHUK (Kigali City) | 6238 736‡ | 513 | 14 | 0·22 | ||
| KFH (Kigali City) | 10 117 029† | 130 | 5 | 0·04 | ||
| CHUB (Southern Province) | 3 471 372‡ | 420 | 4 | 0·11 | ||
| National total | 10 117 029† | 7597 | 124 | 1·22 |
District hospital population estimates were derived from catchment populations self-reported by the district hospitals, based on the most recent population statistics at their Ministry of Health (MOH)-appointed referring health centres.
Population projection for 2009 from the National Institute of Statistics of Rwanda was used for whole-country estimates12.
Estimates were made by summing the catchment area populations of the district hospitals that referred to each university hospital, as delineated by the MOH. However, there was a degree of cross-referencing, depending on which hospital offered a particular service, for example neurosurgery at Centre Hospitalier Universitaire Kigali (CHUK) or dialysis at Centre Hospitalier Universitaire Butare (CHUB). KFH, King Faisal Hospital.
Hospital equipment
Hospitals were generally well equipped with basic infrastructure for surgical care as defined by the WHO; however, availability of basics such as oxygen, running water and electricity was not universal. Although every hospital had at least one operating room, fewer than half had areas dedicated to postoperative care or emergency care. Table 2 details the availability of basic infrastructure supplies and resources stratified by province.
Table 2.
Availability of infrastructure supplies (available all the time)
| Kigali City (n = 6) |
Northern Province (n = 6) |
Southern Province (n = 11) |
Eastern Province (n = 9) |
Western Province (n = 12) |
Total (n = 44) |
|
|---|---|---|---|---|---|---|
| Operating room | 6 | 6 | 11 | 9 | 12 | 44 |
| Oxygen cylinder | 6 | 3 | 9 | 4 | 4 | 26 |
| Oxygen concentrator | 5 | 5 | 8 | 4 | 11 | 33 |
| Running water | 6 | 6 | 7 | 6 | 11 | 36 |
| Electricity | 6 | 5 | 6 | 8 | 11 | 36 |
| Generator | 6 | 6 | 8 | 8 | 8 | 36 |
| Basic laboratory | 6 | 6 | 11 | 8 | 12 | 43 |
| Anaesthesia machine | 6 | 5 | 5 | 5 | 6 | 27 |
| X-ray machine | 6 | 6 | 8 | 6 | 7 | 33 |
| Ultrasound machine | 6 | 5 | 8 | 7 | 12 | 38 |
| Blood bank* | 3 | 4 | 8 | 3 | 9 | 27 |
| Dedicated postop. area | 5 | 1 | 10 | 1 | 4 | 21 |
| Dedicated emergency area | 4 | 3 | 3 | 4 | 5 | 19 |
Every hospital has a blood refrigerator for basic red cell availability. Further blood availability is at National Blood Transfusion Centres, which are available in every province. This represents a self-reported assessment of emergency blood supply at hospital level.
Trained personnel
Table S1 (supporting information) details trained personnel (including Rwandan and expatriate personnel) in Rwanda as of November 2010 in the following specialties: surgery, obstetrics and gynaecology, anaesthesiology, radiology and pathology. Surgery includes general surgery, orthopaedics, neurosurgery, otolaryngology, paediatric surgery, ophthalmology, urology, maxillofacial and cardiothoracic specialties.
Fourteen of 20 full-time consultants in obstetrics and gynaecology were working in Kigali. Anaesthesia care was primarily provided by anaesthesia technicians; there were only 13 trained anaesthetists. Six of 44 hospitals had no trained anaesthesia provider (qualified anaesthetist or certified anaesthesia technician). Only one hospital reported that general doctors provided anaesthesia care. The seven full-time radiologists were practising almost exclusively at referral hospitals in the capital. Radiology technicians were available but four of 44 hospitals reported that they had no such personnel to perform imaging studies. Trained mechanics/engineers to service biomedical equipment and expertise in pathology (anatomical, histological and laboratory) were identified in interviews as major unmet needs in Rwanda.
There were fewer than 50 full-time trained surgeons in all specialties. The majority of full-time consultant surgeons were working in Kigali. Only seven full-time surgical specialists were working in district hospitals (three ophthalmologists); the majority of trained specialists outside of Kigali were expatriate surgeons. With only 50 surgeons in the country, on a per-capita basis, there were 0·49 surgeons per 100 000 persons, 0·15 general surgeons per 100 000 and 0·09 orthopaedic surgeons per 100 000. These numbers include expatriate surgeons; there were no Rwandan paediatric, cardiothoracic, plastic or oncological surgeons. A breakdown of surgical specialists in Rwanda is shown in Table S2 (supporting information).
Surgical procedures and emergency interventions
Hospital personnel were asked to identify which of 32 surgical interventions and four anaesthesia interventions, as determined by the WHO GIEESC as emergency and essential surgical procedures that should be performed at district hospital level, were performed at their hospital. Respondents were asked to identify whether they sometimes referred to a higher-level hospital for the procedure and, if so, was this due to inadequate training of providers or insufficient materials. Many of the surgical procedures for which the district hospitals reported the least capability to perform (fewer than two-thirds of hospitals reporting capacity) were emergency/injury-related procedures including cricothyrotomy/tracheostomy, open fracture care and regional anaesthetic blocks. Reasons for transfer were often multifactorial, being influenced both by training and availability of materials (Table S3, supporting information).
Table S4 (supporting information) provides an overview of available materials. The most notable gap in materials was lack of availability of tools and materials designed for paediatric use. Fig. 2 shows the 15 items that were the least available overall; two-thirds of these were related to airway or breathing. Many hospitals stated that they did not have need for items such as scalp vein infusion sets, self-contained water-seal systems and batteries for flashlights, or used alternative materials.
Fig. 2.
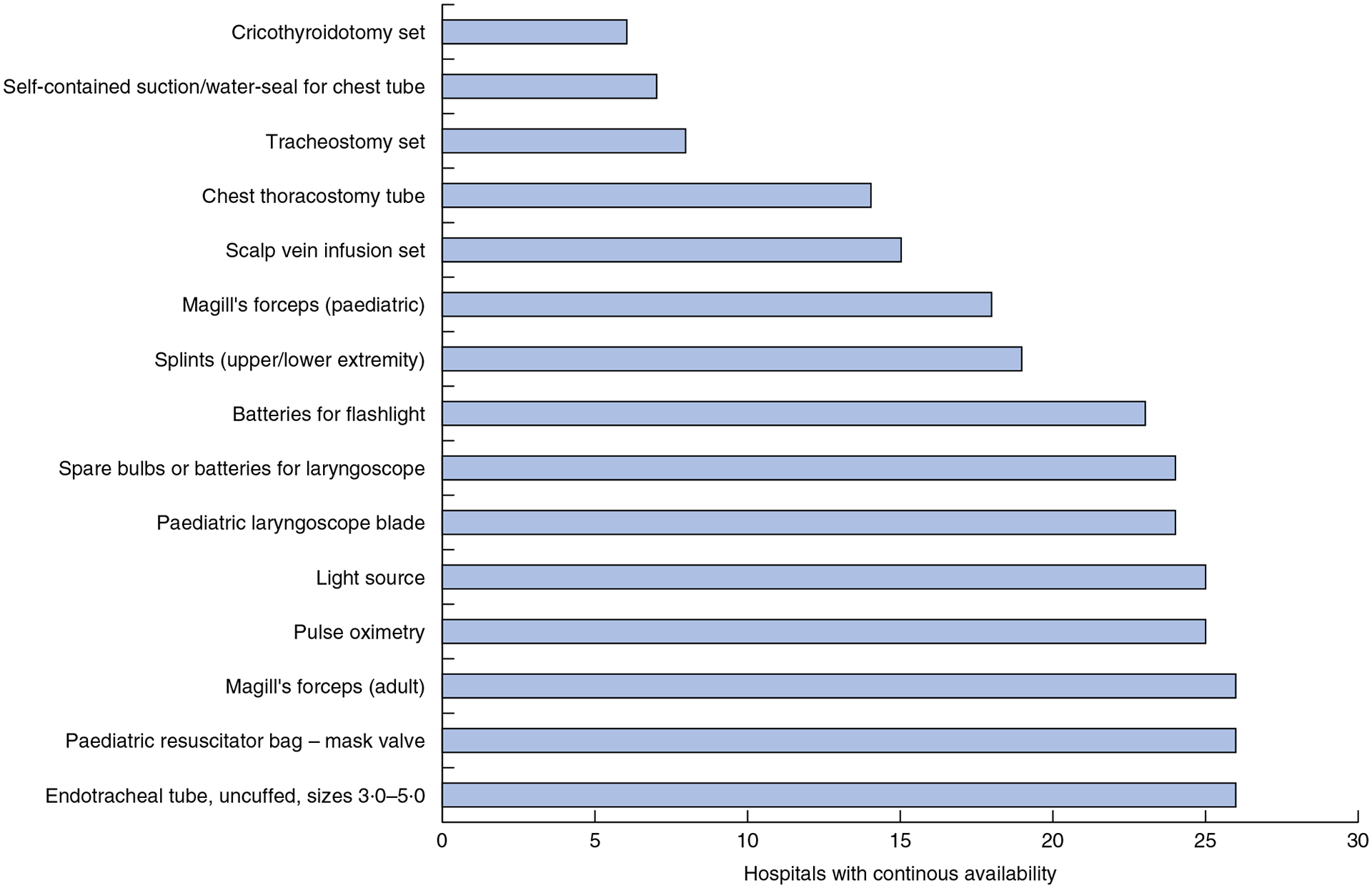
Least available materials in 44 hospitals in Rwanda
Nineteen of 44 hospitals reported an absence or shortage in the availability of pulse oximetry (Fig. 3). Of these, nine had oxygen shortages, whereas ten said that oxygen was reliably available. Thirteen of 44 centres reported a complete inability to perform and record pulse oximetry, six of which had absent or insufficient oxygen. Overall, a quarter of hospitals (12 of 44) reported absent or insufficient oxygen. Fig. 3 shows the pulse oximetry and oxygen deficiencies by province/region.
Fig. 3.
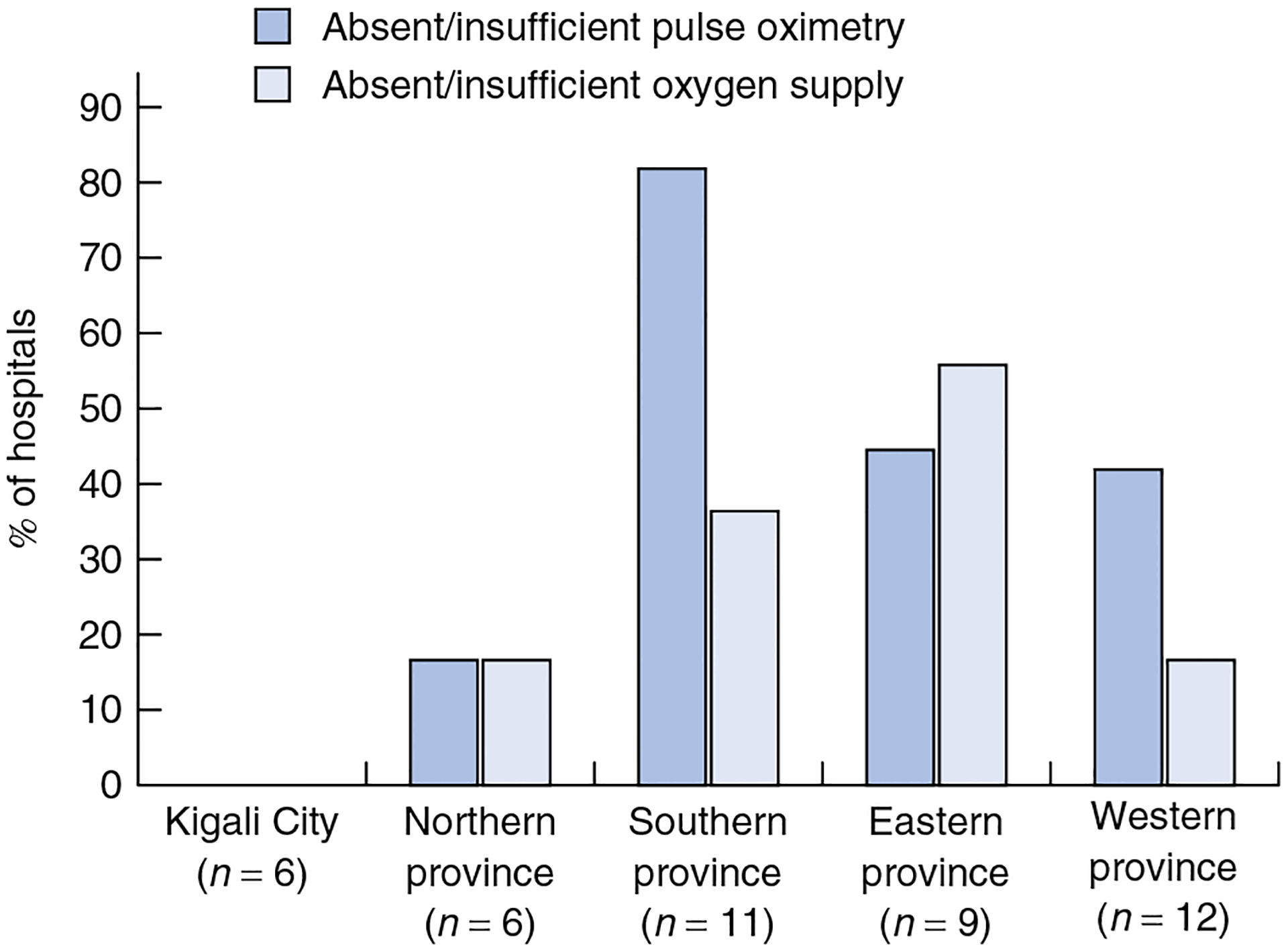
Shortages of pulse oximetry and oxygen by province
Surgical volume
In 2009 and 2010, over 80 000 surgical procedures (major and minor) were recorded annually in Rwanda. Evaluation of surgical registers and annual hospital reports at the referral hospitals (CHUB Annual Report 2009, KFH and CHUK Annual Report 2010) showed that 82·5 per cent of major surgical procedures were performed in district hospitals. The majority of these procedures were caesarean sections, with over 60 per cent of major procedures being listed under the ‘obstetrics’ category. Table S5 (supporting information) and Table 3 detail surgical volumes at district and referral levels.
Table 3.
Surgical volumes at district and referral hospital level
| Population Served | Major operations per year | Major and minor operations per year | Major operations per 100 000 population | Major and minor operations per 100 000 population | |
|---|---|---|---|---|---|
| District hospitals | 10 117 029* | 43 389 | 71 432 | 428·9 | 706·1 |
| Kigali City (n = 4) | 882 011 | 7015 | 10 985 | 795·3 | 1245·4 |
| Northern Province (n = 6) | 1 852 517 | 6328 | 10 267 | 341·6 | 554·2 |
| Southern Province (n = 10) | 2 355 891 | 11 189 | 14 461 | 474·9 | 613·8 |
| Eastern Province (n = 9) | 2 168 518 | 7949 | 11 913 | 366·5 | 549·4 |
| Western Province (n = 12) | 2 451 171 | 10 908 | 23 806 | 445·0 | 971·2 |
| Referral hospitals | 10 117 029* | 8310 | 14 609 | 82·1 | 144·4 |
| CHUK | 6 238 736 | 4164 | 7682 | 66·7 | 123·1 |
| KFH | 10 117 029 | 1658 | 2401 | 16·4 | 23·7 |
| CHUB | 3 471 372 | 2488 | 4526 | 71·7 | 130·4 |
District hospital data are from the Ministry of Health central statistical system, 2009. Procedures recorded for the referral hospitals are from annual hospital reports – 2009 for Centre Hospitalier Universitaire Butare (CHUB), and 2010 for Centre Hospitalier Universitaire Kigali (CHUK) and King Faisal Hospital (KFH).
The most recent population projection from the National Institute of Statistics of Rwanda (2009) was used for population calculations involving the whole country12.
Discussion
Comprehensive country-level data on surgical capacity are lacking in the global literature. Previous surveys using the WHO tool have almost exclusively used a sampling methodology to gain inferential knowledge of whole-country healthcare capacity7–10. Other available literature on global surgical capacity used statistical modelling techniques to estimate disparities and operative volumes3,15. Most of these analyses had the aim of informing the international surgical community regarding disparities in district-level surgical capacity worldwide. To date, only one full-country assessment of district-level surgical capacity is available16 and there are no comprehensive surveys of all surgical facilities in a single country.
This study revealed significant deficiencies in infrastructure, personnel and training in Rwanda. In November 2010, all 44 hospitals surveyed had at least one functional operating theatre and performed some breadth of surgery. Although a universal standard does not exist, a previously published multicountry study of operating room availability found an average of six operating theatres per 100 000 persons worldwide, with high-income countries having 14–25 theatres per 100 000 persons. Consistent with the present results in Rwanda (1·2 per 100 000 persons), sub-Saharan Africa had the least global availability of operating theatres (1·0–1·2 per 100 000 persons)3. The survey results indicate that the majority of Rwandan hospitals have basic infrastructure for surgical services, but access is not universal. To compare within Africa, a survey of a representative sample of government hospitals in Sierra Leone showed major deficiencies in the availability of electricity and running water, with only 40 per cent of government hospitals having oxygen capacity7. A study from Ghana reported better infrastructure availability, but still only 77 per cent of hospitals with oxygen capacity6. Access to pulse oximetry has been used by the WHO Safe Surgery Saves Lives programme as a marker of adequate operating theatre resources and an important safety resource. In high-income nations, use is practically universal, but within sub-Saharan Africa 50–70 per cent of hospitals do not have adequate pulse oximetry3,17. Material deficiencies in Rwanda were found to be most pronounced in emergency airway supplies – particularly those for paediatric use – and materials for lifesaving procedures such as cricothyroidotomy and chest tube placement.
Like much of Africa, Rwanda has a scarcity of surgical personnel, more than tenfold fewer than averages in the USA and Europe. The Health Policy Research Institute of the American College of Surgeons recommends a minimum of six general surgeons per 100 000 persons18. This is a drastic difference from the 0·15 general surgeons per 100 000 found in the present study.A study in neigh-bouring Uganda similarly reported 0·27 general surgeons per 100 000 population (75 for 27 million people)19. In Rwanda the majority of surgical care at the district hospital level is provided by general practitioners, most of whom are young doctors, fresh from medical school, who lack the experience, confidence and skills to perform operative procedures with proficiency. Anaesthesia also poses a challenge; six of 44 hospitals in this survey were providing surgical care without a trained anaesthesia technician. Yet, major operations were being performed.
Previous authors have estimated that a mean(s.d.) of 295(53) procedures are performed per 100 000 persons in low-income countries compared with 11 110(1300) procedures for high-income countries15. At the district hospital level in Rwanda, a mean of 428·9 major procedures per 100 000 persons and 706·1 total surgical interventions per 100 000 persons were performed in 2009. Although it is reassuring that Rwanda is ahead of many of its peers in terms of surgical volumes, it is alarming that outcomes and safety data are not readily accessible.
Although not an immediate aim of the WHO tool, one benefit of performing a comprehensive survey of all government district and referral hospitals is the ability to gain some insight into surgical referral patterns and challenges. In Rwanda, over 80 per cent of surgical procedures in 2009 occurred at the district hospital level, the majority being caesarean sections. At the time of the survey, over 80 per cent of operating theatres were located in district hospitals, but 80 per cent of trained surgeons were working in the capital. The survey revealed several deficiencies in patterns of referral for surgical care at the district hospital. Many cases become unnecessarily more complex owing to delayed presentation and poor communication during the transfer process. Several of the deficiencies in the availability of surgical care in the district hospitals (such as care of open fractures) serve to create overcrowding and backlogs at the referral hospitals.
Many published capacity surveys have used convenience sampling of district-level health facilities to characterize deficiencies for the global community, highlighting the extreme disparities in access to surgical care and raising international awareness20. Data collection costs and logistical limitations in many locations make convenience sampling the most cost- and time-effective method of evaluation. However, the ability to survey every hospital within a healthcare system provides a more specific and complete picture of capacity and deficiencies, which augments the utility and validity of the data collected. Furthermore, a whole-country survey allows evaluation of the referral systems and regional differences that tend to interest healthcare planners.
This descriptive study has several limitations. It provides only a static impression of surgical infrastructure and personnel. Many of the hospitals have acquired new operating theatres or equipment since the survey was carried out and, as such, continuous monitoring and evaluation are necessary. Personnel are also fluid, and comparison with other Rwandan surveys reveals inconsistencies in reported surgical personnel20. The study probably under-represented the surgical procedures and complications in Rwanda as it did not evaluate the volumes or outcomes of surgery performed by short-term missions, private practice clinics or health centres. Thus, the true burden of surgical disease can be assessed only at the community level. Given the scarcity of surgical services in Rwanda, this hospital-based survey of volumes and capacity probably measures just the tip of the iceberg with regard to the true burden of surgical disease.
Prospective analyses based on trauma and cancer registries are needed to evaluate epidemiology and outcomes at a hospital level, and community-based studies are needed to evaluate the prevalence of surgical disease and disability in local villages and neighbourhoods. The survey used in the present study was developed by the WHO as a global tool to assess capacity based on WHO guidelines for the generic district hospital. Although some quantitative data can be obtained, it is primarily a qualitative assessment with wide interpretation. In order to assess surgical capacity and development better, a more quantitative survey with clearly defined areas of measurement needs to be developed. Not only would this enable better consistency in an initial assessment, it would also allow quantitative assessment of quality improvement measures.
Supplementary Material
Table S1 Surgical and surgery-related care providers, November 2010 (Word document)
Table S2 Trained surgical specialists in Rwanda (Word document)
Table S3 Hospital interventions (Word document)
Table S4 Availability of hospital equipment and materials (Word document)
Table S5 Summary of procedures carried out at district hospitals (Word document)
Acknowledgements
The authors thank the MOH and the Faculty of Medicine at the National University of Rwanda for logistical support throughout the study, and the WHO for development of the survey tool and initial discussions regarding implementation. This work was funded through a Fogarty International Clinical Research Fellowship, National Institutes for Health and International Clinical Research Fellows Program at Vanderbilt University, Nashville, Tennessee, USA (R24 TW007988).
Footnotes
Disclosure: The authors declare no conflict of interest.
Supporting information
Additional supporting information may be found in the online version of this article:
Please note: John Wiley & Sons Ltd is not responsible for the functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.Debas H, Gosselin R, McCord C, Thind A, Jamison DT, Breman JG et al. Surgery. In Disease Control Priorities in Developing Countries (2nd edn), Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB et al. (eds). World Bank: Washington, DC, 2006; 1245–1260. [Google Scholar]
- 2.Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg 2008; 32: 533–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Funk LM, Weiser TG, Berry WR, Lipsitz SR, Merry AF, Enright AC et al. Global operating theatre distribution and pulse oximetry supply: an estimation from reported data. Lancet 2010; 376: 1055–1061. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO). Global Initiative for Emergency and Essential Surgical Care. http://www.who.int/surgery/globalinitiative/en/[accessed 24 November 2009]. [DOI] [PMC free article] [PubMed]
- 5.Bickler SW, Spiegel D. Improving surgical care in low- and middle-income countries: a pivotal role for the World Health Organization. World J Surg 2010; 34: 386–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO). Tool for Situational Analysis to Assess Emergency and Essential Surgical Care. http://www.who.int/surgery/publications/QuickSitAnalysisEESCsurvey.pdf [accessed 24 November 2009]. [DOI] [PMC free article] [PubMed]
- 7.Kingham TP, Kamara TB, Cherian MN, Gosselin RA, Simkins M, Meissner C et al. Quantifying surgical capacity in Sierra Leone: a guide for improving surgical care. Arch Surg 2009; 144: 122–127. [DOI] [PubMed] [Google Scholar]
- 8.Choo S, Perry H, Hesse AA, Abantanga F, Sory E, Osen H et al. Assessment of capacity for surgery, obstetrics and anaesthesia in 17 Ghanaian hospitals using a WHO assessment tool. Trop Med Int Health 2010; 15: 1109–1115. [DOI] [PubMed] [Google Scholar]
- 9.Spiegel DA, Choo S, Cherian M, Orgoi S, Kehrer B, Price RR et al. Quantifying surgical and anesthetic availability at primary health facilities in Mongolia. World J Surg 2011; 35: 272–279. [DOI] [PubMed] [Google Scholar]
- 10.Contini S, Taqdeer A, Cherian M, Shokohmand AS, Gosselin R, Graaff P et al. Emergency and essential surgical services in Afghanistan: still a missing challenge. World J Surg 2010; 34: 473–479. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health of Rwanda (MOH), National Institute of Statistics of Rwanda (NISR) and ICF Macro. Rwanda Interim Demographic and Health Survey 2007–08. MOH, NISR and ICF Macro: Calverton, 2009. [Google Scholar]
- 12.National Institute of Statistics of Rwanda (NISR). National Population Projection, 2007–2022. NISR: Kigali, 2009. [Google Scholar]
- 13.The World Bank. Rwanda. http://data.worldbank.org/country/rwanda [accessed 10 April 2011].
- 14.Ministry of Health of Rwanda (MOH). Midterm HSSP-I Review. MOH: Kigali, 2008. [Google Scholar]
- 15.Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 2008; 372: 139–144. [DOI] [PubMed] [Google Scholar]
- 16.Sherman L, Clement PT, Cherian MN, Ndayimirije N, Noel L, Dahn B et al. Implementing Liberia’s poverty reduction strategy: an assessment of emergency and essential surgical care. Arch Surg 2011; 146: 35–39. [DOI] [PubMed] [Google Scholar]
- 17.Walker IA, Newton M, Bosenberg AT. Improving surgical safety globally: pulse oximetry and the WHO Guidelines for Safe Surgery. Paediatr Anaesth 2011; 21: 825–828. [DOI] [PubMed] [Google Scholar]
- 18.Gaul K, Poley ST, Ricketts TC III, Walker E, Groves J. Mapping the Supply of Surgeons in the United States, 2009. American College of Surgeons Health Policy Research Institute: Chapel Hill, 2010. [Google Scholar]
- 19.Ozgediz D, Kijjambu S, Galukande M, Dubowitz G, Mabweijano J, Mijumbi C et al. Africa’s neglected surgical workforce crisis. Lancet 2008; 371: 627–628. [DOI] [PubMed] [Google Scholar]
- 20.Notrica MR, Evans FM, Knowlton LM, Kelly McQueen KA. Rwandan surgical and anaesthesia infrastructure:a survey of district hospitals. World J Surg 2011; 35: 1770–1780. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Surgical and surgery-related care providers, November 2010 (Word document)
Table S2 Trained surgical specialists in Rwanda (Word document)
Table S3 Hospital interventions (Word document)
Table S4 Availability of hospital equipment and materials (Word document)
Table S5 Summary of procedures carried out at district hospitals (Word document)


