Abstract
Objective:
Ear, nose, throat, and respiratory infections (ENTRI) may affect children with complex chronic conditions (CCC) differently than their peers. We compared ENTRI prevalence and spending in children with and without CCCs.
Methods:
Retrospective analysis of 3,880,456 children ages 0-to-18 years enrolled in 9 US state Medicaid programs in 2018 contained in the IBM Watson Marketscan Database. Type and number of CCCs were distinguished with Feudtner’s system. ENTRI prevalence, defined as ≥1 healthcare encounters for ENTRI, and Medicaid spending on ENTRI were compared by CCC using chi-square tests and logistic regression.
Results:
ENTRIs were greater in children with vs. without a CCC (57.7% vs 43.5% [P < .001]). Children with a CCC (5.5%, n = 213,425) accounted for nearly one-fourth ($145.8 million [US]) of total spending on ENTRI. Aside from throat and sinus infection, ENTRI prevalence increased with number of CCCs (P< .001). For example, as number of CCCs increased from zero to ≥3, lower-airway infection increased from 12.5% to 37.5%, P < .001 (OR 4.10; 95% CI 3.95–4.26). ENTRI spending attributable to inpatient care increased from 9.7% to 92.8% (P< .001) as the number of CCCs increased from zero to ≥3.
Conclusion:
Most children with a CCC pursued care for ENTRI in 2018 and these children accounted for a disproportionate share of ENTRI spending. Children with multiple CCCs had a high prevalence of lower-airway infection; most of their ENTRI spending was for inpatient care. Providers can use these findings to counsel patients and families and to inform future investigations on how best to manage ENTRI in children with CCCs.
Keywords: acute illness, children, chronic conditions, respiratory infections
Ear, nose, throat, and respiratory infections (ENTRIs) are a common source of acute illness among children. ENTRIs encompass a variety of bacterial and viral infections, affecting the upper airway system (nose, sinuses, oropharynx, etc.), lower airway (lungs), and related organs. While most ENTRIs cause low severity of illness in children, they can result in frequent and recurrent healthcare visits that, collectively, account for a large amount of healthcare spending.1 ENTRIs can also cause substantial morbidity and mortality, particularly in populations at risk for experiencing them.2 In our clinical experience, children with lifelong, complex chronic conditions (CCCs) may represent one such population.3–7 The medical fragility and functional impairment associated with CCCs—especially those affecting multiple body systems—can exacerbate the physiologic impact of ENTRIs.
To our knowledge, the epidemiology and healthcare spending of ENTRI in children with and without CCCs have not been compared. The groundbreaking studies on the prevalence and expenditures of respiratory infection in children from prior decades occurred before children with CCCs emerged as a distinct population.8–12 Understanding similarities and differences of ENTRI in children with and without CCCs is important. Pediatric clinicians, especially those practicing in complex care, find it challenging to counsel families of children with CCCs on risk of ENTRI, beyond speculating that the children may have an increased risk. Population health and care coordination initiatives often target children with CCCs to decrease utilization and healthcare spending for emergency department and hospital care. It remains unknown how much ENTRI healthcare spending for children with CCCs is attributable to those health services, especially for lower respiratory infections that may pose a more serious threat to their health and function.
Therefore, we conducted a multi-US-state study of children with and without CCCs to1 measure and compare the prevalence and healthcare spending of children with ENTRI; and2 examine patient characteristics that associate with increased risk of lower respiratory infection. Achieving these aims will advance knowledge of ENTRI, especially among children with CCCs, to help improve clinical practice and inform future research that will optimize ENTRI diagnosis and treatment.
Patients and Methods
Study Design, Population, and Setting
This was a retrospective cohort study of the 2018 MarketScan Medicaid Database (IBM Watson Health, Armonk, New York) which included children in Medicaid fee-for-service and managed care plans from 9 states within all geographic regions of the United States. Medicaid is a joint US state and federal government program that provides healthcare coverage to people with disabilities and to people with low income. MarketScan includes data on paid Medicaid claims for all healthcare encounters across the care continuum, basis of eligibility for Medicaid, and enrollee demographic and clinical characteristics. The 2018 database was used because it is the most current data available to the study team. Multiple years of data were not used because of inconsistent participation of US states across years. Children ages 0-to-18 years were included if continuously enrolled for 11 or 12 months from January 1st to December 31st 2018. This study of de-identified data was exempt from review by the Boston Children’s Hospital Institutional Review Board; informed consent was not possible given the de-identified data.
Main Outcome Measures
Our primary outcome measure was prevalence of ENTRI, measured with one or more healthcare encounters for ENTRIs with a healthcare claim during 2018. We defined a healthcare encounter for ENTRI as an outpatient visit (ie, to primary care, specialty care, etc.), emergency department visit, or inpatient admission with a ENTRI primary International Classification of Diseases, 10th Revision (ICD-10) diagnosis code, distinguished from the Agency for Healthcare Research and Quality Clinical Classification System.13,14
ENTRI codes were grouped into six categories, informed by ICD-10-CM diagnosis codes used prior investigations and by categorization of previously unused codes identified from expert review by study team members1: throat, including pharyngitis, tonsillitis, and adenoiditis2; ear, including otitis media and externa3; sinuses, including sinusitis and sinus abscess4; upper airway, including croup, epiglottitis, and laryngitis, tracheitis, and laryngotracheitis5; lower airway, including pneumonia, bronchiolitis, influenza; and6 upper respiratory infection, not otherwise specified. These categories were collectively labeled, “ENTRI”, to simplify the reporting of results, recognizing that the categories represent a broad range of infections of the airways and related organs. Codes for symptoms (eg, cough, rhinorrhea, wheezing) were not used to distinguish RI.
Our secondary outcome was standardized Medicaid spending for ENTRI healthcare encounters. To account for differences in reimbursement across states as well as to generate claim-level spending for capitated patients, we used a per-unit level of spend to apply to all claims associated with a primary diagnosis code for ENTRI. Medicaid spending for ENTRI was categorized by health service, including outpatient, emergency department, inpatient, diagnostic testing, laboratory, pharmacy, etc.
Patients’ Clinical and Demographic Characteristics
We assessed chronic conditions for each child with ICD codes using the Complex Chronic Condition (CCC), Version 2, to identify the subset with CCCs known to be associated with high morbidity and resource use, which includes a “technology-dependent” category to identify children who rely on technology, such as ventilator or gastrostomy.15 Examples of CCCs types include a neonatal (eg, extreme prematurity and very low birth weight), gastrointestinal (eg, inflammatory bowel disease), neurologic (eg, cerebral palsy), and respiratory (eg, cystic fibrosis).
We also assessed demographic characteristics, including age in years, sex, race and ethnicity (precategorized in the dataset as mutually exclusive groups including Hispanic, Black, White, and other), and type of Medicaid plan (fee for service vs managed care) to assess the generalizability of the study population and in order to understand differences in outcomes among subgroups.
Statistical Analysis
We used descriptive statistics to describe demographics and clinical characteristics of the study population as well as assess relationships with ENTRI. Comparisons between categorical variables of interest across healthcare encounter for various ENTRIs were conducted using chisquare tests. The linear association between the number of CCCs (0, 1, 2, and 3 or more) and ENTRI was tested with a Mantel-Haenszel chi square test. A multivariable analysis was derived a priori with logistic regression to assess the adjusted likelihood of lower-airway infection accounting for demographic (age, gender, type of Medicaid plan) and clinical characteristics (number of CCCs). All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC), and P-values <.01 were considered statistically significant due to the large sample size.
Results
Characteristics of Study Population
There were 3,880,456 children ages 0-to-18 years in the cohort. The population was predominately White (47.9%), male (51.7%), and enrolled in a capitated Medicaid plan (64.1%). Children with CCCs represented 5.5% of the study population (n = 213,425; Table 1).
Table 1.
Demographic and Clinical Characteristics of Children With Versus Without an Ear, Nose, Throat, or Respiratory Infection
| Characteristic | Proportion of Children*,†,‡ | ||
|---|---|---|---|
|
| |||
| All N = 3,880,456 | Ear, Nose, Throat, or Respiratory Infection N = 1,720,054 |
No Ear, Nose, Throat, or Respiratory Infection N = 2,160,402 |
|
|
| |||
| Age in years | |||
| 0 | 1.0% | 1.5% | 0.6% |
| 1–2 | 11.9% | 18.5% | 6.6% |
| 3–5 | 18.1% | 22.2% | 14.9% |
| 6–12 | 42.1% | 39.3% | 44.3% |
| 13–17 | 26.9% | 18.5% | 33.6% |
| Race and Ethnicity | |||
| White | 47.9% | 54.6% | 42.6% |
| Black | 34.7% | 27.8% | 40.2% |
| Hispanic | 8.1% | 7.2% | 8.8% |
| Other | 4.2% | 4.4% | 4.1% |
| Missing | 5.1% | 6.0% | 4.3% |
| Sex | |||
| Male | 51.6% | 50.0% | 52.9% |
| Female | 48.4% | 50.0% | 47.1% |
| Capitation | |||
| No | 35.9% | 30.2% | 40.4% |
| Yes | 64.1% | 69.8% | 59.6% |
| Complex Chronic Condition | |||
| No | 94.5% | 92.8% | 95.8% |
| Yes | 5.5% | 7.2% | 4.2% |
Shown are column percentages for each characteristic.
P values were generated from Chi Square test.
All comparisons statistically significant at P < .001.
ENTRI Prevalence and Healthcare Spending
Overall, 44.3% (n = 1,720,054) of children in the study cohort had a healthcare encounter with a diagnosis of ENTRIs during the study year. ENTRIs of the throat (23.4%), upper respiratory infections not otherwise specified (18.3%), and ear (16.0%) were most common. Lower airway (12.9%), sinus (6.6%), and upper airway infections (that were specified; 2.1%) were less common.
Total Medicaid spending on ENTRI healthcare encounters was $628.9 million (US), which was 7.3% of total Medicaid spending on all healthcare encounters for the study population. The largest proportion of ENTRI spending was attributable to lower airway (36.2%), throat (23.6%), and ear (17.8%). The smallest proportion of ENTRI spending was attributable to sinus (4.0%) and upper airway (3.2%). Of ENTRI types, upper and lower airway infections were associated with the greatest proportion of ENTRI spending attributable to inpatient care (39.0% for upper airway; 56.7% for lower airway) compared with the other ENTRIs (all <5.0%), P < .001. Sinus and ear were associated with the greatest proportion of total Medicaid spending on ENTRI attributable to outpatient care (59.5% for sinus; 42.4% for ear).
ENTRI Prevalence and Spending for Children With and Without a Complex Chronic Condition
ENTRIs were higher in children with versus without a CCC (57.7% vs 43.5%; P < .001). Twenty-three percent ($145.8 million [US]) of total Medicaid spending on ENTRI encounters were attributable to children with a CCC. ENTRI varied by CCC category (Appendix Table). The proportion with healthcare encounters for ENTRI was highest among patients with respiratory (76.6%) and neonatal (73.1%) CCCs. A smaller percentage of children with malignancy (56.9%) and metabolic (52.7%) CCCs had an ENTRI encounter (Appendix Table).
Lower-airway infections were most prevalent in children with respiratory (43.4%), neonatal (38.3%), technology assistance (31.9%), and gastrointestinal (30.2%) CCCs. The percentage of children with ENTRI was smaller with a metabolic CCC (15.7%); however, this percentage was still greater than that in children with no CCC (12.5%; P < .001) (Table 2).
Table 2.
Adjusted Odds Ratios of Healthcare Encounter for Lower Airway Infection by Demographic and Clinical Characteristics
| Characteristic | Adjusted Odds Ratio of Lower Respiratory Infection (95% CI) |
|---|---|
|
| |
| Age in Years | |
| 0 | 3.57 (3.48, 3.66) |
| 1–2 | 4.28 (4.23, 4.32) |
| 3–5 | 2.53 (2.51, 2.56) |
| 6–12 | 1.66 (1.65, 1.68) |
| 13–17 | Ref |
| Sex | |
| Male | 1.03 (1.03, 1.04) |
| Female | Ref |
| Type of Medicaid Coverage | |
| Fee for Service | 0.83 (0.82, 0.83) |
| Capitation | Ref |
| Complex Chronic Condition | |
| 0 | Ref |
| 1 | 1.62 (1.60, 1.64) |
| 2 | 2.20 (2.14, 2.27) |
| 3+ | 4.10 (3.95, 4.26) |
ENTRI Prevalence and Healthcare Spending by Number of Complex Chronic Conditions
Aside from throat and sinus infection, ENTRI increased for each ENTRI subtype with increasing number of CCCs (Fig. 1). For example, upper-airway infection not otherwise specified increased from 17.9% to 31.4% as the number of CCCs increased from zero to ≥3 (P < .001). Similarly, lower-airway infection increased from 12.5% to 37.5% as the number of CCCs increased from zero to ≥3 (P <.001). This trend was not observed for throat or sinus infection. Throat infection was greatest in children with one CCC (30.1%); sinus infection was greatest in children with two CCCs (12.9%; Fig. 1).
Figure 1.
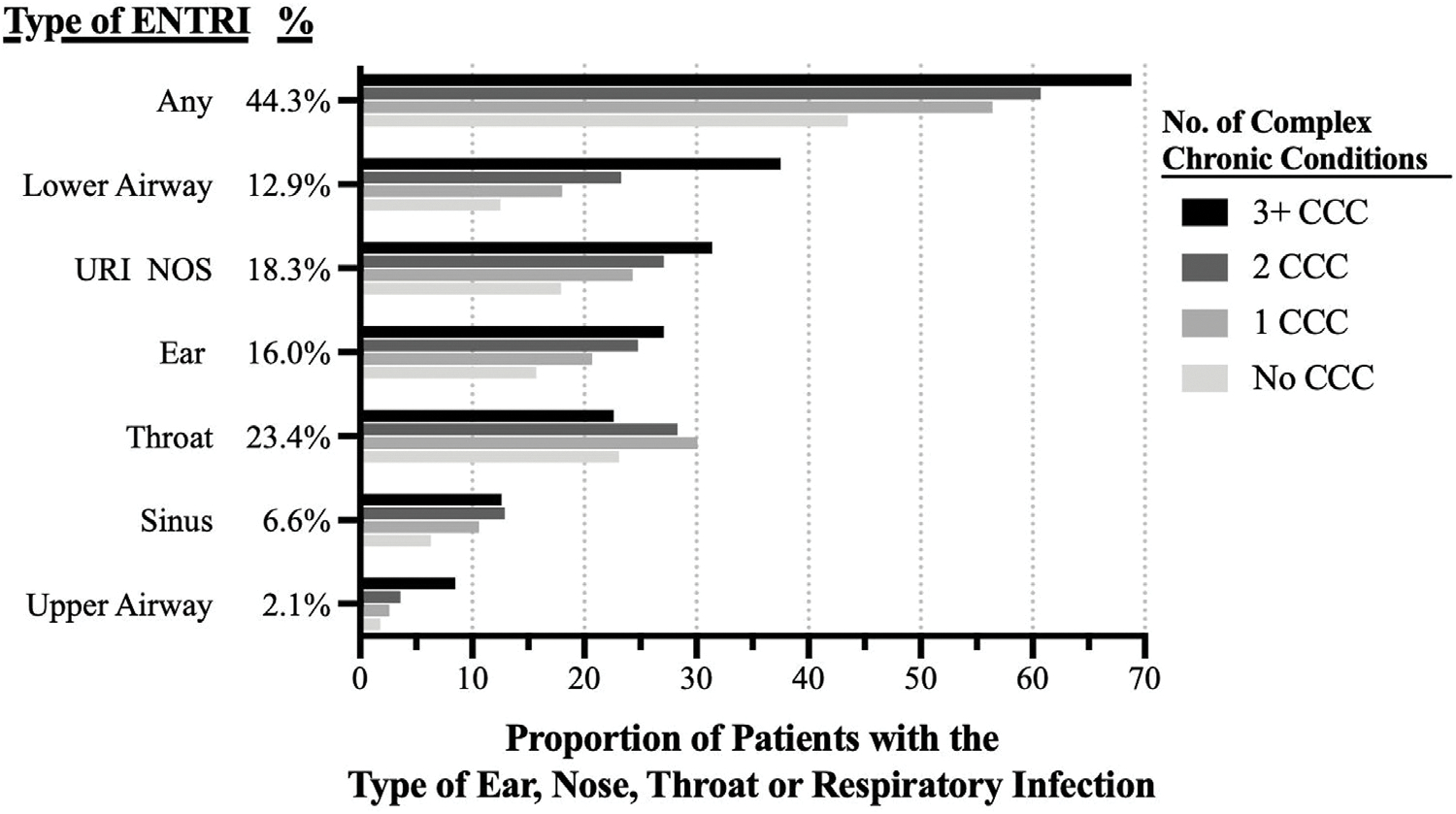
Proportion of children with a healthcare encounter for ear, nose, throat, or respiratory infection by number of complex chronic conditions. URI NOS = upper respiratory infection not otherwise specified. Upper airway included croup, epiglottitis, and laryngitis, tracheitis, and laryngotracheitis. All proportions within a respiratory infection type varied significantly (P < .001) by number of complex chronic conditions.
Medicaid spending for ENTRI by health service varied significantly by number of CCCs (Fig. 3). For example, the percentage of ENTRI spending attributable to inpatient care increased from 9.7% to 92.8% as the number of CCCs increased from zero to ≥3 (P < .001; Fig. 2). In contrast, the percentage of ENTRI spending attributable to outpatient primary and specialty care decreased from 37.5% to 2.4% as the number of CCCs increased from zero to ≥3 (P < .001). Similarly, the percentage of ENTRI spending attributable to emergency department care decreased from 31.1% to 2.2% as the number of CCCs increased from zero to ≥3 (P < .001; Fig. 3).
Figure 3.
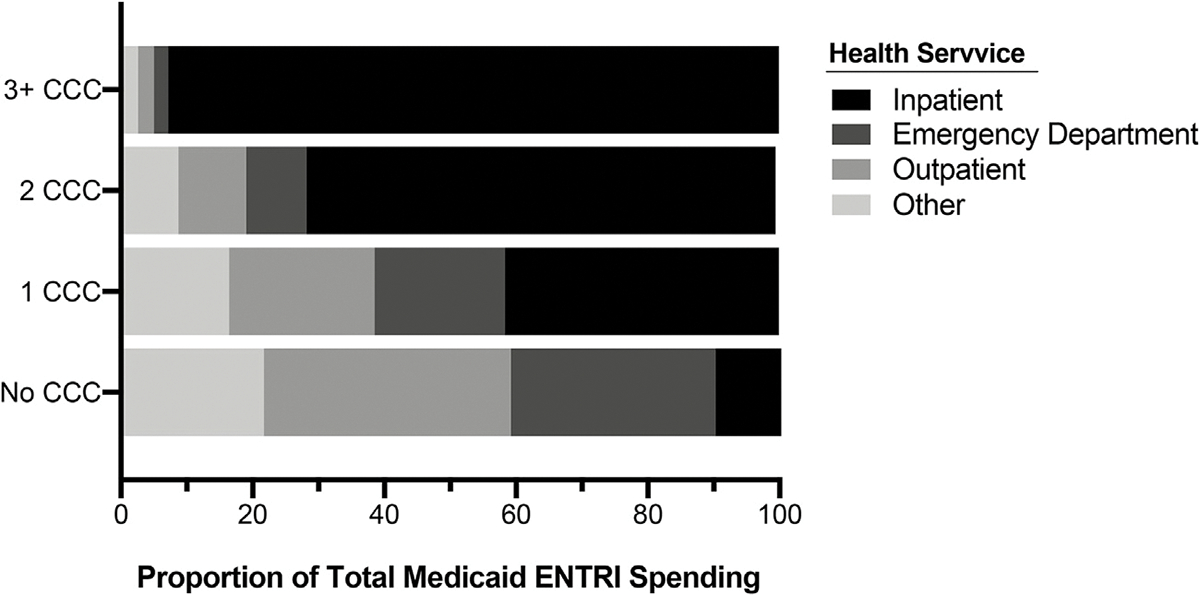
Distribution of Medicaid spending on ear, nose, throat, or respiratory infection by number of complex chronic conditions. Bars represent percentage of total Medicaid ENTRI Spending by the number of CCCs. For example, 93% of ENTRI spending for children with 3 + CCC was attributable to inpatient care (ie, the black bar grouped with inpatient). Other spending includes diagnostic testing, laboratory testing, and prescription medications.
Figure 2.
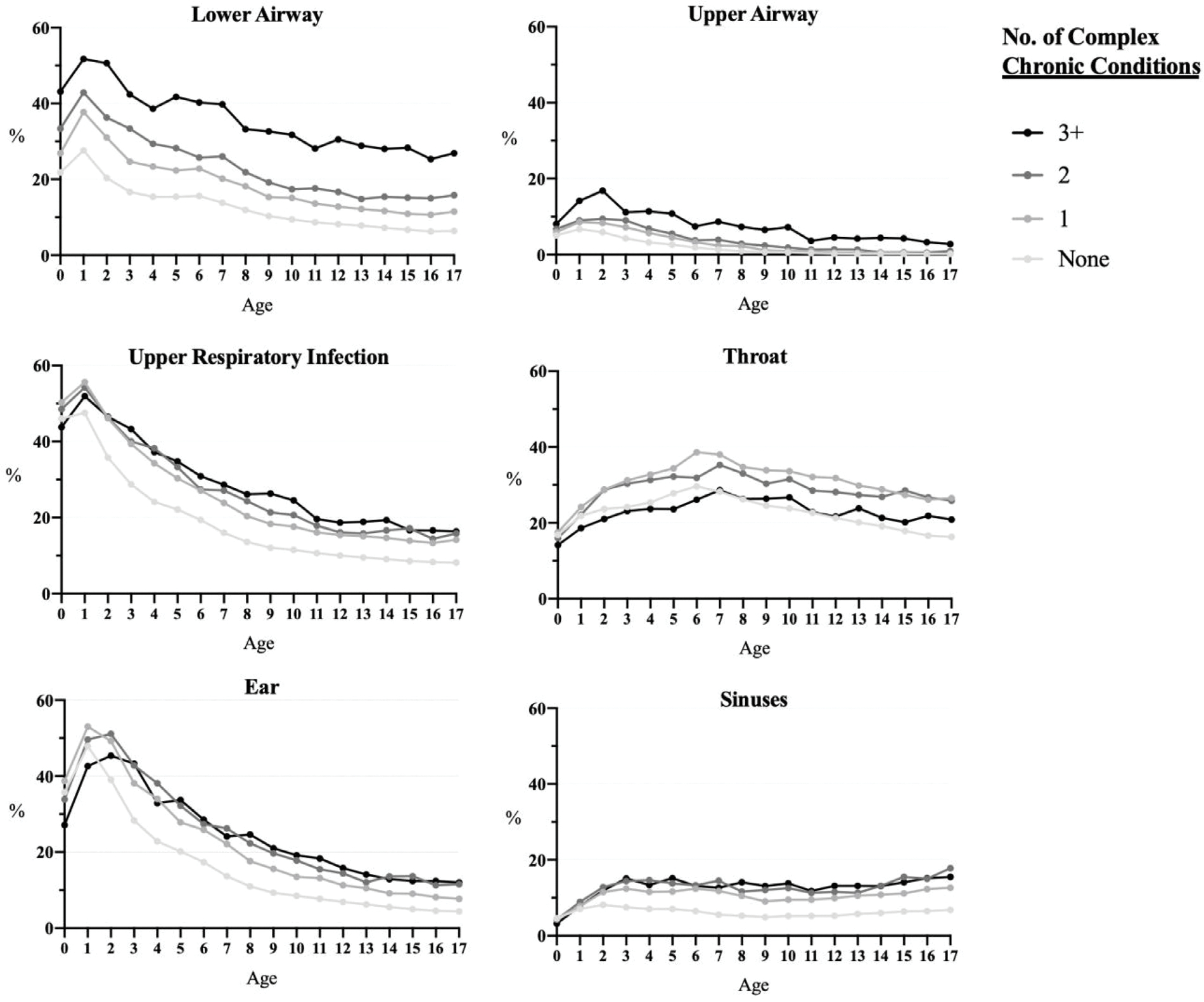
Age trends in proportion of children with healthcare encounter for ear, nose, throat, or respiratory infection by number of complex chronic conditions. Age in years is presented on the x-axis. Upper airway included croup, epiglottitis, and laryngitis, tracheitis, and laryngotracheitis. Upper respiratory infection included upper respiratory infections not otherwise specified.
ENTRI by Age and Number of Complex Chronic Conditions
For all ENTRIs combined, prevalence was higher with younger versus older age. The highest percentages were observed for age of one year, ranging from 73.2% for infants without a CCC to 81.3% for infants with ≥3 CCCs (P < .001). The lowest percentages of ENTRI encounters occurred at age 16 years, ranging from 27.4% to 54.3% for no CCCs versus ≥3 CCCs (P < .001; data not shown). Similar trends occurred with all ENTRI subtypes, aside from sinus and throat infection (Fig. 2). Sinus infection peaked at age 5-to-7 years of age. Throat infection peaked at age 3 years and remained stable in prevalence through age 17 years.
Multivariable Analysis of Patient Characteristics and Lower Airway Infection Healthcare Encounters
After controlling for patients’ other demographic and clinical characteristics, young age was associated with higher odds of lower-airway infection (Table 3). Odds ratios (ORs) for lower airway infection healthcare encounters was 3.57 (95% CI 3.48–3.66) for children age 0 years and 4.30 (95% CI 4.23–4.32) for children ages 1-to-2 years, compared with the reference group of ages 13-to-17 years. Having any CCC was also associated with nearly twice the odds of a healthcare encounter for lower airway infection (OR 1.82; 95% CI, 1.80–1.84); having three or more CCCs was associated with 4 times the odds of a healthcare encounter for lower airway infection (OR 4.10; 95% CI 3.95–4.26; Table 2).
Discussion
The main findings from the current study suggest that most children with a CCC who used Medicaid sought medical care for an ENTRI over the course of a year. Children with a CCC accounted for one-fourth of Medicaid spending on ENTRI. Aside from throat and sinus infections, the prevalence of ENTRI increased with number of CCCs. Nearly 2 in 5 children with 3+ CCCs experienced a lower respiratory infection during the study year. Medicaid spending on children with ENTRI varied substantially by presence of CCCs. For children with none or one CCC, the vast majority of spending was attributable to outpatient and emergency department care. For children with multiple CCCs, the vast majority of spending was attributable to inpatient care.
Although it is well established that ENTRIs are very common in children, the high prevalence of ENTRI—especially lower airway infection—in children with multiple CCCs warrants further attention. For example, severity of lower respiratory infection, including pneumonia, is considered sensitive to treatment in the ambulatory care setting. It is unclear how sensitive pneumonia—and other lower respiratory infections—is to ambulatory treatment in children with CCCs, who may have impaired airway clearance, hypoventilation, bacterial colonization, immunosuppression, and other risk factors that might influence pneumonia severity and treatment.16–23 With the majority of ENTRI spending going to inpatient care for children with multiple CCCs, further investigation is needed to assess how often these children engage with outpatient providers prior to hospitalization in an attempt to diagnosis and treat ENTRIs, thereby mitigating ENTRI severity.
The study findings highlight the importance of counseling patients and families of children with CCCs about the high prevalence of ENTRIs. In our outpatient clinical experience with pediatric complex care, discussion of ENTRIs in the context of anticipatory guidance is often overlooked or overshadowed by the myriad other healthcare issues and needs that the children experience, including those related to co-existing chronic conditions, chronic medications, durable medical equipment, etc. More common than asthma in children with CCCs, ENTRIs may deserve special attention with anticipatory guidance, including development of specific action plans. Evaluation of ENTRI plans—including early signs/symptoms to recognize, where to go for rapid response and help, manipulations of existing respiratory treatments (eg, suctioning, oxygen, nebulized medications)—will advance knowledge on their benefit for children with CCCs.
The study findings also bring attention to throat infections in children with CCCs. The prevalence of throat infections did not increase with number of CCCs in the same fashion as other ENTRIs. Further investigation to the oropharyngeal exam in children with CCCs—especially multiple ones—is needed. This exam can be challenging to conduct in children with CCCs who have limitations in comprehensive and expressive speech abilities to describe symptoms, facial spasticity, large tongues, and sialorrhea. Therefore, it is possible that some children with CCCs may be at risk for a limited oropharyngeal exam. As a result, the children may be at risk for under-diagnosis and work-up of throat infections. Examination of diagnostic study use related to throat infections (eg, throat culture) in children with and without CCCs could help assess this situation.
The study findings must be considered in the context of several limitations. The IBM Watson Marketscan Medicaid Database is limited to children covered by Medicaid. Therefore, the study findings may generalize best to children using Medicaid. We were unable to capture ENTRI that did not generate a billing encounter. For example, ENTRIs managed in the home without seeking medical attention, or ENTRIs triaged by phone are not captured in the database used. Additionally, important data such as manner of presentation, patient/family concerns are not available. We did not measure ENTRIs using codes for symptoms (eg, cough) or for asthma. As such, we likely underestimate the absolute prevalence of ENTRI. The data did not permit distinction of the etiology of ENTRIs (eg, viral vs bacterial infection).
Although we report findings on Medicaid spending for ENTRI, the current study was not intended to specific healthcare encounters, including combinations, for ENTRI. These important explorations in future studies will provide additional insights into ENTRI for children. Finally, this study used data generated across one year before the COVID-19 pandemic. As such, its generalizability to patients and providers at present and in the future may be limited by evolutions in infection control practices and social distancing patterns. Although 2018 is not considered an atypical pre-COVID year for prevalence, severity, or burden of RI in children, longitudinal studies will be necessary to assess trends in pediatric ENTRI over time.
Despite these limitations, the findings from the current study on ENTRI prevalence and spending among US children enrolled in Medicaid with and without CCC may be useful in several ways. We hope the findings assist providers when counseling children and their families about ENTRI risk. In particular, complex care clinicians—who often exclusively provide care for children with multiple CCCs—may find it beneficial to convey the risk of lower-respiratory infection during discussions of anticipatory guidance. Beyond this, we hope that health service and clinical researchers evaluate opportunities to treat ENTRIs in the outpatient setting for children with CCCs. Especially for children with multiple CCCs, whose ENTRI spending predominately goes to inpatient care, more investigation is necessary to assess how amenable their ENTRIs are to outpatient management. Understanding how to mitigate severity of illness related to ENTRI in the outpatient setting will advance knowledge on the derivation and implementation of ENTRI action plans.
Supplementary Material
WHAT’S NEW.
Ear, nose, throat, and respiratory infections (ENTRI) are more common in children with complex chronic conditions (CCC) than their peers. Two-in-five children with multiple CCCs pursue care for lower-respiratory infection annually. Children with CCCs account for one-fourth of Medicaid spending on ENTRI.
Acknowledgment
Funding:
Supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) (UA6MC31101 to JB, MH and JR); The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (K23-HD097276 to SS); the Leadership Education in Neurodevelopmental and Related Disorders Training Program (LEND) (T73-MC11047 to SS); the Agency for Healthcare Research and Quality (AHRQ) (K08-HS025138 to JT).
Role of Funder:
Neither the HRSA, HHS, LEND, AHRQ nor the NIH had any role in 1) study design, 2) the collection, analysis and interpretation of data, 3) the writing of the report, and 4) the decision to submit the paper for publication.
Abbreviations:
- CCC
Complex Chronic Condition
- ENTRI
Ear, nose, throat, and respiratory infection
- ICD-10
International Classification of Diseases, 10th Revision
- OR
Odds ratio
Footnotes
All authors have no conflicts of interest to disclose.
Supplementary Data
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.acap.2022.07.004.
Contributor Information
Peter J. Dunbar, Department of Medicine, Brigham and Women’s Hospital, Boston, Mass.
Sarah A. Sobotka, Section of Developmental and Behavioral Pediatrics, Department of Pediatrics, The University of Chicago, Chicago, Ill.
Jonathan Rodean, Children’s Hospital Association, Lenexa, Kans.
Christian D. Pulcini, Department of Surgery and Pediatrics, University of Vermont Medical Center and Children’s Hospital, Burlington.
Michelle L. Macy, Department of Pediatrics, Feinberg School of Medicine, Northwestern University, Chicago, Ill.
Joanna Thomson, Division of Hospital Medicine, Cincinnati Children’s Hospital Medical Center, Ohio; Department of Pediatrics, University of Cincinnati College of Medicine, Ohio.
Debbi Harris, Family Voices of Minnesota, St. Paul.
Ryan J. Coller, Department of Pediatrics, University of Wisconsin School of Medicine and Public Health, Madison.
Anna Desmarais, Complex Care, Department of Medicine, Division of General Pediatrics, Boston Children’s Hospital, Mass..
Matthew Hall, Children’s Hospital Association, Lenexa, Kans.
Jay G. Berry, Complex Care, Department of Medicine, Division of General Pediatrics, Boston Children’s Hospital, Mass..
References
- 1.Dixon RE. Economic costs of respiratory tract infections in the United States. Am J Med. 1985;78:45–51. [DOI] [PubMed] [Google Scholar]
- 2.Troeger C, Forouzanfar M, Rao PC, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:1133–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen E, Berry JG, Sanders L, et al. Status complexicus? The emergence of pediatric complex care. Pediatrics. 2018;141(Suppl 3): S202–SS11. [DOI] [PubMed] [Google Scholar]
- 4.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126:647–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bucholz EM, Toomey SL, Schuster MA. Trends in pediatric hospitalizations and readmissions: 2010–2016. Pediatrics. 2019;143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berry JG, Ash AS, Cohen E, et al. Contributions of children with multiple chronic conditions to pediatric hospitalizations in the United States: a retrospective cohort analysis. Hosp Pediatr. 2017;7:365–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen E, Berry JG, Camacho X, et al. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130:e1463–e1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gruber C, Keil T, Kulig M, et al. History of respiratory infections in the first 12 yr among children from a birth cohort. Pediatr Allergy Immunol. 2008;19:505–512. [DOI] [PubMed] [Google Scholar]
- 9.Hay AD, Heron J, Ness A, et al. The prevalence of symptoms and consultations in pre-school children in the Avon Longitudinal Study of Parents and Children (ALSPAC): a prospective cohort study. Fam Pract. 2005;22:367–374. [DOI] [PubMed] [Google Scholar]
- 10.Griffin MR, Walker FJ, Iwane MK, et al. Epidemiology of respiratory infections in young children: insights from the new vaccine surveillance network. Pediatr Infect Dis J. 2004;23(11):S188–S192. Suppl. [DOI] [PubMed] [Google Scholar]
- 11.Vissing NH, Chawes BL, Rasmussen MA, et al. Epidemiology and risk factors of infection in early childhood. Pediatrics. 2018;141. [DOI] [PubMed] [Google Scholar]
- 12.Selwyn BJ. The epidemiology of acute respiratory tract infection in young children: comparison of findings from several developing countries. Rev Infectious Dis. 1990;12(8):S870–SS88. Suppl. [DOI] [PubMed] [Google Scholar]
- 13.Nakamura M, Zaslavsky A, Toomey S, et al. Pediatric readmissions after hospitalizations for lower respiratory infections. Pediatrics. 2017;140(2): e20160938. [DOI] [PubMed] [Google Scholar]
- 14.Steuart R, Tan R, Melink K, et al. Discharge before return to respiratory baseline in children with neurologic impairment. J Hosp Med. 2020;15(9):531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feinstein JA, Russell S, DeWitt PE, et al. R Package for pediatric complex chronic condition classification. JAMA Pediatr. 2018;172:594–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirsch AW, Monuteaux MC, Fruchtman G, et al. Characteristics of children hospitalized with aspiration pneumonia. Hosp Pediatr. 2016;6:659–666. [DOI] [PubMed] [Google Scholar]
- 17.Owayed AF, Campbell DM, Wang EL. Underlying causes of recurrent pneumonia in children. Arch Pediatr Adolesc Med. 2000;154:190–194. [DOI] [PubMed] [Google Scholar]
- 18.Weir K, McMahon S, Barry L, et al. Oropharyngeal aspiration and pneumonia in children. Pediatr Pulmonol. 2007;42:1024–1031. [DOI] [PubMed] [Google Scholar]
- 19.Pelton SI, Shea KM, Farkouh RA, et al. Rates of pneumonia among children and adults with chronic medical conditions in Germany. BMC Infect Dis. 2015;15:470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomson J, Hall M, Berry JG, et al. Diagnostic testing and hospital outcomes of children with neurologic impairment and bacterial pneumonia. J Pediatr. 2016;178:156–63 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hasegawa K, Goto T, Hirayama A, et al. Respiratory virus epidemiology among US infants with severe bronchiolitis: analysis of 2 multicenter, multiyear cohort studies. Pediatr Infect Dis J. 2019;38:e180–e1e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quinton LJ, Walkey AJ, Mizgerd JP. Integrative Physiology of Pneumonia. Physiol Rev. 2018;98:1417–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berry JG, Harris D, Coller RJ, et al. The interwoven nature of medical and social complexity in US children. JAMA Pediatr. 2020;174:891–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


