Abstract
Objective:
Shared medical decision making is most important when there are competing options for repair such as in treatment of abdominal aortic aneurysm (AAA). We sought to understand the sources of patients’ pre-existing knowledge about AAA to better inform treating physicians about patients’ needs for preoperative counseling.
Methods:
We performed a multi-center survey of patients facing AAA repair at 20 Veterans Affairs hospitals across the United States as part of the PReferences for Open Versus Endovascular Repair of AAA (PROVE-AAA) study. A validated survey instrument was administered to examine the sources of information available and commonly used by patients to learn about their repair options. The survey was administered by study personnel before the patient had any interaction with the vascular surgeon, as survey data was collected prior to the vascular clinic visit.
Results:
Preliminary analysis of data from 99 patients showed that our cohort was primarily male (99%) and elderly (mean age 73 years). They commonly had a history of hypertension (86%), prior myocardial infarction (32%), diabetes (32%), and were overweight (58%). Patients arrived at their surgeon’s office appointment with limited information. A majority of patients (52%) reported that they had not talked to their Primary Care Physician at all about their options for AAA repair, and half (50%) reported that their view of the different surgical options had not been influenced by anyone. Slightly less than half of patients reported that they did not receive any information about open surgical repair (OAR) and endovascular aortic aneurysm repair (EVAR) (41% and 37% respectively). Few patients indicated using the internet as their main source of information about OAR and EVAR (10% and 11% respectively).
Conclusions:
Patients are commonly referred for AAA repair having little to no information regarding AAA pathology or repair options. Fewer than one in five patients searched the internet or had accessed other sources of information on their own. Most vascular surgeons should assume that patients will present to their first vascular surgery appointment with minimal understanding of the treatment options available to them.
Table of Contents Summary
This survey revealed that among 99 veterans referred for elective AAA repair, 52% did not talk with their PCP about repair options and only 10% used the internet as a main source of information prior to their initial vascular surgery appointment.
Introduction
Abdominal aortic aneurysm (AAA) is the 14th leading cause of death among men over age 60, and is a common condition among United States veterans.1, 2 Nearly 5,000 patients undergo surgical repair of AAA each year in Veterans Affairs (VA) hospitals.3 Randomized trials, including the VA-based Open Versus Endovascular Repair (OVER) trial, have shown endovascular abdominal aortic aneurysm repair (EVAR) is associated with lower perioperative morbidity and mortality when compared with traditional open surgical aneurysm repair (OAR).4,5 However, OAR is associated with fewer long-term complications, such as late aneurysm rupture and need for re-intervention.5 Both repair modalities have been shown to have similar long term survival.6 Given these tradeoffs, it is important to consider patient preference when deciding on AAA repair modality. Patient preference surrounding repair options for AAA is an area of ongoing study worldwide.7, 8 However, the process of decision making and sources of information have not been well studied for patients in the United States, where EVAR use is most common when compared to other countries.9
Shared decision making has been used extensively in other specialties to help patients make the best choices in accordance with their personal values.10, 11 Patient involvement in the decision making process has been shown to increase satisfaction, and can significantly influence the type of surgical intervention ultimately performed.11 One frequently employed method of facilitating this involvement in a standardized way is through the use of decision aids.12 Research has shown that high quality decision aids directly add value by creating more realistic expectations and improving agreement between values and choices.13 Decision aids also increase patient knowledge and reduce decisional conflict.14, 15 However, the use of decision aids in the field of vascular surgery is not well described.
Treatment decisions for AAA must be aligned with individual patient values when clinical factors such as anatomy and comorbidities allow. For example, a patient for whom a rapid recovery is a priority and long-term durability is a lesser concern is likely to have a treatment preference that aligns with endovascular repair. Similarly, a patient who wishes to avoid the need for repeated follow-up appointments is likely to have a treatment preference that aligns with open surgical repair. Understanding a patient’s baseline level of knowledge is imperative in using shared decision making to arrive at the treatment modality best suited to the patient’s preferences and values. To that end, we sought to determine patients’ baseline knowledge about AAA treatment and the information sources they used to acquire this knowledge. Here, we describe a preliminary analysis related to patient information sources studied in the PRreferences for Open Versus Endovascular Repair of AAA (PROVE-AAA) randomized trial.16, 17 Primary aims of the PROVE-AAA trial include characterizing factors that contribute to patient preferences among aneurysm repair modalities, and determining whether the use of a validated decision aid can better align patient preferences with the repair type ultimately performed. Within that broader scope, this analysis focuses specifically on identifying sources of information patients have been exposed to prior to consultation with a vascular surgeon for AAA repair.
Methods
Twenty VA Medical Centers and associated vascular surgery teams participated in this study. Study sites included only hospitals where both EVAR and OAR are commonly performed, and were selected to recruit a nationally representative sample population (Appendix 1). Institutional review board (IRB) approval was obtained at each local site as well as VA Central IRB. Sites were divided into a control arm and intervention arm via a stratified randomization scheme designed to minimize potential bias and ensure balance with regard to operative volume and complexity.
At each site, new AAA consultations were reviewed by a designated site study coordinator to identify patients with AAA measuring 5.0 cm in diameter or larger. The site principal investigator (attending vascular surgeon) then reviewed the imaging study and the patient’s electronic health record to ensure the patient was a candidate for both endovascular and open repair. Patients who were not potential candidates for both OAR and EVAR, or who had already undergone AAA repair, were excluded from the study.
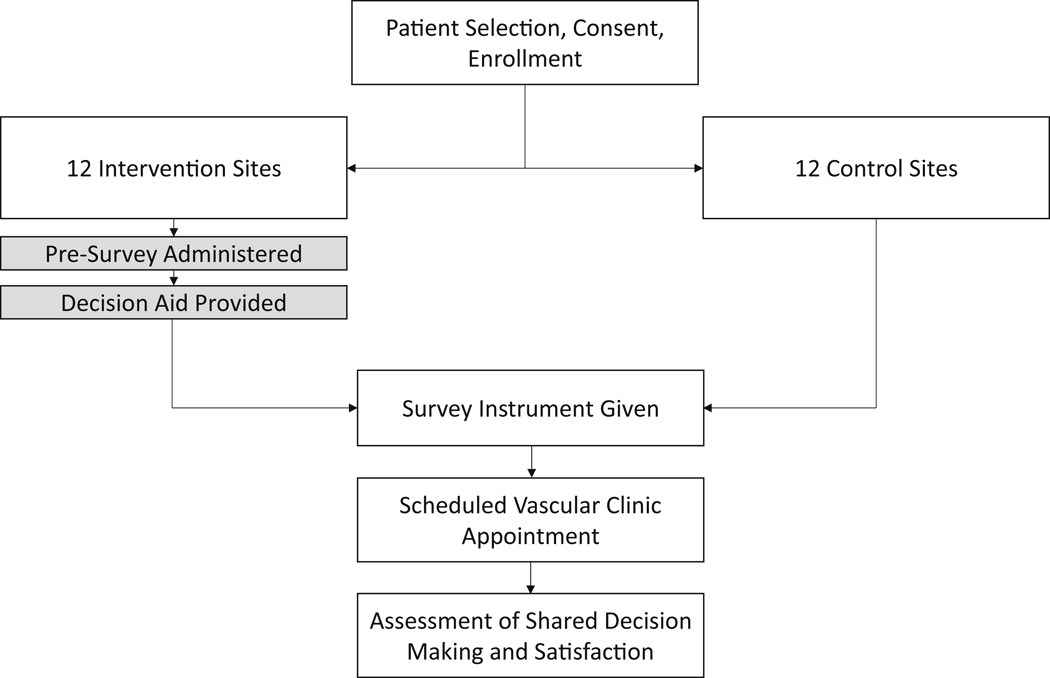
Enrollment was capped at twelve patients per study site for a total enrollment goal of 240 study participants split evenly between the control and intervention arms of the study. Screening, informed consent, and enrollment were performed by a site study coordinator on the day of the patient’s scheduled appointment with the vascular surgeon (Figure 1).
Figure 1:
Study design for our study of preferences for abdominal aortic aneurysm repair type.
Control and Intervention Site Protocols
At control sites, the site study coordinator then administered a survey instrument comprised of 31 questions assessing four major domains: Patient Information Sources, Patient Knowledge of the Decision, Understanding of Preferences, and Shared Decisions (Table I). The survey instrument was developed and validated by experts in survey research at the Picker Institute in England and, with their guidance, it was revised to use United States English language at the 8th grade level (Appendix 2).18
Table 1:
Domains and sample questions in our survey instrument
| Major Domains - objectives | Sample question (examples) |
|---|---|
| Patient Information Sources - To learn who provides knowledge and influences Veterans about their AAA | Before you looked at your decision aid, who or what were the main sources of information about endovascular repair? |
| Patient Knowledge of the Decision - To learn how Veterans understand their AAA and their options | Before you looked at your decision aid, would you say you had considered or not considered the options for repair? |
| Understanding preferences - To understand the factors that Veterans use to make their decisions | Open surgery involves an abdominal incision, after which you can’t lift heavy items for more than a month; the recovery time is shorter (one to two weeks) for endovascular repair. How important to you is the duration of your recovery? |
| Shared Decisions: The Veteran Collaboration and sharing the decision | The decision aid prepared me to talk to my hospital doctor or surgeon about what matters most to me (Yes, To some extent, No, Unsure). |
At intervention sites, the site study coordinator administered a pre-survey comprised of a single question evaluating the patient’s initial preference (if she/he had one). The patient was then provided with a decision aid describing the risks and choices involved in AAA treatment options. The decision aid used in this study was validated in prior studies in the National Health System18, and was adapted and tested for use in VA hospitals (Appendix 2). After reviewing the decision aid, the patient was given a validated survey instrument functionally identical to the one used in the control arm of the study (Appendix 2).
All study materials were administered in paper format with the help of site study coordinators to control for variation in availability of computers across sites. After completion of the study survey instruments, patients at both control and intervention sites underwent standard, outpatient vascular surgery consultation and proceeded with either aneurysm repair or observation and interval follow-up after their visit. All patient information was collected and de-identified as part of the study protocol and stored on secure central VA study servers. The full study design and administration have been previously published.17
Survey questions related to the information source
The survey instrument administered at the time of enrollment for each patient contained several questions related to the sources of information the patient was exposed to before meeting with the vascular surgeon. These questions, shown in Figures 2–5 below, were integrated in the context of the central study survey instruments for patients at both control and intervention sites. These questions describe the type and nature of the information available to patients who are considering repair. Given that these questions did not relate to the central study question, the topic of patient information sources regarding aneurysm repair options was explored in this study prior to addressing the central PROVE-AAA study question related to the effect of decision aids on patient preferences for aortic aneurysm repair. Our site investigator committee reviewed the use of the information source questions and approved preliminary exploration of the study questions related to this topic.
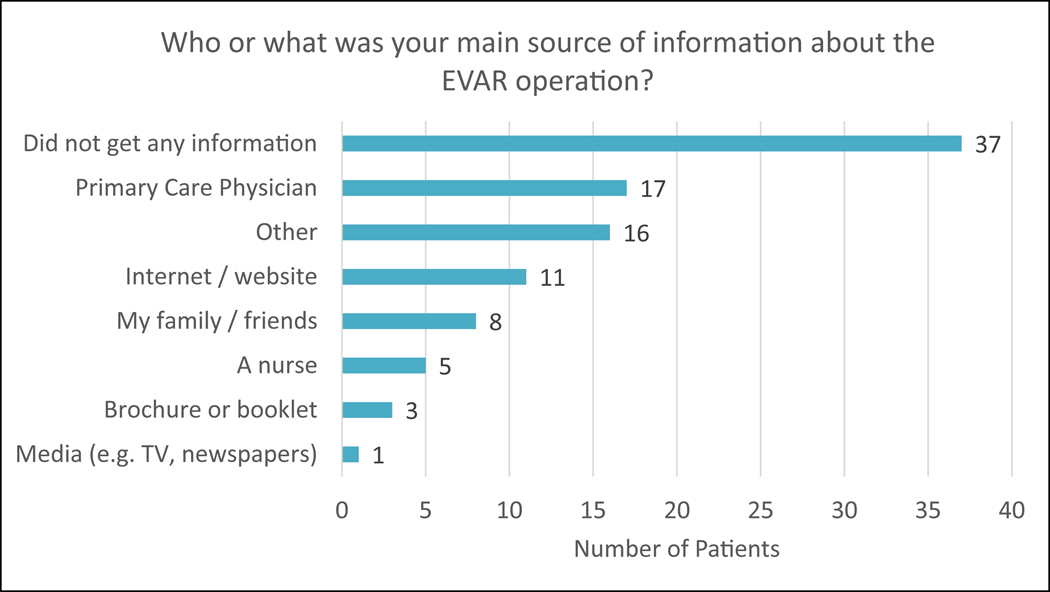
Figure 2:
Survey results assessing main source of information about EVAR.
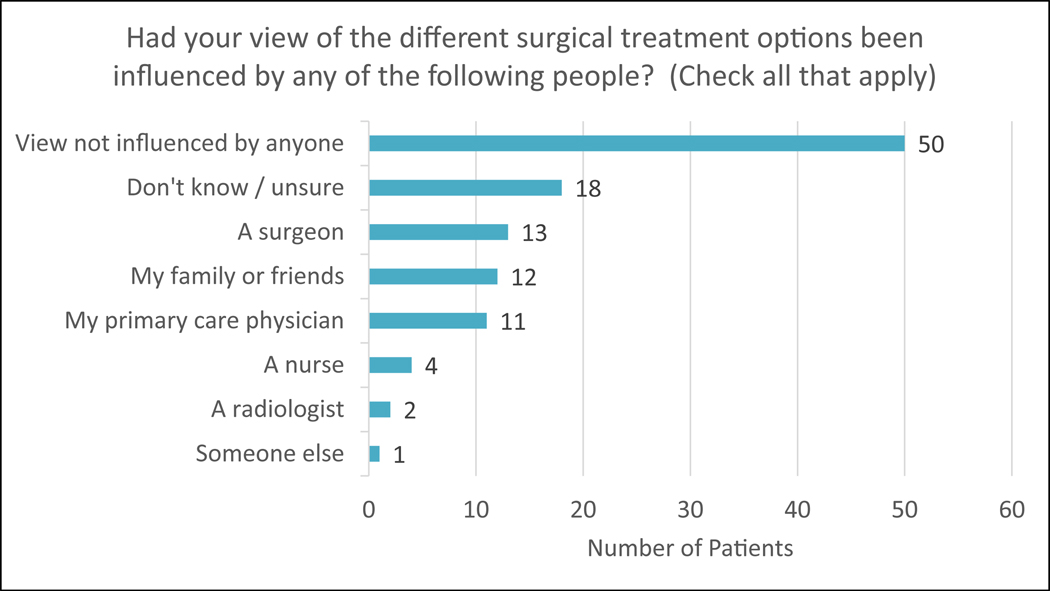
Figure 5:
Survey results assessing how patient’s views of treatment options have been influenced.
Results
The first 99 patients of the PROVE-AAA study were analyzed. This represents the cohort of patients enrolled in either the control or intervention group with survey data available for analysis as of August 31, 2018. Mean patient age was 73 years, gender was 99% male, and our cohort was predominantly white (87%). Demographics, medical history and risk factors of patients enrolled in the study were representative of patients facing aneurysm repair in the veteran population (Table II).2
Table 2:
Demographic and medical characteristics of study cohort (n=99)
| Variable | Values |
|---|---|
| Age mean (SD) | 72.7 (5.9) |
| Male gender | 99% |
| White race | 87% |
| Medical Comorbidities | |
| Hypertension | 86% |
| Overweight (BMI > 25) | 58% |
| Prior myocardial infarction | 32% |
| Diabetes | 32% |
| Congestive heart failure | 28% |
| Chronic kidney disease (Creatinine >1.7) | 21% |
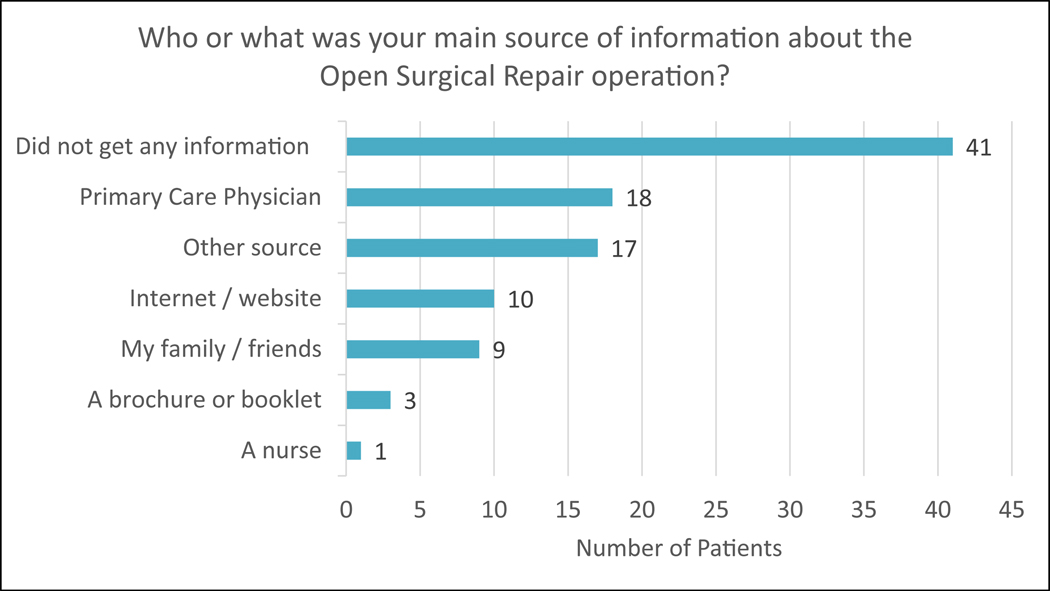
Overall, 37% (n=37) of patients reported that they did not receive any information at all about the options for EVAR, and 41% (n=41) reported not receiving information about OAR. When asked about internet usage, 11% (n=11) of patients reported using the internet as their main source of information about EVAR, and 10% (n=10) used the internet to learn about OAR. Additionally, 17% (n=17) of patients obtained their baseline knowledge about EVAR from their PCP, and 18% (n=18) learned about OAR from their PCP. With regards to other sources, 16% (n=16) of patients selected “Other” as their primary source of information about EVAR and 17% (n=17) selected this option for about OAR. Of those who made this selection, many indicated that a previous encounter with a vascular surgeon was their main source of information about EVAR or OAR (Figures 2 and 3).
Figure 3:
Survey results assessing main source of information about OAR.
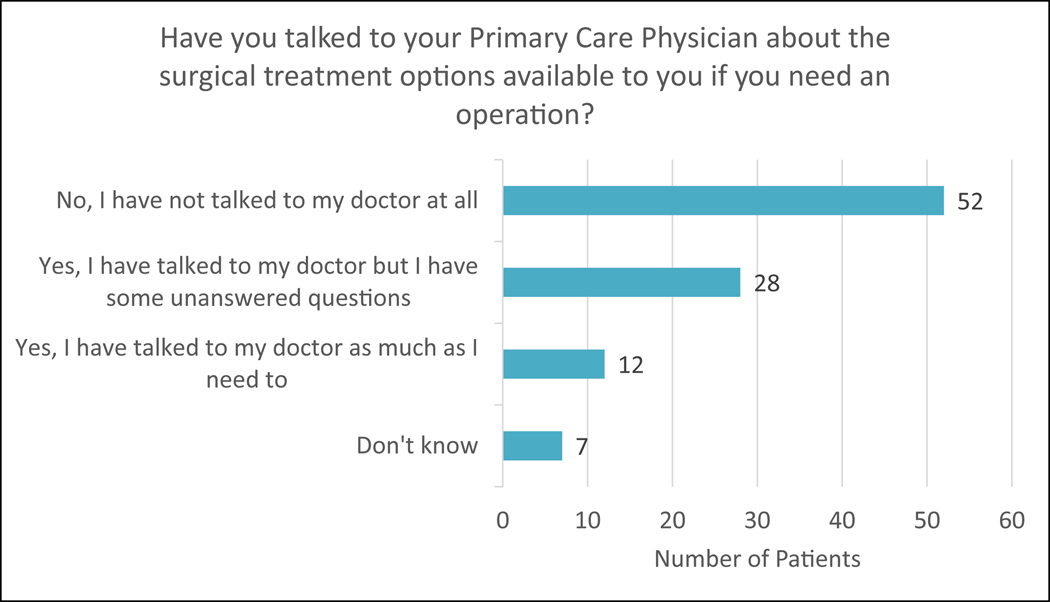
When asked about interactions with their primary care physician, 52% (n=52) of patients indicated that their primary care physician did not talk with them at all about their options for AAA treatment, 28% (n=28) marked that they had talked to their doctor but still had unanswered questions, and 12% (n=12) reported having talked to their primary care physician “as much as I need to” (Figure 4).
Figure 4:
Survey results assessing whether patient has spoken to PCP about treatment options.
Regarding external influences, 50% (n=50) of study participants reported that their views on the different surgical treatment options had not been influenced at all by anyone, and 18% (n=18) were unsure. A previous encounter with a surgeon had influenced 13% (n=13) of study participants, family and friends influenced 12% (n=12), and 11% (n=11) of patients said that their primary care physician had influenced their views (Figure 5).
Discussion
We administered a validated survey instrument to 99 patients facing AAA repair as part of a prospective, cluster-randomized, multicenter study investigating the influence of decision aid usage on preoperative shared decision making. The survey instrument was designed to measure patient preferences, values and baseline information sources pertaining to AAA treatment modalities. We found that very few patients searched the internet for information prior to their vascular surgery appointment, and around half reported having no external influences at all. These findings imply that patients will frequently present to their initial encounter with a vascular surgeon having little to no understanding of AAA pathology or treatment.
Our study provides insight into sources of information commonly utilized by patients prior to their first meeting with a vascular surgeon. This was characterized for patients facing AAA repair in the United Kingdom in 2008, where a postal survey with 167 respondents showed that only 10% had discussed repair options with a doctor, and 89% had not received any written information about EVAR or OAR.7 However, this area of inquiry has remained relatively underexplored in the United States in more recent times.
Perhaps most surprising is our finding that only 10% of patients facing AAA repair used the internet as a main source of information about OAR or EVAR. Patient consumption of online medical information is becoming more widespread across many age groups and demographics in the United States.19 For example, it is estimated that 15.1% to 47% of Emergency Department patients research symptoms online prior to seeking care.20 However, it has also been shown that older patients are less likely to access online medical information, and this could be a factor in our results.21 Survey data from 32,139 adults in the 2011 National Health Interview Study showed that among those over 60 years in age, only 16.71% reported searching the internet for health information.19 While innovative technology-based forms of preoperative patient education have shown great promise in fields such as orthopedic, plastic and urological surgery, they have not been studied as thoroughly for application in vascular surgery where patients are frequently older and have more medical comorbidities. 22 Vascular surgeons must take these factors into account when considering matters of patient education and counseling patients facing these important decisions.
Greater than half (52%) of our study participants reported not talking to their primary care physician at all about the potential treatment options, and slightly less than half received no written information about OAR or EVAR (41% and 37% respectively). These findings have important implications for vascular surgeons who regularly receive consultations from referring physicians for patients with abdominal aortic aneurysm. Despite an extensive familiarity within our own specialty of the available treatment options for patients with AAA, vascular surgeons should not presume that patients, or their referring physicians, have the same a priori knowledge of the treatment options available, nor their advantages and disadvantages. Especially given the current debates about the long-term durability of endovascular repair, as well as current trends in the volumes of open surgical repair, a candid discussion with patients about their preferences for treatment options is a necessary component of an initial consultation when patients are referred for aneurysm treatment. For example, simply telling a patient “you are a good candidate for a stent” without soliciting the patient’s opinion about their ability to adhere to post-operative surveillance may create circumstances wherein surgeon preferences and patient preferences are misaligned. As the sole arbiter of advanced vascular education and intervention for patients with aortic aneurysm, we believe excelling in aligning patient and surgeon preferences in AAA care is an important goal for vascular surgeons, and this process begins at the initial clinic visit. We hope that the results of this study will serve to more clearly define patients’ baseline level of knowledge and help vascular surgeons calibrate their patient education efforts in order to provide the best care possible.
Our study has several limitations. First, the veteran cohort studied herein does somewhat limit generalizability to the AAA population in total. There is a lack of diversity in our patient population with this cohort exhibiting a higher proportion of male and White non-Hispanic patients than the general AAA population. 23 Our study sites were, however, carefully selected to recruit a nationally representative sample of veterans. Second, patients who receive care through the VHA are known to experience primary care provider turnover at a higher rate than the national average, and this can negatively impact their experience of care.24 Patients who experience turnover may feel that they have little rapport with their primary care provider, and may not see him or her as a realistic source of information about AAA repair. Third, with regard to age and comorbidity profile, our study cohort is slightly older, and has more comorbidities than patients enrolled in large randomized trials comparing open and endovascular repair of AAA. Fourth, we did not specifically collect information regarding patients’ ability to access technology. As some patients may not have access to computers or the internet, it is difficult to ascertain whether low rates of online health information usage are due to a lack of access or due to favoring other education modalities. Related to this issue, it is important to note that this analysis does not control for variations in socioeconomic status, education level, or geographic factors. This information was collected as part of the study, but the decision was made to leave the data blinded until completion of the enrollment phase of our trial when we will be able to draw more statistically powerful conclusions from it. These important challenges are an area of active study for our group and will receive significant attention in future analyses of the PROVE-AAA trial. Nonetheless, our cohort is representative of patients facing AAA repair in general and may help better understand the ways decisions are made in real-world practice.25
Conclusion
Patients are commonly referred for AAA repair having little to no information regarding this pathology or repair options. Our study suggests that patients also are unlikely to search the internet or access other sources of information on their own. Therefore, patients frequently present to their first vascular surgery appointment with minimal understanding of the treatment options that may be available to them. The ultimate responsibility for a fair and balanced examination of the advantages of open and endovascular abdominal aortic aneurysm repair rests squarely with vascular surgeons who treat patients with AAA.
Supplementary Material
ARTICLE HIGHLIGHTS.
Type of Research:
Multicenter prospective randomized controlled trial
Key Findings:
Among 99 veterans referred for elective AAA repair, 52% did not talk with their PCP about repair options and only 10% used the internet as a main source of information prior to their initial vascular surgery appointment.
Take home Message:
When approaching patient education and shared decision making, surgeons should assume that patients will frequently present to their first vascular surgery appointment with minimal understanding of AAA pathology and the treatment options that may be available to them.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Eliason JL, Upchurch GR Jr. Endovascular abdominal aortic aneurysm repair. Circulation. 2008;117(13):1738–44. [DOI] [PubMed] [Google Scholar]
- 2.Lederle FA, Johnson GR, Wilson SE, Chute EP, Hye RJ, Makaroun MS, et al. The aneurysm detection and management study screening program: validation cohort and final results. Aneurysm Detection and Management Veterans Affairs Cooperative Study Investigators. Archives of internal medicine. 2000;160(10):1425–30. [DOI] [PubMed] [Google Scholar]
- 3.Lederle FA, Stroupe KT, Open Versus Endovascular Repair Veterans Affairs Cooperative Study G. Cost-effectiveness at two years in the VA Open Versus Endovascular Repair Trial. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2012;44(6):543–8. [DOI] [PubMed] [Google Scholar]
- 4.Lederle FA, Freischlag JA, Kyriakides TC, Padberg FT Jr., Matsumura JS, Kohler TR, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA : the journal of the American Medical Association. 2009;302(14):1535–42. [DOI] [PubMed] [Google Scholar]
- 5.Lederle FA, Freischlag JA, Kyriakides TC, Matsumura JS, Padberg FT Jr., Kohler TR, et al. Long-term comparison of endovascular and open repair of abdominal aortic aneurysm. The New England journal of medicine. 2012;367(21):1988–97. [DOI] [PubMed] [Google Scholar]
- 6.Schermerhorn ML, Buck DB, O’Malley AJ, Curran T, McCallum JC, Darling J, et al. Long-Term Outcomes of Abdominal Aortic Aneurysm in the Medicare Population. The New England journal of medicine. 2015;373(4):328–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reise JA, Sheldon H, Earnshaw J, Naylor AR, Dick F, Powell JT, et al. Patient preference for surgical method of abdominal aortic aneurysm repair: postal survey. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2010;39(1):55–61. [DOI] [PubMed] [Google Scholar]
- 8.Winterborn RJ, Amin I, Lyratzopoulos G, Walker N, Varty K, Campbell WB. Preferences for endovascular (EVAR) or open surgical repair among patients with abdominal aortic aneurysms under surveillance. Journal of vascular surgery. 2009;49(3):576–81 e3. [DOI] [PubMed] [Google Scholar]
- 9.Beck AW, Sedrakyan A, Mao J, Venermo M, Faizer R, Debus S, et al. Variations in Abdominal Aortic Aneurysm Care: A Report From the International Consortium of Vascular Registries. Circulation. 2016;134(24):1948–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Veterans Administration Makes Shared Decision Making Resources Available to Help with Long Term Care Choices. The Informed Medical Decisions Foundation; [cited 2014]; Available from: http://www.informedmedicaldecisions.org/2013/03/28/the-veterans-administration-makes-shared-decision-making-resources-availableto-help-with-long-term-care-choices/. [Google Scholar]
- 11.Katz SJ, Lantz PM, Janz NK, Fagerlin A, Schwartz K, Liu L, et al. Patient involvement in surgery treatment decisions for breast cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2005;23(24):5526–33. [DOI] [PubMed] [Google Scholar]
- 12.Boss EF, Mehta N, Nagarajan N, Links A, Benke JR, Berger Z, et al. Shared Decision Making and Choice for Elective Surgical Care: A Systematic Review. Otolaryngol Head Neck Surg. 2016;154(3):405–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinstein JN, Clay K, Morgan TS. Informed patient choice: patient-centered valuing of surgical risks and benefits. Health affairs. 2007;26(3):726–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chabrera C, Zabalegui A, Bonet M, Caro M, Areal J, Gonzalez JR, et al. A Decision Aid to Support Informed Choices for Patients Recently Diagnosed With Prostate Cancer: A Randomized Controlled Trial. Cancer Nurs. 2015;38(3):E42–50. [DOI] [PubMed] [Google Scholar]
- 16.Preferences for Open Vs. Endovascular Repair for Aortic Abdominal Aneurysm. Available from: https://ClinicalTrials.gov/show/NCT03115346.
- 17.Columbo JA, Goodney PP, Kang R, Spangler EL, Newhall K, Brooke BS, et al. Design of The PReferences for Open Versus Endovascular Repair of Abdominal Aortic Aneurysm (PROVE-AAA) Trial. Ann Vasc Surg (In Press). 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute TP. Survey of Patient Preference for Method of Abdominal Aortic Aneurysm Repair. In: Institute TP, editor. [Google Scholar]
- 19.Amante DJ, Hogan TP, Pagoto SL, English TM, Lapane KL. Access to care and use of the Internet to search for health information: results from the US National Health Interview Survey. J Med Internet Res. 2015;17(4):e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCarthy DM, Scott GN, Courtney DM, Czerniak A, Aldeen AZ, Gravenor S, et al. What Did You Google? Describing Online Health Information Search Patterns of ED patients and Their Relationship with Final Diagnoses. West J Emerg Med. 2017;18(5):928–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scott G, McCarthy DM, Aldeen AZ, Czerniak A, Courtney DM, Dresden SM. Use of Online Health Information by Geriatric and Adult Emergency Department Patients: Access, Understanding, and Trust. Acad Emerg Med. 2017;24(7):796–802. [DOI] [PubMed] [Google Scholar]
- 22.Villanueva C, Talwar A, Doyle M. Improving informed consent in cardiac surgery by enhancing preoperative education. Patient education and counseling. 2018;101(12):2047–53. [DOI] [PubMed] [Google Scholar]
- 23.NCVAS. Profile of Veterans: 2014. Data from the American Community Survey. 2016. [Google Scholar]
- 24.Reddy A, Pollack CE, Asch DA, Canamucio A, Werner RM. The Effect of Primary Care Provider Turnover on Patient Experience of Care and Ambulatory Quality of Care. JAMA Intern Med. 2015;175(7):1157–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kent KC, Zwolak RM, Egorova NN, Riles TS, Manganaro A, Moskowitz AJ, et al. Analysis of risk factors for abdominal aortic aneurysm in a cohort of more than 3 million individuals. Journal of vascular surgery. 2010;52(3):539–48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.