Abstract
BACKGROUND
Esophageal carcinoma presents as 2 types, esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC) with the frequency of both changing in the United States (US).
AIM
To investigate EAC/ESCC incidence time trends among the 3 main US racial groups and investigate trends in US EAC survival by ethnicity.
METHODS
Twenty-five years (1992-2016) of data from SEER 13 program was analyzed to compare incidence trends in EAC and ESCC between non-Hispanic whites (nHW), non-Hispanic Blacks (nHB) and Hispanics (Hisp) using SEERStat®. In addition, SEER 18 data, from 1975-2015, on EAC in the US was analyzed to evaluate racial disparities in incidence and survival using SEERStat® and Ederer II method.
RESULTS
In the 3 major US ethnic groups, age-adjusted incidence of ESCC has declined while EAC has continued to rise from 1992-2016. Of note, in Hisp, the EAC incidence rate increased while ESCC decreased from 1992 to 2016, resulting in EAC as the predominant esophageal cancer subtype in this group since 2011, joining nHW. Furthermore, although ESCC remains the predominant tumor in nHB, the difference between ESCC and EAC has narrowed dramatically over 25 years. EAC survival probabilities were worse in all minority groups compared to nHw.
CONCLUSION
Hisp have joined nHW as US ethnic groups more likely to have EAC than ESCC. Of note, EAC incidence in nHB is increasing at the highest rate nationally. Despite lower EAC incidence in all minority groups compared to nHW, these populations have decreased survival compared to nHW.
Keywords: Esophageal carcinoma, Ethnicity, Incidence, Survival, Disparity, Race
Core Tip: There is a higher incidence of esophageal adenocarcinoma (EAC) in non-Hispanic whites (nHw). Esophageal squamous cell carcinoma (ESCC) is more common than EAC in non-Hispanic Blacks. Previous research reported higher incidence of ESCC compared to EAC in Hispanics (Hisp) as well. This study reveals that Hisp have joined nHw as US ethnic groups with EAC as the predominant esophageal cancer. Despite lower EAC incidence in all minority groups compared to nHw, these populations have lower survival compared to nHw.
INTRODUCTION
Esophageal carcinoma (EC) is the eight most common malignancy and the sixth leading cause of cancer related mortality globally[1,2]. The 5 year survival rate of esophageal carcinoma is 15%-30%, making it one of the most lethal malignancies[3-5]. There are 2 main histological subtypes of esophageal carcinoma, esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC). Depending on the histological subtype, incidence of esophageal carcinoma is 3-10 times higher in males compared to females[6].
Ethnic disparities in esophageal carcinoma incidence and prevalence have been evaluated in the past. Higher incidence of EAC in non-Hispanic White (nHW) males is well known and it has been reported to be the most rapidly increasing solid organ malignancy in this ethnic and gender group[7]. In contrast, ESCC is more common than EAC in non-Hispanic Blacks (nHB)[8]. In addition to environmental factors, genetic factors are also thought to play an important role in EC ethnic disparities[9].
Hispanics (Hisp) comprise 18.5% of the total US population, making them the largest minority ethnic group in the United States (US) per the US Census Bureau[10]. Very limited data is available evaluating esophageal cancer in Hisp. Ricardo et al[11] reported higher number of metastatic and untreated EC cases in Hisp despite lower prevalence compared to nHW. Previous research also reported higher incidence of ESCC in Hisp[12]. In addition, incidence trends of EAC in other minority ethnic groups like Hisp, non-Hispanic American Indians/Alaska native (nHAI/AN), non-Hispanic Asians/Pacific islanders (nHA/PI) have not been well assessed. Furthermore, EAC-related survival in US minority groups has not been studied. Thus, the primary study aim was to examine EC incidence time trends (both EAC & ESCC) between the 3 main US racial groups, with a focus on Hisp, assessing 25 years of data and the second aim of our study was to investigate temporal trends in incidence of EAC over the last 40 years in the US and highlight ethnic disparities in survival.
MATERIALS AND METHODS
Phase 1
Using data from the Surveillance, Epidemiology, and End Results 13 (SEER) program of cancer registries, we collected 25 years (1992-2016) data on EAC and ESCC in the US. This data was adjusted for age to the US 2000 standard population using SEERStat®. After age adjustment, this data was plotted using Microsoft Excel® to visually compare incidence trends in EAC and ESCC over 25 years in nHW, nHB and Hisp. Annual percent change (APC) was calculated using weighted least squares method and p values were calculated using SEERStat® and t-test.
Phase 2
Using data from the Surveillance, Epidemiology, and End Results 18 (SEER) program of cancer registries, we collected 40 years (1975-2015) data on esophageal adenocarcinoma in the US. After adjusting for age using SEERStat®, this data was plotted to visually compare trends over the last 40 years in different ethnic groups. Ten years of (2006-2016) data was used to calculate relative survival rates at 1, 2, 3, 4, and 5 years for different ethnic groups using Ederer II method and compared between these groups.
RESULTS
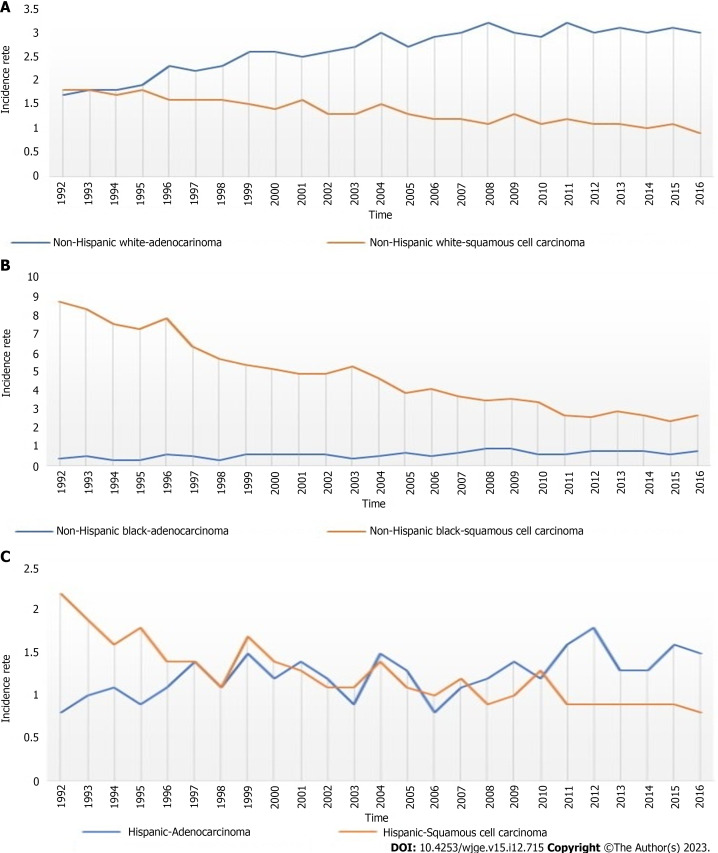
In phase 1 of this study, 25 years of data from SEER 13 cancer registry was analyzed. For the 3 largest ethnic groups in the US (nHw, nHB, Hisp), EAC age adjusted incidence increased during the study period while the ESCC rate declined. In Hisp, the incidence rate of EAC increased from 0.8 to 1.5/100000 (APC = 1.5, P < 0.001) compared to ESCC decreasing from 2.2 to 0.8/100000 over the study period (APC = -3.1, P < 0.001, Figure 1, Table 1). This change over time has resulted in EAC becoming the predominant esophageal cancer since 2011 in Hisp. Among nHw, the EAC incidence rate increased from 1.7 to 3/100000 (APC = 2.2, P < 0.001) while ESCC incidence decreased from 1.8 to 0.9/100000 (APC = -2.5, P < 0.001, Figure 1, Table 1). This has lead to EAC as the predominant esophageal cancer since 1993 within this group. For nHB, EAC incidence increased from 0.4 to 0.8/100000 (APC = 2.6, P < 0.001) while ESCC dramatically decreased from 8.8 to 2.7/100000 (APC = -5.2, P < 0.001, Figure 1, Table 1) over the study interval. Despite these EC changes in nHB, ESCC remains the predominant esophageal cancer in this group.
Figure 1.
Age adjusted incidence rates (1992-2016) of esophageal adenocarcinoma and squamous cell carcinoma in non-Hispanic White, non-Hispanic Black, and Hispanics. A: Non-Hispanic White; B: Non-Hispanic Black; C: Hispanics.
Table 1.
Age adjusted incidence rates per 100000 (1992-2016) and annual percent change in esophageal squamous cell and adenocarcinoma for different racial groups in the United States
|
nHW
|
nHB
|
Hisp
|
||||
|
EAC
|
ESCC
|
EAC
|
ESCC
|
EAC
|
ESCC
|
|
| 1992-2016 APC | 2.2 | -2.5 | 2.6 | -5.2 | 1.5 | -3.1 |
| P value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Year | Rate | Rate | Rate | Rate | Rate | Rate |
| 1992 | 1.7 | 1.8 | 0.4 | 8.8 | 0.8 | 2.2 |
| 1993 | 1.8 | 1.8 | 0.5 | 8.4 | 1 | 1.9 |
| 1994 | 1.8 | 1.7 | 0.3 | 7.6 | 1.1 | 1.6 |
| 1995 | 1.9 | 1.8 | 0.3 | 7.3 | 0.9 | 1.8 |
| 1996 | 2.3 | 1.6 | 0.6 | 7.9 | 1.1 | 1.4 |
| 1997 | 2.2 | 1.6 | 0.5 | 6.4 | 1.4 | 1.4 |
| 1998 | 2.3 | 1.6 | 0.3 | 5.7 | 1.1 | 1.1 |
| 1999 | 2.6 | 1.5 | 0.6 | 5.4 | 1.5 | 1.7 |
| 2000 | 2.6 | 1.4 | 0.6 | 5.2 | 1.2 | 1.4 |
| 2001 | 2.5 | 1.6 | 0.6 | 4.9 | 1.4 | 1.3 |
| 2002 | 2.6 | 1.3 | 0.6 | 4.9 | 1.2 | 1.1 |
| 2003 | 2.7 | 1.3 | 0.4 | 5.3 | 0.9 | 1.1 |
| 2004 | 3 | 1.5 | 0.5 | 4.7 | 1.5 | 1.4 |
| 2005 | 2.7 | 1.3 | 0.7 | 3.9 | 1.3 | 1.1 |
| 2006 | 2.9 | 1.2 | 0.5 | 4.1 | 0.8 | 1 |
| 2007 | 3 | 1.2 | 0.7 | 3.7 | 1.1 | 1.2 |
| 2008 | 3.2 | 1.1 | 0.9 | 3.5 | 1.2 | 0.9 |
| 2009 | 3 | 1.3 | 0.9 | 3.6 | 1.4 | 1 |
| 2010 | 2.9 | 1.1 | 0.6 | 3.4 | 1.2 | 1.3 |
| 2011 | 3.2 | 1.2 | 0.6 | 2.7 | 1.6 | 0.9 |
| 2012 | 3 | 1.1 | 0.8 | 2.6 | 1.8 | 0.9 |
| 2013 | 3.1 | 1.1 | 0.8 | 2.9 | 1.3 | 0.9 |
| 2014 | 3 | 1 | 0.8 | 2.7 | 1.3 | 0.9 |
| 2015 | 3.1 | 1.1 | 0.6 | 2.4 | 1.6 | 0.9 |
| 2016 | 3 | 0.9 | 0.8 | 2.7 | 1.5 | 0.8 |
ESCC: Esophageal squamous cell; EAC: Adenocarcinoma; nHB: Non-Hispanic Blacks; nHW: Non-Hispanic Blacks; Hisp: Hispanics.
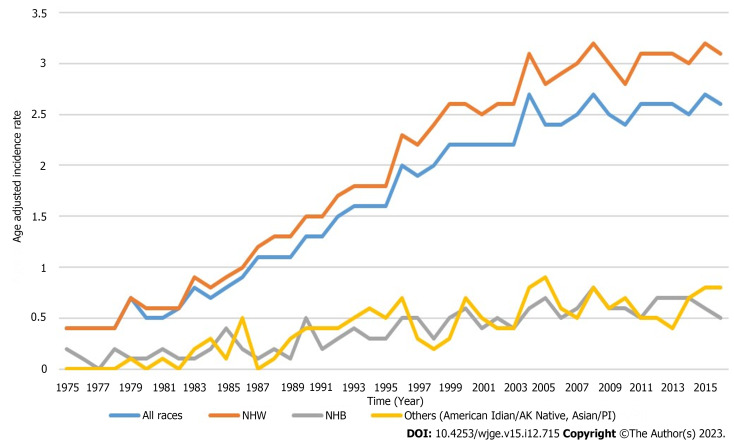
In phase 2, 40 years of EAC data was analyzed (1975 to 2015). The overall age adjusted incidence rate of EAC progressively increased from 1975 to 2007 in the US (0.4/100000 to 2.8/100000). Following, a plateau in the age adjusted incidence rate was observed (Age adjusted incidence rate of EAC for all races in 2007 = 3/100000, age adjusted incidence rate of EAC for all races in 2016 = 3/100000) (Table 2, Figure 2). A similar trend was observed in nHw and nHB. In nHw, age adjusted incidence rate of EAC was 3/000000 in 2007 and 3.1/100000 in 2016. In nHB, age adjusted incidence rate of EAC was 0.6/100000 in 2007 and 0.5/100000 in 2016 (Table 2, Figure 2). However, in the other minority group (a combination of nHAI/AN and nHA/PI), EAC incidence continues to rise after 2007. The age adjusted incidence rate was 0.5/100000 in 2007 and 0.8/100000 in 2016 in the combined other minority group.
Table 2.
Age adjusted esophageal adenocarcinoma incidence rates per 100000, United States ethnic groups (1975-2015)
|
Year
|
All races
|
nHW
|
nHB
|
Others (American Indian/AK Native, Asian/PI)
|
| 1975 | 0.4 | 0.4 | 0.2 | 0 |
| 1976 | 0.4 | 0.4 | 0.1 | 0 |
| 1977 | 0.4 | 0.4 | 0 | 0 |
| 1978 | 0.4 | 0.4 | 0.2 | 0 |
| 1979 | 0.7 | 0.7 | 0.1 | 0.1 |
| 1980 | 0.5 | 0.6 | 0.1 | 0 |
| 1981 | 0.5 | 0.6 | 0.2 | 0.1 |
| 1982 | 0.6 | 0.6 | 0.1 | 0 |
| 1983 | 0.8 | 0.9 | 0.1 | 0.2 |
| 1984 | 0.7 | 0.8 | 0.2 | 0.3 |
| 1985 | 0.8 | 0.9 | 0.4 | 0.1 |
| 1986 | 0.9 | 1 | 0.2 | 0.5 |
| 1987 | 1.1 | 1.2 | 0.1 | 0 |
| 1988 | 1.1 | 1.3 | 0.2 | 0.1 |
| 1989 | 1.1 | 1.3 | 0.1 | 0.3 |
| 1990 | 1.3 | 1.5 | 0.5 | 0.4 |
| 1991 | 1.3 | 1.5 | 0.2 | 0.4 |
| 1992 | 1.5 | 1.7 | 0.3 | 0.4 |
| 1993 | 1.6 | 1.8 | 0.4 | 0.5 |
| 1994 | 1.6 | 1.8 | 0.3 | 0.6 |
| 1995 | 1.6 | 1.8 | 0.3 | 0.5 |
| 1996 | 2 | 2.3 | 0.5 | 0.7 |
| 1997 | 1.9 | 2.2 | 0.5 | 0.3 |
| 1998 | 2 | 2.4 | 0.3 | 0.2 |
| 1999 | 2.2 | 2.6 | 0.5 | 0.3 |
| 2000 | 2.2 | 2.6 | 0.6 | 0.7 |
| 2001 | 2.2 | 2.5 | 0.4 | 0.5 |
| 2002 | 2.2 | 2.6 | 0.5 | 0.4 |
| 2003 | 2.2 | 2.6 | 0.4 | 0.4 |
| 2004 | 2.7 | 3.1 | 0.6 | 0.8 |
| 2005 | 2.4 | 2.8 | 0.7 | 0.9 |
| 2006 | 2.4 | 2.9 | 0.5 | 0.6 |
| 2007 | 2.5 | 3 | 0.6 | 0.5 |
| 2008 | 2.7 | 3.2 | 0.8 | 0.8 |
| 2009 | 2.5 | 3 | 0.6 | 0.6 |
| 2010 | 2.4 | 2.8 | 0.6 | 0.7 |
| 2011 | 2.6 | 3.1 | 0.5 | 0.5 |
| 2012 | 2.6 | 3.1 | 0.7 | 0.5 |
| 2013 | 2.6 | 3.1 | 0.7 | 0.4 |
| 2014 | 2.5 | 3 | 0.7 | 0.7 |
| 2015 | 2.7 | 3.2 | 0.6 | 0.8 |
| 2016 | 2.6 | 3.1 | 0.5 | 0.8 |
nHB: Non-Hispanic Blacks; nHW: Non-Hispanic Blacks; PI: Pacific islanders.
Figure 2.
Age adjusted incident rates of esophageal adenocarcinoma for all ethnicities (1975-2015).
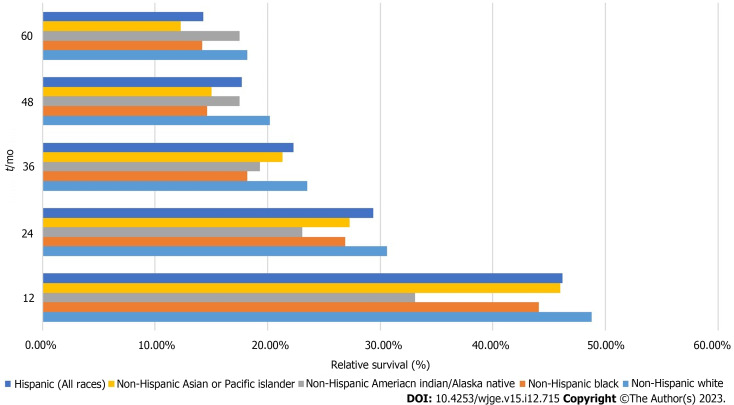
The comparison of relative survival in EAC yields noteworthy results. Minority groups had much worse EAC survival probabilities compared to nHw despite lower incidence rates. Relative survival was 44% in nHB, 46% in Hisp and 48% in nHW after 1 year of diagnosis with the worst 1 year EAC survival probability noted in non-Hispanic American Indians/Alaska Natives (nHAI/AN) at 33%. Five year survival rate was 14% for Hisp and nHB while 18% for nHw with worst 5 year survival probability seen for nHA/PI with relative survival rate of 12% only (Figure 3, Table 3).
Figure 3.
Racial disparities in relative survival after diagnosis of esophageal adenocarcinoma (2007-2016).
Table 3.
Relative survival rates of different ethnic and racial groups for esophageal adenocarcinoma (2007-2016)
|
Mo
|
Non-Hispanic White (%)
|
Non-Hispanic Black (%)
|
Non-Hispanic American Indian/Alaska Native (%)
|
Non-Hispanic Asian or Pacific Islander (%)
|
Hispanic (%)
|
| 12 | 48.80 | 44.10 | 33.10 | 46.00 | 46.20 |
| 24 | 30.60 | 26.90 | 23.10 | 27.30 | 29.40 |
| 36 | 23.50 | 18.20 | 19.30 | 21.30 | 22.30 |
| 48 | 20.20 | 14.60 | 17.50 | 15.00 | 17.70 |
| 60 | 18.20 | 14.20 | 17.50 | 12.30 | 14.30 |
DISCUSSION
EC is a malignancy with dismal survival probabilities. It shows significant racial disparities in incidence and survival rates. Thus, it became important to obtain and assess updated data on EC for analysis to study ongoing EC trends in minority groups.
In phase 1 of our study, we gathered 25 years of (1992-2016) data using the SEER 13 cancer registry and studied trends in both EAC and ESCC in 3 main racial groups in the US. The most prevalent esophageal cancer subtype among Hisp initially was ESCC. Revel et al[12] showed ESCC comprised 59.8% cases compared to 40.8% of EAC among Hisp diagnosed with EC from 2003 to 2008. The significant finding of the current investigation is the shift in incidence of histologic subtypes of esophageal cancer among Hisp. In this group, EAC incidence increased over 25 years from 0.8 to 1.5/100000 while ESCC incidence fell during this interval from 2.2 to 0.8/100000, resulting in EAC as the predominant esophageal cancer in Hisp. Our study is the first to report this change. Recent studies have also reported changing trends of EC subtypes in nHB. Ashktorab et al[13] reported decreased frequency of ESCC as part of overall EC cases from 97% in 1960s to 68% in 2000s while noting an increase in EAC from 2.7% to 31% over the same period. The current study showed age adjusted incidence rate of EAC increased from 0.4 to 0.8/100000 and incidence of ESCC declined from 8.8 to 2.7/100000 in nHB. If current trends continue over the next two decades, it is likely that nHB will join nHW and Hisp in terms of higher EAC incidence compared to ESCC.
In phase 2 of our study, using 40 years (1975-2015) of data from SEER 18 cancer registries, we focused on EAC and investigated ethnic disparities in incidence and survival probabilities. The overall age-adjusted incidence rate of EAC increased progressively between 1975 to 2007. Similar trends were reported by Heitmiller et al[14] using the data from Johns Hopkins tumor registry and by Daly et al[15] using the National Cancer Database. The etiology of the changing trend remains to be elucidated, but it is noteworthy that it is accompanied by a parallel rise in the incidence of cancer of gastroesophageal junction, the precursor of which is Barrett's esophagus and metaplastic changes induced by reflux disease[16,17]. After 2007, the incidence rate of EAC seems to plateau in nHw and while increasing slowly in all minority groups. There is limited literature for EAC incidence and ethnic disparities after 2007. In a study using the United States Cancer Statistics database, Patel et al[18] showed recent trends in EAC which were similar to our findings. Similar to multiple prior studies, our study again showed that EAC incidence remains higher in nHW compared to other minority ethnic groups (2016; nHW = 2.6/100000, nHB = 0.5/100000, others = 0.8/100000)[8,19-22].
Gastroesophageal reflux disease (GERD) and obesity are major risk factors for EAC, amongst others[4,23]. A recent systematic review by El-Serag showed increasing prevalence of GERD worldwide, and the same is true for the trends of obesity[24,25]. GERD poses a directly proportional risk for EAC which explains increasing incidence trend of EAC in our study[26]. Bersentes and colleagues showed comparable trends of prevalence of Barrett's esophagus between nHw and Hisp which may explain increasing incidence of EAC in Hisp observed in the current investigation[27]. Genetic factors can also potentially explain the change in incidence trends observed in our study. Genome-wide association studies have identified various susceptibility loci for EAC that demonstrate familial clustering, leading to a shift in ethnic trends in incidence and prevalence of EAC[4,28,29].
Although ethnic disparities in survival have been reported previously for EC, only one study has been performed previously to evaluate disparities specifically for EAC. In addition, very limited research has been performed to evaluate survival probabilities for minority ethnic groups like Hisp, nHAI/AN, nHA/PI. Greenstein et al[30] showed higher mortality rates among nHB when compared to nHw after EC diagnosis. Multiple investigators also showed similar trends and confirmed that nHB, Hisp and other minority groups show greater mortality and poor survival than nHw[12,31,32]. Adams et al[19] showed ethnicity is not an independent risk factor for EC in their population-based analysis of EC cases. In contrast, Laszkowska et al[33] suggested mortality was higher in EAC in nHW than nHB, Hisp and nHA/PI. However, this study used incidence-based mortality assessment for statistical analysis which lacks information about disease onset. In the present study, the latest data over a decade was evaluated to investigate survival probabilities in different racial groups at 1, 2, 3, 4, and 5 years after diagnosis. The results showed nHw with decreased mortality rates compared to all minority groups at 1 and 5 years. Prior studies investigating poor EC survival have pointed out that advanced stage malignancy at presentation and underutilized cancer-directed surgical therapy in potentially resectable tumors results in poor survival in minority groups[12,31,34]. Socioeconomic factors, cultural beliefs, and language barriers in minority groups may also be other potential contributory factors to survival disparities. Moreover, the rapidly accumulating amount of genetic and transcriptomic date will hopefully allow for improved stratification resulting in optimal therapy and prognosis based on molecular subtype[35].
This investigation has limitations that require comment. First, the presence or absence of Barrett’s esophagus was not reported. Second, other known clinical risk factors such as smoking, alcohol use, obesity or ongoing reflux disease was not assessed because information on these items is not available in the SEER database. Furthermore, errors may be present in the database due to misclassification of patient race/ethnicity information.
Conversely, there are strengths to the current study. The sample size allows for improved understanding of trends in incidence and survival of EC subtypes in different races. In addition, demonstration of opposing ethnic trends in different histologic types of esophageal cancer in the same population confers internal validity to the study results.
CONCLUSION
In summary, Hisp have joined nHw as US ethnic groups with EAC as the predominant esophageal cancer. Furthermore, nHB have the highest APC in EAC incidence among the 3 main US racial groups. Regrettably, all US minority groups with EAC have lower survival than nHw despite a decreased incidence of this cancer compared to nHw. Understanding EAC in Hisp may provide insight regarding changes in EAC incidence among US minority groups. In addition, evaluation of potential factors contributing to worse short and long-term survival for US minority EAC patients is warranted.
ARTICLE HIGHLIGHTS
Research background
Esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC) frequency have changed and are continuing to change in the United States (US).
Research motivation
To determine EAC/ESCC incidence among the 3 main US racial groups and investigate US EAC survival by ethnicity.
Research objectives
To investigate time trends in EAC/ESCC incidence among the 3 main US racial groups and investigate trends in US EAC survival by ethnicity.
Research methods
Analysis of 25 years (1992-2016) SEER 13 data to compare incidence trends in EAC and ESCC between non-Hispanic whites (nHW), non-Hispanic Blacks (nHB) and Hispanics (Hisp). In addition, SEER 18 data, from 1975-2015, on EAC in the US was analyzed to evaluate racial disparities in incidence and survival among nHW, nHB and Hisp.
Research results
In Hisp, the EAC incidence rate increased while ESCC decreased from 1992 to 2016, resulting in EAC as the predominant esophageal cancer subtype in this group since 2011, joining nHW. Furthermore, although ESCC remains the predominant tumor in nHB, the difference between ESCC and EAC has narrowed dramatically over 25 years. EAC survival probabilities were worse in all minority groups compared to nHw.
Research conclusions
Hisp are the 2nd US ethnic group to have EAC as their predominant EC cancer type. Of note, EAC incidence in nHB is increasing at the highest rate nationally. Despite lower EAC incidence in all minority groups compared to nHW, these populations have decreased survival compared to nHW.
Research perspectives
Understanding EAC in Hisp may provide insight regarding changes in EAC incidence among US minority groups. In addition, evaluation of potential factors contributing to worse short and long-term survival for US minority EAC patients is warranted.
Footnotes
Institutional review board statement: Studies using SEER database are considered exempt by the Institutional Review Board of Augusta University-Medical College of Georgia.
Informed consent statement: This study utilized SEER cancer incidence and mortality data from population-based cancer registries covering approximately 47.9 percent of the U.S. population which did not require a specific informed consent.
Conflict-of-interest statement: All the authors have no relevant financial or non-financial interests to disclose.
STROBE statement: The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Gastroenterological Association; American College of Gastroenterology; American Society for Gastrointestinal Endoscopy.
Peer-review started: September 5, 2023
First decision: September 29, 2023
Article in press: November 13, 2023
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He X, China S-Editor: Liu JH L-Editor: A P-Editor: Cai YX
Contributor Information
Hafiz Muhammad Sharjeel Arshad, Division of Gastroenterology & Hepatology, Augusta University - Medical College of Georgia, Augusta, GA 30912, United States.
Umer Farooq, Department of Internal Medicine, Loyola Medicine/MacNeil Hospital, Berwyn, IL 60402, United States.
Ayesha Cheema, Division of Gastroenterology & Hepatology, Augusta University - Medical College of Georgia, Augusta, GA 30912, United States.
Ayesha Arshad, Department of Medicine, Fatima Memorial Medical College, Lahore 54000, Punjab, Pakistan.
Muaaz Masood, Department of Medicine, Augusta University - Medical College of Georgia, Augusta, GA 30912, United States.
Kenneth J Vega, Division of Gastroenterology & Hepatology, Augusta University - Medical College of Georgia, Augusta, GA 30912, United States. kvega@augusta.edu.
Data sharing statement
No additional data are available.
References
- 1.Xie Y, Shi L, He X, Luo Y. Gastrointestinal cancers in China, the USA, and Europe. Gastroenterol Rep (Oxf) 2021;9:91–104. doi: 10.1093/gastro/goab010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Rustgi AK, El-Serag HB. Esophageal carcinoma. N Engl J Med. 2014;371:2499–2509. doi: 10.1056/NEJMra1314530. [DOI] [PubMed] [Google Scholar]
- 4.Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, Bonaventure A, Valkov M, Johnson CJ, Estève J, Ogunbiyi OJ, Azevedo E Silva G, Chen WQ, Eser S, Engholm G, Stiller CA, Monnereau A, Woods RR, Visser O, Lim GH, Aitken J, Weir HK, Coleman MP CONCORD Working Group. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnold M, Rutherford MJ, Bardot A, Ferlay J, Andersson TM, Myklebust TÅ, Tervonen H, Thursfield V, Ransom D, Shack L, Woods RR, Turner D, Leonfellner S, Ryan S, Saint-Jacques N, De P, McClure C, Ramanakumar AV, Stuart-Panko H, Engholm G, Walsh PM, Jackson C, Vernon S, Morgan E, Gavin A, Morrison DS, Huws DW, Porter G, Butler J, Bryant H, Currow DC, Hiom S, Parkin DM, Sasieni P, Lambert PC, Møller B, Soerjomataram I, Bray F. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995-2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol. 2019;20:1493–1505. doi: 10.1016/S1470-2045(19)30456-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vizcaino AP, Moreno V, Lambert R, Parkin DM. Time trends incidence of both major histologic types of esophageal carcinomas in selected countries, 1973-1995. Int J Cancer. 2002;99:860–868. doi: 10.1002/ijc.10427. [DOI] [PubMed] [Google Scholar]
- 7.Brown LM, Devesa SS. Epidemiologic trends in esophageal and gastric cancer in the United States. Surg Oncol Clin N Am. 2002;11:235–256. doi: 10.1016/s1055-3207(02)00002-9. [DOI] [PubMed] [Google Scholar]
- 8.Baquet CR, Commiskey P, Mack K, Meltzer S, Mishra SI. Esophageal cancer epidemiology in blacks and whites: racial and gender disparities in incidence, mortality, survival rates and histology. J Natl Med Assoc. 2005;97:1471–1478. [PMC free article] [PubMed] [Google Scholar]
- 9.Erkizan HV, Johnson K, Ghimbovschi S, Karkera D, Trachiotis G, Adib H, Hoffman EP, Wadleigh RG. African-American esophageal squamous cell carcinoma expression profile reveals dysregulation of stress response and detox networks. BMC Cancer. 2017;17:426. doi: 10.1186/s12885-017-3423-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.United States Census Bureau. Quick Facts. 2019 [January 8, 2021]; Available from: https://www.census.gov/quickfacts/fact/table/US/RHI725219 .
- 11.Ricardo J, Conte J, Alkayali T, Salem A, Huston J, Shridhar R, Meredith KL. Esophageal cancer in Hispanic patients: A demographic analysis of the National Cancer Database. J Clin Oncol. 2019;37(15_suppl):6561–6561. [Google Scholar]
- 12.Revels SL, Morris AM, Reddy RM, Akateh C, Wong SL. Racial disparities in esophageal cancer outcomes. Ann Surg Oncol. 2013;20:1136–1141. doi: 10.1245/s10434-012-2807-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ashktorab H, Nouri Z, Nouraie M, Razjouyan H, Lee EE, Dowlati E, El-Seyed el-W, Laiyemo A, Brim H, Smoot DT. Esophageal carcinoma in African Americans: a five-decade experience. Dig Dis Sci. 2011;56:3577–3582. doi: 10.1007/s10620-011-1853-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heitmiller RF, Sharma RR. Comparison of prevalence and resection rates in patients with esophageal squamous cell carcinoma and adenocarcinoma. J Thorac Cardiovasc Surg. 1996;112:130–136. doi: 10.1016/s0022-5223(96)70187-3. [DOI] [PubMed] [Google Scholar]
- 15.Daly JM, Karnell LH, Menck HR. National Cancer Data Base report on esophageal carcinoma. Cancer. 1996;78:1820–1828. doi: 10.1002/(sici)1097-0142(19961015)78:8<1820::aid-cncr25>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 16.Pera M, Cameron AJ, Trastek VF, Carpenter HA, Zinsmeister AR. Increasing incidence of adenocarcinoma of the esophagus and esophagogastric junction. Gastroenterology. 1993;104:510–513. doi: 10.1016/0016-5085(93)90420-h. [DOI] [PubMed] [Google Scholar]
- 17.Blot WJ, Devesa SS, Kneller RW, Fraumeni JF Jr. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991;265:1287–1289. [PubMed] [Google Scholar]
- 18.Patel N, Benipal B. Incidence of Esophageal Cancer in the United States from 2001-2015: A United States Cancer Statistics Analysis of 50 States. Cureus. 2018;10:e3709. doi: 10.7759/cureus.3709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adams MA, Prenovost KM, Dominitz JA, Holleman RG, Kerr EA, Krein SL, Saini SD, Rubenstein JH. Predictors of Use of Monitored Anesthesia Care for Outpatient Gastrointestinal Endoscopy in a Capitated Payment System. Gastroenterology. 2017;153:1496–1503.e1. doi: 10.1053/j.gastro.2017.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pickens A, Orringer MB. Geographical distribution and racial disparity in esophageal cancer. Ann Thorac Surg. 2003;76:S1367–S1369. doi: 10.1016/s0003-4975(03)01202-5. [DOI] [PubMed] [Google Scholar]
- 21.Mathieu LN, Kanarek NF, Tsai HL, Rudin CM, Brock MV. Age and sex differences in the incidence of esophageal adenocarcinoma: results from the Surveillance, Epidemiology, and End Results (SEER) Registry (1973-2008) Dis Esophagus. 2014;27:757–763. doi: 10.1111/dote.12147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.González L, Magno P, Ortiz AP, Ortiz-Ortiz K, Hess K, Nogueras-González GM, Suárez E. Esophageal cancer incidence rates by histological type and overall: Puerto Rico versus the United States Surveillance, Epidemiology, and End Results population, 1992-2005. Cancer Epidemiol. 2013;37:5–10. doi: 10.1016/j.canep.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lagergren J, Lagergren P. Recent developments in esophageal adenocarcinoma. CA Cancer J Clin. 2013;63:232–248. doi: 10.3322/caac.21185. [DOI] [PubMed] [Google Scholar]
- 24.El-Serag HB. Time trends of gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol. 2007;5:17–26. doi: 10.1016/j.cgh.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 25.Romero CX, Romero TE, Shlay JC, Ogden LG, Dabelea D. Changing trends in the prevalence and disparities of obesity and other cardiovascular disease risk factors in three racial/ethnic groups of USA adults. Adv Prev Med. 2012;2012:172423. doi: 10.1155/2012/172423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubenstein JH, Taylor JB. Meta-analysis: the association of oesophageal adenocarcinoma with symptoms of gastro-oesophageal reflux. Aliment Pharmacol Ther. 2010;32:1222–1227. doi: 10.1111/j.1365-2036.2010.04471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bersentes K, Fass R, Padda S, Johnson C, Sampliner RE. Prevalence of Barrett's esophagus in Hispanics is similar to Caucasians. Dig Dis Sci. 1998;43:1038–1041. doi: 10.1023/a:1018834902694. [DOI] [PubMed] [Google Scholar]
- 28.Orloff M, Peterson C, He X, Ganapathi S, Heald B, Yang YR, Bebek G, Romigh T, Song JH, Wu W, David S, Cheng Y, Meltzer SJ, Eng C. Germline mutations in MSR1, ASCC1, and CTHRC1 in patients with Barrett esophagus and esophageal adenocarcinoma. JAMA. 2011;306:410–419. doi: 10.1001/jama.2011.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levine DM, Ek WE, Zhang R, Liu X, Onstad L, Sather C, Lao-Sirieix P, Gammon MD, Corley DA, Shaheen NJ, Bird NC, Hardie LJ, Murray LJ, Reid BJ, Chow WH, Risch HA, Nyrén O, Ye W, Liu G, Romero Y, Bernstein L, Wu AH, Casson AG, Chanock SJ, Harrington P, Caldas I, Debiram-Beecham I, Caldas C, Hayward NK, Pharoah PD, Fitzgerald RC, Macgregor S, Whiteman DC, Vaughan TL. A genome-wide association study identifies new susceptibility loci for esophageal adenocarcinoma and Barrett's esophagus. Nat Genet. 2013;45:1487–1493. doi: 10.1038/ng.2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greenstein AJ, Litle VR, Swanson SJ, Divino CM, Packer S, McGinn TG, Wisnivesky JP. Racial disparities in esophageal cancer treatment and outcomes. Ann Surg Oncol. 2008;15:881–888. doi: 10.1245/s10434-007-9664-5. [DOI] [PubMed] [Google Scholar]
- 31.Gupta DR, Liu Y, Jiang R, Walid S, Higgins K, Landry J, McDonald M, Willingham FF, El-Rayes BF, Saba NF. Racial Disparities, Outcomes, and Surgical Utilization among Hispanics with Esophageal Cancer: A Surveillance, Epidemiology, and End Results Program Database Analysis. Oncology. 2019;97:49–58. doi: 10.1159/000499716. [DOI] [PubMed] [Google Scholar]
- 32.Taioli E, Wolf AS, Camacho-Rivera M, Kaufman A, Lee DS, Bhora F, Flores RM. Racial disparities in esophageal cancer survival after surgery. J Surg Oncol. 2016;113:659–664. doi: 10.1002/jso.24203. [DOI] [PubMed] [Google Scholar]
- 33.Laszkowska M, Tramontano AC, Kim J, Camargo MC, Neugut AI, Abrams JA, Hur C. Racial and ethnic disparities in mortality from gastric and esophageal adenocarcinoma. Cancer Med. 2020;9:5678–5686. doi: 10.1002/cam4.3063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Then EO, Lopez M, Saleem S, Gayam V, Sunkara T, Culliford A, Gaduputi V. Esophageal Cancer: An Updated Surveillance Epidemiology and End Results Database Analysis. World J Oncol. 2020;11:55–64. doi: 10.14740/wjon1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lavery A, Turkington RC. Transcriptomic biomarkers for predicting response to neoadjuvant treatment in oesophageal cancer. Gastroenterol Rep (Oxf) 2020;8:411–424. doi: 10.1093/gastro/goaa065. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.