Abstract
Background
Malnutrition is a common geriatric syndrome and can be targeted preoperatively to decrease the risk of postoperative delirium (POD) in older adult patients. To analyze the value of the prognostic nutritional index (PNI) to predict the incidence of POD in older adult patients with hip fractures.
Methods
This was a prospective, observational, cohort study of older adult patients with hip fractures. Preoperative PNI was calculated as 10 × serum albumin (g/dL) + 0.005 × total lymphocyte count (/μL) using preoperative laboratory results. Patients were divided into POD and non-POD groups using the Confusion Assessment Method (CAM). The risk factors associated with POD as well as the relationship between PNI values and the incidence of POD were analyzed using univariate and multivariate logistic regression analyses. The predictive value of PNI for POD was assessed using receiver operating characteristic curve analysis.
Results
In this cohort of 369 patients who underwent hip fracture surgery, 67 patients (18.2%) were diagnosed with POD by the CAM results. Low PNI increased the risk of POD (odds ratio (OR) = 0.928, 95% confidence interval (CI): 0.864–0.997). General anesthesia (OR = 2.307, 95% CI: 1.279–4.162) and Mini-Mental State Examination (MMSE) score (OR = 0.956, 95% CI: 0.920–0.994) were also identified as risk factors for POD. Receiver operating characteristic curve analysis suggested that PNI combined with the anesthetic method and MMSE score may be used as a potential predictive indicator of POD after hip fracture surgery.
Conclusion
Preoperative PNI value is related to POD in older adult patients with hip fractures.
Trial registration
This secondary analysis study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (approval No. M2022578) and registered in the Chinese Clinical Trial Registry (ChiCTR2300070569).
Keywords: Nutritional status, Prognostic nutritional index, Postoperative delirium, Hip fracture, Older adult patients
Background
Postoperative delirium (POD) is an acute neuropsychiatric syndrome characterized by inattention, fluctuating levels of consciousness, and/or disorganized thinking, which is associated with increased morbidity, mortality, and health care costs [1, 2]. As anesthetic and surgical care continues to improve, a significantly greater number of older adult patients are undergoing elective surgical procedures. However, these procedures are associated with an increased POD risk perioperatively. It is of great importance to perform interventions for older adult patients preoperatively to optimize perioperative management and prevent POD.
Age, malnutrition, perioperative low albumin, pre- and postoperative pain, blood transfusions, and intraoperative hypotension are risk factors for POD [3, 4]. Malnutrition is a common geriatric syndrome and can be recognized and targeted preoperatively to decrease the risk of POD in older adult patients. The presence of malnutrition is determined using a series of scales, namely, the Mini-Nutritional Assessment, Mini-Nutritional Assessment Short Form, Nutrition Risk Screening 2002, and several laboratory parameters [5]. However, assessment scales have limitations. For example, completing questionnaires may be time-consuming and complex for older adult patients, and subjective errors are inevitable. Instead, laboratory parameters, such as serum albumin and total lymphocyte count, which reflect a patient’s nutritional status prior to surgery, are more objective than assessment scales, and the results are easier to obtain in surgical patients [6–9].
Recently, the prognostic nutritional index (PNI) has been popularized, which is calculated as 10 × serum albumin (g/dL) + 0.005 × total lymphocyte count (/μL). Low PNI is a significant risk factor for POD in older adult patients with colorectal cancer and patients who undergo adult spinal deformity surgeries [10, 11]. Unfortunately, few studies have evaluated the association between preoperative nutritional status and the incidence of POD in older adult patients with hip fractures who undergo surgical repair. These patients are more susceptible to preoperative malnutrition and POD compared with other patient groups [12]. However, the effectiveness of PNI as a dependable predictive index for POD must be verified.
In the present study, we hypothesized that in older adult patients who undergo surgical repair for hip fractures, low PNI is associated with the incidence of POD. The study aimed to prove that preoperative nutritional status can be objectively and easily predicted to identify patients susceptible to POD.
Methods
This was a secondary analysis based on two prospective, observational, single-center, cohort studies performed in the Geriatric Orthopedics Unit of Beijing Jishuitan Hospital from June 2020 to March 2022. The primary objective of the study was to explore the association between PNI and the incidence of POD in older adult patients with hip fractures. Accordingly, we analyzed PNI as a predictive factor of POD in older adult patients who underwent surgical repair for hip fractures. This study aimed to identify patients at high risk of developing POD using PNI, and to administer preoperative nutritional support as early as possible, to prevent POD.
Ethics approval and clinical registration
This secondary analysis study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (approval No. M2022578) and registered in the Chinese Clinical Trial Registry (ChiCTR2300070569). The original two prospective, observational, single-center, cohort studies were approved by the Medical Science Research Ethics Committees of Beijing Jishuitan Hospital (JLKS201901-04, JLKS202009-10, respectively) and registered in the Chinese Clinical Trial Registry (ChiCTR1900027393, ChiCTR2000038924, respectively). All patients provided informed consent for the collection and analysis of their clinical data and serum samples.
Patients
This study was a secondary analysis performed at Beijing Jishuitan Hospital between 1 June 2020 and 30 March 2022. According to the previous study [13], the inclusion criteria were: age ≥ 65 years, hospital admission for surgical treatment of hip fracture, and American Society of Anesthesiologists physical status classification I–III. The exclusion criteria were: central nervous system disorders already existed preoperatively or with a previous history of such diseases, including preoperative delirium, Parkinson’s disease, dementia (including dementia due to Parkinson’s disease, Alzheimer’s disease, and Lewy body dementia), stroke within the previous 6 months or other central nervous system disorders; other factors that might affect the incidence of POD including multiple traumas and transfer to the intensive care unit postoperatively; communication difficulties and severe hearing or vision impairment which were unable to finish assessment scales, and unwillingness to participate in the study or unexpected discharge.
Perioperative clinical assessment
Nutritional status was assessed via PNI, which was calculated as 10 × serum albumin (g/dL) + 0.005 × total lymphocyte count (/μL). Serum albumin and total lymphocyte count were obtained from preoperative laboratory results.
All participants were interviewed the day before surgery, and the following baseline data were collected: demographic information, laboratory results, American Society of Anesthesiologists physical status, age-adjusted Charlson comorbidity index [14], Mini-Mental State Examination (MMSE) [15], education level, and Activities of Daily Living [16]. Pain intensity was assessed using a numerical rating scale [17]. Other information namely comorbidities, medical history, and fracture classification was collected from the patients’ medical records. The laboratory results were collected from the preoperative examinations processed 2 ~ 5 days before surgery. History collection and physical evaluation were performed by trained investigators.
Diagnosis of POD
The Confusion Assessment Method (CAM) was used to exclude patients with preoperative delirium and to diagnose POD, as previously described [13, 18]. Four items (acute onset and fluctuating course, inattention, disorganized thinking, altered level of consciousness) constitute the CAM. When diagnosing delirium, it is important to obtain information from a reliable source about the patient's acute onset and fluctuating course. Inattention may be indicated by difficulty focusing attention, while disorganized thinking may be shown by incoherent thoughts. The patient's level of consciousness may be altered, categorized as consciousness, vigilant, lethargic, stupor, or coma. To diagnose delirium using the CAM method, the first two items must be present along with either of the last two items. All participants were followed for the first 2 postoperative days, a period in which POD is usually diagnosed after hip fracture surgery in older adult patients. Cognitive assessment was performed through twice-daily visits and by a fixed geriatric-care physician.
Anesthesia and analgesia
No sedatives and/or anticholinergic drugs were administered to any patients as adjuvant medications before anesthesia. The anesthesia method (general anesthesia or spinal anesthesia) was determined by anesthesiologists in communication with the patients. After entering the operation room, patients received inhalational mask oxygen at 6 L/min. Heart rate, electrocardiography, and pulse oximetry were monitored. Radial artery catheterization was performed to directly measure mean arterial pressure and for blood gas analysis. All patients received an ultrasound-guided iliac fascia block and were given 30 mL of 0.33% ropivacaine for regional anesthesia and postoperative analgesia. Patients who received spinal anesthesia underwent single-dose subarachnoid spinal anesthesia as an injection of 8–10 mg of 0.3% ropivacaine at the L2–3 or L3–4 levels, and the anesthesia plane reached T10. Patients who received general anesthesia underwent intravenous induction with propofol and fentanyl. Rocuronium or cisatracurium was administered intravenously when the patient lost consciousness. Endotracheal intubation or laryngeal mask placement was performed 2 min later. Sevoflurane, remifentanil, rocuronium, or cisatracurium were used for anesthetic maintenance. The end-tidal partial pressure of carbon dioxide and bispectral index value were monitored intraoperatively in patients who underwent general anesthesia. During the operation, mean arterial pressure and heart rate were maintained within 20% of the baseline values, partial pressure end-tidal carbon dioxide was maintained at 30–35 mmHg, and the bispectral index value was maintained at 40–60 for patients who underwent general anesthesia.
For postoperative analgesia, all patients received intravenous patient-controlled analgesia with 1.5 μg/kg fentanyl, 200 mg flurbiprofen axetil, and 10 mg tropisetron hydrochloride in 100 ml saline in addition to the preoperative iliac fascia block.
Sample size calculation
An observational study conducted in China showed that patients with POD had a PNI of 39.4 ± 10.2, whereas those without POD had a PNI of 47.4 ± 11.7 [19]. Based on the calculated PNI mean, the study estimated that both the POD and non-POD groups needed to recruit 29 effective cases to achieve an 80% power at an α value of 0.05. To control for confounding factors such as age, hip fracture type, ASA classification, duration of surgery, intraoperative bleeding, etc., it was proposed to use logistic regression analysis. With an Events Per Variable equal to 5, 25 patients would be required in the POD group. As the incidence of POD in our previous study was 18.9%, the total sample size needed for the study was calculated to be 132 participants. To account for a potential dropout rate of 10%, the study aimed to recruit 147 participants.
Statistical analysis
The Kolmogorov–Smirnov test was used to analyze the distribution of quantitative variables. Measurement data that followed a normal distribution were presented as mean ± standard deviation, and the independent sample’s t-test was used for analysis. Measurement data that did not follow a normal distribution were expressed as median (minimum, maximum), and the rank sum test was used for analysis. The chi-square test was used to analyze the enumeration data. The patients were divided into a POD group and a non-POD group based on the CAM results. Univariate analysis was used to screen for differences in POD-associated factors between the groups, and binary logistic regression was used to identify the risk factors for POD. The areas under the receiver operating characteristic curve (AUCs) of the risk factors were then calculated. All data were statistically analyzed using SPSS 25.0 (IBM Corp., Armonk, NY, USA), and P < 0.05 was considered statistically significant.
Results
Baseline characteristics
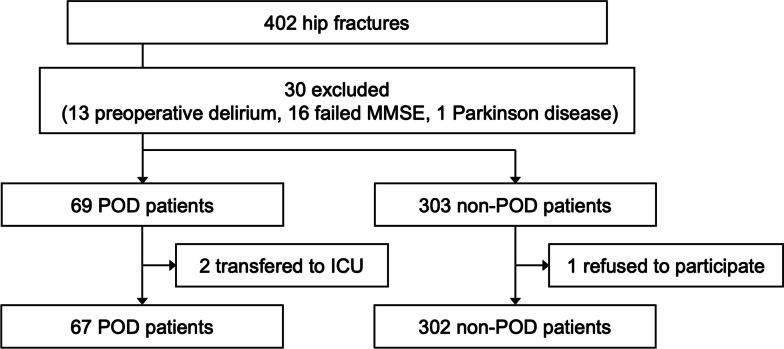
A total of 369 older adult patients with hip fractures were included in this study. Of these, 67 patients were diagnosed with POD on the basis of the CAM results (Fig. 1). Overall baseline and clinical characteristics and the majority of the intraoperative characteristics were well-balanced between the POD and non-POD groups except for the comorbidity of hypertension, MMSE score, and anesthesia method (Table 1). Specifically, hypertension, low MMSE, and general anesthesia were risk factors for POD (p < 0.05).
Fig. 1.
Flowchart of the research design. A total of 369 older adult patients with hip fractures were included in this study. MMSE, Mini-Mental State Examination; POD, postoperative delirium; ICU, intensive care unit
Table 1.
Comparison of baseline characteristics and other covariables between patients with and without postoperative delirium
| Non-POD (n = 302) | POD (n = 67) | p-value | Standardized difference | |
|---|---|---|---|---|
| Sex, male | 221 (73.2%) | 44 (65.7%) | 0.217 | 0.158 |
| Age, yr | 78.54 ± 6.78 | 79.85 ± 7.32 | 0.16 | 0.179 |
| Weight, kg | 61.27 ± 11.09 | 61.69 ± 10.92 | 0.782 | 0.038 |
| BMI, kg/m2 | 23.45 ± 3.62 | 23.79 ± 3.61 | 0.485 | 0.095 |
| ASA physical status class | 0.595 | 0.096 | ||
| I | 5 (1.66%) | 0 (0%) | ||
| II | 194 (64.24%) | 41 (61.19%) | ||
| III | 103 (34.11%) | 26 (38.81%) | ||
| ACCI | 3 (2,4) | 4 (2.2,4) | 0.116 | 0.230 |
| Hypertension | 179 (59.3%) | 49 (73.1%) | 0.035 | 0.313 |
| Diabetes | 85 (28.1%) | 25 (37.3%) | 0.138 | 0.190 |
| Ischemic heart disease | 71 (23.5%) | 18 (26.9%) | 0.561 | 0.076 |
| Stroke | 65 (21.5%) | 11 (16.4%) | 0.35 | 0.138 |
| Chronic obstructive pulmonary disease | 33 (11.0%) | 7 (10.4%) | 0.902 | 0.017 |
| Smoking status, yes | 59 (19.5%) | 16 (23.9%) | 0.424 | 0.102 |
| Alcohol abuse, yes | 27 (8.9%) | 10 (14.9%) | 0.140 | 0.168 |
| ADL, points | 14 (14,15) | 14 (14,16) | 0.122 | 0.236 |
| Education, yr | 9 (4,12) | 9 (6,12) | 0.683 | 0.054 |
| MMSE, points | 26 (22,28) | 24 (18,27.5) | 0.009 | 0.327 |
| Anesthesia method | 0.004 | 0.390 | ||
| Spinal anesthesia | 189 (62.6%) | 29 (43.3%) | ||
| General anesthesia | 113 (37.4%) | 38 (56.7%) | ||
| Duration of anesthesia, min | 90 (70,110) | 90 (75,100) | 0.886 | 0.109 |
| Duration of surgery, min | 60 (40,80) | 60 (30,75) | 0.387 | 0.243 |
| Time from injury to surgery, hours | 96 (70,124.6) | 81.8 (63.8,144.9) | 0.492 | 0.143 |
| Type of fracture | 0.641 | 0.008 | ||
| Intertrochanteric | 152 (50.3%) | 34 (50.7%) | ||
| Femoral neck | 148 (49%) | 32 (47.8%) | ||
| Subtrochanteric | 2 (0.7%) | 1 (1.5%) | ||
| Hospital stay, days | 4 (3,5) | 5 (3,5) | 0.621 | 0.093 |
Categorical variables are expressed as n (%). Data with a normal distribution are presented as mean ± standard deviation, whereas non-normally distributed data are presented as median (25th percentile, 75th percentile). POD postoperative delirium, BMI body mass index, ASA American Society of Anesthesiologists, ACCI age-adjusted Charlson comorbidity index, ADL activities of daily living, MMSE mini-mental state examination
Preoperative nutritional status and laboratory results
Patients with low PNI, low serum albumin, and low thyroid stimulating hormone concentrations, were more likely to be diagnosed with POD compared with those without POD. Since the distribution of the PNI data is non-normal, we pre-suppose the median PNI of 45.6 as the cut-off value. We then divided PNI into low and high PNI by the cut-off value of 45.6, and we found that PNI < 45.6 could be used as a predictive factor for the incidence of POD. In contrast, lymphocyte count and other laboratory results showed no significant differences between POD and non-POD patients (Table 2).
Table 2.
Comparison of nutritional and laboratory results between patients with and without postoperative delirium
| Non-POD (n = 302) | POD (n = 67) | p-value | |
|---|---|---|---|
| PNI | 46.8 (44.2,49.3) | 45.6 (43.5,47.8) | 0.019 |
| PNI | 0.039 | ||
| < 45.6 | 122 (41.36%) | 37 (55.22%) | |
| ≥ 45.6 | 173 (58.64%) | 30 (44.78%) | |
| Albumin, g/L | 41.3 (39.2,43.2) | 40.6 (38.6,41.8) | 0.028 |
| Lymphocyte, × 109/L | 1.1 (0.8,1.4) | 1.1 (0.8,1.5) | 0.619 |
| Leukocyte, × 109/L | 9.7 (7.9,11.7) | 9.6 (8.1,11.5) | 0.827 |
| Erythrocyte, × 1012/L | 4 (3.6,4.3) | 3.9 (3.6,4.2) | 0.827 |
| Hemoglobin, g/L | 121 (110,130) | 119.5 (107,127.5) | 0.361 |
| Platelet, × 109/L | 198.5 (161.2,238.8) | 205 (174,257) | 0.246 |
| Sodium, mmol/L | 138 (136,140) | 138 (136.2,140) | 0.831 |
| Chlorine, mmol/L | 103 (100,105.2) | 102 (99.2,105) | 0.12 |
| Potassium, mmol/L | 3.9 (3.7,4.2) | 3.9 (3.6,4.2) | 0.496 |
| Calcium, mmol/L | 2.2 (2.1,2.3) | 2.2 (2.1,2.3) | 0.22 |
| ALT, IU/L | 14 (11,17) | 12 (10,16) | 0.063 |
| AST, IU/L | 18 (16,22) | 18 (15,22) | 0.425 |
| Urea, mmol/L | 6.5 (5.3,8.3) | 7.4 (5.7,9.4) | 0.061 |
| Creatine, μmol/L | 57 (47.8,70) | 59.5 (52.2,75.8) | 0.107 |
| Total protein, g/L | 65.9 (62,70.6) | 65.7 (62,68.2) | 0.386 |
| Glucose, mmol/L | 7.7 (6.6,10.1) | 7.7 (6.6,9) | 0.448 |
| Glycosylated hemoglobin, % | 5.8 (5.4,6.4) | 6 (5.5,6.6) | 0.239 |
| PaCO2, mmHg | 32.5 (29.4,36.1) | 32.2 (29.5,34.6) | 0.774 |
| PaO2, mmHg | 73.7 (66.8,81.4) | 72.3 (66.9,78.9) | 0.252 |
| Lactic acid, mmol/L | 1.1 (0.8,1.6) | 0.9 (0.7,1.4) | 0.472 |
| C-reactive protein, mg/L | 18 (4.6,58.1) | 39.6 (6.9,65.6) | 0.219 |
| Thyroid stimulating hormone, mIU/L | 1.8 (1,3.2) | 1.3 (0.7,1.9) | 0.003 |
| Total tetraiodothyroxine, ng/ml | 97.4 (83.4,112.9) | 100.2 (86.4,113.6) | 0.329 |
| Total triiodothyroxine, ng/ml | 1.2 (1.1,1.6) | 1.3 (1.1,1.6) | 0.939 |
| Free tetraiodothyroxine, ng/ml | 16.5 (14.4,18.7) | 16.1 (14.4,18.8) | 0.914 |
| Free triiodothyroxine, ng/ml | 3.3 (2.9,3.8) | 3.1 (2.7,3.5) | 0.054 |
Non-normally distributed data are presented as median (25th percentile, 75th percentile). POD postoperative delirium, PNI prognostic nutritional index, ALT alanine aminotransferase, AST aspartate aminotransferase, PaCO2 partial pressure of arterial carbon dioxide, PaO2 partial pressure of arterial oxygen
Multiple logistic regression of the predisposing factors for POD
After adjusting for confounders, binary logistic regression showed that the significant preoperative risk factors for POD after hip fracture surgery were PNI [adjusted odds ratio (OR) = 0.928, 95% confidence interval (CI): (0.864, 0.997)], general anesthesia [(adjusted OR = 2.307, 95% CI: (1.279, 4.162)), and MMSE score [adjusted OR = 0.956, 95% CI: (0.920, 0.994)] (Table 3).
Table 3.
Multiple logistic regression analysis of the predisposing factors for postoperative delirium
| Adjusted OR | 95% CI | p-value | |
|---|---|---|---|
| PNI | 0.928 | (0.864, 0.997) | 0.040 |
| Anesthesia method | 2.307 | (1.279, 4.162) | 0.005 |
| MMSE | 0.956 | (0.920, 0.994) | 0.022 |
| Hypertension | 1.709 | (0.902, 3.237) | 0.100 |
| Thyroid stimulating hormone, mIU/L | 0.944 | (0.842, 1.058) | 0.323 |
OR odds ratio, CI confidence interval, PNI prognostic nutritional index, MMSE mini-mental state examination.
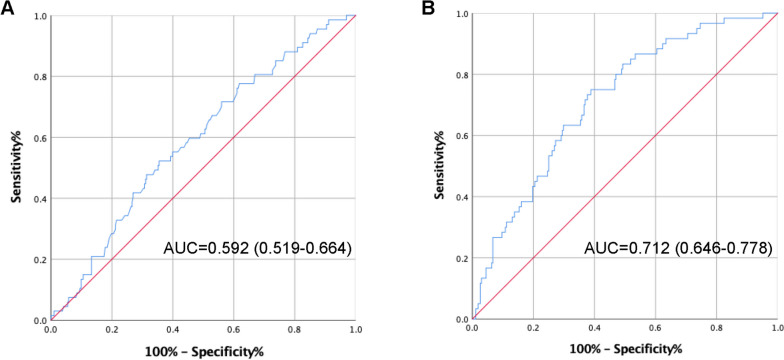
Evaluation of PNI as a potential prognostic marker for POD
The risk factors associated with POD shown in Table 3 were examined by receiver operating characteristic curve (ROC) analyses, and the AUC value for PNI was 0.592 [95% CI: (0.519, 0.664), sensitivity = 52.2%, specificity = 64.5%] (Fig. 2A). According to Youden index, the optimal cut-off values were verified as 45.675 for PNI. After combining general anesthesia and MMSE score, the AUC was 0.712 [95% CI: (0.646, 0.778), sensitivity = 75.0%, specificity = 61.2%] with a median predictive accuracy (Fig. 2B), suggesting that PNI combined with the anesthetic method and MMSE score rather than PNI alone may be used as a potential predictive indicator of POD after hip fracture surgery.
Fig. 2.
Receiver operating characteristic curve analysis of the prognostic nutritional index (PNI) and other risk factors for postoperative delirium; (A) results of PNI alone; (B) result of PNI combined with the anesthetic method and Mini-Mental State Examination score. AUC, area under the curve
Discussion
Although PNI is a convenient, objective, and easy-to-perform indicator to estimate a patient’s nutritional status, its effectiveness as a dependable predictive index for POD must be verified. In this secondary analysis of two prospective cohort studies, we evaluated PNI as a prognostic tool in older adult patients who underwent hip fracture surgery and found that low preoperative PNI was associated with an increased risk of POD compared with high preoperative PNI. Preoperative PNI combined with other risk factors, namely general anesthesia and a low MMSE score, could be used as a median-accurate comprehensive prognostic method for predicting POD, with an AUC value of 0.712 compared to preoperative PNI alone with an AUC value of 0.592.
PNI was first advanced in 1980 by Buzby et al. as a quantitative evaluation indicator to analyze the association between the risk of postoperative complications and baseline nutritional status [20]. In 1984, Onodera et al. revised the calculation of PNI as the present formula [21]. PNI has been used as a prognostic predictor in cancer patients [22, 23] and recently, has also been used to predict the incidence of POD in surgical patients because frailty and malnutrition are associated with POD [24]. Several studies have evaluated PNI as a useful factor for predicting POD after noncardiac surgery [25–27]. Additionally, one study found that older adult patients with hip fractures tended to present with an inadequate nutrient intake for their requirements and had a higher prevalence of malnutrition compared with younger patients [12]. Hence, we evaluated older adult patients with hip fractures in the present study.
The etiology of POD remains unclear. Our previous prospective cohort clinical trial found that the anesthetic method was associated with the incidence of POD, and patients diagnosed with POD were more likely to have lower MMSE scores compared with those without POD [13], which was consistent with the results in the present study. In the present study, the anesthetic method and MMSE score combined with PNI was a stronger predictive method of the incidence of POD compared with PNI alone. However, the MMSE score is an uncorrectable factor preoperatively, while PNI can be corrected easily in a short period before surgery and as a long-term lifestyle improvement in older adult patients. A meta-analysis showed that oral nutritional intervention before surgery could increase serum total protein concentration and decrease the incidence of postoperative complications [28]. A clinical trial found that perioperative taurine supplementation in older adult patients with hip fractures attenuated postoperative oxidative stress [29], as a potential mechanism of POD [30, 31]. However, the efficacy of preoperative nutritional intervention on PNI and the incidence of POD must be studied further.
PNI is often associated with systemic immune-inflammatory response index (SII) to assess the prognosis of cancer patients [32, 33], suggesting PNI is not only a nutritional index but also an inflammation-related marker. On one hand, hypoalbuminemia is associated with postoperative infection and inflammation. Specifically, inflammation increases capillary permeability and the escape of serum albumin, leading to hypoalbuminemia. While hypoalbuminemia is also an independent risk factor of postoperative infection [34]. On the other hand, lymphocytes are an important component of the immune process, low lymphocyte count is used as a marker of inflammation and immunosuppression [35, 36]. With these considerations, PNI is a comprehensive predictor of POD, which is consistent with findings in animal studies demonstrating that systematic inflammation plays a role in the mechanism of POD [37, 38]. Further exploration is needed to determine the precise association between low PNI and neuroinflammation rather than systemic inflammation.
The major strength of our study is that we demonstrated PNI as a prognostic predictor of POD in older adult patients with hip fractures. Through preoperative laboratory examinations, the nutritional status of older adult patients with hip fractures was objectively evaluated. The susceptible patients of POD could be identified and nutritional status could be intervened preoperatively such as albumin supplementation, which provided a preliminary basis for reducing the incidence of POD. However, the current study has several limitations. Firstly, we did not measure plasma inflammatory cytokines in this study, which is a possible limitation. Secondly, this was a single-center study, and the results may not be generalizable to the general population of older adult patients. Thirdly, we used the median PNI value in POD patients as the cut-off value, and the reliability of this cut-off value requires further external validation.
Conclusion
The current secondary analysis of two prospective, observational cohort studies demonstrated that PNI is an objective prognostic predictor of POD in older adult patients with hip fractures. Preoperative PNI combined with other risk factors, namely general anesthesia and low MMSE score, can be used as a comprehensive prognostic method of predicting POD. Perioperative management of older adult patients should involve preoperative nutritional support to decrease the incidence of POD and other complications.
Acknowledgements
Not applicable.
Authors’ contributions
This study protocol was carried out in collaboration between all authors. ZL and YY had the project idea. All authors were involved in the design of the study protocol. XM, YS, YJ and KL developed the intervention with revision of all authors. XM wrote the first draft of the manuscript. TL and DH calculated the sample size according to data analysis plan and wrote the statistical section. XM, YJ, NY, GW and XG have been involved in the drafting and contributed significantly to the revision of this manuscript and have given approval of the final manuscript.
Funding
This research was funded by the grants from National Natural Science Foundation of China (82271222, 81971012, 81873726, 81901095, 81701052, and 81801070), Key Clinical Projects of Peking University Third Hospital (BYSYZD2019027), Peking University “Clinical Medicine plus X” Youth Project (PKU2020LCXQ016).
Availability of data and materials
Data can be obtained from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (approval No. M2022578) and registered in the Chinese Clinical Trial Registry (ChiCTR2300070569). All participants and their legal guardians will be informed about the study goals. Written informed consent will be obtained from all participants or their legal guardians prior to the study enrollment. The study follows according to the Declaration of Helsinki. Participants as well as their relatives or legal guardians can withdraw consent at any time. All participant information and data will be stored securely and identified by a coded ID number only to maintain participants’ confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xinning Mi and Yunyang Jia contributed equally to this work.
Contributor Information
Yi Yuan, Email: julietyy@sina.com.
Zhengqian Li, Email: zhengqianli@hsc.pku.edu.cn.
References
- 1.Rudolph JL, Marcantonio ER. Review articles: postoperative delirium: acute change with long-term implications. Anesth Analg. 2011;112:1202–1211. doi: 10.1213/ANE.0b013e3182147f6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li T, Li J, Yuan L, Wu J, Jiang C, Daniels J, Mehta RL, Wang M, Yeung J, Jackson T, Melody T, Jin S, Yao Y, Wu J, Chen J, Smith FG, Lian Q. Effect of regional vs general anesthesia on incidence of postoperative delirium in older patients undergoing hip fracture surgery: the RAGA randomized trial. JAMA. 2022;327:50–58. doi: 10.1001/jama.2021.22647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu C, Wang B, Yin J, Xue Q, Gao S, Xing L, Wang H, Liu W, Liu X. Risk factors for postoperative delirium after spinal surgery: a systematic review and meta-analysis. Aging Clin Exp Res. 2019 doi: 10.1007/s40520-019-01319-y. [DOI] [PubMed] [Google Scholar]
- 4.Nomura Y, Nakano M, Bush B, Tian J, Yamaguchi A, Walston J, Hasan R, Zehr K, Mandal K, LaFlam A, Neufeld KJ, Kamath V, Hogue CW, Brown CHt. Observational study examining the association of baseline frailty and postcardiac surgery delirium and cognitive change. Anesth Analg. 2019;129:507–514. doi: 10.1213/ane.0000000000003967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Q, Yu S, Li Q, Zhang M, Meng L, Hu S. Preoperative nutritional status in elderly inpatients with gastrointestinal cancer and its linear association with frailty. Nutr Cancer. 2022;74:1376–1387. doi: 10.1080/01635581.2021.1955284. [DOI] [PubMed] [Google Scholar]
- 6.Symeonidis PD, Clark D. Assessment of malnutrition in hip fracture patients: effects on surgical delay, hospital stay and mortality. Acta Orthop Belg. 2006;72:420–427. [PubMed] [Google Scholar]
- 7.Nozoe T, Ninomiya M, Maeda T, Matsukuma A, Nakashima H, Ezaki T. Prognostic nutritional index: a tool to predict the biological aggressiveness of gastric carcinoma. Surg Today. 2010;40:440–443. doi: 10.1007/s00595-009-4065-y. [DOI] [PubMed] [Google Scholar]
- 8.Tokunaga R, Sakamoto Y, Nakagawa S, Miyamoto Y, Yoshida N, Oki E, Watanabe M, Baba H. Prognostic nutritional index predicts severe complications, recurrence, and poor prognosis in patients with colorectal cancer undergoing primary tumor resection. Dis Colon Rectum. 2015;58:1048–1057. doi: 10.1097/DCR.0000000000000458. [DOI] [PubMed] [Google Scholar]
- 9.Feng JF, Chen QX. Significance of the prognostic nutritional index in patients with esophageal squamous cell carcinoma. Ther Clin Risk Manag. 2014;10:1–7. doi: 10.2147/TCRM.S56159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tei M, Wakasugi M, Kishi K, Tanemura M, Akamatsu H. Incidence and risk factors of postoperative delirium in elderly patients who underwent laparoscopic surgery for colorectal cancer. Int J Colorectal Dis. 2016;31:67–73. doi: 10.1007/s00384-015-2335-2. [DOI] [PubMed] [Google Scholar]
- 11.Oe S, Togawa D, Yamato Y, Hasegawa T, Yoshida G, Kobayashi S, Yasuda T, Banno T, Arima H, Mihara Y, Ushirozako H, Yamada T, Matsuyama Y. Preoperative age and prognostic nutritional index are useful factors for evaluating postoperative delirium among patients with adult spinal deformity. Spine (Phila Pa) 2019;1976(44):472–478. doi: 10.1097/brs.0000000000002872. [DOI] [PubMed] [Google Scholar]
- 12.Malafarina V, Reginster JY, Cabrerizo S, Bruyère O, Kanis JA, Martinez JA, Zulet MA. Nutritional status and nutritional treatment are related to outcomes and mortality in older adults with hip fracture. Nutrients 2018;10. 10.3390/nu10050555. [DOI] [PMC free article] [PubMed]
- 13.Song Y, Liu Y, Yuan Y, Jia X, Zhang W, Wang G, Jia Y, Wang X, Liu L, Li W, Li X, Cai N, Liu C, Li Y, Han Y, Zhou Y, Mi X, Shi C, Wang JQ, Vuylsteke A, Guo X, Li Z. Effects of general versus subarachnoid anaesthesia on circadian melatonin rhythm and postoperative delirium in elderly patients undergoing hip fracture surgery: a prospective cohort clinical trial. EBioMedicine. 2021;70:103490. doi: 10.1016/j.ebiom.2021.103490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 15.Girard TD, Thompson JL, Pandharipande PP, Brummel NE, Jackson JC, Patel MB, Hughes CG, Chandrasekhar R, Pun BT, Boehm LM, Elstad MR, Goodman RB, Bernard GR, Dittus RS, Ely EW. Clinical phenotypes of delirium during critical illness and severity of subsequent long-term cognitive impairment: a prospective cohort study. Lancet Respir Med. 2018;6:213–222. doi: 10.1016/s2213-2600(18)30062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. STUDIES of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. Jama. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 17.Bahreini M, Jalili M, Moradi-Lakeh M. A comparison of three self-report pain scales in adults with acute pain. J Emerg Med. 2015;48:10–18. doi: 10.1016/j.jemermed.2014.07.039. [DOI] [PubMed] [Google Scholar]
- 18.Yuan Y, Li Z, Yang N, Han Y, Ji X, Han D, Wang X, Li Y, Liu T, Yuan F, He J, Liu Y, Ni C, Zou P, Wang G, Guo X, Zhou Y. Exosome α-Synuclein release in plasma may be associated with postoperative delirium in hip fracture patients. Front Aging Neurosci. 2020;12:67. doi: 10.3389/fnagi.2020.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xing H, Xiang D, Li Y, Ji X, Xie G. Preoperative prognostic nutritional index predicts postoperative delirium in elderly patients after hip fracture surgery. Psychogeriatrics. 2020;20:487–494. doi: 10.1111/psyg.12511. [DOI] [PubMed] [Google Scholar]
- 20.Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980;139:160–167. doi: 10.1016/0002-9610(80)90246-9. [DOI] [PubMed] [Google Scholar]
- 21.Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85:1001–1005. [PubMed] [Google Scholar]
- 22.Xishan Z, Ye Z, Feiyan M, Liang X, Shikai W. The role of prognostic nutritional index for clinical outcomes of gastric cancer after total gastrectomy. Sci Rep. 2020;10:17373. doi: 10.1038/s41598-020-74525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okamura Y, Sugiura T, Ito T, Yamamoto Y, Ashida R, Ohgi K, Sasaki K, Narimatsu H, Uesaka K. The prognostic roles of the prognostic nutritional index in patients with intraductal papillary mucinous neoplasm. Sci Rep. 2021;11:568. doi: 10.1038/s41598-020-79583-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ringaitienė D, Gineitytė D, Vicka V, Žvirblis T, Šipylaitė J, Irnius A, Ivaškevičius J, Kačergius T. Impact of malnutrition on postoperative delirium development after on pump coronary artery bypass grafting. J Cardiothorac Surg. 2015;10:74. doi: 10.1186/s13019-015-0278-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen J, Zheng C, Zhong J, Zhao G, Shi J, Huang G, Wei Y, Wang S, Yu J, Xia J. Preoperative prognostic nutritional index is useful factor for predicting postoperative delirium after primary total joint arthroplasty. BMC Musculoskelet Disord. 2021;22:778. doi: 10.1186/s12891-021-04626-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kurosu K, Oe S, Hasegawa T, Shimizu S, Yoshida G, Kobayashi S, Fujita T, Yamada T, Ide K, Watanabe Y, Nakai K, Yamato Y, Yasuda T, Banno T, Arima H, Mihara Y, Ushirozako H, Matsuyama Y. Preoperative prognostic nutritional index as a predictive factor for medical complication after cervical posterior decompression surgery: a multicenter study. J Orthop Surg (Hong Kong) 2021;29:23094990211006869. doi: 10.1177/23094990211006869. [DOI] [PubMed] [Google Scholar]
- 27.Liu H, Dai M, Guan H, Gao X, Zhou Y, Sun X, Zhou J, Hu X, Li X, Song Y, Han Y, Cao J. Preoperative prognostic nutritional index value is related to postoperative delirium in elderly patients after noncardiac surgery: a retrospective cohort study. Risk Manag Healthc Policy. 2021;14:1–8. doi: 10.2147/rmhp.S280567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu M, Yang J, Yu X, Huang X, Vaidya S, Huang F, Xiang Z. The role of perioperative oral nutritional supplementation in elderly patients after hip surgery. Clin Interv Aging. 2015;10:849–858. doi: 10.2147/cia.S74951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Stijn MF, Bruins AA, Vermeulen MA, Witlox J, Teerlink T, Schoorl MG, De Bandt JP, Twisk JW, Van Leeuwen PA, Houdijk AP. Effect of oral taurine on morbidity and mortality in elderly hip fracture patients: a randomized trial. Int J Mol Sci. 2015;16:12288–12306. doi: 10.3390/ijms160612288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lopez MG, Hughes CG, DeMatteo A, O'Neal JB, McNeil JB, Shotwell MS, Morse J, Petracek MR, Shah AS, Brown NJ, Billings FTt. Intraoperative oxidative damage and delirium after cardiac surgery. Anesthesiology. 2020;132:551–561. doi: 10.1097/aln.0000000000003016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han Y, Zhang W, Liu J, Song Y, Liu T, Li Z, Wang X, Yang N, Li Y, Han D, Mi X, Zhou Y, Li M, Guo X, Zhong L, Wang G, Yuan Y. Metabolomic and lipidomic profiling of preoperative CSF in elderly hip fracture patients with postoperative delirium. Front Aging Neurosci. 2020;12:570210. doi: 10.3389/fnagi.2020.570210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kubota K, Ito R, Narita N, Tanaka Y, Furudate K, Akiyama N, Chih CH, Komatsu S, Kobayashi W. Utility of prognostic nutritional index and systemic immune-inflammation index in oral cancer treatment. BMC Cancer. 2022;22:368. doi: 10.1186/s12885-022-09439-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ding P, Guo H, Sun C, Yang P, Kim NH, Tian Y, Liu Y, Liu P, Li Y, Zhao Q. Combined systemic immune-inflammatory index (SII) and prognostic nutritional index (PNI) predicts chemotherapy response and prognosis in locally advanced gastric cancer patients receiving neoadjuvant chemotherapy with PD-1 antibody sintilimab and XELOX: a prospective study. BMC Gastroenterol. 2022;22:121. doi: 10.1186/s12876-022-02199-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Soeters PB, Wolfe RR, Shenkin A. Hypoalbuminemia: pathogenesis and clinical significance. JPEN J Parenter Enteral Nutr. 2019;43:181–193. doi: 10.1002/jpen.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamamoto T, Kawada K, Obama K. Inflammation-related biomarkers for the prediction of prognosis in colorectal cancer patients. Int J Mol Sci 2021;22. 10.3390/ijms22158002. [DOI] [PMC free article] [PubMed]
- 36.Fanetti G, Polesel J, Fratta E, Muraro E, Lupato V, Alfieri S, Gobitti C, Minatel E, Matrone F, Caroli A, Revelant A, Lionello M, Zammattio Polentin V, Ferretti A, Guerrieri R, Chiovati P, Bertolin A, Giacomarra V, Paoli A, Vaccher E, Sartor G, Steffan A, Franchin G. Prognostic nutritional index predicts toxicity in head and neck cancer patients treated with definitive radiotherapy in association with chemotherapy. Nutrients 2021;13. 10.3390/nu13041277. [DOI] [PMC free article] [PubMed]
- 37.Mi X, Cao Y, Li Y, Li Y, Hong J, He J, Liang Y, Yang N, Liu T, Han D, Kuang C, Han Y, Zhou Y, Liu Y, Shi C, Guo X, Li Z. The non-peptide angiotensin-(1–7) mimic AVE 0991 attenuates delayed neurocognitive recovery after laparotomy by reducing neuroinflammation and restoring blood-brain barrier integrity in aged rats. Front Aging Neurosci. 2021;13:624387. doi: 10.3389/fnagi.2021.624387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 2020;125:492–504. doi: 10.1016/j.bja.2020.06.063. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be obtained from the corresponding author upon reasonable request.