Abstract
Purpose
To analyze internal tibial rotation through magnetic resonance imaging (MRI) of patients with anterior cruciate ligament (ACL) injuries with and without an unstable medial meniscal ramp lesion (MMRL).
Methods
Retrospective analysis of prospectively data was performed to include all consecutive patients who underwent primary ACL reconstruction (ACLR) between January 2022 and June 2022. Two groups, ACLR + unstable MMRL and ACLR without MMRL, were constituted. Propensity score matching analysis was used to limit selection bias. The angle between surgical epicondylar axes (SEAs) and the tangent line of the posterior tibial condyles (PTCs) was measured to analyze the rotational alignment between distal femur and proximal tibia. MMRLs were defined unstable if they were ≥1 cm, if the lesions extend beyond the lower pole of the femoral condyle, and/or if there was displacement into the medial compartment by anterior probing.
Results
Twenty-eight propensity-matched pairs were included. The ACLR + unstable MMRL presented a significantly greater internal rotation of the tibia compared to ACLR without MMRL (P < .001). An internal tibial rotation was associated with unstable ramp lesions in ACL-injured patients (odds ratio [OR], 0.36; 95% CI, 0.25-0.41; P < .0001). If SEA-PTC was 0°, the sensitivity and specificity of the SEA-PTC angle to detect unstable MMRL were respectively 100% (95% CI, 85%-100%) and 18% (95% CI, 8%-36%). Otherwise, if SEA-PTC angle was –10°, the sensitivity and specificity of the SEA-PTC angle to detect unstable MMRL were respectively 43% (95% CI, 27%-61%) and 96% (95% CI, 81%-100%). Bone edema of the posterior medial tibial plateau was significantly associated with unstable ramp lesions (OR, 1.58; 95% CI, 1.21-2.06; P = .029).
Conclusions
Unstable MMRL concomitant to an ACL rupture was associated with an increased tibial internal rotation.
Level of Evidence
Level III, retrospective comparative trial.
A medial meniscal ramp lesion (MMRL) is defined as a detachment between the posterior horn of the medial meniscus and the articular capsule.1 The true incidence of MMRL is unknown due to the high rate of underdiagnosis, even though recent studies revealed an incidence ranging from 9% to 42% during anterior cruciate ligament (ACL) injury with a higher incidence in elite athletes.2, 3, 4, 5, 6 Willinger et al.4 reported an association between MMRL, medial collateral ligament (MCL) injuries, and medial tibia bone bruising on magnetic resonance imaging (MRI). The authors hypothesized a specific injury mechanism as anterior translation and/or external rotatory subluxation of the medial tibial plateau during ACL tear resulting in MMRL, MCL injuries, and bone edema of posterior medial tibial plateau (MTP).4,7
Despite some publications describing MMRLs and their diagnosis,4,8 the role of these lesions in knee instability needs to be deepened. MMRLs were classified as stable if they were ≤1 cm, if they did not extend beyond the lower pole of the femoral condyle, and if the medial meniscus did not displace into the medial compartment with anteriorly directed probing at the time of surgery. Otherwise, MMRLs were classified as unstable.9, 10, 11
It has been shown that unstable MMRL was associated with an increase in anteroposterior instability in the ACL-deficient knee.12,13 Moreover, recent studies revealed a plausible increase of internal tibial rotation in case of meniscotibial ligament injury14 defined by Thaunat and colleagues15 in 2016 as type III ramp lesions.
Some studies pointed out the role of ACL as a restraint to anterior translation and internal rotation of the tibia relative to the femur.16, 17, 18 Although measurement of femorotibial rotation using a static MRI could be questionable, because it does not reproduce the internal rotation of the tibia during the pivot-shift phenomenon in the ACL-deficient knee, several authors measured the degree of internal rotation of the tibia in the ACL-deficient knee using axial MRI images.13,14 Hence, Vassalou et al.19 indicated that adult knees demonstrated a mean 7° increase in the internal rotation when the ACL was ruptured. Moreover, Mitchell et al.20 found a significant increase in internal tibial rotation in ACL-deficient knees compared to intact knees in the adolescent population. Hong et al.21 reported that aged patients with ACL tears exhibited significantly greater tibial internal rotation compared to younger patients (5.6° vs 4.2°). The purpose of this study was to analyze the femorotibial rotation through the MRI of patients with ACL injuries with and without unstable MMRL. We hypothesized that unstable MMRL would be associated with an increase in internal tibia rotation, inferring a plausible role of these lesions on rotatory stability of ACL-deficient knees.
Methods
The present retrospective study was conducted in accordance with the Declaration of Helsinki Ethical Principles and Good Clinical Practices and was approved by the ethical committee of the Medical University of Innsbruck (AN2015-0050 346/4.28). Informed consent was obtained from all individual participants included in the study. A retrospective analysis of prospectively collected data from the database of a specialized joint surgery clinic was conducted. All patients who underwent arthroscopic primary ACL reconstruction (ACLR) between January 2022 and June 2022 were considered for study eligibility. The study flowchart is represented in Figure 1. Two groups, ACLR + unstable MMRL and ACLR without MMRL, were constituted. Two senior surgeons (C.F. and C.H.) performed all the surgeries in both groups. Preoperatively, all patients had sustained an ACL tear, diagnosed based on clinical examination and MRI. All patients were assessed preoperatively by the senior surgeon (C.F. or C.H.). Patients of both groups were excluded if they had the following: fractures around the knee, a history of knee surgery, other combined surgical procedures such as osteotomy, revision ACL, incomplete clinical data, poor radiologic evaluations, time from MRI to surgery greater than 3 months, and stable MMRL. Stable MMRLs were excluded from eligibility because their role in rotational knee stability in the ACL-deficient knee has not been clearly established. Indeed, Albayrak et al.22 reported that leaving the stable MMRL unrepaired does not negatively affect clinical or functional outcomes, pivot-shift grade, and return-to-sports rates after ACLR at 3 years of follow-up. Moreover, Balazs et al.9 reported at 2 years of follow-up that the treatment of stable MMRL might not have clinical benefit in ACL-deficient knees.
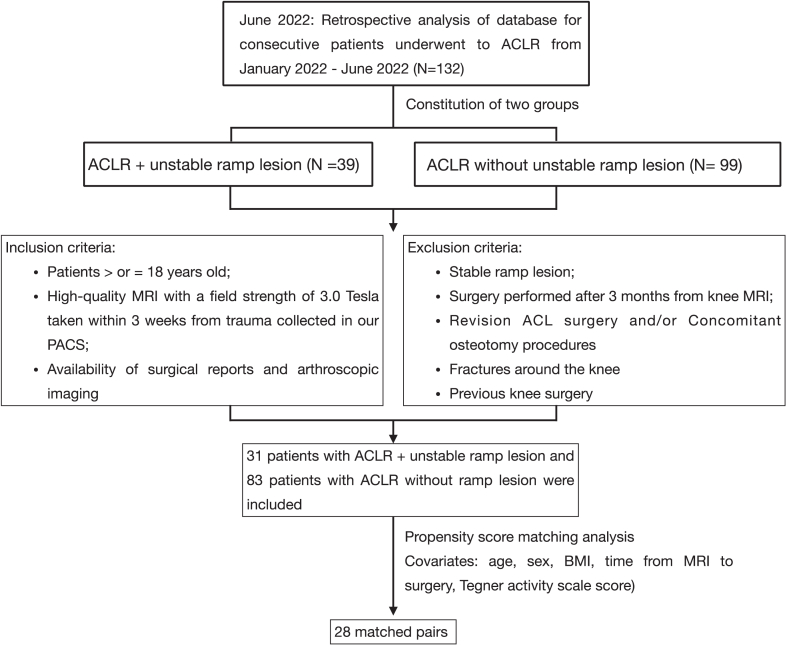
Fig 1.
Flowchart of the study.
Arthroscopic Evaluation
Standard anteromedial and anterolateral portals were applied for ACLR, and a routine diagnostic assessment was made. To detect the type III ramp lesion according to the Thaunat et al.15 classification, the stability of the medial meniscus was first assessed by meticulous probing through anterior visualization during surgery.23 The posteromedial compartment was routinely assessed by advancing a 30° arthroscope from the anterolateral portal into the posteromedial recess between the posterior cruciate ligament and medial femoral condyle (Gillquist maneuver).24 To aid this, the knee could be held in slight flexion with valgus stress applied or a switching stick could be used.25 Despite some authors recommending the use of an accessory posteromedial portal to detect ramp lesions,26 the senior author used increased knee flexion with internal rotation of the tibia to better visualize the ramp region. A posteromedial portal was made in case of repair or doubt. MMRLs were defined stable if they were ≤1 cm, if they did not extend beyond the lower pole of the femoral condyle, and if there was lack of displacement into the medial compartment by anteriorly directed probing.9, 10, 11 On the contrary, unstable MMRLs were defined if they were ≥1 cm, if the lesions extended beyond the lower pole of the femoral condyle, and/or if there was displacement into the medial compartment by anterior probing.11
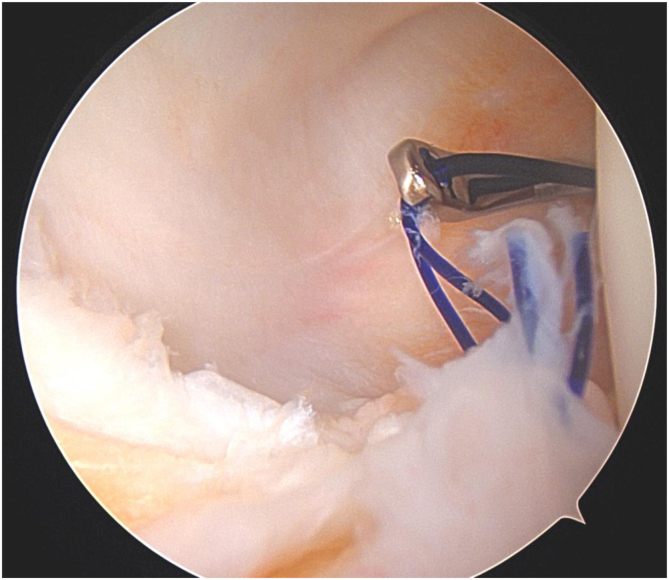
If an unstable ramp lesion was identified, a shaver was routinely used to prepare both surfaces of the tear. A 25° suture hook (SutureLasso; Arthrex), angled to the left for a right-sided knee and to the right for a left-sided knee, loaded with a No. 0 absorbable monofilament suture (PDS; Ethicon) was then inserted through the posteromedial portal, and between 1 and 3 separate sutures were used to repair (Fig 2).
Fig 2.
Right knee. Unstable medial ramp lesion repaired with 2 separate N.0-PDS sutures inserted through the posteromedial portal.
Radiologic Assessment
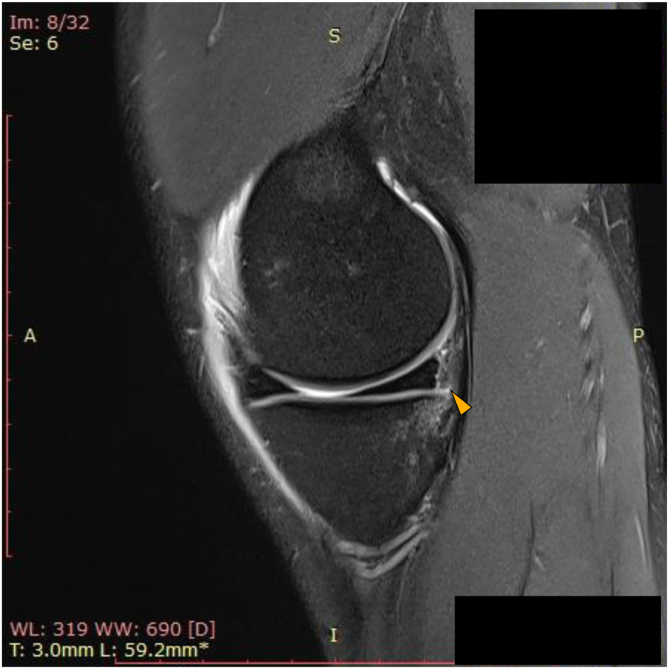
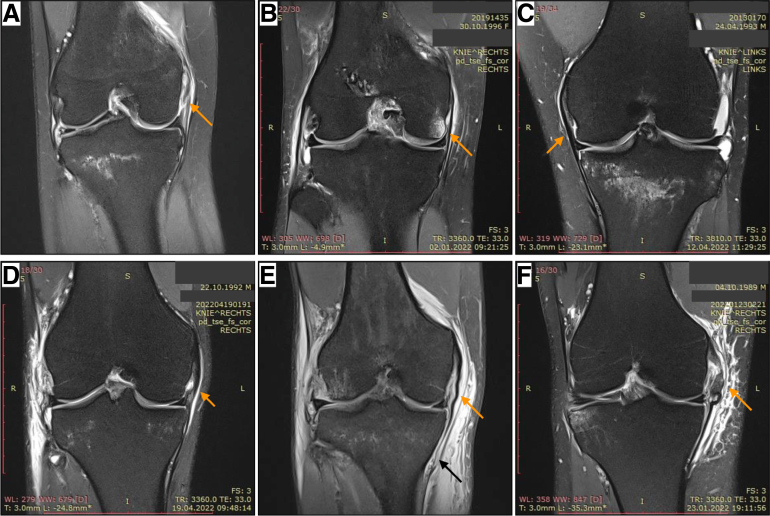
Two sports knee surgery fellows (L.F. and A.M.) independently analyzed all MRI images obtained before surgery (Fig 3). Bone marrow edema was defined as increased signal intensity on the fat-suppressed water-sensitive images within the bone. Bone marrow edema of the medial/lateral tibial plateau and medial/lateral femoral condyle was reported in each group. Deep and superficial MCL injuries were assessed by coronal T2-weighted MRI with fat saturation (Figs 4 and 5). MCLs were considered injured if there were (1) direct signs of injury such as a clear discontinuity in the MCL fibers or a femoral/tibial avulsion was visible, or (2) there were indirect signs of injury such as thickening and/or intra-substance signal change of the MCL fibers, focal bone marrow edema at the MCL insertion site to the femur, soft tissue edema in the region of the MCL, or a wavy appearance to the MCL fibers.
Fig 3.
Sagittal T2-weighted magnetic resonance imaging (MRI) with fat saturation of the left knee. Head arrow: medial meniscus ramp lesion.
Fig 4.
Coronal T2-weighted MRI with fat saturation. (a, b, d, e, f) right knee; (c) left knee. (a, c, d) Note fluid superficially and deep to the deep meniscofemoral ligament injured (orange arrow) accompanying an anterior cruciate ligament (ACL) rupture. (b) Typical MRI bone edema (orange arrow) at the medial femoral condyle adjacent to the deep MCL (dMCL) attachment site. (e) Distal grade III medial collateral ligament (MCL) rupture (black arrow) concomitant with deep MCL tear (orange arrow) and ACL rupture. (f) Midportion grade III MCL tear (orange arrow) with concomitant deep MCL tear and ACL rupture.
Fig 5.
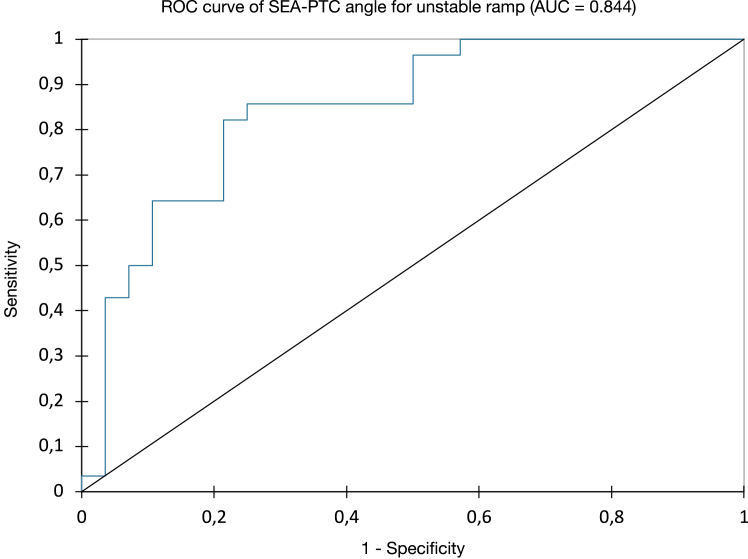
Receiving operating curve (ROC) of the model. (AUC, area under the curve; PTC, posterior tibial condyle; SEA, surgical epicondylar axis.)
To measure the axial alignment of the distal femur and proximal tibia, 2 sections were identified from each MRI.27 The first slice was taken in the mid-throchlear region of the femoral condyle, identified by the Roman arch appearance of the intercondylar groove with the apex of the Roman arch corresponding to one-third of the height of the condyle. The surgical epicondylar axes (SEAs) from the lateral epicondyle and medial sulcus were delineated. The second slice was taken in correspondence with the proximal tibial plateau above the end of the proximal tibiofibular joint where the semimembranosus tendon inserts into the tibial bone. The tangent line of the posterior tibial condyles (PTCs) was delineated. The angle between SEA-PTC was measured (Fig 4).27,28 A negative value was defined as internal torsion and a positive value as external torsion of the distal segment.
Statistical Analysis
A priori power analysis was performed to determine the appropriate sample size for the study. Considering an α level with P = .05, a power of 95%, and an effect size of 0.5, it was estimated that 24 matched pairs of participants would be needed respectively in the ramp and control groups to detect a statistically significant difference in SEA-PTC angle. The sample size calculation was performed with the use of the G-Power software (G-Power version 3.1).29 Data were collected and organized using Excel (Microsoft). Statistical analyses were performed using the XLSTAT statistical software packages (Addinsoft LLC). Categorical variables were expressed in numbers and percentages. The normal distribution of variables was verified through the Shapiro-Wilk test. The angle SEA-PTC did not show a normal distribution (P < .05). Mean and standard deviation or median and interquartile range (IQR) were used to summarize the variables according to their distribution. Differences in angles between the 2 groups were assessed through the Wilcoxon rank-sum test. The Student t test for unpaired data was performed in the case of normally distributed variables. Differences between categorical variables were evaluated with the Fisher exact test. Binomial logistic regression analysis was performed to evaluate SEA-PTC angle and bone edema of MTP for the presence of unstable MMRL. Logit model was adjusted by body mass index (BMI), sex, and time from MRI to surgery. The Wald test was used to assess significance. The validity of the logistic model in detecting the presence of ramp injury was evaluated by the receiver operating characteristic (ROC) where sensitivity was defined as the probability of correctly detecting the presence of ramp and specificity as the probability of correctly detecting the absence of ramp. The area under the curve (AUC) was reported. The included factors were chosen in accordance with previous studies.1,4 Inter-rater correlation coefficient (ICC) was calculated for inter-rater reliability for measuring SEA-PTC and detection of deep and superficial MCL injuries. The significance threshold was set at P = .05. A post hoc power analysis was performed.
Propensity Matching
The covariates included in the model were age at the time of surgery, sex, BMI, the time interval between MRI and surgery, and Tegner activity scale score. Then, each patient with ACLR + unstable MMRL was matched with a patient who underwent ACLR without MMRL, according to the nearest corresponding propensity score. In the evaluation of covariates, a predefined caliper width of 0.1 without case replacement was used to reach enough similarity between groups to allow comparison.30
Results
Population
The flowchart of the study flow is presented in Figure 1. Overall, 132 patients underwent ACLR during the study period from January 2022 to June 2022. From analysis of surgical report and arthroscopic imaging, 2 groups were identified: ACLR + unstable MMRL and ACLR without MMRL. Thirty-nine and 99 patients were respectively included in the groups. The incidence of unstable MMRL was 29.5% (39 of 132 patients).
Of these, 31 patients in the ACLR + unstable ramp group and 83 patients in the ACLR without ramp lesion group fulfilled the inclusion and exclusion criteria and were eligible for the matching process. The final population comprised 28 propensity-matched pairs. The demographic characteristics of the study population are summarized in Table 1.
Table 1.
Patients’ Demographic Characteristics (28 Matched Pairs)
| Unstable MMRL + ACLR | ACLR Without MMRL | |
|---|---|---|
| Characteristic | ||
| Age, y | ||
| Mean (SD) [range] | 25.2 (5.4) [18-37] | 27.1 (3.6) [21-34] |
| Median (IQR, quartiles 1-3) | 24.5 (6.3, 22-28.3) | 26.5 (5.5, 24.8-30.3) |
| Sex, n (%) | ||
| Male | 13 (46%) | 16 (57%) |
| Female | 15 (54%) | 12 (43%) |
| BMI | ||
| Mean (SD) [range] | 22.8 (1.8) [19.4-26.1] | 24.9 (2.8) [20.0-34.0] |
| Median (IQR, quartiles 1-3) | 22.8 (2.1, 21.9-24.0 | 23.7 (3.4, 22-25.4) |
| Time from MRI to surgery, d | ||
| Mean (SD) [range] | 8.4 (10.5) [0-47] | 7.1 (7.9) [0-26] |
| Median (IQR, quartiles 1-3) | 5 (14, 0-14) | 2 (12, 1-13) |
| Preoperative Tegner Activity Scale score | ||
| Mean (SD) [range] | 7.2 (1.2) [5-10] | 6.8 (1.2) [3-10] |
| Median (IQR, quartiles 1-3) | 7 (1.25, 6.75-8.0) | 7 (1, 6-7) |
NOTE. Statistical analyses of mean differences between groups and the resulting P values are not required after propensity matching.
ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; IQR, interquartile range; MMRL, medial meniscus ramp lesion; MRI, magnetic resonance imaging.
The ICC value for the reliability of SEA-PTC was 0.90, indicating an excellent agreement. The ICC values for the reliability of deep and superficial MCL injuries were respectively 0.83 and 0.85, indicating satisfying agreement.
Surgical and Radiologic Factors
There were no statistically significant differences in terms of superficial and deep MCL injuries and lateral meniscus injuries between the 2 matched groups (Table 2). The ACLR + unstable MMRL presented a significantly greater internal rotation of the tibia (SEA-PTC) compared to ACLR without MMRL (P < .001) (Table 3). From logistic analysis, it has been reported that internal tibial rotation was strongly associated with unstable ramp lesions (odds ratio [OR] 0.36; 95% CI, 0.25-0.41, P < .0001).
Table 2.
Magnetic Resonance Imaging and Surgical Characteristics of the 2 Groups (28 Matched Pairs)
| Characteristic | Unstable MMRL + ACLR, n (%) | ACLR Without MMRL, n (%) | P Value |
|---|---|---|---|
| Superficial MCL | |||
| Intact | 20 (71.4) | 21 (75.0) | 1.00 |
| Injured | 8∗ (28.6) | 7† (25.0) | |
| Deep MCL | |||
| Intact | 12 (42.9) | 13 (46.4) | 1.00 |
| Injured | 16 (57.1) | 15 (53.6) | |
| Lateral meniscus injury | |||
| Intact | 13 (46.4) | 11 (39.3) | .788 |
| Injured | 15 (53.6) | 17 (60.7) |
ACLR, anterior cruciate ligament reconstruction; MCL, medial collateral ligament; MMRL, medial meniscus ramp lesion.
Three patients with grade I, 3 with grade II, and 2 with grade III lesion.
Three patients with grade I, 3 with grade II, 1 patient with grade III lesion.
Table 3.
Concomitant Edema on MRI and Tibia Rotation in Relation to the Presence or Absence of Intraoperative Meniscal Ramp Lesions (28 Matched Pairs)
| Characteristic | Unstable MMRL + ACLR | ACLR Without MMRL | P Value |
|---|---|---|---|
| Edema MTP | |||
| Yes | 16 (57.1) | 7 (25.0) | .029 |
| No | 12 (42.9) | 21 (75.0) | |
| Edema LTP | |||
| Yes | 18 (64.3) | 23 (82.1) | .227 |
| No | 10 (35.7) | 5 (17.9) | |
| Edema MFC | |||
| Yes | 1 (3.6) | 0 (0) | 1.00 |
| No | 27 (96.4) | 28 (100) | |
| Edema LFC | |||
| Yes | 14 (50.0) | 10 (35.7) | .418 |
| No | 14 (50.0) | 18 (64.3) | |
| SEA-PTC angle | |||
| Mean (SD) [range] | –9.2 (3.9) [–19.9 to –2] | –3.5 (3.9) [–14 to 4] | <.001 |
| Median (IQR, quartiles 1-3) | –9.3 (4.3, –11.4 to –7.1) | –2.9 (4.9, –5.9 to –1.0) |
NOTE. Values are presented as number (%) unless otherwise indicated. Bold values indicate significant (P < .05).
ACLR, anterior cruciate ligament reconstruction; LFC, lateral femoral condyle; LTP, lateral tibial plateau; MFC, medial femur condyle; MMRL, medial meniscus ramp lesion; MTP, medial tibial plateau; PTC, posterior tibial condyle; SEA, surgical epicondylar axis.
Specifically, if SEA-PTC was set to 0°, the sensitivity and specificity of the SEA-PTC angle to detect unstable MMRL were respectively 100% (95% CI, 85%-100%) and 18% (95% CI, 8%-36%). Otherwise, if the SEA-PTC angle was set to –10° of internal tibial tibia rotation, the sensitivity and specificity of the SEA-PTC angle to detect unstable MMRL were respectively 43% (95% CI, 27%-61%) and 96% (95% CI, 81%-100%). The AUC related to the logit model considering only the SEA-PTC variable with the association of unstable ramp was 0.844 (Fig 5). Bone edema of MTP was significantly associated with unstable ramp lesions (OR, 1.58; 95% CI, 1.21-2.06; P = .029) (Table 4). The AUC related to the logit model considering SEA-PTC angle and bone edema of MTP as variables in association with the unstable ramp was 0.878.
Table 4.
Logistic regression analysis Showing the Association Between the Presence of Ramp Lesion and Internal Tibial Rotation and Bone Edema of MTP
| Factor | Regression Coefficient (β) | SE | OR (95% CI) | P Value |
|---|---|---|---|---|
| Bone edema MTP | 0.456 | 0.209 | 1.58 (1.21-2.06) | .029 |
| SEA-PTC | –1.024 | 0.273 | 0.36 (0.25-0.51) | <.001 |
NOTE. Nagelkerke R2 = 0.532.
Bold values indicate significance (P < .05).
MTP, medial tibial plateau; OR, odds ratio; PTC, posterior tibial condyle; SEA, surgical epicondylar axis.
Discussion
The most important finding of the present study was that an increased internal tibial rotation was associated with unstable MMRL in the ACL-injured knee. The MMRL group was characterized by 9.2° of internal tibial rotation compared to 3.5° in matched patients without unstable MMRL. If the SEA-PTC angle was set to –10° of internal tibia rotation, the specificity of the SEA-PTC angle to detect an unstable MMRL lesion was 96% (95% CI, 81%-100%). In patients with ACL injury who show an internal tibial rotation greater than –10° on preoperative MRI, a careful assessment and suspicion for ramp lesion should be considered. Anatomic and biomechanical studies of the posteromedial corner of the knee can explain these findings, especially in light of recent discoveries about the anatomy and biomechanics of ramp injury and meniscotibial ligaments.31, 32, 33, 34 Recent studies have revealed the close anatomic relation between the semimembranosus tendon and the posterior meniscocapsular region.23,35,36 It is assumed that the sudden contraction of the semimembranosus muscle secondary to anterior translation of the tibia during ACL injury and/or contrecoup mechanism could stress the meniscocapsular area, leading to ramp injury and anteromedial instability.32,35,37
The emerging relation between ramp lesions and anteromedial instability is being increasingly recognized.38 Despite several structures constituting the posteromedial corner of the knee as the posterior oblique ligament, posterior medial capsule, semimembranosus, and medial gastrocnemius tendon, recent biomechanical studies by Ahn et al.39 and Peltier et al.31 have reported an increase in anteroposterior instability in ACL-injured knees in case of unstable MMRL. Moreover, other studies pointed out a significant increase in internal tibial rotation following the creation of an unstable MMRL and meniscotibial ligament lesion.31,33
The effect of unstable MMRL on native ACL or graft after reconstruction has been also extensively studied.13,40, 41, 42, 43, 44, 45, 46 Unrecognized MMRLs significantly increase stress on the ACL, leading to a higher risk of graft failure after ACLR.13,42, 43, 44, 45, 46 In addition, an isolated ACLR in the presence of unstable and unrepaired MMRL does not restore normal knee kinematics with consequent chronic residual laxity.13,31 Unfortunately, we were unable to show the effect of MMRL repair on the internal tibia rotation. However, several authors reported that MMRL repair contributes to improving the rotational stability in ACL-deficient knees.33,38 Specifically, rotational stability of the knee was restored when meniscocapsular and meniscotibial repairs were performed concomitantly.40
Furthermore, it has been shown that lateral extra-articular tenodesis (LET) reduces rotational laxity when combined with ACLR.47,48 Sonnery-Cottet et al.42 revealed that the failure rate of MMRL repair was significantly lower after combined ACLR and anterolateral ligament reconstruction (ALLR).40,49 Although isolated ACLR reliably restores anteroposterior stability, excessive tibial rotation may persist.43 For these reasons, adding ALLR or LET should be considered in the case of ACLR and MMRL repair to decrease rotational laxity and reduce the risk of failure of MMRL repair and ACLR.40,43,50
From recent literature, several risk factors have been proposed for unstable MMRL in the ACL-deficient knee. Hence, steep medial tibial and meniscal slope and increased lateral femoral condyle ratio were associated with unstable MMRL.51, 52, 53
Numerous authors have investigated the association of bone edema of MTP and ramp lesions.4,54, 55, 56, 57 Our results confirmed previous studies. Bone edema of MTP was significantly associated with unstable MMRL (OR, 1.58; 95% CI, 1.21-2.06; P = .029). Moreover, we reported bone edema of MTP in 57.1% of patients with unstable MMRL vs 25.0% of the control group.
Hence, Cristiani et al.54 reported tibia bone marrow edema in 61% of patients with ramp. This percentage raised respectively to 71% and 87.5% in recent studies published by DePhillipo et al.55 and Willinger et al.4
Regarding the association between MCL injuries and unstable MMRL, we reported no significant differences in terms of deep and superficial MCL injuries between groups. Our results were in contrast to those reported by Willinger et al.,4 where patients with unstable MMRL were characterized by deep and superficial MCL injuries respectively in 62.5% and 93.8% of cases. However, the same authors reported that the 67% of consecutive patients who underwent ACLR had concomitant injuries to their medial ligament complex that were not evident on preoperative clinical examination.58
Limitations
This study has limitations to consider when interpreting its results. First, its retrospective nature is subject to confounders and makes it not possible to infer causality from their findings. Indeed, other factors could act on the intra-articular internal tibia rotation. The varus alignment and internal tibial rotation that results as contrecoup injury after ACL tear55 could aggravate the anterior sliding of the medial femoral condyle on the medial tibial plateau, resulting in higher stress on the posterior meniscocapsular junction in case of increased internal tibial rotation.51 For these reasons, we cannot establish if the internal tibial rotation represents a risk factor for unstable MMRL or the greater internal tibia rotation that we observed in the unstable MMRL group was due to greater rotatory knee instability caused by unstable MMRL. Although the limitations of a retrospective study are well recognized, including selection bias, successful propensity matching reduced this effect. The study was carried out by analyzing static measurement (static MRI of knee performed after trauma). Therefore, dynamic analysis is necessary to confirm the hypothesis. The sample size was limited, but the results are original, and the patients enrolled were allowed to reach an adequate power for the study from previous statistical analysis. Femoral anteversion, tibial torsion, and contralateral femoral tibial rotation of the knee were not considered in both groups, representing limitations of our study.
Conclusions
Unstable MMRL concomitant to an ACL rupture was associated with an increased tibial internal rotation.
Disclosures
The authors report the following potential conflicts of interest or sources of funding: B.S.-C. reports stock from AREAS and personal fees from Arthrex outside the submitted work. C.F. reports personal fees from Storz and fellowship support from Zimmer outside the submitted work. All other authors (L.F., A.M., T.D.V., C.P., A.G., E.A., and C.H.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Acknowledgments
The study group thanks all the participants of the study for their efforts.
Supplementary Data
References
- 1.Qalib Y.O., Tang Y., Wang D., Xing B., Xu X., Lu H. Ramp lesion of the medial meniscus. EFORT Open Rev. 2021;6:372–379. doi: 10.1302/2058-5241.6.200126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guimaraes J.B., Schwaiger B.J., Gersing A.S., et al. Meniscal ramp lesions: Frequency, natural history, and the effect on knee cartilage over 2 years in subjects with anterior cruciate ligament tears. Skeletal Radiol. 2021;50:551–558. doi: 10.1007/s00256-020-03596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tashiro Y., Mori T., Kawano T., et al. Meniscal ramp lesions should be considered in anterior cruciate ligament-injured knees, especially with larger instability or longer delay before surgery. Knee Surg Sports Traumatol Arthrosc. 2020;28:3569–3575. doi: 10.1007/S00167-020-06161-8. [DOI] [PubMed] [Google Scholar]
- 4.Willinger L., Balendra G., Pai V., et al. Medial meniscal ramp lesions in ACL-injured elite athletes are strongly associated with medial collateral ligament injuries and medial tibial bone bruising on MRI. Knee Surg Sports Traumatol Arthrosc. 2022;30:1502–1510. doi: 10.1007/s00167-021-06671-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meena A., Farinelli L., Hoser C., et al. Revision ACL reconstruction using quadriceps, hamstring and patellar tendon autografts leads to similar functional outcomes but hamstring graft has a higher tendency of graft failure. Knee Surg Sports Traumatol Arthrosc. 2023;31:2461–2468. doi: 10.1007/s00167-022-07200-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farinelli L., Abermann E., Meena A., Ueblacker P., Hahne J., Fink C. Return to play and pattern of injury after ACL rupture in a consecutive series of elite UEFA soccer players. Orthop J Sport Med. 2023;11 doi: 10.1177/23259671231153629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grassi A., Tosarelli F., Agostinone P., Macchiarola L., Zaffagnini S., Della Villa F. Rapid posterior tibial reduction after noncontact anterior cruciate ligament rupture: Mechanism description from a video analysis. Sports Health. 2020;12:462–469. doi: 10.1177/1941738120936673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sonnery-Cottet B., Conteduca J., Thaunat M., Gunepin F.X., Seil R. Hidden lesions of the posterior horn of the medial meniscus: A systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921–926. doi: 10.1177/0363546514522394. [DOI] [PubMed] [Google Scholar]
- 9.Balazs G.C., Greditzer H.G., Wang D., et al. Non-treatment of stable ramp lesions does not degrade clinical outcomes in the setting of primary ACL reconstruction. Knee Surg Sport Traumatol Arthrosc. 2020;28:3576–3586. doi: 10.1007/s00167-020-06017-1. [DOI] [PubMed] [Google Scholar]
- 10.Liu X., Zhang H., Feng H., Hong L., Wang X., Song G. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? A prospective randomized controlled trial. Am J Sports Med. 2017;45:1004–1011. doi: 10.1177/0363546516682493. [DOI] [PubMed] [Google Scholar]
- 11.Tuphé P., Foissey C., Unal P., et al. Long-term natural history of unrepaired stable ramp lesions: A retrospective analysis of 28 patients with a minimum follow-up of 20 years. Am J Sports Med. 2022;50:3273–3279. doi: 10.1177/03635465221120058. [DOI] [PubMed] [Google Scholar]
- 12.Kaiser J.T., Meeker Z.D., Horner N.S., et al. Meniscal ramp lesions—Skillful neglect or routine repair? J Orthop. 2022;32:31–35. doi: 10.1016/j.jor.2022.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stephen J.M., Halewood C., Kittl C., Bollen S.R., Williams A., Amis A.A. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44:400–408. doi: 10.1177/0363546515617454. [DOI] [PubMed] [Google Scholar]
- 14.Cristiani R., Mouton C., Stålman A., Seil R. Meniscal ramp lesions: A lot is known, but a lot is also unknown. Knee Surg Sports Traumatol Arthrosc. 2023;31:2535–2539. doi: 10.1007/s00167-022-07292-w. [DOI] [PubMed] [Google Scholar]
- 15.Thaunat M., Fayard J.M., Guimaraes T.M., Jan N., Murphy C.G., Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5:e871–e875. doi: 10.1016/j.eats.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Engebretsen L., Wijdicks C.A., Anderson C.J., Westerhaus B., LaPrade R.F. Evaluation of a simulated pivot shift test: A biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2012;20:698–702. doi: 10.1007/s00167-011-1744-1. [DOI] [PubMed] [Google Scholar]
- 17.Frank J.M., Moatshe G., Brady A.W., et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: A biomechanical study. Orthop J Sport Med. 2017;5 doi: 10.1177/2325967117695756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lian J., Diermeier T., Meghpara M., et al. Rotatory knee laxity exists on a continuum in anterior cruciate ligament injury. J Bone Joint Surg Am. 2020;102:213–220. doi: 10.2106/JBJS.19.00502. [DOI] [PubMed] [Google Scholar]
- 19.Vassalou E.E., Klontzas M.E., Kouvidis G.K., Matalliotaki P.I., Karantanas A.H. Rotational knee laxity in anterior cruciate ligament deficiency: An additional secondary sign on MRI. AJR Am J Roentgenol. 2016;206:151–154. doi: 10.2214/AJR.15.14816. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell B.C., Siow M.Y., Bastrom T., et al. Coronal lateral collateral ligament sign: A novel magnetic resonance imaging sign for identifying anterior cruciate ligament-deficient knees in adolescents and summarizing the extent of anterior tibial translation and femorotibial internal rotation. Am J Sports Med. 2021;49:928–934. doi: 10.1177/0363546521988938. [DOI] [PubMed] [Google Scholar]
- 21.Hong C.-K., Lin Y.-J., Cheng T.-A., et al. Adult patients with ACL tears have greater tibial internal rotation in MRI compared to adolescent patients. J Orthop Surg Res. 2022;17:17. doi: 10.1186/s13018-022-02912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Albayrak K., Buyukkuscu M.O., Kurk M.B., Kaya O., Kulduk A., Misir A. Leaving the stable ramp lesion unrepaired does not negatively affect clinical and functional outcomes as well as return to sports rates after ACL reconstruction. Knee Surg Sport Traumatol Arthrosc. 2021;29:3773–3781. doi: 10.1007/s00167-020-06402-w. [DOI] [PubMed] [Google Scholar]
- 23.Guy S., Ferreira A., Carrozzo A., et al. Isolated meniscotibial ligament rupture: The medial meniscus “belt lesion.”. Arthrosc Tech. 2022;11:e133–e138. doi: 10.1016/j.eats.2021.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gillquist J., Hagberg G., Oretorp N. Arthroscopic examination of the posteromedial compartment of the knee joint. Int Orthop. 1979;3:13–18. doi: 10.1007/BF00266321. [DOI] [PubMed] [Google Scholar]
- 25.Lee J.Y., Chia Z.Y., Jiang L., Ang B., Chang P. A review of the Gillquist maneuver: Modifications for a safer and easily reproducible approach for knee transintercondylar notch posterior compartment arthroscopy. Arthrosc Tech. 2020;9:e435–e438. doi: 10.1016/J.EATS.2019.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thaunat M., Jan N., Fayard J.M., et al. Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: Outcome study with a minimum 2-year follow-up. Arthroscopy. 2016;32:2269–2277. doi: 10.1016/J.ARTHRO.2016.02.026. [DOI] [PubMed] [Google Scholar]
- 27.Farinelli L., Baldini M., Bucci A., Ulisse S., Carle F., Gigante A. Axial and rotational alignment of lower limb in a Caucasian aged non-arthritic cohort. Eur J Orthop Surg Traumatol. 2021;31:221–228. doi: 10.1007/s00590-020-02763-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Farinelli L., Baldini M., Faragalli A., Carle F., Ulisse S., Gigante A. Surgical epicondylar axis of the knee and its relationship to the axial tibia alignment in knee osteoarthritis: The concept of proximal twist tibia. J Knee Surg. 2023;36:710–715. doi: 10.1055/s-0041-1740998. [DOI] [PubMed] [Google Scholar]
- 29.Kang H. Sample size determination and power analysis using the G∗Power software. J Educ Eval Health Prof. 2021;18:17. doi: 10.3352/jeehp.2021.18.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stuart E.A., Lee B.K., Leacy F.P. Prognostic score-based balance measures can be a useful diagnostic for propensity score methods in comparative effectiveness research. J Clin Epidemiol. 2013;66(suppl):S84–S90.e1. doi: 10.1016/j.jclinepi.2013.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peltier A., Lording T., Maubisson L., Ballis R., Neyret P., Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23:2967–2973. doi: 10.1007/s00167-015-3751-0. [DOI] [PubMed] [Google Scholar]
- 32.DePhillipo N.N., Moatshe G., Chahla J., et al. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: Defining meniscal ramp lesions. Am J Sports Med. 2019;47:372–378. doi: 10.1177/0363546518814258. [DOI] [PubMed] [Google Scholar]
- 33.DePhillipo N.N., Moatshe G., Brady A., et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: A biomechanical study. Am J Sports Med. 2018;46:2422–2431. doi: 10.1177/0363546518774315. [DOI] [PubMed] [Google Scholar]
- 34.DePhillipo N.N. Meniscal ramp lesions: Anatomy, biomechanics and clinical outcomes (PhD Academy Award) Br J Sports Med. 2021;55(5):283LP–284. doi: 10.1136/bjsports-2020-102367. [DOI] [Google Scholar]
- 35.Vieira T.D., Pioger C., Frank F., et al. Arthroscopic dissection of the distal semimembranosus tendon: An anatomical perspective on posteromedial instability and ramp lesions. Arthrosc Tech. 2019;8:e987–e991. doi: 10.1016/j.eats.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cavaignac E., Sylvie R., Teulières M., et al. What is the relationship between the distal semimembranosus tendon and the medial meniscus? A gross and microscopic analysis from the SANTI Study Group. Am J Sports Med. 2021;49:459–466. doi: 10.1177/0363546520980076. [DOI] [PubMed] [Google Scholar]
- 37.Sims W.F., Jacobson K.E. The posteromedial corner of the knee: Medial-sided injury patterns revisited. Am J Sports Med. 2004;32:337–345. doi: 10.1177/0363546503261738. [DOI] [PubMed] [Google Scholar]
- 38.Sonnery-Cottet B., Serra Cruz R., Vieira T.D., Goes R.A., Saithna A. Ramp lesions: An unrecognized posteromedial instability? Clin Sports Med. 2020;39:69–81. doi: 10.1016/j.csm.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 39.Ahn J.H., Bae T.S., Kang K.-S., Kang S.Y., Lee S.H. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med. 2011;39:2187–2193. doi: 10.1177/0363546511416597. [DOI] [PubMed] [Google Scholar]
- 40.Gousopoulos L., Hopper G.P., Saithna A., et al. Suture hook versus all-inside repair for longitudinal tears of the posterior horn of the medial meniscus concomitant to anterior cruciate ligament reconstruction: A matched-pair analysis from the SANTI Study Group. Am J Sports Med. 2022;50:2357–2366. doi: 10.1177/03635465221100973. [DOI] [PubMed] [Google Scholar]
- 41.Hatayama K., Terauchi M., Saito K., Takase R., Higuchi H. Healing status of meniscal ramp lesion affects anterior knee stability after ACL reconstruction. Orthop J Sport Med. 2020;8 doi: 10.1177/2325967120917674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sonnery-Cottet B., Praz C., Rosenstiel N., et al. Epidemiological evaluation of meniscal ramp lesions in 3214 anterior cruciate ligament-injured knees from the SANTI Study Group Database: A risk factor analysis and study of secondary meniscectomy rates following 769 ramp repairs. Am J Sports Med. 2018;46:3189–3197. doi: 10.1177/0363546518800717. [DOI] [PubMed] [Google Scholar]
- 43.Robb C., Kempshall P., Getgood A., et al. Meniscal integrity predicts laxity of anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23:3683–3690. doi: 10.1007/s00167-014-3277-x. [DOI] [PubMed] [Google Scholar]
- 44.Wu W.H., Hackett T., Richmond J.C. Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: A long-term prospective study. Am J Sports Med. 2002;30:845–850. doi: 10.1177/03635465020300061501. [DOI] [PubMed] [Google Scholar]
- 45.Shelbourne K.D., Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med. 2000;28:446–452. doi: 10.1177/03635465000280040201. [DOI] [PubMed] [Google Scholar]
- 46.Costa G.G., Perelli S., Grassi A., Russo A., Zaffagnini S., Monllau J.C. Minimizing the risk of graft failure after anterior cruciate ligament reconstruction in athletes. A narrative review of the current evidence. J Exp Orthop. 2022;9:26. doi: 10.1186/s40634-022-00461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hewison C.E., Tran M.N., Kaniki N., Remtulla A., Bryant D., Getgood A.M. Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: A systematic review of the literature. Arthroscopy. 2015;31(10):2022–2034. doi: 10.1016/j.arthro.2015.04.089. [DOI] [PubMed] [Google Scholar]
- 48.Sonnery-Cottet B., Lutz C., Daggett M., et al. The involvement of the anterolateral ligament in rotational control of the knee. Am J Sports Med. 2016;44:1209–1214. doi: 10.1177/0363546515625282. [DOI] [PubMed] [Google Scholar]
- 49.Sonnery-Cottet B., Saithna A., Blakeney W.G., et al. Anterolateral ligament reconstruction protects the repaired medial meniscus: A comparative study of 383 anterior cruciate ligament reconstructions from the SANTI Study Group with a minimum follow-up of 2 years. Am J Sports Med. 2018;46:1819–1826. doi: 10.1177/0363546518767659. [DOI] [PubMed] [Google Scholar]
- 50.Inderhaug E., Stephen J.M., Williams A., Amis A.A. Anterolateral tenodesis or anterolateral ligament complex reconstruction: Effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med. 2017;45:3089–3097. doi: 10.1177/0363546517724422. [DOI] [PubMed] [Google Scholar]
- 51.Kim S.H., Park Y.-B., Won Y.-S. An increased lateral femoral condyle ratio is an important risk factor for a medial meniscus ramp lesion including red-red zone tear. Arthroscopy. 2021;37(10):3159–3165. doi: 10.1016/j.arthro.2021.03.078. [DOI] [PubMed] [Google Scholar]
- 52.Kunze K.N., Wright-Chisem J., Polce E.M., DePhillipo N.N., LaPrade R.F., Chahla J. Risk factors for ramp lesions of the medial meniscus: A systematic review and meta-analysis. Am J Sports Med. 2021;49:3749–3757. doi: 10.1177/0363546520986817. [DOI] [PubMed] [Google Scholar]
- 53.Park Y.-B., Kim H., Lee H.-J., Baek S.-H., Kwak I.-Y., Kim S.H. The clinical application of machine learning models for risk analysis of ramp lesions in anterior cruciate ligament injuries. Am J Sports Med. 2023;51:107–118. doi: 10.1177/03635465221137875. [DOI] [PubMed] [Google Scholar]
- 54.Cristiani R., van de Bunt F., Kvist J., Stålman A. High prevalence of meniscal ramp lesions in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2023;31:316–324. doi: 10.1007/s00167-022-07135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.DePhillipo N.N., Cinque M.E., Chahla J., Geeslin A.G., Engebretsen L., LaPrade R.F. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:2233–2237. doi: 10.1177/0363546517704426. [DOI] [PubMed] [Google Scholar]
- 56.Balazs G.C., Greditzer H.G., Wang D., et al. Ramp lesions of the medial meniscus in patients undergoing primary and revision ACL reconstruction: Prevalence and risk factors. Orthop J Sport Med. 2019;7:5. doi: 10.1177/2325967119843509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thaunat M., Ingale P., Penet A., et al. Ramp lesion subtypes: Prevalence, imaging, and arthroscopic findings in 2156 anterior cruciate ligament reconstructions. Am J Sports Med. 2021;49:1813–1821. doi: 10.1177/03635465211006103. [DOI] [PubMed] [Google Scholar]
- 58.Willinger L., Balendra G., Pai V., et al. High incidence of superficial and deep medial collateral ligament injuries in “isolated” anterior cruciate ligament ruptures: A long overlooked injury. Knee Surg Sports Traumatol Arthrosc. 2022;30:167–175. doi: 10.1007/s00167-021-06514-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.