Abstract
BACKGROUND
Osteonecrosis of the femoral head (ONFH) is a prevalent orthopedic issue, leading to the collapse and fragmentation of the femoral head in its advanced stages, which can severely impair patients' quality of life. Total hip arthroplasty (THA) is a clinical intervention frequently used to alleviate ONFH symptoms and reinstate hip functionality. The conventional surgical technique is invasive and comes with an extended recuperation period, posing significant challenges for patients. With the progression of medical technology, the use of the mini-incision technique in minimally invasive THA (MITHA) has become more prevalent. However, comparative studies examining the effectiveness of these two surgical procedures in treating ONFH remain scarce. Furthermore, understanding patients' psychological well-being is crucial given its profound influence on postoperative recuperation.
AIM
To evaluate the impact of mini-incision MITHA on ONFH treatment and to identify the risk factors associated with postoperative anxiety and depression.
METHODS
A retrospective study was conducted on 125 patients treated for ONFH at Xi’an Hong Hui Hospital between February 2020 and January 2022, with the term "consecutive" indicating that these patients were treated in an unbroken sequence without any selection. Among these, 60 patients (control group) underwent traditional THA, while 65 patients (observation group) were treated with mini-incision MITHA. Variations in the visual analog scale (VAS) score and the Harris hip score were monitored. Additionally, shifts in pre- and posttreatment Hamilton anxiety (HAMA) and Hamilton depression (HAMD) scale scores were recorded. Patients with both postoperative HAMA and HAMD scores of ≥ 8 were identified as those experiencing negative emotions. Logistic regression was utilized to analyze the determinants influencing these negative emotional outcomes. Comparative analyses of surgical and postoperative metrics between the two groups were also conducted.
RESULTS
Posttreatment results indicated a significantly higher VAS score in the control group than in the observation group, while the Harris score was considerably lower (P < 0.0001). The observation group benefited from a notably shorter operation duration, reduced blood loss, diminished incision size, and a decreased postoperative drainage time (P < 0.0001), accompanied by a reduced hospital stay and lower treatment costs (P < 0.0001). The control group had elevated posttreatment HAMA and HAMD scores in comparison to the observation group (P < 0.0001). Multivariate logistic regression revealed that being female [odds ratio (OR): 4.394, 95%CI: 1.689-11.433, P = 0.002], having a higher postoperative VAS score (OR: 5.533, 95%CI: 2.210-13.848, P < 0.0001), and having higher treatment costs (OR: 7.306, 95%CI: 2.801-19.057, P < 0.0001) were significant independent determinants influencing postoperative mood disturbances.
CONCLUSION
Compared to conventional THA, mini-incision MITHA offers advantages such as reduced operation time, minimal bleeding, and a shorter incision in ONFH patients. Moreover, factors such as sex, postoperative pain (reflected in the VAS score), and treatment costs significantly impact postoperative anxiety and depression.
Keywords: Necrosis of the femoral head, Total hip arthroplasty, Minimally invasive total hip arthroplasty, Postoperative recovery, Anxiety, Depression
Core Tip: Minimally invasive total hip arthroplasty has shown significant advantages in the treatment of osteonecrosis of the femoral head, including a short operation time and less bleeding. However, the psychological stress of postoperative patients, especially female patients, those with high postoperative pain scores, and those with high treatment costs, cannot be ignored as these patients are more susceptible to adverse emotions. Therefore, although improvements in technology and surgical methods are essential, psychological counseling, which can help improve the treatment effect and the quality of life of patients, is equally important.
INTRODUCTION
Necrosis of the femoral head (ONFH) is a disease that causes partial or total ischemia of the femoral head due to blood circulation interruption or injury, which leads to the death of osteocytes, bone marrow hematopoietic cells and adipocytes and may eventually trigger a series of structural changes, such as femoral head collapse[1]. Such a disease is considered to be a disease with a high disability rate in orthopedics[2]. Early diagnosis of ONFH is challenging due to the atypicality of its clinical presentation[3]. As the condition worsens, the femoral head collapses on images, and complete loss of the original femoral head shape occurs in severe cases, which can further develop into degenerative hip osteoarthritis[4]. Therefore, choosing effective treatment methods to improve the patient's condition is critical.
Clinically, total hip arthroplasty (THA) is a common treatment that can achieve joint function reconstruction in patients with ONFH, thus significantly improving patient quality of life[5]. However, conventional THA has some drawbacks, such as a large incision, heavy trauma, and a high incidence of surgical complications[6,7]. Hence, it is necessary to reduce the risk of surgical trauma and complications while ensuring the safety and effectiveness of surgery. In recent years, there has been an increase in the application of minimally invasive THA (MITHA) with the development of minimally invasive technology[8]. This procedure has the advantages of less trauma and quick recovery, which can more effectively help patients relieve pain and restore joint function[9,10]. However, whether MITHA is advantageous over conventional THA with a more significant effect on improving patients' conditions remains to be further studied.
Currently, the treatment of ONFH relies mainly on surgery, which results in a long recovery time, especially for elderly patients. During the recovery period, patients may experience a great reduction or even loss of self-care ability, as well as varying degrees of motor system damage. These factors have placed great pressure on the physiology and psychology of patients, predisposing them to psychological stress and negative emotions (NEs).
Accordingly, the purpose of this study was to explore the effect of MITHA in the treatment of ONFH and to analyze the risk factors that may affect postoperative anxiety and depression. This study can provide more rigorous evidence for clinical treatment and intervention, with important practical significance for improving patient quality of life and mental health.
MATERIALS AND METHODS
Patient data
A retrospective analysis was performed on 125 ONFH patients who were treated at Xi’an Hong Hui Hospital from February 2020 to January 2022. Among them, 60 patients who received conventional THA and 65 patients who received MITHA were assigned to the control group and observation group, respectively.
Eligibility and exclusion criteria
The inclusion criteria were as follows: (1) Patients whose physical condition was at an acceptable level and with an American Association of Anesthesiologists score ranging from 1 to 3 points[11]; (2) Those meeting the indications for THA; (3) Diagnosis of CNFH by imaging examination; (4) Awareness of and voluntary participation in the study by patients and their families; (5) Unilateral lesions that met surgical indications; and (6) Complete clinical data.
The exclusion criteria were as follows: (1) Severe cardio-cerebrovascular diseases and other chronic wasting diseases; (2) Multiple hip replacement procedures; (3) Concurrent surgery of other parts; (4) Incomplete information or loss to follow-up; or (5) Active infection in the affected hip or surgical area.
Treatment methods
Patients in the control group underwent conventional THA. The procedure was performed under general anesthesia with the patient placed in a lateral decubitus position. After successful anesthesia, the surgeon successively cut the skin of the patient to expose the femoral head and the acetabulum edge, viewing the acetabulum damage and repairing it. Then, an appropriate prosthesis was selected for implantation according to the patient’s specific condition. After confirmation of the correct placement of the implant, the surgeon cleaned the incision and placed a drainage tube to complete the procedure.
Patients in the observation group underwent MITHA using a mini-incision technique, with the anesthesia method and surgical position the same as the control group. During the operation, the surgeon made a small incision of 6 to 10 cm along the gluteus maximus muscle fibers on the posterior side of the greater trochanter of the femur. The gluteus maximus muscle was then cut open, and the external rotators at the attachment of the trochanter were cut off and pulled posteriorly so that the joint capsule could be exposed for incision to expose the femoral head and acetabulum. Then, within 10 to 15 cm of the femur, the surgeon used a chainsaw to cut the neck of the femur and remove the severed femoral head. Next, the stump of the ligamentum teres of the acetabulum and the glenoid lip were removed, and the exposed ligamentum teres fossa was ground flat. At the same time, reaming was performed on the acetabulum with an anteversion angle of 20° and an abduction angle of 45°. Then, a prosthesis with a suitable size was selected for a trial mold, and the prosthesis was implanted after confirming its stability and tightness. At the end of the surgery, the surgeon drilled 3 to 4 holes in the suture of the external rotators, washed the operation field and placed a drainage tube to end the operation. Both groups received routine anti-infection therapy after surgery.
Clinical data collection
The following information was collected: (1) Clinical data, namely, age, sex, body mass index (BMI), pathogeny, affected side, smoking history, alcoholism history, education level, annual income and marital status; (2) Surgical indicators, namely, operation time, intraoperative blood loss, incision length, and postoperative drainage time; (3) Postoperative indicators, namely, length of stay and treatment cost; (4) Scoring indices, namely, visual analog scale (VAS) scores[11] and Harris hip score (HHS) before and after operation; and (5) Pre- and posttreatment Hamilton anxiety and depression scale scores, namely, the Hamilton anxiety scale (HAMA) and Hamilton depression scale (HAMD) scores[12].
Outcome measures
Primary outcome measures: Changes in VAS and HHS scores before and after treatment were observed. Alterations in pre- and posttreatment HAMA and HAMD scores were compared between the two groups. According to postoperative scores, patients with both HAMA and HAMD scores ≥ 8 were considered to have NEs, and the risk factors affecting the occurrence of NEs were analyzed by logistic regression.
Secondary outcome measures: Clinical data, surgical indicators and postoperative indicators were compared.
Statistical analysis
SPSS 26.0 and GraphPad Prism 9 were used for data analysis, and the threshold of statistical significance was P < 0.05. Count data are expressed as frequencies (percentages), and comparisons between groups were made by means of the χ2 test. Measurement data are expressed as the mean ± SD. Two independent samples t tests were used for comparisons between groups, independent samples t tests were used for comparisons between groups, and paired t tests were used for comparisons within groups. Logistic regression was used to analyze the risk factors affecting patients' NEs.
RESULTS
Comparison of clinical data
In the comparisons of the patients’ clinical data, it was found that the observation and control groups were not significantly different in age, sex, BMI, pathogeny, affected side, smoking history, alcoholism history, education level, annual income, or marital status (P > 0.05, Table 1).
Table 1.
Comparison of clinical data
|
Factors
|
|
Control group (n = 60)
|
Observation group (n = 65)
|
P value
|
| Age | 0.569 | |||
| ≥ 60 years old | 34 | 40 | ||
| < 60 years old | 26 | 25 | ||
| Sex | 0.650 | |||
| Male | 34 | 40 | ||
| Female | 26 | 25 | ||
| BMI | 0.503 | |||
| ≥ 25 kg/m2 | 15 | 13 | ||
| < 25 kg/m2 | 45 | 52 | ||
| Pathogeny | 0.434 | |||
| Trauma | 29 | 22 | ||
| Hormone | 20 | 27 | ||
| Alcohol | 7 | 10 | ||
| Others | 4 | 6 | ||
| Affected side | 0.264 | |||
| Left | 27 | 36 | ||
| Right | 33 | 29 | ||
| Smoking history | 0.650 | |||
| With | 34 | 40 | ||
| Without | 26 | 25 | ||
| History of alcoholism | 0.444 | |||
| With | 5 | 8 | ||
| Without | 55 | 57 | ||
| Education level | 0.490 | |||
| ≥ Junior high school | 25 | 23 | ||
| < Junior high school | 35 | 42 | ||
| Annual income | 0.531 | |||
| ≥ 50000 CNY | 18 | 16 | ||
| < 50000 CNY | 42 | 49 | ||
| Marital status | 0.569 | |||
| Married | 44 | 50 | ||
| Divorced | 9 | 10 | ||
| Others | 7 | 5 |
BMI: Body mass index.
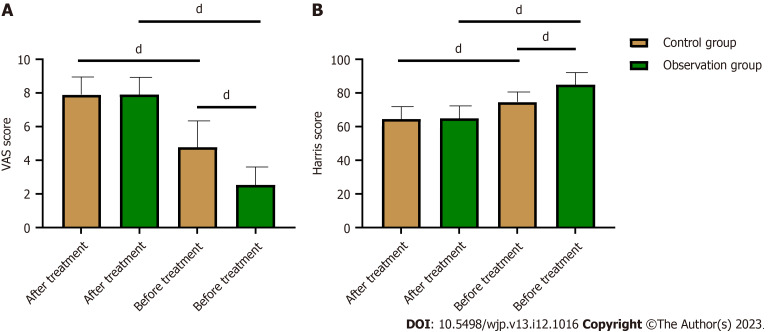
Changes in pain and functional scores
Changes in VAS and HHS scores before and after treatment were compared between groups. The two groups did not differ significantly in terms of their pretreatment VAS or HHS scores (P > 0.05). A reduction in the VAS score and an increase in the HHS score were observed in both groups after treatment (P < 0.0001). Further intergroup comparison revealed a higher VAS score and a lower HHS score in the control group than in the observation group (P < 0.0001, Figure 1).
Figure 1.
Changes of visual analogue scales and Harris hip score scores in patients before and after treatment. A: Comparison of visual analogue scales score; B: Comparison of Harris hip score; VAS: Visual analogue scales. dP < 0.0001.
Comparison of surgical indices
The intergroup comparison of surgical indices showed that the operation time was significantly shorter in the observation group than in the control group, with less intraoperative blood loss, shorter incision length, and less postoperative drainage time (P < 0.0001, Figure 2).
Figure 2.
Comparison of surgical indexes. A: Comparison of operation time; B: Comparison of intraoperative blood loss; C: Comparison of incision length; D: Comparison of postoperative drainage time. dP<0.0001.
Comparison of postoperative indices
Comparing the postoperative indices, it was found that the length of stay and treatment cost of patients were significantly lower in the observation group than in the control group (P < 0.0001, Figure 3).
Figure 3.
Comparison of postoperative indexes. A: Comparison of length of stay; B: Comparison of treatment cost. dP<0.0001.
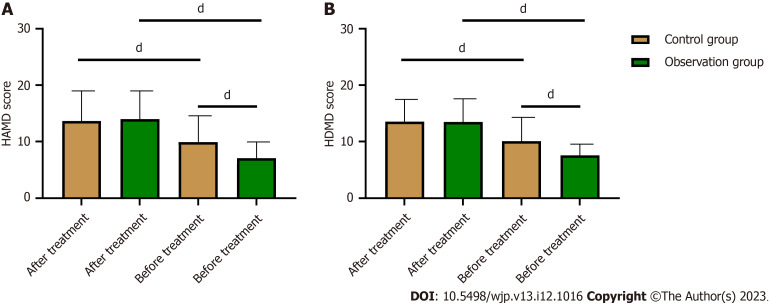
Evaluation of patients' NEs
Patients’ anxiety and depression were evaluated before and after treatment. There were no significant difference in the pretreatment HAMA or HAMD scores between the two groups (P > 0.05). However, significantly reduced HAMA and HAMD scores were observed in both groups after treatment (P < 0.0001). Further comparison showed that the posttreatment HAMA and HAMD scores were significantly higher in the control group than in the observation group (P < 0.0001, Figure 4).
Figure 4.
Changes of Hamilton anxiety scale and Hamilton depression scale scores before and after treatment. A: Comparison of Hamilton anxiety scale score; B: Comparison of Hamilton depression scale score. HAMA: Hamilton anxiety scale; HAMD: Hamilton depression scale. dP<0.0001.
Analysis of risk factors affecting patients' NEs
We conducted a statistical evaluation of the postoperative HAMA and HAMD scores. Using a screening threshold of a postoperative score ≥ 8, we identified 71 patients exhibiting postoperative anxiety and 77 manifesting postoperative depression. Based on these findings, patients were categorized into two distinct groups: the NE group (n = 71) and the emotional stability group (n = 54). In the univariate analysis, several factors emerged as potential risk determinants affecting patients' NEs. These included age ≥ 60 years, female sex, an education level below middle school, an annual income less than 50000 CNY, opting for the conventional surgical plan, elevated postoperative VAS scores, prolonged operation times, and increased treatment costs (P < 0.05, Table 2). To refine our understanding, we assigned numerical values to the identified variables, as shown in Table 3. Our subsequent multivariate logistic regression analysis highlighted three prominent factors. Specifically, being female, having a higher postoperative VAS score, and incurring elevated treatment costs were significant independent risk factors influencing postoperative NEs in patients (P < 0.01, Table 4).
Table 2.
Univariate analysis
|
Factors
|
Negative emotion group (n = 71)
|
Emotional stability group (n = 54)
|
P value
|
|
| Age | 0.002b | |||
| ≥ 60 years old | 50 | 24 | ||
| < 60 years old | 21 | 30 | ||
| Sex | 0.003b | |||
| Male | 34 | 40 | ||
| Female | 37 | 14 | ||
| BMI | 0.460 | |||
| ≥ 25kg/m2 | 14 | 14 | ||
| < 25kg/m2 | 57 | 40 | ||
| Pathogeny | 0.423 | |||
| Trauma | 33 | 18 | ||
| Hormone | 25 | 22 | ||
| Alcohol | 9 | 8 | ||
| Others | 4 | 6 | ||
| Affected side | 0.937 | |||
| Left | 36 | 27 | ||
| Right | 35 | 27 | ||
| Smoking history | 0.060 | |||
| With | 37 | 37 | ||
| Without | 34 | 17 | ||
| History of alcoholism | 0.866 | |||
| With | 7 | 6 | ||
| Without | 64 | 48 | ||
| Education level | 0.026a | |||
| ≥ Junior high school | 21 | 27 | ||
| < Junior high school | 50 | 27 | ||
| Annual income | 0.038a | |||
| ≥ 50000 CNY | 14 | 20 | ||
| < 50000 CNY | 57 | 34 | ||
| Marital status | 0.752 | |||
| Married | 52 | 42 | ||
| Divorced | 11 | 8 | ||
| Others | 8 | 4 | ||
| Treatment methods | 0.032 | |||
| Minimally invasive | 31 | 34 | ||
| Conventional | 40 | 20 | ||
| Postoperative VAS score | 4.28 ± 1.59 | 2.70 ± 1.50 | < 0.0001d | |
| Postoperative harris hip score | 79.50 ± 8.06 | 80.33 ± 8.77 | 0.585 | |
| Operation time (min) | 95.69 ± 8.36 | 92.63 ± 7.18 | 0.033a | |
| Intraoperative blood loss (mL) | 14.15 ± 3.89 | 11.57 ± 4.23 | 0.074 | |
| Incision length (cm) | 436.59 ± 190.14 | 441.17 ± 210.32 | 0.898 | |
| Postoperative drainage time (min) | 459.11 ± 203.95 | 343.56 ± 192.78 | 0.075 | |
| Length of stay (d) | 11.26 ± 2.96 | 12.29 ± 4.16 | 0.109 | |
| Treatment cost (CNY) | 40006.21 ± 5472.16 | 34272.05 ± 6033.42 | < 0.0001d | |
P < 0.05.
P < 0.01.
P < 0.0001.
BMI: Body mass index; VAS: Visual analogue scales.
Table 3.
Assignment table
|
Factors
|
Assignment
|
| Age | ≥ 60 years old = 1, < 60 years old = 0 |
| Sex | Male = 0, female = 1 |
| Education level | ≥ Junior high school = 0, < Junior high school = 1 |
| Annual income | ≥ 50000 CNY = 0, < 50000 CNY = 1 |
| Surgical plan | Minimally invasive = 0, conventional = 1 |
| Postoperative VAS score | ≥ 4 = 1, < 4 = 0 |
| Operation time | ≥ 95 min = 1, < 95 min = 0 |
| Treatment cost | ≥ 35000 CNY = 1, < 35000 CNY = 0 |
| Anxiety and depression | Negative emotion group = 1, emotional stability group = 0 |
VAS: Visual analogue scales.
Table 4.
Multivariate analysis
|
Factors
|
β
|
Standard error
|
χ
2
|
P value
|
OR
|
95%CI
|
|
|
Lower bound
|
Upper bound
|
||||||
| Age | 0.578 | 0.465 | 1.545 | 0.214 | 1.782 | 0.716 | 4.434 |
| Sex | 1.480 | 0.488 | 9.206 | 0.002b | 4.394 | 1.689 | 11.433 |
| Education level | 0.809 | 0.462 | 3.064 | 0.080 | 2.246 | 0.908 | 5.557 |
| Annual income | 0.704 | 0.521 | 1.829 | 0.176 | 2.023 | 0.729 | 5.614 |
| Surgical plan | 0.183 | 0.487 | 0.141 | 0.707 | 1.201 | 0.462 | 3.120 |
| Postoperative VAS score | 1.711 | 0.468 | 13.354 | <0.001c | 5.533 | 2.210 | 13.848 |
| Operation time | 0.643 | 0.494 | 1.695 | 0.193 | 1.902 | 0.723 | 5.004 |
| Treatment cost | 1.989 | 0.489 | 16.532 | <0.001c | 7.306 | 2.801 | 19.057 |
P < 0.01.
P < 0.001.
VAS: Visual analog scales; OR: Odds ratio.
DISCUSSION
ONFH is a common condition in orthopedics with symptoms such as femoral head collapse and fragmentation in the later stage, which can cause great pain to patients and even loss of mobility[13]. The interruption of the blood supply to the femoral head leads to the production of free radicals, as well as hypoxia and reperfusion injury, which can accelerate osteocyte death and eventually lead to the necrosis of bone marrow stromal stem cells or the formation of adipocytes, leading to local osteoporosis[14]. Hip replacement has been clinically shown to be an effective method to relieve hip pain and restore hip function in ONFH patients[15]. However, this procedure is highly invasive and is associated with a long postoperative recovery period and long-term bed rest, which increases the difficulty of rehabilitation training and the risk of developing lower extremity deep venous thrombosis, affecting postoperative rehabilitation.
The development of minimally invasive surgery technology has enabled the gradual application and popularization of mini-incision MITHA in clinical practice[16]. In addition, the rapid development of medical technology and equipment has made it possible to improve and optimize the incision method of THA[17]. In long-term clinical practice, mini-incision THA has become a standard surgical approach with many advantages. However, little has been reported about the difference between conventional and minimally invasive THA procedures for the treatment of ONFH. Repantis et al[18] found no significant difference in intraoperative blood loss between the two THA methods but identified markedly lower postoperative pain scores in the minimally invasive group. The present study also comparatively analyzed the two surgical modalities and found a significantly shorter operation time in patients undergoing MITHA vs those receiving conventional THA, with less intraoperative bleeding, a shorter incision length, less surface peeling and clear joint exposure, which greatly shortened the operation time and reduced the body's traumatic stress response.
For patients with either osteoporotic fracture or ONFH, THA will cause psychological stress and cause greater psychological pressure[19]. Anxiety and depression are the most common psychological complications, both of which have a certain impact on patients' cognitive and psychological states[19,20]. In addition, anxiety and depression can significantly reduce patients' motivation and adherence to treatment during hospitalization, leading to a significant decline in treatment effectiveness. Evidence has shown that psychological factors have an impact on the outcome of THA[21]. In contrast, a good state of mind helps patients recover as quickly as possible. Therefore, identifying factors that influence anxiety and depression helps clinical medical staff to take relevant nursing measures and carry out targeted treatment in time. In our study, anxiety and depression were found before surgery in both groups and were relieved in some patients after treatment. To determine the risk factors for postoperative NEs in ONFH patients, we performed a regression analysis. The results showed that sex, postoperative VAS score, and treatment cost were risk factors for postoperative NEs in ONFH patients. The reason may be that women, who are affected by psychological and physiological characteristics, are more sensitive and emotional and therefore more susceptible to NEs after illness. In addition, the activity limitation of postsurgical patients leads to aggravated depression and anxiety. In the research of Liu and Wang[22], the incidence of anxiety and depression increased significantly among female patients after gastric cancer surgery and was related to poor prognosis, which was the main risk factor. Pain itself is a kind of physical discomfort that can negatively affect the individual's mood and behavior. Pain can also lead to decreased sleep quality, further aggravating the patient's emotional distress. Persistent pain can cause the patient to worry about the prospect of future recovery, exacerbating anxiety and depression. Park et al[23] suggested that severe postoperative pain was a risk factor for postoperative anxiety and depression in patients with lung cancer. Although ONFH does not require long-term treatment, conventional replacement surgery is not affordable for all families, increasing the financial burden on patients’ families. In addition, from the perspective of the patients, the psychological pressure felt is enormous due to fear of becoming a burden to their families. They may also worry that they will not be able to pay for medical expenses in the long term and that follow-up treatment will be difficult to guarantee, resulting in negative feelings such as guilt and anxiety[24,25]. Therefore, to improve patients' psychological states, it is necessary to strengthen communication with patients and encourage them to express their inner thoughts. For patients with NEs, targeted psychological counseling can be implemented to help relieve stress. In addition, those patients with effectively controlled conditions after treatment and a good state of mind can be invited to share their treatment experiences and exchange opinions on overcoming difficulties. Such measures are helpful to improve patients' confidence in treatment and prevent the occurrence of NEs.
In this study, we determined the therapeutic effect of MITHA on ONFH patients and the risk factors for postoperative NEs through analyses. However, this study still has some limitations. First, the insufficient sample size may lead to errors in the results of the regression analysis. Second, patients’ long-term follow-up cannot be determined due to the retrospective nature of this study, resulting in uncertainty regarding the long-term outcomes of patients treated by the two surgical methods. Finally, as a single-center study, the applicability and generalizability of the results of this study need to be validated and supported by external data. Therefore, the hope is that more in-depth research can be carried out in the future and that more samples will be collected to support the conclusions of this study.
CONCLUSION
In this paper, the application and clinical effectiveness of THA in ONFH patients, particularly the influence of MITHA on patients’ treatment outcomes, were studied. The results show that MITHA contributes to a shorter operation time, less blood loss and a shorter incision length. At the same time, anxiety and depression before surgery were prevalent in all patients, and these NEs may be related to the patient's sex, postoperative pain score, and treatment cost.
ARTICLE HIGHLIGHTS
Research background
Osteonecrosis of the femoral head (ONFH) is a complex and multifactorial disease, which can seriously affect the quality of life of patients at the advanced stage. Although conventional total hip arthroplasty (THA) is effective in relieving symptoms, the procedure is invasive, resulting in a long recovery period for patients. Minimally invasive THA (MITHA) has begun to be used clinically with the development of minimally invasive techniques.
Research motivation
There is a lack of studies comparing MITHA with conventional THA, especially its effects on postoperative pain, recovery, and psychological distress in patients with ONFH.
Research objectives
This study aims to compare the effects of MITHA vs conventional THA in patients with ONFH and to further explore risk factors for postoperative negative emotions (NEs).
Research methods
The two surgical methods were comparatively analyzed, and the emotional state of the patients before and after surgery was investigated and analyzed using the regression model.
Research results
Patients undergoing MITHA had shorter operation time, less intraoperative bleeding and smaller incision length. Both groups of patients developed anxiety and depression before surgery, but some of them experienced emotional relief after treatment. Sex, postoperative pain score, and treatment cost were identified as risk factors affecting postoperative NEs of ONFH patients.
Research conclusions
MITHA is obvious advantageous over conventional THA in the treatment of ONFH, with short operation time and less bleeding. Sex, postoperative pain score, and treatment cost are risk factors that affect patients' postoperative mood. Targeted psychological counseling can effectively relieve the pressure of patients.
Research perspectives
A larger sample size and a long-term patient follow-up are needed to further determine the long-term effects of MITHA, as well as the depth and durability of the psychological impact on patients. Meanwhile, we need to better understand and deal with patients' postoperative psychological problems to improve the overall effectiveness of treatment.
Footnotes
Institutional review board statement: This study was approved by the Institutional Review Board of the Xi’an Hong Hui Hospital.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: August 30, 2023
First decision: September 13, 2023
Article in press: November 8, 2023
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Madigan S, Canada; Rathipriya AG, United States S-Editor: Li L L-Editor: A P-Editor: Xu ZH
Contributor Information
Wen-Xing Yu, Osteonecrosis and Joint Reconstruction Ward, Xi’an Hong Hui Hospital, Xi'an Jiaotong University, Xi’an 710054, Shaanxi Province, China.
Yang-Quan Hao, Osteonecrosis and Joint Reconstruction Ward, Xi’an Hong Hui Hospital, Xi'an Jiaotong University, Xi’an 710054, Shaanxi Province, China.
Chao Lu, Osteonecrosis and Joint Reconstruction Ward, Xi’an Hong Hui Hospital, Xi'an Jiaotong University, Xi’an 710054, Shaanxi Province, China.
Hui Li, Osteonecrosis and Joint Reconstruction Ward, Xi’an Hong Hui Hospital, Xi'an Jiaotong University, Xi’an 710054, Shaanxi Province, China.
Yuan-Zhen Cai, Osteonecrosis and Joint Reconstruction Ward, Xi’an Hong Hui Hospital, Xi'an Jiaotong University, Xi’an 710054, Shaanxi Province, China. bonny17173@163.com.
Data sharing statement
The data for this study can be obtained from the corresponding author upon request at bonny17173@163.com.
References
- 1.Hines JT, Jo WL, Cui Q, Mont MA, Koo KH, Cheng EY, Goodman SB, Ha YC, Hernigou P, Jones LC, Kim SY, Sakai T, Sugano N, Yamamoto T, Lee MS, Zhao D, Drescher W, Kim TY, Lee YK, Yoon BH, Baek SH, Ando W, Kim HS, Park JW. Osteonecrosis of the Femoral Head: an Updated Review of ARCO on Pathogenesis, Staging and Treatment. J Korean Med Sci. 2021;36:e177. doi: 10.3346/jkms.2021.36.e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen-Rosenblum A, Cui Q. Osteonecrosis of the Femoral Head. Orthop Clin North Am. 2019;50:139–149. doi: 10.1016/j.ocl.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 3.George G, Lane JM. Osteonecrosis of the Femoral Head. J Am Acad Orthop Surg Glob Res Rev. 2022;6 doi: 10.5435/JAAOSGlobal-D-21-00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mont MA, Salem HS, Piuzzi NS, Goodman SB, Jones LC. Nontraumatic Osteonecrosis of the Femoral Head: Where Do We Stand Today?: A 5-Year Update. J Bone Joint Surg Am. 2020;102:1084–1099. doi: 10.2106/JBJS.19.01271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karachalios TS, Koutalos AA, Komnos GA. Total hip arthroplasty in patients with osteoporosis. Hip Int. 2020;30:370–379. doi: 10.1177/1120700019883244. [DOI] [PubMed] [Google Scholar]
- 6.Galakatos GR. Direct Anterior Total Hip Arthroplasty. Mo Med. 2018;115:537–541. [PMC free article] [PubMed] [Google Scholar]
- 7.Lu M, Phillips D. Total Hip Arthroplasty for Posttraumatic Conditions. J Am Acad Orthop Surg. 2019;27:275–285. doi: 10.5435/JAAOS-D-17-00775. [DOI] [PubMed] [Google Scholar]
- 8.Migliorini F, Pintore A, Eschweiler J, Oliva F, Hildebrand F, Maffulli N. Factors influencing the outcomes of minimally invasive total hip arthroplasty: a systematic review. J Orthop Surg Res. 2022;17:281. doi: 10.1186/s13018-022-03168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Migliorini F, Biagini M, Rath B, Meisen N, Tingart M, Eschweiler J. Total hip arthroplasty: minimally invasive surgery or not? Meta-analysis of clinical trials. Int Orthop. 2019;43:1573–1582. doi: 10.1007/s00264-018-4124-3. [DOI] [PubMed] [Google Scholar]
- 10.Koutserimpas C, Raptis K, Tsakalou D, Karaiskos I, Kourelis K. Anterolateral Minimally Invasive Total Hip Arthroplasty: Pitfalls During the Learning Curve and Clinical Outcomes. Maedica (Bucur) 2021;16:394–399. doi: 10.26574/maedica.2021.16.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kivrak S, Haller G. Scores for preoperative risk evaluation of postoperative mortality. Best Pract Res Clin Anaesthesiol. 2021;35:115–134. doi: 10.1016/j.bpa.2020.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg LI. The Ham-D is not Hamilton's Depression Scale. Psychopharmacol Bull. 2022;52:117–153. [PMC free article] [PubMed] [Google Scholar]
- 13.Shi W, Zhang X, Xu C, Pang R, Fan Z, Wan X, Jiang Z, Li H, Li Z, Zhang H. Identification of Hub Genes and Pathways Associated with Oxidative Stress of Cartilage in Osteonecrosis of Femoral Head Using Bioinformatics Analysis. Cartilage. 2022;13:19476035221074000. doi: 10.1177/19476035221074000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen K, Liu Y, He J, Pavlos N, Wang C, Kenny J, Yuan J, Zhang Q, Xu J, He W. Steroid-induced osteonecrosis of the femoral head reveals enhanced reactive oxygen species and hyperactive osteoclasts. Int J Biol Sci. 2020;16:1888–1900. doi: 10.7150/ijbs.40917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nan K, Pei JP, Fan LH, Zhang YK, Zhang X, Liu K, Shi ZB, Dang XQ, Wang KZ. Resveratrol prevents steroid-induced osteonecrosis of the femoral head via miR-146a modulation. Ann N Y Acad Sci. 2021;1503:23–37. doi: 10.1111/nyas.14555. [DOI] [PubMed] [Google Scholar]
- 16.Clesham K, Sheridan GA, Greidanus NV, Masri BA, Garbuz DS, Duncan CP, Howard LC. Minimally Invasive Intermuscular Approaches Versus Conventional Approaches in Total Hip Arthroplasty: A Systematic Review and Meta-Analysis. J Arthroplasty. 2022;37:1658–1666. doi: 10.1016/j.arth.2022.03.071. [DOI] [PubMed] [Google Scholar]
- 17.Lenze F, Hinterwimmer F, Fleckenstein L, Lazic I, Dammerer D, VON Eisenhart-Rothe R, Harrasser N, Pohlig F. Minimally Invasive Total Hip Arthroplasty: A Comparison of Restoring Hip Biomechanics With and Without a Traction Table. In Vivo. 2022;36:424–429. doi: 10.21873/invivo.12720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Repantis T, Bouras T, Korovessis P. Comparison of minimally invasive approach versus conventional anterolateral approach for total hip arthroplasty: a randomized controlled trial. Eur J Orthop Surg Traumatol. 2015;25:111–116. doi: 10.1007/s00590-014-1428-x. [DOI] [PubMed] [Google Scholar]
- 19.Zalikha AK, Karabon P, Hajj Hussein I, El-Othmani MM. Anxiety and Depression Impact on Inhospital Complications and Outcomes After Total Knee and Hip Arthroplasty: A Propensity Score-Weighted Retrospective Analysis. J Am Acad Orthop Surg. 2021;29:873–884. doi: 10.5435/JAAOS-D-20-00721. [DOI] [PubMed] [Google Scholar]
- 20.Pan X, Wang J, Lin Z, Dai W, Shi Z. Depression and Anxiety Are Risk Factors for Postoperative Pain-Related Symptoms and Complications in Patients Undergoing Primary Total Knee Arthroplasty in the United States. J Arthroplasty. 2019;34:2337–2346. doi: 10.1016/j.arth.2019.05.035. [DOI] [PubMed] [Google Scholar]
- 21.Kazarian GS, Anthony CA, Lawrie CM, Barrack RL. The Impact of Psychological Factors and Their Treatment on the Results of Total Knee Arthroplasty. J Bone Joint Surg Am. 2021;103:1744–1756. doi: 10.2106/JBJS.20.01479. [DOI] [PubMed] [Google Scholar]
- 22.Liu P, Wang Z. Postoperative anxiety and depression in surgical gastric cancer patients: their longitudinal change, risk factors, and correlation with survival. Medicine (Baltimore) 2022;101 doi: 10.1097/MD.0000000000028765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park S, Kang CH, Hwang Y, Seong YW, Lee HJ, Park IK, Kim YT. Risk factors for postoperative anxiety and depression after surgical treatment for lung cancer†. Eur J Cardiothorac Surg. 2016;49:e16–e21. doi: 10.1093/ejcts/ezv336. [DOI] [PubMed] [Google Scholar]
- 24.Aggarwal A, Naylor JM, Adie S, Liu VK, Harris IA. Preoperative Factors and Patient-Reported Outcomes After Total Hip Arthroplasty: Multivariable Prediction Modeling. J Arthroplasty. 2022;37:714–720.e4. doi: 10.1016/j.arth.2021.12.036. [DOI] [PubMed] [Google Scholar]
- 25.Stone AH, MacDonald JH, King PJ. The Effect of Psychiatric Diagnosis and Psychotropic Medication on Outcomes Following Total Hip and Total Knee Arthroplasty. J Arthroplasty. 2019;34:1918–1921. doi: 10.1016/j.arth.2019.04.064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data for this study can be obtained from the corresponding author upon request at bonny17173@163.com.