Abstract
BACKGROUND
Sarcoidosis is a multisystem disease characterized by granuloma formation in various organs. Sarcoidosis-related flexor tendon contractures are uncommon in clinical settings. This contracture is similar to stenosing tenosynovitis and potentially leads to misdiagnosis and mistreatment. Herein, we report a rare case of sarcoidosis-related finger flexor tendon contracture that was misdiagnosed as tenosynovitis.
CASE SUMMARY
A 44-year-old woman presented to our department with flexion contracture of the right ring and middle fingers. The patient was misdiagnosed with tenosynovitis and underwent acupotomy release of the A1 pulley of the middle finger in another hospital that resulted in iatrogenic rupture of both the superficial and profundus flexors. Radiological presentation showed multiple sarcoid involvements in the pulmonary locations and ipsilateral forearm. A diagnosis of sarcoidosis was made based on the presence of non-caseating granulomas with tubercles consisting of Langhans giant cells with lymphocyte infiltration on biopsy, and the patient underwent surgical repair for the contracture. After 2 mo, the patient experienced another spontaneous rupture of the repaired middle finger tendon and underwent surgical re-repair. Satisfactory results were achieved at the 10 mo follow-up after reoperation.
CONCLUSION
Sarcoidosis-related finger contractures are rare; thus, caution should be exercised when dealing with such patients to avoid incorrect treatment.
Keywords: Sarcoidosis, Finger, Contracture, Iatrogenic, Misdiagnosis, Case report
Core Tip: Finger contracture due to tenosynovitis is frequently encountered in clinical settings. However, misdiagnosis can occur when rare causes such as sarcoidosis are neglected. Here, we report a case in which such a misdiagnosis led to an iatrogenic injury. The mainstream treatment method for contractures related to sarcoidosis is surgical excision of muscular lesions, with varied outcomes in several case reports. In our case, considering the contracture lesion at the flexor digitorum profundus (FDP) and the initial iatrogenic tendon rupture, cross-lengthening of the flexor digitorum superficialis and FDP was attempted to restore flexion and achieve satisfactory results.
INTRODUCTION
Granulomatous involvement of the skeletal muscles (also known as granulomatous myopathy) is common in patients with sarcoidosis, and most cases are asymptomatic[1]. However, cases of finger flexion contractures are extremely rare. To the best of our knowledge, only a few cases of such contractures have been reported in the English literature[2-6].
Contracture of finger flexors is frequently observed in tenosynovitis (also known as trigger finger) in clinical settings[7]. Trigger finger is caused by inflammation and constriction of the retinacular sheath through which the flexor tendons run as they pass from the palm of the hand to the finger, leading to pain and movement restriction. The management of tenosynovitis is well established, ranging from conservative to surgical treatment[7-9]. Because finger contractures of other causes, such as sarcoidosis, are rare, misdiagnosis of tenosynovitis could occur, leading to empirical treatment with poor outcomes or severe complications.
Herein, we present a patient with finger contractures who was misdiagnosed with trigger finger and received acupotomy release[10,11] (similar to percutaneous release), resulting in iatrogenic rupture of both the superficial and profundus flexors of the right middle finger. We also conducted a systematic literature review of finger contractures caused by sarcoidosis.
CASE PRESENTATION
Chief complaints
A 44-year-old healthy woman presented to our hand surgery department with spontaneous flexor tendon rupture of the right middle finger and contracture of the right ring finger.
History of present illness
The patient was diagnosed with tenosynovitis of the right ring finger and middle finger at a local hospital and underwent acupotomy release of her middle finger 2 wk prior to admission. Five days after the release, a sudden complete loss of active flexion of the right middle finger was observed during routine domestic activities. Two months after the surgery, re-rupture of the repaired middle finger tendon was encountered when the patient was pulling on her pants.
History of past illness
The patient denied any past illnesses.
Personal and family history
The patient denied any personal or family history of related diseases.
Physical examination
Loss of active flexion of the right middle finger and contracture of the right ring finger were observed. There was no swelling, tenderness, or numbness of the digits. No other positive findings were observed during systematic physical examination. During the operation, all lacerations of the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) of the right middle finger were identified in Zone II around the metacarpophalangeal (MCP) joint (Figure 1). Significantly, a high level of tension and loss of elasticity were observed at the proximal end of the FDP, whereas the proximal FDS seemed normal in tension and elasticity.
Figure 1.
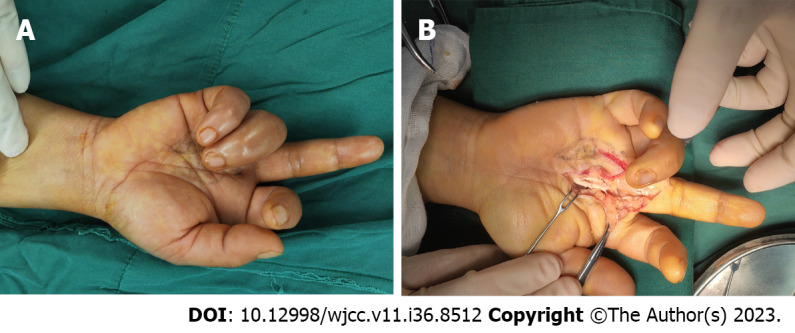
Findings during the first surgery. A: The extended middle finger and flexed ring finger before exploration; B: Intraoperative view of the rupture of both flexor digitorum superficialis and flexor digitorum profundus tendon at the metacarpophalangeal joint of the middle finger.
Laboratory examinations
Initial laboratory studies revealed high alkaline phosphatase (116 U/L, normal range: 35–100 U/L) and normal serum creatinine, creatine phosphokinase, and calcium levels. No further positive findings were noted in the laboratory examinations.
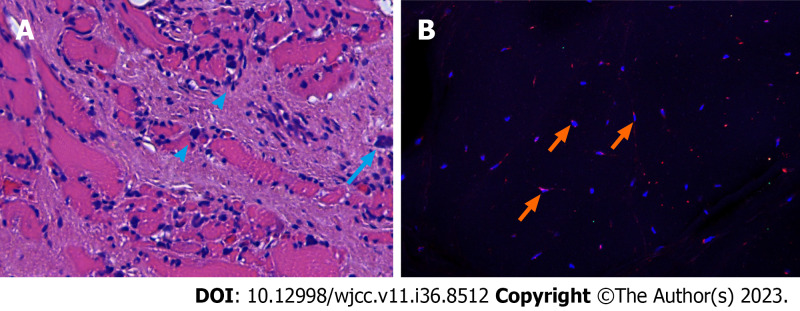
Histopathology revealed granulomatous involvement in the FDP muscles and tendons, showing a typical sarcoid shape with tubercles consisting of Langhans' giant cells and lymphocytes (Figure 2).
Figure 2.
Results of hematoxylin and eosin staining and immunofluorescence staining of the flexor digitorum profundus muscle. A: Interstitial diffuse infiltration of scattered lymphocytes (arrowheads) and multinucleated giant cells (arrow) in the muscle tissue; B: The cells were stained for nuclei (DAPI, blue) and CD68 (red). This highlights the giant cells that are positively immunostained for CD68 (arrows).
Imaging examinations
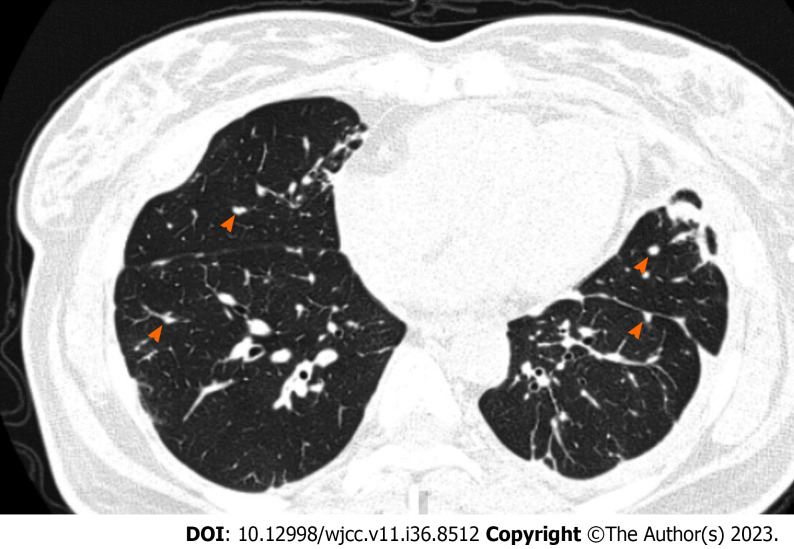
High-resolution computed tomography (CT) revealed widespread nodules in both the lungs (Figure 3).
Figure 3.
High-resolution computed tomographic section showing widespread nodules (arrowheads) in both lungs.
Magnetic resonance imaging (MRI) revealed a central dark star surrounded by a peripheral high-signal area in the right forearm muscles on axial images and a three-stripe pattern on coronal and sagittal images, typical of sarcoid myopathy (Figure 4)[12-14].
Figure 4.
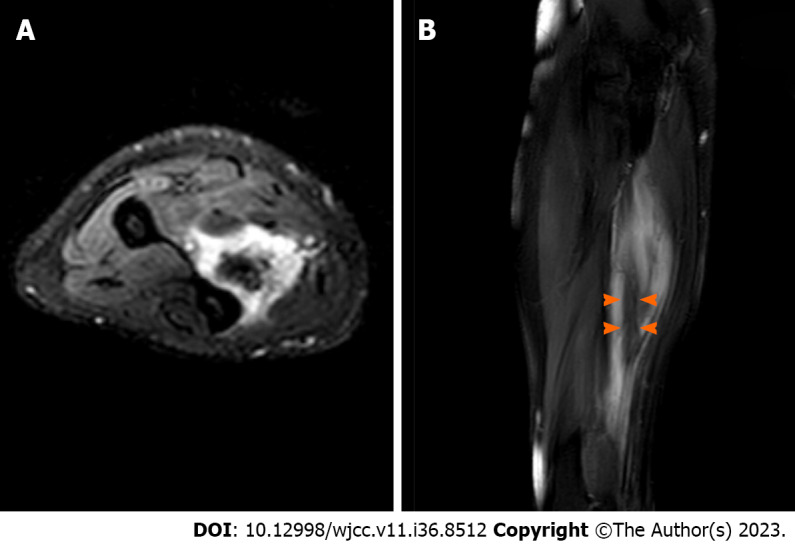
Magnetic resonance imaging revealing a lesion located at the flexor digitorum profundus muscle. A: T2-weighted fat saturated axial image of the forearm shows a nodule of increased signal intensity, while the center structure shows decreased signal intensity; B: T2-weighted fat saturated sagittal image of the forearm shows an inner stripe of decreased signal intensity (arrowheads) and outer stripes of increased signal intensity.
FINAL DIAGNOSIS
The patient was diagnosed with sarcoidosis-related flexor tendon contractures and iatrogenic flexor tendon rupture.
TREATMENT
During the first surgical exploration, the distal FDP of the middle finger was anastomosed with the proximal end of the FDS to restore flexion. Surprisingly, the ring finger remained in contracture after complete open release of the A1 pulley, indicating that the contracture was not due to tenosynovitis. No further intraoperative intervention was performed after discussion with the patient. Routine postoperative management was performed, including splinting for 4 wk and corresponding rehabilitation.
Unfortunately, 2 mo after the operation, re-rupture of the repaired tendon was encountered when the patient was pulling on her pants (Figure 5A). Repeat operations were performed on the right middle and ring fingers. Anastomoses of the proximal FDS to the distal FDP using tendon grafting were performed for the middle finger and direct repair was performed for the ring finger (Figure 5B).
Figure 5.
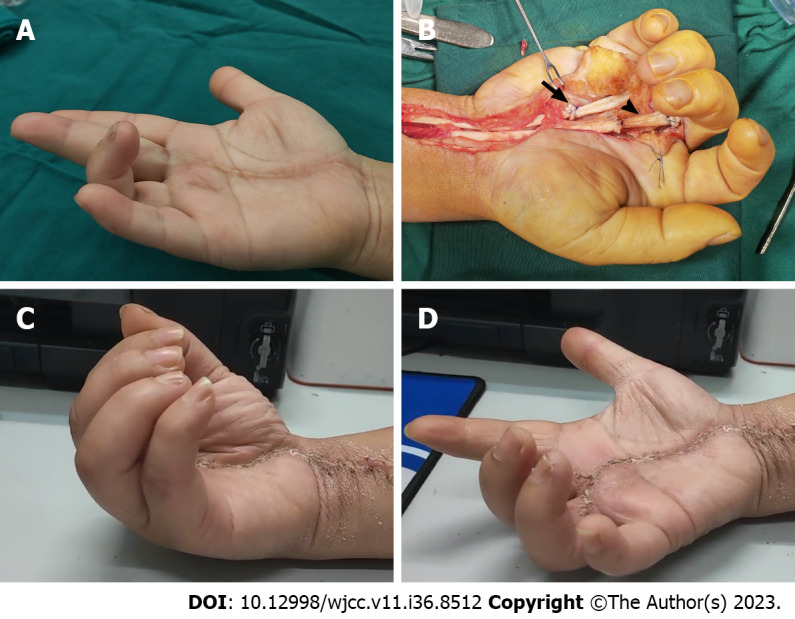
The second surgery and follow-up. A: The extended middle finger and flexed ring finger before reexploration; B: Intraoperative view of the repaired tendons of the middle and ring fingers. Arrow: The repaired site of the ring finger with suturing the distal end of the flexor digitorum profundus to the proximal end of the flexor digitorum superficialis. Arrowhead: The repaired site of the middle finger with tendon grafting; C and D: Range of active motion of the affected fingers 10 mo after reoperation.
OUTCOME AND FOLLOW-UP
The patient partially regained the motion of her middle finger, while contracture of her right ring finger persisted after the first surgical attempt. After reoperation, the patient could use the hand without discomfort despite persistent mild stiffness at the 10 mo follow-up (Figure 5C and D).
DISCUSSION
In the present case, surgery was performed when the patient presented with an iatrogenic rupture. Sarcoidosis was not considered until the second surgical attempt and was confirmed after MRI and chest CT. After the re-rupture, a comprehensive medical history revealed an additional experience of mild discomfort with tenderness on physical examination around the forearm flexor muscles, indicating a muscular lesion. Furthermore, tenosynovitis should have been ruled out because the patient denied experiencing pain or triggering around the MCP joint or had a history of aggravation after housework.
Although contractures due to sarcoidosis are extremely rare, neglecting these distinct symptoms and the absence of a systematic examination resulted in misdiagnosis and subsequent mistreatment.
The diagnosis of sarcoidosis is not well established, but is recommended according to three major aspects: A compatible clinical and/or radiological presentation, histological evidence of non-necrotizing granulomatous inflammation in one or more tissues, and exclusion of alternative causes of granulomatous disease[15].
Chest radiography has been the cornerstone of sarcoidosis diagnosis since 1961, when Scadding[16] proposed a standardized staging system. Chest CT is currently the reference standard for the assessment of pulmonary findings and mediastinal lymph nodes[17]. In our case, MRI and biopsy revealed lesions in the forearm muscles, whereas a clear diagnosis of sarcoidosis was made only after CT imaging.
The treatment of sarcoidosis-related contractures has been reported in several case reports with varied results[2-5,18-21] (Table 1).
Table 1.
Literature review of published cases of flexor contractures associated with sarcoidosis
|
Ref.
|
Sex
|
Age
|
Affected hands
|
Affected fingers
|
Treatment
|
Outcomes of contractures
|
| Warburg[20] | F | 56 | L and R | All fingers | None | NA |
| Simmonds and Hoffbrand[19] | F | 58 | L and R | 3rd fingers | Prednisolone and dapsone | Worsened |
| M | 65 | R | 4th finger | Steroids, and Azathioprine | Cured after duration of 6 yr | |
| Ikeda et al[2] and Tada et al[4] | F | 63 | R | 2-4th fingers | Granulomatous lesion excision | Worsened two years postoperatively |
| Motomiya et al[5] | F | 61 | L and R | 5th fingers | Granulomatous lesion excision | NA |
| Bowers et al[3] | M | 14 | L | 3-5th fingers | Occupational therapy | Improved |
| Ueba and Obara[18] | F | 58 | L and R | 4, 5th fingers | Granulomatous lesion excision | Cured at a follow-up of 2.5 yr |
| Walter et al[21] | M | 36 | L and R | 3-5th fingers | Low-dose thalidomide therapy | Markedly improved |
F: Female; M: Male; L: Left hand; R: Right hand; NA: Not available.
Acute sarcoid myopathy improves with systemic treatment in most patients, while patients with chronic sarcoid myopathy commonly experience severe disability such as flexor contractures and seldom recover after corticosteroid, immunosuppressive, or anti-tumor necrosis factor-α treatment[22,23]. Surgical intervention has been attempted in such chronic cases of finger contractures[2,4,5,18]. In 1996, Ikeda et al[2] reported that contractures due to sarcoidosis could be successfully treated by surgical excision of the lesion. However, in 2009, they reported that even with complete excision of the granulomatous lesion, a new lesion may appear in a previously healthy area; therefore, radical cure by surgery alone is difficult[4]. Conservative treatments have also been reported. Walter et al[21] reported a case in which the contractures improved after 9 mo of treatment with low-dose thalidomide. Bowers reported a 14-year-old patient who improved with occupational therapy[3]. Notably, while in previous cases, biopsy tests focused on forearm muscles, our biopsy results revealed a lesion at the tendon as well.
Coincidentally, Motomiya et al[5] also reported a patient with sarcoidosis-related flexor contracture who was initially misdiagnosed with trigger finger and underwent open surgery. Fortunately, the tendon was fully exposed during the operation, and the misdiagnosis of tenosynovitis was realized. In our case, the patient was misdiagnosed with tenosynovitis and treated by acupotomy (a type of blind release) during the first visit to a local hospital. The operation did not provide further information about the contracture, inevitably resulting in iatrogenic flexor rupture when pursuing complete finger flexion. Therefore, the treatment of tenosynovitis using acupotomy should be performed with great caution in preoperative diagnosis.
In our case, because of the initial iatrogenic flexor tendon rupture, tendon grafting was performed to repair the FDP tendon by connecting the proximal end of the FDS to the distal FDP. Notably, open surgery of the digit revealed normal tension at the FDS, and the FDS muscle was later proven to be free of lesions based on biopsy results; thus, this surgery was able to partially restore flexion to the affected fingers. In conclusion, this method was adapted because of the initial attempt to repair the tendon rupture and achieved satisfactory results in alleviating the contractures at the 10 mo follow-up.
CONCLUSIONS
Sarcoid involvement of the musculoskeletal system that causes finger contractures is rare and can lead to misdiagnosis if clinicians are not aware. Our case shows that finger contracture release by connecting the normal proximal end of the FDS to the distal FDP may be an option for such cases, although the management of sarcoidosis-related flexor contractures remains controversial, with varied outcomes based on a literature review.
ACKNOWLEDGEMENTS
We thank Dr. Mazhar Ali Raza for the editing assistance.
Footnotes
Informed consent statement: The study participant provided written informed consent before study enrollment.
Conflict-of-interest statement: The authors have no conflicts of interest related to this manuscript.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: August 26, 2023
First decision: November 9, 2023
Article in press: December 7, 2023
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bernardes A, Portugal S-Editor: Lin C L-Editor: Wang TQ P-Editor: Lin C
Contributor Information
Rui Yan, The Second Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou 310053, Zhejiang Province, China.
Zhe Zhang, Department of Orthopedics (Division of Hand Surgery), The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou 325026, Zhejiang Province, China.
Long Wu, Department of Orthopedics (Division of Hand Surgery), The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou 325026, Zhejiang Province, China.
Zhi-Peng Wu, Department of Orthopedics (Division of Hand Surgery), The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou 325026, Zhejiang Province, China.
He-De Yan, Department of Hand Surgery, The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou 325026, Zhejiang Province, China. yanhede@hotmail.com.
References
- 1.Baydur A, Pandya K, Sharma OP, Kanel GC, Carlson M. Control of ventilation, respiratory muscle strength, and granulomatous involvement of skeletal muscle in patients with sarcoidosis. Chest. 1993;103:396–402. doi: 10.1378/chest.103.2.396. [DOI] [PubMed] [Google Scholar]
- 2.Ikeda K, Saito M, Sueyoshi Y, Ichizen H, Tomita K. Flexion contracture of fingers due to sarcoidosis--a case report. Acta Orthop Scand. 1996;67:623–625. doi: 10.3109/17453679608997770. [DOI] [PubMed] [Google Scholar]
- 3.Bowers B, Patel AM, Mirza N, Seidman RJ. Paediatric contracturing granulomatous myositis. Scand J Rheumatol. 2008;37:394–395. doi: 10.1080/03009740802093878. [DOI] [PubMed] [Google Scholar]
- 4.Tada K, Ikeda K, Tomita K. Flexion contracture of the fingers caused by sarcoidosis: an 11-year follow-up. Scand J Plast Reconstr Surg Hand Surg. 2009;43:171–173. doi: 10.1080/02844310701510306. [DOI] [PubMed] [Google Scholar]
- 5.Motomiya M, Iwasaki N, Kawamura D. Finger flexion contracture due to muscular involvement of sarcoidosis. Hand Surg. 2013;18:85–87. doi: 10.1142/S0218810413720015. [DOI] [PubMed] [Google Scholar]
- 6.Thulasidoss K, Sridharan S, Ashokan L, Chandra P. A Rare Case of Sarcoidosis Presenting as Diffuse Contracturing Granulomatous Myositis on Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography. Indian J Nucl Med. 2018;33:148–151. doi: 10.4103/ijnm.IJNM_154_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giugale JM, Fowler JR. Trigger Finger: Adult and Pediatric Treatment Strategies. Orthop Clin North Am. 2015;46:561–569. doi: 10.1016/j.ocl.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 8.Vasiliadis AV, Itsiopoulos I. Trigger Finger: An Atraumatic Medical Phenomenon. J Hand Surg Asian Pac Vol. 2017;22:188–193. doi: 10.1142/S021881041750023X. [DOI] [PubMed] [Google Scholar]
- 9.Huisstede BM, Gladdines S, Randsdorp MS, Koes BW. Effectiveness of Conservative, Surgical, and Postsurgical Interventions for Trigger Finger, Dupuytren Disease, and De Quervain Disease: A Systematic Review. Arch Phys Med Rehabil. 2018;99:1635–1649.e21. doi: 10.1016/j.apmr.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Li D, Wang X, Fang T, Chen Y, Xiang S, Qi J, Liang C, Ren C, Zhao X, Qiu Z, Liu F, Yan X. Acupotomy in the treatment of tenosynovitis of hand flexor tendons: A systematic review and meta-analysis. Medicine (Baltimore) 2022;101:e31504. doi: 10.1097/MD.0000000000031504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shen Y, Zhou Q, Sun X, Li S, Zhang W. Percutaneous Release of the First Extensor Tendon Compartment in De Quervain's Disease by Acupotomy with US-Guidance: A Cadaveric Study. J Pain Res. 2022;15:3995–4005. doi: 10.2147/JPR.S375309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Otake S, Banno T, Ohba S, Noda M, Yamamoto M. Muscular sarcoidosis: findings at MR imaging. Radiology. 1990;176:145–148. doi: 10.1148/radiology.176.1.2353084. [DOI] [PubMed] [Google Scholar]
- 13.Otake S. Sarcoidosis involving skeletal muscle: imaging findings and relative value of imaging procedures. AJR Am J Roentgenol. 1994;162:369–375. doi: 10.2214/ajr.162.2.8310929. [DOI] [PubMed] [Google Scholar]
- 14.Venkata Ramanan R, Pudhiavan A, Venkataramanan A. The "cluster of black pearls" sign of sarcoid lymphadenopathy: a new sign on thin-section contrast-enhanced multidetector CT. Clin Radiol. 2017;72:729–736. doi: 10.1016/j.crad.2017.03.031. [DOI] [PubMed] [Google Scholar]
- 15.Sève P, Pacheco Y, Durupt F, Jamilloux Y, Gerfaud-Valentin M, Isaac S, Boussel L, Calender A, Androdias G, Valeyre D, El Jammal T. Sarcoidosis: A Clinical Overview from Symptoms to Diagnosis. Cells. 2021;10 doi: 10.3390/cells10040766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.SCADDING JG. Prognosis of intrathoracic sarcoidosis in England. A review of 136 cases after five years' observation. Br Med J. 1961;2:1165–1172. doi: 10.1136/bmj.2.5261.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nunes H, Brillet PY, Valeyre D, Brauner MW, Wells AU. Imaging in sarcoidosis. Semin Respir Crit Care Med. 2007;28:102–120. doi: 10.1055/s-2007-970336. [DOI] [PubMed] [Google Scholar]
- 18.Ueba Y, Obara A. Sarcoidosis manifested by gradual flexion contracture of fingers. Hand. 1974;6:91–94. doi: 10.1016/0072-968x(74)90018-7. [DOI] [PubMed] [Google Scholar]
- 19.Simmonds NJ, Hoffbrand BI. Contracturing granulomatous myositis: a separate entity. J Neurol Neurosurg Psychiatry. 1990;53:998–1000. doi: 10.1136/jnnp.53.11.998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WARBURG M. A case of symmetrical muscular contractures due to sarcoidosis. J Neuropathol Exp Neurol. 1955;14:313–315. doi: 10.1097/00005072-195507000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Walter MC, Lochmüller H, Schlotter-Weigel B, Meindl T, Müller-Felber W. Successful treatment of muscle sarcoidosis with thalidomide. Acta Myol. 2003;22:22–25. [PubMed] [Google Scholar]
- 22.Le Roux K, Streichenberger N, Vial C, Petiot P, Feasson L, Bouhour F, Ninet J, Lachenal F, Broussolle C, Sève P. Granulomatous myositis: a clinical study of thirteen cases. Muscle Nerve. 2007;35:171–177. doi: 10.1002/mus.20683. [DOI] [PubMed] [Google Scholar]
- 23.Androdias G, Maillet D, Marignier R, Pinède L, Confavreux C, Broussolle C, Vukusic S, Sève P. Mycophenolate mofetil may be effective in CNS sarcoidosis but not in sarcoid myopathy. Neurology. 2011;76:1168–1172. doi: 10.1212/WNL.0b013e318212aafb. [DOI] [PubMed] [Google Scholar]