Abstract
The purpose of this study was to explore the daily activity spaces of female sex workers living with HIV in the Dominican Republic and assess the relationship between activity path and location-based risk exposure measures and daily drug use. The study employed a micro-longitudinal observational study design using an innovative 7-day travel diary to capture daily activity routes and a 7-day mobile health (mHealth) daily diary to collect daily substance use behaviors among 51 female sex workers. To estimate between-subject variability, a series of crude and adjusted modified logPoisson repeated measures regression models with generalized estimating equations (GEE), clustering by individual with a compound symmetry working correlation structure were fit to estimate the relative risks and 95% confidence intervals. Controlling for individual level factors, findings showed that female sex workers exposed to a higher number of risk outlets (e.g., liquor stores, bars, hotels, nightclubs, brothels, etc.) within 200 and 100-meters of sex work locations were at an increased risk of daily drug use (RRadj: 1.03, 95%CI: 1.01, 1.05, RRadj: 1.05, 95%CI: 1.01, 1.09). No association was detected between activity path exposure and daily drug use. These findings illustrate the importance of moving beyond static residential neighborhood boundaries for measuring risk exposures and highlight the significant role that daily work environments have on drug harms among a highly stigmatized and vulnerable population.
Keywords: HIV/AIDS, female sex workers, risk environments, drug use, Dominican Republic
Introduction
Globally, female sex workers are disproportionately affected by high rates of HIV.1 According to a systematic review on the burden of HIV among female sex workers from 50 low-and middle-income countries (LMIC), the odds ratio for living with HIV is 13.5 times higher for female sex workers compared to all women of reproductive age.1,2 Despite their increased risk of HIV acquisition and transmission, female sex workers are less likely to access care, have lower uptake of antiretroviral therapy (ART), and are disproportionately lost at each stage of the HIV care cascade.3–5 Female sex workers living with HIV are confronted with multiple barriers that may impede successful HIV care and treatment including drug use. Drug use is a common part of many female sex workers’ daily lives,6–8 and has been consistently linked to ART non-adherence, increased sexual risk behaviors, decreased health care utilization, and poorer immunologic and virologic outcomes.9–11 Drug use increases HIV susceptibility directly through unsafe injection practices (i.e., needle sharing), and indirectly through mechanisms that effect judgement and decision making ability, impair perception, and weaken the ability to process social cues.12,13
There is increasing recognition that variability in drug use behavior is intrinsically linked to the social and physical characteristics of the environments in which individuals live their daily lives.14–16 According to Rhodes and colleagues, risk environments encompass all the spaces “whether social or physical in which a variety of factors interact to increase the chances of harm occurring.”17 Previous work on populations that use drugs has documented positive correlations between neighborhood risk environments and illegal drug use.18,19 For example, in their study on neighborhood determinants of cocaine and heroin use, Williams and Latkin found that individuals living in neighborhoods with higher poverty rates had an increased odds of drug use independent of individual-level factors.20 Another study on drug markets reported that geographic residential proximity to illicit drug sales was associated with higher rates of drug consumption and relapse among those in substance use disorder treatment programs.21,22
Examination of female sex workers risk environments often focuses on the internal characteristics of the sex work venue.23–25 However, considering the substantial increase in non-establishment-based sex work, sex worker mobility, and the pervasive societal stigma attached to sex work, the venue may not be the only relevant space influencing female sex worker decision-making processes and associated behaviors.26 Moreover, with the aid of social media and text-based mobile platforms, the notion of a “fixed” sex work environment has evolved. Additionally, because sex work often intersects with drug scenes women are more likely to be in isolated and less frequented spaces with greater exposure to violence, environmental stressors, and less access to resources. Female sex worker daily activity patterns likely traverse many areas, exposing them to multiple social and physical contexts and experiences that may impact their drug use behavior.
Several researches have recently begun to explore the effects of non-venue based environments on HIV-related behaviors including drug use among female sex worker populations.27–29 Goldenberg et al. examined the effect of residential neighborhood criminalization and violence on ART interruption among female sex workers living with HIV in Vancouver.28 Another study by Deering et al. examined the effects of spatial isolation of the work environment (cross street for place of client solicitation) on sex-for-drug exchanges among street-based female sex workers in Vancouver.29 Both studies found that environmental conditions were associated with increased risk behaviors, underscoring the importance of how context may influence health and vulnerability. These studies, however, face the same methodological problems as other neighborhood effects research.30–32 The spatial exposure measures were derived based on static administrative areas. Time and human mobility were not accounted for in environmental exposure calculations which can lead to erroneous results and spatial misclassification.31,33
In recent years, the concept of ‘activity space’, coupled with the availability of real-time geographic positioning system (GPS) tracking technologies, has emerged as a more accurate and objective approach to measuring place-based exposure and access to resources and opportunities as compared to the traditional use of fixed administrative boundaries. Activity space can be defined as “the local areas within which individuals habitually move about in the course of their daily activities.”31 Activity space research examines all spaces, whether physical or social, in which daily activities occur.32 The examination of activity spaces provides for more precise operationalized measures that capture the complexities of human spatial behavior and all the accompanying psychological, social, and health-related experiences within those spaces.30,34
The purpose of the present study was to describe the daily activity spaces of female sex workers living with HIV in the Dominican Republic (DR) and to assess the association between activity space risk exposure and drug use. An activity space approach will yield more accurate risk exposure measures as well as help identify and understand the potential variation in spatial inequality and social isolation between drug using and non-drug using female sex workers living with HIV. Resulting information may be used to develop efficacious drug harm prevention and treatment services that are geographically targeted and designed to modify the social and environmental contexts that influence drug use, a strong determinant of ART non-adherence. This is particularly important for countries like the DR where there is a concentrated HIV epidemic, no formal drug harm reduction policies, and widespread stigma of sex work, HIV, and drug use.
Setting
The DR is one of the largest sex tourism destinations in the Caribbean with an estimated 100,000 women involved in the sex industry.35 Sex work is not explicitly illegal in the country for people over the age of 18. Even though sex work is not illegal in the country, harassment by police and other law enforcement officials is common.36,37 Historically, the majority of sex work was establishment-based, but recent estimates suggest that more than 60% of female sex workers independently solicit clients from streets, parks, beaches or other public places. Female sex workers who are establishment-based tend to work in brothels, bars, discos, liquor stores, or car washes.26 Although the country has made significant gains in HIV risk reduction among the general population, rates among female sex workers remain disproportionately high, with prevalence ranging between 1.7–6.3% compared to 0.9% among women of reproductive age and 0.7% among the general population.35,38,39
In recent years, the DR has experienced a dramatic increase in the use and transport of illegal drugs.40,41 According to the National Drug Control Directorate, cocaine confiscations in the country increased by approximately 50% between 2010 and 2011, suggesting an increase in local drug availability.42 Furthermore, the drugscene in the country is amplified by the large sex tourism economy. The main drugs consumed in the country are powder and crack cocaine and marijuana, and to a much lesser extent heroin.43 Under the current Dominican drug law (Law 50–88), anyone found in possession of illegal drugs may be classified as a narcotrafficker and can be sentenced to years in prison.44 Government investment in drug treatment and harm reduction programs is low, with most rehabilitation programs provided by nongovernmental organizations (NGO) and focused on abstinence. The country has no formal drug harm reduction policy and all spectrums of drug use are heavily stigmatized and criminalized.45 Despite the evidence that drug use contributes to the concentrated HIV epidemic among key populations, including sex workers, integration of drug prevention and treatment services within HIV policies are largely non-existent.
Methods
Study design
This study employed a micro-longitudinal observational study design and was nested within an ongoing five-year (2016–2021) National Institutes of Health (NIH)funded parent study (5R01MH110158) in the DR.46 Details on the parent study can be found elsewhere (see Kerrigan et al. 2020).47 Data collection activities in this microlongitudinal study included a mobile health (mHealth) daily behavior diary collected for 7 days, a paper-based daily travel diary collected for 7 days, and secondary data from the Dominican National Office of Statistics (ONE), the 2014 PLACE study (USAID/MEASURE Evaluation)48, and the parent study. Data collection instruments and measures were piloted with 5 female sex workers, translated to Spanish, and adapted to the Dominican context. Written informed consent was obtained from all participants. Study enrollment was held at the Instituto Dermatológico Dominicano y Cirugía de Piel (IDCP) in Santo Domingo where the parent study was located. Ethics approval from the Internal Review Boards (IRB) at Tulane University and IDCP was obtained.
Study participants and recruitment
Women were eligible to participate in the study if they met the parent study’s inclusion criteria (which included being at least 18 years of age, having a confirmed HIV positive diagnosis determined by a single rapid test, and having exchanged sex for money in the month prior to study enrollment), had used drugs in the 6 months prior to data collection [required for half the sample], were willing and able to complete a paperbased travel diary for 7 days, and were willing and able to answer electronic daily behavior diary questions for 7 days. Participants were recruited from the parent study using selective/purposive sampling based on drug use. Female sex worker peer navigators were used to contact and recruit participants. Participants received $10 USD for participating in the study and an additional $3 USD per day for completion of the electronic daily behavior diary and the daily travel diary over the 7-day data collection period (1 travel diary, 1 behavior diary x 7 days= $21). Transportation to and from the study site was covered for 2 trips. At the time of enrollment, cellphones were loaded with a pre-paid 7-day data package to cover Internet costs for the daily diary survey.
Data collection procedures
Daily behavior diary
Daily behaviors were captured using a mobile web-based daily diary survey. The daily diary survey collected information on daily drug use (type, location of consumption, and with whom), daily alcohol use (quantity, location of consumption, and with whom), daily affect, daily violence experience, sex exchange, drugs in the environment, social support, and daily ART adherence. The survey was generated using Qualtrics Mobile Survey Platform (https://www.qualtrics.com), which provides secure, encrypted mobile technology messaging services. Prior to data collection, diary items were reviewed with participants to ascertain their comprehension of the items and to ensure consistency in the interpretation of potentially ambiguous items. Participants were sent the link to the web-based survey via Short Message Service (SMS) text message once a day in the morning with participants reporting on the previous day’s behaviors. Morning was chosen as the optimal time given that many participants worked at night and allowing them to reflect on the entire evening prior to the morning survey. Participants had 24 hours to complete the survey before it became invalid. Diaries could be completed in 23 minutes. Daily diary completion was monitored and any participant who did not complete the diary questions was sent a reminder message. Results from the online diary were automatically stored for each participant according to their unique study ID in a Qualtrics password-protected database.
Secondary spatial data
Shapefiles of Santo Domingo neighborhoods and administrative boundaries were obtained from the Dominican National Office of Statistics (ONE). Shapefiles are a vector data storage format used for storing the location, shape, and attributes of geographic features. Data on sex work locations/venues were obtained from the USAID/MEASURE Evaluation 2014 PLACE study.48 PLACE 2014 was conducted in 6 regions of the country known to have high HIV prevalence. One objective of the study was to characterize and map risk outlets (e.g., car washes, liquor stores, bars, hotels, construction areas, nightclubs, brothels etc.) frequented by key populations. Outlets were identified and captured via interviews with community informants about where key populations socialized and met sexual partners. We plotted the geographic coordinates of these risk outlets (N=743) on the Santo Domingo base map. Neighborhood boundaries were defined based on the smallest administrative unit (barrio paraje) for which data is available in the DR.
Daily travel diary
The best practice for activity space mapping is to use GPS technology because it minimizes recall and respondent bias and requires minimal investment by the participant; location, time, and speed are recorded in real-time at pre-determined time intervals (e.g., every minute). However, considering the study population and the context of sex work, the research team was hesitant to use GPS for issues related to privacy and vulnerability (among others). Thus, as an alternative, participant activity paths were recorded prospectively for 7 days using a paper-based travel diary.
During study enrollment, participants received 7 travel diary forms, one for each day. They were asked to record the place (name and address), time, main activity, transport method, and whom they were with for each place they visited from the time they woke up until they went to sleep. Despite the limitations of this approach (e.g., lost diary, untruthful reporting, spatial misclassification, etc.), paper-based diaries have been successfully used to document daily mobility patterns in other female sex worker studies.23,32
To verify daily completion, participants were asked to send a photo of the completed travel diary labeled with the date and the participant’s unique ID to a member of the research team via SMS or WhatsApp. At the end of the 7-day data collection period, participants returned the paper travel diaries and were asked to clarify any entries that lacked information that was necessary for recording the latitude and longitude of each location. With the help of the participants, using Google Street View, each location visited during the week was plotted on a Google Map file and the latitude and longitude were recorded in an Excel file for that participant.
Key measures
The primary outcome was daily drug use. Daily drug use was examined as a binary variable (1= ‘Yes’, 0= ‘No’) from the daily diary responses. Participants were asked the following questions to capture drug use: “Since yesterday, have you consumed drugs?” [response: yes, no, no response]; “What type of drugs did you use?” [select all that apply: marijuana, cocaine, crack, pills, heroine, other, no response]; “With whom did you use?” [select all that apply: alone, client, partner, friend, family, other, no response]; and “Where did you consume?” [select all that apply: home, street, park, hotel, bar, disco, colmado (corner store that sells alcohol), other, no response].
The primary exposure variables included activity path and activity location risk exposures.
Activity path risk.
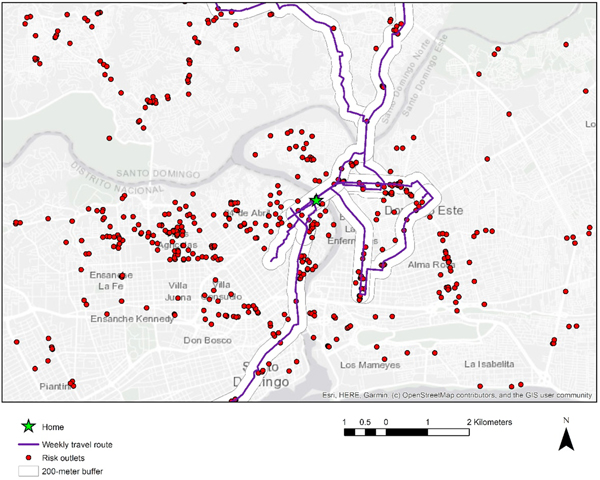
Activity paths were generated by connecting daily activity points using the shortest roadway network distance tool in ArcGIS 10.6 (ESRI, Redlands, CA). Fifty-meter, 100-meter, and 200-meter buffers were calculated around the activity paths. These distances were selected to reflect exposure to environmental features on either side of the street that participants walked down and to capture exposures within a city block of each trip path and are consistent with distances employed in prior research.49,50 Point locations of risk outlets from the 2014 PLACE study were plotted and the total number of outlets within the activity path buffers were aggregated to get unweighted counts within each of the buffer distances.48 To account for different durations that participants were exposed to risk outlets, we weighted the total number of outlets within the activity path buffers by the estimated duration of each corresponding polyline segment, then divided by the total estimated time each participant was tracked per day to get daily activity path exposure measures. Measures were examined as continuous and binary variables cut at the 75th percentile.
Activity location-based risk.
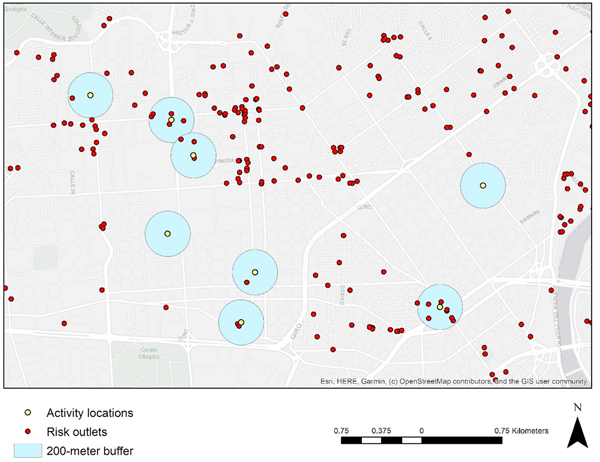
Individual activity locations from the daily travel diaries were plotted in ArcGIS 10.6 (ESRI, Redlands, CA) and 50, 100, and 200-meter circular buffers were drawn around each location. Point locations of risk outlets from the 2014 PLACE study were plotted and the total number of outlets within the buffer distances of each activity location were summed and then aggregated to get a total count of location-based risk exposure per day.48 Location-based exposure measures specific to place of residence and sex work locations were also examined. Measures were examined as continuous and binary variables cut at the 75th percentile.
Sociodemographic characteristics came from the parent study (except for age diagnosed with HIV and age started sex work). The people living with HIV (PLHIV) perceived stigma scale consisted of an aggregated 5-item measure with a 4-point Likert scale.47 The sex work discrimination measure was assessed as an aggregate measure with a score ranging from 0–12 with higher numbers reflecting higher self-perceived sex work discrimination.47 Daily behavior measures (e.g., daily alcohol use, daily exposure to violence, daily sex exchange, etc.) came from the daily diary responses.
Data management and statistical analysis
Data were collected and managed in different platforms. Each participant’s activity path was derived in ArcGIS 10.6 (ESRI, Redlands, CA) resulting in 51 activity path files (one file per woman). Each file contained descriptive data fields (e.g., location, latitude, longitude, date, time, activity, distance, etc.). Using ArcGIS 10.6 (ESRI, Redlands, CA), activity path files were joined with the Santo Domingo base map and the risk outlet data from the 2014 PLACE study.48 Data were then imported and appended in SAS 9.4 (SAS Institute Inc. Cary, NC) where activity location and path measures were calculated. Each participant also had a .csv file with data from the daily behavior diary. The data files were imported and appended to create one dataset with repeated behavior and exposure measures for each participant.
All statistical analyses were performed using SAS 9.4 (SAS Institute Inc. Cary, NC). Standard errors, 95% confidence intervals and unless otherwise stated, a p-value <0.05 was used to define statistically significant associations. Descriptive statistics (frequency distributions, means, and standard deviations) and exploratory spatial mapping were utilized to examine daily and weekly activity patterns and daily diary responses. Chi-square analysis and two-sample t tests were employed to examine differences in activity space risk exposure between drug using and non-drug using participants. A series of crude and adjusted repeated measures modified log-Poisson regression models with generalized estimating equations (GEE), robust variance estimation and compound symmetry working correlation structure, clustering by individual were fit to estimate relative risks and 95% confidence intervals.51 GEE is an extension of generalized linear models designed for longitudinal and repeated measures studies. GEE controls for within-subject clustering of observations, modeling the average or between-subject effects.52 A supplementary analysis using matched conditional logistic regression and adjusting for covariates was also conducted to estimate odds ratios and 95% confidence intervals for within-subject effects. In both the GEE and conditional logistic regression models, control variables were modeled as fixed effects. Variables that created 10% or greater difference between the unadjusted and adjusted effects were considered confounders and controlled for in the final model. Covariates with significant statistical associations to both the outcome and exposure in bivariate analyses were included in the regression models, in addition to variables that were not statistically significant but that are important theoretical confounders to drug use among PLHIV.
Results
Sample demographic characteristics are presented in Table 1. Demographics of the current sample were similar to the parent study sample, with exception of alcohol and drug use which were higher in the current sample due to eligibility criteria. The mean age of participants was approximately 40 years [range 24–59]. The average age participants were diagnosed with HIV was 30 [range 16–53] and began sex work at age 20 [range 10–45]. The mean number of children was 3 [range 0–9]. Slightly more than 30% of women were in steady partnerships, 35% were separated, and 28% were single. Participants had an average monthly income of 11484 [range 3000–30000] Dominican pesos, equivalent to $230 US dollars of which 63% came from sex work. Drug users had a slightly higher monthly income than non-drug users ($246 vs. $222) but a higher percentage of drug users’ monthly income came from sex work, 71% vs. 30%. All participants reported having some education and significant differences in level of education achieved by drug use status were detected (t-value= 6.5, p<0.01). Eightyone percent of drug users had some primary education, 13% some secondary education, and 6% some university. Forty-three percent of non-drug users had some primary education, 40% some secondary education, and 17% some university. Viral load was non-detectable in 74% of the sample. There was no significant difference in viral load detectability by drug use. Over 90% of participants were alcohol users with 100% of drug users reporting alcohol use in the past 6 months compared to 86% of non-drug users. Approximately 61% of the sample consumed 6 or more drinks per week according to the Alcohol Use Disorder Test (AUDIT) scale.53 On average, participants reported engaging with 6 [range 0–42] clients per week and the majority of participants, 82%, were street-based/self-employed. The mean sex work discrimination score was 4 [range 0–11] and the mean perceived HIV stigma score was 13 [range 5–18].
Table I.
Socio-demographic characteristics of female sex workers living with HIV (N=151)
| Drug Users (N=16) | Non-Drug Users (N=35) | Total (N=51) | Test Statistic | df | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean / % | SD | Range | Mean / % | SD | Range | Mean / % | SD | Range | |||
| Average age (years) | 39 | 7.3 | [24–59] | 38 | 7.4 | [24–52] | 40 | 7.3 | [24–59] | 0.7 | 49 |
| Average age diagnosed with HIV (years) | 29 | 7.3 | [16–43] | 31 | 8.2 | [18–53] | 30 | 7.9 | [16–53] | 0.6 | 49 |
| Average age started sex work (years) | 18 | 4.7 | [10–29] | 21 | 7.5 | [12–45] | 20 | 6.8 | [10–45] | 1.5 | 49 |
| Average number of children | 3 | 2.0 | [1–9] | 3 | 1.3 | [0–6] | 3 | 1.5 | [0–9] | −1.2 | 49 |
| Current relationship status | 1.1 | 3 | |||||||||
| Partnered | 37.5% | 31% | 33% | ||||||||
| Separated | 37.5% | 34% | 35% | ||||||||
| Single | 25% | 29% | 28% | ||||||||
| Other | 0% | 6% | 4% | ||||||||
| Average monthly income (Dominican peso) | 12300 | 7814.0 | [3000–30000] | 11111 | 5765.9 | [3000–25000] | 11484 | 6421.6 | [3000–30000] | −0.6 | 49 |
| Average monthly income from sex work only (Dominican peso) | 8719 | 7694.4 | [300–30000] | 6506 | 3295.0 | [700–15000] | 7200 | 5120.5 | [300–30000] | −1.5 | 49 |
| Education | 6.5** | 2 | |||||||||
| Primary | 81% | 43% | 55% | ||||||||
| Secondary | 13% | 40% | 31% | ||||||||
| University | 6% | 17% | 14% | ||||||||
| Viral Load (mL) | 1.8 | 1 | |||||||||
| ≤400 mL | 87% | 69% | 74% | ||||||||
| >400 mL | 13% | 31% | 26% | ||||||||
| Current alcohol use (past 6 months) | 100% | 86% | 90% | 2.5 | 1 | ||||||
| Alcohol Use Disorder Test (AUDIT) | 3.2 | 2 | |||||||||
| Abstainer | 0% | 14.3% | 10% | ||||||||
| 1–6 drinks per week | 25% | 31.4% | 29% | ||||||||
| >= 6 drinks per week | 75% | 54.3% | 61% | ||||||||
| Average number of clients per week | 7 | 7.4 | [1–25] | 6 | 7.5 | [0–42] | 6 | 7.4 | [0–42] | −0.8 | 49 |
| Location of Sex Work | 0.2 | 1 | |||||||||
| Street-based | 81% | 83% | 82% | ||||||||
| Venue-based | 19% | 17% | 18% | ||||||||
| Sex work discrimination a | 4 | 3.9 | [0–11] | 4 | 3.4 | [0–11] | 4 | 3.3 | [0–11] | 0.1 | 49 |
| PLHIV perceived stigma b | 12 | 2.5 | [5–15] | 13 | 2.8 | [5–18] | 13 | 2.7 | [5–18] | 1.0 | 49 |
Scored 0–12 with a higher score indicating higher sex work discrimination
Scored 1–20 with a higher score indicating higher perceived HIV stigma.
p<0.01.
Notes. PLHIV=People living with HIV; df= degrees of freedom; SD= standard deviation; Mean / % based on non-missing data (<10% missing on any variables).
Table 2 presents means and frequency analysis from the daily behavior diary stratified by current drug use status. The total number of observations was 326 of 357 possible with a 91% response rate. The minimum number of diary days completed was 2, the maximum 7, and an average of 6 days. During the 7-day diary, 22% of the sample used drugs of which 18% reported consuming cocaine, 6% marijuana, 2% crack, and 3% other drugs (not shown in table). Among drug users, 69% engaged in drug use during the week of data collection and drugs were consumed an average of 3 days per week [range 0–7]. Cocaine was consumed on 32% of response days, marijuana 13% of response days, and crack on 4% of response days. Drug consumption occurred most frequently with friends (36%), clients (34%), and partners (13%) (not shown in table). Most frequent locations of drug use included household (54%), bar/disco (20%), street (11%) (not shown in table). Drug users were statistically more likely to have been exposed to drug environments during the week compared to non-drug users, (64% vs. 37%, t-value= −2.4, p<0.001). The weekly negative affect score was 2 [range 0–13]. The weekly experience with violence was low with a mean of 0.5 [range 0–4], with drug users having a slightly higher mean than non-drug users, 0.6 [range 0–3] vs. 0.5 [range 0–4]. Sex exchange occurred an average of 3 days [range 0–7] per week. The average number of drinks per day was 2 [range 0–9]. Non-drug users consumed a higher number of drinks per week than drug users, 15 [range 0–40] vs.12 [range 0– 37].
Table 2.
Daily behavior diary results among female sex workers living with HIV (N=51 participants, 326 observations over 7 days)
| Drug Users (N=16) | Non-Drug Users (N=35) | Total (N=51) | Test Statistic | df | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean / % | SD | Range | Mean / % | SD | Range | Mean / % | SD | Range | |||
| Average number of diary days completed (days) | 6 | 1.3 | [4–7] | 7 | 1.0 | [2–7] | 6 | 1.1 | [2–7] | 1.2 | 49 |
| Average weekly negative affect score | 3 | 3.1 | [0–13] | 2 | 2.4 | [0–10] | 2 | 2.6 | [0–13] | −0.7 | 49 |
| Average weekly experience with violence | 0.6 | 1.0 | [0–3] | 0.5 | 1.0 | [0–4] | 0.5 | 1.0 | [0–4] | −0.3 | 49 |
| Average number of days sex exchanged | 3 | 2.3 | [0–7] | 3 | 2.0 | [0–7] | 3 | 2.1 | [0–7] | 0.9 | 49 |
| % of response days sex exchanged | 41 | 33.3 | [0–100] | 46 | 29.0 | [0–100] | 45 | 30.2 | [0–100] | 0.6 | 49 |
| Average number of drinks per week | 12 | 10.0 | [0–37] | 15 | 11.5 | [0–40] | 14 | 11.1 | [0–40] | 1.0 | 49 |
| Average number of drinks per day | 2 | 3.0 | [0–8] | 2 | 3.2 | [0–8] | 2 | 3.1 | [0–8] | 0.9 | 308 |
| Average number of days drugs consumed | 3 | 2.4 | [0–7] | -- | -- | -- | 0.9 | 1.9 | [0–7] | -- | -- |
| % of response days drugs consumed | 47 | 37.2 | -- | -- | -- | 15 | 29.9 | [0–100] | -- | -- | |
| % of response days marijuana consumed | 13 | 29.9 | [0–100] | -- | -- | -- | 4 | 17.4 | [0–100] | -- | -- |
| % of response days cocaine consumed | 32 | 36.5 | [0–86] | -- | -- | -- | 9 | 23.1 | [0–86] | -- | -- |
| % of response days crack consumed | 4 | 15.0 | [0–60] | -- | -- | -- | 1 | 8.4 | [0–60] | -- | -- |
| % of response days other drugs consumed | 3 | 10.4 | [0–20] | -- | -- | -- | 0.7 | 3.4 | [0–20] | -- | -- |
| % of response days exposed to drug environment | 64 | 35.1 | [0–100] | 37 | 36.5 | [0–100] | 45 | 37.9 | [0–100] | −2.5**** | 49 |
Notes. df= degrees of freedom; SD=standard deviation; Mean / % based on non-missing data (<10% missing on any variable).
p <0.001.
Table 3 provides summary statistics for participant exposure to risk outlets within activity locations and activity paths. A total of 311 of 357 travel diaries were submitted on time equating to a response rate of 87% and the average number of diaries completed on time was 6 with a minimum of 0 and a maximum of 7.
Table 3.
Daily activity space characteristics among female sex workers living with HIV (N=51 participants, 1740 points recorded over 7 days, 339 observations over 7 days)
| Drug Users (N=16) | Non-Drug Users (N=35) | Total (N=51) | Test Statistic | df | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean / % | SD | Range | Mean / % | SD | Range | Mean / % | SD | Range | |||
| Average number of travel diary days completed (days) | 5 | 2.4 | [0–7] | 7 | 1.1 | [3–7] | 6 | 0.9 | [0–7] | 1.8 | 18 |
| Average number of activity locations per day | 4 | 1.5 | [1–11] | 4 | 1.5 | [1–9] | 4 | 1.5 | [1–11] | 2.6* | 337 |
| Average time tracked per day (minute) | 1163 | 395.6 | [30–1440] | 1180 | 352.8 | [30–1440] | 1175 | 365.1 | [30–1440] | 0.4 | 337 |
| Average path distance per day (meters) | 17149 | 41357.4 | [0–395569] | 1716 | 22246.5 | [15–14066] | 17158 | 29022.0 | [0–395569] | 0.0 | 121 |
| Activity location measures | |||||||||||
| % time spent at home per day (plus transit time to and from) | 49 | 28.9 | [0–100] | 51 | 28.9 | [0–99] | 50 | 28.9 | [0–100] | 0.4 | 324 |
| % time spent at sex work per day (plus transit time to and from) | 14 | 24.4 | [0–100] | 13 | 20.1 | 13 | 21.7 | [0–100] | −0.4 | 154 | |
| Average number of risk outlets within 200meters of activity locations per day | 7 | 9.7 | [0–44] | 5 | 6.1 | [0–31] | 6 | 7.3 | [0–44] | −1.4* | 129 |
| Average number of risk outlets within 100meters of activity locations per day | 3 | 5.1 | [0–24] | 1 | [0–13] | 2 | 3.3 | [0–24] | −3.4*** | 111 | |
| Average number of risk outlets within 50meters of activity locations per day | 1 | 2.3 | [0–10] | 1 | 1.1 | [0–6] | 1 | 1.6 | [0–10] | −2.8** | 118 |
| Average number of risk outlets within 200meters of home (day) | 1 | 1.7 | [0–5] | 1 | 3.5 | [0–20] | 1 | 3.1 | [0–20] | 1.4 | 331 |
| Average number of risk outlets within 100meters of home (day) | 1 | 1.1 | [0–4] | 0.2 | [0–1] | 0 | 0.7 | [0–4] | −4.2*** | 101 | |
| Average number of risk outlets within 50meters of home (day) | 0 | 0.5 | [0–2] | 0 | 0.2 | [0–1] | 0 | 0.3 | [0–2] | −2.13* | 105 |
| Average number of risk outlets within 200meters of sex work location (day) | 3 | 7.0 | 1 | 3.4 | [0–30] | 2 | 5.0 | [0–41] | −1.9* | 117 | |
| Average number of risk outlets within 100meters of sex work location (day) | 2 | 4.0 | [0–24] | 1 | 1.5 | [0–12] | 1 | 2.4 | [0–24] | −2.2* | 110 |
| Average number of risk outlets within 50meters of sex work location (day) | 1 | 1.7 | [0–10] | 0 | 0.8 | [0–5] | 1 | 1 | [0–10] | −2.3* | 117 |
| Activity path measures | |||||||||||
| Average number of risk outlets within 200meter buffer of daily activity path | 38 | 41.3 | [0–202] | 41 | 41.1 | [0–188] | 40 | 41.2 | [0–202] | 0.58 | 337 |
| Average number of risk outlets within 100meter buffer of daily activity path | 26 | 29.1 | [0–136] | 26 | 28.5 | [0–147] | 26 | 28.6 | [0–147] | −0.15 | 337 |
| Average number of risk outlets within 50meter buffer of daily activity path | 18 | 20.6 | [0–93] | 17 | 30.6 | [0–119] | 18 | 20.6 | [0–119] | −0.34 | 337 |
| % time exposed to any risk outlet per day (200-meter buffer) |
67 | 40.1 | [0–100] | 74 | 34.9 | [0–100] | 72 | 36.6 | [0–100] | 1.62 | 337 |
Notes. df= degrees of freedom; SD=standard deviation; Mean / % based on non-missing data (<10% missing on any variable).
p<0.05
p<0.01
p <0.001.
A total of 1740 points were recorded over the one-week data collection period. Average time tracked per day was 1175 minutes [range 30–1440] and average daily distance traveled was 17158 meters [range 0–395569]. The mean number of activity locations per day was 4 [range 1–11]. Participants spent an estimated 50% of their time at home and 13% at sex work per day. Participants were exposed to a daily average of 6 [range 0–44] risk outlets within 200-meters of activity locations with drug users exposed to a slightly higher number of outlets compared to non-drug users, 7 [range 0–44] vs. 5 [range 0–31]. Drug users had a higher daily mean exposure to outlets within 200-meters of sex work locations compared to their non-drug using counterparts, 3 [range 0–41] vs.1 [range 0–30]. Daily mean exposure to risk outlets within 200-meters of homes was similar across participants with an average of 1 [range 0–20]. Difference of means tests found significant differences in activity location-based risk exposure for drug users and non-drug users within 50, 100, and 200-meters.
Activity paths were successfully joined for all participants. Two participants had two polyline segments that would not snap to the roadway network. Participants were exposed to an average of 40 [range 0–202] risk outlets within 200-meters of their daily activity paths, 26 [range 0–147] within 100-meters of their daily activity paths, and 18 [range 0–119] within 50-meters of their daily activity paths. Participants were exposed to any risk outlet within 200-meters of their daily activity paths 72% of their time, with nondrug users exposed 74% of their time compared to 67% among drug users. Difference of means tests found no significant differences in activity path risk exposure between drug users and non-drug users.
Figure 1. is an example of one participant’s weekly activity locations with 200- meter buffers around each location and overlaid on a base map of risk outlets. Figure 2 is an example of one participant’s weekly activity path with a 200-meter buffer overlaid on a base map of risk outlets.
Figure 1.
Participant weekly activity locations with 200-meter buffer overlaid on risk outlets Santo Dominication Republic, 2019
Figure 2.
Participant weekly activity path with 200-meter buffer overlaid on risk outlets Santo Domingo,Dominican Republic, 2019
GEE crude relative risks and 95% confidence intervals of daily drug use regressed on the multiple measures of activity space risk exposure are presented in Table 4. Of all the activity path and location-based measures tested, only activity location-based measures had significant associations with daily drug use. Exposure to risk outlets within 200, 100, and 50-meters of daily activity locations was associated with an increased risk of daily drug use, such that participants exposed to a higher number of risk outlets (per unit increase) within 200, 100, and 50-meters of their activity locations were 1.02, 1.06, and 1.14 times more likely to use drugs. Likewise, participants exposed to higher number of risk outlets (per unit increase) within 200, 100, 24 50-meters of where they conducted or solicited sex work were 1.03, 1.06, and 1.17 times more likely to use drugs.
Table 4.
Crude relative risks and 95% confidence intervals (CI) between daily drug use and daily activity space risk exposure (N=51 participants, 326 observations)
| Relative Risk | 95% CI | P-Value | |
|---|---|---|---|
| Activity path | |||
| Daily exposure to risk outlets within 200-meter buffer of activity path weighted by time exposed | |||
| Low (ref) | |||
| High | 1.10 | 0.70,1.72 | 0.677 |
| Daily exposure to risk outlets within 100-meter buffer of activity path weighted by time exposed | |||
| Low (ref) | |||
| High | 1.00 | 0.62, 1.63 | 0.990 |
| Daily exposure to risk outlets within 50meter buffer of path weighted by time exposed | |||
| Low (ref) | |||
| High | 1.17 | 0.72, 1.89 | 0.517 |
| Activity location | |||
| Daily exposure to risk outlets within 200-meter of all activity locations | 1.02 | 1.00, 1.04 | 0.010 |
| Daily exposure to risk outlets within 200-meter buffer of sex work location | 1.03 | 1.00, 1.05 | 0.014 |
| Daily exposure to risk outlets within 200-meter buffer of home | 0.86 | 0.65, 1.14 | 0.290 |
| Daily exposure to risk outlets within 100-meter buffer of all activity locations | 1.06 | 1.01, 1.10 | 0.009 |
| Daily exposure to risk outlets within 100-meter buffer of sex work location | 1.06 | 1.01, 1.11 | 0.019 |
| Daily exposure to risk outlets within 100-meter buffer of home | 1.32 | 0.76, 2.27 | 0.321 |
| Daily exposure to risk outlets within 50meter of all activity locations | 1.14 | 1.03, 1.28 | 0.016 |
| Daily exposure to risk outlets within 50meter buffer of sex work location | 1.17 | 1.00, 1.36 | 0.045 |
Note. Not enough variation in daily exposure to risk outlets within 50-meter buffer of home to produce stable estimates.
Table 5 presents adjusted relative risks and 95% confidence intervals from the GEE repeated measures analysis between daily drug use and activity space risk exposures. In adjusted models, only sex work location-based risk remained significantly associated with daily drug use. After controlling for income, education, age, age diagnosed with HIV, age started sex work, sex work discrimination, perceived HIV stigma, daily alcohol use, daily negative affect, daily sex exchange, and daily experience with violence, per unit increase in risk outlets within 200 and 100-meters of where participants conducted or solicited sex work was associated with an increased risk of drug consumption (RRadj: 1.03, 95%CI: 1.01,1.05, RRadj: 1.05, 95%CI: 1.01, 1.09).
Table 5.
Generalized Estimated Equations (GEE) repeated measures analysis: Adjusted relative risks and 95% confidence intervals (CI) between daily drug use and activity space risk exposure (N=51 participants, 326 observations)1
| Relative Riskadj | 95% CI | P-Value | |
|---|---|---|---|
| Daily exposure to risk outlets within 200-meter buffer of sex work location | 1.03 | 1.01, 1.05 | 0.013 |
| Daily exposure to risk outlets within 100-meter buffer of sex work location | 1.05 | 1.01, 1.09 | 0.022 |
| Daily exposure to risk outlets within 50-meter buffer of sex work location | 1.12 | 0.99, 1.26 | 0.074 |
Controlled for age, age diagnosed with HIV, age started sex work, income, education, sex work discrimination, perceived HIV stigma, daily alcohol use, daily negative affect, daily sex exchange, and daily experience with violence.
Note. adj=adjusted, controlling for potential confounders.
As a supplementary analysis to test within-subject variability, we ran matched conditional logistic regression models. In crude models, similar to GEE models, the 3 sex work location-based exposure measures as well as all 3 activity location-based measures were significantly associated with an increased odds of daily drug use. No path-based exposures were related to daily drug use. In adjusted models, no measures remained statistically associated with daily drug use at p<0.05 (table not shown).
Discussion
This study examined the relationship between daily drug use and exposure to environmental conditions among female sex workers living with HIV in the DR. We calculated exposure measures based on residential location, daily activity locations, sex work location, and daily activity paths. To our knowledge, this is the first study to examine activity path risk exposure in association with daily drug use among female sex workers living with HIV in a LMIC context. Associations were strongest for sex work location measures. Individuals exposed to a higher density of risk outlets (e.g., bars, hotels, drug spots, brothels, etc.) within 200 and 100-meters of their sex work locations had an increased risk of daily drug use after controlling for socio-demographic factors and other confounders. No associations were detected between daily activity path exposure measures and daily drug use. Likewise, null findings from the supplemental conditional logistic regression analysis indicate little within-subject variability for daily drug use and risk environment exposure.
One mechanism that may explain how exposure to risk outlets within proximity of sex work locations may lead to increased risk of drug use among female sex workers is psychological stress. Social disorganization theory posits that when neighborhoods have higher levels of social and ecological disorder, it indicates a breakdown in social control and weak community cohesion, engendering fear and mistrust among residents.54 Research has shown that social disorganization can lead to substance use via stress and strain.55 A proposed reason for this relationship is that toxic and disadvantaged areas present numerous stressors in coping with life in these areas and drug use is one strategy for reducing stress. In the case of this study, drug use may be a coping mechanism for the individual stress and anxiety of engaging in commercial sex work as well as the stress associated with exchanging or soliciting sex in areas where there is a higher concentration of risk establishments and likely more exposure to social stressors such as violence, drunkenness, societal stigma, presence of drugs, and conflict between sex workers. In areas where there is a greater presence of drug use, the norms for using are also greater and potentially may influence women to use.
Research on risk environments and sex work has shown that the health impacts of sex work vary greatly depending on the setting in which sex workers exchange and solicit sex.56 While results likely vary by country context and sex work legality, some studies have indicated that venue/brothel-based sex work is regarded as a safer sex work environment due to establishment-based practices and policies that protect the sex workers from internal and external micro and macro level harms. Conversely, street-based sex workers may be more exposed to un-controlled environmental risks including greater movement of drugs, hostility and violence from clients, hostility from other sex workers, and excessive alcohol consumption.7 This in turn, may trigger a stress response leading to increased risky behaviors and consumption of drugs to cope with the disordered environment.
While the lack of association between activity path measures and the outcome may seem somewhat surprising given the greater space-time precision of activity path measures compared to location-based measures, it can be explained for several reasons. First, it is possible that more precise activity path data is not needed to accurately characterize a relationship when the linking mechanism does not heavily rely on dose-responsiveness (i.e., social mechanisms). Second, the spatial layout and social structure of the study setting may impact the relevance of activity path exposure on the outcome. To date, most activity path research has taken place in the U.S. cities which have different geographic layouts than cities in LMIC like Santo Domingo. In Santo Domingo, there is little separation between residential neighborhoods and commercial areas, which may minimize variability in exposure. Finally, without the use of GPS, exact routes could not be calculated. Activity paths were derived based on self-report and connecting points based on shortest roadway network which makes assumptions about routes taken and likely influenced exposure (see limitations for further discussion of this point).
This study is not without limitations. First, because most measures were selfreport, the study is subject to information bias, particularly social desirability, which may threaten internal validity. Validated measurements and multiple modes of data collection were used to minimize misclassification bias. Nonetheless, given the stigma associated with HIV, sex work, and drug use in the DR, it is likely that some measures (e.g., current drug use, sex exchange, etc.) were underreported. Second, given that geographic data was not collected using GPS devices, but based on participants reporting of the address and then locating the address on google maps, spatial imprecision and error are likely present. Time was not recorded for travel and location separately so activity locations could not be weighted by absolute time spent at each location, and because time was self-report it is subject to recall and reporting bias. Third, while method of transport from one location to another was collected, participants often took multiple forms of transportation to get from point A to B, making it difficult to estimate speed of travel which is an important determinant when calculating exposure to risk environments. Without the minute-to-minute GPS readings, travel routes were calculated using the shortest roadway network method to connect activity locations. While this method is commonly used for generating activity paths, especially in the absence of minute-tominute GPS data, it relies on the assumption that participants take the shortest roadway route between points which may not represent actual routes taken and barriers crossed.50,57 This in turn, can lead to imprecise exposure estimates due to spatial misclassification.
During the piloting phase of this study, we did attempt to reconstruct daily travel routes to get more precise data, but participants could not locate routes taken on Google Maps. Additionally, we did not specifically ask participants on exact location or route for where drugs were obtained. Without precise route data we were not able to determine if drug users take different routes compared to non-drug users to obtain drugs. As such, the issue of selective mobility bias is likely present. The presence of selective daily mobility bias is a concern for activity path measures. Selective daily mobility bias is the concern that exposure to environmental conditions may only predict health outcomes because people who engage in those behaviors deliberately choose to visit those locations (reverse causation).58 So, in the case of this study, one may question if it is truly the environmental exposure that leads to drug use or is it that sex workers who use drugs choose to frequent riskier environments. To make statements about causality, future studies should consider the issue of selective mobility bias. Potential methods include collecting outcome data at multiple time points throughout the day and calculating lagged effects, as well as accounting for places intentionally visited throughout the day.58 Finally, the activity location-based method is also likely to produce imprecise estimates given that it does not account for exposure to risk outlets or environments during transit.
Sensitivity analysis was conducted to evaluate if results differed for women who were not able to answer the electronic daily dairy by phone (N=6) and had to be called by the PI, and for the one woman who needed help completing the daily travel diary. The results of the sensitivity analysis for the main exposure variables were similar to the primary analysis. Finally, generalizability of results (external validity) is limited considering that study participants were female sex workers in treatment and thus, not representative of all female sex workers living with HIV.
Despite limitations, this study has several strengths. The study adds to the limited body of place-based research in an international setting. There has been limited research in the DR that has used socio-spatial methods to examine risk environments of key populations, especially those already infected with HIV. Documenting and analyzing activity spaces of female sex workers living with HIV provides a detailed picture of the social and spatial risk environments in their daily lives, and how such contextual exposures may contribute to drug use behaviors. This research demonstrated the importance of using both activity path and activity location measures. The detected associations with drug use would have been missed if only residential based measures had been assessed.
The high response rate among both the daily behavior diary (91% response rate) and travel diary (87% response rate) suggests that longitudinal mHealth studies are feasible and acceptable among stigmatized and vulnerable populations. Using an incentive-based survey completion system for daily diaries and travel diaries where compensation increased per item completed appears to have a positive effect and minimized respondent drop-out. In exit interviews with study participants, women reported that they enjoyed both the travel and daily behavior diaries. The travel diary was slightly more difficult than the electronic daily behavior diary as it involved notetaking and paying attention to locations. Most participants had little difficulty accessing the online daily diary survey. All participants reported that in future studies they would be open to using a GPS tracker to record their daily travel paths. It is important to note that the drug using participants, while often difficult to contact for recruitment, once enrolled, were eager to participate, had a high level of comprehension, completed 4 or more daily diary surveys, and all but one participant completed 2 or more travel diaries on time, and all but one returned for the exit survey.
Conclusion
The findings from this study could be used to help inform structural interventions and policies that focus on reducing environmental risks in areas with a high density of risk outlets. Focusing on geographic areas surrounding popular sex work environments could be a good point of intervention given that risk of drug use was associated with increased exposure to risk outlets at sex work locations. Interventions to promote ‘enabling environments’ including safer living and working spaces, community-based peer-led strategies to better integrate drug users into HIV care services including treatment and counseling for drug use and associated traumas, alongside policy reforms and decriminalization of sex work should be explored. Previous environmentalstructural interventions in the DR directed at improving community solidarity between female sex workers and sex work venue and establishment owners were successful in improving sexual risk behaviors.59 This model could be adapted to include solidarity building with police who patrol high risk environments and increase their awareness about sex worker rights. Evidence from several police education sex worker interventions have shown positive results with reductions in violence against sex workers, improved condom use, and decreased sexually transmitted infections (STIs).60,61 It is possible that an increase in safety would reduce the anxiety and stress associated with environmental risks. This in turn, coupled with integrated HIV, substance use, and mental health care, could lead to decreased consumption of illegal substances.
Finally, future studies are needed to further elucidate the pathways through which geographic stressors may enhance use of substances as well as sustained use of ART. For example, research among female sex workers in Canada has shown that women who experience heavy policing and harassment often have their daily routines interrupted, leading to disruptions in healthcare and medication.28 Future research could employ Ecological Momentary Assessment (EMA) methods and GPS tracking to pinpoint exact environmental risk locations, their characteristics, and triggers at time of drug use events.
Highlights.
Activity location risk exposures were associated with daily drug use
Greater sex work location-based risk was associated with increased daily drug use
Female sex workers in the Dominican Republic are highly mobile
Paper travel diaries provided an alternative approach to collect activity space data
Mobile health data collection was feasible among female sex workers living with HIV
Acknowledgments
We thank the research participants for their willingness to participate in the study. We acknowledge the hard work and time devoted by the local study team in the Dominican Republic. The study was supported by grants from the National Institutes of Health (E. Felker-Kantor, NIH/NIDA 5F31DA042714 and D. Kerrigan, NIH/NIMH 5R01MH110158).
Footnotes
Compliance with Ethical Standards
Protocols were approved by Tulane University and the Instituto Dermatológico Dominicano y Cirguía de Piel Institutional Review Boards and all subjects provided informed consent.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Baral SD, Breyer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and metaanalysis. Lancet Infect Dis. 2012;12:538–549. [DOI] [PubMed] [Google Scholar]
- 2.Shannon K, Strathdee SA, Goldenberg SM, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants Lancet. 2015;385(9962):55–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lancaster K, Cernigliaro D, Zulliger R, et al. HIV care and treatment experiences among female sex workers living with HIV in sub-Saharan Africa: A systematic review. Afr J AIDS Res. 2016;15(4):377–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mountain E, Mishra S, Vickerman P, et al. Antiretroviral Therapy Uptake, Attrition, Adherence, and Outcomes among HIV-infected Female Sex Workers: A Systematic Review and Meta-Analysis. PloS ONE. 2014;9(9):e105645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mountain E, Mishra S, Vickerman P, et al. The HIV care cascade and antiretroviral therapy in female sex workers: implications for HIV prevention. Expert Rev Anti Infect Ther. 2014:1–17. [DOI] [PubMed] [Google Scholar]
- 6.Surratt H, Grady C, Kurtz S, et al. HIV Testing and Engagement in Care among Highly Vulnerable Female Sex Workers: Implications for Treatment as Prevention Models. J Health Care Poor Underserved. 2014;25(3):1360–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strathdee SA, West BS, Reed E, et al. Substance use and HIV among Female Sex Workers and Female Prisoners: Risk environments and implications for prevention, treatment, policies. J Acquir Immune Defic Syndr. 2015;69(01):S110S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tran T, Detels R, Long H, et al. Drug use among female sex workers in Hanoi, Vietnam. Addiction. 2004;100:619–625. [DOI] [PubMed] [Google Scholar]
- 9.Chander G, Lau B, Moore R. Hazardous Alcohol Use: A Risk Factor for NonAdherence and Lack of Viral Suppression in HIV Infection. J Acquir Immune Defic Syndr. 2006;43(4):411–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Durvasula R, Miller T. Substance abuse treatment in persons with HIV/AIDS: Challenges in managing triple diagnosis. Behav Med. 2014;40(2):43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kipp A, Desruisseau A, Qian H. Non-injection Drug Use and HIV Disease Progression in the Era of Combination Antiretroviral Therapy. J Subst Abuse Treat. 2011;40(4):386–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jorquez J. The retirement phase of heroin using careers. J Drug Iss. 1983;13:343–365. [Google Scholar]
- 13.Stockman J, Strathdee S. HIV among People who Use Drugs: A Global Perspective of Populations at Risk. J Acquir Immune Defic Syndr. 2010;55(suppl 1):S17–S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stockdale S, Wells K, Tang L, et al. The Importance of Social Context: Neighborhood Stressors, Stress-Buffering Mechanisms, and Alcohol, Drug, and Mental Health Disorders. Soc Sci Med. 2007;65(9):1867–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Latkin C, Wallace M, Vlahov D, et al. People and Places: Behavioral Settings and Personal Network Characteristics as Correlates of Needle Sharing. J Acqui Immune Defic Synd. 1996;13(3):273–280. [DOI] [PubMed] [Google Scholar]
- 16.Cooper H, Tempalski B. Integrating place into research on drug use, drug user’s health, and drug policy. Int J Drug Policy. 2014;25(3):503–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rhodes T, Singer M, Bourgois P, et al. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–1044. [DOI] [PubMed] [Google Scholar]
- 18.Latkin C, Williams C, Wang J, et al. Neighborhood Social Disorder as a Determinant of Drug Injection Behaviors: A Structural Equation Modeling Approach. Health Psychol. 2005;24(1):96–100. [DOI] [PubMed] [Google Scholar]
- 19.Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. Int J Drug Policy. 2009;20:193–201. [DOI] [PubMed] [Google Scholar]
- 20.Williams C, Latkin C. Neighborhood Socioeconomica Status, Personal Network Attributes, and Use of Heroin and Cocaine. Am J Prev Med. 2007;32(6):S203S210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Freisthler B, Gruenewald P, Johnson F, et al. An exploratory study examining the spatial dynamics of illicit drug availability and rats of drug use. J Drug Educ. 2005;35(15–27). [DOI] [PubMed] [Google Scholar]
- 22.Heslin K, Singzon T, Famer M, et al. Therapy or treat? Inadvertent exposure to alcohol and illicit drug cues in the neighborhoods of sober living homes. Health Soc Care. 2013;21:500–508. [DOI] [PubMed] [Google Scholar]
- 23.Conners E, West B, Roth A, et al. Quantitative, Qualitative and Geospatial Methods to Characterize HIV Risk Environments. PLoS One. 2016;11(5):e0155693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pitpitan E, Kalichman S, Eaton L, et al. HIV/STI risk among venue-based female sex workers across the globe: a look back and the way forward. Curr HIV/AIDS Rep. 2013;10:65–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jain A, Saggurti N. The Extent and Nature of Fluidity in Typologies of Female Sex Work in Southern India: Implicatations for HIV Prevention Programs. J HIV AIDS Soc Serv. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerrigan D, Wirtz A, Baral S, et al. The Global HIV Epidemics among Sex Workers. Washington, DC: World Bank; 2013. [Google Scholar]
- 27.Shannon K, Rusch M, Shoveller J, et al. Mapping violence and policing as an environmental-structural barrier to health service and syringe availability among substance-using women in street-level sex work. Int J Drug Policy. 2008;19(2):140–147. [DOI] [PubMed] [Google Scholar]
- 28.Goldenberg S, Deering K, Amram O, et al. Community mapping of sex work criminalization and violence: impacts on HIV treatment interruptions among marginalized women living with HIV in Vancouver, Canada. INT J STD AIDS. 2017;28(10):1001–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deering K, Rusch M, Amram O, et al. Piloting a ‘Spatial Isolation Index: The Built Environment and Sexual and Drug Use Risks to Sex Workers. Int J Drug Policy. 2014;25(3):533–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kwan M-P. From place-based to people-based exposure measures. Soc Sci Med. 2009;69. [DOI] [PubMed] [Google Scholar]
- 31.Matthews S, Yang T. Spatial Polygamy and Contextual Exposures (SPACES): Promoting Activity Space Approaches in Research on Place and Health. Am Behav Sci. 2013;57:1057–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kwan M-P. Beyond Space (As We Knew It): Toward Temporally Integrated Geographies of Segregation, Health, and Accessibility. Ann Am Assoc Geogr. 2013;103(5):1078–1086. [Google Scholar]
- 33.Kawachi I, Berkman L, eds. Neighborhoods and Health. Oxford: Oxford University Press Inc.; 2003. [Google Scholar]
- 34.Kestens Y, Wasfi R, Naud A. “Contextualizing Context”: Reconciling Environmental Exposures, Social Networks, and Location Preferences in Health Research. Curr Environ Health Rep. 2017;4(1):51–60. [DOI] [PubMed] [Google Scholar]
- 35.Rojas P, Malow R, Ruffin B, et al. The HIV/AIDS Epidemic in the Dominican Republic: Key Contributing Factors. J Int Assoc Physicians AIDS Care (Chic). 2011;10(5):306–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carrasco M, Barrington C, Kennedy C, et al. ‘We talk, we do not have shame’: addressing stigma by reconstructing identiy through enchancing social cohesion among femalse sex workers living with HIV in the Dominican Republic. Cult Health Sex. 2017;19(5):543–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carrasco M, Nguyen T, Barrington C, et al. HIV Stimga Mediates the Association Between Social Cohesion and Consistent Condom Use Among Female Sex Workers Living with HIV in the Dominican Republic. Arch Sex Behav. 2018;47(5):1529–1539. [DOI] [PubMed] [Google Scholar]
- 38.Halperin D, Antonio de Moya E, Perez-Then E, et al. Understanding the HIV Epidemic in the Dominican Republic: A Prevnetion Success Story in the Caribbean? J Acquir Immune Defic Syndr. 2009;51:s52–s59. [DOI] [PubMed] [Google Scholar]
- 39.USAID. Dominican Republic: Country Operational Plan. USAID;2016. [Google Scholar]
- 40.Guilamo-Ramos V, Lee J, Ruiz Y, et al. Illicit drug use and HIV risk in the Dominican Republic: Tourism areas create drug use opportunities. Global Public Health. 2015;10(3):318–330. [DOI] [PubMed] [Google Scholar]
- 41.UNODC. World Drug Report. United Nationas Office on Drugs and Crime;2012. [Google Scholar]
- 42.IADACC. Dominican Republic evaluation of progress in drug control 2007–2009. Washington, D.C.: Inter-American Drug Abuse Control Commission;2010. [Google Scholar]
- 43.Budhwani H, Herald K, Milner A, et al. Transgender Women’s Drug Use in the Dominican Republic. Transgend Health. 2017;2(1):188–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Padilla M, Matiz-Reyes A, Colon-Burgos J. Adaption of Photovoice methodology to promote policy dialog among street-based drug users in Santo Domingo, Dominican Republic. Arts & Health. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Day M. A Situational Assessment of Responses to HIV and drug use from a Harm Reduction and Rights-Based Persepctive in Santo Domingo, Dominican Republic, Kingston, Jamaica, and Port of Spain Trinidad. The Caribbean Vulnerable Communities Coalition;2012. [Google Scholar]
- 46.Kerrigan D. Stigma, cohesion, and HIV outcomes among vulnerable women across epidemic settings. Dominican Republic: National Institute of Mental Health; 2016. [Google Scholar]
- 47.Kerrigan D, Sanchez Karver T, Muraleethran O, et al. “A dream come true”: Perspectives on long-acting injectable antiretroviral therapy among female sex workers living with HIV from the Dominican Republic and Tanzania. PloS ONE. 2020;15(6):e0234666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.USAID. Prioridades para los esfuerzos locale de control de VIH (PLACE) en la Republica Dominicana. Chapel Hill, NC: USAID;2014. [Google Scholar]
- 49.Culyba A, Guo W, Branas C, et al. Comparing residence-based to actual pathbased methods for defining adolescents environmental exposures using granular spatial data. Health Place. 2018;49:39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morrison C, Byrnes H, Miller B, et al. Assessing Individuals’ Exposure to Environmental Conditions Using Residence-based Measures, Activity Locationbased Measures, and Activity Path-based Measures. Epidemiology. 2019;30(2):166–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yelland L, Salter A, Ryan P. Performance of the modified Poisson regression approach for estimating relative risk from clustered prospective data. Am J Epidemiol. 2011;174(8):984–992. [DOI] [PubMed] [Google Scholar]
- 52.Hardin J, Hilbe J. Generalized Estimating Equations (GEE). Second Edition ed. New York: Chapman and Hall/CRC; 2013. [Google Scholar]
- 53.Bohn M, Babor T, Kranzler H. The Alcohol Use Disorder Identification Test (AUDIT): validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol and Drugs. 1995;56(4). [DOI] [PubMed] [Google Scholar]
- 54.Sampson R, Morenoff J, Gannon-Rowley T. Assessing “Neighborhood Effects”: Social Processes and New Directions in Research. Annu Rev Sociol. 2002;28(1):443–478. [Google Scholar]
- 55.Yabiku S, Rayle A, Okamat S, et al. The Effect of Neighborhood Context on the Drug Use of American Indian Youth of the Southwest. J Ethn Sust Abuse. 2007;6(2):181–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Goldenberg S, Strathdee S, Gallardo M, et al. How important are venue-based HIV risks among male clients of female sex workers? A mixed methods analysisof the risk environment in nightlife venues in Tijuana, Mexico. Health Place. 2011;17(3):748–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Duncan M, Mummery K. GIS or GPS? A Comparison of Two Methods For Assessing Route Taken During Activity Transport. Am J Prev Med. 2007;33(1). [DOI] [PubMed] [Google Scholar]
- 58.Shrestha S, Kestens Y, Thomas F, et al. Spatial access to sport facilities from the multiple places visited and sport practice: Assessing and correcting biases related to selective daily mobility. Soc Sci Med. 2019;236:112406. [DOI] [PubMed] [Google Scholar]
- 59.Kerrigan D, Moreno L, Rosario S, et al. Environmental-Structural Interventions to Reduce HIV/STI Risk Among Female Sex Workers in the Dominican Republic. Am J Public Health. 2003;96(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Beattie T, Bhattacharjee P, Ramesh B, et al. Violence against female sex workers in Karnataka state, south India: impact on health, and reductions in violence following an intervention program. BMC Public Health. 2010;10(476). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tenni B, Capenter J, Thomson N. HIV: Fostering Partnerships between Sex Workers and Police to Reduce HIV Risk and Promote Professionalization within Police Institutions: A Realist Review. PloS ONE. 2015;10(10). [DOI] [PMC free article] [PubMed] [Google Scholar]