Abstract
Background
Telomerase reverse transcriptase (TERT) gene promoter mutations have been explored, as biomarkers of improved survival for patients with cancer receiving immune checkpoint inhibitors. We sought to investigate their prevalence by race and sex across different cancer types to inform patient selection in clinical trials.
Results
In this observational study, 31 925 patients with cancer underwent next-generation sequencing of their tumors with 88% (27 970) patients self-reported being Whites, 7.1% (2273) Asians, and 5.3% (1682) Blacks. Examining the distribution of TERT promoter mutations by race, White patients with melanoma harbored more TERT promoter mutations than Asian and Black patients (OR = 25.83; 95%CI, 6.84-217.42; P < .001). In contrast, Asian patients with head and neck cancer (HNC) harbored more TERT promoter mutations compared to White patients (OR = 2.47; 95%CI, 1.39-4.37; P = .004). In addition, the distribution of TERT promoter mutations differed by sex. Males were enriched for TERT gene promoter mutations compared to females with melanoma (OR = 1.82; 95%CI, 1.53-2.16; P < .001), cancer of unknown primary (OR = 1.96; 95%CI, 1.43-2.69; P < .001), hepatobiliary (OR = 3.89; 95%CI, 2.65-5.69; P < .001), and thyroid cancers (OR = 1.42; 95%CI, 1.10-1.84; P = .0087), while females were more enriched for TERT promoter mutations compared to males for HNC (OR = 0.56; 95%CI, 0.39-0.81; P = .0021).
Conclusions
The prevalence of TERT gene promoter mutations varies among patients with cancer based on race and sex. These findings inform our understanding of cancer biology and can assist in the design of future clinical trials that leverage drugs targeting TERT promoter dependencies.
Keywords: TERT mutation, disparities in cancer care, immune checkpoint inhibitor
TERT gene promoter mutations have been explored as biomarkers of improved survival for patients with cancer receiving immune checkpoint inhibitors. This article reports their prevalence by race and sex across different cancer types to inform patient selection in clinical trials.
Implications for Practice.
The findings of this study illustrate that there are major differences in the prevalence of TERT promoter mutations in various cancer types across patient populations when stratifying them by sex and ethnic groups. The data presented in this work highlight the necessity of investing more resources in mutation analyses of non-White populations. These efforts will mitigate racial disparities, assist in equitable future clinical trial design, and potentially lead to better biological insights that can justify the observed differences in mutational landscapes.
Introduction
Telomerase is a reverse transcriptase that synthesizes the 3ʹ end of linear chromosomes.1,2 In human somatic cells, telomeres shorten with each cellular replication, as DNA polymerase cannot fully replicate the 3ʹ end of DNA.3,4 Telomere shortening is a cardinal feature of the aging process, where cells undergo senescence, apoptosis, or genomic instability.5 Telomerase counteracts this process by adding telomeres and is inhibited in most normal human cells across different tissue types. Exceptions include continually regenerating cells (eg, stratum basalis of the skin, testes, or ovaries) and cells seeking to maintain cell proliferation and avoid senescence (ie, cancer cells).6,7
The telomerase reverse transcriptase (TERT) gene encodes the enzymatic subunit of the telomerase complex.8 In cancer cells, activating mutations in the TERT promoter region can increase TERT protein production and the subsequent activity of telomerase, resulting in increased telomere length.9 Many studies have investigated the regulation of TERT in healthy tissues and its aberrant expression in malignant cells.10-13 In addition, by promoting the epithelial-mesenchymal transition,14TERT promoter mutations can increase PD-L1 expression15 and thus increase response to ICI therapy. While genetic risk assessments in the clinic do not routinely test for TERT promoter mutations, currently, the notion is gaining traction as a strategy for helping determine prognosis.16 In the era of immune checkpoint inhibitors (ICIs), De Kouchkovsky et al17 recently suggested that the presence of TERT promoter mutations in urothelial cancer was a predictor of improved overall survival in a cohort of 119 patients treated with ICIs. In addition, a recent pan-cancer analysis of 10 336 patients sequenced using MSK-IMPACT showed variability in the prevalence of TERT mutations across cancer types and found an association between the presence of TERT promoter mutations and higher tumor mutational burden (TMB) and neoantigen load. The authors also noted better overall survival outcomes with anti-CTLA4 therapy, among patients with melanoma harboring TERT promoter mutations.18
Given the importance of TERT promoter mutations in cancer development and their potential use as a biomarker for clinical outcomes and response to treatment with ICIs, we investigated the distribution of TERT promoter mutations by sex and race across different solid tumors. Their prevalence across specific groups of patients can potentially guide future patient selection in clinical trials and therapeutic strategies.
Methods
Study Design
Patients diagnosed with 1 of the 10 solid tumors most commonly harboring TERT gene promoter mutations (thyroid cancer, soft-tissue sarcoma, non-small cell lung cancer (NSCLC), melanoma, hepatobiliary cancer (HPBC), head and neck cancer (HNC), glioma, colorectal cancer, cancer of unknown primary, and bladder cancer) were identified from the American Association for Cancer Research (AACR) Project Genomics Evidence Neoplasia Information Exchange (GENIE) 11.0-registry.19 As the bait-set coverage of the TERT gene was available from Dana-Farber Cancer Institute (DFCI) and Memorial Sloan Kettering Cancer Center (MSKCC), we selected patients from these 2 cancer centers for this analysis. All patients underwent next-generation sequencing of tumors with CLIA-/ISO-certified panels obtained from the respective institution from which they were recruited. Mutational analyses in this study were focused on TERT promoter mutations. Patients whose tumors were sequenced using DFCI OncoPanel version 1 were excluded, because it does not cover the entire TERT gene sequence. Methodology for tissue collection, DNA extraction and sequencing using the DFCI-ONCOPANEL, and MSK-IMPACT for DFCI and MSKCC patients, respectively, were previously described in detail.20-23 Additional details on methodology are provided in Supplementary material.
Statistical Analysis
The prevalence of TERT promoter mutations was summarized as “N” and percentage by sex and race across different solid tumors. The strength of associations was quantified as the odds ratio (OR) with 95% confidence intervals (95%); 2-sided Fisher’s exact tests were applied. FDR-adjusted Q-values were also calculated to correct P-values using the Benjamini-Hochberg method. P-values < .05 were considered significant as long as they maintained a Q-value < .05 on multiple test corrections.
Results
A total of 31 925 patients from DFCI and MSKCC were included (Table 1; Supplementary Table S1). In our cohort, 88% (27 970) patients self-reported being Whites, 7.1% (2273) Asians, and 5.3% (1682) Blacks. TERT promoter mutations were identified in 56% (1346/2411) bladder cancers, 43% (966/2243) melanomas, 39% (1403/3614) gliomas, 41% (395/959) thyroid cancers, and 23% (183/782) HNC (Fig. 1; Supplementary Table S2).
Table 1.
Clinical and pathological characteristics of the 31 925 patients with cancer and available TERT sequencing data.
| Patients with cancer | n | Percent (%) |
|---|---|---|
| Sex | ||
| Female | 15 350 | 48.1 |
| Male | 16 575 | 51.9 |
| Self-reported race | ||
| Asian | 2273 | 7.1 |
| Black | 1682 | 5.3 |
| White | 27 970 | 87.6 |
| Type | ||
| Non-small cell lung cancer | 9434 | 29.6 |
| Colorectal cancer | 6311 | 19.8 |
| Glioma | 3614 | 11.3 |
| Soft tissue sarcoma | 2466 | 7.7 |
| Bladder cancer | 2411 | 7.6 |
| Melanoma | 2243 | 7.0 |
| Cancer of unknown primary | 2137 | 6.7 |
| Hepatobiliary cancer | 1568 | 4.9 |
| Thyroid cancer | 959 | 3.0 |
| Head and neck cancer | 782 | 2.4 |
Figure 1.
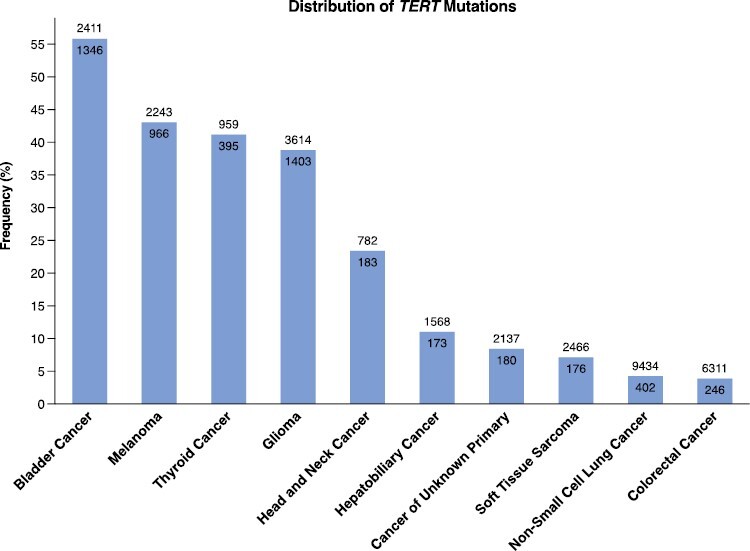
The distribution of TERT promoter mutations across the top 10 cancer types.
Examining the differences in the distribution of TERT promoter mutations by race, it was notable that there were differential distributions among patients with the same cancer type but belonging to different racial groups (Supplementary Tables S3 and S4). For example, White patients with melanoma (44%, n = 964/2176) harbored more TERT promoter mutations compared to Asian and Black patients (3%, n = 2/67) (OR = 25.83; 95%CI, 6.84-217.42; Q < .001) (Supplementary Table S4). Similarly, TERT promoter mutations were differentially enriched among patients by sex (Supplementary Table S5). TERT promoter mutations were significantly more frequent among male patients as compared to their female counterparts with melanoma (49%, n = 638/1298 vs. 35%, n = 328/945, respectively) (OR = 1.82; 95%CI, 1.53-2.16; Q < .001), HPBC (17%, n = 137/827 vs. 4.9%, n = 36/741, respectively) (OR = 3.89; 95%CI, 2.65-5.69; Q < .001), cancer of unknown primary (11%, n = 116/1065 vs. 5.9%, n = 64/1081, respectively) (OR = 1.96; 95%CI, 1.43-2.69; Q < .001), and thyroid cancer (46%, n = 213/468 vs. 37%, n = 182/491, respectively) (OR = 1.42; 95%CI, 1.10-1.84; Q = .017). In contrast, male patients with HNC (21%, n = 118/575) harbored significantly fewer TERT promoter mutations than female patients (31%, n = 65/207) (OR = 0.56; 95%CI, 0.39-0.81; Q = .005) (Fig. 2). When examining patients by ethnicity, there were no significant differences in the distribution of TERT promoter mutations between Hispanic and non-Hispanic patients (Supplementary Table S6).
Figure 2.
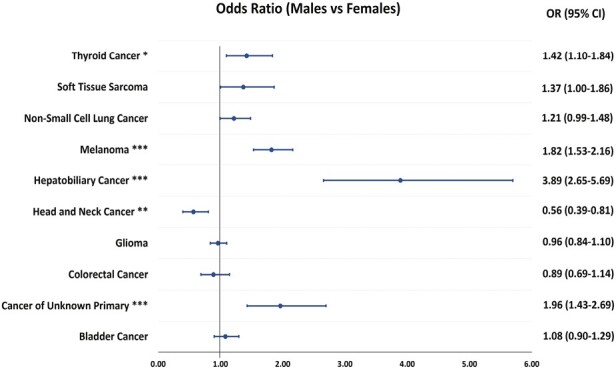
The frequency of TERT promoter mutations in solid tumors among males compared to females. Abbreviations: OR: Odds ratio; 95%CI: 95% confidence interval; *Q-value < 005; **Q-value < .01; ***Q-value < .001.
Furthermore, TERT promoter mutations differed between males and females within the same race or between different racial groups in patients with the same sex. For example, TERT promoter mutations occurred more often in White males with HPBC (16%, n = 112/692) compared to their female counterparts (4.9%, n = 31/635) (OR = 3.76; 95%CI, 2.49-5.69; Q < .001), and Black males (28%, n = 13/46) harbored more TERT promoter mutations than Black females (4.1%, n = 2/49) (OR = 9.26; 95%CI, 1.96-43.9; Q = 0.008) (Fig. 3; Supplementary Table S7). Whereas in patients with HNC, Asian males (37%, n = 22/60) were significantly more enriched for TERT promoter mutations relative to White males (19%, n = 93/489) (OR = 2.47; 95%CI, 1.39-4.37; P = .004) (Fig. 3; Supplementary Table S7). No significant differences in TERT promoter mutations distribution were determined across racial and sex subgroups among patients with glioma, soft-tissue sarcoma, bladder, colorectal, NSCLC, and thyroid cancers (Fig. 3; Supplementary Table S7). Further exploration of HNC tumors revealed that oral cavity squamous cell carcinoma (OSCC) tumors (44%, n = 85/192) were associated with higher TERT promoter mutations vs. other HNC subtypes (17%, n = 98/590) (OR = 3.98; 95%CI, 2.74-5.79; Q = .03). Asian patients with OSCC (70%, n = 14/20) harbored more mutations vs. non-Asian patients with OSCC (41%, n = 71/172) (OR = 3.3; 95%CI, 1.2-9.0; P = .019) (Supplementary Table S8).
Figure 3.

The frequency of TERT promoter mutations in different subgroups across cancer types.
Finally, the distribution of TERT promoter mutations was compared between primary and metastatic tumor samples. Mutations were significantly more frequent among samples from primary tumors as compared with samples from metastatic tumors in patients with bladder cancer (58.4%, n = 1076/1843 vs. 38.3%, n = 270/559, respectively) (OR = 1.5; 95%CI, 1.2-1.8; Q < .001), cancer of unknown primary (12.6%, n = 33/261 vs. 8.2%, n = 133/1613, respectively) (OR = 1.6; 95%CI, 1.1-2.4; Q = .0248), colorectal cancer (4.5%, n = 191/4219 vs. 2.5%, n = 51/2053, respectively) (OR = 1.9, 95%CI, 1.4-2.6; Q < .001), glioma (42.3%, n = 1287/3039 vs. 25.3%, n = 102/403, respectively) (OR = 2.2; 95%CI, 1.7-2.7; Q < .001), HNC (27.4%, n = 116/423 vs. 19%, n = 67/352, respectively) (OR = 1.6; 95%CI, 1.1-2.3; Q = .0091), HPBC (13.3%, n = 148/966 vs. 5.8%, n = 25/433, respectively) (OR = 2.5; 95%CI, 1.6-3.9; Q < 0.001). However, samples from primary tumors were significantly less enriched with TERT promoter mutations than those from metastatic tumors in patients with melanoma (31%, n = 223/720 vs. 49.6%, n = 741/1495, respectively) (OR = 0.5; 95%CI, 0.4-0.6; Q < .001), soft-tissue sarcoma (6.3%, n = 99/1578 vs. 8.9%, n = 75/838, respectively) (OR = 0.7, 95%CI, 0.5-0.9; Q = .03), and thyroid cancer (35.2%, n = 177/503 vs. 48%, n = 217/452, respectively) (OR = 0.6; 95%CI, 0.5-0.8; Q < .001) (Supplementary Fig. S1; Supplementary Table S9,). The distribution of TERT promoter mutations were also evaluated across race and sex groups in primary (Supplementary Table S10) and metastatic (Supplementary Table S11) samples, respectively.
Discussion
In this study, we report for the first time, differences in the distribution of TERT promoter mutations by race and sex across different cancer types. Our findings reveal that TERT promoter mutations are frequent events in many cancer types, including bladder cancer, melanoma, thyroid cancer, glioma, and HNC. TERT promoter mutations are found to be more prevalent among male patients than their female counterparts with most cancer types, except for HNC where the opposite held true. Additional noteworthy results include a more significant enrichment among patients of White race with melanoma and patients of Asian race with HNC, particularly OSCC.
The prevalence of TERT promoter mutations in melanoma varies between 29% and 71%.24,25 In our cohort, 43% of 2243 melanoma cases harbored TERT promoter mutations. A higher frequency of TERT mutations among male patients in melanoma compared with their female counterparts has been described.26 In addition, our findings reveal ethnic differences in this disease, with patients of White race carrying significantly more TERT promoter mutations compared to other groups. Variations in skin color and the protective effects of darker skin against ultraviolet radiation may counterpart some of this difference.27 Griewank et al28 found a considerably higher frequency of TERT promoter mutations in cutaneous melanomas of UV-exposure-prone areas than in tumors arising in areas with minimal or absent sun exposure.
Other factors may be implicated in these differences based on race. For example, TERT promoter mutations have been associated with increased patient age at diagnosis, as well as increased Breslow thickness, tumor ulceration, and tumor growth rate in patients with melanoma.28-31 In keeping with this, more adverse outcomes and worse survival have been consistently reported among patients with melanoma who harbor TERT promoter mutations compared to those who do not.28,32,33 However, it is notable that Black patients have a higher prevalence of advanced cutaneous melanoma34 with worse pathologic features (ie, tumor ulceration and satellite nodules) and regional and distant metastases.35-37 Rouhani et al38 demonstrated that Black patients presented with a significantly later stage at their time of diagnosis with melanoma compared with White American patients. As such, Black patients might also have worse outcomes due to underlying health disparities and access to care that may have led to delays in diagnosis and treatment compared to groups of patients who have more access to screening, such as skin examinations.39 This may explain why White patients continue to demonstrate better overall survival than non-White groups across different melanoma subtypes, irrespective of TERT promoter mutations.34,36,40
Regarding HNC, Yu et al41 found a mutation rate of 81% in 74 patients with OSCC. TERT promoter mutations were also found to be associated with an increased risk of locoregional failure (subdistribution HR = 2.82; 95%CI, 1.47-5.42; P = .0019) independent of oral cavity primary site and TP53 mutation status. Our study included a larger sample size and found a mutation rate of 44.27% of 192 OSCC with a frequency of 70% in OSCC in Asian patients (n = 20).
While certain cancer types (ie, HNC and HPBC) exhibited a higher rate of TERT promoter mutations in primary tumor samples compared to metastatic samples, mutations were more prevalent in metastatic samples of melanoma and thyroid cancer compared to primary tumors. Prior work by Morris et al42 showed that metastatic HNC tumors demonstrated a higher prevalence of TERT promoter mutations compared to primary tumors. Whereas Hugdahl et al43 found no significant difference in mutation distribution between primary and metastatic melanoma tumors. In addition, Yang et al44 showed that TERT mutant thyroid cancers were linked to a higher occurrence of distant metastasis at the time of diagnosis. Given that primary and metastatic samples may have different genomic alterations, it is imperative that future studies highlight the development of TERT promoter mutations throughout the course of tumor development and its progression to further understand the relationship of these mutations with tumor aggressiveness and spread.
Overall, our results add to the growing body of the literature that serves to enhance our understanding of the variation in TERT promoter mutations across cancer types, sex, and race. Our study has several limitations, as it included patients from tertiary academic centers who may be enriched for unique features based on referral or geographic patterns. In addition, the analyses performed relied on subjective self-reported race, rather than objective parameters (ie, ancestry). However, ancestry-based approaches have similarly found differences in the rate of TERT promoter mutations across ancestral groups. Arora et al45 recently demonstrated that patients with glioblastoma multiforme and hepatocellular carcinoma with east Asian ancestry had lower frequency of TERT promoter mutations compared to patients with European ancestry. Moreover, data on TMB were not available, and we were unable to adjust for it when examining the incidence of TERT promoter mutations across subgroups. Patients with high TMB are more likely to display genomic alterations,46 which may have affected their distribution across different groups. It is also noteworthy to highlight that the reporting of TERT promoter mutations may be significantly influenced by intratumoral heterogeneity especially when examining differences between localized tumor and metastatic specimens. Finally, heterogeneity in tumor subtypes which may have not been fully reported (ie, melanoma) may have introduced bias into our subgroups and subsequent analyses.
In conclusion, our study demonstrates distinct differences in their distribution by sex and race across several cancer types. It will be essential to account for these variations when launching future trials to assess the impact of these mutations on clinical outcomes and their use as a biomarker.
Supplementary Material
Contributor Information
Talal El Zarif, Lank Center for Genitourinary Oncology, Dana-Farber Cancer Institute, Boston, MA, USA; Department of Medicine, Harvard Medical School, Boston, MA, USA; Department of Internal Medicine, Yale New Haven Hospital, New Haven, CT, USA.
Marc Machaalani, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon.
Rashad Nawfal, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon.
Amin H Nassar, Department of Hematology/Oncology, Yale New Haven Hospital, New Haven, CT, USA.
Wanling Xie, Department of Data Sciences, Dana-Farber Cancer Institute, Boston, MA, USA.
Toni K Choueiri, Lank Center for Genitourinary Oncology, Dana-Farber Cancer Institute, Boston, MA, USA; Department of Medicine, Harvard Medical School, Boston, MA, USA.
Mark Pomerantz, Lank Center for Genitourinary Oncology, Dana-Farber Cancer Institute, Boston, MA, USA; Department of Medicine, Harvard Medical School, Boston, MA, USA.
Funding
None.
Conflict of Interest
T.E.Z. received honoraria from art tempi for work unrelated to this work. W.X. serves as consultant for Convergent Therapeutics, Inc. T.K.C. reports institutional and/or personal, paid and/or unpaid support for research, advisory boards, consultancy, and honoraria from Alkermes, AstraZeneca, Aravive, Aveo, Bayer, Bristol Myers-Squibb, Calithera, Circle Pharma, Eisai, EMD Serono, Exelixis, GlaxoSmithKline, Gilead, IQVA, Infinity, Ipsen, Jansen, Kanaph, Lilly, Merck, Nikang, Nuscan, Novartis, Pfizer, Roche, Sanofi/Aventis, Scholar Rock, Surface Oncology, Takeda, Tempest, Up-To-Date, CME events (Peerview, OncLive, MJH, and others), outside the submitted work. Institutional patents filed on molecular alterations and immunotherapy response/toxicity, and ctDNA. Equity: Tempest, Pionyr, Osel, Precede Bio, CureResponse. Committees: NCCN, GU Steering Committee, ASCO/ESMO, ACCRU, KidneyCan. Medical writing and editorial assistance support may have been funded by Communications companies in part. No speaker’s bureau. Mentored several non-US citizens on research projects with potential funding (in part) from non-US sources/Foreign Components. The institution (Dana-Farber Cancer Institute) may have received additional independent funding of drug companies or/and royalties potentially involved in research around the subject matter. T.K.C. is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE (2P50CA101942-16) and Program 5P30CA006516-56, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, Pan Mass Challenge, Hinda and Arthur Marcus Fund, and Loker Pinard Funds for Kidney Cancer Research at DFCI. The other authors indicated no financial relationships.
Author Contributions
Conception/design: all authors. Provision of study material or patients: T.E.Z., M.M., R.N. Collection and/or assembly of data: T.E.Z., M.M., R.N. Data analysis and interpretation: all authors. Manuscript writing and final approval of manuscript: all authors.
Data Availability
The data underlying this article are available in the article and in Supplementary material.
References
- 1. Greider CW, Blackburn EH.. Identification of a specific telomere terminal transferase activity in tetrahymena extracts. Cell. 1985;43(2 Pt 1):405-413. 10.1016/0092-8674(85)90170-9 [DOI] [PubMed] [Google Scholar]
- 2. Yu GL, Bradley JD, Attardi LD, Blackburn EH.. In vivo alteration of telomere sequences and senescence caused by mutated tetrahymena telomerase RNAs. Nature. 1990;344(6262):126-132. 10.1038/344126a0 [DOI] [PubMed] [Google Scholar]
- 3. Cong YS, Wright WE, Shay JW.. Human telomerase and its regulation. Microbiol Mol Biol Rev. 2002;66(3):407-425, table of contents. 10.1128/MMBR.66.3.407-425.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Olovnikov AM. A theory of marginotomy. The incomplete copying of template margin in enzymic synthesis of polynucleotides and biological significance of the phenomenon. J Theor Biol. 1973;41(1):181-190. 10.1016/0022-5193(73)90198-7 [DOI] [PubMed] [Google Scholar]
- 5. Stewart SA, Weinberg RA.. Telomerase and human tumorigenesis. Semin Cancer Biol. 2000;10(6):399-406. 10.1006/scbi.2000.0339 [DOI] [PubMed] [Google Scholar]
- 6. Kim NW, Piatyszek MA, Prowse KR, et al. Specific association of human telomerase activity with immortal cells and cancer. Science. 1994;266(5193):2011-2015. 10.1126/science.7605428 [DOI] [PubMed] [Google Scholar]
- 7. Kolquist KA, Ellisen LW, Counter CM, et al. Expression of TERT in early premalignant lesions and a subset of cells in normal tissues. Nat Genet. 1998;19(2):182-186. 10.1038/554 [DOI] [PubMed] [Google Scholar]
- 8. Daniel M, Peek GW, Tollefsbol TO.. Regulation of the human catalytic subunit of telomerase (hTERT). Gene. 2012;498(2):135-146. 10.1016/j.gene.2012.01.095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Heidenreich B, Kumar R.. TERT promoter mutations in telomere biology. Mut Res Rev Mut Res. 2017;771:15-31. 10.1016/j.mrrev.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 10. Ducrest AL, Szutorisz H, Lingner J, Nabholz M.. Regulation of the human telomerase reverse transcriptase gene. Oncogene. 2002;21(4):541-552. 10.1038/sj.onc.1205081 [DOI] [PubMed] [Google Scholar]
- 11. Greenberg RA, O’Hagan RC, Deng H, et al. Telomerase reverse transcriptase gene is a direct target of c-Myc but is not functionally equivalent in cellular transformation. Oncogene. 1999;18(5):1219-1226. 10.1038/sj.onc.1202669 [DOI] [PubMed] [Google Scholar]
- 12. Kyo S, Takakura M, Fujiwara T, Inoue M.. Understanding and exploiting hTERT promoter regulation for diagnosis and treatment of human cancers. Cancer Sci. 2008;99(8):1528-1538. 10.1111/j.1349-7006.2008.00878.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lin SY, Elledge SJ.. Multiple tumor suppressor pathways negatively regulate telomerase. Cell. 2003;113(7):881-889. 10.1016/s0092-8674(03)00430-6 [DOI] [PubMed] [Google Scholar]
- 14. Stern JL, Hibshman G, Hu K, et al. Mesenchymal and MAPK expression signatures associate with telomerase promoter mutations in multiple cancers. Mol Cancer Res. 2020;18(7):1050-1062. 10.1158/1541-7786.MCR-19-1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mak MP, Tong P, Diao L, et al. A patient-derived, pan-cancer EMT signature identifies global molecular alterations and immune target enrichment following epithelial-to-mesenchymal transition. Clin Cancer Res. 2016;22(3):609-620. 10.1158/1078-0432.CCR-15-0876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Śledzińska P, Bebyn MG, Furtak J, Kowalewski J, Lewandowska MA.. Prognostic and predictive biomarkers in gliomas. Int J Mol Sci. 2021;22(19). 10.3390/ijms221910373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. de Kouchkovsky I, Zhang L, Philip EJ, et al. TERT promoter mutations and other prognostic factors in patients with advanced urothelial carcinoma treated with an immune checkpoint inhibitor. J ImmunoTher Cancer. 2021;9(5):e002127. 10.1136/jitc-2020-002127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Li H, Li J, Zhang C, Zhang C, Wang H.. TERT mutations correlate with higher TMB value and unique tumor microenvironment and may be a potential biomarker for anti-CTLA4 treatment. Cancer Med. 2020;9(19):7151-7160. 10.1002/cam4.3376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. AACR Project GENIE Consortium. AACR Project GENIE: Powering Precision Medicine through an International Consortium. Cancer Discov. 2017;7(8):818-831. 10.1158/2159-8290.Cd-17-0151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Garcia EP, Minkovsky A, Jia Y, et al. Validation of OncoPanel: a targeted next-generation sequencing assay for the detection of somatic variants in cancer. Arch Pathol Lab Med. 2017;141(6):751-758. 10.5858/arpa.2016-0527-OA [DOI] [PubMed] [Google Scholar]
- 21. Sholl LM, Do K, Shivdasani P, et al. Institutional implementation of clinical tumor profiling on an unselected cancer population. JCI Insight 2016;1(19):e87062. 10.1172/jci.insight.87062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zehir A, Benayed R, Shah RH, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med. 2017;23(6):703-713. 10.1038/nm.4333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zehir A, Benayed R, Shah RH, et al. Erratum: mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med. 2017;23(8):1004. 10.1038/nm0817-1004c [DOI] [PubMed] [Google Scholar]
- 24. Vinagre J, Almeida A, Pópulo H, et al. Frequency of TERT promoter mutations in human cancers. Nat Commun. 2013;4:2185. 10.1038/ncomms3185 [DOI] [PubMed] [Google Scholar]
- 25. Huang FW, Hodis E, Xu MJ, et al. Highly recurrent TERT promoter mutations in human melanoma. Science. 2013;339(6122):957-959. 10.1126/science.1229259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li J, Li Z, Zhang C, Zhang C, Wang H.. Male patients with TERT mutation may be more likely to benefit from immunotherapy, especially for melanoma. Aging (Albany NY). 2020;12(17):17288-17294. 10.18632/aging.103684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cress RD, Holly EA.. Incidence of cutaneous melanoma among non-Hispanic whites, Hispanics, Asians, and blacks: an analysis of California Cancer Registry Data, 1988-93. Cancer Causes Control. 1997;8(2):246-252. 10.1023/a:1018432632528 [DOI] [PubMed] [Google Scholar]
- 28. Griewank KG, Murali R, Puig-Butille JA, et al. TERT promoter mutation status as an independent prognostic factor in cutaneous melanoma. J Natl Cancer Inst. 2014;106(9). 10.1093/jnci/dju246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Heidenreich B, Nagore E, Rachakonda PS, et al. Telomerase reverse transcriptase promoter mutations in primary cutaneous melanoma. Nat Commun. 2014;5:3401. 10.1038/ncomms4401 [DOI] [PubMed] [Google Scholar]
- 30. Nagore E, Heidenreich B, Requena C, et al. TERT promoter mutations associate with fast-growing melanoma. Pig Cell Melanoma Res. 2016;29(2):236-238. 10.1111/pcmr.12441 [DOI] [PubMed] [Google Scholar]
- 31. Pópulo H, Boaventura P, Vinagre J, et al. TERT promoter mutations in skin cancer: the effects of sun exposure and X-irradiation. J Invest Dermatol. 2014;134(8):2251-2257. 10.1038/jid.2014.163 [DOI] [PubMed] [Google Scholar]
- 32. Horn S, Figl A, Rachakonda PS, et al. TERT promoter mutations in familial and sporadic melanoma. Science. 2013;339(6122):959-961. 10.1126/science.1230062 [DOI] [PubMed] [Google Scholar]
- 33. Motaparthi K, Kim J, Andea AA, et al. TERT and TERT promoter in melanocytic neoplasms: current concepts in pathogenesis, diagnosis, and prognosis. J Cutan Pathol. 2020;47(8):710-719. 10.1111/cup.13691 [DOI] [PubMed] [Google Scholar]
- 34. Dawes SM, Tsai S, Gittleman H, Barnholtz-Sloan JS, Bordeaux JS.. Racial disparities in melanoma survival. J Am Acad Dermatol. 2016;75(5):983-991. 10.1016/j.jaad.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 35. Byrd KM, Wilson DC, Hoyler SS, Peck GL.. Advanced presentation of melanoma in African Americans. J Am Acad Dermatol. 2004;50(1):21-4; discussion 142-3. 10.1016/s0190-9622(03)02091-7 [DOI] [PubMed] [Google Scholar]
- 36. Cormier JN, Xing Y, Ding M, et al. Ethnic differences among patients with cutaneous melanoma. Arch Intern Med. 2006;166(17):1907-1914. 10.1001/archinte.166.17.1907 [DOI] [PubMed] [Google Scholar]
- 37. Hu S, Soza-Vento RM, Parker DF, Kirsner RS.. Comparison of stage at diagnosis of melanoma among Hispanic, black, and white patients in Miami-Dade County, Florida. Arch Dermatol. 2006;142(6):704-708. 10.1001/archderm.142.6.704 [DOI] [PubMed] [Google Scholar]
- 38. Rouhani P, Hu S, Kirsner RS.. Melanoma in Hispanic and black Americans. Cancer Control. 2008;15(3):248-253. 10.1177/107327480801500308 [DOI] [PubMed] [Google Scholar]
- 39. Martires KJ, Kurlander DE, Minwell GJ, Dahms EB, Bordeaux JS.. Patterns of cancer screening in primary care from 2005 to 2010. Cancer. 2014;120(2):253-261. 10.1002/cncr.28403 [DOI] [PubMed] [Google Scholar]
- 40. Wang Y, Zhao Y, Ma S.. Racial differences in six major subtypes of melanoma: descriptive epidemiology. BMC Cancer. 2016;16(1):691. 10.1186/s12885-016-2747-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yu Y, Fan D, Song X, et al. TERT promoter mutations are enriched in oral cavity cancers and associated with locoregional recurrence. JCO Precis Oncol. 2021:5. 10.1200/po.20.00515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Morris LGT, Chandramohan R, West L, et al. The molecular landscape of recurrent and metastatic head and neck cancers: insights from a precision oncology sequencing platform. JAMA Oncol. 2017;3(2):244-255. 10.1001/jamaoncol.2016.1790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hugdahl E, Kalvenes MB, Mannelqvist M, Ladstein RG, Akslen LA.. Prognostic impact and concordance of TERT promoter mutation and protein expression in matched primary and metastatic cutaneous melanoma. Br J Cancer. 2018;118(1):98-105. 10.1038/bjc.2017.384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yang H, Park H, Ryu HJ, et al. Frequency of TERT promoter mutations in real-world analysis of 2,092 thyroid carcinoma patients. Endocrinol Metab (Seoul). 2022;37(4):652-663. 10.3803/EnM.2022.1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Arora K, Tran TN, Kemel Y, et al. Genetic ancestry correlates with somatic differences in a real-world clinical cancer sequencing cohort. Cancer Discov. 2022;12(11):2552-2565. 10.1158/2159-8290.CD-22-0312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chalmers ZR, Connelly CF, Fabrizio D, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 2017;9(1):34. 10.1186/s13073-017-0424-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in Supplementary material.


