Abstract
Introduction
The COVID-19 pandemic turned biological hazards in the working environment into a global concern. This systematized review of published reviews aimed to provide a comprehensive overview of the specific jobs and categories of workers exposed to biological hazards with the related prevention.
Methods
We extracted reviews published in English and French in PubMed, Embase, and Web of Science. Two authors, working independently, subsequently screened the potentially relevant titles and abstracts recovered (step 1) and then examined relevant full texts (step 2). Disagreements were resolved by consensus. We built tables summarizing populations of exposed workers, types of hazards, types of outcomes (types of health issues, means of prevention), and routes of transmission.
Results
Of 1426 studies initially identified, 79 studies by authors from every continent were selected, mostly published after 2010 (n = 63, 79.7%). About half of the reviews dealt with infectious hazards alone (n = 38, 48.1%). The industrial sectors identified involved healthcare alone (n = 16), laboratories (n = 10), agriculture (including the animal, vegetable, and grain sectors, n = 32), waste (n = 10), in addition of 11 studies without specific sectors. The results also highlighted a range of hazards (infectious and non-infectious agents, endotoxins, bioaerosols, organic dust, and emerging agents).
Conclusion
This systematized overview allowed to list the populations of workers exposed to biological hazards and underlined how prevention measures in the healthcare and laboratory sectors were usually well defined and controlled, although this was not the case in the agriculture and waste sectors. Further studies are necessary to quantify these risks and implement prevention measures that can be applied in every country.
Keywords: Biological risk, Biosafety, Endotoxins, Exposure, Occupational setting
1. Introduction
Biological hazards, both infectious and non-infectious, constitute significant threats to health in numerous industrial sectors and workplaces around the world, often leading to occupational and work-related diseases [[1], [2], [3], [4]]. During the COVID-19 pandemic, controlling biological risks in working environments became a global priority and revealed the urgent need to develop standards and guidelines for managing them [5]. In the context of drafting technical guidelines on biological hazards for the International Labor Organization, the importance of having a global vision has been stressed, and in particular, the need of a systematic view of the occurrence of biological risk in the workplace, with an inventory of the jobs and categories of workers exposed to it and related prevention measures. We, therefore, aimed to perform a systematized overview of the scientific literature in this domain to identify the specific jobs and categories of workers exposed to biological hazards.
2. Methods
Our review was completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [6]. We searched the PubMed, EMBASE, Web of Science, and academic electronic databases without date limits until August 2022. Our search strategy was designed by the researchers and specialist librarians to optimize the string (see Appendix 1).
Because our review was to focus on review articles about biological hazards and occupational health, our research sought selected keywords in article titles and abstracts. The term ‘review’ was considered a keyword rather than a filter to increase the search's sensitivity since we did not only include systematic reviews. We did not exclude any languages in the first selection so as to quantify the total number of reviews and their languages, though only articles in French and English were included in the next stage. Study selection was made using Covidence software (https://www.covidence.org/). All the study records identified in the search were downloaded, and duplicates were identified and deleted. Next, two review authors, working independently (AO, AD), screened the titles and abstracts of potentially relevant articles (step 1) and then examined their full texts (step 2). In step 1, we excluded irrelevant studies (i.e., do not fit inclusion criteria, including wrong study design, population, or setting). Disagreements on which articles should be included were resolved by consensus between the two authors.
In addition to the first author's name, the year of publication, nationality of the first author author's, and the review's design, we also extracted the article's PECO criteria (Population, Exposure, Comparison, Outcome). We also recorded the populations of exposed workers, types of hazards, types of outcomes (types of health issue, means of prevention), and routes of transmission. The review's protocol was registered in PROSPERO as CRD42022351533.
3. Results
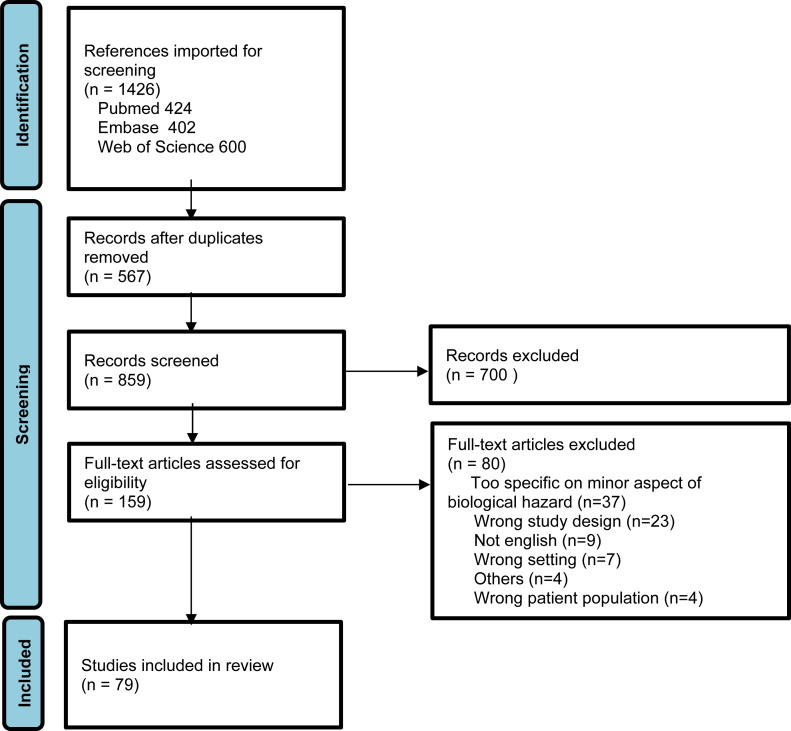
We found 1,426 studies corresponding to our inclusion criteria in the three databases. After eliminating the duplicates (n = 567), 859 studies remained at this first selection step, and 79 of these were included in the final round (Fig. 1, [3,4,[13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89]]).
Fig. 1.
Flow diagram of study selection.
Most of the studies were published after 2010 (n = 63, 79.7%), and they concerned a broad diversity of countries and every continent (Europe, n = 40; the Americas, n = 22; Asia, n = 10; Africa, n = 4; and Oceania, n = 3). Systematic reviews represented less than 40% of the published reviews (2 scoping reviews, 29 systematic reviews), and the others were non-systematic reviews (n = 48). About half of the reviews dealt with infectious hazards only (n = 38, 48.1%), 24 focused on non-infectious hazards only (30.4%) and 17 included both infectious and non-infectious hazards (21.5%).
Summaries of the sectors of economic activity identified in the review process are presented in Table 1, Table 2, Table 3, Table 4, Table 5: all sectors (n = 11, with some focus or exclusion, Table 1), healthcare workers only (n = 16, Table 2), laboratories (n = 10, Table 3), agriculture (including animal, vegetable and grain sectors, n = 32, Table 4), and waste (n = 10, Table 5). Table 1, Table 2, Table 3, Table 4, Table 5 are notable because of the large number of different hazards considered (infectious and non-infectious agents, endotoxins, bioaerosols, and organic dust). The most frequently reported health outcomes were infections and respiratory symptoms. Some papers discussed transmission routes and preventive measures.
Table 1.
Studies looking at all sectors
| Study_ID | Nationality of the first author | Review type | Infectious/Non-infectious | Activity sectors/populations | Hazards | Modes of transmission | Health outcomes | Prevention guidelines (yes/no) |
|---|---|---|---|---|---|---|---|---|
| Acke_2022 | The Netherlands | Systematic | Infectious | All except healthcare occupations | All pathogenic agents | Aerosols, direct contact, percutaneous | Infection | No |
| Douwes_2003 | The Netherlands (with USA) | Non-systematic | Infectious and non-infectious | All except healthcare occupations | Bioaerosols | Aerosols | Respiratory symptoms, infections, allergy | Yes (minor) |
| Dutkiewicz_1988 | USA (with Poland) | Non-systematic | Infectious and non-infectious | All | Biohazards | Aerosols and direct contact | Infections, respiratory symptoms, allergy | No |
| Farokhi_2018 | The Netherlands | Systematic | Non-infectious | All | Endotoxins | Aerosols | Respiratory symptoms | No |
| Franco_2020 | Brazil (with Pakistan) | Systematic | Non-infectious | All | Toxigenic fungi and mycotoxins | Aerosols, direct contact | Respiratory symptoms and toxic effects | No |
| Haagsma_2012 | The Netherlands | Systematic | Infectious | All | All pathogens (Tables 1+3) | All (Tables 2+3) | Not specified | No |
| Liebers_2006 | Germany | Non-systematic | Non-infectious | All with a focus on agriculture, textile industry, wood processing industry, waste collection | Endotoxins | Aerosols | Respiratory symptoms, organic dust toxic syndrome | No |
| Liebers_2020 | Germany | Systematic | Non-infectious | All | Endotoxins | Aerosols | Respiratory symptoms, organic dust toxic syndrome | No |
| Montano_2014 | Germany | Non-systematic | Infectious | All | 50 pathogens (, appendix) | Not detailed | All | No |
| Payton_2000 | UK | Non-systematic | Infectious | All/focus on healthcare workers | Hepatitis B/C and HIV | Percutaneous | Infection | No |
| Rim_2014 | Republic of Korea | Non-systematic | Infectious | All | All pathogenic agents | Aerosol, direct contact/percutaneous | Infection | Yes (engineering, management, training, PPE) |
Table 2.
Studies focused on healthcare workers
| Study ID | Nationality of the first author | Review type | Infectious/Non-infectious | Activity sectors/populations | Hazards | Modes of transmission | Health outcomes | Prevention guidelines (yes/no) |
|---|---|---|---|---|---|---|---|---|
| Andrion_1994 | Italy | Non-systematic | Infectious | Healthcare workers | All (TB, Hepatitis, HIV, …) | Not specified | Infection | Yes (organization, education, occupational health) |
| Barchitta_2019 | Italy | Non-systematic | Infectious | Healthcare workers | Vaccine-preventable diseases | Not specified | Infection/vaccination | Yes (vaccination) |
| Brewczyńska_2015 | Poland | Non-systematic | Infectious | Healthcare workers (emergency medical personnel) | Infectious (mostly), but allergens mentioned | Aerosols, direct contact, percutaneous (bloodborne infections, airborne infection, direct and indirect contact infection mostly) | Infection (mostly), but immunity disorders (asthma) mentioned | No |
| Dearaujo_2022 | Brazil | Systematic | Infectious | Healthcare workers | Respiratory biological agents (SARS, influenza) | Aerosol | Infection (potential) | Yes (effectiveness of masks) |
| Díaz-Guio_2020 | Columbia (with Germany) | Non-systematic | Infectious | Healthcare workers (intensive care) | SARS CoV-2 | Aerosols/droplets, direct- indirect contact | Infection | Yes (PPE, procedure, skills/knowledge) |
| Fyumagwa_2011 | Tanzania | Non-systematic | Infectious | Healthcare workers and livestock workers if epidemic | Phlebovirus | Percutaneous | Rift Valley Fever | Yes (in case of epidemic = health message, PPE, surveillance) |
| Leggat_2007 | Australia (Thailand and Japan) | Non-systematic | Infectious | Healthcare workers (Dentists) | Infectious | Aerosols, direct contact, percutaneous | Infection | Yes (sterilisation/PPE) |
| Low_2005 | Singapore | Non-systematic | Infectious | Healthcare workers | Respiratory hazards | Aerosols/droplets | Respiratory infection (influenza, pertussis, tuberculosis, SARS) | Yes (early identification and precautions, education, vaccination, research) |
| Monteiro_2022 | Portugal | Systematic | Infectious | Healthcare workers | Bacteria (Escherichia coli, Pseudomonas aeruginosa, Staphylococcus spp., Staphylococcus aureus and Micrococcus luteus) | Aerosols, direct contact | Infection | No |
| Pedrosa_2011 | Brazil | Systematic | Infectious | Healthcare workers and laboratory workers | Virus | Aerosol, direct contact/percutaneous | Infection | Yes (biosafety procedures) |
| Rai_2021 | Australia (with Bhutan) | Scoping | Infectious | Healthcare workers | Bloodborne pathogens and tuberculosis | Percutaneous and respiratory | HIV, hepatitis and tuberculosis | No |
| Ridge_2019 | USA | Systematic | Infectious | Healthcare workers (Nurse) | Bloodborne pathogens | Percutaneous | Not detailed | Yes (training, PPE mostly) |
| Szymanska_2012 | Poland | Non-systematic | Infectious | Healthcare workers (Dentist) | Bacterial hazards | Aerosols, direct contact, percutaneous | Bacterial infection | No |
| Tan_1991 | Malaysia | Non-systematic | Infectious | Healthcare workers (Nurse) | Biological hazards (Hepatitis B/C, HIV, tuberculosis, CMV, herpes, clostridium difficile) | Aerosols, direct contact, percutaneous | Infection | No |
| Trevisan_2015 | Italy | Non-systematic | Infectious | Healthcare workers | Hepatitis B | Percutaneous | Hepatitis B | Yes (vaccination) |
| Zemouri_2017 | The Netherlands | Scoping | Infectious | Healthcare workers (hospital and dental environment) | Biological hazards via bioaerosols | Bioaerosols | Infection | No |
Table 3.
Studies focused on laboratories
| Study_ID | Nationality of the first author | Review type | Infectious/Non-infectious | Activity sectors/population | Hazards | Modes of transmission | Health outcomes | Prevention guidelines (yes/no) |
|---|---|---|---|---|---|---|---|---|
| Andrup_1990 | Denmark | Non-systematic | Both infectious and not infectious | Laboratory/Industries with use of recombinant DNA | Microbiological/endo-exotoxin contamination | Aerosols, direct contact | Not detailed | Yes (containment, medical surveillance, regulation) |
| Artika_2017 | Indonesia | Non-systematic | Infectious | Laboratory (with emerging virus) | Emerging virus in 2017 (table 1) | Not specified | Infection | Yes (biosafety with containment, procedures, protection, biosecurity) |
| Coelho_2015 | Portugal | Non-systematic | Infectious | Laboratory | All (Brucella, mycobacterium tuber, Neisseria, parasites and viruses) | Aerosols, direct contact | Infection | Yes (regulation, biosafety biosecurity, organization, training) |
| Collins_2017 | USA | Non-systematic | Infectious | Laboratory animal research | Viral vectors | Direct contact, Percutaneous (with biological fluids, bite, scratch) | Not specified | Yes (regulation, risk assessment, procedures) |
| Ghosh_2020 | USA | Non-systematic | Infectious | Laboratory (using viral vectors systems for gene therapy) | Viral vectors | Not specified | Not specified | Yes (biosafety rules validation Table 1 and Figure 1) |
| Gomez-Tatay_2019 | Spain | Non-systematic | Infectious | Laboratory (Synthetic Biology) | Synthetic Biology | Not specified | Not specified | Yes (biosafety Table 1, biosecurity, regulation) |
| Hankenson_2003 | USA | Non-systematic | Infectious | Laboratory animal research | Zoonotic agents | Aerosols, direct contact, percutaneous | Zoonosis | Yes |
| Pastorino_2017 | France | Non-systematic | Infectious | Laboratory | Infectious (CL-3, infectious agents or toxins that may be transmitted through the air and cause potentially lethal infections) | Aerosol, direct contact/percutaneous | Infection | Yes (biosafety with material/technical, PPE, waste management, disinfection and regulation) |
| Peng_2018 | China (with Mexico collaboration) | Non-systematic | Infectious | Laboratory | Microorganism | Aerosols, direct contact, percutaneous | Injuries | Yes(lessons learned) |
| Schlimgen_2016 | USA | Non-systematic | Not infectious | Laboratory (lentiviral vector facilities) | Lentiviral vector exposures | Not detailed | Oncogenic | Yes (antiretroviral drugs, regulation) |
Table 4.
Studies focused on agriculture/animal, vegetable workers
| Study_ID | Nationality of the first author | Review types | Infectious/Non-infectious | Activity sectors/populations | Hazards | Modes of transmission | Health outcomes | Prevention guidelines (yes/no) |
|---|---|---|---|---|---|---|---|---|
| Agunos_2016 | Canada | Systematic | Infectious and non-infectious | Poultry exposed occupations | All pathogens (including all HxNx viruses, Erysipelothrix sp bacteria, MRSA, Aspergillus sp fungi and allergens) | Aerosols, direct contact | Infection, allergic response, MRSA carriage | Yes (list of preventive measures) |
| Basinas_2015 | Denmark (with The Netherlands) | Non-systematic | Non-infectious | Livestock farmers | Organic dust, endotoxins | Aerosols | Not investigated | No |
| Chamba_2016 | Mozambique | Non-systematic | Non-infectious | Wood processing industry | Wood dust | Aerosols | Asthma, respiratory symptoms | Yes, some information on potential preventive measures |
| Cole_2000 | USA | Non-systematic | Infectious and non-infectious | Pig industry | Zoonotic pathogens and antibiotic-resistant bacteria carriage and endotoxins, dust, airborne bacteria | Aerosols, direct contact | Infection and respiratory symptoms | No |
| Dadar_2022 | Iran | Systematic | Infectious | Workers in contact with livestock, wildlife and pets | Brucella sp | Aerosols and direct contact | Brucellosis | No |
| Davidson_2018 | Australia | Non-systematic | Non-infectious | Cannabis production and handling | Organic dust, bioaerosols, pollen, plant allergens | Aerosol, direct contact | Respiratory symptoms, allergy, byssinosis | Yes, Australian OEL |
| Déléry_2009 | France | Non-systematic | Non-infectious | Agriculture, wood and waste industries | Endotoxins | Aerosols | Respiratory symptoms | Yes, report on current recommendations (OEL) from different countries |
| Dias_2022 | Portugal | Systematic | Non-infectious | Sawmills | Wood dust, bioaerosols | Aerosols | Allergy, respiratory symptoms | No |
| Dignard_2019 | USA | Non-systematic | Infectious and non-infectious | Animal workers | Zoonotic pathogens, antibiotic-resistant bacteria carriage | Aerosols, direct contact | Infection | No |
| Donham_1985 | USA | Non-systematic | Infectious | Agriculture | Zoonotic agents | Aerosols, direct contact | Zoonoses, respiratory symptoms | No |
| Dutkiewicz_2011 | Poland | Non-systematic | Infectious and non-infectious | Mainly outdoor workers (agriculture, forestry) | Zoonotic agents, bioaerosols | Aerosols, direct contact | Zoonoses, respiratory symptoms | No |
| Fontana_2017 | Italy | Systematic | Non-infectious | Agriculture | Organic dust, endotoxins | Aerosols | COPD | No |
| Gessain_2008 | France | Non-systematic | Infectious | Animal workers: Hunters, laboratory workers, zoo, veterinarians | Simian foamy virus | Direct contact, percutaneous | Infection | No |
| Lebouquin_2011 | France | Non-systematic | Infectious and non-infectious | Poultry industry | Zoonotic agents and organic dust, bioaerosols, endotoxins | Aerosols and direct contact | Zoonoses, respiratory symptoms | Yes |
| Magri_2021 | Brazil | Systematic | Infectious and non-infectious | Poultry industry | Zoonotic pathogens, organic dust | Aerosols, direct contact | Infections and respiratory symptoms | No |
| May_2012 | USA | Non-systematic | Non-infectious | Large animal farms | Bioaerosol, organic dust | Aerosols | Respiratory symptoms | No |
| Omland_2002 | Denmark | Non-systematic | Non-infectious | Livestock farmers | Bioaerosols, organic dust, endotoxins | Aerosols | Respiratory symptoms, allergy, asthma | No |
| Pereira_2020 | Brazil | Systematic | Infectious | Rural, abattoir (butchers), veterinarians, laboratory workers and hunters | Brucella sp | Direct contact with infected animals or contaminated material | Brucellosis | No |
| Reynolds_2013 | USA (with Australia, Denmark, Sweden) | Systematic | Non-infectious | Dairy workers | Bioaerosols, organic dust | Aerosols | Respiratory symptoms, | No |
| Ricco_2021 | Italy | Systematic | Infectious | Agriculture and forestry workers | Hantavirus | Aerosols | Infection | No |
| Richard_2015 | Switzerland | Non-systematic | Infectious | Forestry workers | Borrelia sp, Francisella tulerensis, Leptospira interrogans | Aerosols, vector-borne, direct contact | Lyme disease, tularemia and leptospirosis | Yes (biosafety) |
| Samadi_2013 | The Netherlands (with Iran) | Non-systematic | Infectious and non-infectious | Veterinarians | Zoonotic agents, bioaerosols and allergens | Aerosols, direct contact, percutaneous | Zoonosis, respiratory symptoms, allergy | No |
| Sigsgaard_2020 | Denmark (with Germany, The Netherlands) | Non-systematic | Non-infectious | Livestock farmers | Bioaerosols, organic dust | Aerosols | Respiratory symptoms, asthma, rhinitis | Yes, citing literature reporting engineering and production parameters affecting farmers' exposure to bioaerosols |
| Tsapko_2011 | Ukraine (with Poland) | Non-systematic | Non-infectious | Agriculture | Bioaerosols, organic dust | Aerosols | Not mentioned | No |
| Wangia_2019 | USA | Non-systematic | Non-infectious | Farming, grain milling, animal husbandry and textile production | Aflatoxin | Aerosols, direct contact | Cancer | No |
| Wilhelm_2011 | Canada | Systematic | Infectious | Workers in contact with pigs | Hepatitis E virus | Percutaneous | Hepatitis | No |
| Youssef_2021 | UK | Systematic | Infectious | Livestock farmers | Zoonotic agents | Not detailed | Zoonosis | No |
| Burdzik_2012 | South Africa | Non-systematic | Non-infectious | Food and seafood processing workers | Allergic proteins, irritant proteins | Direct contact with food | Contact dermatitis | No |
| Jeebhay_2010 | South Africa (with Canada) | Non-systematic | Non-infectious | Seafood industry | Respiratory symptoms, asthma | Aerosols | Respiratory symptoms, asthma | Yes |
| Lai_2013 | USA | Non-systematic | Non-infectious | Textile workers | Dust, endotoxins | Aerosols | Asthma and COPD | No |
| Nafees_2016 | Pakistan | Systematic | Non-infectious | Textile workers | Cotton dust, endotoxins | Aerosols | Byssinosis | Yes (effectiveness of prevention) |
| Nafees_2022 | Pakistan (with UK, Italy) | Systematic | Non-infectious | Textile workers | Cotton dust, endotoxins | Aerosols | Byssinosis | No |
Table 5.
Studies focused on waste sectors
| Study_ID | Nationality of the first author | Review type | Infectious/Non-infectious | Activity sectors/populations | Hazards | Health outcomes | Prevention guidelines (yes/no) | Modes of transmission |
|---|---|---|---|---|---|---|---|---|
| Anzivino-Viricel_2012 | France | Systematic | Infectious and non-infectious | Waste | Mainly non-infectious hazards | Irritation, respiratory symptoms, gastrointestinal symptoms | No | Aerosols, direct contact |
| Corrao_2013 | Italy | Systematic | Infectious | Waste | Hepatitis B virus | Hepatitis | No | Percutaneous exposure to body fluids |
| Han_2021 | China | Non-systematic | Infectious and non-infectious | Waste | Bioaerosols, antimicrobial-resistant gene | Infections, respiratory symptoms, skin symptoms | No | Aerosols, direct contact |
| Madsen_2021 | Europe | Non-systematic | Infectious and non-infectious | Waste | Biological hazards | Infection, respiratory symptoms, toxic effects, gastrointestinal effects | Yes (Table 3, appendix) | Aerosols, direct contact |
| Muzaini_2021 | Malaysia | Systematic | Not infectious | Waste | Bioaerosols, organic dust, endotoxins | Respiratory symptoms | No | Aerosols |
| Oza_2022 | USA (with Switzerland) | Systematic | Infectious and non-infectious | Waste | Infectious agents | Bacterial and parasitological infections, respiratory symptoms, | No | Aerosols, direct contact |
| Poole_2017 | UK | Systematic | Infectious and non-infectious | Waste | Infectious agents and bioaerosols | Infections, respiratory and skin symptoms | No | Aerosols, direct contact, percutaneous |
| Van_Kampen_2020 | Germany | Systematic | Infectious and non-infectious | Waste | Infectious agents and dust (bioaerosols) | Infection, respiratory symptoms | No | Aerosols, direct contact, percutaneous |
| Pearson_2015 | UK | Systematic | Infectious and non-infectious | Composting facilities | Bioaerosols, organic dust, Aspergillus fumigatus | Respiratory symptoms, infection, allergy | No | Aerosols, direct contact |
| Robertson_2019 | UK | Systematic | Not infectious | Waste | Bioaerosols, organic dust | Respiratory symptoms, gastrointestinal symptoms | No | Aerosols |
Reviews involving healthcare workers described many professions, from nurses to dentists, including different specialties (e.g., emergency, intensive care, and pathology) to illustrate the diversity of potential exposures in the healthcare sector (Table 2). Reviews involving laboratory workers detailed laboratory-acquired infections and injuries, such as needle sticks, cut, and scrapes, and provided information on prevention procedures or biosafety guidelines (Table 3). Agricultural sector reviews included animal farmers, animal food industry workers, veterinarians, abattoir workers, grain industry workers, cannabis industry workers and, by extension, professions working with trees (e.g., forestry, sawmill industries) and plant-based textiles (e.g., cotton, other non-synthetic textiles) (Table 4). Reviews involving waste industries included wastewater treatment plant workers, composting workers, and solid-waste handlers (in collecting, sorting, and treatment) (Table 5).
4. Discussion
This systematized overview provides a comprehensive description of the published academic works describing populations of workers exposed to biological hazards, including information on preventive and safety measures implemented for them.
In the healthcare and laboratory sectors, the importance of emerging hazards (new pathogens and new technologies) was stressed long before the COVID-19 pandemic, with a focus on anticipating potential risks at 15, 25, 26, 38, 56, 67, 73, 90. At the same time, workers in these sectors are also exposed to known biological hazards, such that basic precautions and preventive measures should already be applied continuously (e.g., safety procedures, vaccination), not only in industrialized countries but worldwide.
In the agriculture and waste sectors, workers are mainly exposed to organic dust and bioaerosols. A bioaerosol is an airborne collection of biological material. They can be composed of bacterial cells and cellular fragments (endotoxins), fungal spores and fungal hyphae, viruses, and the by-products of microbial metabolism. Pollen grains and other biological material can also be airborne as bioaerosols [1]. Of the various biological substances present in bioaerosols, only endotoxins (lipopolysaccharides of the walls of gram-negative bacteria) have an OEL of 90 EU/m3 for an 8-hours work exposure, proposed by Dutch Expert Committee on Occupational Standards. In animal farming (pig, dairy, horse and poultry farming), the average levels of personal exposure to endotoxins vary from 220 to 9,609 EU/m3, with a maximum of 374,000 EU/m3 measured in pig farming [17]. In the grain sector, average concentration of 1,115 EU/m3 is observed, while it reached 1,800 EU/m3 in the seed processing sector, with medians of 56,000 and 160,000 EU/m3 for grain storage and dried grass processing, respectively. In the cotton sector, the averages were from 20 to 4,850 EU/m3, with maximum of 30,450 EU/m3, and in the forestry sector, the maximum averages were 7,070 EU/m3. The most frequent health effects associated with occupational exposure to organic dust are respiratory symptoms. However, the dose–response relationship between levels of exposure and health outcomes is difficult to establish since exposure characterization suffers from a lack of standard protocols for bioaerosol sampling and analysis. Thus, there are no occupational exposure limits available to ensure workplace safety. Several countries provide recommendations, but there is no international consensus. Only the Netherlands has proposed an occupational exposure limit for endotoxins, although without defining a methodology for sampling and analysis. Forestry workers and hunters are potentially exposed to zoonotic agents from wild animals, whereas animal farmers, workers in the animal food industry, veterinarians, and abattoirs workers are exposed not only to zoonotic agents from livestock but also the risk of being colonized by antimicrobial-resistant bacteria transmitted from animals. This last issue is a rather ‘new’ investigative research area and has, therefore, not yet been fully taken into account in review papers. In the waste sectors, in addition to exposure to non-infectious agents, there is a great risk of workers coming into contact with human pathogens [13,64,67,70,74].
Different limits should be mentioned. First, it is not a systematic review but a systematized review, since our goal was to provide an overview of populations and risks, without answering any single precise question [7]. Second, relevant original studies, could not be included, if they were not referenced as review papers or guidelines not focusing on biological risk. Furthermore, the low proportion of systematic reviews, with very different focuses (from the effectiveness of prevention methods to the jobs exposed), did not enable us to assess the quality of their evidence, their effect size and did not allow to perform sensitivity analyses. Therefore, to avoid confusion, the term ‘umbrella review’ was not used. For instance, exposures to the many different biological hazards described were measured using diverse, non-comparable methods (sampling and analysis). Moreover, descriptions of the methods used to collect and/or quantify viruses or protein allergens were very scarce, as these methods were only in the development stage. Finally, dose–response relationship between exposure to biological hazards and their associated health effects (dose-response curve) were rarely investigated.
Furthermore, our investigation focused on published reviews on biological hazards. Publication bias is probable since we only chose reviews pertinent to the overview's aim. Indeed, many worthwhile original studies were not included. As we focused our attention on review papers alone, we may have missed new or emerging issues that have not yet been targeted by reviews of the literature. It is probable that some relevant studies on very specific aspects of biological hazards have been missed due to their novelty: for instance, as we mentioned earlier, healthcare workers' fitness to work [8], states of the arts without reviews [90] or with no relationship with health issues [91], the proportion of workers exposed to COVID-19 and job-exposure matrices [9,10], exposure to antimicrobial-resistant bacteria, exposure to some biological risks and effects on mental health [11], and reviews or guidelines on general preventive, health, and safety issues that included biological hazards were not included in this overview [12]. We also focused only on publications in English and French, but we found articles concerning a great diversity of countries and covering a long period.
In conclusion, the biological hazards present in working environments are very significant in many occupational activities, involving different modes of exposure and different health outcomes. Further studies are necessary to quantify these risks and thus establish occupational exposure limits, to help implement prevention measures that can be applied to all workplaces and to combat all hazards to human health, including new emerging ones.
Conflicts of interest
The authors declare no conflicts of interest.
Disclamer
The views expressed in this paper are those of the authors and do not necessarily reflect the views of the aforementioned institutions.
Acknowledgments
All the authors are paid by their home institutions. AD is Editor in Chief of Archives des maladies professionnelles et de l'environnement. AD and JT are members of the board of the International Commission on Occupational Health. No direct funding.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.shaw.2023.10.008.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Stetzenbach L.D. Encyclopedia of Microbiology. 2009. Airborne infectious microorganisms; p. 175. [DOI] [Google Scholar]
- 2.Chan G., Tsing C., Koh D. In: Global occupational health. Guidotti T.L., editor. Oxford University Press; 2011. Biological hazards at work. [DOI] [Google Scholar]
- 3.Rim K.-T., Lim C.-H. Biologically hazardous agents at work and efforts to protect workers' health: a review of recent reports. Saf Health Work. 2014;5:43–52. doi: 10.1016/j.shaw.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acke S., Couvreur S., Bramer W., Schmickler M., De Schryver A., Haagsma J. Global infectious disease risks associated with occupational exposure among non-healthcare workers: a systematic review of the literature. Occup Environ Med. 2022;79:63–71. doi: 10.1136/oemed-2020-107164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tripartite validation of the technical guidelines on biological hazards. 2022. http://www.ilo.org/global/topics/safety-and-health-at-work/events-training/events-meetings/WCMS_846243/lang--en/index.htm [Google Scholar]
- 6.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009 Oct;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. Epub 2009 Jul 23. PMID: 19631507. [DOI] [PubMed] [Google Scholar]
- 7.Nambiema A., Fouquet J., Guilloteau J., Descatha A. [The systematic review and other types of literature reviews: what is it, when, how, why?] Arch des Mal Prof et de l'Environnement. 2021;82:539–552. doi: 10.1016/j.admp.2021.03.004. [DOI] [Google Scholar]
- 8.Porru S., Crippa M., Lucchini R., Carta A., Placidi D., Alessio L. Fitness for work in difficult cases: an occupational medicine experience in a University Hospital. Med Lav. 2006;97:521–528. [PubMed] [Google Scholar]
- 9.Descatha A., Fadel M., Pitet S., Verdun-Esquer C., Esquirol Y., Legeay C., Dinh A., Clodore B., Duprat P., Cartégnie S., Dagrenat C., Andujar P., Leclerc J.P., Letheux C., Investigateurs de Mat-O-Covid SARS-CoV-2 (COVID-19) Job Exposure Matrix: “Mat-O-Covid” Creation (COVID-Mate in French), accuracy study, and perspectives. Arch des Mal Prof et de l'Environnement. 2021;82(5):487–493. doi: 10.1016/j.admp.2021.07.008. [DOI] [Google Scholar]
- 10.Descatha A., Pitet S., Badreau M., Gilbert F., Sembajwe G. Mat-O-Covid: How to use it? Arch des Mal Prof et de l'Environnement. 2022;83:215–219. doi: 10.1016/j.admp.2022.01.011. https://WwwNcbiNlmNihGov/Pmc/Articles/PMC9091162/ [DOI] [Google Scholar]
- 11.Pollock A., Campbell P., Cheyne J., Cowie J., Davis B., McCallum J., McGill K., Elders A., Hagen S., McClurg D., Torrens C., Maxwell M. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. 2020 Nov 5;11(11):CD013779. doi: 10.1002/14651858.CD013779. PMID:33150970; PMCID: PMC8226433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Occupational safety and health in public health emergencies: a manual for protecting health workers and responders. 2018. http://www.ilo.org/global/topics/safety-and-health-at-work/resources-library/publications/WCMS_633233/lang--en/index.htm [Google Scholar]
- 13.Madsen A.M., Raulf M., Duquenne P., Graff P., Cyprowski M., Beswick A., Laitinen S., Rasmussen P.U., Hinker M., Kolk A., Górny R.L., Oppliger A., Crook B. Review of biological risks associated with the collection of municipal wastes. Sci Total Environ. 2021;791:148287. doi: 10.1016/j.scitotenv.2021.148287. Epub 2021 Jun 5. PMID: 34139489. [DOI] [PubMed] [Google Scholar]
- 14.Rai R., El-Zaemey S., Dorji N., Rai B.D., Fritschi L. Exposure to occupational hazards among health care workers in low-and middle-income countries: a scoping review. Int J Environ Res Public Health. 2021;18:1–41. doi: 10.3390/ijerph18052603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Díaz-Guio D.A., Díaz-Guio Y., Pinzón-Rodas V., Díaz-Gomez A.S., Guarín-Medina J.A., Chaparro-Zúñiga Y., Ricardo-Zapata A., Rodriguez-Morales A.J. COVID-19: biosafety in the intensive care unit. Curr Trop Med Rep. 2020;7(4):104–111. doi: 10.1007/s40475-020-00208-z. Epub 2020 Aug 27. Erratum in: Curr Trop Med Rep. 2020 Sep 8;:1. PMID: 32868986; PMCID: PMC7449784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liebers V., Brüning T., Raulf M. Occupational endotoxin exposure and health effects. Arch Toxicol. 2020;94:3629–3644. doi: 10.1007/s00204-020-02905-0. [DOI] [PubMed] [Google Scholar]
- 17.Sigsgaard T., Basinas I., Doekes G., De Blay F., Folletti I., Heederik D., Lipinska-Ojrzanowska A., Nowak D., Olivieri M., Quirce S., Raulf M., Sastre J., Schlünssen V., Walusiak-Skorupa J., Siracusa A. Respiratory diseases and allergy in farmers working with livestock: a EAACI position paper. Clin Transl Allergy. 2020;10 doi: 10.1186/s13601-020-00334-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Franco L.T., Ismail A., Amjad A., Oliveira C.A.F.D. Occurrence of toxigenic fungi and mycotoxins in workplaces and human biomonitoring of mycotoxins in exposed workers: a systematic review. Toxin Rev. 2020:1–16. doi: 10.1080/15569543.2020.1795685. [DOI] [Google Scholar]
- 19.Dignard C., Leibler J.H. Recent research on occupational animal exposures and health risks: a narrative review. Curr Environ Health Rep. 2019;6:236–246. doi: 10.1007/s40572-019-00253-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ridge L.J., Dickson V.V., Stimpfel A.W. The occupational health of nurses in the Economic Community of West African States: a review of the literature. Workplace Health Saf. 2019;67:554–564. doi: 10.1177/2165079919859383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robertson S., Douglas P., Jarvis D., Marczylo E. Bioaerosol exposure from composting facilities and health outcomes in workers and in the community: a systematic review update. Int J Hyg Environ Health. 2019;222:364–386. doi: 10.1016/j.ijheh.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Peng H., Bilal M., Iqbal H.M.N. Improved biosafety and biosecurity measures and/or strategies to tackle laboratory-acquired infections and related risks. Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15122697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davidson M., Reed S., Oosthuizen J., O'Donnell G., Gaur P., Cross M., Dennis G. Occupational health and safety in cannabis production: an Australian perspective. Int J Occup Environ Health. 2018;24(3-4):75–85. doi: 10.1080/10773525.2018.1517234. Epub 2018 Oct 3. PMID: 30281413; PMCID: PMC6237171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farokhi A., Heederik D., Smit L.A.M. Respiratory health effects of exposure to low levels of airborne endotoxin - a systematic review. Environ Health. 2018;17 doi: 10.1186/s12940-018-0360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Collins D.E., Reuter J.D., Rush H.G., Villano J.S. Viral vector biosafety in laboratory animal research. Comp Med. 2017;67:215–221. [PMC free article] [PubMed] [Google Scholar]
- 26.Artika I.M., Ma'roef C.N. Laboratory biosafety for handling emerging viruses. Asian Pac J Trop Biomed. 2017;7:483–491. doi: 10.1016/j.apjtb.2017.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agunos A., Pierson F.W., Lungu B., Dunn P.A., Tablante N. Review of nonfoodborne zoonotic and potentially zoonotic poultry diseases. Avian Dis. 2016;60:553–575. doi: 10.1637/11413-032416-Review.1. [DOI] [PubMed] [Google Scholar]
- 28.Chamba P., Nunes E. Work-related asthma among workers in the wood-processing industry: a review. Curr Allergy Clin Immunol. 2016;29:110–117. [Google Scholar]
- 29.Trevisan A., Nicolli A., Chiara F. Hepatitis B: prevention, protection and occupational risk. Future Virol. 2015;10:53–61. doi: 10.2217/fvl.14.90. [DOI] [Google Scholar]
- 30.Brewczyńska A., Depczyńska D., Borecka A., Winnicka I., Kubiak L., Skopińska-Rozewska E., Niemcewicz M., Kocik J. The influence of the workplace-related biological agents on the immune systems of emergency medical personnel. Cent Eur J Immunol. 2015;40(2):243–248. doi: 10.5114/ceji.2015.52838. Epub 2015 Aug 3. PMID: 26557040; PMCID: PMC4637399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Montano D. Chemical and biological work-related risks across occupations in Europe: a review. J Occup Med Toxicol. 2014;9 doi: 10.1186/1745-6673-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Samadi S., Wouters I.M., Heederik D.J.J. A review of bio-aerosol exposures and associated health effects in veterinary practice. Ann Agric Environ Med. 2013;20:206–221. [PubMed] [Google Scholar]
- 33.Lai P.S., Christiani D.C. Long-term respiratory health effects in textile workers. Curr Opin Pulm Med. 2013;19:152–157. doi: 10.1097/MCP.0b013e32835cee9a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anzivino-Viricel L., Falette N., Carretier J., Montestrucq L., Guye O., Philip T., Fervers B. Domestic waste management: State of current knowledge and health effects assessment in general and occupational populations. Environ Risques et Sante. 2012;11:360–377. doi: 10.1684/ers.2012.0559. [DOI] [Google Scholar]
- 35.Haagsma J.A., Tariq L., Heederik D.J., Havelaar A.H. Infectious disease risks associated with occupational exposure: a systematic review of the literature. Occup Environ Med. 2012;69:140–146. doi: 10.1136/oemed-2011-100068. [DOI] [PubMed] [Google Scholar]
- 36.Dutkiewicz J., Cisak E., Sroka J., Wójcik-Fatla A., Zajac V. Biological agents as occupational hazards - selected issues. Ann Agric Environ Med. 2011;18:286–293. [PubMed] [Google Scholar]
- 37.Fyumagwa R.D., Ezekiel M.J., Nyaki A., Mdaki M.L., Katale Z.B., Moshiro C., Keyyu J.D. Response to Rift Valley Fever in Tanzania: challenges and opportunities. Tanzan J Health Res. 2011;13(5 Suppl 1):332–339. doi: 10.4314/thrb.v13i5.3. PMID: 26591988. [DOI] [PubMed] [Google Scholar]
- 38.Tsapko V.G., Chudnovets A.J., Sterenbogen M.J., Papach V.V., Dutkiewicz J., Skórska C., Krysińska-Traczyk E., Golec M. Exposure to bioaerosols in the selected agricultural facilities of the Ukraine and Poland - a review. Ann Agric Environ Med. 2011;18(1):19–27. PMID: 21736265. [PubMed] [Google Scholar]
- 39.Pedrosa P.B.S., Cardoso T.A.O. Viral infections in workers in hospital and research laboratory settings: a comparative review of infection modes and respective biosafety aspects. Int J Infect Dis. 2011;15:e366–e376. doi: 10.1016/j.ijid.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jeebhay M.F., Cartier A. Seafood workers and respiratory disease: an update. Curr Opin Allergy Clin Immunol. 2010;10:104–113. doi: 10.1097/ACI.0b013e3283373bd0. [DOI] [PubMed] [Google Scholar]
- 41.Déléry L., Cicolella A. Occupational and environmental endotoxin exposure from agricultural and industrial workplaces, a literature review. Environ Risques et Sante. 2009;8:35–45. doi: 10.1684/ers.2009.0214. [DOI] [Google Scholar]
- 42.Leggat P.A., Kedjarune U., Smith D.R. Occupational health problems in modern dentistry: a review. Ind Health. 2007;45:611–621. doi: 10.2486/indhealth.45.611. [DOI] [PubMed] [Google Scholar]
- 43.Liebers V., Brüning T., Raulf-Heimsoth M. Occupational endotoxin-exposure and possible health effects on humans. Am J Ind Med. 2006;49:474–491. doi: 10.1002/ajim.20310. [DOI] [PubMed] [Google Scholar]
- 44.Low J.G.H., Wilder-Smith A. Infectious respiratory illnesses and their impact on healthcare workers: a review. Ann Acad Med Singap. 2005;34:105–110. [PubMed] [Google Scholar]
- 45.Hankenson F.C., Johnston N.A., Weigler B.J., Di Giacomo R.F. Zoonoses of occupational health importance in contemporary laboratory animal research. Comp Med. 2003;53:579–601. [PubMed] [Google Scholar]
- 46.Omland Ø. Exposure and respiratory health in farming in temperate zones - a review of the literature. Ann Agric Environ Med. 2002;9:119–136. [PubMed] [Google Scholar]
- 47.Payton C. Biological hazards: an overview. Occup Med. 2000;50:375–376. doi: 10.1093/occmed/50.6.375. [DOI] [PubMed] [Google Scholar]
- 48.Andrup L., Nielsen B.H., Kolvraa S. Biosafety considerations in industries with production methods based on the use of recombinant deoxyribonucleic acid. Scand J Work Environ Health. 1990;16:85–95. doi: 10.5271/sjweh.1812. [DOI] [PubMed] [Google Scholar]
- 49.Dutkiewicz J., Jablonski L., Olenchock S.A. Occupational biohazards: a review. Am J Ind Med. 1988;14:605–623. doi: 10.1002/ajim.4700140511. [DOI] [PubMed] [Google Scholar]
- 50.Donham K.J. Zoonotic disease of occupational significance in agriculture: a review. Int J Zoonoses. 1985;12:163–191. [PubMed] [Google Scholar]
- 51.Barchitta M., Basile G., Lopalco P.L., Agodi A. Vaccine-preventable diseases and vaccination among Italian healthcare workers: a review of current literature. Future Microbiol. 2019;14:15–19. doi: 10.2217/fmb-2018-0237. [DOI] [PubMed] [Google Scholar]
- 52.Pastorino B., de Lamballerie X., Charrel R. Biosafety and biosecurity in European containment level 3 laboratories: focus on French recent progress and essential requirements. Front Public Health. 2017;5:121. doi: 10.3389/fpubh.2017.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fontana L., Lee S.J., Capitanelli I., Re A., Maniscalco M., Mauriello M.C., Iavicoli I. Chronic obstructive pulmonary disease in farmers: a systematic review. J Occup Environ Med. 2017;59(8):775–788. doi: 10.1097/JOM.0000000000001072. PMID: 28594705. [DOI] [PubMed] [Google Scholar]
- 54.Zemouri C., de Soet H., Crielaard W., Laheij A. A scoping review on bio-aerosols in healthcare and the dental environment. PLoS One. 2017;12 doi: 10.1371/journal.pone.0178007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schlimgen R., Howard J., Wooley D., Thompson M., Baden L.R., Yang O.O., Christiani D.C., Mostoslavsky G., Diamond D.V., Duane E.G., Byers K., Winters T., Gelfand J.A., Fujimoto G., Hudson T.W., Vyas J.M. Risks associated with lentiviral vector exposures and prevention strategies. J Occup Environ Med. 2016;58(12):1159–1166. doi: 10.1097/JOM.0000000000000879. PMID: 27930472; PMCID: PMC5152689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coelho A.C., García Díez J. Biological risks and laboratory-acquired infections: a reality that cannot be ignored in health biotechnology. Front Bioeng Biotechnol. 2015;3:56. doi: 10.3389/fbioe.2015.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pearson C., Littlewood E., Douglas P., Robertson S., Gant T.W., Hansell A.L. Exposures and health outcomes in relation to bioaerosol emissions from composting facilities: a systematic review of occupational and community studies. J Toxicol Environ Health B Crit Rev. 2015;18:43–69. doi: 10.1080/10937404.2015.1009961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.May S., Romberger D.J., Poole J.A. Respiratory health effects of large animal farming environments. J Toxicol Environ Health B Crit Rev. 2012;15:524–541. doi: 10.1080/10937404.2012.744288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Douwes J., Thorne P., Pearce N., Heederik D. Bioaerosol health effects and exposure assessment: progress and prospects. Ann Occup Hyg. 2003;47:187–200. doi: 10.1093/annhyg/meg032. [DOI] [PubMed] [Google Scholar]
- 60.Burdzik A., Jeebhay M., Todd G. Occupational dermatitis in food processing workers with a special focus on the seafood processing industry - a review. Curr Allergy Clin Immunol. 2012;25:88–93. [Google Scholar]
- 61.Reynolds S.J., Nonnenmann M.W., Basinas I., Davidson M., Elfman L., Gordon J., Kirychuck S., Reed S., Schaeffer J.W., Schenker M.B., Schlünssen V., Sigsgaard T. Systematic review of respiratory health among dairy workers. J Agromedicine. 2013;18(3):219–243. doi: 10.1080/1059924X.2013.797374. PMID: 23844790. [DOI] [PubMed] [Google Scholar]
- 62.Andrion A., Pira E. What's new in managing health-hazards in pathology departments. Pathol Res Pract. 1994;190:1214–1223. doi: 10.1016/S0344-0338(11)80453-X. [DOI] [PubMed] [Google Scholar]
- 63.Le Bouquin S., Huneau-Salaun A., Eniafe-Eveillard B. 2011. Health risks for workers in egg production systems and methods of control; pp. 415–442. (Improving the safety and quality of eggs and egg products, Vol 1: Egg chemistry, production and consumption). [Google Scholar]
- 64.Corrao C., Del Cimmuto A., Marzuillo C., Paparo E., La Torre G. Association between waste management and HBV among solid municipal waste workers: a systematic review and meta-analysis of observational studies. Sci World J. 2013 doi: 10.1155/2013/692083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gomez-Tatay L., Hernandez-Andreu J. Biosafety and biosecurity in synthetic biology: a review. Crit Rev Environ Sci Technol. 2019;49:1587–1621. doi: 10.1080/10643389.2019.1579628. [DOI] [Google Scholar]
- 66.Nafees A., Fatmi Z. Available interventions for prevention of cotton dust-associated lung diseases among textile workers. J Coll Physicians Surg Pak. 2016;26:685–691. [PubMed] [Google Scholar]
- 67.Oza H., Lee M., Boisson S., Pega F., Medlicott K., Clasen T. Occupational health outcomes among sanitation workers: a systematic review and meta-analysis. Int J Hyg Environ Health. 2022;240 doi: 10.1016/j.ijheh.2021.113907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dos Anjos Magri C., Garófallo Garcia R., Binotto E., Duarte da Silva Lima N., de Alencar Nääs I., Sgavioli S., de Castro Burbarelli M.F. Occupational risk factors in health of broiler-farm workers: a systematic review. Arch Environ Occup Health. 2021;76(8):482–493. doi: 10.1080/19338244.2020.1832036. Epub 2020 Oct 15. PMID: 33054688. [DOI] [PubMed] [Google Scholar]
- 69.Tan C. Occupational-health problems among nurses. Scand J Work Environ Health. 1991;17:221–230. doi: 10.5271/sjweh.1709. [DOI] [PubMed] [Google Scholar]
- 70.Poole C., Basu S. Systematic Review: Occupational illness in the waste and recycling sector. Occup Medi (Oxf) 2017;67:626–636. doi: 10.1093/occmed/kqx153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ghosh S., Brown A., Jenkins C., Campbell K. Viral vector systems for gene therapy: a comprehensive literature review of progress and biosafety challenges. Appl Biosaf. 2020;25:7–18. doi: 10.1177/1535676019899502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ricco M., Peruzzi S., Ranzieri S., Magnavita N. Occupational hantavirus infections in agricultural and forestry workers: a systematic review and metanalysis. Viruses. 2021;13 doi: 10.3390/v13112150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dadar M., Tabibi R., Alamian S., Caraballo-Arias Y., Mrema E., Mlimbila J., et al. Safety concerns and potential hazards of occupational brucellosis in developing countries: a review. J Publ Health-Heidelberg. 2022 [Google Scholar]
- 74.van Kampen V., Hoffmeyer F., Seifert C., Bruning T., Bunger J. Occupational health hazards of street cleaners - a literature review considering prevention practices at the workplace. Int J Occup Med Environ Health. 2020;33:701–732. doi: 10.13075/Ijomeh.1896.01576. [DOI] [PubMed] [Google Scholar]
- 75.Youssef D., Wieland B., Knight G., Lines J., Naylor N. The effectiveness of biosecurity interventions in reducing the transmission of bacteria from livestock to humans at the farm level: a systematic literature review. Zoonoses Public Health. 2021;68:549–562. doi: 10.1111/zph.12807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pereira C.R., Cotrim de Almeida J.V.F., Cardoso de Oliveira I.R., Faria de Oliveira L., Pereira L.J., Zangeronimo M.G., Lage A.P., Dorneles E.M.S. Occupational exposure to Brucella spp.: a systematic review and meta-analysis. PLOS Negl Trop Dis. 2020;14(5) doi: 10.1371/journal.pntd.0008164. PMID: 32392223; PMCID: PMC7252629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wilhelm B., Rajic A., Greig J., Waddell L., Trottier G., Houde A., Harris J., Borden L.N., Price C.A. A systematic review/meta-analysis of primary research investigating swine, pork or pork products as a source of zoonotic hepatitis E virus. Epidemiol Infect. 2011;139:1127–1144. doi: 10.1017/S0950268811000677. Epub 2011 Apr 18. PMID: 21554782. [DOI] [PubMed] [Google Scholar]
- 78.Han Y., Li L., Wang Y., Ma J., Li P., Han C., Liu J. Composition, dispersion, and health risks of bioaerosols in wastewater treatment plants: a review. Front Environ Sci Eng. 2021;15 doi: 10.1007/s11783-020-1330-1. [DOI] [Google Scholar]
- 79.Dias M., Gomes B., Cervantes R., Pena P., Viegas S., Viegas C. Microbial occupational exposure assessments in sawmills-a review. Atmosphere. 2022;13 doi: 10.3390/atmos13020266. [DOI] [Google Scholar]
- 80.Muzaini K., Yasin S., Ismail Z., Ishak A. Systematic review of potential occupational respiratory hazards exposure among sewage workers. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.646790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cole D., Todd L., Wing S. Concentrated swine feeding operations and public health: a review of occupational and community health effects. Environ Health Perspect. 2000;108:685–699. doi: 10.2307/3434721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wangia R., Tang L., Wang J. Occupational exposure to aflatoxins and health outcomes: a review. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2019;37:215–234. doi: 10.1080/10590501.2019.1664836. [DOI] [PubMed] [Google Scholar]
- 83.Richard S., Oppliger A. Zoonotic occupational diseases in forestry workers - Lyme borreliosis, tularemia and leptospirosis in Europe. Ann Agric Environ Med. 2015;22:43–50. doi: 10.5604/12321966.1141368. [DOI] [PubMed] [Google Scholar]
- 84.Basinas I., Sigsgaard T., Kromhout H., Heederik D., Wouters I., Schluenssen V. A comprehensive review of levels and determinants of personal exposure to dust and endotoxin in livestock farming. J Expo Sci Environ Epidemiol. 2015;25:123–137. doi: 10.1038/jes.2013.83. [DOI] [PubMed] [Google Scholar]
- 85.Gessain A., Calattini S. Emergence of simian foamy viruses in humans: facts and unanswered questions. Future Virol. 2008;3:71–81. doi: 10.2217/17460794.3.1.71. [DOI] [Google Scholar]
- 86.Monteiro A., Cardoso J., Guerra N., Ribeiro E., Viegas C., Cabo Verde S., et al. Exposure and Health Effects of Bacteria in Healthcare Units: An Overview. Appl. Sci. 2022;12:1958. doi: 10.3390/app12041958. [DOI] [Google Scholar]
- 87.Szymanska J., Sitkowska J. Bacterial hazards in a dental office: an update review. Afr J Microbiol Res. 2012;6:1642–1650. doi: 10.5897/AJMR11.1002. [DOI] [Google Scholar]
- 88.de Araujo C.M., Guariza-Filho O., Goncalves F.M., Basso I.B., Schroder A.G.D., Cavalcante-Leao B.L., Ravazzi G.C., Zeigelboim B.S., Stechman-Neto J., Santos R.S. Front lines of the COVID-19 pandemic: what is the effectiveness of using personal protective equipment in health service environments?-a systematic review. Int Arch Occup Environ Health. 2022;95(1):7–24. doi: 10.1007/s00420-021-01775-y. Epub 2021 Oct 21. PMID: 34674034; PMCID:PMC8528650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nafees A., De Matteis S., Burney P., Cullinan P. Contemporary prevalence of byssinosis in low- and middle-income countries: a systematic review. Asia Pac J Public Health. 2022;34:483–492. doi: 10.1177/10105395211073051. [DOI] [PubMed] [Google Scholar]
- 90.Corrao C.R., Mazzotta A., La Torre G., De Giusti M. Biological risk and occupational health. Ind Health. 2012;50(4):326–337. doi: 10.2486/indhealth.ms1324. [DOI] [PubMed] [Google Scholar]
- 91.Burzoni S., Duquenne P., Mater G., Ferrari L. Workplace biological risk assessment: review of existing and description of a comprehensive approach. Atmosphere. 2020;11:741. doi: 10.3390/atmos11070741. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.