Abstract
Objectives
To assess the spectrum of underlying pathologies, the intrauterine course and postnatal outcome of 46 fetuses with megacystis that underwent intrauterine vesico-amniotic shunting (VAS) with the Somatex® shunt in a single center.
Methods
Retrospective analysis of 46 fetuses with megacystis that underwent VAS either up to 14 + 0 weeks (early VAS), between 14 + 1 and 17 + 0 weeks (intermediate VAS) or after 17 + 0 weeks of gestation (late VAS) in a single tertiary referral center. Intrauterine course, underlying pathology and postnatal outcome were assessed and correlated with the underlying pathology and gestational age at first VAS.
Results
46 fetuses underwent VAS, 41 (89%) were male and 5 (11%) were female. 28 (61%) fetuses had isolated and 18 (39%) had complex megacystis with either aneuploidy (n = 1), anorectal malformations (n = 6), cloacal malformations (n = 3), congenital anomalies overlapping with VACTER association (n = 6) or Megacystis–Microcolon Intestinal–Hypoperistalsis Syndrome (MMIHS) (n = 2). The sonographic ‘keyhole sign’ significantly predicted isolated megacystis (p < 0.001). 7 pregnancies were terminated, 4 babies died in the neonatal period, 1 baby died at the age of 2.5 months and 34 (74%) infants survived until last follow-up. After exclusion of the terminated pregnancies, intention-to-treat survival rate was 87%. Mean follow-up period was 24 months (range 1–72). The underlying pathology was highly variable and included posterior urethral valve (46%), hypoplastic or atretic urethra (35%), MMIHS or prune belly syndrome (10%) and primary vesico-ureteral reflux (2%). In 7% no pathology could be detected postnatally. No sonographic marker was identified to predict the underlying pathology prenatally. 14 fetuses underwent early, 24 intermediate and 8 late VAS. In the early VAS subgroup, amnion infusion prior to VAS was significantly less often necessary (7%), shunt complications were significantly less common (29%) and immediate kidney replacement therapy postnatally became less often necessary (0%). In contrast, preterm delivery ≤ 32 + 0 weeks was more common (30%) and survival rate was lower (70%) after early VAS compared to intermediate or late VAS. Overall, 90% of liveborn babies had sufficient kidney function without need for kidney replacement therapy until last follow-up, and 95% had sufficient pulmonary function without need for mechanical respiratory support. 18% of babies with complex megacystis suffered from additional health restrictions due to their major concomitant malformations.
Conclusions
Our data suggest that VAS is feasible from the first trimester onward. Early intervention has the potential to preserve neonatal kidney function in the majority of cases and enables neonatal survival in up to 87% of cases. Despite successful fetal intervention, parents should be aware of the potential of mid- or long-term kidney failure and of additional health impairments due to concomitant extra-renal anomalies that cannot be excluded at time of intervention.
Keywords: Lower urinary tract obstruction, Megacystis, Somatex®, Shunting, Prenatal, Ultrasound
What does this study add to the clinical work
| Fetal megacystis comprises a heterogeneous group of conditions with high mortality if untreated prenatally. The underlying pathology of megacystis is highly variable, but prenatal differentiation is not possible. As prenatal vesico-amniotic shunting (VAS) is feasible from the first trimester onward, it should be performed as early as possible, because it has the potential to preserve neonatal kidney function in the majority of cases and enables neonatal survival in up to 87% of cases. But despite successful fetal intervention, parents should be aware of the potential risk of mid- or long-term kidney failure as the long-term effect of VAS on kidney function is unknown. In addition, the prevalence of concomitant severe extra-renal anomalies is high. Therefore, serial ultrasound examinations are mandatory after fetal intervention, because a significant proportion of these anomalies cannot be detected at the time of intrauterine intervention. |
Introduction
Fetal megacystis comprises a heterogeneous group of conditions. The underlying pathology is highly variable ranging from isolated obstructive megacystis due to posterior urethral valves (PUV) to complex cloacal anomalies (CA) or non-obstructive neurogenic megacystis in Megacystis–Microcolon Intestinal–Hypoperistalsis Syndrome (MMIHS) [1]. Regardless of the underlying pathology, persistent megacystis due to restricted urinary bladder drainage may lead to pediatric kidney failure with high mortality, if untreated prenatally [2–8].
As postnatal therapy of megacystis is frequently too late to rescue kidney and respiratory function, several antenatal treatment options have been developed to enable continuous urinary drainage of megacystis into the amniotic cavity, including serial vesicocentesis [9–11], vesico-amniotic shunting (VAS) [12–26] or cystoscopic laser valve ablation [21, 27, 28]. All previously published series on antenatal interventions including our own previous studies [20, 24, 25] showed an increase in perinatal survival with the best renal and respiratory outcome after VAS. Indeed, data on intervention-related complications, intrauterine demise, preterm rupture of membrane and preterm delivery varied considerably between the published series, as the numbers of treated fetuses were small and VAS was performed by different operators in different centers at varying gestational ages with different shunt systems. In addition, the ideal gestational age for VAS is still unclear, as VAS before 17 weeks has been deemed unsuitable due to an assumed increased complication rate. However, in a previous comparative study we could show that VAS with the Somatex®shunt can already be performed safely before 17 + 0 weeks and survival rates as well as kidney und pulmonary function improved with the earlier gestational age at intervention [25]. Regardless of any intrauterine intervention, the outcome of megacystis remains difficult to predict due to the heterogenic underlying pathology and the high prevalence of complex concomitant urinary, anorectal and genital anomalies [29]. It has been demonstrated that the severity of these concomitant anomalies is the most powerful determinant of perinatal survival and morbidity [30].
The aim of this single-center study was to assess the outcome of a large cohort of fetuses with megacystis that underwent VAS exclusively with the Somatex®shunt at different gestational ages. The underlying pathologies and additional anomalies were assessed, the intrauterine course and all shunt-related complications are described and correlated with survival rate and postnatal morbidity. In addition, we looked for early sonographic predictors to prenatally identify the underlying pathology and to differentiate between obstructive and non-obstructive as well as isolated and complex megacystis, as this may have a significant impact on perinatal mortality and postnatal morbidity.
Methods
We conducted a retrospective cohort study in a large tertiary referral center in Cologne, Germany, and included all cases of fetal megacystis that underwent intrauterine VAS with the Somatex® shunt with known outcome over a period of 6 years (2017–2022).
Megacystis in the first trimester was defined as bladder diameter ≥ 15 mm [31] and in the second and third trimester as a permanently enlarged bladder without evidence of adequate emptying in combination with reduced amniotic fluid volume. Hydronephrosis was defined as pelvic anterior–posterior diameter ≥ 4 mm in the first and ≥ 7 mm in the second trimester. All fetuses underwent several detailed anomaly scans, and karyotyping was offered to all parents.
Regarding the high prevalence of associated anomalies, we classified megacystis either as isolated or complex megacystis.
Isolated megacystis without major concomitant anomalies included megacystis due to
Posterior urethral valve (PUV),
Urethral stenosis, hypoplasia or atresia,
Primary vesico-ureteral reflux (VUR) or
Prune Belly syndrome (PBS).
Complex megacystis included megacystis with either concomitant
Chromosomal anomalies,
Anorectal malformations (ARM) with additional developmental anomalies of the distal anus, rectum or genitourinary tract or cloacal malformations,
Multiple congenital abNormalities (MCA) overlapping with those of VACTERL association or
Neurogenic bladder in Megacystis–Mikrocolon Intestinal Hypoperistalsis-Syndrome (MMIHS).
Due to the overlapping use of the terms Cloacal Malformation, Cloacal Dysgenesis Sequence and Urorectal Septum Malformation Sequence in literature, we defined cloacal malformation in our cohort as absence of anal and genitourinary orifices and confluence of rectum, vagina and/or bladder in the urogenital sinus (as defined by Wheeler et Weaver [32]).
After first diagnosis, all fetuses underwent VAS with the Somatex® Intrauterine shunt (Somatex Medical Technologies, Berlin, Germany) immediately or, if fetal position was unfavorable for immediate VAS, within the next 24 h. VAS was offered from 11 + 0 weeks of gestation onward and was exclusively performed by one of two experienced fetal operators (either C.B. or I.G.) using a technique as previously described by Strizek et al. [24, 25]. Genetic testing was offered to all patients, but was not mandatory prior to intrauterine intervention. If genetic testing was not yet done but desired by the patients, karyotyping was performed during VAS, as the design of the Somatex® Intrauterine shunt allows to acquire amniotics fluid through the same cannula after shunt deployment. If amniotic fluid aspiration during VAS failed, chorionic villus sampling or amniocentesis was performed depending on the gestational age.
If deemed necessary, amniotic fluid was infused prior to VAS using an 18gauge spinal needle and 5% glucose solution. After VAS, all fetuses underwent detailed two weekly ultrasound anomaly scans to assess the fetal anatomy and the shunt position and function. In cases of shunt dislocation or migration, VAS was repeated as soon as possible.
All pediatric and surgical medical files of postnatal ultrasound, micturating cystourethrography or surgery were reviewed until final follow-up to establish the final diagnosis and to assess the underlying pathology, all neonatal complications, the postnatal surgical interventions and therapy. Kidney function within the first days of life was either assessed by local age-dependent reference values for creatinine, ß2-microglobulin and urea or by description of renal function in external pediatric records and charts. All follow-up examinations were either performed in our institutional departments of pediatrics, pediatric surgery and urology or in the participating local centers for pediatrics in standardized procedures.
Three patients of out cohort that underwent VAS before 2018 were already included in a previous feasibility study [24] and their outcome has already been published in another previous publication [25].
In a subgroup analysis, the outcome was correlated with regard to gestational age at first shunting. First VAS up to 14 + 0 weeks was classified as early VAS group, first VAS between 14 + 1 and 17 + 0 weeks as intermediate VAS group and VAS after 17 + 1 week gestation as late VAS group.
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS 22.0, SPSS Inc., Chicago, Ill., USA) statistical software. A p value of < 0.05 was considered significant. This retrospective study was approved by the local ethical committee of human research (No 20–1517).
Results
During the 6-year study period, 46 cases of fetal megacystis were referred to our center, including 1 dichorionic twin and 45 singleton pregnancies. Among the 46 affected fetuses, 41 (89.1%) were male and 5 (10.9%) were female. At first ultrasound all fetuses had megacystis and bilateral hydronephrosis, 39 (84.8%) fetuses had an additional ‘keyhole sign’.
Characteristics of the cohort
Twenty-eight (60.9%) fetuses had isolated megacystis without any major additional anomalies and 18 (39.1%) had complex megacystis with major additional anomalies (Table 1). With the exception of the hymenal atresia that was postnatally diagnosed all additional anomalies were correctly described prenatally and confirmed postnatally. The three most common major additional anomalies were imperforated anus in 26%, followed by recto-genito-urinary fistulas and genital malformations in 12% each (Table 2). Although a proportion of these additional anomalies escaped detection at first trimester ultrasound, prenatal diagnosis was achieved during subsequent ultrasound examinations (with the exception of hymenal atresia).
Table 1.
Antenatal characteristics, outcome and postnatal findings in 46 cases with megacystis
| GA @ 1st diagnosis | Sex | Isolated/complex megacystis | Keyhole-sign | Additional anomalies @ 1st diagnosis | AFI @ 1st diagnosis | GA @ 1st shunting | Amnion infusion before shunting | Shunt complications | Additional shunting | Underlying cause postnatally | Postnatal diagnosis | Additional extra-renal anomalies postnatally confirmed | Additional renal anomalies postnatally confirmed | gestational age @ birth |
Outcome | Impairment postnatally | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 13 + 0 | Female | Complex | Yes | Pes equinovarus | Normal | 13 + 0 | – | – | – | – | MCA | Lumbo–sacral myelomeningocele + esophageal atresia | – | – | TOP | – |
| 2 | 11 + 4 | Male | Complex | Yes | Nasal bone aplasia, enterolithiasis | Normal | 12 + 5 | – | – | – | – | MCA | Hydrocephaly + thoraco-lumbal scoliosis | – | – | TOP | – |
| 3 | 13 + 1 | Male | Complex | Yes | – | Normal | 13 + 1 | – | – | – | – | Chrosmosomal | Trisomy 18 | – | – | TOP | – |
| 4 | 12 + 1 | Male | Complex | Yes | – | Normal | 13 + 6 | – | – | – | – | ARM | Imperforated anus | MCDKD, contralateral renal dysplasia | – | TOP | – |
| 5 | 12 + 6 | Female | Complex | No | – | Normal | 12 + 6 | – | – | – | Urethral atresia | Cloacal malformation | Imperforate anus + vesico-intestinal fistula + indifferential genitalia | Renal agenesis,contralateral renal dysplasia | 30 (PROM + cord prolapse) | NND | Palliative care |
| 6 | 13 + 6 | Male | Complex | Yes | Dichorionic twins | Oligo | 13 + 6 | – | Iatrogenic shunt displacement | Vesico-amn | Urethral atresia | ARM | Imperforate anus + clubfeet + pulmonary hypoplasia | – | 24 (amniotic sac prolapse + preterm labor) | NND | Extreme prematurity, palliative care |
| 7 | 13 + 6 | Male | Isolated | Yes | – | Normal | 13 + 6 | – | – | – | PUV | – | Bilateral double kidney, unilateral urinoma | 33 (PROM) | CHD | Lethal lung hypoplasia | |
| 8 | 13 + 4 | Male | Complex | Yes | Cord cyst | Normal | 13 + 4 | – | – | – | Urethral hypoplasia | ARM | Imperforated anus + rectoprostatic fistula | – | 39 | Survivor | – |
| 9 | 12 + 6 | Male | Isolated | Yes | – | Normal | 12 + 6 | – | – | – | No reason found | – | Severe bilateral megaureters | 39 | Survivor | – | |
| 10 | 12 + 6 | Male | Complex | No | Cord cysts,hyper-echogenic intestines, enterolithiasis | Oligo | 13 + 3 | Yes | – | – | Urethral atresia | ARM | Imperforated anus + rectourethral fistula | – | 40 | Survivor | – |
| 11 | 13 + 6 | Male | Isolated | Yes | Bilateral club feet | Oligo | 13 + 6 | – | Spontaneous dislocation @ 30 weeks | Abd-amn | PUV | Cryptorchism | Unilateral double kidney | 32 (PROM) | Survivor | – | |
| 12 | 13 + 5 | Male | Isolated | Yes | – | Normal | 13 + 5 | – | Spontaneous dislocation @ 17 weeks | Abd-amn | Urethral stenosis, urethral hypoplasia | Cryptorchism + intestinal perforation due to intra-abdominally dislocated shunt | Unilateral double kidney | 38 | Survivor | – | |
| 13 | 14 + 0 | Male | Isolated | No | – | Oligo | 14 + 0 | – | – | – | No reason found | – | Unilateral urinoma | 40 | Survivor | – | |
| 14 | 14 + 0 | Male | Isolated | Yes | – | Normal | 14 + 0 | – | – | – | PUV, urethral hypoplasia | – | Unilateral urinoma | 39 | Survivor | – | |
| 15 | 14 + 3 | Male | Complex | Yes | Atypically shaped megacystis with ventral diverticle | Normal | 14 + 5 | - | – | – | – | MCA/VATER | Imperforate anus + duodenal atresia | Unilateral MCDKD | – | TOP | – |
| 16 | 14 + 2 | Male | Complex | Yes | Cervical MMC | Oligo | 14 + 3 | Yes | – | – | – | MCA/VACTER | Myelomeningocele + severe fetal growth restriction (FGR) + Coarctatio aortae | – | – | TOP | – |
| 17 | 13 + 3 | Female | Complex | Yes | – | Normal | 14 + 3 | – | – | – | – | MCA/VATER | Spinal dysraphia + imperforated anus | Horseshoe kidney | – | TOP | – |
| 18 | 14 + 3 | Female | Complex | Yes | – | anhydr | 14 + 3 | Yes | – | – | Urethral atresia | Cloacal malformation | Hymenal atresia (postnatally diagnosed) + imperforated anus + rectouterine fistula | Bilateral renal hypoplasia | 36 | NND | Lethal respiratory insufficiency |
| 19 | 14 + 3 | Male | Complex | Yes | Atypically shaped megacystis | Oligo | 14 + 3 | Yes | – | – | Urethral atresia, urethral hypoplasia | ARM | Imperforate anus + scrotum bifidum + penoscrotal transposition | Unilateral renal hypoplasia | 40 | NND | End-stage renal failure, uremic pericarditis |
| 20 | 14 + 5 | Male | Isolated | Yes | – | Oligo | 14 + 5 | Yes | – | – | Prune belly | Mild prune belly + severe megaureters + VUR III° | – | 38 | Survivor | Mildly impaired by recurrent infections and prune belly | |
| 21 | 14 + 3 | Female | Complex | No | SUA | Oligo | 14 + 3 | – | – | – | Urethral atresia | Cloacal malformation | Hymenal atresia + imperforate anus + indifferent genialia + scoliosis + cor triatriatum + aplasia cutis congenita right thigh | Horseshoe kidney | 40 | Survivor | Moderately impaired by stoma |
| 22 | 14 + 3 | Male | Isolated | Yes | ARSA | Oligo | 14 + 3 | – | – | – | PUV | Urethral duplication + VUR left | Unilateral renal hypoplasia | 40 | Survivor | – | |
| 23 | 14 + 2 | Male | Complex | No | Intestinal dilatation, enterolithiasis | Normal | 14 + 2 | – | – | – | Urethral hypoplasia | ARM | Imperforated anus + rectovesical fistula + VUR | Unilateral renal hypoplasia | 39 | Survivor | Mildly impaired by stoma |
| 24 | 13 + 1 | Male | Isolated | Yes | – | Normal | 14 + 1 | – | – | – | VUR | – | – | 38 | Survivor | – | |
| 25 | 14 + 2 | Male | Complex | Yes | Cord cyst, megalourethra | Normal | 14 + 2 | – | – | – | Urethral hypoplasia | ARM | Imperforated anus + recto-vesical fistula + clumsy penis + scrotum bifidum + cryptorchism | Unilateral renal hypoplasia | 40 | Survivor | – |
| 26 | 14 + 1 | Male | Complex | No | Inestinal dilatation | Normal | 14 + 1 | – | Spontaneous dislocation @ 31 weeks | Abd-amn | Neurogenic | MMIHS | Congenital mikrocolon + intestinal malrotation + clubfeet | Bilateral hydronephrosis + megaureters | 31 (AIS) | Survivor | Mildly impaired by stoma |
| 27 | 15 + 1 | Male | Complex | No | – | Normal | 15 + 1 | – | – | – | Neurogenic | MMIHS | Congenital microcolon | Bilateral hydronephrosis + megaureters | 37 | Survivor | Severely impaired by parenteral nutrition |
| 28 | 15 + 4 | Male | Isolated | Yes | – | Oligo | 15 + 4 | – | – | – | PUV | Mild pulmonary hypoplasia + mild muscular hypotonia | – | 38 | Survivor | – | |
| 29 | 15 + 0 | Male | Isolated | Yes | – | Oligo | 15 + 1 | – | – | – | PUV | Cryptorchism | – | 37 | Survivor | Asymptomatic mild chronic renal insufficiency | |
| 30 | 15 + 2 | Male | Isolated | Yes | – | Oligo | 15 + 2 | – | Spontaneous dislocation @ 27 weeks | Abd-amn | PUV | – | – | 31 (PROM) | Survivor | – | |
| 31 | 15 + 1 | Male | Isolated | Yes | – | Oligo | 15 + 1 | Yes | – | – | Prune belly | Prune belly syndrome + cryptorchism | – | 32 (AIS) | Survivor | Mildly impaired due to aplasia of abdominal muscles | |
| 32 | 16 + 2 | Male | Isolated | Yes | – | Oligo | 16 + 1 | – | – | – | PUV | – | – | 38 | Survivor | – | |
| 33 | 16 + 4 | Male | Isolated | Yes | PA + VSD + MAPCAs | Normal | 16 + 4 | – | – | – | PUV | Pulmonary valve atresia with VSD and MAPCAs | – | 39 | Survivor | – | |
| 34 | 16 + 5 | Male | Isolated | Yes | – | Normal | 16 + 5 | – | Spontaneous dislocation @ 28 and 31 weeks | Abd-amn | PUV, urethral hypoplasia | – | – | 36 | Survivor | – | |
| 35 | 16 + 3 | Male | Isolated | Yes | – | Oliog | 16 + 3 | Yes | – | – | Urethral hypoplasia | – | – | 39 | Survivor | – | |
| 36 | 16 + 6 | Male | Isolated | Yes | – | Oligo | 16 + 6 | – | Spontaneous dislocation @ 29 weeks | Abd-amn | PUV | – | – | 37 | Survivor | – | |
| 37 | 16 + 2 | Male | Isolated | Yes | – | Normal | 16 + 2 | – | – | – | No reason found | Pulmonary hypoplasia | Bilateral cystic dysplastic kidneys | 40 | Survivor | Requiring dialysis | |
| 38 | 15 + 6 | Male | Isolated | Yes | – | Oligo | 15 + 6 | Yes | – | – | PUV | Unilateral VUR | Unilateral cystic dysplastic kidney | 34 (PROM) | Survivor | – | |
| 39 | 18 + 2 | Male | Isolated | Yes | Unilateral renal agenesis | Oligo | 18 + 2 | Yes | Spontaneous dislocation @ 27 weeks | Abd-amn | PUV | Aplasia cutis right thigh | Unilateral renal agenesis | 36 | Survivor | – | |
| 40 | 18 + 1 | Male | Isolated | Yes | – | Oligo | 18 + 1 | – | – | – | PUV | – | Bilateral hypoplastic kidneys | 37 | Survivor | – | |
| 41 | 19 + 4 | Male | Isolated | Yes | – | Oligo | 18 + 2 | Yes | – | – | PUV | Urachus diverticulum + mild pulmonary hypoplasia | Cystic dysplastic kidney, contralateral dysplastic double kidney | 36 | Survivor | Required kidney-transplantation | |
| 42 | 19 + 6 | Male | Isolated | Yes | – | Anhydr | 18 + 3 | Yes | Iatrogenic shunt displacement | Vesico-amn | Long-distance urethral hypoplasia | Cryptorchism | Cystic dysplastic kidney, contralateral urinoma | 36 | Survivor | – | |
| 43 | 20 + 4 | Male | Isolated | Yes | – | Oligo | 21 + 4 | – | Spontaneous dislocation @ 30 weeks | Abd-amn | PUV | VUR IV° + omental prolaps (iatrogenic gastroschisis) | Unilateral urinoma | 35 | Survivor | Asymptomatic mild chronic renal insufficiency | |
| 44 | 24 + 0 | Male | Isolated | Yes | – | Oligo | 24 + 0 | Yes | Spontaneous dislocation @ 28 weeks | Abd-amn | PUV | – | – | 39 | Survivor | – | |
| 45 | 24 + 5 | Male | Isolated | Yes | – | Oligo | 24 + 5 | Yes | – | – | PUV | – | – | 29 (PROM) | Survivor | – | |
| 46 | 25 + 0 | Male | Isolated | Yes | – | Anhydr | 25 + 2 | Yes | Iatrogenic shunt displacement | Vesico-amn | Hypoplastic urethra | – | Bilateral cystic dysplastic kidneys | 37 | Survivor | Requiring dialysis |
Table 2.
Type and prevalence of additional anomalies in 18 cases with complex megacystis
| Type of additional anomalies | Prevalence n (%) |
|---|---|
| Imperforate anus | 12 (26) |
| Fistulas (recto-vesical, recto-prostatic, recto-urethral, recto-uterine) | 6 (12) |
| Genital malformations (ambiguous genitalia, scrotum bifidum, clumsy penis cryptorchism) | 6 (12) |
| Neural tube defects (myelomeningocele, spinal dysgraphia) | 3 (6) |
| Cardiac anomalies | 3 (6) |
| Esophageal/duodental atresia | 2 (4) |
| vertebral scoliosis | 2 (4) |
| Clubfeet (without neural tube defects) | 2 (4) |
| Hymenal atresia (*) | 2 (4) |
| Congenital megacystis–microcolon intestinal–hypoperistalsis syndrome | 2 (4) |
| Aplasia cutis congenita | 2 (4) |
| Hydrocephaly (without neural tube defect) | 1 (2) |
| Trisomy 18 | 1 (2) |
| Severe fetal growth restriction (FGR) | 1 (2) |
*Postnatally diagnosed
Among the 5 female fetuses all had complex megacystis with additional cloacal malformation in 3 cases and VACTERL association in 2 fetuses. Two of the five pregnancies were terminated, 2 babies died in the neonatal period, and 1 girl survived. She was moderately impaired by her stoma at last follow-up at an age of 4 years. Therefore, female sex was a significant predictor of severe and complex megacystis with adverse outcome.
Prenatal genetic testing prior to or during VAS was performed in 24 (52.2%) cases. In the remaining 22 (47.8%) patients, genetic testing was carried out postnatally. All but one case had a normal karyotype (97.8%). In the only case with abnormal karyotype, the initial genetic testing during VAS failed due to insufficient cell growth, making an amniocentesis inevitable 2 weeks later. Karyotyping then revealed a trisomy 18. Consequently, this pregnancy was terminated.
VAS
Early VAS was performed in 14 (30.4%) cases, intermediate VAS in 24 (52.2%) cases and late VAS in 8 (17.4%) cases (Table 3). Technically successful first VAS was achieved in 43 (93.5%) cases, whereas in three (6.5%) cases the initial shunt was positioned incorrectly into the fetal abdomen and a second shunt had to be placed within the next day. Amniotic fluid index at first diagnosis was significantly reduced in 26 (56.5%) cases and amnion infusion prior to VAS was warranted in 14 (30.4%) cases.
Table 3.
Characteristics of early, intermediate and late VAS subgroups
| Early VAS ≤ 14 + 0 weeks | Intermediate VAS 14 + 1–17 + 0 weeks | Late VAS > 17 + 0 weeks | All | Significance (p < 0.05) | |
|---|---|---|---|---|---|
| Number of fetuses (n) | 14 | 24 | 8 | 46 | |
| Prevalence of isolated megacystis | 6/14 (42.9%) | 14/24 (58.3%) | 8/8 (100%) | 28/46 (60.9%) | p = 0.029* |
| Amnion infusion prior to VAS | 1/14 (7.1%) | 7/24 (29.2%) | 6/8 (75%) | 14 /46 (30.4%) | p = 0.004* |
| 1st VAS (weeks of gestation) | 13 + 1 (range, 11 + 4–14 + 0) | 15 + 1 (range, 14 + 1–16 + 6) | 21 + 6 (range, 18 + 1–25 + 2) | 15 + 6 (range, 11 + 4–25 + 2) | |
| Shunt complications | 4/14 (28.6%) | 5/24 (20.8%) | 6/8 (75%) | 15/46 (32.6%) | p = 0.015* |
| TOP | 4/14 (33.3%) | 3/24 (12.5%) | 0/8 (0%) | 7/46 (15.2%) | |
| Preterm delivery ≤ 32 weeks | 3/10 (30%) | 3/21 (14.3%) | 1/8 (12.5%) | 7/39 (17.9%) | p = 0.512 |
| Gestational age @ delivery | 31 + 5 (range, 23 + 1–40 + 6) | 36 + 5 (range, 30 + 5–40 + 0) | 35 + 1 (range, 28 + 0–38 + 6) | ||
| Intention to treat survival | 7/10 (70%) | 19/21 (90.5%) | 8/8 (100%) | 34/39 (87.2%) | p = 0.134 |
| Restricted renal function @birth | 0/10 (0%) | 3/21 (14.3%) | 3/8 (37.5%) | 6/39 (15.4%) | p = 0.089 |
| Restricted pulmonary function @birth | 1/10 (10%) | 1/21 (4.8%) | 0/8 (0%) | 2/39 (5.1%) | p = 0.629 |
| Follow-up (months) | 18 (range, 2–68) | 27 (range, 1–72) | 36 (range, 2–72) | 24 (range, 1–72) |
*Statistically significant, the early VAS group was compared to the intermediate and late VAS groups
Further shunt complications such as spontaneous dislocation or migration of the shunt into the fetal abdomen in the further course of pregnancy occurred in another 10 (21.7%) cases, at a median gestational age of 28 weeks (range, 17–31). In these cases, an additional peritoneo-amniotic shunt was placed in the fetal abdominal wall to drain the urinary ascites. Fetal injuries due to the shunt itself occurred in another 2 (4.3%) cases and included intestinal perforation by the dislocated shunt in one newborn and a small abdominal wall defect with omental prolapse at the shunt insertion site in another newborn baby.
Therefore, the likelihood of an unsuccessful first VAS in our cohort was 6.5% and the necessity of a second and third VAS due to spontaneous shunt dislocation was 19.5% and 2.2%, respectively. No spontaneous intrauterine demise occurred.
Overall, preterm delivery prior to 32 + 0 weeks of gestation due to preterm rupture of membrane (PROM), amniotic sac-prolapse, amniotic infection syndrome or preterm labor occurred in 17.9% and was more common after early VAS (30%) (p = 0.512), although these numbers did not reach significance. Median gestational age at delivery was 35 + 1 weeks of gestation (range, 30 + 5–40 + 0). Median follow-up was 72 months (range, 2–72).
Mortality, survival rate and postnatal morbidity
Seven (15.2%) pregnancies were terminated (TOP), all had complex megacystis (Table 1, Fig. 1). Four (8.7%) liveborn babies died in the neonatal period (NND), all had complex megacystis. Two of them were born at 23 and 29 weeks of gestation and died after palliative care within the first 10 h of life, one died of lung hypoplasia after 8 days of life and another one after 9 days due to uremic pericarditis. Another male baby died of sequelae of lung hypoplasia at the age of 2.5 months. He had isolated megacystis and underwent early VAS.
Fig. 1.
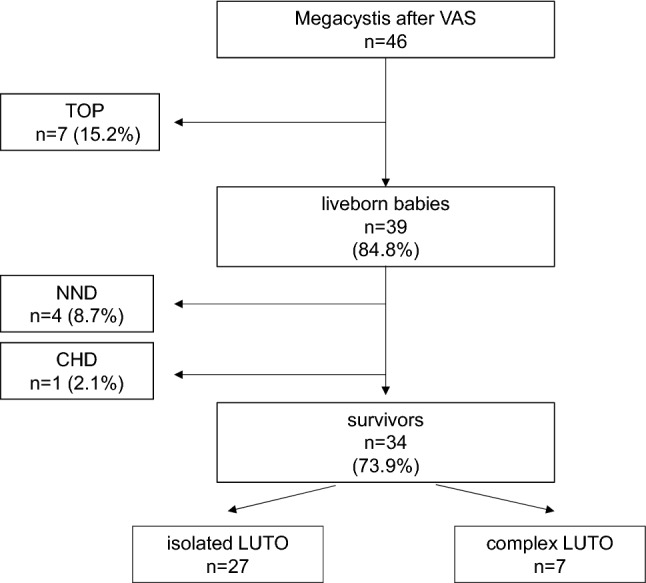
Outcome of the 46 fetuses with megacystis after VAS
Thirty-four (73.9%) babies were alive at last follow-up. Median follow-up was 24 months (range, 1–72 months). After exclusion of TOP, the mortality rate in our cohort was 12.8% with an overall survival of 87.2%. However, there was a significantly higher survival amongst fetuses with isolated (96.4%) versus complex megacystis (63.6%) (p = 0.025).
Among the 39 liveborn babies, 33 (84.6%) babies had sufficient kidney function without need for immediate dialysis after birth as well as at last follow-up at a median age of 2 years of age (range 1–6 years). Two (5.1%) babies were born with asymptomatic mild chronic renal insufficiency without need of dialysis at last follow-up at a median age of 3.6 years, and 4 (10.3%) babies were born with kidney failure. Among them, one required kidney transplantation after his first year of life with well-functioning transplant at last follow-up 2 years later, and the remaining three were on chronic dialysis at a median age of 1.5 years of life. Kidney function was better after early VAS as all babies with impaired kidney function had either intermediate or late VAS. However, these findings did not reach significance (p = 0.089). Despite successful VAS, subsequent prenatal sonographies revealed significant alterations of the kidneys or the urinary tract in nearly all cases that could also be confirmed postnatally. Significant hydronephrosis or megaureters was diagnosed in 14 cases, cystic–dysplastic kidneys in 7, urinoma in 5, significant renal hypoplasia in 4 and unilateral renal agenesis in 3 cases.
Pulmonary size and function at birth was adequate in 37 (94.9%) of the 39 liveborn without need for mechanical respiratory support. Two (5.1%) babies had lung hypoplasia and fatal respiratory insufficiency. Pulmonary size and function did not differ between the subgroups of early, intermediate or late VAS.
With regard to the overall health status, 6 (17.6%) of the 34 survivors had additional health restrictions as a consequence of their concomitant extra-renal anomalies, either by their stoma due to underlying imperforate anus (n = 3), by their hypoplastic abdominal muscles due to the underlying prune belly syndrome (n = 2) or by parenteral nutrition due to an underlying MMIHS (n = 1). Accordingly, overall health status was better among survivors with isolated compared with complex megacystis (p = 0.116). Among survivors with isolated megacystis, 74.1% were healthy without any renal, pulmonary or other limitations, compared with only 42.9% survivors with complex megacystis. Due to the small number of survivors with complex megacystis the result did not reach statistical significance (p = 0.116).
Underlying pathology of megacystis
Most common underlying pathologies of megacystis among the 39 liveborn babies with known outcome were PUV in 18 (46.2%) cases, followed by hypoplastic or stenotic urethra in 7 (20.6%) and atretic urethra in 6 (15.4%) cases, neurogenic bladder due to MMIHS or Prune belly syndrome in 2 (5.1%) cases, each, and primary VUR due to insufficient flap-valves in 1 (2.6%) case (Table 1). In 3 (7.7%) cases no underlying pathology for megacystis could be detected postnatally, although all 3 newborns had significant additional urinary abnormalities including megaureters, urinoma or end-stage cystic dysplastic kidney disease.
‘Keyhole sign’
Among the 39 liveborn babies with known outcome, 32 (82.1%) had megacystis with ‘keyhole sign’ at time of first diagnosis and 7 (17.9%) had megacystis without ‘keyhole sign’ (Table 1). Among those with ‘keyhole sign’, 27 (84.4%) had isolated megacystis and 5 (15.6%) had complex megacystis with either additional anorectal (n = 4) or cloacal malformations (n = 1). Twenty-five (78.1%) of the 32 babies with ‘keyhole sign’ survived without severe postnatal impairment. In contrast, among the 7 babies without ‘keyhole sign’, only 1 (14.3%) had isolated and 6 (85.7%) had complex megacystis with either additional anorectal (n = 2), cloacal malformations (n = 2) or MMIHS (n = 2). Only 2 (28.6%) of the 7 babies without ‘keyhole sign’ survived without any impairment. Therefore, the presence of the ‘keyhole sign’ was significantly associated with isolated megacystis and consequently with an overall better outcome in our cohort (p < 0.001).
However, the ‘keyhole sign’ was no reliable marker to predict the underlying pathology or to differentiate between obstructive or non-obstructive megacystis (p = 0.137). Among the 32 babies with ‘keyhole sign’, 27 (84,4%) had obstructive megacystis due to PUV or hypoplastic or atretic urethra and 5 (15.6%) had non-obstructive megacystis. In contrast, among the 7 babies without ‘keyhole sign’ only 3 (42.9%) babies had non-obstructive and 4 (57.1%) had obstructive megacystis.
When these results are analyzed according to the gestational age at VAS, amnion infusion was significantly more often necessary prior to intermediate or late VAS than to early VAS (p = 0.004) and shunt complications occurred significantly more often after late VAS (p = 0.015), whereas preterm delivery ≤ 32 + 0 weeks occurred noticeably more often after early VAS (p = 0.512). Prevalence of isolated megacystis was significantly higher (p = 0.029) and survival rates noticeably higher in the intermediate or late VAS group (p = 0.134), but renal function was noticeably better after early VAS (p = 0.089) (Table 2).
Discussion
We present the outcome of a large cohort of fetuses with megacystis treated by vesico-amniotic shunting (VAS) with the Somatex® Intrauterine Shunt by two experienced operators in a single center. Our data suggest that VAS is feasible from the first trimester onward and early intervention has the potential to preserve kidney function in the majority of cases.
Mild megacystis < 15 mm is often a transient finding in the first trimester, that spontaneously resolves during ongoing weeks of pregnancy [7, 31, 33, 34], whereas megacystis > 15 mm is strongly suggestive of significant restricted urinary bladder drainage and a spontaneous resolution is unlikely [1–5, 8]. Untreated, a persistent megacystis is associated with high mortality and severe postnatal morbidity caused by lung hypoplasia and impaired kidney function, regardless of the underlying pathology [2–6, 8, 16, 17, 35–39].
Several authors have evaluated prognostic factors to predict the risk of kidney failure [4–6, 8, 21, 33, 40–45] and different fetal therapies have been evaluated to enable continuous drainage into the amniotic cavity and to prevent renal damage and pulmonary hypoplasia [46]. In a recently published review, the ERKNet CAKUT-Obstructive Uropathy Work Group confirmed data from the randomized PLUTO trial [16, 17] and recommended VAS as the therapy of choice in selected cases with moderate and severe megacystis, ideally performed before 27 weeks of gestation [8]. In three previously published own series we also confirmed that VAS is a safe and effective intervention that can enable survival in up to 78% and preserves normal kidney function in up to 86% of the survivors [20, 24, 25].
The embryonic kidneys develop from the fourth week of gestation onward and nephrogenesis passes through 3 stages [47]. Any disturbance during this period may negatively influence the normal ureteric bud branching and metanephric mesenchymal differentiation. As the duration of urinary obstruction is crucial for the development of renal dysplasia [48], fetal intervention should be performed as soon as possible after first diagnosis of megacystis. However, so far, there are only very few studies on VAS before 17 weeks of gestation, because it has been considered to be associated with high complication rates [17, 26, 49]. However, in a previously published feasibility study we demonstrated that VAS using the Somatex® VAS system with its smaller introduction cannula is already feasible < 17 weeks without significantly more frequent shunt complications [24, 25]. In this study VAS was performed from the 12th week of gestation onward and kidney function could be preserved in all cases if VAS was performed ≤ 14 + 0 weeks of gestation. In addition, the amount of amniotic fluid is usually unchanged in first trimester megacystis; therefore, amnion infusion prior to VAS could be avoided in nearly all cases.
In previously published trials on VAS, the prevalence of shunt-related complications and survival rates differed significantly. This might be explained by poorly comparable and predominantly small cohorts in which different types of shunt systems were used in different centers with different local protocols and at different gestational ages (before or after 17 + 0 weeks of gestation) [12–26]. In contrast, our data are derived from a large single-center cohort, where exclusively, the Somatex® shunt was used. Overall survival in our cohort was 74% and noticeably better than those reported in literature, where 12 months survival rates of less than 44% are reported [16, 17, 22, 46].
In the literature, VAS-related complications occur in 40% of cases and include shunt dislocation or migration, shunt blockage, preterm rupture of membrane and preterm labor, abdominal wall herniation or intrauterine fetal death [8, 14–19, 23–25]. In our cohort shunt complications occurred in 22% of cases and were limited to shunt dislocation or migration and were even less common after early VAS compared with late VAS. There was no case of fetal loss. Intervention-related preterm delivery prior to 32 + 0 weeks due to preterm rupture of membrane or preterm labor occurred in 18% of cases. Therefore, we conclude that VAS is an effective treatment that ideally should be performed in the first trimester, as it shows the best results concerning kidney and pulmonary function, although it carries an 18% risk of preterm delivery.
More than one third of our cohort had complex megacystis (39%) with additional severe anomalies, including anorectal malformations with additional developmental anomalies of the distal anus, rectum or genitourinary tract, cloacal malformations or congenital malformations overlapping with those of VACTERL association. However, since kidney function can successfully be preserved by early VAS, the severeness of these additional anomalies influenced survival and postnatal morbidity more significantly than renal insufficiency. Consequently, survival in fetuses with complex megacystis was only 64% compared with 96% in isolated megacystis in our cohort. Unfortunately, a significant proportion of those additional anomalies, especially anorectal or cloacal malformations, escaped detection in the first trimester, when VAS was performed. This resulted in second trimester terminations of pregnancy in 15% of cases. In literature, about 50% of pregnancies were terminated after diagnosis of megacystis [2, 4–7, 16, 17, 31, 40, 50–52]. It may be assumed that the high termination rate in literature was caused mainly by parental fear of end-stage renal failure that may now be avoided by early VAS.
The etiology of megacystis is described to be highly variable causing obstructive or non-obstructive megacystis [2, 4–7, 16, 17, 31, 40, 51, 52]. Most commonly, obstructive megacystis in male fetuses is caused by isolated urethral anomalies such as posterior (or anterior) urethral valves in 57% of cases, urethral hypoplasia, stenosis or atresia or megalourethra in 7.4%. In these cases, the synonym lower urinary tract obstruction (LUTO) with megacystis can be used to correctly describe the situation. Most common non-obstructive megacystis are caused by vesico-ureteral reflux (VUR) that can mimic obstructive megacystis. Less commonly, but more complex are non-obstructive megacystis due to neuromuscular anomalies such as Prune Belly Syndrome (PBS) in 3.8%, Megacystis–Microcolon Intestinal–Hypoperistalsis Syndrome (MMIHS) in 1.1% or Cloacal Malformations in 0.7% of cases. Cloacal malformations usually affect female fetuses and carry an extremely bad prognosis. In one third of all published series a definite diagnosis of the underlying pathology was not made [2, 4–7, 16, 17, 31, 40, 51, 52]. Our cohort showed comparable results concerning type and prevalence of the underlying pathology, with PUV or stenotic or atretic urethra in 46%, 20% and 15% of cases, respectively. Neurogenic bladder due to MMIHS or Prune belly syndrome occurred in 5% each, and primary VUR due to insufficient flap-valves in 2.6%. Indeed, in 7.7% of our cases no underlying obstructive or non-obstructive pathology for megacystis could be detected postnatally, although all newborn babies had significant additional urinary anomalies including megaureters, urinoma or end-stage cystic–dysplastic kidney failure. These findings suggest that there must have been a disturbed urinary bladder drainage in the past maybe due to a stenotic or hypoplastic urethra that spontaneously improved through the general growth in size during ongoing pregnancy. Until now, no accurate sonographic marker was identified to reliably differentiate the underlying pathology in the prenatal situation. Therefore, the precise diagnosis of the underlying pathology still remains uncertain until birth and parents should be made aware of the residual risk of long-term urinary, intestinal, neurological and motoric co-morbidity in cases of complex megacystis or cloacal malformations. All physicians involved in the prenatal situation should be aware that due to the prenatal intervention a subset of severely affected children survive that would have died without intrauterine treatment. Especially affected female patients with complex cloacal malformations might not be corrected satisfactorily in some cases, leading to severe livelong morbidity and impairment. Accordingly, among the 3 female babies of our cohort with postnatally confirmed cloacal malformation the diagnosis was prenatally suspected in only 2 cases. In the third case, pregnancy was terminated prior to 22 weeks of gestation when intestinal and genital anomalies cannot be detected yet. Therefore, definite diagnosis was achieved postmortem.
Previously published studies described a low sensitivity of the ‘keyhole sign’ in detecting PUV [43, 53], as it was also observed in some fetuses with PBS and MMIHS [54]. Therefore, prenatal diagnosis of PUV was erroneous in more than 50% [1, 2, 54]. We could confirm that the ‘keyhole sign’ is no reliable marker to predict the underlying pathology or to differentiate between obstructive or non-obstructive megacystis (p = 0.137). However, we could demonstrate that the presence of the ‘keyhole sign’ was a reliable predictor of isolated megacystis (p = 0.001) even in the first trimester. In contrast, female sex was associated with complex megacystis in all cases and overall survival in female fetuses (with or without ‘keyhole sign’) was only 20%. We concluded, that the ‘keyhole sign’ is a reliable predictor of good outcome, whereas the absence of the ‘keyhole sign’ and female sex predict high mortality and morbidity. Those prognostic markers might help counseling parents in the prenatal situation.
In our cohort, 8 fetuses underwent late VAS > 17 + 0 weeks, all had severe oligo- or anhydramnios. First VAS in this subset of fetuses was performed at an average of 22 weeks of gestation (range, 19–26 weeks). Although some reports suggested that megacystis first diagnosed in the second trimester is more likely to result in live births [5], oligo- or anhydramnios was reported to be a strong predictor of lung hypoplasia and neonatal death [40, 42]. Therefore, we decided to perform late VAS, and although shunt complications occurred in 75% of cases and renal function was impaired in 37.5% postnatally, all fetuses survived with adequate pulmonary size and function without any need for mechanical respiratory support. We conclude that late VAS may be too late to prevent kidney damage in all cases but it may have a positive impact on pulmonary development and survival.
Fetal urine production starts as early as 9 weeks of gestation and the urinary bladder can be identified sonographically from this week on. In addition, nephrogenesis begins early at 4 weeks of gestation and is not completed prior to 34–36 weeks of gestation [47]. Because impaired drainage due to early onset obstruction of the lower urinary tract carries a substantial risk of impaired glomerulo- and nephrogenesis and longer duration significantly worsens kidney function, early detection of megacystis with timely intervention is crucial to avoid irreversible kidney damage. Therefore, every sonographer performing screening ultrasound in pregnancy should be aware of early signs of impaired bladder drainage and megacystis, especially during first trimester examinations.
A limitation of this study is its retrospective design. Furthermore, our cohort is small due to the naturally low prevalence of megacystis. In addition, although our trial described one of the largest single-center series so far, the total number of treated fetuses is still small and larger prospective series are desirable in future. A standardized approach to timing the VAS is needed. Therefore, we started a prospective clinical trial on VAS in the first trimester using the Somatex shunt with standardized postnatal follow-up protocol in our center in 2021 (DRKS00017779). In addition, a re-evaluation of the cohort described in this present paper will be conducted next year to assess the mid- and long-term effects of VAS on kidney and pulmonary function.
Conclusions
Early prenatal VAS is feasible from 12 weeks onward, can preserve neonatal kidney function in the majority of cases and enables survival in up to 96% of cases. It should be no longer a matter of debate that VAS should be offered to all fetuses with moderate or severe megacystis as early as possible. However, despite successful fetal intervention, parents should be aware of the potential risk of postnatal mid- or long-term kidney failure and of additional health impairment due to concomitant extra-renal anomalies that cannot be excluded at time of intervention.
Author contribution
IG: protocol/project development, data collection management, manuscript writing, CB: data analysis, TM: data collection, JSA: data collection, AK: data collection, MD: data collection, JK: data collection, GC: data collection, CT: data collection, SH: data collection, ML: data collection, TMB: data collection, ECW: manuscript editing.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors have not disclosed any funding.
Data availability
The author (IG) can confirm that all relevant data are included in the article.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abbott JF, Levine D, Wapner R. Posterior urethral valves: inaccuracy of prenatal diagnosis. Fetal Diagn Ther. 2005;13:179–183. doi: 10.1159/000020834. [DOI] [PubMed] [Google Scholar]
- 2.Robyr R, Benachi A, Daikha-Dahmane F, Martinovich J, Dumez Y, Ville Y. Correlation between ultrasound and anatomical findings in fetuses with lower urinary tract obstruction in the first half of pregnancy. Ultrasound Obstet Gynecol. 2005;25:478–482. doi: 10.1002/uog.1878. [DOI] [PubMed] [Google Scholar]
- 3.Warady BA, Chadha V. Chronic kidney disease in children: the global perspective. Pediatr Nephrol. 2007;22:1999–2009. doi: 10.1007/s00467-006-0410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bornes M, Spaggiari E, Schmitz T, Dreux S, Czerkiewicz I, Delezoide AL, El-Ghoneimi A, Oury JF, Muller F. Outcome and etiology of fetal megacystis according to the gestational age at diagnosis. Prenat Diagn. 2013;33:1162–1166. doi: 10.1002/pd.4215. [DOI] [PubMed] [Google Scholar]
- 5.Fievet L, Faure A, Coze SP, Harper L, Panait N, Braunstein D, Carson J, Gorincour G, Chaumoitre K, Guys JM, Alessandrini P, E’Ercole C, Merrot T. Fetal megacystis: etiologies, management, and outcome according to the trimester. Urology. 2014;84:185–189. doi: 10.1016/j.urology.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 6.Müller Brochut AC, Thomann D, Kluwe W, Di Naro E, Kuhn A, Raio L. Fetal megacystis: experience of a single tertiary center in Switzerland over 20 years. Fetal Diagn Ther. 2014;36:215–222. doi: 10.1159/000358300. [DOI] [PubMed] [Google Scholar]
- 7.Taghavi K, Sharpe C, Striger MD. Fetal megacystis: a systemativ review. J Pediatr Urol. 2017;13:7–15. doi: 10.1016/j.jpurol.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Capone V, Persico N, Berrettini A, Decramer S, De Marco EA, De Palma D, Familiari A, Feitz W, Herthelius M, Kazlauskas V, Liebau M, Manzoni G, Maternik M, Mosiello G, Schanstra JP, Vande Walle J, Wühl E, Ylinen E, Zurowska A, Schaefer F, Montini G. Definition, diagnosis and management of fetal lower urinary tract obstruction: consensus of the ERKNet CAKUT-obstrutive uropathy work group. Nat Rev. 2022;19:295–303. doi: 10.1038/s41585-022-00563-8. [DOI] [PubMed] [Google Scholar]
- 9.Nicolini U, Tannirandom Y, Vaughan J, Fisk NM, Nicolaides P, Rodeck CH. Further predictors of renal dysplasia in fetal obstructive uropathy: bladder pressure and biochemistry of fresh urine. Prenat Diagn. 1991;11:159–166. doi: 10.1002/pd.1970110305. [DOI] [PubMed] [Google Scholar]
- 10.Lipitz S, Ryan G, Samuell C, Haeusler MC, Robson SC, Dhillon HK, Nicolini U, Rodeck CH. Fetal urine analysis for the assessment of renal function in obstructive uropathy. Am J Obstet Gynecol. 1993;168:174–179. doi: 10.1016/S0002-9378(12)90909-6. [DOI] [PubMed] [Google Scholar]
- 11.Freedman AL, Bukowski TP, Smith CA, Evans MI, Johnson MP, Gonzalez R. Fetal therapy for obstructive uropathy: specific outcomes diagnosis. J Urol. 1996;156:720–724. doi: 10.1016/S0022-5347(01)65795-1. [DOI] [PubMed] [Google Scholar]
- 12.Crombleholme TM, Harrison MR, Golbus MS, Longaker MT, Langer JC, Allen PW, Anderson RL, Goldstein RB, Filly RA. Fetal intervention in obstructive uropathy: prognostic indicators and efficacy of intervention. Am J Obstet Gynecol. 1990;162:1239–1244. doi: 10.1016/0002-9378(90)90026-4. [DOI] [PubMed] [Google Scholar]
- 13.McLorie G, Farhat W, Khoury A, Geary D, Ryan G. Outcome analysis of vesicoamniotic shunting in a comprehensive population. J Urol. 2001;166:1036–1040. doi: 10.1016/S0022-5347(05)65913-7. [DOI] [PubMed] [Google Scholar]
- 14.Morris RK, Malin GL, Khan KS, Kilby MD. Systematic review of the effectiveness of antenatal intervention for the treatment of congenital lower urinary tract obstruction. BJOG. 2010;117:382–390. doi: 10.1111/j.1471-0528.2010.02500.x. [DOI] [PubMed] [Google Scholar]
- 15.Morris RK, Ruano R, Kilby MD. Effectiveness of fetal cystoscopy as a diagnostic and therapeutic intervention for lower urinary tract obstruction: a systematic review. Ultrasound Obstet Gynecol. 2011;37:629–637. doi: 10.1002/uog.8981. [DOI] [PubMed] [Google Scholar]
- 16.Morris R, Malin GL, Quinlan-Jones E, Middleton LJ, Diwakar L, Hemming K, Burke D, Daniels J, Denny E, Barton P, Roberts TE, Khan KS, Deeks JJ, Kilby MD. The percutaneous shunting in lower urinary tract obstruction (PLUTO) study and randomized controlled trial: evaluation of the effectiveness, cost-effectiveness and acceptability of percutaneous vesicoamniotic shunting for lower urinary tract obstruction. Health Technol Assess. 2013;17:1–232. doi: 10.3310/hta17590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris RK, Malin GL, Quinlan-Jones E, Middleton LJ, Hemming K, Burke D, Daniels JP, Khan KS, Deeks J, Kilby MD. Percutaneous vesicoamniotic shunting versus conservative management for fetal lower urinary tract obstruction (PLUTO): a randomized trial. Lancet. 2013;382:1496–1506. doi: 10.1016/S0140-6736(13)60992-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morris RK, Middleton LJ, Malin GL, Quinlan-Jones E, Daniels J, Khan KS, Deeks J, Kilhy MD. PLUTO Collaborative group. outcome in fetal lower urinary tract obstruction: a prospective registry study. Ultrasound Obstet Gynecol. 2015;456:424–431. doi: 10.1002/uog.14808. [DOI] [PubMed] [Google Scholar]
- 19.Ruano R, Sananes N, Sangi-Haghpeykar H, Hernandez-Ruano S, Moog R, Becmeuer F, Zaloszyc A, Giron AM, Morin B, Favre R. Fetal intervention for severe lower urinary tract obstruction: a multicenter case-control study comparing fetal cystoscopy with vesicoamniotic shunting. Ultrasound Obstet Gynecol. 2015;45:452–458. doi: 10.1002/uog.14652. [DOI] [PubMed] [Google Scholar]
- 20.Stadie R, Strizek B, Gottschalk I, Geipel A, Gembruch U, Berg C. Intrauterine vesicoamniotic shunting for fetal megacystis. Arch Gynecol Obstet. 2016;294:1175–2118. doi: 10.1007/s00404-016-4152-4. [DOI] [PubMed] [Google Scholar]
- 21.Ruano R, Dunn T, Braun MC, Angelo JR, Safdar A. Lower urinary tract obstruction: fetal intervention based on prenatal staging. Pediatr Nephrol. 2017;32:1871–1878. doi: 10.1007/s00467-017-3593-8. [DOI] [PubMed] [Google Scholar]
- 22.Nassr AA, Shazly AM, Abdelmagied AM, Araujo Junior E, Tonni G, Kilby MD, Ruano R. Effectiveness of vesicoamniotic shunt in fetuses with congenital lower urinary tract obstruction: an updated systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017;49:696–703. doi: 10.1002/uog.15988. [DOI] [PubMed] [Google Scholar]
- 23.Vinit N, Gueneuc A, Bessières B, Dreux S, Heidet L, Salomon R, Lapillonne A, De Bernardis G, Salomon LJ, Stirnemann JJ, Blanc T, Ville Y. Fetal cystoscopy and vesicoamniotic shunting in lower urinary tract obstruction: long-term outcome and current technical limitations. Fetal Diagn Ther. 2020;47:74–83. doi: 10.1159/000500569. [DOI] [PubMed] [Google Scholar]
- 24.Strizek B, Gottschalk I, Recker F, Weber E, Flöck A, Gembruch U, Geipel A, Berg C. Vesicoamniotic shunting for fetal megacystis in the first trimester with a somatex®intrauterine shunt. Arch Gynecol Obstet. 2020;302:133–140. doi: 10.1007/s00404-020-05598-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strizek B, Spicher T, Gottschalk I, Böckenhoff P, Simonini C, Berg C, Gembruch U, Geipel A. Vesicoamniotic shunting before 17+0 weeks in fetuses with lower urinary tract obstruction (LUTO): comparison of Somatex vs harrison shunt systems. J Clin Med. 2022;11:2359. doi: 10.3390/jcm11092359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kohl T, Fimmers R, Axt-Fliedner J, Degenhardt J, Brückmann M. Vesico-amniotic shunting prior to the completion of 16 weeks results in improved preservation of renal function in surviving fetuses with isolated severe lower urinary tract obstruction (LUTO) J Pediatr Urol. 2022;18:129–130. doi: 10.1016/j.jpurol.2022.02.014. [DOI] [PubMed] [Google Scholar]
- 27.Quintero RA, Johnson MP, Romero R, Smith C, Arias F, Guevara-Zuloaga F, Cotton DB, Evans MI. In-utero percutaneous cystoscopy in the management of fetal lower obstructive uropathy. Lancet. 1995;346:537–540. doi: 10.1016/S0140-6736(95)91381-5. [DOI] [PubMed] [Google Scholar]
- 28.Sananes N, Favre R, Koh CJ, Zaloszyc A, Braun MC, Roth DR, Moog R, Becmeur F, Belfort MA, Ruano R. Urological fistulas after fetal cystoscopic laser ablation of posterior urethral valves: surgical technical aspects. Ultrasound Obstet Gynecol. 2015;45:183–189. doi: 10.1002/uog.13405. [DOI] [PubMed] [Google Scholar]
- 29.Puzzo L, Giunta G, Caltabiano R, Cianci A, Salvatorelli L. Fetal Megacystis: a new morphologic, immunohistological and embryogenetic approach. Appl Sci. 2019;9:1–9. doi: 10.3390/app9235155. [DOI] [Google Scholar]
- 30.Smith-Harrison LI, Hougen HY, Timberlake MD, Corbett ST. Current applications of in utero intervention for lower urinary tract obstruction. J Pediatr Urol. 2015;11:341–347. doi: 10.1016/j.jpurol.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 31.Sebire NJ, Von KC, Rubio C, Snijders RJ, Nicolaides KH. Fetal megacystis at 10–14 weeks of gestation. Ultrasound Obstet Gynecol. 1996;8:387–390. doi: 10.1046/j.1469-0705.1997.08060387.x. [DOI] [PubMed] [Google Scholar]
- 32.Wheeler PG, Weaver DD. Partial urorectal septum malformation sequence: a report of 25 cases. Am J Med Genet. 2001;103:99–105. doi: 10.1002/ajmg.1510. [DOI] [PubMed] [Google Scholar]
- 33.Lesieur E, Barrois M, Bourdon M, Blanc J, Loeuillet L, Delteil C, Torrents J, Bretelle F, Grange G, Tsatsaris V, Anselem O. Megacystis in the first trimester of pregnancy: prognostic factors and perinatal outcomes. PLoS ONE. 2021 doi: 10.1371/journal.pone.0255890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kagan KO, Staboulidou I, Syngelaki A, Cruz J, Nicolaides KH. The 11–13 week scan: diagnosis and outcome of holoprosencephaly, exomphalos and megacystis. Ultrasound Obstet Gynecol. 2010;36:10–14. doi: 10.1002/uog.7646. [DOI] [PubMed] [Google Scholar]
- 35.Mercer LJ, Brown LG. Fetal outcome with oligohydramnios in the second trimester. Obstet Gynecol. 1986;67:840–842. doi: 10.1097/00006250-198606000-00019. [DOI] [PubMed] [Google Scholar]
- 36.Shipp TD, Bromley B, Pauker S, Frigoletto FD, Jr, Benacerraf BR. Outcome of singleton pregnancies with severe oligohydramnios in the second and third trimester. Ultrasound Obstet Gynecol. 1996;7:108–113. doi: 10.1046/j.1469-0705.1996.07020108.x. [DOI] [PubMed] [Google Scholar]
- 37.Jouannic JM, Hyett JA, Pandya PP, Gulbis B, Rodeck CH, Jauniaux E. Perinatal outcome in fetuses with megacystis in the first half of pregnancy. Prenat Diagn. 2003;23:340–344. doi: 10.1002/pd.593. [DOI] [PubMed] [Google Scholar]
- 38.Maizels M, Alpert SA, Houston JT, Sabbagha RE, Parilla BV, MacGregor SN. Fetal bladder sagittal length: a simple monitor to assess normal and enlarged fetal bladder size, and forecast clinical outcome. J Urol. 2004;172:1995–1999. doi: 10.1097/01.ju.0000142136.17222.07. [DOI] [PubMed] [Google Scholar]
- 39.Maymon R, Ben-Ami I, Vaknin Z, Reish O, Herman A. Is there an increased rate of megacystis in twins? Ultrasound Obstet Gynecol. 2005;26:197–199. doi: 10.1002/uog.1952. [DOI] [PubMed] [Google Scholar]
- 40.Lee J, Kimber C, Shakleton PO, Cheng W. Prognostic factors of severe foetal megacystis. ANZ J Surg. 2011;81:552–555. doi: 10.1111/j.1445-2197.2010.05578.x. [DOI] [PubMed] [Google Scholar]
- 41.Iuculano A, Peddes C, Monni G. Early fetal megacystis: is it possible to predict the prognosis in the first trimester? J Perinat Med. 2018;46:1035–1039. doi: 10.1515/jpm-2017-0351. [DOI] [PubMed] [Google Scholar]
- 42.Moxey-Mims M, Raju TNK. Anhydramnios in the setting of renal malformations: the national institutes of health workshop summary. Obstet Gynecol. 2018;131:1069–1079. doi: 10.1097/AOG.0000000000002637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fontanella F, Duin LK, Adama van Scheltema PN, Cohen-Overbeek TE, Pajkrt E, Bekker M, Willekes C, Bax CJ, Gracchi V, Oepkes D, Bilardo CM. Prenatal diagnosis of LUTO: improving diagnostic accuracy. Ultrasound Obstet Gynecol. 2018;52:739–743. doi: 10.1002/uog.18990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fontanella F, Maggio L, Verheij JB, Duin LK, VanScheltema PN, Cohen-Overbeek TA, Pajkrt E, Bekker M, Willekes C, Bax CJ, Gracchi V, Oepkes D, Bilardo CM. Fetal megacystic: a lot more than LUTO. Ultrasound Obstet Gynecol. 2019;53:779–787. doi: 10.1002/uog.19182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fontanella F, Van Schltema PNA, Duin L, Cohen-Oberbeek TE, Pajkrt E, Bekker MN, Willekes C, Oepkes D, Bilardo CM. Antenatal staging of congenital lower urinary tract obstruction. Ultrasound Obstet Gynecol. 2019;53:520–524. doi: 10.1002/uog.19172. [DOI] [PubMed] [Google Scholar]
- 46.Saccone G, D’Alessandro P, Escolino M, Esposito R, Arduino B, Vitigliano A, Quist-Nelson J, Berghella V, Espositio C, Zullo F. Antenatal intervention for congenital fetal lower urinary tract obstruction (LUTO): a systematic review and meta-analysis. J Mat Fetal Neonat Med. 2020 doi: 10.1080/14767058.2018.1555704. [DOI] [PubMed] [Google Scholar]
- 47.Krause M, Rak-Raszewska A, Pietilä I, Quaggin SE, Vainio S. Signaling durch kidney development. Cells. 2015;2:112–132. doi: 10.3390/cells4020112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harrison MR, Ross N, Noall R, de Lorimier AA. Correction of congenital hydronephrosis in uteri. I. The mode: fetal urethral obstruction produces hydronephrosis and pulmonary hypoplasia in fetal lambs. J Pediatr Surg. 1983;18:247–256. doi: 10.1016/S0022-3468(83)80094-3. [DOI] [PubMed] [Google Scholar]
- 49.Kurtz MP, Koh CJ, Jamail GA, Sangi-Haghpeykar H, Shamshirsaz AA, Espinoza J, Cass DL, Olutoye OO, Olutoye OA, Braun MC, Roth DR, Belfort MA, Ruano R. Factors associated with fetal shunt dislodgment in lower urinary tract obstruction. Prenat Diagn. 2016;36:720–725. doi: 10.1002/pd.4850. [DOI] [PubMed] [Google Scholar]
- 50.Liao AW, Sebire NJ, Geerts L, Cicero S, Nicolaides KH. Megacystis at 10–14 weeks of gestation: chromosomal defects and outcome according to bladder length. UOG. 2003;21:338–341. doi: 10.1002/uog.81. [DOI] [PubMed] [Google Scholar]
- 51.Ruano R, Yoshisaki CT, Salustiano EMA, Giron AM, Srougi M, Zugaib M. Early fetal cystoscopy for first-trimester severe megacystis. Ultrasound Obstet Gynecol. 2011;37:696–710. doi: 10.1002/uog.8963. [DOI] [PubMed] [Google Scholar]
- 52.Al-Hazmi H, Dreux S, Delezoide AL, Dommergues M, Lortat J, Oury JFB, El-Ghoneimi A, Muller F. Outcome of prenatally detected bilateral higher urinary tract obstruction or megacystis: sex-related study on a series of 709 cases. Prenat Diagn. 2012;32:649–654. doi: 10.1002/pd.3877. [DOI] [PubMed] [Google Scholar]
- 53.Bernardes LS, Aksnes G, Saada J, Masse V, Elie C, Dumez Y, Lortat-Jacob SL, Benachi A. Keyhole sigh: how specific is it for the diagnosis of posterior urethral valves? Ultrasound Obstet Gynecol. 2009;34:419–423. doi: 10.1002/uog.6413. [DOI] [PubMed] [Google Scholar]
- 54.Osborne NG, Bonilla-Musoles F, Machade LE, Raga F, Bonilla F, Ruiz F, Perez Guardia CM, Ahluwalia B. Fetal megacystis differential diagnosis. J Ultrasound Med. 2011;30:833–841. doi: 10.7863/jum.2011.30.6.833. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The author (IG) can confirm that all relevant data are included in the article.


