1. The landscape of mental health in Africa
The World Health Organization (WHO) points out that African countries have the highest suicide rates, predominantly driven by depression and anxiety [1]. Eleven people per 100,000 die by suicide in the African region. This figure is higher than the global average of nine per 100,000 people [1]. The male suicide rate in Africa is the highest of all regions at 18 per 100,000, while the global male average is 12.2 per 100,000 people [1]. About 29 million people suffer from depression in Africa [2], and according to the 2023 World Happiness Report, 17 out of the 24 countries with less happiness are found in Africa [3].
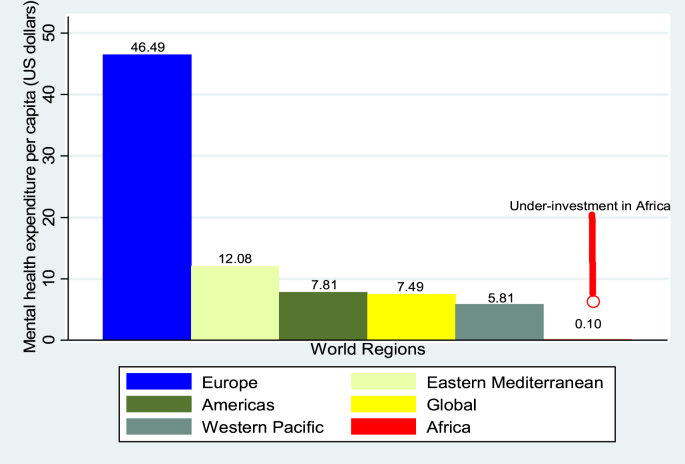
Despite these worrying statistics --mental health programs remain grossly underfunded in the continent (See Fig. 1). For example, in 2020, Africa spent less than 1.00 US$ per capita on mental health, while continents like Europe spent US$ 46.49 per capita [4]. It is, therefore, not surprising that the continent records higher suicide rates considering the under-investment in mental health. The current global spending on mental health is US$ 7.49 per capita [4] (See Fig. 1).
Fig. 1.
2020 governments expenditure on mental health per capita.
Source: Authors analysis using 2023 data from Statista [4].
The lack of mental health investments and political apathy displayed by many African governments in addressing mental health is unfortunate [5]. The continent has one mental health worker per 100,000 people, compared with a global average of nine per 100,000 [5]. The continent also performs poorly in terms of the number of psychiatrists, the number of hospital beds for patients with mental illness, and the coverage of outpatient facilities. Hence, the proportion of Africans who receive treatment and care for mental health ill-health is unacceptably low [6]. For example, the global annual rate of visits to mental health outpatient facilities is 1051 per 100,000 populations; in Africa, the rate is 14 per 100,000 [5].
The WHO has already called on African governments and private sectors to acknowledge mental health as a priority and increase the necessary investments [7]. Indeed, a continent will only be able to meet the mental health needs of its population if it mobilizes additional funds and human resources for mental health. Africa must reflect on the current under-investment and find innovative strategies to improve funding for mental health programs urgently [6].
2. What could be a solution to the mental health crisis in Africa?
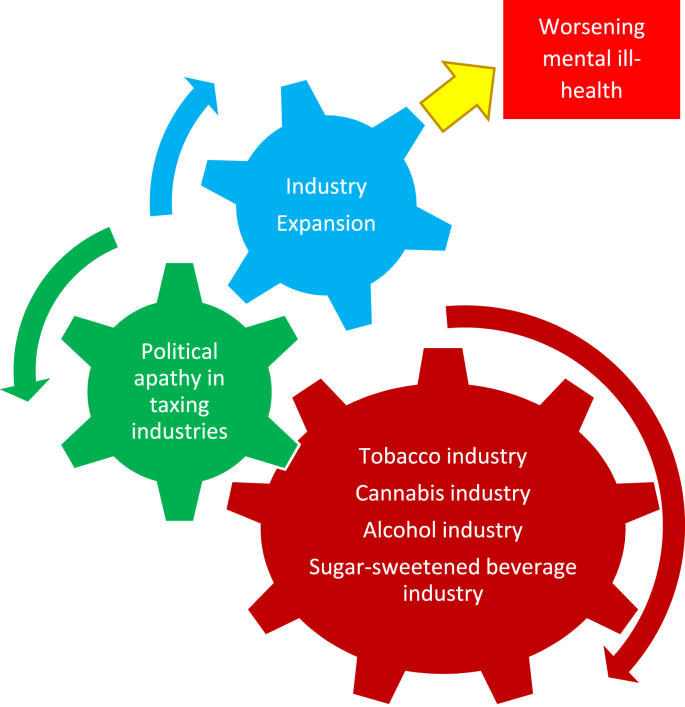
In our view-commercial determinants factors contribute to a significant proportion of mental, neurological, and substance use disorders and are associated with accelerating behavioral and psychosocial risk factors. Government active involvement through progressive tax policies designed to prevent the harmful effects of these commercial determinants factors is essential. Indeed, the political apathy in taxing industries associated with worsening mental ill-health is regressive (See Fig. 2) and Africa need to correct this error immediately.
Fig. 2.
Commercial determinants factors that worsens mental ill-health.
Source: Authors analysis based on meek taxation policies to make these industries account for mental health erosions.
For example, in 2019, Africa contributed US$37 billion to the global cannabis market [8]. Currently, there is political apathy in taxing the cannabis sector for mental health investment in Africa even though cannabis consumption worsens mental ill-health [9]. Countries like Canada and the United States of America (US) are using cannabis taxation to fund mental health and other public health programs [10,11]. Such taxation strategies could be adopted in Africa to mitigate the economic burden of mental ill-health.
However, the cannabis industry is not the only culprit that could be targeted to fund mental health programs. Several other industries could be taxed or made to pay for preventing or treating mental health issues. These include the sugar-sweetened beverage (SSB) industry (2023 revenue valued at US$ 70 billion in Africa and projected to reach US$78 billion in 2028) [12], the tobacco industry (2023 revenue valued at US$56 million in Africa and projected to reach US$143 million in 2028) [12], and the alcohol industry (2023 revenue valued US$367 million in Africa and projected to reach US$ 437 million in 2028) [12]. We identified all these industries based on the profitability in the continent, their role in aggravating mental ill-health, and their lack of accountability in financing African mental health programs to date.
For example, a large body of evidence suggests that a possible contributor to depression and anxiety is sugar overconsumption [13]. However, no African country implements a sugar tax to address mental health conditions. Eswatini, for example, has not implemented an SSB tax policy [14] despite having a depression prevalence of 47% in the women population group [15] and being the influential producer of sugar for Africa, US, and European markets [16]. The Eswatini government could prioritize SSB taxation to finance not only obesity and diabetes but also mental health programs. In other countries, the US, for example—uses a portion of SSB tax revenues to fund mental health [17]. African countries can do the same.
The tobacco industry is another culprit. Evidence from various population studies shows that smoking has adverse impacts on mental health in terms of both enhancing the risk of mental illness and increasing psychiatric symptoms in those with and without diagnosed conditions [18]. Therefore, the African governments needs to tax the tobacco industry aggressively considering that-it does contribute to worsening mental health problems.
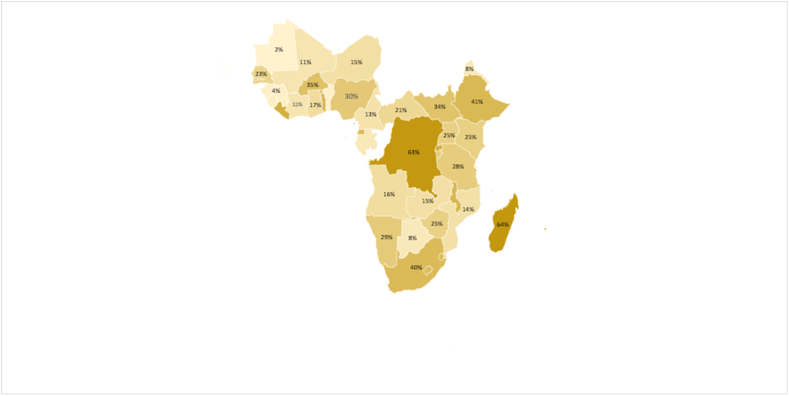
In 2020, Africa scored 1.36 out of 5 on the tobacconomics tax scorecard [19]. A score of 5 represents the best tobacco tax regime that reduces tobacco consumption. Africa's score is lower than the average score for lower-middle-income countries (1.51), lower than the average score for upper-middle-income countries (2.13), and lower than the global average score (2.07). Such poor tobacco tax score reflects the rising tobacco consumption due to meek tobacco taxation policies. For example, the WHO recommends at least 75% excise tax share on tobacco products [20]. Currently -no Sub-Saharan African countries has achieved the 75% WHO recommendation [21] (See Fig. 3).
Fig. 3.
Percentage of the excise tax share in most sold brands of cigarettes in Sub-Saharan African countries.
Source: Authors analysis based on 2021 World Health Organisation Global Tobacco Control Report [22].
Hence, there is still a fiscal space for aggressive tobacco taxation in the continent, which could benefit both tobacco users [23] and those already suffering from mental ill-health. Kenya, for example, loses US$40 billion per year from the tobacco industry due to a poor tax collection system [24]. This figure is five times the 2023 Kenyan national revenue and could easily finance the existing poorly funded mental health programs. Recently, representatives from the United Nations have recommended that developing countries must use tobacco tax to fund the neglected mental health agenda [25].
Lastly, alcohol consumption also contributes to mental ill-health [26]. However, the African governments have not implemented progressive tax policies [27] to make the alcohol industry account for its share in contributing to poor mental health. According to the recent review article - doubling alcohol taxes or introducing aggressive minimum unit price reduced alcohol consumption by 10% [28]. Africa need to adopt such progressive policies.
The growing influence of the alcohol industry, measured by possible donations to global health institutions like the World Health Organization [29], is worrying and can be perceived as an instrument to buy influence to exempt the alcohol industry from accountability. African governments need to reconsider the role of alcohol and tax this industry more aggressively to maximize revenue collection for mental health funding.
3. Conclusion
We submit that economic data does not support the notion that Africa does not have enough internal resources to finance mental health programs. The cost of inaction in this realm is tremendous. For example, the estimated annual national costs of Dementia alone ranged between US$1.04 million (in low income countries with gross national income per capita that is less than $1036) to US$195 billion (in upper middle-income countries with gross national income per capita between US$4096 and US$12 695) [30].
Indeed, the continent must invest in protecting brain health, which is critical to societal prosperity and individual well-being. Industries that do the most damage to brain health should be taxed to support Africa's mental health programs. Governments can and must do much more by taxing the cannabis, sugar, tobacco, and alcohol industries to fund mental health programs. After all, these sectors are commercial determinants of mental ill-health, and the WHO has called upon corporates to play a meaningful role in improving brain health.
Data availability statement
All economic figures come from the 2023 Statista database.
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
Contributorship statement
CM led the writing of the manuscript with input from ON, CU, MK, TT, EB, KB, MK, DT and ZM.
CM, ON, MK, MK and CU provided the African mental health landscape. CM provided senior oversight to the economic arguments of the manuscript. All authors edited and approved the final version.
Ethical approval
Our institution does not require ethical approval for this type of study.
Funding
We are grateful to receive support from BMI -Aga Khan University internal funding
Availability of data and materials
The data that support the findings of this paper is available from the 2020 Statista database upon reasonable request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors are grateful to the funding from Aga Khan University. Brain and Mind Institute.
Acknowledgments
None.
References
- 1.World Health Organization . WHO data; 2023. Suicide Mortality Rate (Per 100 000 Population)https://www.who.int/data/gho/data/indicators/indicator-details/GHO/suicide-mortality-rate-(per-100-000-population Available at: [Google Scholar]
- 2.Gbadamosi I., et al. Depression in sub-Saharan Africa. IBRO Neurosci. Rep. 2022 Mar 17;12:309–322. doi: 10.1016/j.ibneur.2022.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helliwell F., Huang H., Norton M., Goff L., Wang S. World Happiness Report. eleventh ed. Sustainable Development Solutions Network; 2023. World happiness, trust and social connections in times of crisis.https://worldhappiness.report/ed/2023/world-happiness-trust-and-social-connections-in-times-of-crisis/#ranking-of-happiness-2020-2022 (Chapter 2) [Google Scholar]
- 4.https://www.statista.com/ Statista. Government expenditure on Mental Health per capita in 2020 by region (USD). Statista 2022. Available at.
- 5.Sankoh O., Sevalie S., Weston M. Mental health in Africa. Lancet Global Health. 2018 Sep;6(9):e954–e955. doi: 10.1016/S2214-109X(18)30303-6. [DOI] [PubMed] [Google Scholar]
- 6.Nicholas A., Joshua O., Elizabeth O. Accessing mental health services in Africa: current state, efforts, challenges and recommendation. Ann. Med. Surg. (Lond) 2022 Sep. 81 doi: 10.1016/j.amsu.2022.104421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mugarisi V. Call for increased investments towards mental health services. https://www.afro.who.int/news/call-increased-investments-towards-mental-health-services-vivian-mugarisi WHO .2020.10. Available at:
- 8.Mostert C. Cannabis corporates should be taxed to fund mental health programmes. The conversation. 2022;10 doi: 10.1016/j.puhip.2022.100314. https://theconversation.com/cannabis-corporates-should-be-taxed-to-fund-mental-health-programmes-191624#:~:text=The%202019%20Africa%20Regional%20Hemp,African%20mental%20health%20prevention%20programmes [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mostert C., et al. A call for prudent taxation of cannabis corporates to fund mental health programmes. Pub. Health Practice. 2022;4 doi: 10.1016/j.puhip.2022.100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Purtle J., Brinson K., Stadnick N.A. Earmarking excise taxes on recreational cannabis for investments in mental health: an underused financing strategy. JAMA Health Forum. 2022;3(4) doi: 10.1001/jamahealthforum.2022.0292. [DOI] [PubMed] [Google Scholar]
- 11.Shanahan M., Cyrenne P. Cannabis policies in Canada: how will we know which is best? Int. J. Drug Pol. 2021 May;91 doi: 10.1016/j.drugpo.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 12.https://www.statista.com/outlook/emo/tobacco-products/smoking-tobacco/Africa Soft Drinks - Africahttps://www.statista.com/outlook/cmo/non-alcoholic-drinks/soft-drinks/africa Alcoholic Drinks - Africahttps://www.statista.com/outlook/emo/beverages/alcoholic-drinks/africa Statista dataset: Smoking Tobacco - Africa: Available at: 04/14/2024.
- 13.Kim J., et al. Sucrose withdrawal induces depression and anxiety-like behavior by Kir2. 1 Upregulat. Nucl. Accumbens Neuropharmacol. 2018;130:10–17. doi: 10.1016/j.neuropharm.2017.11.041. [DOI] [PubMed] [Google Scholar]
- 14.EQUINET Discussion Paper 130. Taxing for Health: Taxes on Sugar-Sweetened Beverages in East and Southern African Countries. Training and Research Support Centre. 2023. https://equinetafrica.org/sites/default/files/uploads/documents/EQ%20Disss%20130%20SSB%20taxation%20July2023_0.pdf 07. Available at: [Google Scholar]
- 15.Dlamini L.P., Mahanya S., Dlamini S.D., Shongwe M.C. Prevalence and factors associated with postpartum depression at a primary healthcare facility in Eswatini. S. Afr. J. Psychiatr. 2019 Oct 24;25(0):1404. doi: 10.4102/sajpsychiatry.v25i0.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moobi M., Woody K. 2023. https://apps.fas.usda.gov/newgainapi/api/Report/DownloadReportByFileName?fileName=Sugar%20Annual_Pretoria_Eswatini_SZ2023-0001.pdf (Sugar Annual [Eswatini]. Global Agricultural Information Network). Report Number SZ2023-0001. 04.26. [Google Scholar]
- 17.Krieger J., Magee K., Hennings T., Schoof J., Madsen K.A. How sugar-sweetened beverage tax revenues are being used in the United States. Prev. Med. Rep. 2021 Apr 30;23 doi: 10.1016/j.pmedr.2021.101388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Firth J., Wootton R.E., Sawyer C., Taylor G.M. Clearing the air: clarifying the causal role of smoking in mental illness. World Psychiatr. 2023 Feb;22(1):151–152. doi: 10.1002/wps.21023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaloupka F., Drope J., Siu E., Vulovic V., Stoklosa M., Mirza M., RodriguezIglesias G., Lee H. Health Policy Center, Institute for Health Research and Policy. University of Illinois Chicago; Chicago, IL: 2020. www.tobacconomics.org (Tobacconomics Cigarette Tax Scorecard). [Google Scholar]
- 20.World Health Organization . World Health Organization; Geneva: 2019. WHO global tobacco control report.https://www.who.int/tobacco/global_report/en/ (2019: Offer to Help Quit Tobacco). [Google Scholar]
- 21.Egbe C.O., Magati P., Wanyonyi E., et al. Landscape of tobacco control in sub-Saharan Africa. BMJ Tobacco Control. 2022;31:153–159. doi: 10.1136/tobaccocontrol-2021-056540. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization . Geneva World Health Organization; 2021. https://www.who.int/teams/health-promotion/tobacco-control/global-tobacco-report-2021 (WHO Report on the Global Tobacco Epidemic 2021: Addressing New and Emerging Products). [Google Scholar]
- 23.Ho L., Schafferer C., Lee M., et al. Raising cigarette excise tax to reduce consumption in low-and middle-income countries of the Asia-Pacific region: a simulation of the anticipated health and taxation revenues impacts. BMC Publ. Health. 2018;18:1187. doi: 10.1186/s12889-018-6096-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.University of Bath Kenya- country profile. https://tobaccotactics.org/article/kenya-country-profile/ Available at:
- 25.Uji K., Oh C. UNDP Online Pulication. 2023. Why tobacco on World mental health day? p. 10.https://www.undp.org/asia-pacific/blog/why-tobacco-world-mental-health-day#:~:text=The%20strategic%20use%20of%20increased,to%20prevent%20tobacco%20industry%20interference [Google Scholar]
- 26.Nunes E. Alcohol and the etiology of depression. Am. J. Psychiatr. 2023;180:179–181. doi: 10.1176/appi.ajp.20230004. [DOI] [PubMed] [Google Scholar]
- 27.International Movendi. 2022. Policy News: Special Feature: Africa's Alcohol Burden.https://movendi.ngo/news/2022/08/22/special-feature-africas-alcohol-burden/ 07.22. [Google Scholar]
- 28.Kilian C., et al. Reducing alcohol use through alcohol control policies in the general population and population subgroups: a systematic review and meta-analysis. E Clin. Med. 2023 May 10;59 doi: 10.1016/j.eclinm.2023.101996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Commentary The WHO Foundation should not accept donations from the alcohol industry. BMJ Glob. Health. 2022 doi: 10.1136/bmjgh-2022-008707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mattap S., Mohan D., McGrattan A.M., et al. The economic burden of dementia in low- and middle-income countries (LMICs): a systematic review. BMJ Glob. Health. 2022;7 doi: 10.1136/bmjgh-2021-007409. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All economic figures come from the 2023 Statista database.
The data that support the findings of this paper is available from the 2020 Statista database upon reasonable request.