Abstract
Background
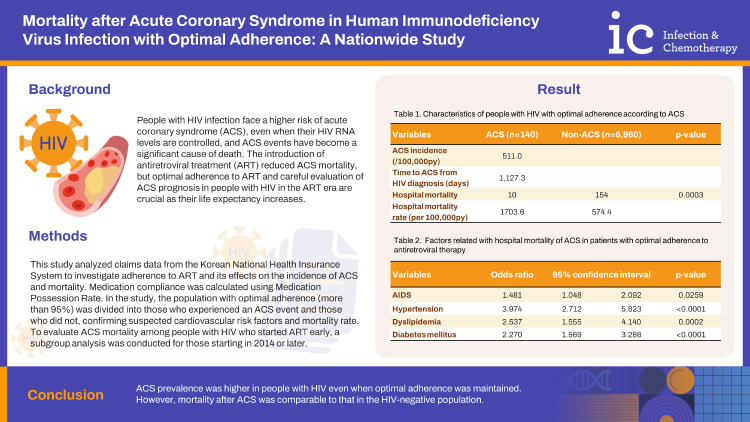
There have been few studies on the outcome of acute coronary syndrome (ACS) in human immunodeficiency virus (HIV) infection in the era when antiretroviral therapy (ART) is generalized and most of them have achieved viral suppression. Using claims data, we aimed to assess the mortality after atherosclerotic cardiovascular events in people with HIV (PWH) who maintain optimal adherence to ART.
Materials and Methods
We used claims data from the National Health Insurance of the Korea to confirm newly diagnosed PWH from 2009 to 2019, and measured ART adherence. ACS and mortality were confirmed in PWH who showed optimal adherence to ART.
Results
Among 7,100 PWH with optimal adherence and during 27,387 person-year of follow-up duration, ACS was confirmed in 140 (2.0%) cases, which was 1.3 times greater than statistics of the Korean general population (511.0 vs. 383.1 per 100,000). Acquired immunodeficiency syndrome, hypertension, dyslipidemia, and diabetes mellitus were associated with the development of ACS in PWH with optimal adherence. Mortality was confirmed in 10 cases, which is 7.1% overall and 2.9% when limited to myocardial infarction. It was comparable with the mortality rate of the Korean general population after myocardial infarction (8.9%).
Conclusion
ACS prevalence was higher in PWH even when optimal adherence was maintained. However, mortality after ACS was comparable to that in the HIV-negative population.
Keywords: HIV, Insurance claim review, Myocardial infarction, Anti-retroviral agents, Epidemiology
Graphical Abstract
Introduction
People with human immunodeficiency virus (HIV) infection are one and a half to two times more likely to be at risk of atherosclerotic cardiovascular disease than the HIV-negative population [1]. The underlying mechanisms for HIV-associated cardiovascular disease include the effects of the HIV proteins on immune and vascular cells, the immunodeficiency caused by the HIV infection, co-infection with cytomegalovirus, microbial translocation from the gut, chronic inflammation, and immune cell activation [2]. People with HIV-1 RNA levels of less than 500 copies/mL still have an excess risk of 1.39 times compared to HIV-negative individuals [3]. The incidence of cardiovascular disease is expected to rise further as people with HIV (PWH) aging becomes more pronounced.
Cardiovascular events have become a significant cause of death in PWH [4]. There are reports that PWH have worse outcomes after cardiovascular events than the HIV-negative population. HIV infection is related to a higher mortality [5], and a higher incidence of ischemic heart failure after myocardial infarction [6]. In the United States, cardiovascular disease is the third highest cause of death or hospitalization for PWH [7].
Higher HIV viral load and lower CD4-positive cell count were found to be predictors of mortality [8]. However, the introduction of antiretroviral therapy decreased mortality of cardiovascular disease between 1995 and 2001 [9]. As the widespread use of highly active antiretroviral therapy increases the life expectancy of PWH, a low CD4-positive T cell count is no longer associated with an increased risk of cardiovascular mortality [10]. Optimal adherence to ART reduces inflammation. Incomplete adherence is associated with an increased risk of death even in patients with viral suppression [11]. Because the majority of PWH are in controlled viral status and maintain optimal adherence, the prognosis of cardiovascular events in PWH needs to be re-evaluated in the anti-retroviral therapy (ART) era.
The Korea has a national health insurance (NHI) system. As the incidence of acute coronary syndrome (ACS) is as low as 1.2 myocardial infarction (MI) case per 1,000 person-years in PWH [12], assessing the difference of outcome according to ART adherence is limited at the individual hospital level. Therefore, we aimed to elucidate the outcome of ACS in PWH based on adherence to ART using the claims data of NHI.
Materials and methods
1. Data source
This study used claims data for reimbursement to the hospital from NHI. Korean National Health Insurance System is a universal health insurance system for the whole nation. Ninety seven percent of citizens have this form of medical insurance, and 3% of them in the form of medical aid. After a clinic visit by a patient, medical institutions file claims, which are evaluated by the Health Insurance Review & Assessment Service [HIRA]. All diagnostic codes and orders recorded by the medical institution, and all test items and medication prescriptions, are collected. Information about national regions and medical visits, such as inpatient, emergency room, or outpatient, are included.
2. Ethics statement
The institutional review board of the Seoul National University Boramae Medical Centre (IRB No. 07-2017-8/052) approved this study. The board waived informed consent due to the use of an existing secondary database.
3. Study population
We screened our study population using the International Classification of Diseases 10th Revision (ICD-10) code of HIV diagnosis from 2007 to 2019. We included newly diagnosed PWH in calculating compliance with ART after excluding PWH who visited the clinic for two years between 2007 and 2009. Then we collected PWH who were prescribed ART for more than six months to investigate the long-term effect. We excluded individuals believed to be having treatment for hepatitis B considering the contents of prescription (e.g., tenofovir monotherapy) and who were prescribed ART as postexposure prophylactic measures.
4. Definitions of variables
PWH were defined as people with any ICD-10 codes including HIV (B20-B24) and prescription of antiretroviral agent in combination use. Underlying diseases was confirmed with ICD-10 codes. Acquired immunodeficiency syndrome (AIDS) was confirmed by specific antibiotics prescription for prophylaxis of opportunistic infections (i.e., prophylactic dosage of trimethoprim-sulfamethoxazole or dapsone).
A related diagnosis, which was recorded during admission confirmed the presence of ACS (I20-I23). MI was defined similarly in diagnostic codes (I21-I23) [13,14]. Patients with ACS were selected when there was (or were) at least one ACS diagnosis (or diagnoses) on the claims issued after HIV infection diagnosis. ACS diagnosis without admission event was classified as underlying diseases. The date of the first admission with an ACS diagnosis was defined as the date of the ACS event. Mortality rates after ACS were collected using mortality codes, and hospital mortality of ACS admission was defined as ACS group mortality. In the non-ACS group, all-cause hospital mortality cases were collected. Moreover, major cardiovascular risk factor comorbidities were searched by diagnosis.
5. Statistical analysis
The medication possession ratio (MPR) was used to calculate medication adherence to ART. We followed the same procedure as in our previous study [15]. Briefly, MPR calculated as the total sum of HAART prescribed days, divided by the time elapsed between the date of the first ART prescription date to December 31, 2019, the last day of the follow-up period. Optimal adherence was defined as more than 95% of MPR.
Descriptive analyses were performed for independent variables/time-dependent outcome variables in total person-years. The incidence rate was re-calculated as 100,000 person-years for standardization. The study population was divided into two groups: those who had an ACS event, and those who did not, and the results were compared using the Chi-square test or Fisher’s exact test were used along to the frequency of cell. Then a logistic regression model was designed using variables that showed significant differences in univariate analysis and suspected cardiovascular risk factors.
Then a subgroup analysis was performed for the population after 2014, when the general ART guideline was distributed in Korea. For the 2013 Korean guideline, ART was recommended in all PWH regardless CD4-positive T cell count. The subgroup analysis for PWH patients who started ART after 2014 was conducted, to determine the ACS mortality in relatively healthy PWH who started ART early. All data analysis was conducted using SAS Enterprise Guide 7.1 (SAS Institute Inc., Cary, NC, USA).
Results
Total 24,459 had HIV diagnostic ICD-10 codes on their claim data during the study period (2007 - 2019). After excluding patients who had an HIV diagnosis prior to 2009, the number of newly diagnosed people in the study period was 17,179. We retrieved 15,764 after ruling out mono-treatment for hepatitis B. Then, 10,363 PWH who had been on ART for more than 180 days were confirmed. Finally, 68.5% of them (n = 7,100) were classified as population with the optimal adherence. Total follow-up period of the study population was 27,396 person-year.
The population aged 40 - 59 was 35.1% (n = 2,491) and the population aged over 60 was 7.1% (n = 504, Supplementary Table 1). Men were 93.2% (n = 6,620). AIDS was confirmed in 32.1% (n = 2,279). ACS was confirmed in 140 PWH with optimal adherence and mortality was confirmed in 10 cases in the ACS group. Among 140, MI was 41 (29.3%). It is calculated as 511.0 per 100,000py of ACS events incidence. The mean time to ACS event from HIV diagnosis was 1,127.3 days.
There were more older people in the ACS group, compared to the non-ACS group, such as those aged 40-59 as 62.9% vs. 34.5% and those aged over 60 as 27.1% vs. 6.7% (Table 1). There was no significant difference in the male to female ratio. There were more AIDS patients in the ACS group (44.3% vs. 31.9%, P = 0.0006). By insurance type, beneficiaries of the Medical Aids were more likely in ACS group without statistical significance (7.1% vs.3.7%, P = 0.2130). Regards to underlying diseases, hypertension, dyslipidemia, diabetes, chronic kidney disease, malignancy and psychiatric disease were more in the ACS group. Chronic hepatitis B and C were more common in ACS group without statistical significance.
Table 1. Characteristics of people with human immunodeficiency virus infection with optimal adherence according to acute coronary syndrome (n = 7,100).
| Variables | ACS (n = 140) | Non-ACS (n = 6,960) | P-value | |
|---|---|---|---|---|
| Follow-up duration (py) | 742 | 26,654 | ||
| Age (yrs) | <0.0001 | |||
| Under 20 | 0 | 198 (2.8) | ||
| 20 - 39 | 14 (10.0) | 3,893 (55.9) | ||
| 40 - 59 | 88 (62.9) | 2,403 (34.5) | ||
| Over 60 | 38 (27.1) | 466 (6.7) | ||
| Male | 133 (95.0) | 6,487 (93.2) | 0.7072 | |
| National Medical Aid | 10 (7.1) | 260 (3.7) | 0.2130 | |
| Tertiary hospital | 90 (64.3) | 4,397 (61.7) | 0.7005 | |
| Region of clinics | 0.6163 | |||
| Greater Seoula | 95 (67.9) | 4,762 (68.4) | ||
| Others | 45 (32.1) | 2,217 (31.9) | ||
| AIDS | 62 (44.3) | 2,217 (31.9) | 0.0006 | |
| Comorbidities | ||||
| Hypertension | 87 (62.1) | 1,342 (19.3) | <0.0001 | |
| Dyslipidemia | 120 (85.7) | 4,158 (59.7) | <0.0001 | |
| Diabetes mellitus | 69 (49.3) | 1,154 (16.6) | <0.0001 | |
| Chronic hepatitis B | 5 (3.6) | 309 (4.4) | 1.0000 | |
| Chronic hepatitis C | 7 (5.0) | 236 (3.4) | 0.2942 | |
| Chronic kidney disease | 11 (7.9) | 141 (2.0) | 0.0378 | |
| Malignancy | 74 (57.1) | 2,488 (35.7) | 0.0012 | |
| Psychiatric disease | 80 (57.1) | 2,971 (42.7) | 0.0139 | |
| Clinical outcomes | 0.0003 | |||
| Hospital mortality | 10 | 154 | ||
| Hospital mortality rate (per 100,000 py) | 1,703.60 | 574.4 | ||
The value denotes the subject number (%) unless otherwise indicated.
aSeoul, Incheon, and Kyeonggi-do.
ACS, acute coronary syndrome; py, person-year; yrs, years; AIDS, acquired immunodeficiency syndrome.
All-cause hospital mortality cases of whom experienced ACS among PWH with optimal adherence were 10 (7.1% of ACS group). Non-ACS group showed all-cause mortality of 154 cases (2.2%) during the study period. The all-cause hospital mortality rate was higher as 1,703.6 per 100,000 person-year, compared to 574.4 per 100,000 person-year in the non-ACS group. The duration of ACS to death was 357.7 days. MI events were confirmed in 41 (29.3%) in the ACS group with hospital mortality rate of 9.8% (4 cases).
In the logistic regression model, variables such as AIDS, hypertension, dyslipidemia, and diabetes mellitus showed a significant association with the occurrence of ACS in PWH with optimal adherence (odd ratio [OR] for AIDS 1.481, 95% confidence interval [CI]: 1.048 - 2.092; OR for hypertension 3.974, 95 CI: 2.712 - 5.823, OR for dyslipidemia 2.537, 95 CI: 1.555 - 4.140; OR for diabetes mellitus 2.270, 95 CI: 1.569 - 3.286, Table 2). Malignancy showed a marginal association. Variables that showed significant differences in univariate analysis such as National Medical Aid chronic kidney disease, and psychiatric disease lost their statistical significance.
Table 2. Factors related with hospital mortality of acute coronary syndrome in patients with optimal adherence to anti-retroviral therapy (n = 140).
| Variables | Univatiate | Multiple | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Odds ratio | 95% confidence interval | P-value | Odds ratio | 95% confidence interval | P-value | ||||
| Age at diagnosis | |||||||||
| Under 20 | <0.001 | <0.001 | >999.999 | 0.9571 | |||||
| 20 - 39 | Ref | Ref | Ref | Ref | |||||
| 40 - 59 | 10.183 | 5.781 | 17.939 | 0.9451 | |||||
| Over 60 | 22.675 | 12.195 | 42.162 | 0.9327 | |||||
| Male | 1.384 | 0.644 | 2.976 | 0.4051 | |||||
| National medical aid | 1.983 | 1.030 | 3.817 | 0.0405 | 1.096 | 0.557 | 2.160 | 0.7900 | |
| Tertiary hospital | 1.116 | 0.787 | 1.582 | 0.5939 | |||||
| Region of clinics | 0.974 | 0.681 | 1.394 | 0.8868 | |||||
| AIDS | 1.701 | 1.214 | 2.383 | 0.0020 | 1.481 | 1.048 | 2.092 | 0.0259 | |
| Comorbidities | |||||||||
| Hypertension | 6.872 | 4.859 | 9.719 | <0.0001 | 3.974 | 2.712 | 5.823 | <0.0001 | |
| Dyslipidemia | 4.043 | 2.512 | 6.507 | <0.0001 | 2.537 | 1.555 | 4.140 | 0.0002 | |
| Diabetes mellitus | 4.890 | 3.490 | 6.852 | <0.0001 | 2.270 | 1.569 | 3.286 | <0.0001 | |
| Viral hepatitis B | 0.797 | 0.324 | 1.961 | 0.6218 | |||||
| Viral hepatitis C | 1.500 | 0.694 | 3.242 | 0.3030 | |||||
| Chronic kidney disease | 4.124 | 2.179 | 7.804 | <0.0001 | 1.339 | 0.688 | 2.607 | 0.3910 | |
| Malignancy | 2.015 | 1.441 | 2.819 | <0.0001 | 1.430 | 1.011 | 2.022 | 0.0433 | |
| Psychiatric disease | 1.790 | 1.277 | 2.510 | 0.0007 | 1.160 | 0.815 | 1.651 | 0.4087 | |
Ref, reference; AIDS, Acquired immune deficiency syndrome.
The incidence of ACS in PWH diagnosed after 2014 was 602.9 per 100,000 person-year (py) (48 ACS patients among 11,445 total follow-up py) and their case fatality were 7.2% (5/69, Table 3). By the characteristics of the ACS and the non-ACS subgroups after 2014, there were more patients between 20 and 40 in the non-ACS group than in the ACS group (4.3% vs. 59.5%, P <0.0001, Table 3). The fact that the middle age of 40 - 59 years of age accounted for half of the ACS group was similar to the entire study population. AIDS were significantly more in the ACS group, along with the entire study population (47.8% vs. 28.0%, respectively). There was no difference between the ACS group and the non-ACS group in grade and region of hospital, the same as the entire study population. In terms of underlying diseases, the subgroup analysis after 2014 showed the same distribution as the entire study population analysis, as hypertension, dyslipidemia, diabetes mellitus, malignancy, and chronic kidney disease were more in the ACS group. Chronic hepatitis B and C were more common in ACS group, however, still were not different significantly. Hospital mortality was also significantly higher in the ACS group as the entire study population analysis. In the logistic regression model, the relationship trends for most variables were the same in the subgroup analysis (Table 4). However, dyslipidemia lost a positive relationship with ACS and chronic kidney diseases showed an association with ACS as OR = 2.553, 95 CI: 1.123 - 5.807.
Table 3. Characteristics of people with human immunodeficiency virus infection after 2014 with optimal adherence according to acute coronary syndrome (n = 4,836).
| Variables | ACS (n = 69) | Non-ACS (n = 4,767) | P-value | |
|---|---|---|---|---|
| Follow-up duration (py) | 198 | 11,246 | ||
| Age (yrs) | <0.0001 | |||
| Under 20 | 0 (0) | 130 (2.7) | ||
| 20 to 39 | 3 (4.3) | 2,853 (59.5) | ||
| 40 to 59 | 42 (60.9) | 1,489 (31.2) | ||
| Over 59 | 24 (34.8) | 295 (6.2) | ||
| Male | 65 (94.2) | 4,457 (93.5) | 1.0000 | |
| National medical aid | 4 (5.8) | 152 (3.2) | 1.0000 | |
| Tertiary hospital | 48 (69.6) | 2,856 (59.9) | 0.1399 | |
| Region of clinics | 0.5366 | |||
| Greater Seoula | 47 (68.1) | 3,265 (68.5) | ||
| Others | 22 (31.9) | 1,502 (31.5) | ||
| AIDS | 33 (47.8) | 1,334 (28.0) | 0.0002 | |
| Comorbidities | ||||
| Hypertension | 44 (63.8) | 769 (16.2) | <0.0001 | |
| Dyslipidemia | 56 (81.2) | 2,639 (55.4) | 0.0011 | |
| Diabetes mellitus | 38 (55.1) | 657 (13.8) | <0.0001 | |
| Chronic hepatitis B | 2 (2.9) | 169 (3.5) | 0.6870 | |
| Chronic hepatitis C | 2 (2.9) | 90 (1.9) | 0.6041 | |
| Chronic kidney disease | 3 (4.3) | 80 (1.7) | 0.0485 | |
| Malignancy | 40 (58.0) | 1,587 (33.3) | 0.0018 | |
| Psychiatric disease | 29 (42.0) | 2,848 (59.7) | 0.1059 | |
| Clinical outcomes | 0.0003 | |||
| Hospital mortality | 5 | 57 | ||
| Hospital mortality rate (per 100,000py) | 4,807.7 | 502.6 | ||
| MI events | 15 (39.5) | |||
| Hospital mortality in MI patients | 2 | |||
| Case fatality in MI patients (%) | 13.3 | |||
| Duration of ACS to death (mean, days) | 65.0 | |||
The value denotes the subject number (%) unless otherwise indicated.
aSeoul, Incheon, and Kyeonggi-do.
py, person-year; yrs, years; ACS, acute coronary syndrome; AIDS, acquired immunodeficiency syndrome; MI; myocardial infarction.
Table 4. Factors related with hospital mortality of acute coronary syndrome in patients with optimal adherence to anti-retroviral therapy after 2014 (n = 69).
| Variables | Univatiate | Multiple | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Odds ratio | 95% confidence interval | P-value | Odds ratio | 95% confidence interval | P-value | ||||
| Age at diagnosis | |||||||||
| Under 20 | <0.001 | <0.001 | >999.999 | 0.9634 | |||||
| 20 - 39 | Ref | Ref | Ref | Ref | |||||
| 40 - 59 | 26.825 | 8.301 | 86.687 | 0.9541 | |||||
| Over 60 | 77.369 | 23.159 | 258.473 | 0.9408 | |||||
| Male | 1.130 | 0.409 | 3.122 | 0.8134 | |||||
| National medical aid | 1.869 | 0.672 | 5.195 | 0.2307 | |||||
| Tertiary hospital | 1.529 | 0.913 | 2.562 | 0.1066 | |||||
| Region of clinics | 0.983 | 0.590 | 1.636 | 0.9466 | |||||
| AIDS | 2.359 | 1.465 | 3.799 | 0.0004 | 1.980 | 1.211 | 3.236 | 0.0065 | |
| Comorbidities | |||||||||
| Hypertension | 9.152 | 5.568 | 15.042 | <0.0001 | 4.152 | 2.383 | 7.236 | <0.0001 | |
| Dyslipidemia | 3.474 | 1.895 | 6.368 | <0.0001 | 1.804 | 0.953 | 3.415 | 0.0700 | |
| Diabetes mellitus | 7.669 | 4.739 | 12.411 | <0.0001 | 3.291 | 1.936 | 5.595 | <0.0001 | |
| Viral hepatitis B | 0.812 | 0.197 | 3.343 | 0.7733 | |||||
| Viral hepatitis C | 1.551 | 0.374 | 6.429 | 0.5450 | |||||
| Chronic kidney disease | 8.205 | 3.793 | 17.747 | <0.0001 | 2.553 | 1.123 | 5.807 | 0.0253 | |
| Malignancy | 2.764 | 1.707 | 4.475 | <0.0001 | 1.828 | 1.109 | 3.013 | 0.0181 | |
| Psychiatric disease | 2.049 | 1.265 | 3.313 | 0.0035 | 1.327 | 0.803 | 2.193 | 0.2691 | |
Ref, reference; AIDS, Acquired immune deficiency syndrome.
Discussion
The ACS incidence and mortality rate of ACS in PWH with optimal adherence were confirmed using a large-scale cohort for PWH from data of the Korean universal health insurance system, NHI. PWH with optimal adherence had a higher incidence of ACS than in the HIV-negative population. The incidence of ischemic heart disease in Korea in 2018 was 383.1 per 100,000 people, according to the Korean annual statistics report [13]. According to our findings, incidence of ACS was about 1.3 times higher in PWH with optimal adherence. However, the hospital mortality rate was 7.1% (10/140), whereas the mortality rate after hospitalized myocardial infarction in Korea`s general population reported to the OECD in 2019, was 8.9% [16,17]. The mortality rate of optimal adherent PWH was similar to the general population.
Proposed mechanisms for HIV-related cardiovascular risk are HIV-specific immune dysfunction, upregulation of inflammatory and thrombotic markers, and vascular injury and dysfunction [15]. These factors increase the incidence of ACS as well as the mortality of PWH. We confirmed that conventional risk factors, such as hypertension, diabetes mellitus, and dyslipidemia were still significant in PWH. These results were consistent with previous reports [18]. As the life expectancy of PWH increases, it is expected that more attention may need to be paid to the presence of chronic metabolic diseases.
HIV viremia itself, gut microbiome translocation, cytomegalovirus, and chronic hepatitis C infection could provoke inflammatory response, which have been suggested as a triggering factor of cardiovascular diseases [19]. Diagnosing PWH early and connecting them to treatment offers various benefits. Additionally, it plays a role in mitigating risk associated with ACS. Chronic HCV co-infection is also known to be a risk factor for ACS in PWH, as it was reported to increase 24 - 33% risk of cardiovascular disease [20]. Chronic inflammation is thought to be related with the complications in coinfected patients since inflammatory markers were decreased after HCV eradication [21]. Our findings also indicated a higher prevalence of hepatitis C coinfections in the ACS group, although this difference was not statistically significant, possibly due to the limited sample size of outcome.
With early ART initiation, our study found that the hospital mortality rate was 7.1%, when all ACS were counted and 2.9%, when MI was counted. Hospital mortality rates vary widely when an ACS event occurs in patients with optimal compliance. It was 4.0% in the 1997 - 2006 PWH and 2.0% in the non-HIV population in another study [5]. Another study analyzing myocardial infarction at PWH from 1996 to 2014 found that the 1-year mortality rate after myocardial infarction was 27.0% [8]. However, PWH might get suboptimal treatment than the HIV-negative population, as a previous study detected [5,22,23]. It is unreliable to compare differing study designs. As previous studies were conducted in the early stages of the ART era, this study can provide evidence for cardiovascular outcomes in PWH who start ART early and maintain it with optimal adherence.
PWH who received ART after 2014 are, strictly speaking, people in the universal ART era. We again analyzed mortality rates for MI after 2014. Mortality after MI case was reported in a few cases, so statistical analysis could not be applied. The variables showing a significant difference between the ACS group and the non-ACS group were not much different with the total study population, such as age, AIDS, hypertension, dyslipidemia, diabetes mellitus, chronic kidney disease, and malignancy. The logistic regression model demonstrated a similar trend in the total population, but it showed a significant association between chronic kidney disease which is one of traditional risk factors in cardiovascular events and mortality. This study's findings reveal inconclusive evidence regarding any significant difference in chronic kidney disease across the overall population. It is uncertain whether chronic kidney disease displayed a significant increase in impact post-2014, as the absolute number of cases in the ACS group (7/140 vs. 2/69) was too limited to draw clear conclusions.
Our study is significant in that the account of atherosclerotic cardiovascular complications, which occurs in only a small percentage of patients was confirmed in the optimal adherence group by using a large cohort of PWH using claims data. Based on our findings and existing epidemiological data from the general population in Korea, we discovered that PWH with optimal adherence had no higher hospital mortality than the HIV-negative population.
This study has some limitations. This is a secondary analysis based on claims data. We could not get access to conventional atherosclerotic risk factors like smoking or body mass index. However, it is possible to get more attention for lifestyle modification through the regular HIV clinic visits in PWH with optimal adherence. In one study, women with HIV had better control of their hypertension and diabetes than HIV-negative women [24]. Second, using annual statistics from the Korean government, this study compared mortality among HIV-negative people. Age-matched analysis was not used to obtain the results.
In conclusion, even with ideal adherence, PWH had a higher prevalence of ACS. However, their mortality after ACS was comparable to that of the HIV-negative population in the generalized ART era.
Footnotes
Funding: None.
Conflict of Interest: No conflict of interest.
- Conceptualization: JB.
- Data curation: HJ, JR.
- Formal analysis: HJ, EL, JR, JYL, JB.
- Methodology: EL, JB.
- Resources: JB.
- Writing - original draft: EL.
- Writing - review & editing: HJ, JYL, JB.
SUPPLEMENTARY MATERIAL
Characteristics of patients with human immunosuppression virus who have optimal adherence of antiretroviral therapy
References
- 1.Triant VA. Cardiovascular disease and HIV infection. Curr HIV/AIDS Rep. 2013;10:199–206. doi: 10.1007/s11904-013-0168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsue PY, Waters DD. HIV infection and coronary heart disease: mechanisms and management. Nat Rev Cardiol. 2019;16:745–759. doi: 10.1038/s41569-019-0219-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freiberg MS, Chang CC, Kuller LH, Skanderson M, Lowy E, Kraemer KL, Butt AA, Bidwell Goetz M, Leaf D, Oursler KA, Rimland D, Rodriguez Barradas M, Brown S, Gibert C, McGinnis K, Crothers K, Sico J, Crane H, Warner A, Gottlieb S, Gottdiener J, Tracy RP, Budoff M, Watson C, Armah KA, Doebler D, Bryant K, Justice AC. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614–622. doi: 10.1001/jamainternmed.2013.3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feinstein MJ, Bahiru E, Achenbach C, Longenecker CT, Hsue P, So-Armah K, Freiberg MS, Lloyd-Jones DM. Patterns of cardiovascular mortality for HIV-infected adults in the United States: 1999 to 2013. Am J Cardiol. 2016;117:214–220. doi: 10.1016/j.amjcard.2015.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pearce D, Ani C, Espinosa-Silva Y, Clark R, Fatima K, Rahman M, Diebolt E, Ovbiagele B. Comparison of in-hospital mortality from acute myocardial infarction in HIV sero-positive versus sero-negative individuals. Am J Cardiol. 2012;110:1078–1084. doi: 10.1016/j.amjcard.2012.05.045. [DOI] [PubMed] [Google Scholar]
- 6.Lorgis L, Cottenet J, Molins G, Benzenine E, Zeller M, Aube H, Touzery C, Hamblin J, Gudjoncik A, Cottin Y, Quantin C. Outcomes after acute myocardial infarction in HIV-infected patients: analysis of data from a French nationwide hospital medical information database. Circulation. 2013;127:1767–1774. doi: 10.1161/CIRCULATIONAHA.113.001874. [DOI] [PubMed] [Google Scholar]
- 7.Palella FJ, Jr, Baker RK, Moorman AC, Chmiel JS, Wood KC, Brooks JT, Holmberg SD HIV Outpatient Study Investigators. Mortality in the highly active antiretroviral therapy era: changing causes of death and disease in the HIV outpatient study. J Acquir Immune Defic Syndr. 2006;43:27–34. doi: 10.1097/01.qai.0000233310.90484.16. [DOI] [PubMed] [Google Scholar]
- 8.Feinstein MJ, Nance RM, Delaney JAC, Heckbert SR, Budoff MJ, Drozd DR, Burkholder GA, Willig JH, Mugavero MJ, Mathews WC, Moore RD, Eron JJ, Napravnik S, Hunt PW, Geng E, Hsue P, Peter I, Lober WB, Crothers K, Grunfeld C, Saag MS, Kitahata MM, Lloyd-Jones DM, Crane HM. Mortality following myocardial infarction among HIV-infected persons: the Center for AIDS Research Network Of Integrated Clinical Systems (CNICS) BMC Med. 2019;17:149. doi: 10.1186/s12916-019-1385-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bozzette SA, Ake CF, Tam HK, Chang SW, Louis TA. Cardiovascular and cerebrovascular events in patients treated for human immunodeficiency virus infection. N Engl J Med. 2003;348:702–710. doi: 10.1056/NEJMoa022048. [DOI] [PubMed] [Google Scholar]
- 10.Trickey A, May MT, Vehreschild J, Obel N, Gill MJ, Crane H, Boesecke C, Samji H, Grabar S, Cazanave C, Cavassini M, Shepherd L, d’Arminio Monforte A, Smit C, Saag M, Lampe F, Hernando V, Montero M, Zangerle R, Justice AC, Sterling T, Miro J, Ingle S, Sterne JA Antiretroviral Therapy Cohort Collaboration (ART-CC) Cause-specific mortality in HIV-positive patients who survived ten years after starting antiretroviral therapy. PLoS One. 2016;11:e0160460. doi: 10.1371/journal.pone.0160460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castillo-Mancilla JR, Cavassini M, Schneider MP, Furrer H, Calmy A, Battegay M, Scanferla G, Bernasconi E, Günthard HF, Glass TR Swiss HIV Cohort Study. Association of incomplete adherence to antiretroviral therapy with cardiovascular events and mortality in virologically suppressed persons with HIV: The Swiss HIV cohort study. Open Forum Infect Dis. 2021;8:ofab032. doi: 10.1093/ofid/ofab032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alonso A, Barnes AE, Guest JL, Shah A, Shao IY, Marconi V. HIV infection and incidence of cardiovascular diseases: an analysis of a large healthcare database. J Am Heart Assoc. 2019;8:e012241. doi: 10.1161/JAHA.119.012241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee HH, Cho SMJ, Lee H, Baek J, Bae JH, Chung WJ, Kim HC. Korea heart disease fact sheet 2020: analysis of nationwide data. Korean Circ J. 2021;51:495–503. doi: 10.4070/kcj.2021.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimm H, Yun JE, Lee SH, Jang Y, Jee SH. Validity of the diagnosis of acute myocardial infarction in Korean national medical health insurance claims data: the Korean heart study (1) Korean Circ J. 2012;42:10–15. doi: 10.4070/kcj.2012.42.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim J, Lee E, Park BJ, Bang JH, Lee JY. Adherence to antiretroviral therapy and factors affecting low medication adherence among incident HIV-infected individuals during 2009-2016: A nationwide study. Sci Rep. 2018;8:3133. doi: 10.1038/s41598-018-21081-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi H, Lee JH, Park HK, Lee E, Kim MS, Kim HJ, Park BE, Kim HN, Kim N, Jang SY, Bae MH, Yang DH, Park HS, Cho Y. Impact of the COVID-19 pandemic on patient delay and clinical outcomes for patients with acute myocardial infarction. J Korean Med Sci. 2022;37:e167. doi: 10.3346/jkms.2022.37.e167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.OECD iLibrary. Health at a Glance 2021: OECD indicators. Mortality following acute myocardial infarction (AMI) 2021. [Accessed 20 April 2023]. Available at: https://www.oecd-ilibrary.org/sites/ae3016b9-en/1/3/6/6/index.html?itemId=/content/publication/ae3016b9-en&_csp_=ca413da5d44587bc56446341952c275e&itemIGO=oecd&itemContentType=book.
- 18.Hsue PY, Waters DD. HIV infection and coronary heart disease: mechanisms and management. Nat Rev Cardiol. 2019;16:745–759. doi: 10.1038/s41569-019-0219-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nou E, Lo J, Grinspoon SK. Inflammation, immune activation, and cardiovascular disease in HIV. AIDS. 2016;30:1495–1509. doi: 10.1097/QAD.0000000000001109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osibogun O, Ogunmoroti O, Michos ED, Spatz ES, Olubajo B, Nasir K, Madhivanan P, Maziak W. HIV/HCV coinfection and the risk of cardiovascular disease: A meta-analysis. J Viral Hepat. 2017;24:998–1004. doi: 10.1111/jvh.12725. [DOI] [PubMed] [Google Scholar]
- 21.Zuccalà P, Latronico T, Marocco R, Savinelli S, Vita S, Mengoni F, Tieghi T, Borgo C, Kertusha B, Carraro A, D’Ettorre G, Vullo V, Mastroianni CM, Liuzzi GM, Lichtner M. Longitudinal assessment of multiple immunological and inflammatory parameters during successful DAA therapy in HCV monoinfected and HIV/HCV coinfected subjects. Int J Mol Sci. 2022;23:11936. doi: 10.3390/ijms231911936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parks MM, Secemsky EA, Yeh RW, Shen C, Choi E, Kazi DS, Hsue PY. Longitudinal management and outcomes of acute coronary syndrome in persons living with HIV infection. Eur Heart J Qual Care Clin Outcomes. 2021;7:273–279. doi: 10.1093/ehjqcco/qcaa088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CROI. Parks M. Postdischarge outcomes following acute coronary syndrome in HIV. 2020. [Accessed 10 November 2023]. Available at: https://croiwebcasts.org/console/player/44613?mediaType=audio&.
- 24.Hanna DB, Jung M, Xue X, Anastos K, Cocohoba JM, Cohen MH, Golub ET, Hessol NA, Levine AM, Wilson TE, Young MA, Kaplan RC. Trends in nonlipid cardiovascular disease risk factor management in the women’s interagency HIV study and association with adherence to antiretroviral therapy. AIDS Patient Care STDS. 2016;30:445–454. doi: 10.1089/apc.2016.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics of patients with human immunosuppression virus who have optimal adherence of antiretroviral therapy