Abstract
Treatment of patients with Mayo stage IIIb light chain (AL) amyloidosis is still challenging, and the prognosis remains very poor. Mayo stage IIIb patients were excluded from the pivotal trial leading to the approval of daratumumab in combination with bortezomib-cyclophosphamide-dexamethasone. This retrospective, multicenter study evaluates the addition of daratumumab to first-line therapy in patients with newly diagnosed stage IIIb AL amyloidosis. In total, data from 119 consecutive patients were analyzed, 27 patients received an upfront treatment including daratumumab, 63 a bortezomib-based regimen without daratumumab, eight received therapies other than daratumumab or bortezomib and 21 pretreated patients or deceased prior to treatment were excluded. In the daratumumab group, median overall survival was not reached after a median follow-up time of 14.5 months, while it was significantly worse in the bortezomib- and the otherwise treated group (6.6 and 2.2 months, respectively) (P=0.002). Overall hematologic response rate at 2 and 6 months was better in the daratumumab group compared to the bortezomib group (59% vs. 37%, P=0.12, 67% vs. 41%, P=0.04, respectively). Landmark survival analyses revealed a significantly improved overall survival in patients with partial hematologic response or better, compared to non-responders. Cardiac response at 6 months was 46%, 21%, 0% in the daratumumab-, bortezomib- and otherwise treated groups, respectively (P=0.04). A landmark survival analysis revealed markedly improved overall survival in patients with cardiac very good partial response vs. cardiac non-responders (P=0.002). This study demonstrates for the first time the superiority of an upfront treatment with daratumumab over standard-of-care in stage IIIb AL amyloidosis.
Introduction
Systemic light chain (AL) amyloidosis is a rare acquired protein misfolding disorder with an incidence of about 5-13 cases per million person-years.1 It is characterized by extracellular deposition of misfolded amyloidogenic immuno-globulin light chain fibrils secreted most often from clonal plasma cells in the bone marrow.2 With the exception of the central nervous system, all organs can be affected, most commonly the heart and kidneys.2,3
The outcome of patients with AL amyloidosis is strongly associated with the severity of organ involvement, especially the heart. Cardiac Mayo classifications from 2004 and 2012 were established to assess the severity of the disease.4-6 In particular, patients with Mayo stage IIIb, who are often excluded from clinical trials, have the worst prognosis and thus represent the group of patients for whom new, efficient treatment strategies need to be developed.6-8
Current treatment protocols for patients with Mayo stage IIIb amyloidosis are based on anti-plasma cell drugs.9,10 Bortezomib, a proteasome inhibitor, has been the most frequently administered drug in first-line treatment since 2010.8 In the case of existing contraindications, other treatments, such as melphalan and dexamethasone, immunomodulatory drugs or bendamustine, are used.8,11
In 2021, daratumumab, an IgGκ monoclonal anti-CD38-antibody, was approved for the treatment of patients with AL amyloidosis due to the results from a randomized phase III clinical trial (ANDROMEDA).12 However, in this trial, patients with Mayo stage IIIb were excluded. In contrast to other established therapies, the mechanism of action of daratumumab is rather specific, as the antibody is directed against CD38, which is not present on cardiomyocytes. It is, therefore, unlikely to cause additive cardiotoxicity, which may be a factor favoring the use of daratumumab-containing therapies in advanced cardiac disease. In fact, a post-hoc analysis from the ANDROMEDA study showed that patients with cardiac involvement (up to Mayo stage IIIa) were the ones who benefited most from the addition of daratumumab to standard chemotherapy.12,13 In another retrospective study,14 which included patients with relapsed AL amyloidosis, the median overall survival (OS) in patients with N-terminal prohormone of brain natriuretic peptide (NTproBNP) levels above 8,500 pg/mL was 6 months when treated with daratumumab and dexamethasone (34 patients) and 11 months when treated with daratumumab, bortezomib and dexamethasone (25 patients).14 NTproBNP levels above 8,500 pg/mL are characteristic of Mayo stage IIIb. Similar data were recently published in a report on the use of daratumumab in 19 Mayo stage IIIb patients, which showed a promising efficacy and safety profile with a 12-month OS of 67.5%.15 In another retrospective study including 22 patients treated with daratumumabbased regimens, promising hematologic response rates (64% very good partial response [VGPR] or better at 3 months) but no survival data were reported.16
Overall, these findings suggest that daratumumab-containing regimens may also be an effective and tolerable treatment option for patients with Mayo stage IIIb in the first-line setting, potentially representing a step forward in the treatment of this hitherto underserved group of patients. The present multicenter, retrospective study is the first to investigate the efficacy of the addition of daratumumab to first-line therapy in patients with AL amyloidosis and Mayo stage IIIb compared to bortezomib-containing regimens or other less commonly used therapies.
Methods
This retrospective study enrolled 119 consecutive patients with histologically diagnosed AL amyloidosis and Mayo stage IIIb, who presented between 2016 and 2022 at four different sites in Germany and Austria (Amyloidosis Center at the University Hospital of Heidelberg, University Hospital of Essen, University Hospital of Vienna, and University Hospital of Würzburg). The study was approved by the institutional ethics committees at each site (Heidelberg S-123/2006, Essen 21-10467-BO, Vienna 1184/2022, Würzburg 20220913 01) and performed according to the Helsinki Declaration of 1975, as revised in 2013.
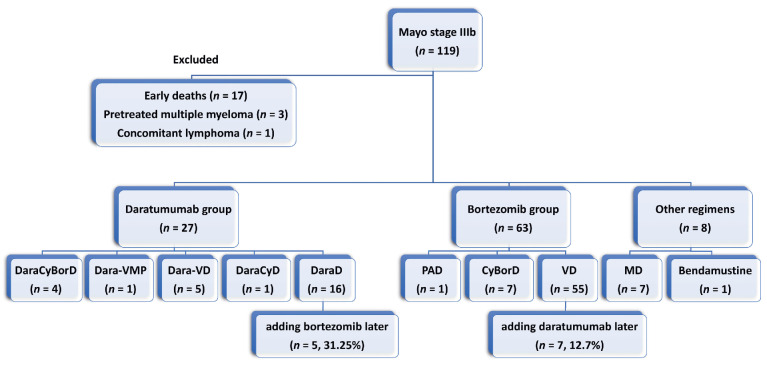
To investigate the role of upfront daratumumab treatment of patients with Mayo stage IIIb, the following treatment groups were compared: (i) patients who received daratumumab with or without bortezomib from the beginning as part of the induction therapy (n=27). Depending on therapy response and toxicity, additional therapy components could be added sequentially during the course. This group was referred to as the daratumumab group; (ii) patients who received bortezomib without daratumumab from the beginning (n=63). Again, in the case of lack of response to therapy, daratumumab could be added during the course. This group was referred to as the bortezomib group; and (iii) patients for whom therapies other than bortezomib or daratumumab were selected (n=8) (Figure 1). Treatment decisions in this retrospective study were left to local physicians' judgement, without any cross-center coordination. Organ involvement was defined according to the consensus criteria of the International Society of Amyloidosis.17 Mayo stage IIIb was defined as NTproBNP level >8,500 pg/mL and cardiac troponin T ≥0.035 ng/mL or high-sensitivity troponin T ≥50 ng/L.4,18 Renal stages were determined according to the 2014 renal classification.19
OS was calculated from the date of treatment initiation to death or loss of follow-up or to the date of heart transplantation. Hematologic responses at 2 and 6 months were assessed as recommended by the International Society of Amyloidosis.20,21 Patients with a small difference between involved and non-involved light chains (dFLC), i.e., <50 mg/L, were excluded. Cardiac response at 6 months was assessed as proposed by Palladini et al. and graded by Muchtar et al.20,22,23 Kaplan-Meier landmark survival analyses of hematologic and cardiac responses were performed.
In the case of absence of data, e.g., treatment or organ responses at certain time points, these data were not assessed in the statistical analyses. All treated patients, including those who died, were included in statistical analyses, as indicated.
Descriptive statistics were used to summarize the patients’ characteristics. Surrogate continuous variables in the three treatment groups were compared using the Kruskal-Wallis test. Hematologic and cardiac response rates in both the daratumumab group and the bortezomib group were compared using the Fisher exact test. Corresponding odds ratios (OR), 95% confidence intervals (95% CI), and two-sided P values were reported. Time-to-event data variables and the median OS were assessed using the Kaplan-Meier method. The median follow-up time was calculated based on the median time to censoring (reversed Kaplan-Meier). Univariate Cox regression analysis predicting possible prognostic factors in the whole Mayo stage IIIb cohort was performed. A forest plot was constructed and the hazard ratios of various variables with their 95% CI were calculated to determine differences between the daratumumab and the bortezomib treatment groups. The statistical software applied to calculate the statistical significance was GraphPad PRISM.
Figure 1.
Schematic representation of all treatment groups and regimens. Bor: bortezomib; Cy: cyclophosphamide; Dara: daratumumab; D: dexamethasone; M: melphalan; VMP: bortezomib, melphalan, prednisone; PAD: bortezomib, doxorubicin, dexamethasone; V: bortezomib.
Results
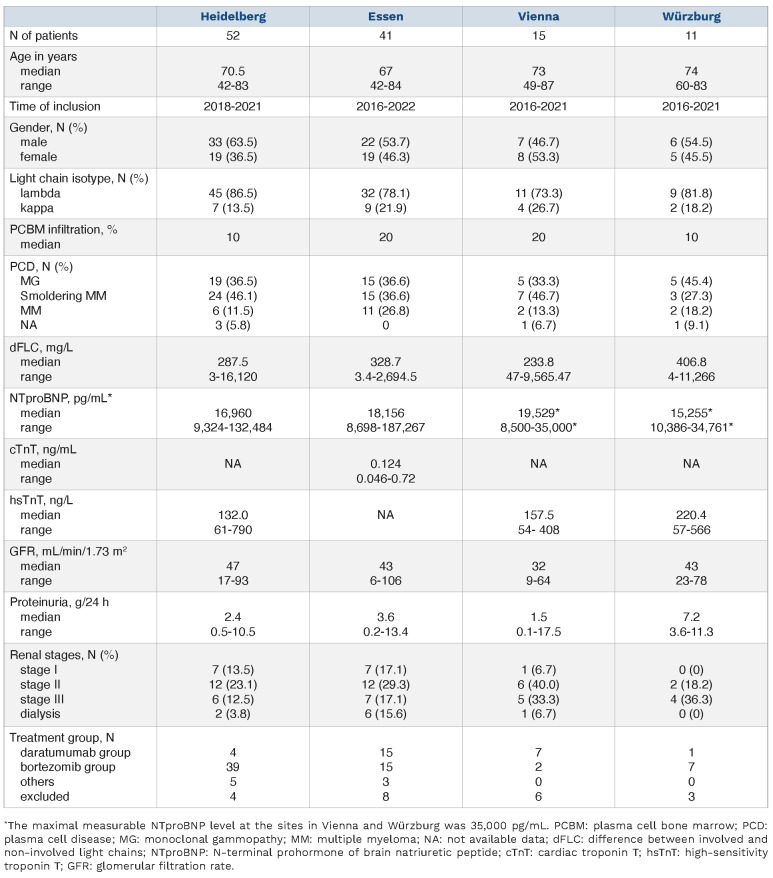
Table 1 shows the baseline characteristics and treatment groups of the included patients broken down by treatment center. While the majority of patients in Heidelberg and Würzburg were treated in the bortezomib group, the larger part of patients in Essen and Vienna were treated in the daratumumab group (Table 1).
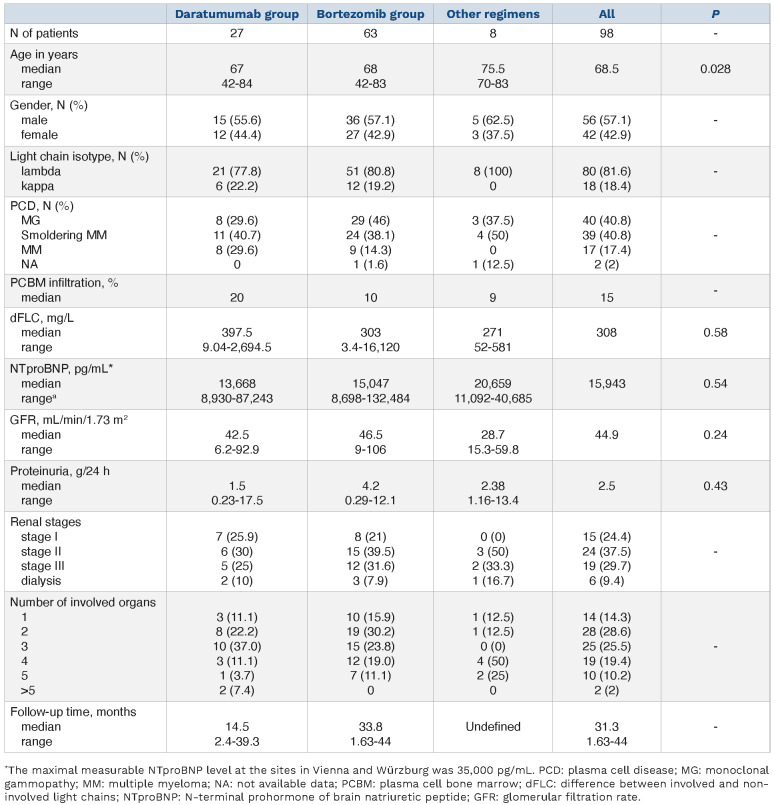
Table 2 shows the baseline characteristics of treated patients broken down by treatment group. There were no significant differences in baseline characteristics between the treatment groups except for the age of patients treated with other therapies; these patients were significantly older than the ones treated in the bortezomib group (75.7 vs. 68 years; P=0.02). Seventeen patients who did not receive therapy because they had previously died or refused therapy are not included in this table, in which therapies are compared. The median NTproBNP in this group was 28,912 pg/mL and significantly (P=0.01) increased compared to the patients who received therapy.
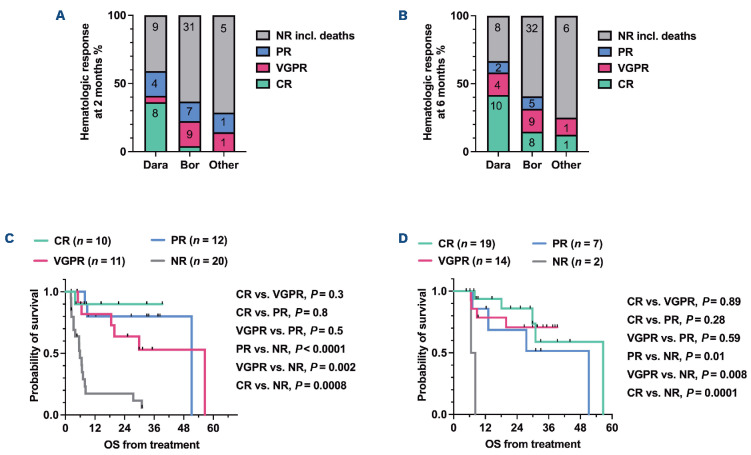
In the group of patients treated from the beginning with daratumumab and dexamethasone (n=16, 59.2% of the whole daratumumab group), five patients (31.25%) received bortezomib additionally later during the course of treatment, while in the group of patients who were treated with bortezomib and dexamethasone from the beginning (n=55, 87.3% of the whole bortezomib group), seven patients (12.7%) later received additional daratumumab (Figure 1). The response rates to first-line regimens and the second-line therapies are listed in Online Supplementary Table S1. Comparison of OS rates between different treatment groups after a median follow-up time of 31.3 months revealed significant differences favoring daratumumab as first-line treatment in Mayo stage IIIb patients (Figure 2). The 6-month OS in the daratumumab group, bortezomib group, and the group treated with other regimens was 70%, 51% and 25%, respectively (log-rank test, P=0.002). The median OS was 6.6 months in the bortezomib group, 2.2 months in the group treated with other regimens, but was not reached in the daratumumab group. Analyzing the OS between single groups also showed significant differences (Figure 2). We also compared hematologic treatment responses at defined timepoints in all evaluable patients. For this purpose, we selected an early timepoint after 2 months and a later one after 6 months. In the daratumumab group, at 2 months the overall response rate (ORR) was 59%, the complete hematologic response (CR) rate was 36.3%, the VGPR rate was 4.5%, and 18.1% of the patients had achieved a partial response (PR). In contrast to that, the ORR was reduced to 36.7% in the bortezomib group. In this group, 4% achieved a CR, 18.3% a VGPR and 14.2% a PR. In the group of patients treated with other regimens, the ORR was 28.5% with none having achieved a CR, 14.2% a VGPR and 14.2% a PR (Figure 3A). Comparing ORR at 2 months revealed non-significant differences between the daratumumab- and bortezomib-treated groups (OR=2.48; 95% CI: 0.848-7.036; P=0.12), whereas comparing both groups with respect to CR did show a statistically significant difference (OR=13.43; 95% CI: 2.553-65.49; P=0.0009). The proportion of patients who died within the first 2 months after initiation of therapy was 22% in the daratumumab group, 27% in the bortezomib group and 25% in the group treated with other regimens.
Table 1.
Basic clinical characteristics of the patients in each cohort at the four sites.
At 6 months after initiating treatment, in the daratumumab group, the ORR was 66.7%; 41.7% had achieved a CR, 16.7% a VGPR and 8.3% a PR. In contrast to that, the ORR was only 40.7% in the bortezomib group. In this group, 14.8% had achieved a CR, 16.7% a VGPR and 9.3% a PR. In the group of patients treated with other regimens, the ORR was 25% with 12.5% achieving a CR, 12.5% a VGPR and none a PR (Figure 3B). Comparing the ORR at 6 months revealed a significant difference between the daratumumab- and bortezomib-treated groups (OR=2.9; 95% CI: 1.076-8.322; P=0.04). Likewise, the difference in CR rate between the two groups was also statistically significant (OR=4.107; 95% CI: 1.36-11.17; P=0.01). The proportion of patients who died within the first 6 months after initiation of therapy was 29.6% in the daratumumab group, 47.6% in the bortezomib group and 75% in the group treated with other regimens.
Table 2.
Basic clinical characteristics in each treatment group.
To evaluate the effect of early hematologic responses on OS we performed landmark survival analyses for survivors starting from 2 and 6 months after treatment initiation (Figure 3C, D). The 12-month OS rates in patients who achieved a CR, VGPR or PR and survived 2 months after treatment initiation were 90%, 82% and 80%, respectively, while it was reduced to 17.4% in hematologic non-responders. Patients who achieved a CR, VGPR or PR and survived 6 months after treatment initiation had a 12-month OS rate of 94%, 79% and 86%, respectively, while all the non-responders who were alive at 6 months after treatment initiation died before completing the first year of treatment. Log-rank tests between the groups with a CR, VGPR or PR did not show statistically significant survival differences, whereas non-responders had a significantly worse survival rate compared to patients with CR, VGPR or PR in both landmark analyses (Figure 3C, 3D).
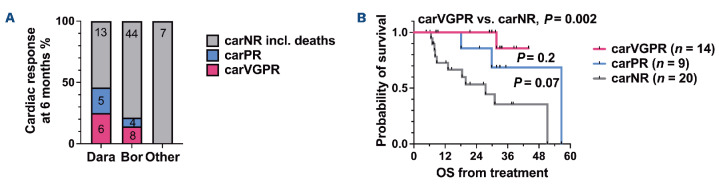
Cardiac response at 6 months after treatment initiation was assessed according to treatment group in all patients with evaluable data. None of the patients achieved a cardiac CR. The cardiac ORR was 45.8% in the daratumumab group, compared to 21.4% in the bortezomib group (OR=3.103; 95% CI: 1.171-8.299; P=0.03) (Figure 4A). Patients in the daratumumab group were more likely to have a cardiac VGPR than those in the bortezomib group (25% vs. 14.3%), respectively (OR=2.0; 95% CI: 0.558-5.984; P=0.3). Patients treated with other regimens did not reach a cardiac response after 6 months (Figure 4A). The 12-month OS was 100% in patients who achieved a cardiac VPGR or cardiac PR, compared to 73% in cardiac non-responders (Figure 4B). The log-rank test between patients with a cardiac VGPR and cardiac PR did not show any significant survival differences, whereas patients with who did not have a cardiac response had a significantly worse survival compared to patients with a cardiac VGPR (P=0.002) (Figure 4B).
Figure 2.
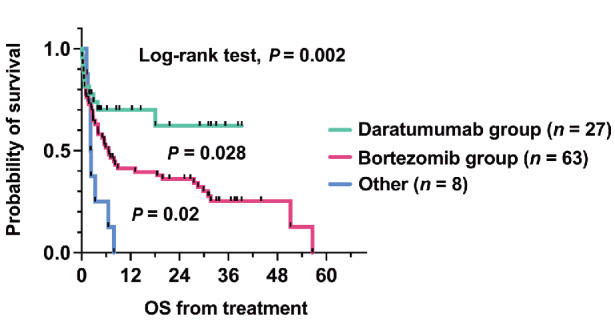
Kaplan-Meier survival analysis showing survival rates according to first-line treatment. OS: overall survival.
Figure 3.
Hematologic response rates at 2 and 6 months and Kaplan-Meier landmark analyses of overall survival regarding hematologic response at 2 and 6 months. (A) Hematologic response rates at 2 months. In 20 patients, response data were not available or dFLC was lower than 50 mg/L (5 in the daratumumab group, 14 in the bortezomib group and 1 in the group treated with other regimens). (B) Hematologic response rates at 6 months. In 12 patients, response data were not available or dFLC was lower than 50 mg/L (3 in the daratumumab group and 9 in the bortezomib group). (C) Overall survival according to hematologic response at 2 months. (D) Overall survival according to hematologic response at 6 months. Dara: group treated with daratumumab; Bor: group treated with bortezomib; Other: group treated with other regimens; NR: no response; PR: partial response; VGPR: very good partial response; CR: complete response; OS: overall survival.
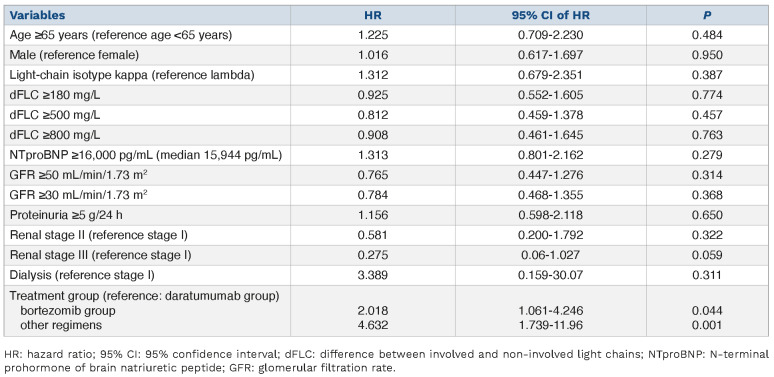
In an univariate Cox regression analysis, no risk factors that could predict OS in the whole Mayo IIIb cohort were identified (Table 3). Of note, surrogate parameters such as dFLC ≥500 mg/L or NTproBNP ≥16,000 pg/mL (median 15,944 pg/mL) were not associated with an increased risk of death. Other variables with their hazard ratios are shown in Table 3. Notably, higher hazard ratios were demonstrated in the bortezomib-treated group than in the daratumumab-treated group.
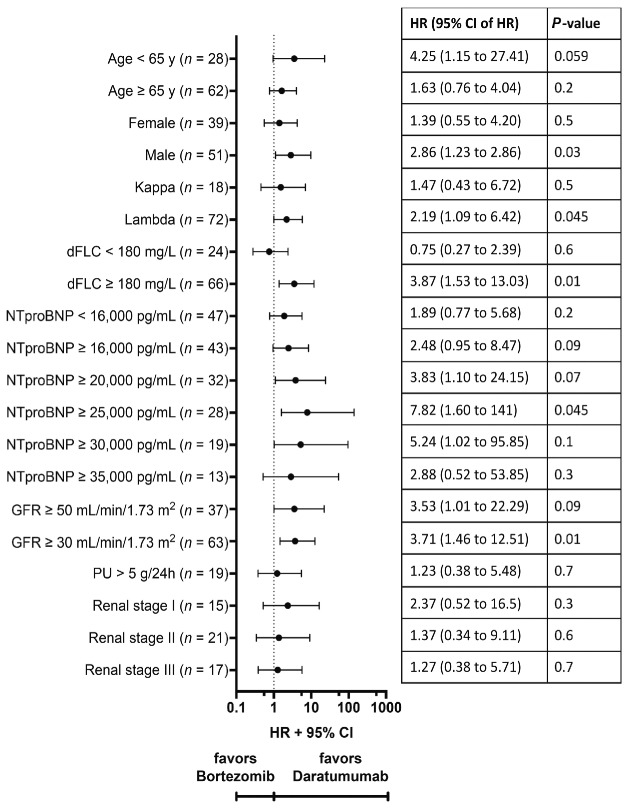
To investigate whether any baseline, clonal or organ variables might have affected OS in a given treatment group, we performed another Cox regression analysis (Figure 5). In particular, patients with elevated clonal or organ parameters (dFLC ≥180 mg/L, NTproBNP ≥16,000 pg/mL and glomerular filtration rate ≥30 mL/min/1.73 m2) benefited markedly from daratumumab in the first-line treatment. The benefit of adding daratumumab to first-line therapy appeared to increase relatively with increasing NTproBNP up to 25,000 pg/mL. However, this advantage appeared to decrease with further increases in NTproBNP (Figure 5).
Figure 4.
Cardiac response at 6 months with landmark survival analysis. (A) Cardiac response in patients with evaluable response data. In 11 patients, response data were not available (3 in the daratumumab group, 7 in the bortezomib group and 1 in the group treated with other regimens). (B) Kaplan-Meier landmark analysis of overall survival regarding cardiac response at 6 months. Dara: group treated with daratumumab; Bor: group treated with bortezomib; Other: group treated with other regimens; carNR: no cardiac response; carPR: partial cardiac response; carVGPR: very good partial cardiac response; OS: overall survival.
Table 3.
Univariate Cox-regression analysis predicting prognostic factors in the whole cohort.
Discussion
To our knowledge, this is the first comparative, multicenter, retrospective study analyzing treatment response and OS in Mayo stage IIIb patients after first-line treatment including daratumumab, compared to bortezomib or other regimens. Patients in the daratumumab group had a significantly better outcome (median OS was not reached after the 14.5 months median follow-up time in the daratumumab group) than patients treated in the bortezomib group (median OS was 6.6 months) or with other regimens (median OS was 2.2 months) (Figure 2). While the 6- and 12-month OS rates remained the same at 70% in the daratumumab group, OS decreased from 51% at 6 months to 41% at 12 months in the bortezomib group (Figure 2). None of the patients who were treated with other regimens survived 1 year after treatment initiation. In comparison to previous studies, the median OS rate for Mayo stage IIIb patients enrolled in the EMN23 study between 2004 and 2010 was 5 months.8 In patients enrolled between 2011 and 2018, when bortezomib-containing regimens were being increasingly used, the median OS was 4.5 months and did not improve in contrast to that of patients with Mayo stages II and IIIa.8 In the ALchemy study, a single-center, prospective, observational study, the median OS for 179 Mayo IIIb patients enrolled between 2009 and 2015 was 6 months.24 Of note, in these studies daratumumab was not included in first-line treatments. In the randomized ANDROMEDA trial, which included patients with Mayo stages I, II and IIIa, no significant survival differences were found between patients treated with CyBorD (cyclophosphamide, bortezomib and dexamethasone) and CyBorD plus daratumumab after a median follow-up time of 11.4 months (see supplementary data of the ANDROMEDA clinical trial).12 To the best of our knowledge, our comparative study shows for the first time an OS benefit from the use of daratumumab as an upfront treatment over bortezomib in the therapy of AL amyloidosis patients with Mayo stage IIIb.
Figure 5.
Forest plot for subgroup analysis of overall survival in patients with AL amyloidosis and Mayo stage IIIb. Data are derived from Cox regression analysis without covariates. HR: hazard ratio; CI: confidence interval; dFLC: difference between involved and non-involved light chains; NTproBNP: N-terminal prohormone of brain natriuretic peptide; GFR: glomerular filtration rate; PU: proteinuria.
In our patients treated in the daratumumab group, bortezomib was added from the beginning, later in the course, or not at all (Figure 1). The addition of bortezomib did not follow a fixed protocol but was based on the assessment/decision of the treating physician. The experience of the physician, the clinical condition of the patient and the therapy response achieved each played a role. Likewise, the dosage of bortezomib, both at the time of addition or as part of the primary therapy, was not fixed. Generally, the initial dosage of bortezomib was 0.7 mg/m2 or 1 mg/m2 and was eventually increased during the course of therapy, depending on the response to therapy and tolerability. Preliminary evaluation of the ongoing EMN22-trial (daratumumab monotherapy, addition of dexamethasone and bortezomib from the fourth cycle in the case of insufficient response) revealed a median OS of 9.4 months.25 There is a recent short report of a median OS of more than 12 months in Mayo IIIb patients who were treated with upfront Dara-VCD (daratumumab, bortezomib, cyclophosphamide and dexamethasone).15
Preliminary hematologic response data from the ongoing EMN22 trial documented a 6-month ORR of 72%.25 Our patients in the daratumumab group showed comparable results with a 6-month ORR of 67%. Upfront treatment consisting of daratumumab in combination with bortezomib, cyclophosphamide and dexamethasone in 19 patients with Mayo stage IIIb showed good efficacy (VGPR or better, 86.7%) and safety, which is in line with the results of our study.15
In the present study, the 6-month cardiac ORR in 24 evaluable (including 8 deceased) patients in the daratumumab group was 46% Preliminary evaluation of cardiac response at 6 months in the ongoing EMN22 trial revealed a cardiac response rate of 27.6%.25 In a recently published study, in which Mayo IIIb patients were treated with up-front Dara-VCD, a cardiac response was found in 80% of ten evaluable patients; however, deceased patients and patients without evaluable data were excluded from this analysis. Furthermore, differences in the baseline characteristics may have led to a relevant bias. Remarkably, median NTproBNP in the upfront Dara-VCD study was 10,702 pg/mL, compared to 15,468 pg/mL in the EMN22 trial and 13,668 pg/mL in our study. Therefore, also due to the small number of cases in any of the studies, a clear statement on the efficacy of different treatment-schemes (upfront Dara-VCD vs. upfront daratumumab [+dexamethasone] and sequential addition of bortezomib) cannot be made at the moment.
We also determined the hematologic response after 2 and 6 months of therapy and performed landmark survival analyses. We found a significant OS advantage for patients who survived 2 and 6 months and achieved at least a PR compared to patients who had no response (Figure 3C, D). Surprisingly, in these landmark analyses, no significant differences in survival proportion rates were found between patients who achieved CR, VGPR or PR at 2 or 6 months. Our 2-month hematologic response data are in line with the analyses performed in the ALchemy study.24 Here, early hematologic response after 30 days of therapy was shown to predict 12-month OS in patients who were still alive after 6 months. In concordance with our data, no significant differences in the depth of hematologic response (CR, VGPR or PR) were found.24
The impact of early treatment response at 1 and 3 months on survival was investigated in 249 consecutive patients newly diagnosed between 2004 and 2018 at the Amyloidosis Research and Treatment Center in Pavia.26 In this series, patients with a CR or VGPR at 1 month and 3 months showed a significant survival advantage over patients with a PR or no response.26 Furthermore, a landmark analysis of 663 patients with Mayo stage IIIb who survived the first 3 months (60%) showed that the median OS clearly depended on the depth of the response achieved; the median OS in patients with a CR was 47 months, whereas it was 36 months in those who achieved a VGPR, 19 months in those who had a PR and 3 months in non-responders.8 Both, the EMN23 study8 and the study at Pavia26 are from the pre-daratumumab era and early mortality was much higher than in the present study. An explanation of why the difference in depth of hematologic response (CR/VGPR/PR) in our dataset did not allow such a clear prediction of survival may be the sequential strategy in our therapeutic approach, in many cases consisting only of daratumumab and dexamethasone at the beginning with a gradual increase in intensity by adding bortezomib, in order to lessen toxicity, so that the 2-month response may not necessarily have served as a biological hematologic response parameter for survival. To shed some light, in a landmark subanalysis of survival dependent on hematologic response at 2 months, we examined only those patients who were not treated with daratumumab at baseline or later (Online Supplementary Figure S1). Although a clear conclusion cannot be drawn due to the small number of cases, when excluding patients treated with daratumumab, the data look similar to those previously published from the pre-daratumumab era. In our view, further studies should be performed to shed more light on this interesting point. Our data lead us to suggest that, with the inclusion of daratumumab as a first-line treatment and sequential addition of further components such as bortezomib, it may become necessary to define modified response criteria, possibly combining hematologic and organ response parameters.26
We found no relevant clonal or organ predictive variables that could influence OS. Only treatment with daratumumab had a significantly positive impact on OS compared to bortezomib and other regimens (Table 3). To illustrate differential influences of variables in different treatment groups we constructed a forest plot (Figure 5). Adjusted cutoff values of NTproBNP revealed an increased advantage up to about 25,000 pg/mL. At even higher NTproBNP levels up to 35,000 pg/mL, this advantage seemed to diminish slightly. These findings indicate that there may be a level at the top at which even the addition of daratumumab does not give advantages anymore, because in these patients the heart disease may already be so severe that even a hematologic response cannot turn the tide. Advanced kidney disease, i.e., renal stages II and III and especially proteinuria >5 g/24 h, reduced the benefit of adding daratumumab, confirming data from Kimmich et al. who showed that the antibody is excreted in the urine in the context of proteinuria and thus loses efficacy.14 Patients with a high dFLC (≥180 mg/L) benefit particularly from the addition of daratumumab. This is probably the reason that in our cohort even a dFLC ≥500 mg/L no longer predicted a poor outcome in univariate Cox regression analysis, as described by Basset et al.26
While there are clear therapy recommendations for patients with Mayo stages I-IIIa, supported by the findings of the ANDROMEDA study12 and the approval of daratumumab in combination with VCD, the situation is less clear for Mayo IIIb patients. Among the patients in our series with multiple myeloma, a relatively higher proportion received treatment with daratumumab (8 out of 17, 47%) due to its approval in combination with bortezomib and dexamethasone for myeloma. Conversely, in patients with monoclonal gammopathy, the proportion in the daratumumab group was lower (8 out of 40, 20%) (Table 2). Consequently, the daratumumab group had a higher representation of patients with advanced plasma cell disease. Despite this bias that may have put the daratumumab group at a disadvantage, patients treated with daratumumab demonstrated better response rates and survival, emphasizing the significance of the data.
Our study has several limitations, most notably the retrospective design and the unavailability of a few clinical parameters or response data in some patients. A further selection bias may limit the information value of our study since not all Mayo IIIb patients may be referred to our treatment centers. However, the baseline characteristics in our study (Table 1) mostly correspond to the baseline characteristics in previous studies including Mayo IIIb patients.8,15,24,26 Another weakness of this study is that therapy-associated side effects were not systematically recorded. However, it can be said that in no case did therapy with daratumumab have to be reduced or discontinued due to side effects and no infection-related deaths occurred.
In conclusion, our study demonstrates for the first time the superiority of an upfront treatment with daratumumab over the current standard-of-care with bortezomib in Mayo stage IIIb patients. The better survival rates in the group treated with daratumumab suggests its efficacy and safety profile in this vulnerable patient population. Further randomized trials should be conducted to confirm our data and to define the best sequence of daratumumab combination therapies.
Supplementary Material
Funding Statement
Funding: This study was supported by a grant from the Deutsche Forschungsgemeinschaft to AC (grant number CA2420/2-1). We acknowledge support from the Open Access Publication Fund of the University of Duisburg-Essen.
References
- 1.Kyle RA, Linos A, Beard CM, et al. Incidence and natural history of primary systemic amyloidosis in Olmsted County, Minnesota, 1950 through 1989. Blood. 1992;79(7):1817-1822. [PubMed] [Google Scholar]
- 2.Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med. 1997;337(13):898-909. [DOI] [PubMed] [Google Scholar]
- 3.Merlini G, Dispenzieri A, Sanchorawala V, et al. Systemic immunoglobulin light chain amyloidosis. Nat Rev Dis Primers. 2018;4(1):38. [DOI] [PubMed] [Google Scholar]
- 4.Dispenzieri A, Gertz MA, Kyle RA, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22(18):3751-3757. [DOI] [PubMed] [Google Scholar]
- 5.Kumar S, Dispenzieri A, Lacy MQ, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol. 2012;30(9):989-995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wechalekar AD, Schonland SO, Kastritis E, et al. A European collaborative study of treatment outcomes in 346 patients with cardiac stage III AL amyloidosis. Blood. 2013;121(17):3420-3427. [DOI] [PubMed] [Google Scholar]
- 7.Oubari S, Naser E, Papathanasiou M, et al. Impact of time to diagnosis on Mayo stages, treatment outcome, and survival in patients with AL amyloidosis and cardiac involvement. Eur J Haematol. 2021;107(4):449-457. [DOI] [PubMed] [Google Scholar]
- 8.Palladini G, Schonland S, Merlini G, et al. The management of light chain (AL) amyloidosis in Europe: clinical characteristics, treatment patterns, and efficacy outcomes between 2004 and 2018. Blood Cancer J. 2023;13(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kyle RA, Bayrd ED. "Primary" systemic amyloidosis and myeloma. Discussion of relationship and review of 81 cases. Arch Intern Med. 1961;107:344-353. [DOI] [PubMed] [Google Scholar]
- 10.Kyle RA, Greipp PR. Primary systemic amyloidosis: comparison of melphalan and prednisone versus placebo. Blood. 1978;52(4):818-827. [PubMed] [Google Scholar]
- 11.Palladini G, Milani P, Merlini G. Management of AL amyloidosis in 2020. Hematol Am Soc Hematol Educ Program. 2020;2020(1):363-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kastritis E, Palladini G, Minnema MC, et al. Daratumumab-based treatment for immunoglobulin light-chain amyloidosis. N Engl J Med. 2021;385(1):46-58. [DOI] [PubMed] [Google Scholar]
- 13.Minnema MC, Dispenzieri A, Merlini G, et al. Outcomes by cardiac stage in patients with newly diagnosed AL amyloidosis: phase 3 ANDROMEDA trial. JACC CardioOncol. 2022;4(4):474-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimmich CR, Terzer T, Benner A, et al. Daratumumab for systemic AL amyloidosis: prognostic factors and adverse outcome with nephrotic-range albuminuria. Blood. 2020;135(18):1517-1530. [DOI] [PubMed] [Google Scholar]
- 15.Chakraborty R, Rosenbaum C, Kaur G, et al. First report of outcomes in patients with stage IIIb AL amyloidosis treated with Dara-VCD front-line therapy. Br J Haematol. 2023;201(5):913-916. [DOI] [PubMed] [Google Scholar]
- 16.Theodorakakou F, Briasoulis A, Fotiou D, et al. Outcomes for patients with systemic light chain amyloidosis and Mayo stage 3B disease. Hematol Oncol. 2023. Mar 27. doi: 10.1002/hon.3135. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Gertz MA, Comenzo R, Falk RH, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004. Am J Hematol. 2005;79(4):319-328. [DOI] [PubMed] [Google Scholar]
- 18.Dispenzieri A, Gertz MA, Kumar SK, et al. High sensitivity cardiac troponin T in patients with immunoglobulin light chain amyloidosis. Heart. 2014;100(5):383-388. [DOI] [PubMed] [Google Scholar]
- 19.Palladini G, Hegenbart U, Milani P, et al. A staging system for renal outcome and early markers of renal response to chemotherapy in AL amyloidosis. Blood. 2014;124(15):2325-2332. [DOI] [PubMed] [Google Scholar]
- 20.Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30(36):4541-4549. [DOI] [PubMed] [Google Scholar]
- 21.Palladini G, Schonland SO, Sanchorawala V, et al. Clarification on the definition of complete haematologic response in light-chain (AL) amyloidosis. Amyloid. 2021;28(1):1-2. [DOI] [PubMed] [Google Scholar]
- 22.Palladini G, Barassi A, Klersy C, et al. The combination of high-sensitivity cardiac troponin T (hs-cTnT) at presentation and changes in N-terminal natriuretic peptide type B (NT-proBNP) after chemotherapy best predicts survival in AL amyloidosis. Blood. 2010;116(18):3426-3430. [DOI] [PubMed] [Google Scholar]
- 23.Muchtar E, Dispenzieri A, Wisniowski B, et al. Graded cardiac response criteria for patients with systemic light chain amyloidosis. J Clin Oncol. 2022;41(7):1393-1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Manwani R, Foard D, Mahmood S, et al. Rapid hematologic responses improve outcomes in patients with very advanced (stage IIIb) cardiac immunoglobulin light chain amyloidosis. Haematologica. 2018;103(4):e165-e168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kastritis E, Minnema MC, Dimopoulos MA, et al. Efficacy and safety of daratumumab monotherapy in newly diagnosed patients with stage 3B light chain amyloidosis: a phase 2 study by the European Myeloma Network. Blood. 2022;140(Suppl 1):1841-1843. [Google Scholar]
- 26.Basset M, Milani P, Foli A, et al. Early cardiac response is possible in stage IIIb cardiac AL amyloidosis and is associated with prolonged survival. Blood. 2022;140(18):1964-1971. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.