Abstract
A 67-year-old woman with a history of poorly controlled asthma was admitted to our hospital with a persistent cough and abnormal chest radiographic findings. Her diagnosis was allergic bronchopulmonary aspergillosis (ABPA). Following treatment with mepolizumab, her symptoms and imaging findings improved initially. However, after approximately 2 years, the patient experienced a recurrent cough with elevated non-specific immunoglobulin E levels and worsening chest imaging findings, thereby changing her diagnosis to recurrent ABPA. Mepolizumab was substituted with dupilumab, and her subjective symptoms and imaging findings improved. Our findings suggest that dupilumab may be effective in ABPA cases following the failure of another antibody therapy.
Keywords: Asthma, Allergic bronchopulmonary aspergillosis, Mepolizumab, Dupilumab, Prednisolone
Highlights
-
•
Humanized monoclonal antibodies are effective in patients with ABPA and may serve as a viable substitute for prednisolone.
-
•
Humanized monoclonal antibodies exhibit initial efficacy against ABPA; however, their effectiveness may attenuate over time.
-
•
Dupilumab may be effective in ABPA cases following the failure of another antibody therapy.
Abbreviations
- ABPA
allergic bronchopulmonary aspergillosis
- IgE
immunoglobulin E
- IL
interleukin
- TSLP
thymic stromal lymphopoietin
- CT
computed tomography
- ACT
Asthma Control Test
- NTM
nontuberculous mycobacteria
- ETosis
eosinophil extracellular trap death
- ILC2
group 2 innate lymphoid cells
1. Introduction
Allergic bronchopulmonary aspergillosis (ABPA) is an immunological pulmonary disease resulting from a hypersensitivity reaction to Aspergillus species and is characterized by uncontrolled asthma, recurrent pulmonary infiltrations, and bronchiectasis [1]. The standard treatment for ABPA is the systemic administration of corticosteroids. However, the broad range of side effects associated with the prolonged administration of corticosteroids renders their utilization problematic in certain ABPA cases, particularly those complicated by concurrent bacterial infection(s) [2]. As the search for an alternative therapeutic approach to corticosteroids continues, it is anticipated that humanized monoclonal antibodies, including anti-immunoglobulin E (IgE) antibody (omalizumab), anti-interleukin-5 (IL-5) antibody (mepolizumab and reslizumab), anti-IL-5 receptor antibody (benralizumab), anti-IL-4 receptor α antibody (dupilumab), and anti-thymic stromal lymphopoietin (TSLP) antibody (tezepelumab), utilized in the management of severe asthma, may prove beneficial in managing ABPA. However, there is paucity of comprehensive knowledge regarding the efficacy of humanized monoclonal antibodies in ABPA. Here, we present a case of asthma complicated by ABPA. Mepolizumab, which was initially effective in managing the condition, aggravated ABPA in the patient during the disease course. Subsequently, by switching to dupilumab, both symptoms and imaging findings once again improved.
2. Case presentation
A 67-year-old woman presented to our hospital with a 6-month history of a gradually worsening cough. She had a 9-year history of asthma, managed on high dose fluticasone/formoterol inhalation monotherapy and no other oral medications. She had no smoking history. However, she used to work in a miso production factory. Miso production commonly involves the use of “koji” a strain belonging to Aspergillus species.
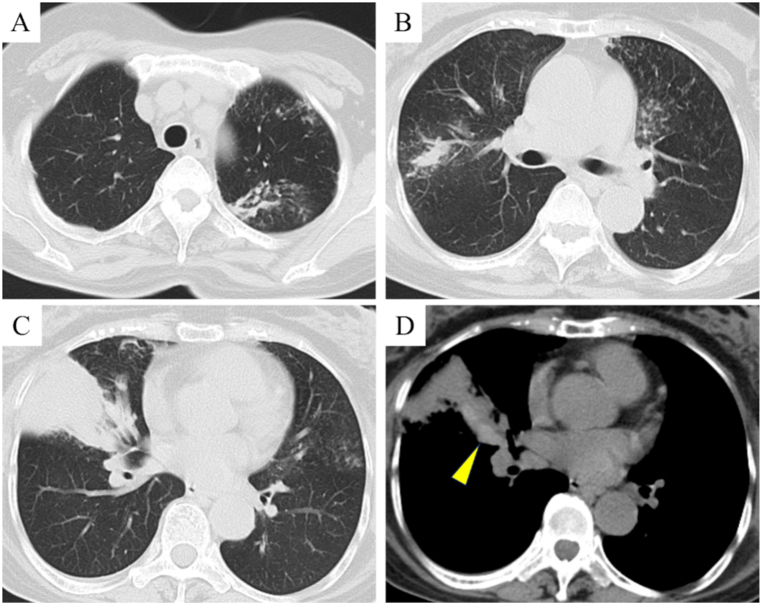
On examination, the right lung showed mild wheezing. Blood tests revealed an elevated white blood cell count of 10,300/μL with eosinophilia (927/μL) and elevated levels of non-specific IgE of 901.6 IU/μL. Additionally, the Aspergillus fumigatus-specific-IgE level was also elevated at 4.44/μL (0–0.34). Chest radiography revealed dense infiltration in the right middle lung field. Chest computed tomography (CT) demonstrated nodules in both upper lobes and an infiltrating shadow in the right middle lobe (Fig. 1A, B, and C). Additionally, high-attenuation mucus was observed in the right middle lobe bronchus (Fig. 1D). Bronchoscopy revealed mucoid impaction containing Aspergillus nidulans in the right middle lobe bronchus. Therefore, the patient was diagnosed with ABPA based on the International Society for Human and Animal Mycology criteria [1].
Fig. 1.
Findings of chest computed tomography (CT) on admission. (A, B, and C) CT scans showing nodules in both upper lobes and an infiltrating shadow in the right middle lobe. (D) CT scan showing high-attenuation mucus (HAM) in the middle lobe bronchus (arrowhead).
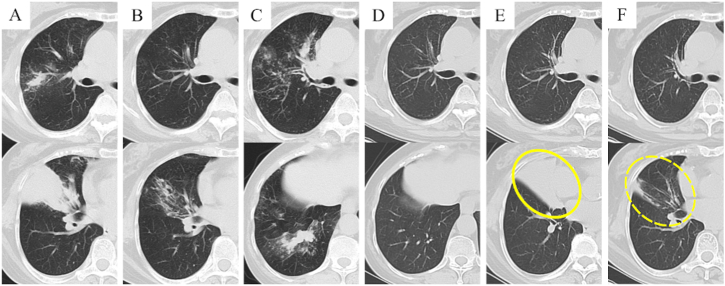
Fig. 2 shows the patient's clinical course while Fig. 3 shows the chest CT imaging findings during the clinical course. She received a 6-month regimen of oral prednisolone therapy, which resulted in the resolution of her symptoms, and concomitant improvement in the Asthma Control Test (ACT) score. Furthermore, serum eosinophil counts and total IgE levels were decreased, alongside improvements in CT findings (Fig. 3B). Thereafter, the patient continued with her asthma management therapy of the high dose inhaled fluticasone/formoterol. However, after 4 years, she experienced symptoms such as cough and wheezing, as well as exacerbations concomitant with a decline in the ACT score. Additionally, serum total IgE levels elevated to 953.8 IU/μL, marking a 59 % escalation from the clinical remission phase, and CT scan revealed worsening nodules in the right upper lobe and an infiltrating shadow in the right lower lobe (Fig. 3C). Nontuberculous mycobacterial (NTM) infection complications were suspected because of the presence of anti-glycopeptidolipid-core IgA antibodies. Subsequent bronchoscopy revealed the recurrence of mucoid impaction containing Aspergillus terreus in the right basal bronchus. However, acid-fast bacilli were not detected in the right upper lobe bronchial lavage fluid smear and culture. Consequently, the patient was diagnosed with recurrent ABPA. Thus, she received a subcutaneous injection of 100 mg mepolizumab monthly instead of prednisolone, considering the inability to definitively exclude NTM infection and the apprehension surrounding potential exacerbation of NTM infection in the presence of prednisolone. Additionally, she retired from her miso production occupation. Although symptoms such as cough and the observed imaging findings initially showed a temporary improvement (Fig. 3D), approximately 2 years later, the symptoms recurred along with a gradual increase in serum total IgE levels to 1207.9 IU/μL, marking a 101 % escalation from the clinical remission phase. Additionally, CT scan revealed the development of atelectasis of the right middle lobe (Fig. 3E). Therefore, mepolizumab was replaced with dupilumab, starting with a subcutaneous injection dose of 600 mg followed by a maintenance dose of 300 mg every 2 weeks.
Fig. 2.
Clinical course of the patient. CT, computed tomography; ACT, Asthma Control Test; Eos, eosinophil; IgE, immunoglobulin E; PSL, prednisolone.
Fig. 3.
Chest computed tomography imaging during the clinical course. (A) Before treatment, nodules were observed in the right upper lobe and an infiltrating shadow along with mucoid impaction was observed in the right middle lobe. (B) After 6 months of prednisolone treatment, the nodules, infiltrating shadow, and mucoid impaction resolved. (C) Four years after the prednisolone treatment, the nodules recurred in the right upper lobe, and the infiltrating shadow and mucoid impaction recurred in the right lower lobe. (D) After treatment with mepolizumab, the nodules and infiltrating shadow improved. (E) After 2 years of mepolizumab treatment, atelectasis of the right middle lobe was observed (circle). (F) Following treatment with dupilumab, atelectasis of the right middle lobe resolved, resulting in the presence of traction bronchiectasis (dotted circle).
After 3 months, she achieved ABPA remission, marked by the resolution of her symptoms, decreased serum total IgE levels, and improved CT findings (Fig. 3F). She remained on the maintenance dupilumab regimen.
3. Discussion
We present a case of refractory asthma complicated by ABPA, which was successfully treated after switching mepolizumab to dupilumab. Currently, humanized monoclonal antibodies, including anti-IgE antibody (omalizumab), anti-IL-5 antibody (mepolizumab and reslizumab), anti-IL-5 receptor antibody (benralizumab), anti-IL-4 receptor α antibody (dupilumab), and anti-TSLP antibody (tezepelumab), have been approved for treating severe bronchial asthma. In recent years, several studies have reported the efficacy of various antibodies against ABPA [[3], [4], [5], [6], [7], [8], [9]]. However, there is limited literature on alternative therapeutic options when antibodies prove ineffective. This case study highlights the clinical benefits of dupilumab in patients with ABPA who show inadequate response to mepolizumab during the disease course.
Eosinophil extracellular trap death (ETosis) is considered to have a significant role in the development of mucoid impaction in patients with ABPA [10]. Given the critical role of IL-5 in eosinophil differentiation, activation, migration, and survival [11], the efficacy of IL-5-targeting agents, such as mepolizumab and benralizumab, against ABPA, has been investigated. Several reports have demonstrated the successful outcomes of using these agents in the treatment of ABPA [[4], [5], [6]]. Dupilumab selectively targets the alpha subunit of the IL-4 receptor, which is common to both IL-4 and IL-13 signaling pathways [12]. In addition to its direct inhibition effect on the IL-13 pathway, it also exerts suppressive effects on IL-5 production through inhibition of group 2 innate lymphoid cells (ILC2) [13]. In so doing, it potentially exhibits comparable efficacy against ABPA, similar to mepolizumab and benralizumab. However, some components of ABPA pathology may not be solely attributed to ETosis. Some reported cases of ABPA yielded positive outcomes with the administration of the anti-IgE antibody omalizumab [7]; in other cases, mepolizumab proved to be ineffective while dupilumab demonstrated successful therapeutic outcomes [8,9]. Blockade of IL-4 inhibits B cell-mediated IgE production, while blockade of IL-13 inhibits airway smooth muscle constriction and epithelial cells hypersecretion [14]. The combined inhibitory impact of dupilumab on type 2 inflammation may offer an advantage in cases of ABPA where other antibody therapies have proven to be ineffective.
In this case, ABPA remission following the use of mepolizumab was temporary. To this end, after approximately 2 years, the clinical response to mepolizumab declined with an elevation in peripheral blood IgE levels, leading to ABPA recurrence. As the patient maintained regular monthly hospital visits and received mepolizumab, poor treatment adherence as a cause of ABPA recurrence was ruled out. While the production of neutralizing antibodies to mepolizumab is a possibility, it has been reported to be extremely rare [15]. Furthermore, the patient's eosinophil count was normal at the time of ABPA recurrence, suggesting a low probability of neutralizing antibody production. One potential environmental factor to consider is the influence of the patient's previous miso production occupation; however, she had retired from that occupation after initiating mepolizumab therapy. Aspergillus colonization may nevertheless persist in the airways even after the exposure to Aspergillus species is discontinued, which could contribute to disease recurrence. Therefore, solely suppressing type 2 inflammation may not provide adequate efficacy in the management of disease recurrence. Standard treatment for ABPA involves the administration of corticosteroids and antifungal agents such as itraconazole. The efficacy of itraconazole, either as monotherapy or in combination with corticosteroids, has been previously reported [16,17]. Notably, the combination therapy of prednisolone and itraconazole has demonstrated a recurrence rate of 20.6 %, which is lower than the 33 % recurrence rate observed in a prednisolone monotherapy group [17]. Therefore, itraconazole combination therapy may be considered as a potential treatment option in this case in the future.
4. Conclusions
We described a patient with refractory asthma accompanied by ABPA who experienced recurrence despite receiving mepolizumab treatment, but exhibited a favorable response to dupilumab. Dupilumab holds potential benefits for patients with ABPA who cannot be administered prednisolone because of its side effects. We anticipate additional evidence on the effectiveness of dupilumab in ABPA, including the results of phase Ⅲ clinical trials.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Funding
This report did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Yasutaka Kawasaki: Conceptualization, Data curation, Formal analysis, Project administration, Writing – original draft, Writing – review & editing. Kazuaki Nishiki: Project administration, Writing – review & editing. Takeshi Ishizaki: Supervision, Writing – review & editing, Project administration.
Declaration of competing interest
The authors have no conflicts of interest associated with this report to declare.
Acknowledgements
We would like to thank Editage (www.editage.jp) for the English language editing.
References
- 1.Agarwal R., Chakrabarti A., Shah A., et al. Allergic bronchopulmonary aspergillosis: review of literature and proposal of new diagnostic and classification criteria. Clin. Exp. Allergy. 2013;43:850–873. doi: 10.1111/cea.12141. [DOI] [PubMed] [Google Scholar]
- 2.Volmer T., Effenberger T., Trautner C., Buh R. Consequences of long-term oral corticosteroid therapy and its side-effects in severe asthma in adults: a focused review of the impact data in the literature. Eur. Respir. J. 2018;52 doi: 10.1183/13993003.00703-2018. [DOI] [PubMed] [Google Scholar]
- 3.Nishimura T., Okano T., Naito M., et al. Complete withdrawal of glucocorticoids after dupilumab therapy in allergic bronchopulmonary aspergillosis: a case report. World. J. Clin. Cases. 2021;9:6922–6928. doi: 10.12998/wjcc.v9.i23.6922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matsuura H., Fujiwara K., Omori H., et al. Successful treatment with benralizumab for allergic bronchopulmonary aspergillosis that developed after disastrous heavy rainfall in western Japan. Intern. Med. 2021;60:1443–1450. doi: 10.2169/internalmedicine.6217-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsubouchi K., Arimura-Omori M., Inoue S., et al. A case of allergic bronchopulmonary aspergillosis with marked peripheral blood eosinophilia successfully treated with benralizumab. Respir. Med. Case. Rep. 2021;32 doi: 10.1016/j.rmcr.2021.101339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eldaabossi S.A.M., Awad A., Anshasi N. Mepolizumab and dupilumab as a replacement to systemic glucocorticoids for the treatment of chronic eosinophilic pneumonia and allergic bronchopulmonary aspergillosis–case series, Almoosa specialist hospital. Respir. Med. Case. Rep. 2021;34 doi: 10.1016/j.rmcr.2021.101520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li J.X., Fan L.C., Li M.H., Cao W.J., Xu J.F. Beneficial effects of omalizumab therapy in allergic bronchopulmonary aspergillosis: a synthesis review of published literature. Respir. Med. 2017;122:33–42. doi: 10.1016/j.rmed.2016.11.109. [DOI] [PubMed] [Google Scholar]
- 8.Kai Y., Yoshikawa M., Matsuda M., et al. Successful management of recurrent allergic bronchopulmonary aspergillosis after changing from mepolizumab to dupilumab: a case report. Respir. Med. Case. Rep. 2022;39 doi: 10.1016/j.rmcr.2022.101723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mikura S., Saraya T., Yoshida Y., et al. Successful treatment of mepolizumab- and prednisolone-resistant allergic bronchopulmonary aspergillosis with dupilumab. Intern. Med. 2021;60:2839–2842. doi: 10.2169/internalmedicine.6679-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ueki S., Hebisawa A., Kitani M., Asano K., Neves J.S. Allergic bronchopulmonary aspergillosis-a luminal hypereosinophilic disease with extracellular trap cell death. Front. Immunol. 2018;9:2346. doi: 10.3389/fimmu.2018.02346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nagase H., Ueki S., Fujieda S. The roles of IL-5 and anti-IL-5 treatment in eosinophilic diseases: asthma, eosinophilic granulomatosis with polyangiitis, and eosinophilic chronic rhinosinusitis. Allergol. Int. 2020;69:178–186. doi: 10.1016/j.alit.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Rabe K.F., Nair P., Brusselle G., et al. Efficacy and safety of dupilumab in glucocorticoid-dependent severe asthma. N. Engl. J. Med. 2018;378:2475–2485. doi: 10.1056/NEJMoa1804093. [DOI] [PubMed] [Google Scholar]
- 13.Patel G., Pan J., Ye L., et al. Blockade of IL-4Rα inhibits group 2 innate lymphoid cell responses in asthma patients. Clin. Exp. Allergy. 2020;50:267–270. doi: 10.1111/cea.13514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walford H.H., Doherty T.A. Diagnosis and management of eosinophilic asthma: a US perspective. J. Asthma Allergy. 2014;7:53–65. doi: 10.2147/JAA.S39119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ortega H.G., Meyer E., Brusselle G., et al. Update on immunogenicity in severe asthma: experience with mepolizumab. J. Allergy Clin. Immunol. Pract. 2019;7:2469–2475. doi: 10.1016/j.jaip.2019.03.042. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal R., Dhooria S., Sehgal I.S., et al. A randomized trial of itraconazole vs prednisolone in acute-stage allergic bronchopulmonary aspergillosis complicating asthma. Chest. 2018;153:656–664. doi: 10.1016/j.chest.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Agarwal R., Muthu V., Sehgal I.S., et al. A randomized trial of prednisolone versus prednisolone and itraconazole in acute-stage allergic bronchopulmonary aspergillosis complicating asthma. Eur. Respir. J. 2021;59 doi: 10.1183/13993003.01787-2021. [DOI] [PubMed] [Google Scholar]