Abstract
Iliopsoas tendinitis following total hip arthroplasty has been linked to retroverted acetabular cup position with associated anterior overhang. For severely malpositioned components, preferred treatment is in the form of revision arthroplasty. However, for a substantial number of cases, iliopsoas tendinitis as well as associated pain and disability are observed in the presence of modest acetabular overhang. In such cases, patients may benefit substantially from arthroscopic iliopsoas fractional lengthening. Given altered postarthroplasty anatomy, we present an arthroscopic approach employing an iliopsoas air bursogram. In such a way, safe and predictable access can be provided for efficient tendon lengthening without capsular violation or inadvertent instrumentation of the nearby medial neurovascular bundle.
Technique Video
Surgical video demonstrating arthroscopic iliopsoas fractional lengthening after total hip arthroplasty using the iliopsoas air bursogram technique. The patient is positioned supine on a hip distraction table, and the right hip is prepared and draped in standard fashion for hip arthroscopy. Fluoroscopic guidance is used to localize and mark the vastus ridge and lesser trochanter on the surgical field. An anterolateral (AL) portal is marked 2 cm medial to the anterior border of the femur, in line with the vastus ridge. A 17-gauge access needle is passed medially under fluoroscopic guidance approximately 1 cm medial to the femur, into the anatomic area of the iliopsoas bursa. An air bursogram is created using a 30-mL syringe. Again, under fluoroscopic guidance, a 1.2-mm nitinol wire is passed through the AL portal into the iliopsoas sheath, and a 5.0-mm inner diameter polymer cannula is advanced over the wire. The wire is then removed and a 70° arthroscope is inserted. Under direct visualization, a modified anterior portal (MAP) is established approximately 3 cm medial and 3 cm distal to the AL portal using a 17-gauge needle, nitinol wire, and 5.0-mm cannula. A 4.2-mm straight shaver is inserted into the MAP and used to gently debride bursal tissue under direct visualization, providing access to the iliopsoas tendon. Once visualized, differentiation of capsule and iliopsoas tendon can be performed under fluoroscopic guidance. The shaver is exchanged for an arthroscopic radiofrequency ablator, and the iliopsoas tendon is cut approximately halfway between the lesser trochanter and femoral implant head-neck junction. The 2 ends of the tendon are observed to spring back 3 to 4 cm, which can be confirmed fluoroscopically using the RF device as a radio-opaque probe.
Iliopsoas tendinitis following total hip arthroplasty has been linked to retroverted acetabular component position with associated anterior overhang. For severely retroverted or mispositioned components, preferred treatment is in the form of revision arthroplasty. However, revision arthroplasty remains a relatively invasive intervention, particularly considering that for a substantial number of cases, iliopsoas tendinitis and associated pain and disability are observed in the presence of modest acetabular overhang and otherwise satisfactory implant positioning. In such cases, patients may benefit substantially from arthroscopic iliopsoas fractional lengthening. Given altered postarthroplasty anatomy, we prefer an arthroscopic approach employing an iliopsoas air bursogram to provide access to the correct potential space of the medial hip, particularly given the nearby femoral nerve, artery, and vein.
The technique is shown in a video (Video 1) along with a list of pearls and pitfalls that the authors have found to be helpful (Table 1). The technique described allows for safe and predictable access to the iliopsoas sheath for efficient tendon lengthening without capsular violation or inadvertent instrumentation of the nearby medial neurovascular bundle.
Table 1.
Pearls and Pitfalls of Arthroscopic Iliopsoas Release
| Pearls | Pitfalls |
|---|---|
| Shift standard AL portal anteriorly (2 cm anterior to femoral cortex) to provide access to iliopsoas “around the corner” of the anterior femoral cortex. | Standard anterior-posterior AL portal location will make visualization around the anterior femoral cortex challenging. |
| Distalize standard AL portal to be in line with the vastus ridge. | Standard proximal-distal AL portal location will lead to difficulty with iliopsoas sheath access given relatively distal location of desired access. |
| Immediately turn on fluid following AL portal trocar placement. | Dry scoping, as is standard for intra-articular hip access, will result in no potential space for triangulation and instrumentation when establishing MAP access. |
| Ensure circumferential iliopsoas tendon release. | Incomplete tendon release will result in bridging fibers that prohibit appropriate fractional lengthening of the iliopsoas. |
AL, anterolateral; MAP, modified anterior portal.
Surgical Technique
Patient Positioning and Preparation
The patient is positioned supine on a hip distraction table with the feet placed into padded boots. Boot tightness need only be to the level to allow for stable patient positioning. We prefer to employ a padded post for further patient stability on the operating table, especially given the importance of precise initial arthroscopic access, which is performed with a medially directed vector of force. The operative extremity is placed in 10° of external rotation. For patients with femoral torsion such that the profile of the lesser trochanter remains hidden behind the medial cortex of the femur, slightly more external rotation can be provided, understanding that this brings both the iliopsoas and the medially based neurovascular bundle closer to the operative field. No distraction is applied. The patient is prepared and draped in standard fashion for hip arthroscopy.
Iliopsoas Air Bursogram and Initial Access
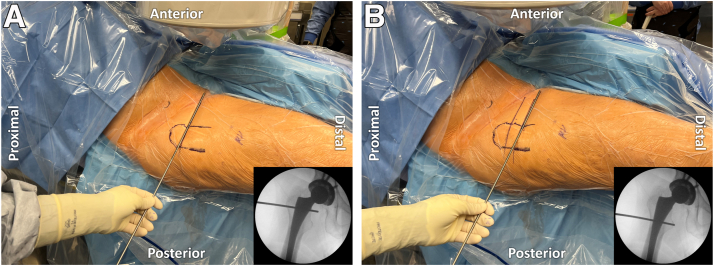
Fluoroscopic guidance is used to localize the vastus ridge as well as the level of the lesser trochanter and mark these on the surgical field (Fig 1). An anterolateral (AL) portal is marked 2 cm medial to the anterior border of the femur, in line with the vastus ridge. Subsequently, a 17-gauge access needle (Portal Entry Kit; Stryker Sports Medicine) is used to march from lateral to medial along the femur, gradually bringing the surgeon’s hand downward in an increasingly horizontal trajectory, such that the needle palpably passes just medial to the anteromedial femoral cortical margin, at the level of the vastus ridge. Upon crossing the medial border of the femur, the needle is advanced approximately 1 cm into the anatomic area of the iliopsoas bursa (Fig 2). The inner stylet of the needle is removed, and a 30-mL syringe is employed to perform an air bursogram (Fig 3). Successful access is confirmed by the presence of a radiolucent soft tissue plane extending down to the lesser trochanter and vertically upward toward the inner pelvic brim, thus representing the course of the iliopsoas. The syringe is removed and carefully exchanged for a 1.2-mm nitinol wire, often with a felt soft stop, corresponding to the iliopsoas sheath. Repeat fluoroscopic imaging is obtained to ensure no movement of the wire whatsoever and no deep penetration medially (Fig 4).
Fig 1.
Patient positioning and fluoroscopic landmarks. The patient is positioned supine, and the right lower extremity is draped in a standard supine hip arthroscopy fashion. A switching stick is used to mark the location of the level of the (A) vastus ridge and (B) lesser trochanter using fluoroscopy (inset images).
Fig 2.
Initial access. Under fluoroscopic guidance, a 17-gauge access needle is inserted until just medial to the anteromedial border of the right femur in the anatomic area corresponding to the iliopsoas sheath and bursas.
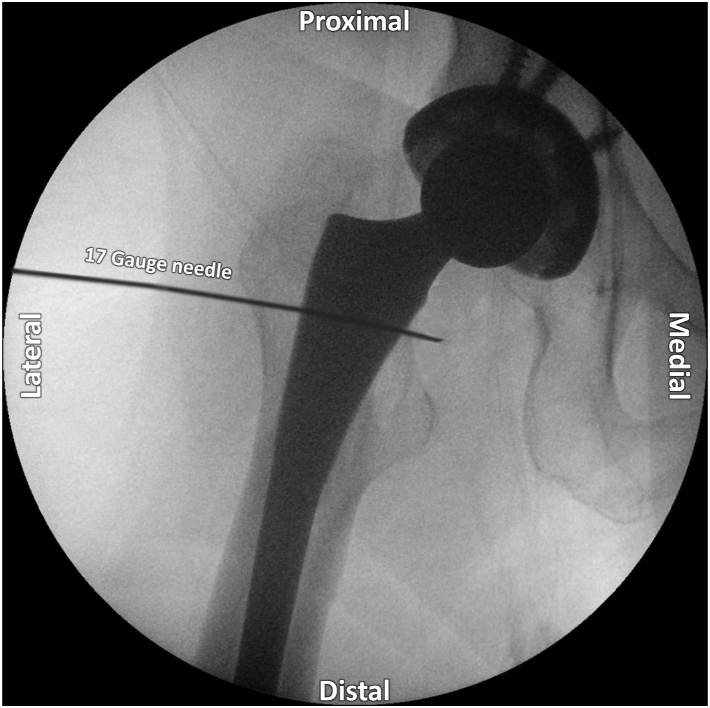
Fig 3.
Air bursogram technique. The air bursogram (dashed lines) is created by removing the inner access needle stylet and insufflation with a 30-mL syringe on a right hip.
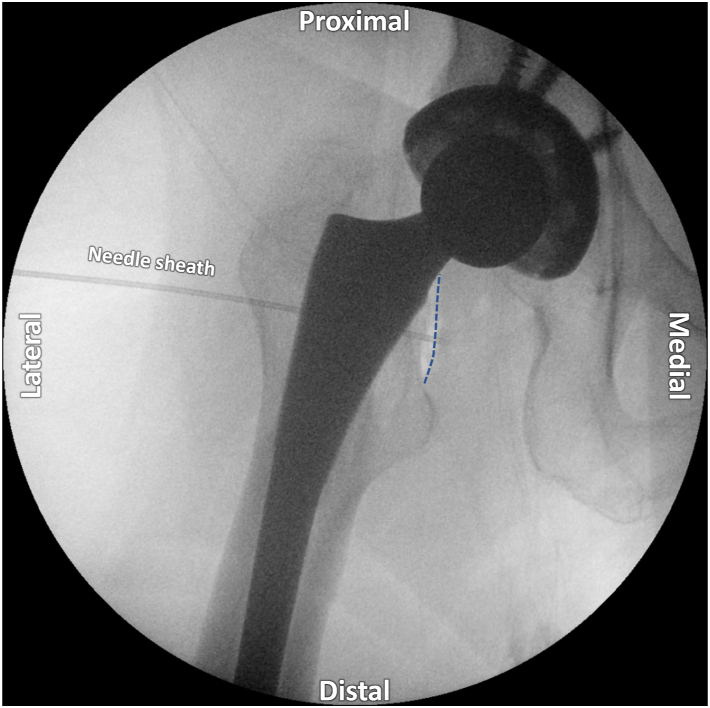
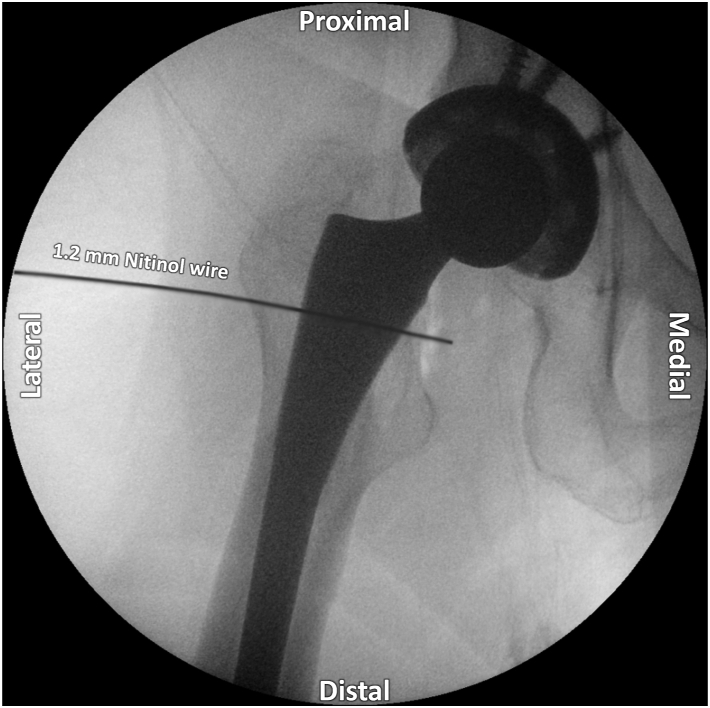
Fig 4.
Wire placement. The syringe used for the air bursogram is carefully exchanged for a 1.2-mm nitinol wire. Repeat fluoroscopic imaging confirms appropriate placement without deep penetration medial to the iliopsoas sheath on a right hip.
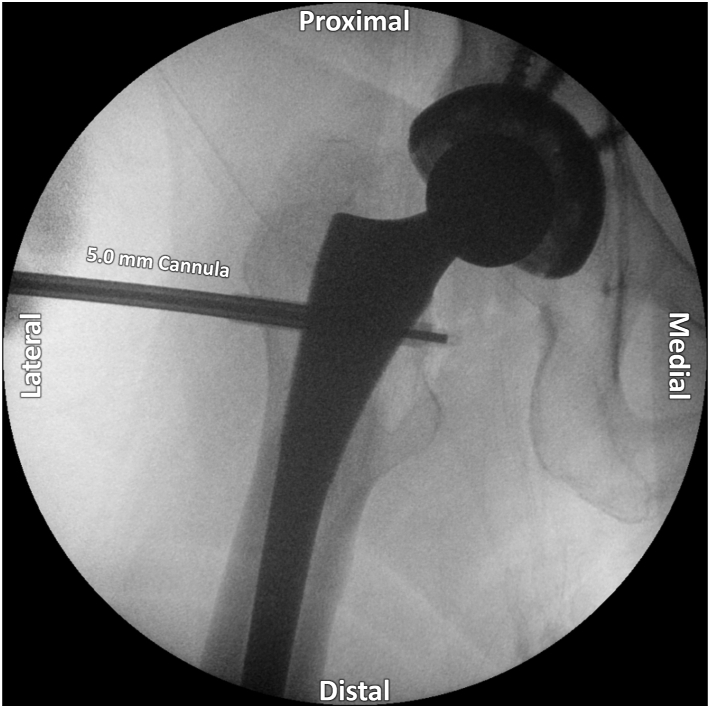
A small incision is made over the wire and a 5.0-mm inner diameter polymer cannula (FlowPort II; Stryker Sports Medicine) is carefully placed over the nitinol wire. Subsequently, the surgical assistant holds the distal end of the wire with both hands, bracing themselves to ensure that the wire does not advance. The surgeon then advances the cannula over the wire under intermittent fluoroscopic guidance to ensure that the cannula comes to the medial tip of the wire but not beyond it (Fig 5). The wire is removed and a 70° arthroscope inserted into the cannula. Water inflow is immediately begun at 35 mm Hg. A second modified anterior portal (MAP) is established approximately 3 cm medial and 3 cm distal to the AL portal, ensuring that this does not cross the line connecting the anterior superior iliac spine and lateral aspect of the patella. This MAP is first triangulated to the tip of the arthroscope with the 17-gauge needle, then a nitinol wire introduced, then a small incision made and the 5.0 mm cannula introduced over the wire to dilate a tract for subsequent instrumentation. The cannula is removed and a 4.2-mm straight shaver (CoolCut; Arthrex) is placed percutaneously into the developed potential space.
Fig 5.
Cannula placement. A 5.0-mm polymer cannula is placed over the nitinol wire and advanced under fluoroscopic guidance to the level of the iliopsoas bursa without medial overadvancement on a right hip.
Tendon Visualization and Release
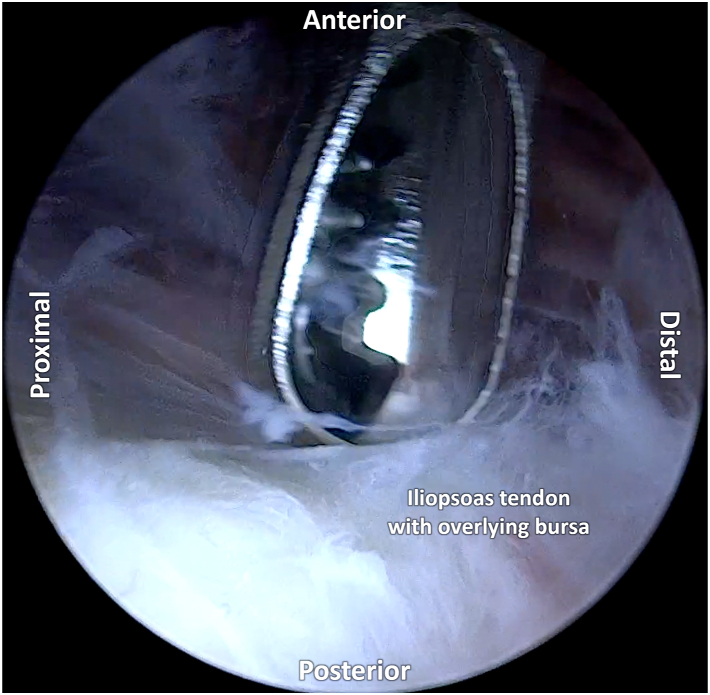
The shaver is used to gently remove bursal tissue under direct visualization and provide access to the iliopsoas tendon (Fig 6). Of note, the anterior joint capsule often contains shiny white longitudinal fibers (the iliofemoral ligament), and fluoroscopic images with the shaver placed on the structure of interest can be helpful in differentiating the capsule from the more medially located iliopsoas tendon tissue (Fig 7). Anatomically, the tendon often courses over the posterior and lateral aspect of the iliopsoas muscle. Once visualized and the bursa has been debrided, the tendon is followed down to the lesser trochanter, confirming the structure’s insertion on fluoroscopy, and then also followed 3 to 4 cm proximally toward the level of the head-neck junction of the implant, again fluoroscopically confirming the correct structure to be released.
Fig 6.
Arthroscopic debridement. An arthroscopic anterolateral portal view of a patient in standard supine (right) hip arthroscopy positioning. Arthroscopic debridement of the bursa overlying the iliopsoas tendon is performed with the shaver placed through the modified anterior portal (MAP).
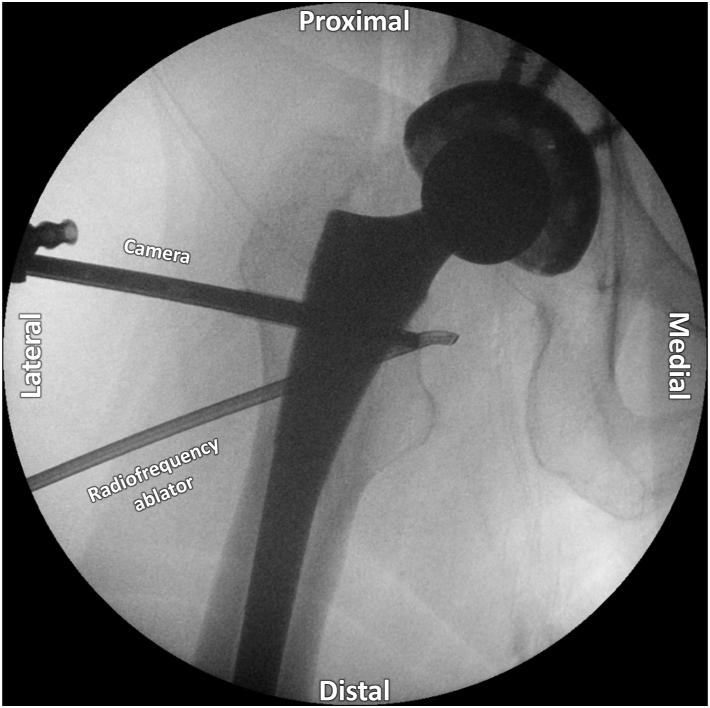
Fig 7.
Iliopsoas tendon release location. Visualization of the radiofrequency ablator location on fluoroscopy confirms identification of iliopsoas tendon tissue, approximately halfway between the lesser trochanter and implant head-neck junction on a right hip.
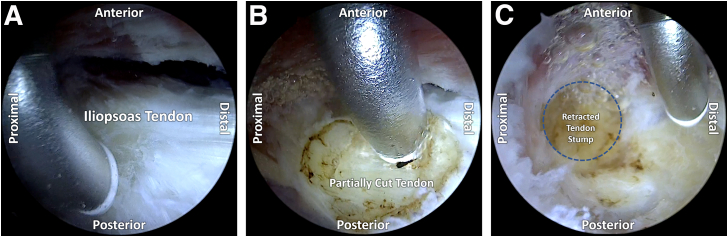
It is the authors’ preference to place the shaver in front of and behind the tendon in order to separate it from the more medially based iliopsoas muscle fibers. Subsequently, the shaver is exchanged for an arthroscopic radiofrequency ablator (50-S Sweep; Stryker Sports Medicine) and cut approximately halfway between the lesser trochanter and femoral implant head-neck junction, ensuring that all tendon fibers are transected without damaging the underlying muscle (Fig 8). The 2 ends of tendon are observed to spring back 3 to 4 cm, the distance of which can be visualized and confirmed fluoroscopically using the tip of the radiofrequency device as a radio-opaque probe.
Fig 8.
Iliopsoas tendon release with the radiofrequency ablator. An arthroscopic anterolateral portal view of a patient in standard supine (right) hip arthroscopy positioning. The ablator is placed through the modified anterior portal (MAP) and positioned over the iliopsoas tendon (A). Partial (B) and then complete (C) release of the tendon is performed, demonstrating proximal retraction of the transected tendon stump.
Closure and Postoperative Rehabilitation
Instruments are removed from the AL and MAP portals. Incisions are closed with 3-0 Nylon sutures in a horizontal mattress fashion and a sterile dressing applied. Patients are allowed to weight bear as tolerated immediately postoperatively, often using crutches for 2 to 3 days until their pain, strength, and gait improve. Patients are seen and evaluated by physical therapy following their 2-week suture removal appointment for gait training, with additional sessions as needed for patients who feel that they could benefit from further formal therapy.
Discussion
Although persistent groin pain after total hip arthroplasty is rare, there is increasing awareness of iliopsoas impingement and tendonitis as an etiology that may account for up to 4% of patients with painful THA.1 Primary initial treatment consists of physical therapy, nonsteroidal anti-inflammatory medications, and tendon sheath injections. The results of nonsurgical management are mixed in the literature, with some studies reporting 50% success as defined by resolution of anterior groin pain and improved pain-free hip flexion.1,2 Surgery is recommended if nonoperative modalities fail to provide durable benefit. Surgical options include acetabular revision or an open or arthroscopic/endoscopic iliopsoas release. Overall surgical management has showed good clinical results with significant improvements in both pain and function.2, 3, 4, 5
As with any surgery, a mutual decision between the surgeon and the patient is determined based on indications,6 potential risks, and benefits of the procedure. In terms of indications, acetabular component revision is often reserved for patients with significant implant malposition (≥8 mm acetabular prominence).2 Open surgeries are associated with higher morbidity rates than arthroscopic procedures, making minimally invasive techniques, when indicated, an appealing alternative to conventional surgery.3,7 Specific to this cohort, minimally invasive procedures shield the patient from the potential morbidity of an additional open procedure and are ideal in the setting of THA to potentially decrease the risk of surgical site infection and postoperative instability. For patients with modest acetabular overhang, both arthroscopic and endoscopic approaches have been shown to provide good functional and patient-reported outcomes in over 85% of patients.3 In fact, several studies have shown numerous minimally invasive techniques for the treatment of iliopsoas impingement after THA to be as effective as conventional surgery in terms of clinical outcomes while being associated with lower morbidity rates.3, 4, 5,7, 8, 9 Although good clinical results and a low rate of complications have been reported for varying arthroscopic/endoscopic techniques, they each offer a different set of advantages.7, 8, 9
Our technique for arthroscopic iliopsoas fractional lengthening using an air bursogram is both safe and reproducible and offers several distinct advantages (Table 2). This pragmatic approach is performed percutaneously with standard access cannulas and does not require access to the central compartment, obviating the need for hip distraction. Working in the peripheral compartment and maintaining the intact hip capsule without violating the space containing the prosthetic implants may decrease the risk of postoperative instability and surgical site infection and removes the difficulty of operating in surgically altered anatomy adjacent to critical neurovascular structures. Moreover, fluoroscopic identification of the iliopsoas bursa facilitates reproducible access and allows the surgeon to visualize the length of the iliopsoas tendon from the head-neck junction to its insertion on the lesser trochanter, allowing more precise sectioning of the tendon while preserving muscular tissue.
Table 2.
Advantages and Disadvantages, Including Risks and Limitations, of Arthroscopic Iliopsoas Fractional Lengthening With Access Using an Iliopsoas Air Bursogram
| Advantages | Disadvantages, Risks, and Limitations |
|---|---|
| Direct access to the iliopsoas bursa allows for maintenance of intact hip capsule without violating the space containing the prosthetic implant. | Access medial to the capsule and implant is nearby the adjacent neurovascular structures. |
| Use of an iliopsoas bursogram allows for visual confirmation of correct anatomic structure to be exposed and released. | Injection to other nearby potential spaces may create (overlapping) soft tissue shadows that make subsequent successful generation and visualization of an air bursogram difficult. |
| The described technique can be performed percutaneously, with standard (scope) access cannulas, without the need for additional instrumentation or large cannulas. | Surgeons should be comfortable with percutaneous instrumentation of the medial hip. Consideration may be given to use of an instrument skid. |
Conclusions
Using an arthroscopic approach and employing an iliopsoas air bursogram, safe and predictable iliopsoas fractional lengthening can be achieved without capsular violation or inadvertent instrumentation of the nearby medial neurovascular bundle.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: support from the Foderaro-Quattrone Musculoskeletal-Orthopaedic Surgery Research Innovation Fund. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical video demonstrating arthroscopic iliopsoas fractional lengthening after total hip arthroplasty using the iliopsoas air bursogram technique. The patient is positioned supine on a hip distraction table, and the right hip is prepared and draped in standard fashion for hip arthroscopy. Fluoroscopic guidance is used to localize and mark the vastus ridge and lesser trochanter on the surgical field. An anterolateral (AL) portal is marked 2 cm medial to the anterior border of the femur, in line with the vastus ridge. A 17-gauge access needle is passed medially under fluoroscopic guidance approximately 1 cm medial to the femur, into the anatomic area of the iliopsoas bursa. An air bursogram is created using a 30-mL syringe. Again, under fluoroscopic guidance, a 1.2-mm nitinol wire is passed through the AL portal into the iliopsoas sheath, and a 5.0-mm inner diameter polymer cannula is advanced over the wire. The wire is then removed and a 70° arthroscope is inserted. Under direct visualization, a modified anterior portal (MAP) is established approximately 3 cm medial and 3 cm distal to the AL portal using a 17-gauge needle, nitinol wire, and 5.0-mm cannula. A 4.2-mm straight shaver is inserted into the MAP and used to gently debride bursal tissue under direct visualization, providing access to the iliopsoas tendon. Once visualized, differentiation of capsule and iliopsoas tendon can be performed under fluoroscopic guidance. The shaver is exchanged for an arthroscopic radiofrequency ablator, and the iliopsoas tendon is cut approximately halfway between the lesser trochanter and femoral implant head-neck junction. The 2 ends of the tendon are observed to spring back 3 to 4 cm, which can be confirmed fluoroscopically using the radiofrequency device as a radio-opaque probe.
References
- 1.Lachiewicz P.F., Kauk J.R. Anterior iliopsoas impingement and tendinitis after total hip arthroplasty. J Am Acad Orthop Surg. 2009;17:337–344. doi: 10.5435/00124635-200906000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Chalmers B.P., Sculco P.K., Sierra R.J., Trousdale R.T., Berry D.J. Iliopsoas impingement after primary total hip arthroplasty: Operative and nonoperative treatment outcomes. J Bone Joint Surg Am. 2017;99:557–564. doi: 10.2106/JBJS.16.00244. [DOI] [PubMed] [Google Scholar]
- 3.May O. Arthroscopic techniques for treating ilio-psoas tendinopathy after hip arthroplasty. Orthop Traumatol Surg Res. 2019;105:S177–S185. doi: 10.1016/j.otsr.2018.05.017. [DOI] [PubMed] [Google Scholar]
- 4.Di Benedetto P., Niccoli G., Magnanelli S., et al. Arthroscopic treatment of iliopsoas impingement syndrome after hip arthroplasty. Acta Biomed. 2019;90:104–109. doi: 10.23750/abm.v90i1-S.8076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zimmerer A., Hauschild M., Nietschke R., et al. Results after arthroscopic treatment of iliopsoas impingement after total hip arthroplasty. Arch Orthop Trauma Surg. 2022;142:189–195. doi: 10.1007/s00402-020-03623-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blackman A. Editorial commentary: Iliopsoas tenotomy for pain after total hip: A great operation if the diagnosis is right. Arthroscopy. 2021;37:2830–2831. doi: 10.1016/j.arthro.2021.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Guicherd W., Bonin N., Gicquel T., et al. Endoscopic or arthroscopic iliopsoas tenotomy for iliopsoas impingement following total hip replacement. A prospective multicenter 64-case series. Orthop Traumatol Surg Res. 2017;103:S207–S214. doi: 10.1016/j.otsr.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Williams M., Ashworth M. An operative technique for psoas impingement following total hip arthroplasty: A case series of day case, extra articular, arthroscopic psoas tenotomy. Arch Orthop Trauma Surg. 2019;139:211–216. doi: 10.1007/s00402-018-3029-3. [DOI] [PubMed] [Google Scholar]
- 9.Ilizaliturri V.M., Jr., Buganza-Tepole M., Olivos-Meza A., Acuna M., Acosta-Rodriguez E. Central compartment release versus lesser trochanter release of the iliopsoas tendon for the treatment of internal snapping hip: A comparative study. Arthroscopy. 2014;30:790–795. doi: 10.1016/j.arthro.2014.03.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical video demonstrating arthroscopic iliopsoas fractional lengthening after total hip arthroplasty using the iliopsoas air bursogram technique. The patient is positioned supine on a hip distraction table, and the right hip is prepared and draped in standard fashion for hip arthroscopy. Fluoroscopic guidance is used to localize and mark the vastus ridge and lesser trochanter on the surgical field. An anterolateral (AL) portal is marked 2 cm medial to the anterior border of the femur, in line with the vastus ridge. A 17-gauge access needle is passed medially under fluoroscopic guidance approximately 1 cm medial to the femur, into the anatomic area of the iliopsoas bursa. An air bursogram is created using a 30-mL syringe. Again, under fluoroscopic guidance, a 1.2-mm nitinol wire is passed through the AL portal into the iliopsoas sheath, and a 5.0-mm inner diameter polymer cannula is advanced over the wire. The wire is then removed and a 70° arthroscope is inserted. Under direct visualization, a modified anterior portal (MAP) is established approximately 3 cm medial and 3 cm distal to the AL portal using a 17-gauge needle, nitinol wire, and 5.0-mm cannula. A 4.2-mm straight shaver is inserted into the MAP and used to gently debride bursal tissue under direct visualization, providing access to the iliopsoas tendon. Once visualized, differentiation of capsule and iliopsoas tendon can be performed under fluoroscopic guidance. The shaver is exchanged for an arthroscopic radiofrequency ablator, and the iliopsoas tendon is cut approximately halfway between the lesser trochanter and femoral implant head-neck junction. The 2 ends of the tendon are observed to spring back 3 to 4 cm, which can be confirmed fluoroscopically using the RF device as a radio-opaque probe.
Surgical video demonstrating arthroscopic iliopsoas fractional lengthening after total hip arthroplasty using the iliopsoas air bursogram technique. The patient is positioned supine on a hip distraction table, and the right hip is prepared and draped in standard fashion for hip arthroscopy. Fluoroscopic guidance is used to localize and mark the vastus ridge and lesser trochanter on the surgical field. An anterolateral (AL) portal is marked 2 cm medial to the anterior border of the femur, in line with the vastus ridge. A 17-gauge access needle is passed medially under fluoroscopic guidance approximately 1 cm medial to the femur, into the anatomic area of the iliopsoas bursa. An air bursogram is created using a 30-mL syringe. Again, under fluoroscopic guidance, a 1.2-mm nitinol wire is passed through the AL portal into the iliopsoas sheath, and a 5.0-mm inner diameter polymer cannula is advanced over the wire. The wire is then removed and a 70° arthroscope is inserted. Under direct visualization, a modified anterior portal (MAP) is established approximately 3 cm medial and 3 cm distal to the AL portal using a 17-gauge needle, nitinol wire, and 5.0-mm cannula. A 4.2-mm straight shaver is inserted into the MAP and used to gently debride bursal tissue under direct visualization, providing access to the iliopsoas tendon. Once visualized, differentiation of capsule and iliopsoas tendon can be performed under fluoroscopic guidance. The shaver is exchanged for an arthroscopic radiofrequency ablator, and the iliopsoas tendon is cut approximately halfway between the lesser trochanter and femoral implant head-neck junction. The 2 ends of the tendon are observed to spring back 3 to 4 cm, which can be confirmed fluoroscopically using the radiofrequency device as a radio-opaque probe.