Abstract
Purpose
To identify the best internal structure of the Brazilian version of the Anterior Knee Pain Scale (AKPS), comparing different instrument structures (structural validity) and correlating the scores of the versions (criterion validity).
Methods
We included Brazilian volunteers, aged ≥ 18 years, with patellofemoral pain (PFP) for at least 3 months. We used the confirmatory factor analysis and considered the following fit indices: chi-square/degrees of freedom (DF), comparative fit index (CFI), Tucker-Lewis index (TLI), root mean square error of approximation (RMSEA). We considered the structure with the lowest values of the Akaike information criterion (AIC), sample size adjusted Bayesian information criterion (SABIC), and assessed criterion validity using Pearson correlation coefficient (r) to correlate the long and short versions.
Results
The study included 101 participants, mostly women (65.3%), young adults (~ 31 years old), overweight (BMI > 25 kg/m2), incomplete higher education (37.6%), and physically active (64.4%). The original 1-domain, 13-item structure showed adequate fit indices (chi-square/GL < 3.00, TLI and CFI > 0.90, and RMSEA < 0, 08). However, items 11 and 12 had a factorial load of less than 0.23. Therefore, we excluded items 11 and 12 and found adequate fit indices (chi-square/GL < 3.00, TLI and CFI > 0.90, and RMSEA < 0, 08) and lower AIC and SABIC values. We observed a correlation coefficient above the acceptable cutoff of 0.70 (r = 0.966, p-value < 0.001) between the versions.
Conclusion
The 11-item AKPS (without items 11 and 12) is the version with the most adequate internal structure and correlates satisfactorily with the long version of the instrument.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-024-07164-z.
Keywords: Musculoskeletal disorders; Functional status; Factor analysis, statistical
Introduction
Patellofemoral pain (PFP) is a common patellofemoral condition that is characterized by an insidious onset of poorly defined pain, localized to the anterior retropatellar and/or peripatellar region of the knee [1]. The onset of symptoms may be slow or acutely develop with a worsening of pain accompanying lower-limb loading activities [2].
The Anterior Knee Pain Scale (AKPS), or Kujala score, was developed by Kujala et al. [3] in Finland (in English, in 1993) to measure aspects of disability [4] caused by patellofemoral disorders (e.g., PFP, patellar subluxation, and patellar dislocation). The authors validated the construct by finding significantly lower scores in patients with patellofemoral disorders when compared to a control group.
The original instrument has 13 items and scores ranging from 0 to 100, with lower scores indicating greater disability. Since the development of the instrument [3], several studies have been conducted to adapt the AKPS to other cultures, including Turkish [5], Chinese [6], Persian [7], Spanish [8], Dutch [9], Thai [10], Greek [11], Arabic [12], Indonesian [13], Norwegian [14], Italian [15], German [16], and French [17].
In Brazil, two studies translated and adapted the AKPS for the population with PFP. Firstly, Aquino et al. [18] performed the translation and cross-cultural adaptation and did not investigate any other measurement properties. Subsequently, a more robust study translated and adapted the AKPS for the Brazilian population and identified the instrument with adequate internal consistency and reliability, with a valid construct, and with satisfactory responsiveness [4]. However, no validation studies have examined the internal structure of the AKPS through factor analysis, thus reducing its relevance to clinical or research settings.
A systematic review examined the measurement properties of scales and questionnaires for patients with PFP and found that only the Activities of Daily Living Scale (ADLS) and the International Knee Documentation Committee (IKDC) had an internal structure confirmed by factor analysis [19]. Furthermore, according to Hoglund et al. [1, 20], most patient-reported outcome measures used to measure pain and function in patients with PFP have inadequate content validity.
The evaluation of condition-specific patient-reported outcomes is highly recommended by experts [21], with the AKPS being one of the most commonly used instruments and correlating with many physical and non-physical factors [22, 23]. However, the assessment of the measurement properties of AKPS and other patient-reported outcome measures for knee disorders is scarce, as shown by systematic reviews [1, 19, 20].
Therefore, considering this gap in the literature, the objective of the present study was to identify the best internal structure of the Brazilian version of the AKPS, comparing different instrument structures (structural validity) and correlating the scores of the versions (criterion validity) whose measurement provides an adequate indication of the dimensionality of the construct, attribute or factor being measured.
Methods
Study design and ethical aspects
A cross-sectional study to examine the structural validity of the AKPS. Data collection for the study was done using an online form (Google Forms, Mountain View, CA, USA)®. Participants were recruited through advertising in the university community, rehabilitation clinics, and gyms in São Luís (Maranhão, Northeastern Brazil). Social media advertising was also used. The study procedures were approved by the Institutional Research Ethics Committee (protocol number 3.995.226).
Sample size
The sampling was based on the recommendations of the COnsensus-based Standards for the selection of health Measurement INnstruments (COSMIN) [19]. Namely, seven times the number of items of the scale, provided that this value is not less than 100. In this sense, considering 13 items, the present study was composed of at least 100 individuals with PFP.
Eligibility criteria
We included only participants with PFP [2] and adopted the following exclusion criteria: history of trauma, fracture, or acute injury to the knee joint; knee surgery; use of analgesics in the past seven days; physiotherapy treatment for PFP in the past three months; and presence of other chronic pain. The diagnosis was made asynchronously and remotely.
Assessments
Participants reported whether they engaged in physical activity (yes or no), the number of times per week, the duration, and the type of exercise. Afterward, a bachelor of physical education (AP-S) evaluated the reports and classified them according to relevant recommendations for physical activity levels [24].
In addition to the Numerical Pain Rating Scale (NPRS), which assesses the mean pain intensity of the participants, and an initial assessment of personal, sociodemographic, anthropometric and clinical aspects (Table 2), we used the AKPS, a scale adapted to Brazilian Portuguese [4] with 13 items and different response possibilities for each item, corresponding to a specific score, as shown in Table 1. The final score of the scale is obtained by adding the score of each item, ranging from 0 to 100. Lower scores indicate greater disability.
Table 2.
Personal and anthropometric characteristics of the sample (n = 101)
| Variable | Mean (standard deviation) or n (%) |
|---|---|
| Age (years) | 31.77 (12.21) |
| Body mass (kg) | 71.07 (15.19) |
| Stature (m) | 1.65 (0.08) |
| Body mass index (kg/m2) | 25.75 (4.39) |
| Sex | |
| Male | 35 (34.7%) |
| Female | 66 (65.3%) |
| Education | |
| Incomplete primary education | 1 (1%) |
| Complete primary education | 1 (1%) |
| Incomplete secondary education | 1 (1%) |
| Complete secondary education | 12 (11.9%) |
| Incomplete higher education | 38 (37.6%) |
| Complete higher education | 26 (25.7%) |
| Incomplete post-graduate | 5 (5%) |
| Complete post-graduate | 17 (16.8%) |
| Lower limb dominance | |
| Right | 79 (78.2%) |
| Left | 13 (12.9%) |
| Both | 9 (8.9%) |
| Physical activity | |
| Yes | 65 (64.4%) |
| No | 36 (35.6%) |
Table 1.
Score of responses for each item on the Anterior Knee Pain Scale (AKPS)
| Item | Score |
|---|---|
| 1. Limp |
a) 5 b) 3 c) 0 |
| 2. Support |
a) 5 b) 3 c) 0 |
| 3. Walking |
a) 5 b) 3 c) 2 d) 0 |
| 4. Stairs |
a) 10 b) 8 c) 5 d) 0 |
| 5. Squatting |
a) 5 b) 4 c) 3 d) 2 e) 0 |
| 6. Running |
a) 10 b) 8 c) 6 d) 3 e) 0 |
| 7. Jumping |
a) 10 b) 7 c) 2 d) 0 |
| 8. Prolonged sitting with the knees flexed |
a) 10 b) 8 c) 6 d) 4 e) 0 |
| 9. Pain |
a) 10 b) 8 c) 6 d) 3 e) 0 |
| 10. Swelling |
a) 10 b) 8 c) 6 d) 4 e) 0 |
| 11. Abnormal painful kneecap (patellar) movements (subluxations)a |
a) 10 b) 6 c) 4 d) 2 e) 0 |
| 12. Atrophy of thigha |
a) 5 b) 3 c) 0 |
| 13. Flexion deficiency |
a) 5 b) 3 c) 0 |
aExcluded items
Therefore, participants of both sexes, sedentary or active, aged between 18 and 60 years, and with reports of PFP [2] for at least 3 months were included. In addition to the participant's verbal report, the NPRS was used to characterize the participant’s pain intensity: a unidimensional scale from 0 to 10 points, where 0 represents "no pain" and 10 represents "worst pain imaginable", with adequate validity for the Portuguese population [25].
Statistical analysis
We performed descriptive analysis and presented data as means and standard deviations or relative and absolute frequencies. We used confirmatory factor analysis (CFA) to identify the best structure of the AKPS through R Studio software (Boston, MA, USA)®, using the lavaan and semPlot packages. We used the implementation of a polychoric matrix and the robust diagonally weighted least squares (RDWLS) extraction method [26, 27]. We considered appropriate values of fit indices for the following cut-offs: chi-square/degrees of freedom (DF) < 3; comparative fit index (CFI) and Tucker-Lewis index (TLI) > 0.90; and root mean square error of approximation (RMSEA) < 0.08 [28, 29].
For model comparison, the structure with the lowest Akaike Information Criterion (AIC) and Sample Size Adjusted Bayesian Information Criterion (SABIC) values was considered most appropriate [30]. Factor loadings were considered adequate if they were greater than 0.40 [31]. Finally, we assessed validity criteria using the 13-item long version of the AKPS as the gold standard. Therefore, we used the Pearson correlation coefficient (r) to correlate the long and short versions (data with normal distribution according to the Kolmogorov–Smirnov test). A correlation coefficient > 0.70 was considered an appropriate cut-off point for criterion validity [32].
Results
The AKPS proposed in this study consists of 11 items with separate categories related to different levels of knee function. Categories within each item are scored and responses are summed to produce a global index where a score of 85 represents "no deficit" and a score of 0 represents "the highest possible deficit". Response scores for each item on the AKPS are shown in Table 1.
The majority of the sample consists of women (65.3%), young adults (~ 31 years old), overweight (body mass index > 25 kg/m2), with incomplete higher education (37.6%), and practitioners of physical activity (64.4%) (Table 2). Reading the pain characteristics (Table 3), we observed that the majority of the sample has pain in the sitting position (82.2%) or crouching (67.3%), mean pain duration greater than 39 months, and mean pain intensity greater than 4 points on the NPRS. Regarding the side of greater pain, there was a similar distribution between unilateral pain on the right (32.7%), on the left (36.6%), and bilateral (30.7%).
Table 3.
Sample pain characteristics
| Variables | Mean (standard deviation) or n (%) |
|---|---|
| Pain presence | |
| Sitting (yes) | 83 (82.2%) |
| Crouched (yes) | 68 (67.3%) |
| Running (yes) | 62 (61.4%) |
| Jumping (yes) | 62 (61.4%) |
| Up or down stairs (yes) | 66 (65.3%) |
| Time of pain (months) | 39.04 (50.38) |
| Knee in pain | |
| Right | 33 (32.7%) |
| Left | 37 (36.6%) |
| Both | 31 (30.7%) |
| AKPS | |
| 13 items (score, 0–100) | 76.00 (13.09) |
| 11 items (score, 0–85) | 63.74 (12.21) |
| NPRS at rest (score, 0–10) | 4.51 (1.99) |
AKPS Anterior Knee Pain Scale, NPRS Numerical Pain Rating Scale
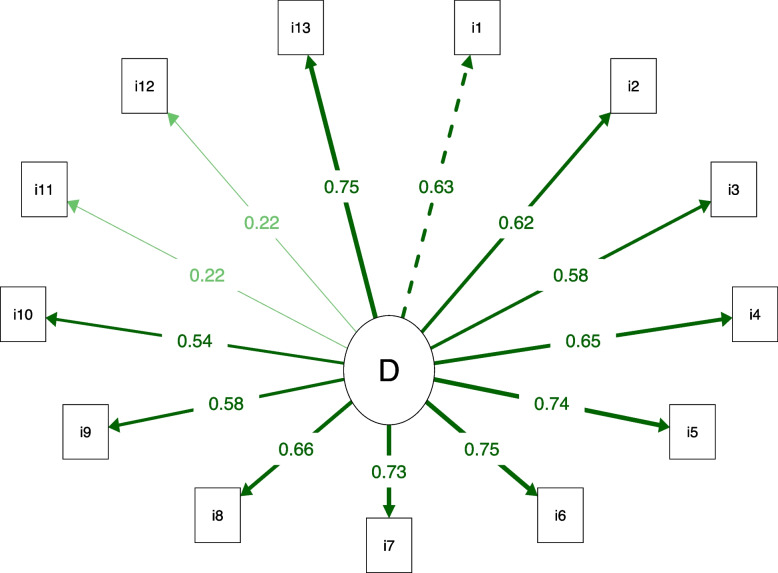
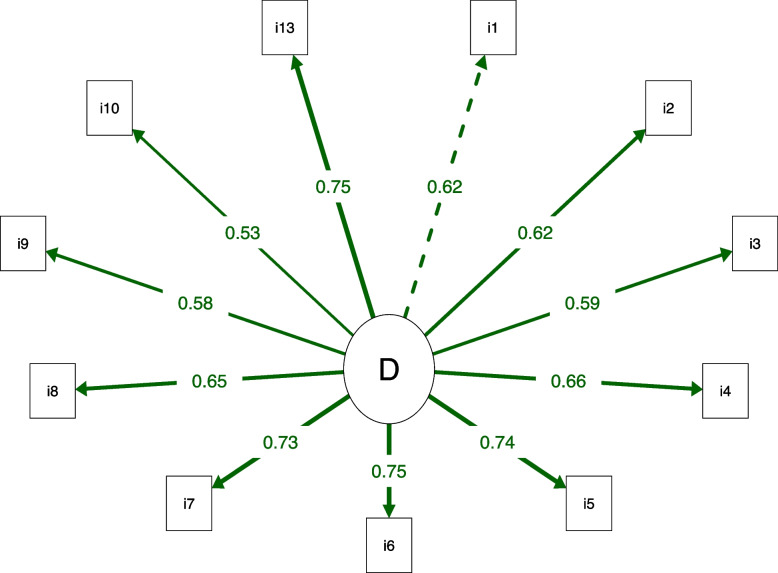
Regarding the internal structure of the AKPS (Table 4), the structure with 1 domain and 13 items showed adequate fit indices (Chi-square/GL < 3.00, TLI and CFI > 0.90, and RMSEA < 0.08). However, items 11 and 12 had a factorial load of less than 0.23, indicating that they were poorly explained by the domain (Fig. 1). Therefore, we excluded items 11 and 12 and found adequate fit indices (chi-square/GL < 3.00, TLI and CFI > 0.90, and RMSEA < 0.08) and lower AIC and SABIC values (Table 4), in addition to factor loadings greater than 0.40 (Fig. 2). Thus, the AKPS structure with 1 domain and 11 items is more appropriate (Additional file 1).
Table 4.
Confirmatory factor analysis of the versions of the Anterior Knee Pain Scale (AKPS)
| Structure | Chi-square/DF | CFI | TLI | RMSEA (90% CI) | AIC | SABIC |
|---|---|---|---|---|---|---|
| 13 items | 1.35 | 0.965 | 0.958 | 0.059 (0.019 to 0.089) | 4824.880 | 4810.754 |
| 11 items | 1.45 | 0.970 | 0.962 | 0.067 (0.024 to 0.101) | 4043.385 | 4031.432 |
DF Degree of freedom, CFI Comparative fit index, TLI Tucker-Lewis index, RMSEA Root mean square error of approximation, CI Confidence interval, AIC Akaike information criterion, SABIC Sample-size adjusted Bayesian information criterion
Fig. 1.
Path diagram of the Anterior Knee Pain Scale (AKPS) with 13 items. All factor loadings above 0.40, except items 11 and 12. The dotted line indicates the first factor item. The thicker the line, the greater the factor loading. D: Disability
Fig. 2.
Path diagram of the Anterior Knee Pain Scale (AKPS) with 11 items. All factor loadings above 0.40. The dotted line indicates the first factor item. The thicker the line, the greater the factor loading. D: Disability
In terms of criterion validity, the correlation between the 11-item and 13-item versions of the AKPS showed a correlation coefficient above the acceptability cutoff of 0.70 (r = 0.966, p-value < 0.001). Thus, even with the reduction of two items, the final scores remain highly correlated.
Discussion
This study showed that the 11-item AKPS, excluding items 11 and 12, is the version with the most adequate internal structure and satisfactorily correlated with the long version of the instrument. Although AKPS has been adapted for Turkish [5], Chinese [6], Persian [7], Spanish [8], Dutch [9], Thai [10], Greek [11], Arabic [12], Indonesian [13], Norwegian [14], Italian [15], German [16], and French [17], the authors did not analyze the internal structure of the AKPS. To date, this is the first validation study to examine the internal structure of the AKPS using factor analysis.
We emphasize that the clinical and scientific relevance of the AKPS is still limited because important measurement properties (e.g., reproducibility, responsiveness, and interpretability) of the AKPS still need to be investigated [1, 20]. Therefore, we suggest that further studies are needed to determine whether this instrument should be added to or removed from the scientific community.
This study has important limitations. First, according to the American College of Rheumatology [33], clinical symptoms related to degenerative lesions in the knee joint begin to appear at 38 years of age, with radiographic evidence becoming detectable at 40 years of age or older; thus, generalizability to the PFP population, which consists primarily of young individuals [34], may be compromised.
Second, although the results support the 11-item AKPS as the version with the most adequate internal structure and satisfactory correlation with the long version of the instrument, we know that the 11-item AKPS has adequate measurement properties only for the Brazilian population. Since this is the first validation study to examine the internal structure of the AKPS through factor analysis, we propose its reproducibility in other countries and its comparison with other instruments. Finally, the sample was predominantly female, and future studies should balance the number of participants by gender.
Conclusion
The 11-item AKPS (without items 11 and 12) is the version with the most adequate internal structure and correlates satisfactorily with the long version of the instrument.
Supplementary Information
Additional file 1. The 11-item Anterior Knee Pain Scale (AKPS). Anterior Knee Pain Scale (AKPS) com 11 items.
Acknowledgements
We thank all the participants who kindly volunteered for this research.
Abbreviations
- AIC
Akaike Information Criterion
- AKPS
Anterior Knee Pain Scale
- SABIC
Sample-Size Adjusted Bayesian Information Criterion
- CFA
Confirmatory Factor Analysis
- CFI
Comparative Fit Index
- COSMIN
COnsensus-based Standards for the selection of health Measurement INstruments
- DF
Degree of freedom
- NPRS
Numeric Pain Rating Scale
- PFP
Patellofemoral pain
- RDWLS
Robust Diagonally Weighted Least Squares
- R
Pearson correlation coefficient
- RMSEA
Root Mean Square Error of Approximation
- TLI
Tucker-Lewis index
Authors’ contributions
FBSJ, AVDF, DCCB, JRRJ, MBSG, ARS, CETC, AP-S, CAFPG, and FOP analyzed and interpreted of the data; All authors wrote the initial draft; All authors read and approved the final manuscript.
Funding
This work was partially supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), finance code 001. The funding source had no involvement in the study design, collection, analysis, interpretation of data, writing of the report, nor in the decision to submit the article for publication.
Availability of data and materials
The data and materials in this paper are available from the corresponding author on request.
Declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the Universidade Federal do Maranhão (protocol number 3.995.226), whose guidelines have been in accordance with the Declarations of Helsinki. All respondents participated in this study freely and signed an informed consent form.
Consent for publication
Not applicable.
Competing interests
AVDF, CAFPG, and AP-S are Associate Editors of the BMC Musculoskeletal Disorders. The other authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoglund LT, Scalzitti DA, Jayaseelan DJ, Bolgla LA, Wainwright SF. Patient-reported outcome measures for adults and adolescents with patellofemoral pain: a systematic review of construct validity, reliability, responsiveness, and interpretability using the COSMIN methodology. J Orthop Sports Phys Ther. 2023;53:1–20. doi: 10.2519/jospt.2023.11730. [DOI] [PubMed] [Google Scholar]
- 2.Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, et al. Patellofemoral pain. J Orthop Sports Phys Ther. 2019;49:CPG1–95. doi: 10.2519/jospt.2019.0302. [DOI] [PubMed] [Google Scholar]
- 3.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/S0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 4.Da Cunha RA, Pena Costa LO, Hespanhol Junior LC, Pires RS, Kujala UM, Lopes AD. Translation, cross-cultural adaptation, and clinimetric testing of instruments used to assess patients with patellofemoral pain syndrome in the Brazilian population. J Orthop Sports Phys Ther. 2013;43:332–339. doi: 10.2519/jospt.2013.4228. [DOI] [PubMed] [Google Scholar]
- 5.Kuru T, Dereli EE, Yaliman A. Validity of the Turkish version of the Kujala patellofemoral score in patellofemoral pain syndrome. Acta Orthop Traumatol Turc. 2010;44:152–156. doi: 10.3944/AOTT.2010.2252. [DOI] [PubMed] [Google Scholar]
- 6.Cheung RTH, Ngai SPC, Lam PL, Chiu JKW, Fung EYH. Chinese translation and validation of the Kujala scale for patients with patellofemoral pain. Disabil Rehabil. 2012;34:510–513. doi: 10.3109/09638288.2011.610494. [DOI] [PubMed] [Google Scholar]
- 7.Negahban H, Pouretezad M, Yazdi MJS, Sohani SM, Mazaheri M, Salavati M, et al. Persian translation and validation of the Kujala patellofemoral scale in patients with patellofemoral pain syndrome. Disabil Rehabil. 2012;34:2259–2263. doi: 10.3109/09638288.2012.683480. [DOI] [PubMed] [Google Scholar]
- 8.Gil-Gámez J, Pecos-Martín D, Kujala UM, Martínez-Merinero P, Montañez-Aguilera FJ, Romero-Franco N, et al. Validation and cultural adaptation of “Kujala score” in Spanish. Knee Surg Sports Traumatol Arthrosc. 2016;24:2845–2853. doi: 10.1007/s00167-015-3521-z. [DOI] [PubMed] [Google Scholar]
- 9.Ummels PEJ, Lenssen AF, Barendrecht M, Beurskens AJHM. Reliability of the Dutch translation of the Kujala patellofemoral score questionnaire. Physiother Res Int. 2017;22:1. [DOI] [PubMed]
- 10.Apivatgaroon A, Angthong C, Sanguanjit P, Chernchujit B. The validity and reliability of the Thai version of the Kujala score for patients with patellofemoral pain syndrome. Disabil Rehabil. 2016;38:2161–2164. doi: 10.3109/09638288.2015.1114035. [DOI] [PubMed] [Google Scholar]
- 11.Papadopoulos C, Constantinou A, Cheimonidou AZ, Stasinopoulos D. Greek cultural adaption and validation of the Kujala anterior knee pain scale in patients with patellofemoral pain syndrome. Disabil Rehabil. 2017;39:704–708. doi: 10.3109/09638288.2016.1161834. [DOI] [PubMed] [Google Scholar]
- 12.Alshehri A, Lohman E, Daher NS, Bahijri K, Alghamdi A, Altorairi N, et al. Cross-cultural adaptation and psychometric properties testing of the Arabic anterior knee pain scale. Med Sci Monit. 2017;23:1559–1582. doi: 10.12659/MSM.901264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mustamsir E, Phatama KY, Pratianto A, Pradana AS, Sukmajaya WP, Pandiangan RAH, et al. Validity and reliability of the Indonesian version of the Kujala score for patients with patellofemoral pain syndrome. Orthop J Sports Med. 2020;8:2325967120922943. doi: 10.1177/2325967120922943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hott A, Liavaag S, Juel NG, Brox JI, Ekeberg OM. The reliability, validity, interpretability, and responsiveness of the Norwegian version of the Anterior Knee Pain Scale in patellofemoral pain. Disabil Rehabil. 2021;43:1605–1614. doi: 10.1080/09638288.2019.1671499. [DOI] [PubMed] [Google Scholar]
- 15.Cerciello S, Corona K, Morris BJ, Visonà E, Maccauro G, Maffulli N, et al. Cross-cultural adaptation and validation of the Italian versions of the Kujala, Larsen, Lysholm and Fulkerson scores in patients with patellofemoral disorders. J Orthop Traumatol. 2018;19:1–7. doi: 10.1186/s10195-018-0508-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dammerer D, Liebensteiner MC, Kujala UM, Emmanuel K, Kopf S, Dirisamer F, et al. Validation of the German version of the Kujala score in patients with patellofemoral instability: a prospective multi-Centre study. Arch Orthop Trauma Surg. 2018;138:527–535. doi: 10.1007/s00402-018-2881-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buckinx F, Bornheim S, Remy G, Van Beveren J, Reginster J, Bruyère O, et al. French translation and validation of the “Anterior Knee Pain Scale” (AKPS) Disabil Rehabil. 2019;41:1089–1094. doi: 10.1080/09638288.2017.1419288. [DOI] [PubMed] [Google Scholar]
- 18.Aquino V da S, Falcon SFM, Neves LMT, Rodrigues RC, Sendín FA. Tradução e adaptação cultural para a língua portuguesa do questionário scoring of patellofemoral disorders: estudo preliminar. Acta Ortop Bras. 2011;19:273–9. doi: 10.1590/S1413-78522011000500002. [DOI] [Google Scholar]
- 19.Esculier JF, Roy JS, Bouyer LJ. Psychometric evidence of self-reported questionnaires for patellofemoral pain syndrome: a systematic review. Disabil Rehabil. 2013;35:2181–2190. doi: 10.3109/09638288.2013.774061. [DOI] [PubMed] [Google Scholar]
- 20.Hoglund LT, Scalzitti DA, Bolgla LA, Jayaseelan DJ, Wainwright SF. Patient-reported outcome measures for adults and adolescents with patellofemoral pain: a systematic review of content validity and feasibility using the COSMIN methodology. J Orthop Sports Phys Ther. 2023;53:23–39. doi: 10.2519/jospt.2022.11317. [DOI] [PubMed] [Google Scholar]
- 21.Barton CJ, De Oliveira SD, Morton S, Collins NJ, Rathleff MS, Vicenzino B, et al. REPORT-PFP: a consensus from the international patellofemoral research network to improve REPORTing of quantitative PatelloFemoral pain studies. Br J Sports Med. 2021;55:1135–1143. doi: 10.1136/bjsports-2020-103700. [DOI] [PubMed] [Google Scholar]
- 22.Botta AFB, de Cássia Pinto da Silva J, Dos Santos Lopes H, Boling MC, Briani RV, de Azevedo FM. Group-and sex-related differences in psychological and pain processing factors in people with and without patellofemoral pain: correlation with clinical outcomes. BMC Musculoskelet Disord. 2023;24:397. doi: 10.1186/s12891-023-06513-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakagawa TH, Serrão FV, Maciel CD, Powers CM. Hip and knee kinematics are associated with pain and self-reported functional status in males and females with patellofemoral pain. Int J Sports Med. 2013;34:997–1002. doi: 10.1055/s-0033-1334966. [DOI] [PubMed] [Google Scholar]
- 24.Maciel E da S, Silva BKR, Figueiredo FWDS, Pontes-Silva A, Quaresma FRP, Adami F, et al. Physical inactivity level and lipid profile in traditional communities in the Legal Amazon: a cross-sectional study : Physical inactivity level in the Legal Amazon. BMC Public Health. 2022;22:542. doi: 10.1186/s12889-022-12973-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152:2399–2404. doi: 10.1016/j.pain.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 26.Li CH. Confirmatory factor analysis with ordinal data: comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods. 2016;48:936–949. doi: 10.3758/s13428-015-0619-7. [DOI] [PubMed] [Google Scholar]
- 27.Ullman J. Structural equation modeling: reviewing the basics and moving forward. J Pers Assess. 2006;87:35–50. doi: 10.1207/s15327752jpa8701_03. [DOI] [PubMed] [Google Scholar]
- 28.Brown T. Confirmatory factor analysis for applied research. New York: Guilford Publications; 2006. [Google Scholar]
- 29.Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. MPR-Online. 2003;8:23–74. [Google Scholar]
- 30.Araujo GGC, Fidelis-de-Paula-Gomes CA, Pontes-Silva A, Pinheiro JS, Mendes LP, Gonçalves MC, et al. Brazilian version of the neck Bournemouth questionnaire does not have a well-defined internal structure in patients with chronic neck pain. Clin Rehabil. 2021;35:1773–1780. doi: 10.1177/02692155211024034. [DOI] [PubMed] [Google Scholar]
- 31.Barreto FS, Avila MA, Pinheiro JS, Almeida MQG, Ferreira C de SB, Fidelis-de-Paula-Gomes CA, et al. Less is more: five-item neck disability index to assess chronic neck pain patients in Brazil. Spine (Phila Pa 1976). 2021;46:E688–93. doi: 10.1097/BRS.0000000000003872. [DOI] [PubMed] [Google Scholar]
- 32.Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1147–1157. doi: 10.1007/s11136-018-1798-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bijlsma JWJ, Berenbaum F, Lafeber FPJG. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377:2115–2126. doi: 10.1016/S0140-6736(11)60243-2. [DOI] [PubMed] [Google Scholar]
- 34.Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, et al. Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PLoS ONE. 2018;13:e0190892. doi: 10.1371/journal.pone.0190892. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. The 11-item Anterior Knee Pain Scale (AKPS). Anterior Knee Pain Scale (AKPS) com 11 items.
Data Availability Statement
The data and materials in this paper are available from the corresponding author on request.