Abstract
Introduction
Non-communicable diseases (NCDs) are rising in low-income and middle-income countries, including Malawi. To inform policy-makers and planners on the preparedness of the Malawian healthcare system to respond to NCDs, we estimated NCD service readiness in publicly financed healthcare facilities in Malawi.
Methods
We analysed data from 564 facilities surveyed in the 2019 Harmonised Health Facility Assessment, including 512 primary healthcare (PHC) and 52 secondary and tertiary care (STC) facilities. To characterise service readiness, applying the law of minimum, we estimated the percentage of facilities with functional equipment and unexpired medicines required to provide NCD services. Further, we estimated permanently unavailable items to identify service readiness bottlenecks.
Results
Fewer than 40% of PHC facilities were ready to deliver services for each of the 14 NCDs analysed. Insulin and beclomethasone inhalers had the lowest stock levels at PHC facilities (6% and 8%, respectively). Only 17% of rural and community hospitals (RCHs) have liver and kidney diagnostics. STC facilities had varying service readiness, ranging from 27% for managing acute diabetes complications to 94% for chronic type 2 diabetes management. Only 38% of STC facilities were ready to manage chronic heart failure. Oral pain medicines were widely available at all levels of health facilities; however, only 22% of RCHs and 29% of STCs had injectable morphine or pethidine. Beclomethasone was never available at 74% of PHC and 29% of STC facilities.
Conclusion
Publicly financed facilities in Malawi are generally unprepared to provide NCD services, especially at the PHC level. Targeted investments in PHC can substantially improve service readiness for chronic NCD conditions in local communities and enable STC to respond to acute NCD complications and more complex NCD cases.
Keywords: health services accessibility, health equity, primary health care, Chronic Disease
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study quantified non-communicable disease (NCD) service readiness critical to achieving universal health coverage (UHC).
The study employed a census sample of publicly financed facilities.
Our analyses by facility and service type can help planners better target investments to lagging areas.
The analysis is limited to service-specific readiness and does not assess broader dimensions of health facility readiness, such as human resources and basic infrastructure.
The Harmonised Health Facility Assessment survey did not collect data on all the equipment and medicines required to manage NCDs and minor surgical conditions, constraining how service readiness is measured.
Introduction
Non-communicable diseases (NCDs) are responsible for 60% of early death and disability globally, and their growing burden in low-income and middle-income countries (LMICs) is particularly concerning. According to the WHO, 77% of the annual global NCD deaths occur in LMICs.1 In 2021, NCDs caused 41 million deaths worldwide, among which 29 million died of the four major conditions, including cardiovascular disease (CVD), cancer, chronic respiratory disease and diabetes. Several studies have reported low levels of NCD service readiness in LMICs.2 3
Located in Sub-Saharan Africa with an 18.6 million population, Malawi remains one of the world’s poorest countries, with a national gross domestic product of only US$645 per capita in 2022.4 Malawi suffers from a high burden of NCDs and their economic consequences, which affect the country’s overall economic development and lead to catastrophic health expenditures for many Malawians.5–7 As of 2019, NCDs accounted for 40% of mortality in Malawi, an increase from 30% in 2010.8
Characterising NCD service readiness in Malawi can help identify areas for investment for health. Several prior studies provisionally assessed the preparedness of the Malawian healthcare system. A 2018 study analysed data from the 2013–2015 Malawi Service Provision Assessment (SPA).3 Another SPA-based study assessed the preparedness of first-referral level hospitals in eight low-income countries, including Malawi, and estimated the percentages of facilities with complete minimal sets of equipment and unexpired medicines needed for thirteen NCD conditions.9 The results from these studies only presented assessments around 2015, when the SPA dataset was published.3 9 A recent study estimated screening, diagnosis, management and rehabilitation service readiness for NCDs based on a survey of 22 health facilities between 2019 and 2020.10 The study employed a limited sample, which warrants caution in extrapolating the findings to all health facilities in Malawi. Having up-to-date and comprehensive information regarding health facilities’ NCD service readiness in Malawi is essential for formulating evidence-informed health policies and judicious resource allocation. This study aims to fill a knowledge gap about service readiness for major NCD conditions using the most recent 2019 Harmonised Health Facility Assessment (HHFA) survey. This study has two main objectives. First, we estimate NCD service readiness by analysing the functionality of essential equipment and medicines to diagnose and treat common NCD conditions. Second, we identify potential bottlenecks that limit NCD service readiness.
Methods
Study setting
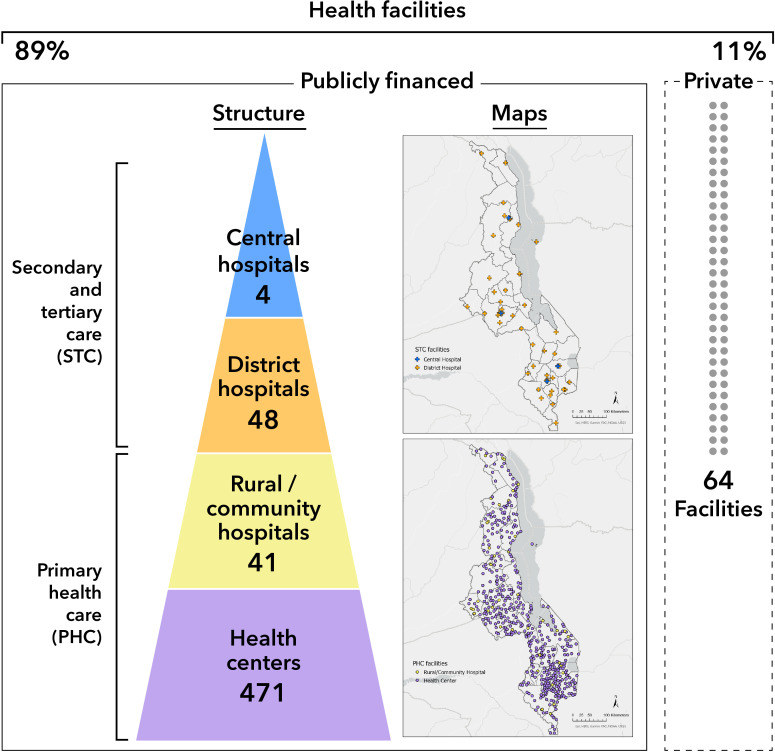
Healthcare in Malawi is delivered through public, private for-profit (PFP) and private not-for-profit (PNFP) facilities.11 The publicly financed sector is intended to be universally accessible without payment at the point of care, while PFP and PNFP facilities are not open to everyone and only represent 11% of the facilities in the Malawian health system.12 13 We focused our analysis on publicly financed facilities owned by the government and the Christian Health Association of Malawi (CHAM). The government is the leading healthcare provider in Malawi, while CHAM offers approximately 75% of healthcare services in remote and rural areas.14 15 Additionally, in 2006, the government sought to enhance healthcare access for underserved rural populations by partnering with CHAM through a service legal agreement, wherein CHAM provides healthcare services at no cost to users and is later reimbursed by the government for the incurred service expenses.15 The health system in Malawi is structured into primary, secondary and tertiary levels. Primary care at health centres and rural community hospitals (RCH) offers ambulatory and maternity services. Secondary care includes first-referral (district) hospitals, while central hospitals constitute tertiary care.11 Our analysis is disaggregated into primary healthcare (PHC) facilities (health centres and RCHs) and secondary and tertiary care (STC) facilities (district and central hospitals) (figure 1).
Figure 1.
Healthcare systems in Malawi. The figure presents the structure of the health system in Malawi and maps the health facilities in the country.
Data source
Our study analyses the 2019 HHFA, funded by the WHO, the World Bank and other collaborators. The HHFA is an update of the Service Availability and Readiness Assessment survey. The 2019 HHFA survey adopted a census sample approach, covering all functional health facilities in Malawi (n=1106). Of the surveyed health facilities, there were 101 hospitals, 492 health centres, and 513 dispensaries, clinics, and health posts. The HFFA assessed service readiness by asking whether the equipment and medicines required to provide different NCD services were available and functional.
Our analysis started with all functioning hospitals and health centres at the time of the survey. We removed one tertiary hospital, Zomba Mental Hospital, from our sample because it did not offer NCD services included in our analysis. According to the Administration of Health records, there were 485 registered health centres. However, only 471 of these were assessed by the HHFA. As a result, the 14 centres that were not surveyed were considered ‘non-functional.’ The final sample we included in our analysis (n=564) consisted of 512 PHC facilities (471 health centres and 41 rural/community hospitals) and 52 STC facilities (48 district hospitals and 4 central hospitals) (online supplemental appendix table 1). The category of district hospitals including large health centres functioning as quasi-district hospitals and first-referral-level CHAM hospitals. The spatial distribution of sampled facilities is displayed in figure 1.
bmjopen-2023-072511supp001.pdf (209KB, pdf)
Data analysis
This study focused on the readiness of basic equipment and medicines to diagnose and treat five acute and nine chronic NCD conditions. The conditions included in the analysis are acute and chronic asthma, hypertension, heart failure, rheumatic heart disease (RHD), diabetes, epilepsy, injuries, minor surgical conditions, and chronic pain (online supplemental appendix table 2). Assessing the service availability for these conditions aligns with recommendations from the Disease Control Priorities Project and related publications on priority interventions for NCDs.16–19 The conditions included in our study are also prioritised in the Malawi Ministry of Health National Action Plan for NCD Prevention and Management 2017–2022.20 We defined service readiness as having functional equipment and unexpired medicines in stock to provide the NCD services. We considered equipment functional if it was operational and present in general outpatient or minor surgical areas. Medicines stock was considered ‘functional’ if medicines were not expired, and appropriately stored in a manner that preserves the medicine’s potency.
Operational definitions and measures
Partners in the Ministry of Health advised us on the expected availability of NCD services at different levels of health facilities based on national guidelines and policies (online supplemental appendix table 2). We extracted the corresponding indicators from the HHFA survey for analysis and examined data missingness to refine our indicator for each service. We detail the conditions, items (medicines or equipment), indicators and related facility types in online supplemental appendix table 3 and present the missingness in online supplemental appendix table 4. When certain services were not expected to be offered at health centres, we only included rural/community hospital data for those services’ indicators.
Regarding missingness, the HHFA survey did not include questions on peak flow metres and micronebulisers required for asthma management in the outpatient setting. Therefore, we examined SPA data to understand how these missing variables might have affected the asthma readiness measure (online supplemental appendix table 5). For the variables with close to 100% missing data, we assumed that the item was not expected to be available at the facility level.
The HHFA survey classifies medicines or equipment as ‘available and functional’, ‘available but not functional’, ‘not available (at this time)’ or ‘never available’ at the facility. Accordingly, we calculated three indicators: (1) functionality, (2) service readiness and (3) permanent unavailability.
Functionality
Functionality refers to the presence of the functioning items (equipment and medicines stock) involved in providing a given NCD service.
Service readiness
For each facility, we estimated service readiness based on the functionality of the set of basic items required to provide a given NCD service.
Permanent unavailability
Permanent unavailability is when the item (medicine or equipment) is never present at the health facility, which is different not temporarily unavailable.
When a facility had all essential components functioning, it was labelled ‘ready’ to provide that service. Otherwise, the facility was labelled as ‘not ready.’
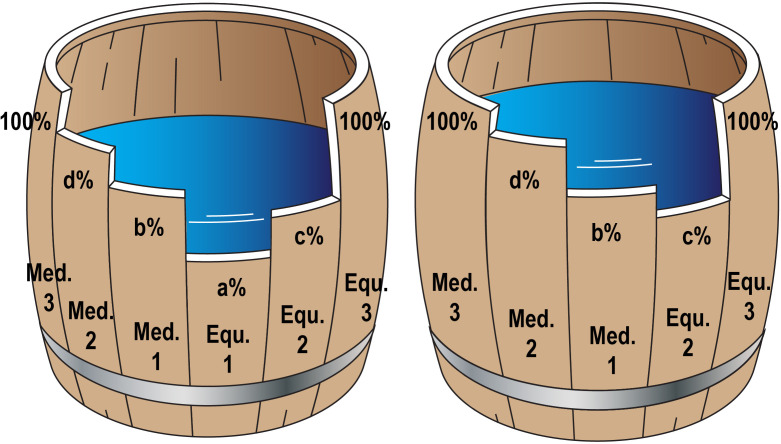
Applying Carl Sprengel’s Law of the Minimum, this study likens service readiness to an organism’s growth.21 We pinpoint the limiting factor impeding readiness, analogous to the lowest point in a barrel regulating water level (figure 2). This method guarantees a robust service readiness assessment, as absent data on non-limiting factors does not bias the results. However, if data on the limiting factor are missing, service readiness may be overestimated, as seen in the difference between the complete and incomplete barrels in figure 2.
Figure 2.
Required items and service readiness relation. The figure presents the relationship between service readiness (water level) and complementary items (bars). Med. = Medicines; Equ. = Equipment.
Patient and public involvement
None.
Results
We included 564 facilities in our analysis. There were 14 non-functioning health centres and 1 specialised tertiary hospital excluded from our analysis. Based on the Ministry of Health guidelines and missing data, we assumed that the following services were not expected to be delivered at health centres: chronic heart failure care, injectable pain care,chronic RHD care, treatment of acute asthma exacerbations, acute complications of diabetes, acute epilepsy (seizures) and injuries (online supplemental appendix table 2). Except for the aforementioned conditions at health centres, all other variables had less than 25% missing data (online supplemental appendix table 4).
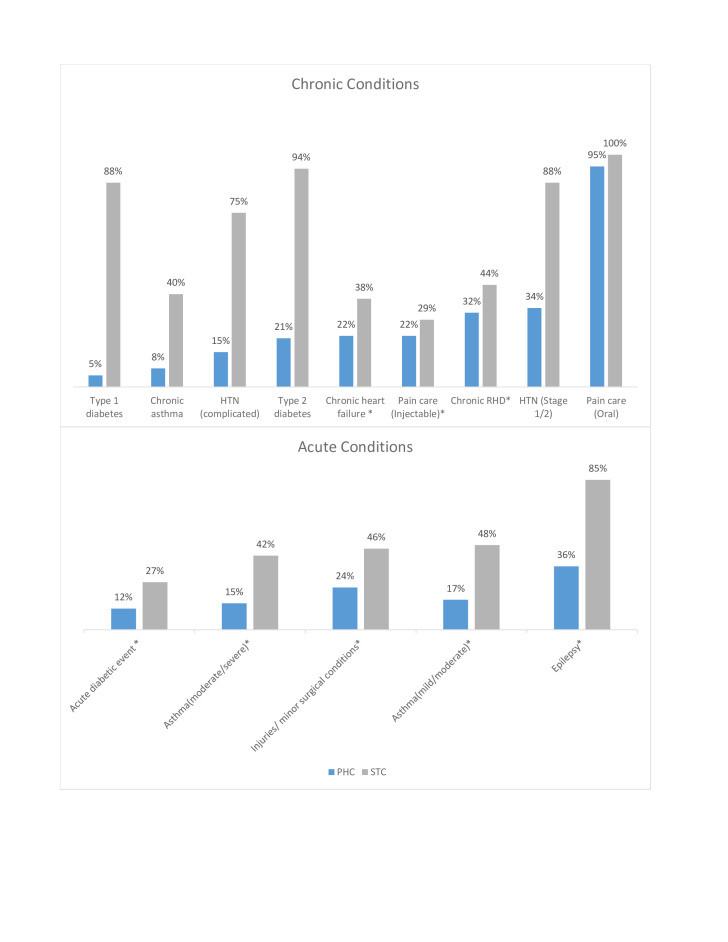
In figure 3, we compared the service readiness of PHC and STC facilities for chronic and acute NCD services. Overall, the readiness of STC facilities was higher than PHCs. We found that the service readiness was lower than 40% for NCD services at PHC facilities. Among the chronic NCD services, PHC facilities were least ready to provide services for type 1 diabetes and chronic asthma (5% and 8%, respectively). Among the acute services included in the analysis, RCHs were least ready to manage acute diabetic events (12%), acute asthma exacerbations (less than 20%) and injuries/acute minor surgical conditions (24%). PHCs had higher readiness scores for managing epilepsy (among RCHs) and stages 1 and 2 hypertension. STC facilities were near full readiness for type 2 diabetes (94%), type 1 diabetes (88%), stages 1 and 2 hypertension (88%), and epilepsy treatment (85%). However, STC facilities were least ready to provide care for acute diabetic events (27%) and had relatively lower readiness for managing chronic asthma, injectable pain care, chronic heart failure, RHD, moderate/severe acute asthma and injuries/acute minor surgical conditions.
Figure 3.
NCD service readiness of the Malawi health system by level. The figure presents the service readiness of chronic and acute NCD conditions, comparing the PHC level to the STC level. NCD, non-communicable disease; PHC, primary healthcare; STC, secondary and tertiary care. HTN, Hypertension; RHD, Rheumatic heart disease. *We only included rural/community hospital (RCH) data in analysis because these services were not expected to be offered at health centres.
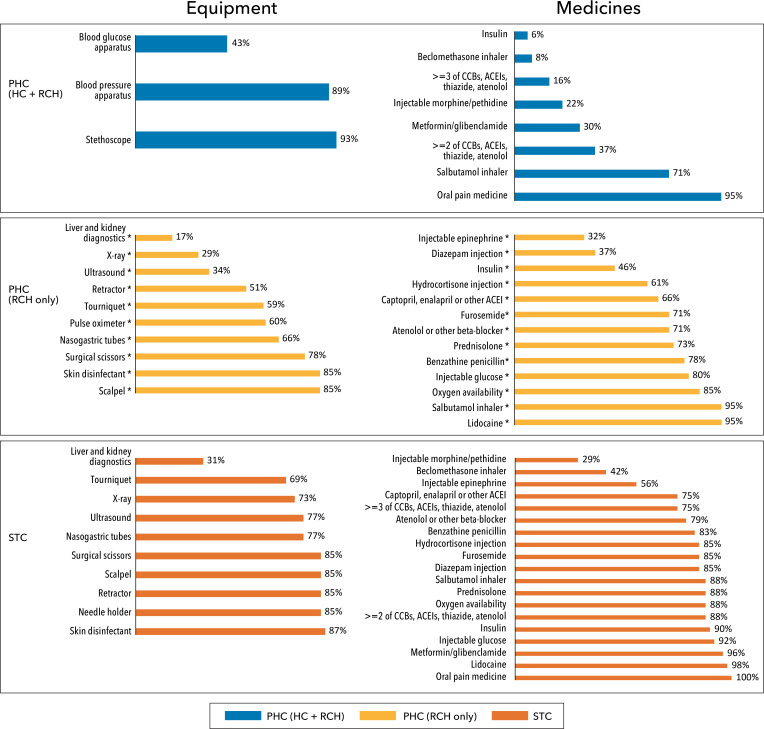
Equipment functionality and medicines stock
Figure 4 shows the functionality of equipment and unexpired medicines in stock required to provide the 14 NCD services we included in the analysis. Insulin for type 1 diabetes and beclomethasone inhalers for managing chronic asthma had the lowest stock at the PHC level (6% and 8%, respectively). Around 90% of STCs had insulin, but beclomethasone inhalers show low stock (42%) at STC facilities. Availability of antihypertensives is low in PHC facilities, with only 16% having ‘at least three or more antihypertensive classes’ of medication and only 37% having at least two, compared with 75% and 88% in STC facilities. The functionality of equipment was limited, especially in RCHs. For example, functional X-ray machines were found in only 29% of the RCHs, and ultrasound was functional at 34%.
Figure 4.
Equipment functionality and medicines stock. PHC, primary healthcare; HC, health centre; RCH, rural and community hospital; STC, secondary and tertiary care. CCB: Calcium channel blockers, ACEI: Angiotensin-converting enzyme inhibitors. *We only included rural/community hospital (RCH) data in analysis because these services were not expected to be offered at health centres.
Additionally, only 46% of RCHs stock insulin for managing acute diabetic events. However, RCHs and STC facilities had low level of functioning diagnostic tests required to manage acute complications of diabetes. Liver and kidney function tests were functional in only 17% of RCHs and 31% of STC facilities. We presented service readiness and item (equipment and medicines) functionality by facility level and by condition in Appendix Figure 1.
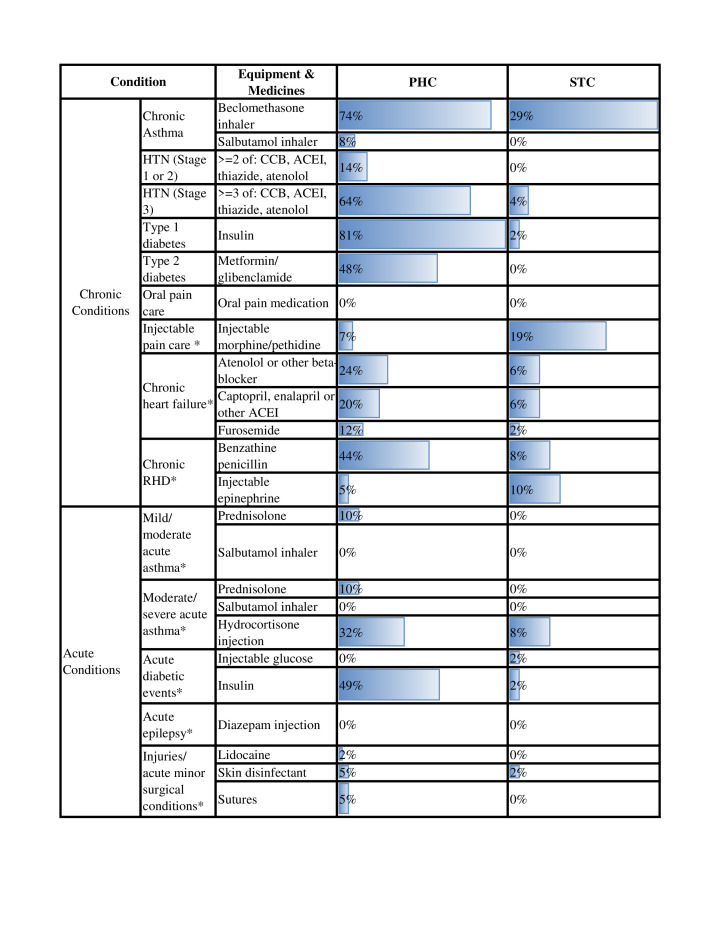
Permanently unavailable items
As shown in figure 5, beclomethasone was a ‘bottleneck item’ for chronic asthma service readiness at all levels since it was never available at 74% of PHC and 29% of STC facilities. Three or more antihypertensives were permanently unavailable in 64% of PHC facilities. Basic medicines for managing types 1 and 2 diabetes and acute complications of diabetes were bottleneck items for diabetes care readiness at PHC facilities. For chronic RHD management, 44% of RCH did not have benzathine penicillin. However, figure 5 also shows that there were items consistently in stock. These include oral pain medicines, salbutamol inhalers and diazepam injections, among others.
Figure 5.
Permanent unavailability by facility level. The figure presents the items that were never available, comparing the PHC and STC levels. PHC, primary healthcare; STC, secondary and tertiary care. CCB: Calcium channel blockers, ACEI: Angiotensin-converting enzyme inhibitors, HTN: Hypertension, RHD: Rheumatic heart disease. *We only included rural/community hospital (RCH) data in analysis because these services were not expected to be offered at health centres.
Discussion
Our analysis reveals significant gaps and disparities in the readiness of health facilities to respond to the growing burden of NCDs in Malawi. Fewer than 40% of PHCs are ready to diagnose and manage each of the 14 NCD services included in the analysis. Although STC facilities had higher readiness scores, 50% or fewer were not ready to diagnose and treat conditions like acute diabetes events, asthma, injuries/minor surgeries, chronic heart failure and, chronic RHD. PHCs were least ready with basic equipment and medicines to manage type 1 diabetes and chronic asthma (less than 10%) and RCHs were most ready to treat acute epilepsy (36%). PHCs had higher readiness to manage stages 1 and 2 hypertension (34%) but were less ready to treat complicated hypertension requiring three or more antihypertensive classes (15%).
Our findings are consistent with prior studies that illustrate an urgent need to invest more in health systems across Sub-Saharan Africa, including Malawi, to respond to NCDs.3 9 10 In line with previous analyses, we found notable gaps and limited readiness to manage NCDs, particularly in PHC facilities.3 10 22 Analysis of 2013–2015 SPA data for primary, secondary and tertiary level facilities in Malawi showed that only 37.7% of PHC facilities were ready to provide services for diabetes, chronic respiratory disease and CVD compared with 96% of STC facilities.3 Compared with the 2013–2015 SPA analysis of 43 first-referral level facilities, chronic asthma service readiness had increased to 40% in STC facilities compared with 5% in 2015.9 STC facility readiness to manage types 1 and 2 diabetes increased from around 40% to 88% for type 1 diabetes and 94% for type 2 diabetes. Readiness for managing hypertension stages 1 and 2 increased from 44% to 88%, while services for hypertension requiring three or more antihypertensive classes increased from 26% to 75%. Readiness of STC facilities increased from 12% to 38% for chronic heart failure and from 9% to 44% for chronic RHD, but there was no increase in readiness for managing acute complications of diabetes. Service readiness for acute epilepsy decreased from 95% to 85%.
These deficiencies in NCD services are not unique to Malawi. Studies analysing SPA data revealed low readiness of NCD services in countries like Tanzania, Singal and Ethiopia.3 9 Additional cross-sectional surveys to assess NCD services readiness revealed a similar pattern in Zambia but slightly higher readiness scores in Kenya, but the difference might stem from the dissimilarity in the service readiness calculation method.22 23 Also, a systematic analysis of survey data focused on diabetes in Sub-Saharan Africa reported low diagnostic capacity and supply of diabetes medicines in 14 African countries.24
Our analysis revealed a number of bottleneck items for NCD care in Malawi, including beclomethasone inhalers. Asthma management is not part of the NCD intervention package included in the essential health package of Malawi, and the Standard Treatment Guidelines for Malawi state that beclomethasone is only expected to be provided at the tertiary level.25 26 However, the WHO considers beclomethasone as an essential and cost-effective intervention for chronic asthma care that can be provided at PHC facilities.27 28 Our study suggests that the 2015 Standard Treatment Guidelines for Malawi could be revised to align with WHO recommendations, ensuring better access to asthma care in the community.
Addressing NCDs is a critical component of the health-related SDGs.19 The essential health package developed by the Ministry of Health specified that management of diabetes, hypertension and injuries be provided at primary and secondary facilities.26 Unfortunately, our study shows that most PHC facilities had low service readiness for these services and others. The Ministry of Health has acknowledged concerns about the suboptimal implementation of the essential health package due to inadequate resources, low awareness among stakeholders and the lack of clear financial mechanisms to ensure the provision of free-of-charge services at the point of care. To make progress on NCD management, the ministry will need to explore options for increasing healthcare financing in a manner that will benefit the entire range of healthcare needs, including NCDs.
This study has several limitations. Notably, our definition of service readiness is constrained by the methodology used in the HHFA survey, which focuses on a specific subset of equipment and medicines. This can introduce bias depending on the criteria and items used to define service readiness. For example, as the HHFA survey does not assess the availability of the nebulisers and peak flow metre in the outpatient departments, we did not include them as part of the essential equipment required for treating acute asthma. To address this, we analysed 2013–2015 SPA data to understand potential bias in our estimates. Data from the 2013–2015 SPA survey about the peak flow metre suggest that we may have overestimated the service readiness for acute asthma (online supplemental appendix table 5). While availability may have grown since 2015, if availability remains unchanged, it may be an alarming limiting factor for the overall readiness for acute asthma care. Second, the HHFA covers a limited range of health conditions and potential services for NCDs. The HFFA survey can be refined to enhance the scope and precision of indicators for a broader set of essential health services.
Additionally, the scope of our analysis is limited to service-specific readiness for a few NCDs and does not assess broader dimensions of health facility readiness, such as human resources and basic infrastructure. A study by Banda et al10 of a smaller number of health facilities assessed other dimensions not included in the HHFA survey, such as whether facilities kept reliable records for patients with NCD, supplemented with qualitative interviews to characterise the constraints.
Conclusion
Our analysis reveals that, despite progress since 2015, health facilities in Malawi have a long way to go to ensure universal access to NCD services. Despite being the first point of care and the ideal platform for early detection and long-term management of most NCDs, PHC facilities in Malawi have low NCD service readiness. While health centres and rural/community hospitals may not be expected to perform complete diagnostics or treatment for complicated conditions, primary care facilities are well positioned to provide basic services for common NCDs. PHC facilities urgently need additional investment to improve NCD service readiness. For other NCDs, a progressive approach to decentralising NCD care would start by building the capacity of RCH that, over time, could allow for extending a broader range of services to PHC facilities. Our list of permanently unavailable items provides a starting point to enhance the supply chain of medicines and equipment. The list can also inform the updating of guidelines to achieve better service readiness for particular conditions sensitive to these identified bottlenecks.
Supplementary Material
Acknowledgments
The authors thank the Ministry of Health in Malawi. We are thankful for the replication of results by Jiashuo Sun and graphic design by Lisa Fox, Meranda Wang, Jingning Wang and Ella Shi. We are also grateful for all the valuable comments from editors, reviewers, and Simon Ding. We are thankful for proofing by copyeditors, Aileen Liang, Owen Fei, Ella Shi, and Joshua Chen.
Footnotes
Twitter: @yanfangsu
Contributors: ZW, YC and SA led the literature review and wrote the first draft of the manuscript. PT and JCB provided data and supporting documents. ZW and LB analysed the data, and MM replicated the estimates. ZW and MM produced the tables. YS, YC and SA created the figures. MMC, PT, EW and DAW contributed to conceiving the study, refining the methods, and interpreting the results. DAW acquired funding for the research. YS led the study design, method development and result interpretation. YS is responsible for the overall content as the guarantor. YS accepts full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish. All authors have made significant intellectual or practical contributions, critically revised the manuscript and approved the final version of this paper.
Funding: This work was supported by the Bergen Centre for Ethics and Priority Setting (BCEPS) with support from the Trond Mohn Foundation and the Norwegian Agency for Development Cooperation (NORAD), project number 874789542.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
As this study was an analysis of an existing dataset, review and approval by an IRB was not required.
References
- 1.World Health Organization . Noncommunicable disease, Available: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- 2.Leslie HH, Spiegelman D, Zhou X, et al. Service readiness of health facilities in Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull World Health Organ 2017;95:738–48. 10.2471/BLT.17.191916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moucheraud C. Service readiness for Noncommunicable diseases was low in five countries in 2013–15. Health Aff (Millwood) 2018;37:1321–30. 10.1377/hlthaff.2018.0151 [DOI] [PubMed] [Google Scholar]
- 4.The World Bank . The World Bank data - Malawi. 2022. Available: https://data.worldbank.org/country/MW
- 5.Kim ET, Singh K, Speizer IS, et al. Availability of health facilities and utilization of maternal and newborn postnatal care in rural Malawi. BMC Pregnancy Childbirth 2019;19:503. 10.1186/s12884-019-2534-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macarayan EK, Gage AD, Doubova SV, et al. Assessment of quality of primary care with facility surveys: a descriptive analysis in ten low-income and middle-income countries. Lancet Glob Health 2018;6:e1176–85. 10.1016/S2214-109X(18)30440-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Q, Brenner S, Kalmus O, et al. The economic burden of chronic non-communicable diseases in rural Malawi: an observational study. BMC Health Serv Res 2016;16:457. 10.1186/s12913-016-1716-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wroe EB, Kalanga N, Dunbar EL, et al. Expanding access to non-communicable disease care in rural Malawi: outcomes from a retrospective cohort in an integrated NCD–HIV model. BMJ Open 2020;10:e036836. 10.1136/bmjopen-2020-036836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta N, Coates MM, Bekele A, et al. Availability of equipment and medications for non-communicable diseases and injuries at public first-referral level hospitals: a cross-sectional analysis of service provision assessments in eight low-income countries. BMJ Open 2020;10:e038842. 10.1136/bmjopen-2020-038842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banda CK, Hosseinipour MC, Kumwenda J, et al. Systems capacity to conduct non-communicable disease focused implementation research in the malawian health sector: A national needs assessment. In Review [Preprint] 2021. 10.21203/rs.3.rs-496152/v1 [DOI]
- 11.Ministry of Health, Malawi . Health care system. 2016. Available: https://www.health.gov.mw/index.php/2016-01-06-19-58-23/national-aids
- 12.Makwero MT. Delivery of primary health care in Malawi. Afr J Prim Health Care Fam Med 2018;10:e1–3. 10.4102/phcfm.v10i1.1799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . Malawi: Country Cooperation Startegy at a glance, . 2018Available: http://apps.who.int/iris/bitstream/handle/10665/136935/ccsbrief_mwi_en.pdf;jsessionid=6622A9B77AC48437784A63B1C127472E?sequence=1
- 14.Zeng W, Sun D, Mphwanthe H, et al. The impact and cost-effectiveness of user fee exemption by contracting out essential health package services in Malawi. BMJ Glob Health 2019;4:e001286. 10.1136/bmjgh-2018-001286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mchenga M, Manthalu G, Chingwanda A, et al. Developing Malawi’s universal health coverage index. Front Health Serv 2021;1:786186. 10.3389/frhs.2021.786186 Available: https://www.frontiersin.org/articles/10.3389/frhs.2021.786186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watkins D, Jamison D, Mills A, et al. Universal health coverage and essential packages of care. In: Jamison T, Gelband H, Horton S, et al., eds. Disease Control Priorities (third edition): Volume 9, Disease Control Priorities,edited by D. Washington, DC: World Bank, Available: https://dcp-3.org/chapter/2551/essential-universal-health-coverage [Google Scholar]
- 17.Prabhakaran D, Anand S, Watkins D, et al. Cardiovascular, respiratory, and related disorders: key messages from disease control priorities, 3RD edition. Lancet 2018;391:1224–36. 10.1016/S0140-6736(17)32471-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Watkins DA, Jamison DT, Mills A, et al. “Annex 3C. essential universal health coverage: interventions and platforms. supplementary material For:“Universal health coverage and essential packages of care.”” In: Jamison DT, Gelband H, Horton S, et al., eds. Disease Control Priorities: Improving Health and Reducing Poverty. Volume 9 of Disease Control Priorities, third edition. Washington, DC: World Bank, Available: http://dcp-3.org/sites/default/files/chapters/Annex%203C_Interventions%20in%20EUHC.pdf [Google Scholar]
- 19.DCP3 . Cardiovascular, Respiratory, and Related Disorders, Available: https://dcp-3.org/cvd
- 20.Ministry of Health, Malawi . National action plan for the prevention and management of non-communicable diseases in Malawi. 2017. Available: https://www.iccp-portal.org/system/files/plans/MWI_B3_s21_Malawi%20NCD%20Strategy_2018.pdf
- 21.Tang J, Riley WJ. Finding Liebig’s law of the minimum. Ecol Appl 2021;31:e02458. 10.1002/eap.2458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shiroya V, Shawa N, Matanje B, et al. Reorienting primary health care services for non-communicable diseases: A comparative preparedness assessment of two Healthcare networks in Malawi and Zambia. Int J Environ Res Public Health 2021;18:5044. 10.3390/ijerph18095044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ammoun R, Wami WM, Otieno P, et al. Readiness of health facilities to deliver non-communicable diseases services in Kenya: a national cross-sectional survey. BMC Health Serv Res 2022;22:985. 10.1186/s12913-022-08364-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nuche-Berenguer B, Kupfer LE. Readiness of sub-Saharan Africa Healthcare systems for the new pandemic, diabetes: A systematic review J Diabetes Res 2018;2018:3419290. 10.1155/2018/3419290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Health, Malawi . Malawi standard treatment guidelines essential medicines list 2015.Pdf. 2015. Available: https://extranet.who.int/ncdccs/Data/MWI_D1_Malawi-Standard-Treatment-Guidelines-Essential-Medicines-List-2015.pdf
- 26.Ministry of Health, Malawi . Health sector strategic plan II, towards universal health coverage. 2017. Available: https://www.health.gov.mw/downloads/
- 27.World Health Organization . 2008-2013 action plan for the global strategy for the prevention and control of Noncommunicable diseases: prevent and control cardiovascular diseases, cancers, chronic respiratory diseases and diabetes. plan action 2008-2013 pour Strat Mond Lutte Contre Mal non Transm. 2009.
- 28.World Health Organization . Prevention and control of noncommunicable diseases: guidelines for primary health care in low resource settings. Geneva: World Health Organization, 2012. Available: https://apps.who.int/iris/handle/10665/76173 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-072511supp001.pdf (209KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available.