Abstract
Objectives
To compare the contribution of physician associates (PAs) to the outcomes of emergency medicine consultations with that of foundation year 1 doctors-in-training (FY1s).
Design
A quantitative study using retrospective chart review of adult patients seen by PAs or FY1s from August 2018 to January 2020 using 16 months of anonymised clinical record data.
Setting
One emergency department (ED) in England.
Participants
The outcomes of 7405 patients seen by 11 PAs and 7 FY1s were recorded, with n=4580 PAs and n=2825 FY1s having complete records.
Outcome measures
The study aimed to evaluate wait times to consultation as the primary outcome. Secondary outcomes included length of stay (LOS), patients leaving without being seen (LWBS) and unplanned returns to the ED within 72 hours with the same complaint.
Results
PAs working in an ED in England treated patients mainly in Majors and Resus and saw more patients out of hours compared with FY1s. Following adjustments for confounding factors, there was no significant difference in wait times to consultation between those PAs or FY1s patients (116 min vs 109 min, respectively, p=0.84). Patients seen by PAs versus FY1s had a significantly longer LOS (52 min); 237 min vs 185 min, p<0.001 (95% CI 45.03 to 59.67). LWBS rates (n=89; 1.94% for PAs vs n=34; 1.2% for FY1s) showed no significant difference (p=0.073). Unplanned reattendance rates patients within 72 hours with the same presenting complaint showed no difference between PAs and FY1s (n=261 (5.70%) vs n=128 (4.58%), respectively, p=0.167).
Conclusion
PAs working in an ED in England managed patients with a range of conditions with a similar level of impact on three emergency medicine outcome measures as FY1s (wait times to consultation, numbers of patients LWBS or returning within 72 hours with the same presenting complaint). However, patients seen by PAs had a longer LOS.
Keywords: Patients, ACCIDENT & EMERGENCY MEDICINE, Health economics, Health Workforce
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study provides a well-powered quantitative comparative analysis of the outcomes of patient care by physician associates and foundation year 1 doctors-in-training in a busy emergency department in England.
We believe this to be the first empirical study of the outcomes of care provided by UK-trained physician associates and foundation year 1 doctors-in-training in the emergency department.
Only one UK emergency department was assessed in this study.
The hospital triage system was not recorded electronically during the times of the study which impaired the study’s ability to fully describe the case mix to its full capacity.
A review of a sample of each of the clinician’s case notes involved in this study could have provided some insight as to whether other factors such as having to obtain a clinician to order investigations such as an X-ray or level of documentation had any influence on the outcome data.
Introduction
The UK National Health Services (NHS) is currently under pressure with financial reductions, staff shortages and a growing ageing population.1 As part of the NHS People Plan, new healthcare professional roles such as medical associate professions are being used to try to address these challenges by supplementing the existing medical staff.2 This is to try and ensure continued effective and safe delivery of patient care.3 One such role is that of the physician associate (PA), formerly known as the physician assistant in the UK. PAs are postgraduates who have as a minimum completed an undergraduate degree in a science related subject before embarking on a 2-year full-time medical model diploma or master’s degree in PA studies.4 Once completed, the PA is certified to work as a generalist; taking histories, formulating diagnoses post investigations and creating management plans with the supervision of a senior doctor (registrar level 4 and above or consultant in secondary care or general practitioner in primary care).5 PAs have been present in the USA for around 40 years with over 100 000 qualified PAs.6 However, the first cohort of PAs in the UK graduated more recently in 2009 and there are currently ~4000 PAs registered on the voluntary managed register held by the faculty of PA (FPA) at the Royal College of Physicians.7
In most states of the USA, Netherlands, Ghana, Australia and Canada; PAs can prescribe.8 Since PAs in the UK are not yet included under a state regulatory framework such as the General Medical Council (GMC) they are not currently legal prescribers of medication or able to order investigations using ionising radiation. Following a consultation, the government announced in October 2018 that they recognise the importance of regulation for PAs in the UK.9 In 2019, the GMC was proposed as the regulatory body for the profession.10 In 2021, the GMC published future professional standards for PAs.11 Regulation of PAs with the GMC was due in 2022; however, this has been delayed (with plans for 2024) due to the pressures associated with COVID-19.12
Once regulated, PAs will remain dependent practitioners but accountable for their own actions.13
The emergency department (ED) has been shown to be particularly prone to increasing waiting times, length of stay (LOS) and departmental ‘gridlock’.14 Wait times, LOS, reattendance rates and those leaving without being seen (LWBS) are NHS clinical quality indicators for EDs in England.15 The NHS long-term plan has a focus on ensuring patients receive the care needed efficiently and also to relieve the current pressures on the emergency care system.16 PAs have been deployed within the ED in various countries and there has been an increase of PAs working within UK EDs.17 Despite the growth of ED PAs, there is limited published evidence regarding the impact of their role in an English ED setting. In this context, the aim of this study was to investigate the contribution of PAs to the outcomes of emergency medicine consultations compared with that of foundation year 1 (FY1) doctors-in-training in an English hospital ED. A comparison of the wait times to consultation, LOS, the number of patients LWBS and the number of patients returning to the ED unplanned within 72 hours with the same presenting complaint between PAs and FY1 in emergency medicine consultations was performed.
Methods
Study design
Following NHS Research Ethical Committee approval, a quantitative observational retrospective chart review of adult patient consultations (from 1 August 2018 to 1 January 2020) by PAs compared with FY1 doctors-in-training was conducted.
Population and sampling
The trust, one of the largest employers of PAs in the country, operates two sites. One consultant-led, 24-hour ED site of the trust with full resuscitation facilities (‘type 1’) was investigated. The annual attendance to the hospital is ~70 000 adult patients. The site is a university district general hospital. The hospital had been recruited as part of a larger study investigating the perception of PAs. FY1 doctors-in-training were selected as the comparator for PAs, as PAs are offered as part of a supplement solution to the junior medical workforce shortages18 and the most junior doctors working in the UK ED at the time were FY1s who also were just introduced to the department at the start of the study period. While FY1s can prescribe some medication and order investigations using ionising radiation; they still have a level of dependence on senior clinicians, for example, for discharge planning and supervision as PAs. FY1s are partially, not fully registered with the GMC until they have successfully completed their first-year post qualification. Table 1 outlines the general scope of working of PAs and FY1s in UK EDs.19 Consultations in the first 2 weeks of an FY1 ED rotation and that of a PA newly starting the ED were omitted prior to being sent for analysis to allow for settling in. Results from three areas of the ED were analysed; the urgent treatment centre (UTC) where more stable, lower acuity patients were seen; Majors where higher acuity less stable patients were seen and the Resus area where higher unstable patients were often seen. The clinician either gets a choice as to which area of the ED they which to work in during their shift or are directed to a specific area by the emergency physician in charge (EPIC).
Table 1.
The general scope of working of physician associates and foundation year 1 doctors in UK ED
| Foundation year 1 doctors-in-training | Physician associates |
| 4–5 year primary undergraduate or postgraduate medical degree | 2-year postgraduate MSc or Pgdip in Physician Associate Studies and an undergraduate degree in health or life sciences |
| Partially registered by the GMC | Not yet regulated by the GMC, due end of 2024 |
| Rotating staff members (4 monthly) | Permanent members of staff |
| Restricted prescribing of medication; no chemotherapeutic agent, immunosuppressant, cytotoxic or controlled drugs. Also, must not prescribe on FP10 forms | Not currently able to prescribe any medication |
| Able to order investigations using ionising radiation | Not currently able to order investigations using ionising radiation |
| Must not work in specialised areas of the ED, that is, paediatrics or Resus without supervision | Able to see undifferentiated cases including Paediatric and Resus patients independently (post 6 months supernumerary period), then discuss with a senior |
| Must not attempt to interpret ECGs independently | If comfortable, can sign off ECG’s independently after working in the ED for 1 year |
| Every patient should be ‘signed off’ by a senior doctor (ST4 or above) before discharge | Every patient should be ‘signed off’ by a senior doctor (ST4 or above) before discharge |
| Must not be rostered to shifts overnight or at other times in the ED when consultants are not physically present | After working in the ED for 12 months can be rostered to night shifts; can work when consultants are not physically present but ST4 or above doctors are physically present after a month supernumerary period. |
Supporting information from 12 19.
ED, emergency department; FP10, English National Health Service Prescription Form; GMC, General Medical Council; ST4, Specialist registrar in fourth year of training.
Selection of outcomes
The primary outcome was wait times to consultation. The secondary outcomes were LOS, those LWBS and the number of patients reattending the department within 72 hours with the same presenting complaint (unplanned).
Patient and public involvement
Healthwatch facilitated a patient and public involvement (PPI) group that provided valuable feedback on the information sheets and consent forms used for a related study. Their comments included a recommendation to investigate ‘PAs efficiencies within the ED’, which informed the design of the current study and ensured wait time to consultation was included as an outcome measure. As part of dissemination activities, the study findings will be shared with the PPI group, Healthwatch media production team and the host hospital’s communications team.
Chart review
For a period of 16 months’ (four standard durations of ED placement for FY1 doctors-in-training in the UK), anonymised, routinely collected electronic records of all patients attended by a PA or FY1 doctor-in-training in the adult ED, provided in Microsoft Excel by the hospital information team at the trust, using queries based on staff job role, dates and requested data items. Hospital staff extracted the required data items (online supplemental material 1)—age, gender, actual time seen, day of the week seen, area of department (UTC, Majors or Resus), presenting complaint, outcome (discharged home or referred to a specialty), LOS (from check-in to discharge, in minutes), wait time to consultation (time from triage to be seen by the clinician; primary outcome), those LWBS and unplanned reattendance within 72 hours with the same presenting complaint. No data linkage was required. The original data set was accessed to identify any patients who appeared more than once in the dataset and if any further data cleaning was required. Data were cleaned by NK.
bmjopen-2023-078511supp001.pdf (37.3KB, pdf)
Power calculation
A sample size calculation for one of the outcome measures (number of reattendances within 72 hours with the same presenting complaint) was performed. This was based on rate of 18.3% (the highest of two rates for nurse practitioners substituting for physicians (at 28 days).20 21 Aiming to find a relative difference of 50%, in a non-inferiority hypothesis, we required 284 patients in each group (calculation from Stata V.11.1 software) to compare 18.3%–27.4% unplanned reconsultations, with conventional 80% power at 5% significance. As with the Halter et al study, an extra 20 participants in each group will allow for adjustment for case mix.22 Therefore, a minimum of 304 patients in total in each group will be required to achieve the said power.
Analysis
SPSS was used for the analysis of the data. The characteristics of patients treated by PAs and FY1 doctors-in-training, LWBS and reattendance data were compared using χ2 tests. Independent t-tests were performed to compare the wait times, LOS and those reattending with the same presenting complaint within 72 hours. Linear mixed models containing a mixture of fixed (confounding factors) and random effects (ie, nesting of individual clinicians since patients seen by the same clinician are likely to be correlated) were performed to obtain the outcomes. The adjustments were for patient age, the time of day the patient was seen, the area of the department the patient was seen in (UTC, Majors or Resus) and disposal (admitted or discharged). Those who LWBS and those who were admitted were excluded from the LOS adjusted analysis because they could affect the results due to those LWBS leaving the department prematurely and those who are being admitted would have the additional wait for a bed, timings of which are dependent on the hospital’s bed capacity at that time.
Results
In the four 16-week rotation periods studied, a total of 7405 patients were seen by 11 PAs and 7 FY1s in the adult ED. All the outcomes were available for all the cases (no missing or incomplete data) and were collected at the site for analysis.
The characteristics of the patients included within the study are shown in table 2.
Table 2.
Characteristics of the chart review sample
| Characteristic | PA n=4580 |
FY1 doctor n=2825 |
Total n=7405 |
P value |
| n (%) | n (%) | n | ||
| Age (years) | ||||
| <18 | 60 (1.3%) | 52 (1.8%) | 112 | <0.001 |
| 18–44 | 1529 (33.4%) | 1261 (44.6%) | 2790 | |
| 45–65 | 1168 (25.5%) | 735 (29.1%) | 1903 | |
| 65+ | 1823 (39.8%) | 777 (27.5%) | 2600 | |
| Gender | ||||
| Male | 1828 (39.9%) | 1225 (43.4%) | 3053 | 0.003 |
| Female | 2752 (60.1%) | 1600 (56.6%) | 4352 | |
| Time of day seen | ||||
| 0800–1600 | 2682 (58.6%) | 2311 (81.8%) | 4993 | <0.001 |
| 1600–0000 | 1897 (41.4%) | 514 (18.2%) | 2411 | |
| Day of week seen | ||||
| Weekday (Monday–Friday) | 3354 (73.2%) | 2620 (92.7%) | 5974 | <0.001 |
| Weekend (Saturday/Sunday) | 1226 (26.8%) | 205 (7.3%) | 1431 | |
| Department | ||||
| UTC | 529 (11.6%) | 1563 (55.3%) | 2092 | 0.000 |
| Majors | 3947 (86.2%) | 1210 (42.8%) | 5157 | |
| Resus | 104 (2.3%) | 52 (1.8%) | 156 | |
| Disposal | ||||
| Admitted | 2011 (43.9%) | 540 (19.1%) | 2551 | <0.001 |
| Discharged | 2569 (56.1%) | 2285 (80.9%) | 4854 | |
FY1, foundation year 1 doctor in training; PA, physician associates; UTC, urgent treatment centre.
Patient age groups
FY1s saw significantly more patients aged between 18 and 44 years n=1261 (44.6%) vs PAs n=1529 (33.4%), p<0.001. PAs saw significantly more patients aged 65 years and over compare to FY1s; n=1823 (39.8%) vs n=777 (27.5%), respectively.
Patient gender
There were also significant differences found between the gender most seen between the two clinicians.
Actual time seen and day of the week
FY1s saw most of their patients between 08:00 and 16:00 hours, n=2311 (81.8%) and less after hours 1600-midnight. PAs saw 41.4% of their patients between 16:00 and midnight, but also saw more of their patients between 08:00 and 16:00 hours; n=2682 (58.6%), p<0.001 (figure 1). 92.7% of FY1 consultations took place on a weekday vs 73.2% of PA consultations. PAs saw more patients on the weekend than patients seen by FY1s (26.8% vs 7.3%), p<0.001.
Figure 1.
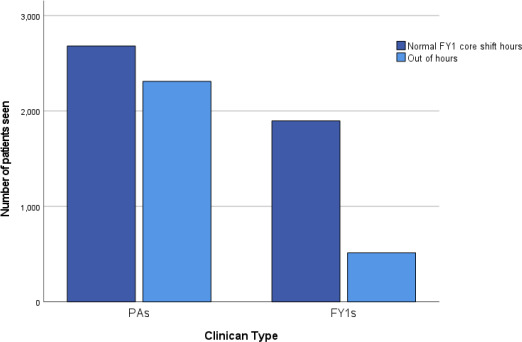
Comparison of the time-of-day patients were seen by physician associates (PAs) versus foundation year 1 (FY1) doctors-in-training in the adult ED. FY1 core shift hours 08:00–16:00 vs outside of normal hours 16:00–08:00 by PAs vs FY1 doctors-in-training (FY1s) in the ED. Night shifts 2200–0800 were covered ad hoc as locum by FY1s. ED, emergency department.
Area of department where the patient was seen
FY1s saw significantly more UTC patients in comparison to that seen by PAs; n=1563 (55.3%) vs n=529 (11.6%), p=0.000, respectively. PAs tended to see higher acuity patients in the Majors or Resus areas n=3947 (86.2%) compared with those seen by FY1s n=1210 (42.8%), p<0.000. Most of the patients seen by PAs were admitted n=2011 (43.9%) vs n=540 (19.1%), p<0.001 as opposed to being discharged; reflecting the area of the department the PAs mostly saw patients from; Majors and Resus.
Outcomes of patients
The majority of patients seen by FY1s were discharged (81%) while the remainder were admitted. For PAs, 56% of patients were discharged with the remainder being admitted. There were no ED patient deaths in either group.
The presenting complaints were grouped into 14 different categories listed in table 3. When comparing the presenting complaints seen by PAs, FY1s saw significantly higher proportion of dermatology, ENT and those generally unwell cases. PAs saw a significantly higher proportion of cardiology, gastroenterology, gynaecology, haematology, mental health, musculoskeletal (MSK), neurology, respiratory, urology and vascular cases, compared with the FY1s. There was no significant difference between the number of ophthalmology cases seen between the two clinicians.
Table 3.
Presenting complaints categories of patients seen by PAs versus FY1s
| Categories | PA | FY1 | Total | P value |
| n (%) | n (%) | |||
| Cardiology* | 413 (9) | 134 (4.7) | 547 | <0.001 |
| Dermatology* | 257 (5.6) | 261 (9.2) | 518 | <0.001 |
| ENT* | 133 (2.9) | 177 (6.3) | 310 | <0.001 |
| Gastroenterology* | 754 (16.5) | 354 (12.5) | 1108 | <0.001 |
| Generally unwell* | 130 (2.8) | 172 (6.1) | 302 | <0.001 |
| Gynaecology* | 183 (4) | 65 (2.3) | 248 | <0.001 |
| Haematology | 56 (1.2) | 23 (0.8) | 79 | <0.001 |
| Mental health* | 196 (4.3) | 73 (2.6) | 269 | <0.001 |
| MSK* | 921 (20) | 897 (31.8) | 1818 | <0.001 |
| Neurology* | 469 (10.3) | 196 (6.9) | 666 | <0.001 |
| Ophthalmology | 26 (0.6) | 14 (0.5) | 40 | 0.78 |
| Respiratory* | 524 (11.4) | 215 (7.6) | 739 | <0.001 |
| Urology* | 473 (10.3) | 230 (8.1) | 703 | <0.001 |
| Vascular | 44 (1) | 14 (0.5) | 58 | <0.001 |
| Total | 4580 | 2825 | 7405 |
*Significant finding p≤0.05.
ENT, ear, nose and throat; FY1, foundation year 1 doctor in training; MSK, musculoskeletal; PA, physician associate.
Wait times to consultation
Patient wait times to consultation between PAs and FY1s
The overall wait time to consultation for any patient to be seen by a PA or FY1 during the study period was 124 min. The unadjusted wait time for patients to see a PA was 132 min vs 105 min to be seen by an FY1 (p<0.001); 26.7 min longer. When adjusting for the department the patient was seen in (UTC, Majors or Resus), age (<18, 18–44, 45–65 or 65+), gender, actual time and day of the week seen and individual clinician; the significant difference in wait times disappeared; (p=0.84); table 4.
Table 4.
Patient wait times to consultation, length of stay, those leaving without being seen and those returning within 72 hours with the same presenting complaint of those seen by Physician Associates vs Foundation Year one doctors in training (whole set, unadjusted and adjusted)
| Clinician | N | Unadjusted mean | Unadjusted 95% CI | P value | Adjusted mean | N | 95% CI | P value | |
| Wait time to consultation | PA | 4580 | 132.11 | 23.42 to 29.96 | <0.001 | 116.15 | 4580 | 27.82 to 204.47 | 0.84 |
| FY1 | 2825 | 105.41 | 109.00 | 2825 | 20.66 to 197.35 | ||||
| LOS | PA | 4580 | 266.33 | 70.027 to 84.25 | <0.001 | 258.25 | 4491 | 251.59 to 264.90 | <0.001 |
| FY1 | 2825 | 189.19 | 198.0 | 2711 | 190.360 to 205.63 | ||||
| LWBS | PA | 89 (1.98%) | 0.022 | 0.001 to 0.013 | <0.001 | 0.022 | 89 | 0.013 to 0.031 | 0.073 |
| FY1 | 34 (1.2%) | 0.013 | 0.002 to 0.013 | 0.015 | 34 | 0.006 to 0.025 | |||
| Reattendance within 72 hours | PA | 261 (5.7%) | 0.06 | 0.001 to 0.022 | <0.001 | 0.085 | 261 | 0.061 to 0.109 | 0.167 |
| FY1 | 128 (4.6%) | 0.05 | 0.001 to 0.022 | 0.076 | 128 | 0.051 to 0.102 |
Adjustments made for; patient age (<18, 18-44, 45-64 or 65+years), patient gender, individual clinician, time and day of week seen and area of department seen in UTC, Majors or Resus and individual clinician.
FY1, Foundation Year One Doctor- In -Training; LOS, Length of Stay; LWBS, Leaving without being seen; PA, Physician Associate.
Length of stay
Resus patients had the longest LOS (326 min) followed by patient’s seen in Majors (262 min) and UTC patients had the lowest LOS (173 min).
The overall LOS for any patient to be seen by a PA or FY1 during the study period was 228 min. The unadjusted LOS for patients seen by a PA was 266 min vs 189 min to be seen by an FY1 (p=0.001); 77.14 min longer (see table 4). When adjusting for the department the patient was seen in (UTC, Majors or Resus), patient age (<18, 18–44, 45–65 or 65+years), patient gender, actual time seen and day of the week seen, individual clinician, omitting those who were admitted and those LWBS; patients were in the department for a significantly longer time (52.35 min) if seen by a PA (p<0.001).
Unplanned reattendance within 72 hours with the same presenting complaint
261 (5.7%) of patients seen by PA reattended the department within 72 hours with the same presenting complaint. 128 (4.6%) of patients seen by FY1s returned within 72 hours with the same presenting complaint. The adjusted mixed linear model (adjusting for the department the patient was seen in (UTC, Majors or Resus), patient age (<18, 18–44, 45–65 or 65+ years), patient gender, actual time and day of the week seen, individual clinician and if the patient LWBS) found no significant difference in the patient reattendance rates between the two clinicians; p=0.167 (table 4).
Left without being seen
Out of the patients waiting to see a PA, 89 (1.98%) left the department without being seen. This is compared to 34 (1.20%) of patients waiting to be seen by FY1 doctors-in-training. However, when taking into account confounding factors such as the department the patient was seen in (UTC, Majors or Resus), patient age (<18; 18–44; 45–65 or 65+ years), patient gender, individual clinician, actual time and day of the week seen; this difference was not statistically significant (p=0.073) (see table 4).
Discussion
Summary of findings
Our study presents evidence from one English ED and has demonstrated no difference in wait time to consultation, LWBS or reattendance rates within 72 hours, but a significant difference in LOS between patients seen by PAs and FY1 doctors-in-training. We report those patients seen by a PA had a longer average LOS in the ED than those seen by FY1s even when statistical adjustments were made for patient age, time and day of the week and area of the department the patient was seen in, omitting those LWBS and those who were admitted. PAs saw more patients in Majors and Resus while FY1s saw more UTC patients.
How this study is similar or different from prior studies
We believe this to be the first empirical study of the quantitative impact on ED metrics provided by UK-trained PAs in the ED in comparison to FY1 doctors-in-training. The primary outcome of wait times to consultation was reported to be not significantly different in patients waiting to be seen by PA compared with an FY1 doctor in training. This finding was similar to that reported in other studies abroad.23–25 LOS was shown to be significantly increased in those patients seen by a PA compared with those seen by an FY1-doctor in training. This was comparable to a study comparing ED PAs to ED physicians. Here, the overall LOS was increased by 8 min if seen by a PA versus ED physician (82 min vs 75 min, 95% CI −10 to −6; p<0.001).26 Other studies abroad have shown PAs presence to improve the ED LOS.27–29 It may be that UK PAs methods of consultation differ to those overseas. Despite this, the adjusted total average LOS in the department of patients seen by a PA or FY1 was 228 min, which is within the target 4 hour standard (the time a patient waits between arriving to the ED to a decision being made about their onward care or discharge) used by NHS England trusts to measure performance.30
There are differences in the practice of care between the two clinicians; in addition to the lack of prescribing rights and ordering of ionising radiation; PAs tended to work more in higher acuity areas—Resus and Majors, whereas FY1s worked more in the UTC. At the hospital investigated the PAs also covered more shift hours as their core hours than FY1s; working beyond 1600 until midnight and included cover at weekends. FY1 doctors rotate every 4 months, whereas PAs are permanent members of staff. Despite adjusting for the area of the department the patient was seen, actual time and day of the week, nesting the individual clinician and omitting those who were admitted or LWBS, there was still significantly longer LOS for patients seen by PAs in comparison to those seen by FY1 doctors-in-training. A previous study of PAs in the ED showed PAs performance to be higher in lower acuity areas.31 Through assessment of clinical notes as Halter et al performed when comparing PAs and FY2—doctors-in-training; we could have obtained a fuller picture of the process involved in seeing more complex patients, that is, the number of patient investigations required, medications to be prescribed by a doctor; senior reviews or discussions; level of documentation, time taken to refer the patient for example. In their study patients seen by a PA were more likely to have an X-ray performed in the ED compared with patients seen by FY2s.22 This could result in additional time taken with the patients since the PA would have to get the investigations ordered on their behalf from a doctor post discussion.
Our finding of no significant difference in the secondary outcome of ED reattendance rate within 72 days with the same presenting complaint for patients of PAs and FY1 doctors-in-training is consistent with a study comparing the reattendance rates of patients seen by PAs compared with ED physicians in 72 hours.32 The findings were also similar to comparisons of FY2 doctors-in-training and PAs patients reattendance within 7 days.22 Other PA literature from the USA such as Merdler et al reported a reduction in the readmission rates within 48 hours in patients seen by PAs compared with ED doctors.23
Those LWBS have been shown to have a considerable effect of the efficiency and quality of care in EDs.33 Our finding of no significant difference of patients LWBS waiting for a PA versus FY1 doctor in training could suggest similar quality and efficiency of care between the two clinicians. Other studies have shown there to be a difference between PAs and ED doctors in terms of the number of patients LWBS. For example, de la Roche et al found that PA presence reduced the number of those LWBS compared with when a doctor was on duty in the absence of a PA (3.4% vs 1.5%, p<0.001).24 Similarly, Ducharme et al discovered that the chances of a patient LWBS were reduced when a PA was present (44% (95% CI 31% to 63%)).27
This study’s strengths lie in the large data set (duration of four 16-week rotations) enabling a well-powered quantitative comparative analysis of the impact of work carried out by PAs and FY 1 doctors-in-training, in a busy UK ED, against national metrics. The study was also able to statistically control for variations within the department and patient characteristics, which may have affected levels of acuity and complexity.
Our study had some limitations. One such limitation is that the triage score was not yet documented on the electronic systems at the time of study, so adjustments according to triage score were unable to be performed. Also, the decision time to admit was not recorded at the time of the study so, LOS readings may have been lower for patients waiting for a hospital bed on a specialty ward. There was also no linkage to staffing levels and bed capacity on each day which would have been useful to adjust for. Furthermore, as this study was purely quantitative in nature, it is only able to describe numerical patterns. Contextual explanation of these patterns would require qualitative and ethnography methods as a mixed-method approach.
Implications for policy and practice
FY1s are not present in all EDs and this study demonstrates their impact working in the ED as being very efficient in all areas, especially in seeing UTC (lower acuity patients). PAs are particularly able to see large volumes of patients in higher acuity areas. Deployments of these type of clinicians within the ED have the potential to address increasing patient demand within the ED, relieving staffing pressures and ultimately assisting with the efficiency of patients seen in different areas of the ED. The findings of the study can assist the EPIC’s assessment of skill mix as to appropriately allocate staff on a busy ED shift. Improvements in overall ED wait times have been shown to stem from improvements in time to triage.34 This could be a potential area of the department the PA could also work in, as other studies have shown them to reduce wait times, LOS and those LWBS when working in triage.35 36
The findings of no statistical difference in those reattending within 72 hours or LWBS demonstrate similar safety and appropriateness practices between the two clinicians. To further assess safety, future studies could compare reported patient adverse events, near misses and errors between the two clinicians. Future studies could also look at patient’s willingness to not have a significant difference in their wait time to be seen but have a longer LOS in the department if being seen by a PA.
Conclusion
The findings from this study have important implications for policy-makers, stakeholders and clinicians who all have a role in improving the efficiency of emergency care. In view of the shortages of junior doctors in the British NHS,37 PAs may be a workforce of consideration to supplement the existing medical workforce; to help meet the ED patient demands while providing continuity; due to being permanent staff members. With the GMC regulation of PAs, their efficiencies are highly likely to improve as they will be able to work more to their full potential in terms of being able to prescribe and order investigations using ionising radiation.
Supplementary Material
Acknowledgments
The authors would like to thank all those clinicians, administrative and information staff in the participating centre who assisted the study at a time of heightened workload within the emergency services in the National Health Service in England. The authors would also like to thank Dr Ngianga Kandala (NdK) who provided statistical advice for the data analysis.
Footnotes
Correction notice: This article has been corrected since it was published. The supplementary material in this article was updated on 18 March 2024.
Contributors: NK, as guarantor, accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish. NK conceived and designed the study ahead of NHS ethics approval with advice from SH. NK supervised the conduct of the study and data collection under supervision by SH. NK undertook recruitment of participating centre and managed the data, including quality. NK undertook the statistical analysis; with advice from NdK, medical statistics and health economics) and SH. NK drafted the manuscript, and SH contributed substantially to its revision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer: The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the Health Service and Delivery Research Programme or the Department of Health.
Competing interests: NK is employed as an Emergency Medicine Physician Associate at the trust this study was conducted. NK is also an honorary senior lecturer on a MSc Physician Associate degree programme and National OSCE examiner. NK is also works for NHS England as an ambassador for the Physician Associate profession.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the NHS Health Research Authority, London Bridge Research Ethics Committee (21/PR/0802).
References
- 1. Morley C, Unwin M, Peterson GM, et al. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One 2018;13:e0203316. 10.1371/journal.pone.0203316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NHS England . NHS long term workforce plan. growing the medical workforce. 2023. Available: https://www.england.nhs.uk/publication/?filter-category=culture-and-leadership [Accessed 26 Jul 2023].
- 3. NHS interim people plan interim-NHS-people-Plan_June2019.Pdf (Longtermplan.Nhs.UK) published 3RD June 2019. Available: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/05/Interim-NHS-People-Plan_June2019.pdf [Accessed 6 Jun 2019].
- 4. Watkins J, Straughton K, King N. “There is no 'I' in team but there may be a PA”. Future Healthc J 2019;6:177–80. 10.7861/fhj.2019-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. The faculty of physician associates at the royal college of physicians. 2023. Available: https://www.fparcp.co.uk/about-fpa/who-are-physician-associates [Accessed Jul 2023].
- 6. Ritsema TS, Cawley JF, Smith N. Physician assistants in urgent care. JAAPA 2018;31:40–4. 10.1097/01.JAA.0000541483.62234.b1 [DOI] [PubMed] [Google Scholar]
- 7. Physician associate voluntary managed register (PAMVR) faculty of physician associates - quality health care across the NHS (Fparcp.Co.UK). n.d. Available: https://www.fparcp.co.uk/pamvr/overview/
- 8. Ross N, Parle J, Begg P, et al. The case for the physician assistant. Clin Med (Lond) 2012;12:200–6. 10.7861/clinmedicine.12-3-200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mahase E. Government to introduce statutory regulation for physician associates. pulse. 2018. Available: http://www.pulsetoday.co.uk/your-practice/regulation/government-to-introduce-statutory-regulation-for-physician-associates/20037615.article
- 10. Hammond S. The regulation of physician associates (PAs) and anaesthesia associates (AAS): written statement- Hcws1741 in: parliament UK. 2019. Available: https://www.parliament.uk/business/publications/written-questions-answers-statements/written-statement/Commons/2019-07-18/HCWS1741/ [Accessed 20 Jan 2020].
- 11. Physician associate regulation consultation: RCP, Available: https://www.rcplondon.ac.uk/news/physician-associate-regulation-public-consultation-released
- 12. FPA, RCP . Guidance for employers and supervisors faculty of physician associates - quality health care across the NHS (Fparcp.Co.UK). n.d. Available: https://www.fparcp.co.uk/employers/guidance
- 13. GMC . Interim standards for physician associates and anaesthesia associates. n.d. Available: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-pas-and-aas/good-medical-practice-interim-standards-for-physician-associates-and-anaesthesia-associates
- 14. Schull MJ, Morrison LJ, Vermeulen M, et al. Emergency department gridlock and out-of-hospital delays for cardiac patients. Acad Emerg Med 2003;10:709–16. 10.1111/j.1553-2712.2003.tb00064.x [DOI] [PubMed] [Google Scholar]
- 15. RCEM: improving quality indicators and system metrics for eds in England (March 2019); Available: RCEM_position_statement_Improving_quality_indicators_and_system_metrics.pdf
- 16. England NHS. NHS England: major plan to recover urgent and emergency care services; Available: https://www.england.nhs.uk/2023/01/major-plan-to-recover-urgent-and-emergency-care-services/
- 17. Ritsema T. The faculty of physician associates census results 2018. faculty of physician associates at the royal college of physicians [Accessed]. Available: http://www.fparcp.co.uk/about-fpa/fpa-census [Accessed 10 Sep 2019].
- 18. The royal college of emergency medicine and the NHS. securing the future workforce for emergency departments in England. 2017. Available: https://improvement.nhs.uk/documents/1826/Emergency_department_workforce_plan_-_111017_Final.3.pdf [Accessed 31 Jul 2019].
- 19. Powell R, Mackaness C, Spittle C. Guidance for the supervision of foundation year 1 trainees i emergency medicine placements. Health Education England. Available: https://www.eastmidlandsdeanery.nhs.uk/sites/default/files/14773204041_role_of_fy1_trainee_in_emergency_medicine.pdf [Accessed 01 Nov 2023]. [Google Scholar]
- 20. Sakr M, Angus J, Perrin J, et al. Care of minor injuries by emergency nurse practitioners or junior doctors: a randomised controlled trial. Lancet 1999;354:1321–6. 10.1016/s0140-6736(99)02447-2 [DOI] [PubMed] [Google Scholar]
- 21. Cooper MA, Lindsay GM, Kinn S, et al. Evaluating emergency nurse practitioner services: a randomized controlled trial. J Adv Nurs 2002;40:721–30. 10.1046/j.1365-2648.2002.02431.x [DOI] [PubMed] [Google Scholar]
- 22. Halter M, Drennan V, Wang C, et al. Comparing physician associates and foundation year two doctors-in-training undertaking emergency medicine consultations in england: a mixed-methods study of processes and outcomes. BMJ Open 2020;10:e037557. 10.1136/bmjopen-2020-037557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Merdler I, Hochstadt A, Sheffy A, et al. The Israeli physician assistant in a tertiary medical center emergency Department. Isr Med Assoc J 2020;22:409–14. [PubMed] [Google Scholar]
- 24. de la Roche MRP, Dyer N, Froats M, et al. Effect of a physician assistant on quality and efficiency metrics in an emergency department: population cohort study. Can Fam Physician 2021;67:e61–7. 10.46747/cfp.6702e61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. King NMA, Habeeb M, Helps S. The contribution of physician associates or assistants to the emergency department: a systematic scoping review. J Am Coll Emerg Physicians Open 2023;4:e12989. 10.1002/emp2.12989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Arnopolin SL, Smithline HA. Patient care by physician assistants and by physicians in an emergency department. JAAPA 2000;13:39–40. [PubMed] [Google Scholar]
- 27. Ducharme J, Alder RJ, Pelletier C, et al. The impact on patient flow after the integration of nurse practitioners and physician assistants in 6 Ontario emergency departments. CJEM 2009;11:455–61. 10.1017/s1481803500011659 [DOI] [PubMed] [Google Scholar]
- 28. Silberman M, Jeanmonod D, Hamden K, et al. Mid- level providers working in a low-acuity area are more productive than in a high-acuity area. West J Emerg Med 2013;14:598–601. 10.5811/westjem.2012.12.12848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hamden K, Jeanmonod D, Gualtieri D, et al. Comparison of resident and mid-level provider productivity in a high-acuity emergency department setting. Emerg Med J 2014;31:216–9. 10.1136/emermed-2012-201904 [DOI] [PubMed] [Google Scholar]
- 30. Department of health clinical exceptions to the 4 hour emergency care target. 2003. Available: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4091871 [Accessed 01 Aug 2023].
- 31. Doan Q, Hooker RS, Wong H, et al. Canadians' willingness to receive care from physician assistants. Can Fam Physician 2012;58:e459–64. [PMC free article] [PubMed] [Google Scholar]
- 32. Pavlik D, Sacchetti A, Seymour A, et al. Physician assistant management of pediatric patients in a general community emergency department: a real-world analysis. Pediatr Emerg Care 2017;33:26–30. 10.1097/PEC.0000000000000949 [DOI] [PubMed] [Google Scholar]
- 33. Baker DW, Stevens CD, Brook RH. Patients who leave a public hospital emergency department without being seen by a physician. causes and consequences. JAMA 1991;266:1085–90. [PubMed] [Google Scholar]
- 34. Yuzeng S, Hui LL. Improving the wait time to triage at the emergency department. BMJ Open Qual 2020;9:e000708. 10.1136/bmjoq-2019-000708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kim TY, Ohmart C, Khan Z, et al. The effect on length of stay after implementation of discharging low acuity patients from triage. Cureus 2021;13:e17640. 10.7759/cureus.17640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nestler DM, Fratzke AR, Church CJ, et al. Effect of a physician assistant as triage liaison provider on patient throughput in an academic emergency department. Acad Emerg Med 2012;19:1235–41. 10.1111/acem.12010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. The royal college of emergency medicine and the NHS securing the future workforce for emergency departments in England. 2017. Available: https://improvement.nhs.uk/documents/1826/Emergency_department_workforce_plan_-_111017_Final.3.pdf [Accessed 01 Aug 2023].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-078511supp001.pdf (37.3KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.


