Abstract
Objective
This study aims to evaluate whether the first wave of the COVID-19 pandemic resulted in a deterioration in the quality of care for socially and/or clinically vulnerable stroke and ST-segment elevation myocardial infarction (STEMI) patients.
Design
Two cohorts of STEMI and stroke patients in the Aquitaine neurocardiovascular registry.
Setting
Six emergency medical services, 30 emergency units, 14 hospitalisation units and 11 catheterisation laboratories in the Aquitaine region in France.
Participants
This study involved 9218 patients (6436 stroke and 2782 STEMI patients) in the neurocardiovascular registry from January 2019 to August 2020.
Primary outcome measures
Care management times in both cohorts: first medical contact-to-procedure time for the STEMI cohort and emergency unit admission-to-imaging time for the stroke cohort. Associations between social (deprivation index) and clinical (age >65 years, neurocardiovascular history) vulnerabilities and care management times were analysed using multivariate linear mixed models, with an interaction on the time period (pre-wave, per-wave and post-first COVID-19 wave).
Results
The first medical contact procedure time was longer for elderly (p<0.001) and ‘very socially disadvantaged’ (p=0.003) STEMI patients, with no interaction regarding the COVID-19 period (age, p=0.54; neurocardiovascular history, p=0.70; deprivation, p=0.64). We found no significant association between vulnerabilities and the admission imaging time for stroke patients, and no interaction with respect to the COVID-19 period (age, p=0.81; neurocardiovascular history, p=0.34; deprivation, p=0.95).
Conclusions
This study revealed pre-existing inequalities in care management times for vulnerable STEMI and stroke patients; however, these inequalities were neither accentuated nor reduced during the first COVID-19 wave. Measures implemented during the crisis did not alter the structured emergency pathway for these patients.
Trial registration number
Keywords: COVID-19, Quality in health care, Health policy, Organisation of health services, Health Services Accessibility, Health Equity
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The study analysed two large high-quality data cohorts comprising almost 10 000 stroke and ST-segment elevation myocardial infarction patients, managed in a large panel of care structures throughout the Aquitaine region, over a period of several months before and after the first wave.
We studied vulnerabilities from two perspectives, a social perspective through an ecological social deprivation index and a clinical perspective through risk factors of severe COVID-19.
The explanatory analyses yield robust results due to the large amount of data collected (clinical and sociogeographical characteristics, acute care management pathway data), enabling integration of a wide variety of confounders.
The exclusion of patients who did not enter the healthcare system prevented quantification of healthcare system avoidance, that is, supposed to have been more frequent among socially and/or clinically vulnerable patients during the COVID-19 pandemic.
The study area was limited to the Aquitaine region, one of the regions least affected by the first wave of the COVID-19 pandemic in France; this situation could have led to the exertion of less pressure on health services.
Introduction
ST-segment elevation myocardial infarction (STEMI) and stroke are life-threatening and highly time-sensitive emergencies. The time elapsed from symptom onset to treatment is a predictor of patients’ mortality and functional recovery.1 2 The standardised and timed care pathways for these two diseases depend initially on a patient’s use of the emergency medical service (EMS) system, followed by close collaboration between emergency structures and specialised technical platforms (eg, catheterisation laboratories, stroke units).1 2 The quality of care is often evaluated under the prism of the time from first medical contact (FMC) to treatment.1 2
In France, patients with acute chest pain or neurological deficit are advised to rapidly call the nationwide EMS using a unique medical dispatch number. In cases of suspected stroke or STEMI, the EMS dispatches rapid transport, including a doctor for STEMI and life-threatening situations, to transfer the patient to a specialised technical platform. If not suspected, the EMS physician may refer the patient to a general practitioner for initial evaluation or advise them to go to the emergency unit (EU).
Patients with STEMI and stroke face social and health inequality issues. Socially vulnerable (ie, disadvantaged) patients with neurocardiovascular diseases have higher morbidity and mortality rates.3 4 Four markers of social position and socioeconomic status have been associated with cardiovascular disease in high-income countries: income level, educational attainment, employment status and environmental factors.5 These inequalities are attributable to a higher prevalence of biological, behavioural and psychosocial cardiovascular risk factors in the more socially disadvantaged population but also to more difficulties in accessing healthcare and lower-quality acute care management.4 6 7 The organisation of the healthcare system, as a social health determinant, leads to health inequalities, due mainly to challenges related to communication and health literacy, implicit bias, and/or a lack of culturally competent care.8
The COVID-19 dramatically modified healthcare systems worldwide and had major consequences for patients’ access to care for stroke and STEMI.9–11 From February to March 2020, many health authorities, including those in France, implemented strict nationwide lockdowns and series of policies to curb the surge of patients requiring critical care. This crisis, and particularly the lockdown periods, induced the major reorganisation of healthcare systems and modified the use of care to accommodate the onslaught of patients with COVID-19.12 Studies of the association between the COVID-19 pandemic and the quality of stroke and STEMI management have yielded contrasting results, with most revealing longer management delays and reductions in the number of procedures performed.9 10 13
During pandemics (eg, of influenza, plague), pre-existing inequalities affecting many aspects of patients’ care pathways (eg, loss of employment and income; social isolation, especially for elderly individuals; and mental health issues, particularly for young people) are usually amplified.14–18 During the COVID-19 pandemic, COVID-19 exposure, severe disease, hospitalisation and death were more frequent among socially disadvantaged people.15 17–19 This population benefited less from the collective protective measures taken against COVID-19, had more difficulty accessing preventative healthcare and had lower rates of COVID-19 testing and vaccination.14 Some experts consider COVID-19 to be a syndemic, rather than a pandemic. These interactions between COVID-19 and pre-existing socioeconomic inequalities in non-communicable diseases are an illustration.16 Indeed, ‘syndemics are characterised by biological and social interactions between conditions and states, interactions that increase a person’s susceptibility to harm or worsen their health outcomes.’16 We hypothesised that socially vulnerable patients, defined as those with low socioeconomic status, may experience longer acute management times during the COVID-19 pandemic.
In France, to protect more vulnerable patients and adapt care, health authorities identified several risk factors of severe COVID-19 based on demographic (advanced age) and medical (especially cardiovascular comorbidities) characteristics.20 For these populations defined as ‘clinically vulnerable patients’, French authorities have stressed the importance of adhering to barrier measures, maintaining physical distancing, particularly during hospitalisation and to limit travel to high-risk areas for SARS-CoV-2 transmission. Information about these risk factors was covered widely in the media, which may have led exposed individuals with these underlying conditions to delay seeking treatment.21 Based on these recommendations, we hypothesised that additional protective measures may have been implemented for these clinically more vulnerable populations, resulting in increased management delays.
To our knowledge, only one study has evaluated whether COVID-19 modified the associations among the educational level, deprivation, hospital admission indicators and quality of hospital care, especially for patients with neurocardiovascular diseases.22 The researchers found larger declines in the hospital access of women, elderly and less-educated individuals; in contrast, the timeliness of percutaneous coronary intervention (PCI) showed no education-related or deprivation-related gradient.
Since 2012, the ‘CNV Registry’ of neurocardiovascular diseases evaluate the care pathways for STEMI and stroke patients in the Aquitaine region of southwestern France (3 million inhabitants). This registry provides a unique opportunity to study differences in care management and their evolution over time in a country with universal health coverage.23
COVID-19 profoundly modified access to and the use and organisation of care, against a backdrop of pre-existing inequalities in neurocardiovascular disease.12 The notion of a ‘syndemic’ and our hypothesis that management times were longer for patients at risk of severe COVID-19 during its first wave prompted our investigation of whether first COVID-19 wave resulted in the deterioration of the quality of care for socially and clinically vulnerable stroke and STEMI patients, using data from the CNV Registry.
Methods
Study design and population
We used two exhaustive retrospective cohorts of adult stroke and STEMI patients admitted to a care structure in the Aquitaine region whose data were entered into the CNV Registry between 1 January 2019 and 31 August 2020.23
The STEMI cohort comprised patients with recent (<24 hours after symptom onset) STEMI managed in one of the six health territories in Aquitaine, each centred around an EMS, comprising 30 EUs and 11 catheterisation laboratories (nearly 1800 STEMIs are seen annually).
The stroke cohort comprised patients with recent ischaemic or haemorrhagic stroke (excluding transient ischaemic attacks), diagnosed by brain imaging and validated by neurovascular physicians, which was managed in 5 health territories in Aquitaine, comprising 14 (7 with stroke units) of the 20 hospitals caring for more than 30 strokes per year in Aquitaine (nearly 5000 strokes are seen annually).
Data collection
The CNV Registry contains information on patients’ sociodemographic (age, gender and place of residence) and clinical (medical history, cardiovascular risk factors, stroke clinical severity (modified Rankin scale and National Institute of Health Stroke Score), stroke type (ischaemic/haemorrhagic)) characteristics, use of care (calls to emergency services, FMC, symptom onset care time), acute care management quality (times between key management steps, prehospital and hospital pathway types, treatment) and structural characteristics of care (care during on-call activity, calls to emergency services during care, hospital administrative status, FMC–catheterisation laboratory distance). Data are collected prospectively by physicians; consolidated retrospectively by clinical research assistants and then extracted from the hospital information system. Data from the two cohorts were integrated into one data warehouse enabling the reconstruction of the STEMI or stroke management pathway.12
Outcomes
The primary endpoints were acute care management times, which reflect the quality of care. For the STEMI cohort, we used the FMC procedure time (delay (in minutes) between the FMC (mobile intensive care unit arrival or EU admission) and the start of a treatment procedure). For the stroke cohort, we used the EU admission imaging time (delay (in minutes) between EU admission and the start of the first imaging). This selection of an interval that focused on the beginning of in-hospital stroke care was required due to the heterogeneity of the prehospital pathways and treatments applied.
Exposure
Clinically vulnerable persons at risk of severe COVID-19 were those aged >65 years; with neurocardiovascular history including previous STEMI, stroke or transient ischaemic attack; and/or with coronary artery disease history. For the STEMI cohort, the history of a PCI, a coronary artery bypass graft was also included.
Due to the lack of individual socioeconomic data, an ecological social deprivation score was assigned to each commune (the smallest administrative unit in France) of patients’ residence using the 2015 deprivation index (Fdep15) to assess social vulnerability.24 This index is associated strongly with mortality at all geographical scales. It served as the first dimension of a principal component analysis (weighted by population size) of four socioeconomic ecological variables: the percentage of high-school graduates ≥15 years old, median household income, percentage of blue-collar workers and unemployment rate. Quintiles of the Fdep15 scores were computed for metropolitan France, whereby the first quintile (Q1) represented the least and the fifth quintile (Q5) the most disadvantaged communes. We calculated the deprivation score for each patient of our sample with reference to the quintiles of the French population.
Statistical analyses
Analyses were performed separately for each cohort and exposure variable. Associations between clinical and social vulnerabilities’ effects on care management times (introduced as continuous variables after logarithmic transformation) were analysed using multivariate linear mixed models (three each for stroke and STEMI), with random effects on hospital and health territories centred around single EMSs. Interactions in the time period were introduced. Three COVID-19 periods were defined according to the dates of first hospital reorganisation (mid-February) and the termination of national lockdown (10 May 2020): pre-wave (1 January 2019–9 February 2020), per-wave (10 February 2020–10 May 2020) and post-wave (11 May 2020–31 August 2020). Inspired by the conceptual framework developed by the Health Care Quality Indicator Project of the Organisation for Economic Co-operation and Development, we categorised determinants in four dimensions: patients, physicians, care organisations and quality of care.25 To develop the causal model, variables were classified into each of these dimensions and confounders were then identified by directed acyclic graphs (DAG; online supplemental material 1). The relationships between vulnerabilities and care management times were quantified (β) using the contrast method, with statistical significance defined as p<0.05. The exponentials of the beta values (exp(β)), associated 95% CIs, and percentage changes (1−exp(β)) were then calculated. The statistical analyses were conducted by using SAS V.9.4.
bmjopen-2023-073933supp001.pdf (1.1MB, pdf)
Patient and public involvement
As members of the CNV registry scientific boards, patient representatives were involved in study conception, implementation and dissemination; they validated data collection and analysis, and results diffusion. Dissemination of results was conducted on the CNV registry website, to the scientific boards and to care-structure physicians.
This study is reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines and is registered with ClinicalTrials.gov (NCT04979208).
Results
Sample characteristics
The sample comprised 9218 patients (6436 with stroke, 2782 with STEMI); 54.9% of the stroke patients and 73.1% of the STEMI patients were male. Patients aged >65 years accounted for 81.3% and 50.1% of the stroke and STEMI patients, respectively. One-quarter of patients had neurocardiovascular history (stroke, 28.6%; STEMI, 20.5%). The distributions of the deprivation index quintiles in our sample, ordered from the most advantaged to the most disadvantaged patients of our sample, were 16.2%, 24.8%, 18.1%, 19.3% and 21.6% for stroke patients and 12.8%, 23.5%, 22.8%, 22.8% and 18.1% for STEMI patients (online supplemental material 2).
bmjopen-2023-073933supp002.pdf (156KB, pdf)
Acute care management times
Stroke cohort
In the pre-wave period, the median admission imaging time was longer for stroke patients aged >65 years than for younger patients (84 vs 79 min) and for patients without than for those with neurocardiovascular history (86 vs 76 min). Acute care management times were longest for the most advantaged and most disadvantaged patients (both 88 min vs 77–86 min for the other social deprivation categories; table 1).
Table 1.
Admission-to-imaging time according to vulnerabilities and COVID-19 periods—Stroke cohort (N=6436)
| Global | Pre-wave | Per-wave | Post-wave | |
| (N=6436) | (N=4140) | (N=1080) | (N=1216) | |
| Median (IQR) (n) | Median (IQR) (n) | Median (IQR) (n) | Median (IQR) (n) | |
| All patients | 86 (47−194) (4819) | 83 (45−201) (3014) | 91 (51−175) (889) | 88 (52−191) (916) |
| Missing value | (1617) | (1126) | (191) | (300) |
| Clinical vulnerability | ||||
| Age | (4819) | (3014) | (889) | (916) |
| [18–65 years[ | 84 (45−193) (868) | 79 (43−208) (536) | 92 (48−177) (157) | 85 (45−174) (175) |
| [65 years and older[ | 86 (48−194) (3951) | 84 (45−199) (2478) | 91 (51−175) (732) | 88 (52−197) (741) |
| Missing value | (1617) | (1126) | (191) | (300) |
| Neurocardiovascular history | (4819) | (3014) | (889) | (916) |
| Absence | 88 (47−197) (3430) | 86 (45−204) (2128) | 93 (51−177) (661) | 86 (50−197) (641) |
| Presence | 83 (48−184) (1389) | 76 (45−187) (886) | 87 (49−173) (228) | 90 (57−189) (275) |
| Missing value | (1617) | (1126) | (191) | (300) |
| Social vulnerability | ||||
| Deprivation (Fdep15) | (4610) | (2821) | (884) | (905) |
| Most advantaged | 87 (47−235) (743) | 88 (46−240) (469) | 80 (44−202) (145) | 90 (54−239) (129) |
| Advantaged | 84 (45−206) (1107) | 77 (42−216) (637) | 97 (51−181) (235) | 85 (48−202) (235) |
| Intermediate | 87 (48−179) (831) | 83 (46−189) (492) | 92 (53−153) (168) | 94 (54−188) (171) |
| Disadvantaged | 86 (47−183) (903) | 86 (46−186) (568) | 86 (47−170) (154) | 86 (51−179) (181) |
| Most disadvantaged | 89 (52−192) (1026) | 88 (51−198) (655) | 95 (55−175) (182) | 82 (52−148) (189) |
| Missing value | (1826) | (1319) | (196) | (311) |
IQR, interquartile range.
The median admission imaging time was longer during the per-wave period than during the pre-wave period, regardless of age or neurocardiovascular history, but was shorter for the most advantaged patients (80 vs 88 min). This time was shorter during the post-wave period than during the per-wave period, regardless of age, but was longer for the most advantaged patients (90 vs 80 min).
STEMI cohort
In the pre-wave period, the median FMC procedure time was longer for STEMI patients aged >65 years than for younger patients (103 vs 96 min). Its length increased with the degree of disadvantage (from 82 min for the most advantaged to 129 min for the most disadvantaged patients; table 2).
Table 2.
FMC-to-procedure time according to vulnerabilities and COVID-19 periods—STEMI cohort (N=2782)
| Global | Pre-wave | Per-wave | Post-wave | |
| (N=2782) | (N=1868) | (N=407) | (N=507) | |
| Median (IQR) (n) | Median (IQR) (n) | Median (IQR) (n) | Median (IQR) (n) | |
| All patients | 99 (71−157) (2364) | 100 (71−158) (1577) | 95 (69−152) (353) | 102 (71−153) (434) |
| Missing value | (418) | (291) | (54) | (73) |
| Clinical vulnerability | ||||
| Age | (2364) | (1577) | (353) | (434) |
| [18–65 years[ | 95 (69−147) (1207) | 96 (69−152) (794) | 93 (68−134) (175) | 94 (69−134) (238) |
| [65 years and older[ | 105 (73−173) (1157) | 103 (74−169) (783) | 101 (70−190) (178) | 117 (74−167) (196) |
| Missing value | (418) | (291) | (54) | (73) |
| Neurocardiovascular history | (2364) | (1577) | (353) | (434) |
| Absence | 98 (71−156) (1699) | 99 (71−157) (1115) | 97 (70−157) (267) | 96 (70−149) (317) |
| Presence | 101 (70−159) (468) | 102 (72−156) (318) | 89 (61−135) (67) | 112 (74−169) (83) |
| Unknown | 98 (74−161) (197) | 97 (73−180) (144) | 97 (81−134) (19) | 118 (78−154) (34) |
| Missing value | (418) | (291) | (54) | (73) |
| Social vulnerability | ||||
| Deprivation (Fdep15) | (2343) | (1565) | (351) | (427) |
| Most advantaged | 90 (64−152) (304) | 82 (63−149) (203) | 92 (62−127) (48) | 119 (79−177) (53) |
| Advantaged | 91 (66−145) (551) | 92 (68−139) (350) | 93 (62−162) (90) | 89 (65−150) (111) |
| Intermediate | 95 (70−150) (538) | 97 (69−156) (378) | 91 (68−157) (71) | 89 (72−129) (89) |
| Disadvantaged | 102 (73−150) (536) | 101 (75−154) (353) | 94 (70−140) (82) | 106 (73−151) (101) |
| Most disadvantaged | 124 (86−204) (414) | 129 (85−215) (281) | 120 (90−198) (60) | 122 (93−180) (73) |
| Missing value | (439) | (303) | (56) | (80) |
FMC, first medical contact; IQR, interquartile range; STEMI, ST-segment elevation myocardial infarction.
The median FMC procedure time was slightly shorter during the per-wave period than during the pre-wave period, regardless of age or neurocardiovascular history, but was longer for the most advantaged patients (92 vs 82 min). This time was longer during the post-wave period than during the per-wave period, especially for elderly patients (117 vs 101 min), those with neurocardiovascular history (112 vs 89 min) and those most advantaged (119 vs 92 min).
Effects of the COVID-19 first wave
Stroke cohort models
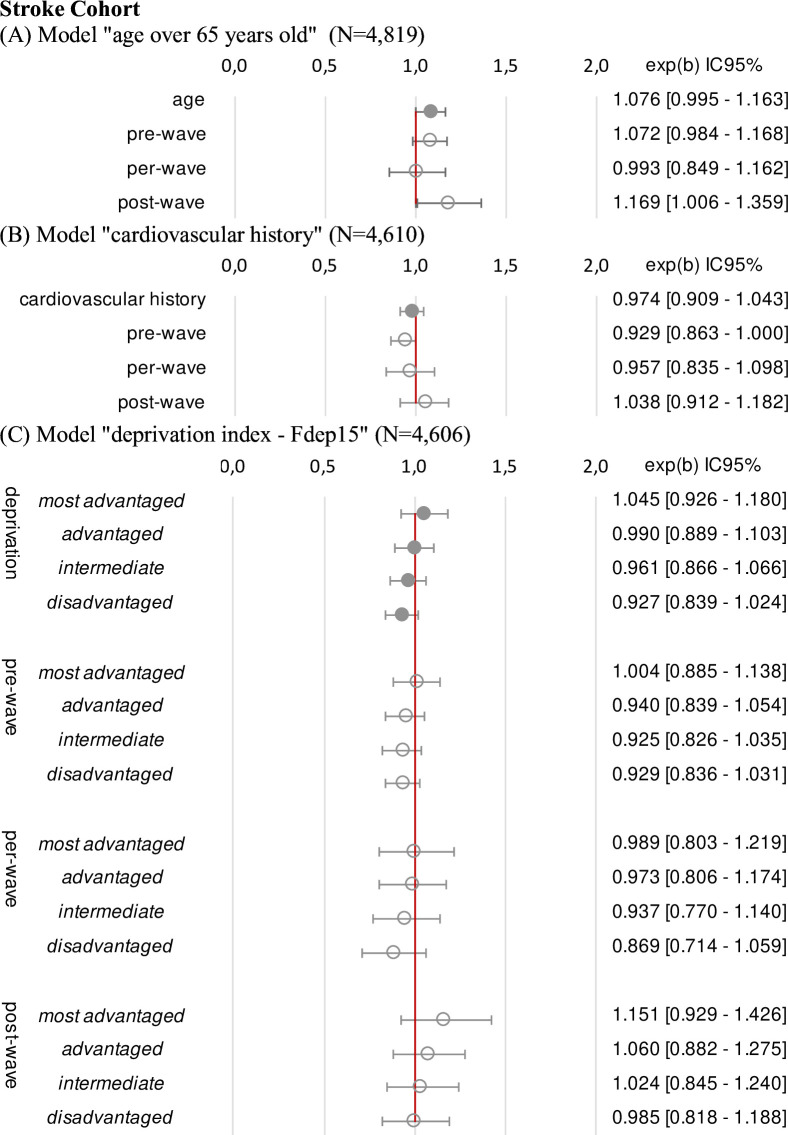
The final stroke models showed no significant association among advanced age (n=4819, exp(β)=1.08, 95% CI 1.00 to 1.16, p=0.07, neurocardiovascular history (n=4610, exp(β)=0.97, 95% CI 0.91 to 1.04, p=0.44), deprivation (n=4606, p=0.30), and the EU admission imaging time, and no interaction with the COVID-19 period (age, p=0.81; neurocardiovascular history, p=0.34; deprivation, p=0.95; figure 1).
Figure 1.
Estimation of each clinical and social factor (95% CI) on emergency unit admission-to-imaging time. Estimated overall effects expressed as exp(ß) with 95% CI; results of multivariate linear regression mixed models; variable to be explained: Y=log (emergency unit admission-to-imaging time); (A) results adjusted on period and gender; (B) cardiovascular history was a history of stroke, transient ischaemic attack, coronary artery disease or myocardial infarction; results adjusted on period, age, gender, diabetes and smoking as risk factors, deprivation index; (C) the reference modality for the deprivation index Fdep15 in five categories was ‘most disadvantaged’; results adjusted on period, age, gender, country of birth, urbanicity of residence.
STEMI cohort models
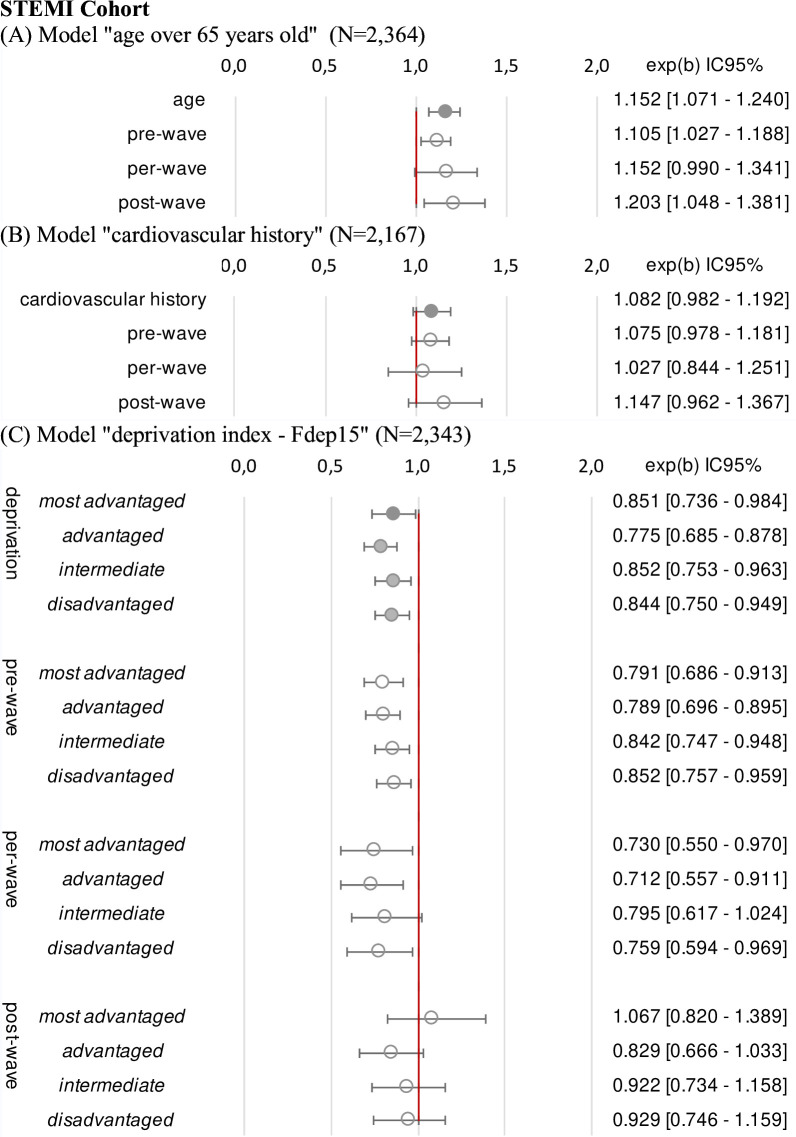
Advanced age was associated with a 15% increase in the FMC–procedure time (n=2364, exp(β) = 1.15, 95% CI 1.07 to 1.24, p<0.001). No significant association was noted between patients’ neuro-cardiovascular history and the FMC procedure time(n=2167, exp(β) = 1.08, 95% CI 0.98 to 1.19, p=0.14). Compared with those in the other four quintiles, FMC procedure times were 15%–22% longer for patients in the most disadvantaged quintile (n=2343, p=0.003). No significant COVID-19 period interaction affected the relationships between the vulnerabilities studied and the FMC procedure time (age, p=0.54; neurocardiovascular history, p=0.70; deprivation, p=0.64; figure 2).
Figure 2.
Estimation of each clinical and social factor (95% CI) on FMC-to-procedure time. Estimated overall effects expressed as exp(ß) with 95% CI; results of multivariate linear regression mixed models; variable to be explained: Y=log (FMC-to-procedure time); (A) results adjusted on period and gender; (B) cardiovascular history was a history of stroke, transient ischaemic attack, coronary artery disease or myocardial infarction; results adjusted on period, age, gender, diabetes, hypertension, dyslipidaemia, obesity and smoking as risk factors; (C) the reference modality for the deprivation index Fdep15 in five categories was ‘most disadvantaged’; results adjusted on period, age, gender, country of birth, urbanicity of residence. FMC, first medical contact; STEMI, ST-segment elevation myocardial infarction.
Discussion
Main results
This analysis of the healthcare pathways for STEMI and stroke patients included in the CNV Registry showed that care management times for socially or clinically vulnerable patients did not worsen during the first wave of the COVID-19 pandemic, despite changes in the access to and use and organisation of care. Nonetheless, regardless of the COVID-19 period, acute care management times were longer for elderly and the most disadvantaged STEMI patients.
Social and clinical vulnerability in stroke and STEMI management during the COVID-19 pandemic
Our results are concordant with those of a study conducted in Italy, which revealed no educational or deprivation gradient for cardiovascular acute care management times.22 Several factors can explain the resilience of stroke and STEMI care pathways for vulnerable populations.
First, STEMI and stroke networks in France are structured as well-defined, organised and dedicated pathways. Highly structured patient-centred clinical pathways improve the quality of care for chronic and acute conditions with predictable trajectories.26 27 Guidelines and national stroke and STEMI improvement programmes recommend the implementation of such structured pathways, which include close collaborations between healthcare professionals and patient orientation to the EMS system and specialised technical platforms. A study of the impacts of changes in the use of care and implementation of hospital reorganisation spurred by the COVID-19 pandemic on acute management times for stroke and STEMI revealed no deep alteration of the emergency pathway construct.12 Socially and/or clinically vulnerable populations have also benefited from the resilience of the STEMI and stroke pathways.
Second, in the particular context of the first COVID-19 wave, the mass media widely relayed information from health institutions. The whole population was worried and very concerned about its health. Lockdown measures made people more available, and routinely exposed, to mainstream media that were highly focused on the pandemic and health messages. These factors are associated with a greater likelihood of the adoption of recommended prevention practices.28 Thus, broad health-related media coverage may have had a positive influence on health literacy for the whole population, which may have positively influenced the use of the healthcare system.29
Third, the EMS was identified as the first contact to limit exposure and regulate urgent calls during the first COVID-19 wave in France. The media relayed this information. French hospitals increased regulation capacities to face the rise in EMS calls, in an attempt to preserve access to care and the capacity to handle vital emergencies for the entire population.30
Fourth, France adopted a specific strategy in March 2020 to support the economy, companies and jobs through measures that include financial support for disadvantaged populations, salary preservation, the prohibition of layoffs and housing assistance.31 Associated with universal healthcare coverage, these actions may have contributed to mitigate the social consequences of the pandemic.
Social and clinical vulnerability in stroke and STEMI management regardless of the COVID-19 pandemic
Several studies, including the present work, have shown that acute care management times are longer for elderly and socially vulnerable STEMI patients.32–34 Concerning stroke, we found no alteration in the acute care management time for elderly and socially vulnerable stroke patients. The results pertaining to stroke patients may be explained by our examination of the EU admission imaging time focused on the beginning of in-hospital care. Unlike the STEMI pathway, this time involves such a small portion of stroke patients’ pathways that it could have been difficult to detect an effect.
Age
Regarding specifically age for STEMI patients, greater initial clinical severity, atypical symptoms and a longer delay in admission may explain these findings.33 Half of the STEMI patients in our sample were aged >65 years. The proportion of stroke patients >65 years was 81%, which made it difficult to demonstrate an effect. To our knowledge, only one study, conducted in England, has revealed an association between older age and a longer admission CT time for stroke patients.35
Socioeconomic status
Findings with respect to socioeconomic status do not converge for STEMI. Biswas et al32 found that the median time to reperfusion in Australia, a country with universal healthcare, between 2005 and 2015 was 4 min longer for lower socioeconomic quintiles than for the highest quintile. Vasaiwala and Vidovich34 found a direct correlation between income levels in the USA and the proportion of patients meeting the guideline-recommended door–balloon time. In contrast, Heo et al36 found no association between the educational level and door–balloon time in Korea. None of these studies involved control for the confounders. Additional dedicated analyses of the relationship between socioeconomic status and acute care management time are needed, especially for elderly patients with accumulated comorbid factors due to their disadvantaged status.
Few studies have involved the exploration of acute stroke management times according to socioeconomic status, with contrasting results explained by the specificities of healthcare systems.3 37 In a study conducted in England, socially vulnerable patients were less likely to undergo high-quality recommended processes and more likely to undergo early supported discharge.3 A study conducted in Sweden showed that university-educated patients were more likely to be treated than were less-educated patients.37
Neurocardiovascular history
Regardless of the COVID-19 period, we found no significant influence of patients’ neurocardiovascular history on acute care management times, consistent with reported findings for STEMI patients.38 To our knowledge, no other study has evaluated this relationship for stroke care.
Implications for clinical practice and health system performance
While the COVID-19 pandemic crisis is nearly resolved, our findings remain valuable for health institutions and professionals to prepare for future health crises. The structured emergency pathway for strokes and STEMI patients and hospital reorganisations ensured sustained care quality.12 In our study, the COVID-19 crisis did not have any differential impact on social health inequalities, suggesting a good resilience of the French healthcare network. Organisational strategies employed, such as a dedicated life-threatening emergency pathway, transversal reorganisations aiming at concentrating resources on emergency care,12 targeted communication and increased regulation capacities, could be replicated in new crises and extended to other conditions. Pre-existing STEMI management inequalities partly result from the healthcare system organisation. In a study about disparities in cardiovascular disease, these inequalities are linked to language challenges, health literacy, implicit bias and the absence of culturally competent care.8 This may lead to less accurate medical interviews and suboptimal medical decisions. Further research is essential to investigate these hypotheses and evaluate potential corrective measures.
Strengths and weaknesses
Our study, one of the first to examine the effects of the COVID-19 crisis on the quality of care for STEMI and stroke patients in Europe with consideration of health and social inequalities, involved the parallel analysis of two high-quality databases containing data on large numbers of stroke and STEMI patients managed in a large panel of care structures in the Aquitaine region.
Our study has some limitations, particularly with regard to the population. The study area was limited to the Aquitaine region, one of the regions least affected by the first wave of the COVID-19 pandemic.39 This situation could have led to the exertion of less pressure on health services (especially the EMS, STEMI and stroke network). Arguments support the sample’s representativeness for stroke and STEMI patients in hospitals during this period, making our results likely applicable to all of France. First, a stroke study showed that the use of care was similar regardless of pandemic intensity.40 Second, a previous study with the same database highlighted results consistent with other French studies on the evolution of stroke and STEMI patient admissions.12 Third, characteristics and acute management times for stroke and STEMI patients in the ‘CNV registry’ align with those in other French regions. It would be interesting to repeat the study in another region, or in another country more affected by the pandemic, to test the external validity of the results.
Moreover, patients who did not enter the healthcare system because they had died or did not benefit from hospital care, as well as STEMI patients with symptoms for >24 hours, were not included. The exclusion of these patients may have generated selection bias and prevented us from quantifying the phenomenon of healthcare system avoidance that could be supposed to be more frequent among socially and/or clinically vulnerable patients during the COVID-19 crisis, as stated in a Danish study41; it also entails the risk that increases in the delay to use of care were underestimated for some patient subgroups. A French study revealed a 24% decrease in emergency consultations for STEMI and an 18% decrease in stroke.42 However, a national survey analysed the characteristics associated with not seeking care, in 2017 and 2020, revealing factors such as younger age, foreign nationality, living alone and lack of general practitioner care.43 The proportion of patients not seeking care increased during COVID-19 pandemic, but the population was not significantly different from the one before, suggesting a limited selection bias.
Our explanatory analyses yield robust results, with the inclusion of appropriate confounding variables identified by the DAG method. The large panel of data collected enabled the integration of a wide variety of confounders, including clinical characteristics and sociogeographical factors.
Given the lack of individual-level socioeconomic data in the CNV Registry, which prevented the assignment of social determinants for each patient, we used a residence area-based measure, which is a major limitation of our study. However, we determined deprivation indices using a validated tool that has been used in many studies conducted in France.24 Moreover, the socioecological measure of deprivation tends to underestimate social inequalities observed using individual data; thus, caution is advised when attributing group-level estimates to individuals.6 Additional limitations of this study include our inability to include all clinical risk factors of severe COVID-19 and information about patients’ educational levels, individual resources and social support to further explore their precariousness and health literacy. The COVID-19 pandemic may have had a greater impact on the access to and quality of care for the most precarious individuals.
A major methodological issue of this study is that we defined the per-wave period according to the implementation of healthcare reorganisation and transformation of societal functioning to fight the COVID-19 pandemic.12 We began the per-wave period at the time of the first hospital reorganisation implementation and ended it at the time of lockdown lifting. Although data for the CNV Registry are collected continuously, we terminated the follow-up period at the end of August 2020 to enable the timely reporting of results.
Finally, we did not explore gender as a distinct vulnerable group9 and short-term or long-term outcomes such as morbidity, mortality, disability or rehospitalisation after initial hospitalisation for STEMI or stroke, for which a wide range of socioeconomic disparities exist.3 41 Separate studies on gender inequalities and inequalities following acute care are currently underway, with a focus on the COVID period.
Conclusions
The first wave of the COVID-19 pandemic induced no deep change in management times for the most socially and/or clinically vulnerable stroke and STEMI patients. Pre-existing inequalities in care management times observed for elderly and most disadvantaged STEMI patients, were neither aggravated nor reduced by changes in the use of care or implementation of hospital reorganisation spurred by the pandemic. These encouraging results may be explained by the well-structured STEMI and stroke networks in France and the reorganisation of the healthcare structure to preserve access and the capacity to care for vital emergencies using the EMS. Additional studies are required to explore findings related to social health inequalities in STEMI management.
Supplementary Material
Acknowledgments
Julien Asselineau, Vincent Bouteloup, Moufid Hajjar, Marion Kret, Vincent Thevenet, Rodolphe Thiebaut, Elodie Martin, Leila Boukami and all healthcare professionals participating in the CNV registry.
Footnotes
Collaborators: Pr Patrick Dehail, Dr Tanguy Martin and the CNV Registry team: Charlotte Boureau, Mathilde Borg, Céline Dupuis, Florian Gilbert, Cristelle Gill, Leslie Larco, Jean-Pierre Legrand, Mélanie Maugeais, Corinne Perez, Olivia Rick.
AVICOVID group: Dr Faucheux Jean-Marc CH Agen, Dr Leca-Radu Eléna CH Agen, Dr Seignolles Gaëlle CH Agen, Dr Chazalon Cécile CH Arcachon, Dr Dan Maria CH Arcachon, Dr Lucas Ludovic CH Arcachon, Dr Péron Julie CH Arcachon, Dr Wong-So Laurent CH Blaye, Dr Martinez Miquel CH Dax, Dr Nocon Claire CH Dax, Dr Hostyn Véronique CH Langon, Dr Papin Jérémy CH Langon, Dr Bordier Philippe CH Langon, Dr Casenave Philippe CH Libourne, Dr Maillard Laurent CH Agen, Dr Ondze Basile CH Mont de Marsan, Dr Argacha Isabelle CH Oloron, Dr Tidahy Eliane CH Oloron, Dr Ferraton Lucie CH Orthez, Dr Mostefai Yousra CH Orthez, Dr Demasles Stéphanie CH Pau, Dr Hubrecht Régis CH Pau, Dr Bakpa Djoumana CH Villeneuve, Dr Bartou Christine CH Villeneuve, Dr Bannier Stéphanie CH Côte Basque, Dr Bernady Patricia CH Côte Basque, Dr Ellie Emmanuel CH Côte Basque, Dr Higue David CH Côte Basque, Dr Marnat Gaultier CHU Bordeaux, Dr Berge Jérôme CHU Bordeaux, Dr Goze-Dupuy Catherine Clinique Lesparre, Dr Lavocat Hélène Clinique Lesparre, Dr Senis Frédéric Clinique Lesparre, Dr Delonglee Virginie CH Agen, Dr Darraillans Didier CH Mont de Marsan, Dr Tarak Mokni CH Côte Basque, Dr Bataille Bertrand CH Pau, Dr Lorendeau Jean-Paul CH Perigueux, Dr Eclancher Anncy CH Bergerac, Dr Trogoff Bruno CH Périgueux, Dr Chartroule Véronique Polyclinique Francheville, Dr Touchard Philippe CH Langon, Dr Leyral Hervé Polyclinique Bordeaux-Nord Aquitaine, Dr Ngounou Fogue Chancel Clinique Mutualiste Pessac, Dr Scouarnec Catherine Clinique Mutualiste Pessac, Dr Orcival François Clinique Wallerstein d’Arès, Dr Goulois Nathalie CHU Bordeaux, Dr Heydel Virginie CH Arcachon, Dr Tahon Bertrand CH Libourne, Dr Py Emmanuel HIA Robert Picque, Dr Bidian Sorina CH Mont de Marsan, Dr Fabre Jean CH Dax, Dr Cherhabil Nidhal Polyclinique les Chênes, Dr Baha Leila CH Villeneuve, Dr Fort Pierre-Arnaud CH Agen, Dr Maisonnave Vincent CH Saint-Palais, Dr Verhoeven Luc Clinique Belharra, Dr Claveries Paul CH Côte Basque, Dr Ansart Emma Polyclinique Aguilera, Dr Lefevre Brice Polyclinique Côte Basque-Sud, Dr Liepa Marie-Pierre CH Orthez, Dr Lacrouts Marc CH Oloron, Dr Coustere Jean-baptiste CH Pau, Dr Fournier Pierre Clinique Esquirol-Saint-Hilaire Agen, Dr Jarnier Philippe CH Périgueux, Dr Delarche Nicolas CH Pau, Dr Banos Jean-Luc GCS cardiologie Bayonne, Dr Marque Nicolas Clinique cardiologique Aressy, Dr Karsenty Bernard Hopital privé Saint-Martin Bordeaux, Dr Perron Jean-Marie CH Libourne, Dr Leymarie Jean-Louis Clinique Saint-Augustin Bordeaux, Dr Hassan Akil CH Mont de Marsan, Dr Casteigt Francois Polyclinique Bordeaux-Nord Aquitaine, Dr Larnaudie Bernard Polyclinique Bordeaux-Nord Aquitaine, Pr Combes Xavier CHU Bordeaux, Dr Laplace Guillaume Clinique cardiologique Aressy.
Contributors: EL, FF, SD, FSaillour and FSevin were responsible for the study concept and design. EL and FF conducted the literature review. EL and FSevin had full access to all of the data and took responsibility for their integrity and accuracy. SD and SM-H performed the statistical analysis. FSaillour, EL, SD, FF, FSevin, SV, LC, PC, FR, IS and CP interpreted the data. EL, FF, SV, FSaillour and SD wrote the manuscript. FSevin, LC, PC, FR, IS and CP critically reviewed the manuscript. EL is responsible for the overall content as the guarantor.
Funding: This work was supported by 'Alliance Tous unis contre le virus', which includes the 'Fondation de France', the 'AP-HP' and the 'Institut Pasteur' grant number 00107870 and the 'Nouvelle-Aquitaine Regional Health Agency'.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Collaborators: AVICOVID group, Jean Faucheux, Elena Leca Radu, Gaëlle Seignolles, Cécile Chazalon, Maria Dan, Ludovic Lucas, Julie Peron, Laurent Wong-So, Miquel Martinez, Claire Nocon, Véronique Hostyn, Jérémy Papin, Philippe Bordier, Philippe Casenave, Laurent Maillard, Basile Ondze, Isabelle Argacha, Eliane Tidahy, Lucie Ferraton, Yousra Mostefai, Stéphanie Demasles, Régis Hubrecht, Djoumana Bakpa, Christine Bartou, Stéphanie Bannier, Patricia Bernady, Emmanuel Ellie, David Higue, Gaultier Marnat, Jérome Berge, Catherine Goze-Dupuy, Hélène Lavocat, Frédéric Senis, Virginie Delonglee, Didier Darraillans, Tarak Mokni, Bertrand Bataille, Jean Lorendeau, Anncy Eclancher, Bruno Trogoff, Véronique Chartroule, Philippe Touchard, Hervé Leyral, Fogue Ngounou, Catherine Scouarnec, François Orcival, Nathalie Goulois, Virginie Heydel, Bertrand Tahon, Emmanuel Py, Sorina Bidian, Jean Fabre, Nidhal Cherhabil, Leila Baha, Pierre-Arnaud Fort, Vincent Maisonnave, Luc Verhoeven, Paul Claveries, Emma Ansart, Brice Lefevre, Marie-Pierre Liepa, Marc Lacrouts, Jean-Baptiste Coustere, Pierre Fournier, Philippe Jarnier, Nicolas Delarche, Jean-Luc Banos, Nicolas Marque, Bernard Karsenty, Jean-Marie Perron, Jean-Louis Leymarie, Akil Hassan, Francois Casteigt, Bernard Larnaudie, Xavier Combes, and Guillaume Laplace
Data availability statement
Data are available on reasonable request. Deidentified participant data will be available on reasonable request. Proposals may be submitted to the corresponding author. Data requestors will need to sign a data access agreement.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The CNV Registry was approved by the French authority on data protection and met the regulatory requirements for the handling of patient information (file 2216283). The study was approved by the Bordeaux University Hospital Ethics Board (CER-BDX 2023-131).
References
- 1.Neumann F-J, Sousa-Uva M, Ahlsson A, et al. ESC/EACTS guidelines on myocardial revascularization. EuroIntervention 2019;14:1435–534. 10.4244/EIJY19M01_01 [DOI] [PubMed] [Google Scholar]
- 2.Terkelsen CJ, Sørensen JT, Maeng M, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010;304:763–71. 10.1001/jama.2010.1139 [DOI] [PubMed] [Google Scholar]
- 3.Bray BD, Paley L, Hoffman A, et al. Socioeconomic disparities in first stroke incidence, quality of care, and survival: a nationwide registry-based cohort study of 44 million adults in England. Lancet Public Health 2018;3:e185–93. 10.1016/S2468-2667(18)30030-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simoni AH, Frydenlund J, Kragholm KH, et al. Socioeconomic inequity in incidence, outcomes and care for acute coronary syndrome: a systematic review. Int J Cardiol 2022;356:19–29. 10.1016/j.ijcard.2022.03.053 [DOI] [PubMed] [Google Scholar]
- 5.Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes. Circulation 2018;137:2166–78. 10.1161/CIRCULATIONAHA.117.029652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schröder SL, Richter M, Schröder J, et al. Socioeconomic inequalities in access to treatment for coronary heart disease: a systematic review. Int J Cardiol 2016;219:70–8. 10.1016/j.ijcard.2016.05.066 [DOI] [PubMed] [Google Scholar]
- 7.Kucharska-Newton AM, Harald K, Rosamond WD, et al. Socioeconomic indicators and the risk of acute coronary heart disease events: comparison of population-based data from the United States and Finland. Ann Epidemiol 2011;21:572–9. 10.1016/j.annepidem.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Javed Z, Haisum Maqsood M, Yahya T, et al. Race, racism, and cardiovascular health: applying a social determinants of health framework to racial/ethnic disparities in cardiovascular disease. Circ Cardiovasc Qual Outcomes 2022;15:e007917. 10.1161/CIRCOUTCOMES.121.007917 [DOI] [PubMed] [Google Scholar]
- 9.Kiss P, Carcel C, Hockham C, et al. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes 2021;7:18–27. 10.1093/ehjqcco/qcaa084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chew NWS, Ow ZGW, Teo VXY, et al. The global effect of the COVID-19 pandemic on STEMI care: a systematic review and meta-analysis. Can J Cardiol 2021;37:1450–9. 10.1016/j.cjca.2021.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao J, Li H, Kung D, et al. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke 2020;51:1996–2001. 10.1161/STROKEAHA.120.030225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lesaine E, Francis-Oliviero F, Domecq S, et al. Effects of healthcare system transformations spurred by the COVID-19 pandemic on management of stroke and STEMI: a registry-based cohort study in France. BMJ Open 2022;12:e061025. 10.1136/bmjopen-2022-061025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siegler JE, Zha AM, Czap AL. Influence of the COVID-19 pandemic on treatment times for acute ischemic stroke. Stroke 2021;52:40–7. 10.1161/STROKEAHA.120.032789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bambra C, Riordan R, Ford J, et al. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:964–8. 10.1136/jech-2020-214401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khanijahani A, Iezadi S, Gholipour K, et al. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int J Equity Health 2021;20:248. 10.1186/s12939-021-01582-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horton R. Offline: COVID-19 is not a pandemic. The Lancet 2020;396:874. 10.1016/S0140-6736(20)32000-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magesh S, John D, Li WT, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw Open 2021;4:e2134147. 10.1001/jamanetworkopen.2021.34147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green H, Fernandez R, MacPhail C. The social determinants of health and health outcomes among adults during the COVID-19 pandemic: a systematic review. Public Health Nurs 2021;38:942–52. 10.1111/phn.12959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vandentorren S, Smaïli S, Chatignoux E, et al. The effect of social deprivation on the dynamic of SARS-Cov-2 infection in France: a population-based analysis. Lancet Public Health 2022;7:e240–9. 10.1016/S2468-2667(22)00007-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chauvin F. Actualisation de L’Avis Relatif aux Personnes À Risque de forme grave de COVID-19 et aux Mesures Barrières Spécifiques À CES Publics. Haut Conseil de La Santé Publique; 2020. Available: https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=807 [Accessed 18 May 2022]. [Google Scholar]
- 21.Naylor-Wardle J, Rowland B, Kunadian V. Socioeconomic status and cardiovascular health in the COVID-19 pandemic. Heart 2021;107:358–65. 10.1136/heartjnl-2020-318425 [DOI] [PubMed] [Google Scholar]
- 22.Di Girolamo C, Gnavi R, Landriscina T, et al. Indirect impact of the COVID-19 pandemic and its containment measures on social inequalities in hospital utilisation in Italy. J Epidemiol Community Health 2022:jech-2021-218452. 10.1136/jech-2021-218452 [DOI] [PubMed] [Google Scholar]
- 23.Lesaine E, Saillour-Glenisson F, Leymarie J-L, et al. The ACIRA Registry: a regional tool to improve the healthcare pathway for patients undergoing percutaneous coronary interventions and coronary angiographies in the French aquitaine region: study design and first results. Crit Pathw Cardiol 2020;19:1–8. 10.1097/HPC.0000000000000199 [DOI] [PubMed] [Google Scholar]
- 24.Rey G, Jougla E, Fouillet A, et al. Ecological association between a deprivation index and mortality in France over the period 1997 – 2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health 2009;9:33. 10.1186/1471-2458-9-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arah OA, Westert GP, Hurst J, et al. A conceptual framework for the OECD health care quality indicators project. Int J Qual Health Care 2006;18 Suppl 1:5–13. 10.1093/intqhc/mzl024 [DOI] [PubMed] [Google Scholar]
- 26.Allen D, Gillen E, Rixson L. Systematic review of the effectiveness of integrated care pathways: what works, for whom, in which circumstances? Int J Evid Based Healthc 2009;7:61–74. 10.1111/j.1744-1609.2009.00127.x [DOI] [PubMed] [Google Scholar]
- 27.Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed 2021;92:e2021093. 10.23750/abm.v92i1.10639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin L, Savoia E, Agboola F, et al. What have we learned about communication inequalities during the H1N1 pandemic: a systematic review of the literature. BMC Public Health 2014;14:484. 10.1186/1471-2458-14-484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peltzer S, Hellstern M, Genske A, et al. Health literacy in persons at risk of and patients with coronary heart disease: a systematic review. Soc Sci Med 2020;245:112711. 10.1016/j.socscimed.2019.112711 [DOI] [PubMed] [Google Scholar]
- 30.Guide Méthodologique Préparation À La phase Épidémique de COVID-19 des Établissements de Santé, de la Médecine de Ville et des Établissements et services Médico-Sociaux Du 16 Mars 2020. 2020. Available: https://www.nouvelle-aquitaine.ars.sante.fr/guide-methodologique-preparation-la-phase-epidemique-de-covid-19-des-etablissements-de-sante-de-la [Accessed 24 Jun 2022].
- 31.Math A. Quoi Qu’Il en Coûte. des Mesures Incomparables pour faire face aux Conséquences Économiques de la Pandémie? - IRES. Chronique Internationale de l’IRES 2022;176:8–31. 10.3917/chii.176.0008 [DOI] [Google Scholar]
- 32.Biswas S, Andrianopoulos N, Duffy SJ, et al. Impact of socioeconomic status on clinical outcomes in patients with ST-segment-elevation myocardial infarction. Circ Cardiovasc Qual Outcomes 2019;12:e004979. 10.1161/CIRCOUTCOMES.118.004979 [DOI] [PubMed] [Google Scholar]
- 33.Nguyen HL, Saczynski JS, Gore JM, et al. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes 2010;3:82–92. 10.1161/CIRCOUTCOMES.109.884361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vasaiwala S, Vidovich M. Impact of socioeconomic status on guideline-recommended care for ST-elevation myocardial infarction in the United States. Int J Cardiol 2010;143:424–5. 10.1016/j.ijcard.2008.11.032 [DOI] [PubMed] [Google Scholar]
- 35.Myint PK, Kidd AC, Kwok CS, et al. Time to computerized tomography scan, age, and mortality in acute stroke. J Stroke Cerebrovasc Dis 2016;25:3005–12. 10.1016/j.jstrokecerebrovasdis.2016.08.020 [DOI] [PubMed] [Google Scholar]
- 36.Heo JY, Hong KJ, Shin SD, et al. Association of educational level with delay of prehospital care before reperfusion in STEMI. Am J Emerg Med 2015;33:1760–9. 10.1016/j.ajem.2015.08.019 [DOI] [PubMed] [Google Scholar]
- 37.Stecksén A, Glader E-L, Asplund K, et al. Education level and inequalities in stroke reperfusion therapy. Stroke 2014;45:2762–8. 10.1161/STROKEAHA.114.005323 [DOI] [PubMed] [Google Scholar]
- 38.Feng L, Li M, Xie W, et al. Prehospital and in-hospital delays to care and associated factors in patients with STEMI: an observational study in 101 non-PCI hospitals in China. BMJ Open 2019;9:e031918. 10.1136/bmjopen-2019-031918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Olié V, Carcaillon-Bentata L, Thiam M-M, et al. Emergency department admissions for myocardial infarction and stroke in France during the first wave of the COVID-19 pandemic: national temporal trends and regional disparities. Arch Cardiovasc Dis 2021;114:371–80. 10.1016/j.acvd.2021.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kansagra AP, Goyal MS, Hamilton S, et al. Collateral effect of COVID-19 on stroke evaluation in the United States. N Engl J Med 2020;383:400–1. 10.1056/NEJMc2014816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andersen J, Strandberg-Larsen K, Gerds T, et al. Risk of major cardiovascular events according to educational level before and after the initial COVID-19 public lockdown: a nationwide study. J Epidemiol Community Health 2021;75:829–35. 10.1136/jech-2020-215133 [DOI] [PubMed] [Google Scholar]
- 42.Thiam M-M, Olié V, Carcaillon-Bentata L, et al. Dynamique des admissions aux Urgences pour Infarctus Du Myocarde et accident Vasculaire Cérébral Durant La Première vague de COVID-19 en France. Santé Publique 2022;Vol. 34:13b. 10.3917/spub.220.0013b [DOI] [Google Scholar]
- 43.Douillet D, Dupont C, Leloup N, et al. Prevalence and characterization of forgoing care: comparison of two prospective multicentre cohorts between pre-COVID-19 era and a lockdown period. Arch Public Health 2022;80:32. 10.1186/s13690-022-00797-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-073933supp001.pdf (1.1MB, pdf)
bmjopen-2023-073933supp002.pdf (156KB, pdf)
Data Availability Statement
Data are available on reasonable request. Deidentified participant data will be available on reasonable request. Proposals may be submitted to the corresponding author. Data requestors will need to sign a data access agreement.