Abstract
Objectives
The relationship between exercise training variables and clinical outcomes in low back pain (LBP) is unclear. The current study aimed to explore the relationship between exercise training parameters and pain intensity in individuals with chronic LBP.
Methods
This study is a secondary analysis of a previously reported randomised controlled trial comparing the effects of general strength and conditioning to motor control exercises and manual therapy. This secondary analysis includes adults with chronic LBP (n=20) randomised to the general strength and conditioning programme only. Primary outcomes of this analysis were exercise training parameters (time under tension, rating of perceived exertion (RPE), session duration, session-RPE and training frequency) and pain intensity (0–100 mm visual analogue acale) measured every 2 weeks from baseline to 6 months follow-up. Linear mixed models with random effects (participants) and allowance for heterogeneity of variance (study date) were used to determine the association between pain intensity and training parameters over time.
Results
Mean (95% CI) pain intensity decreased over time from baseline to 6 months follow-up by 10.7 (2.8 to 18.7) points (p=0.008). Over the 6-month intervention, lower pain intensity was associated with higher RPE (β (95% CI) −27.168 (−44.265 to –10.071), p=0.002), greater time under tension (−0.029 (–0.056 to –0.001), p=0.040) and shorter session duration (1.938 (0.011 to 3.865), p=0.049).
Conclusion
During 6 months of general strength and conditioning, lower pain intensity was associated with higher participant-reported training intensity, greater volume and shorter session duration. To ensure positive outcomes to exercise training, these variables should be monitored on a short-term basis.
Trial registration number
ACTRN12615001270505.
Keywords: Rehabilitation, Exercise physiology, Back injuries, Exercise rehabilitation
WHAT IS ALREADY KNOWN ON THIS TOPIC
Exercise training is recommended for managing chronic low back pain. However, the ideal training parameters (eg, volume and intensity) for maximising outcomes remain unclear.
WHAT THIS STUDY ADDS
This study shows that higher training intensity, greater volume and shorter session duration were associated with lower pain intensity during 6 months of strength and conditioning. Importantly, training frequency did not impact results.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Clinicians should monitor training intensity, volume and session duration over a weekly basis to ensure positive outcomes to exercise training when working with adults with chronic low back pain.
Introduction
Low back pain (LBP) represents a major healthcare issue affecting 7.3% of people worldwide1 and accounts for 63 million disability-adjusted life-years.2 Exercise training is recommended in best-practice guidelines for managing chronic LBP (ie, pain persisting ≥3 months),3 with certain modes (ie, resistance training, Pilates and motor control exercises) more effective at reducing pain intensity and disability when compared across all exercise types.4 However, the ideal training parameters (eg, volume and intensity) for maximising outcomes remain unclear.5 For example, resistance training is widely used in clinical practice for individuals with LBP,6 yet training parameters are based on evidence from untrained healthy populations, where 1–3 sets of 8–12 repetitions of each exercise are recommended to achieve improvements in muscular strength and hypertrophy.6–9 Despite studies exploring ideal exercise training parameters (eg, volume, intensity, duration, frequency) in healthy populations,10–12 there are a limited number of studies that compare how these variables impact recovery in individuals with LBP.
In a meta-regression (50 trials, n=1239) of individuals with chronic LBP, completing stabilisation exercises 3–5 times per week had the largest effect on improving both pain intensity and disability.13 However, completing more than five training sessions per week led to a reduced effect. In this instance, the optimal session duration was 20–30 min, with longer durations (>30 min) shown to be less effective at reducing pain intensity and disability. A separate meta-analysis of 43 trials in chronic LBP (n=3226) compared interventions that included any mode of exercise training (eg, resistance training, stretching and aerobic exercise),14 and showed that high-dose exercise programmes with >20 hours of total exercise training over the intervention were more effective at reducing pain intensity and disability than those consisting of <20 hours. In a narrative review that explored isolated lumbar extensor resistance training, Steele et al15 found that completing low-frequency (1 day per week), high-intensity (training to muscular failure) was most effective at reducing pain intensity and disability in individuals with chronic LBP. Finally, in a study carried out by the current authors, a 6-month periodised strength and conditioning programme was effective at reducing pain intensity in individuals with chronic LBP.16 However, it is not yet clear if specific training parameters (ie, volume, intensity, duration and frequency) were associated with these reductions in pain intensity.
These studies provide preliminary evidence to suggest optimal exercise training parameters may exist for individuals with LBP undertaking an exercise intervention. However, it remains unclear if controlling these training parameters in individual sessions are necessary for improvements seen in exercise training programmes, and if so, which training parameters are most important. Understanding which training variables have the greatest impact on modifying outcomes, such as pain intensity, will help clinicians design more effective exercise training programmes for individuals with LBP. Therefore, the aim of the current study was to explore the relationship between exercise training parameters and pain intensity in individuals with chronic LBP to identify which training parameters are associated with clinical outcomes. The secondary aim was to evaluate whether this relationship differed based on the time period over which they were monitored (ie, per session, week or 2 weeks). It was hypothesised that exercise training volume, intensity and duration would be associated with lower pain intensity and that measuring these variables over a weekly basis would provide the most information to guide exercise training design.
Methods
Trial design
This study is a secondary analysis of a previously reported parallel randomised controlled trial.17 The full study protocol is described in detail elsewhere.18 In brief, the study randomised participants to receive a 6-month exercise intervention consisting of general strength and conditioning or motor control and manual therapy.16 17 Due to differences in the recording of training data in the motor control and manual therapy group, complete information on training parameters was not available for this group. Motor control and manual therapy sessions were completed at a separate site (Advance HealthCare, Boronia, Victoria, Australia) and the training parameters of time under tension and rating of perceived exertion (RPE) were not recorded. Therefore, this analysis includes data only from the 20 participants randomised to general strength and conditioning. Data collection and exercise sessions were completed at Deakin University.
Participants
Adults aged 25–45 years with chronic non-specific LBP (≥3 months) were recruited from the metropolitan Melbourne region via print and web-based advertising. Participants who registered their interest through the study website were screened via phone by one of the researchers involved in the study to assess eligibility. Inclusion and exclusion criteria were based on primary outcomes of intervertebral disc health. Inclusion criteria were pain between the T12 vertebra and gluteal folds of 2–8 points on a 0–10 point Numerical Rating Scale. Exclusion criteria were: (a) previous or planned spinal surgery, (b) traumatic spinal injury (eg, fracture or car accident), (c) cauda equina symptoms, (d) known structural scoliosis, (e) radiculopathy, (f) non‐musculoskeletal causes of LBP, (g) the inability to communicate in English, (h) current LBP treatment or undertaking >150 min per week of self‐reported moderate‐vigorous exercise, (i) current compensable claim for their LBP, (j) currently pregnant, planning a pregnancy or given birth within the last 9 months, (k) current smoker, (l) current anaemia, (m) body mass ≥120 kg, (n) history of seizures, epilepsy, stroke or head injury, (o) taking medications for mental illness, (p) have metal implants unsuitable for MRI, (q) having had nuclear medicine performed in last 3 months or (r) are unable to commit to the entire 6-month programme.
Interventions
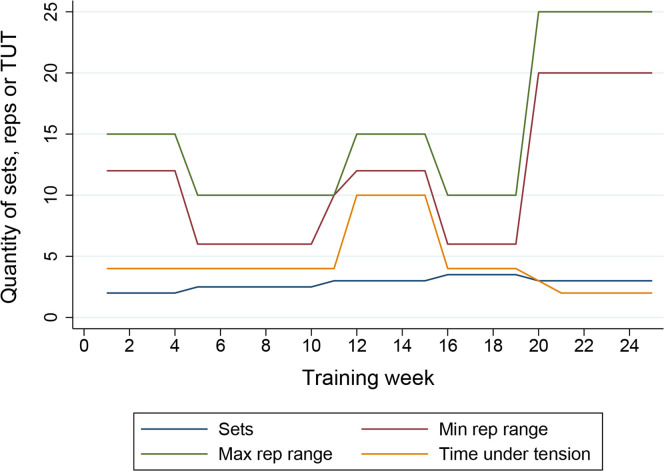
This secondary analysis only examined participants allocated to the general strength and conditioning intervention. Over 6 months, participants were prescribed up to 52 1 hour gym-based sessions supervised by an exercise physiologist (ie, a tertiary qualified exercise professional). Participants attended two sessions per week during weeks 1–13 and then self-selected to attend either one or two sessions per week during weeks 14–26. Sessions included aerobic conditioning, progressive resistance training and proprioceptive exercises. Aerobic conditioning consisted of 20 min of treadmill walking/jogging at the start of each session. This included a 5 min warm-up of increasing intensity, followed by 15 min of sustained effort at 65%–70% maximal heart rate in the first 2 weeks and increasing to 65%–85% from week three onwards. Proprioceptive training consisted of general balance (eg, tandem stance with eyes closed), weight transfer (eg, single leg dumbbell transfer left to right hand) and external perturbation (eg, medicine ball chest throw and catch) exercises. The resistance training component included five exercises each session from a selection of seven exercises grouped according to action: push, pull, lift, trunk extension and trunk flexion (online supplemental table 1). Each set was completed to two repetitions (reps) below volitional fatigue of the target rep range. The programme included six mesocycles (ie, 4–6 weeks training blocks) of varying loads, reps, sets and time under tension, as shown in figure 1. Resistance was progressed in a time-contingent manner and not modified in response to daily changes in reported pain (table 1). During each phase, resistance was increased once the target number of sets and reps were completed in two consecutive training sessions at a given resistance. In addition to gym-based sessions, unsupervised home-based exercise was recommended, consisting of 20–40 min of aerobic exercise (eg, walking or jogging at 65%–85% maximal heart rate), followed by stretching three times per week.
Figure 1.
Planned resistance training programme including weekly repetitions, sets and time under tension. Max rep range: maximum repetitions per set, min rep range: minimum repetitions per set.
Table 1.
Resistance training programme overview
| Week | Goal | Intensity | Time under tension | Progression |
| 1–4 | Familiarisation, motor control and local muscular endurance | 12–15 reps performed at 2 reps below volitional fatigue×2 sets, 1 min rest between sets | 2 s con, 2 s ecc |
Once 2 sets of 15 reps at 2 consecutive training sessions are completed, resistance is increased |
| 5–10 | Muscular strength | 6–10 reps performed at 2 reps below volitional fatigue×2–3 sets, 2 min rest between sets | 2 s con, 2 s ecc |
Once 2 sets of 10 reps at 2 consecutive training sessions are completed, workload increases to 3 sets. Then progression made through increased resistance |
| 11 | Light week | 10 reps at 80% of resistance used in the previous week×3 sets, 2 min rest between sets | 2 s con, 2 s ecc |
None |
| 12–15 | Local muscular endurance | 12–15 reps performed at 2 reps below volitional fatigue×3 sets, 1 min rest between sets | 5 s con, 5 s ecc |
Once 3 sets of 15 reps at 2 consecutive training sessions are completed, resistance is increased |
| 16–19 | Muscular strength | 6–10 reps performed at 2 reps below volitional fatigue×3–4 sets, 2 min rest between sets | 2 s con, 2 s ecc |
Once 3 sets of 10 reps at 2 consecutive training sessions are completed, workload increases to 4 sets. Then progression made through increased resistance |
| 20–25 | Local muscular endurance | 20–25 reps performed at 2 reps below volitional fatigue×3 sets, 1 min rest between sets | 1–2 s con, 1–2 s ecc |
Once 3 sets of 25 reps at 2 consecutive training sessions are completed, resistance is increased |
Con, concentric; ecc, eccentric; reps, repetitions.;
bmjsem-2023-001744supp001.pdf (14.2KB, pdf)
Outcomes
Each outcome is discussed in depth elsewhere18 and in brief below. Average LBP intensity over the previous week was collected every 2 weeks via online questionnaires from baseline to end of intervention (6 months) using a 0–100 mm visual analogue scale (VAS). This is a valid and reliable measure of pain intensity in LBP.19 For individuals with chronic LBP, a 20-point reduction in pain intensity is considered the minimum clinically meaningful difference.20 Self-reported disability due to LBP was collected at baseline using the modified Oswestry Disability Index.21 The questionnaire includes 10 items addressing various aspects of physical function. The total score (0–50 points) is doubled and represented as a score between 0 and 100 with higher scores indicating greater disability. For individuals with LBP, a 10-point reduction in disability is considered the minimum clinically meaningful difference.22 Additionally, exercise training data, including attendance, exercises completed, resistance, sets, reps, session duration and participant-reported RPE (10-point scale), were collected at each supervised training session. From these data, the following additional variables were calculated:
Time under tension is a measure of volume that refers to the total duration a muscle spends under tension during both concentric and eccentric phases of resistance exercise.23 Time under tension per session (sec) was calculated as the sum of time under tension across the five resistance exercises for each training session (eg, week 1, session 1 time under tension=132 reps×4 s time under tension=528 s).
Session-RPE is a measure of training load that takes into consideration both the intensity and the duration of a training session.24 It is calculated as the product of session duration and RPE and expressed in arbitrary units.
In addition to the measures of time under tension, RPE, duration and session-RPE for each individual training session, weekly and 2 weekly totals were calculated by summing the numbers from each session attended during the respective week or 2-week period (eg, week 1 time under tension = (week 1, session 1 time under tension: 132 reps×4 s=528 s)+(week 1, session 2 time under tension: 138 reps×4 s=552 s)=1080 s). Weekly and 2-weekly training frequency was calculated as the total number of sessions attended over the past week or 2-week period.
Sample size
The original sample size calculation was based on intervertebral disc health outcomes for the larger study,17 whereby 20 participants in each group were required to detect a 2.2% between-group net difference in average lumbar intervertebral disc T2.
Randomisation
Participants were randomly assigned (1:1) using block randomisation with random block lengths and stratification for sex obtained from www.random.org. A researcher who had no contact with participants obtained and employed the randomisation schedule (via sequentially numbered, opaque, sealed envelopes).
Blinding
Given the primary outcome of interest was subjective pain intensity, the participant was considered the assessor; therefore, it was not possible to blind the outcome assessor in this secondary analysis.
Statistical methods
All analyses were completed using Stata (V.17, StataCorp). To determine the association between pain intensity and training parameters (time under tension, RPE, session duration, frequency and session-RPE) over 6 months from baseline to follow-up, linear mixed models with random effects (participants) and allowance for heterogeneity of variance according to study date were used. For these associations, each training parameter was examined for the session, week and 2 weeks prior to pain intensity being measured. Missing data were dealt with using a maximum likelihood estimation within linear mixed models, satisfying intention‐to‐treat principles.25 There were 273 missing data points from a possible total of 4260 (6.4% missing) across 5 variables. The greatest number of missing data was from the variable session duration with 126 missing data points from a possible total of 1000 (12.6% missing). An alpha of 0.05 was adopted for all analyses.
Results
Participant flow
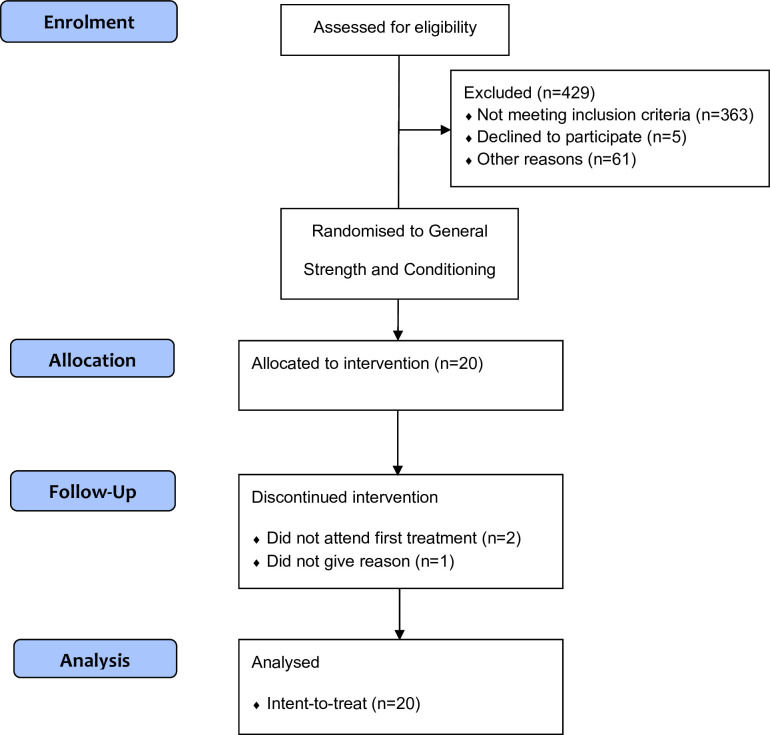
Twenty participants (female: n=10; male: n=10) were randomised to receive general strength and conditioning (figure 2). Three participants withdrew from the study between baseline and follow-up with 17 participants remaining at 6 months (figure 2).
Figure 2.
CONSORT diagram. CONSORT, Consolidated Standards of Reporting Trials.
Recruitment
This study was conducted from December 2015 to December 2016. The trial ended when all recruited participants finished the 6-month follow-up period.
Baseline data
Baseline demographic data are shown in table 2. Mean (SD) age at baseline was 35 (5) years, LBP intensity was 41 (18) points (mild pain)26 and disability was 24.5 (12.1) per cent (moderate disability).27 Females tended to have greater mean (SD) body mass index (female: 29.1 (5.5) kg/m2, male: 25.5 (3.8) kg/m2), age (female: 35.5 (6.3) years, male: 34.2 (3.6) years) and disability (female: 25.1 (11.4) points, male: 24.0 (13.1) points), yet lower pain intensity (female: 36.9 (16.7) points, male: 45.1 (18.5) points).
Table 2.
Baseline demographic data
| Mean (SD) | |
| Age, years | 35 (5) |
| Female, n (%) | 10 (50) |
| Height, cm | 172.5 (9.1) |
| Weight, kg | 76.9 (16.8) |
| Body mass index, kg/m2 | 27.1 (4.9) |
| Pain, 0–100 VAS | 41 (18) |
| Disability, % on Oswestry index | 24.5 (12.1) |
VAS, visual analogue scale.
Numbers analysed
All 20 participants randomised to general strength and conditioning were included in the current study.
Outcomes and estimation
Per session, mean (SD) time under tension was 739.26 (503.38) s, RPE was 7.18 (3.01) points, session duration was 64 (11) min and session-RPE was 460.01 (145.98) arbitrary units. Mean (SD) training frequency was 1.20 (0.85) sessions per week, which equated to 31 out of a possible 52 sessions (60%) over the 6-month intervention.
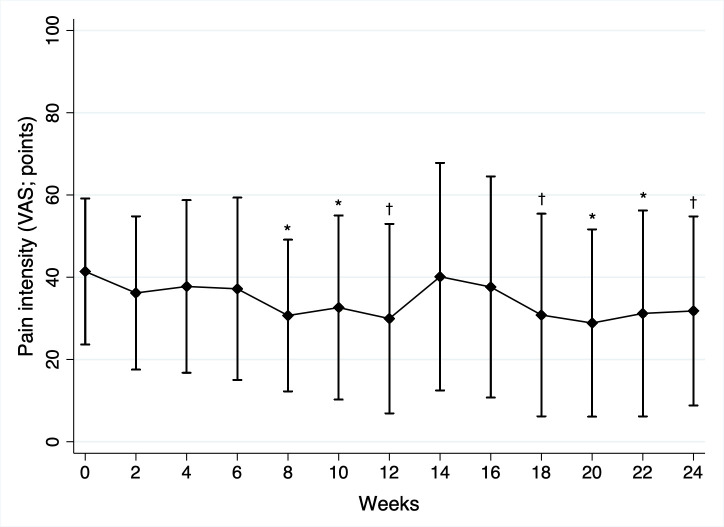
Mean (95% CI) pain intensity decreased from baseline to 6 months follow-up by 10.7 (2.8 to 18.7, p=0.008) points (figure 3). Between baseline and follow-up, pain intensity was negatively associated with time under tension during the preceding week (β (95% CI) −0.029 (−0.056 to –0.001), p=0.040) and RPE of the prior session (−27.168 (−44.265 to –10.071), p=0.002) and positively associated with duration of the prior session (1.938 (0.010 to 3.865), p=0.049; table 3). No association was found between pain intensity and other training parameters at any time point.
Figure 3.
Mean (SD) 2-weekly pain intensity (100-point visual analogue scale (VAS)). *p<0.05, †p<0.01 indicate within‐group change from baseline.
Table 3.
Association between pain intensity and training parameters over the prior session, week and 2-week period
| Training parameter | β | 95% CI | P value | |
| Time under tension | ||||
| Session | 0.004 | −0.449 | 0.457 | 0.985 |
| Week | −0.029* | −0.056 | −0.001 | 0.040 |
| 2 weeks | −0.007 | −0.026 | 0.011 | 0.443 |
| Rating of perceived exertion | ||||
| Session | −27.168* | −44.265 | −10.071 | 0.002 |
| Week | −1.103 | −4.645 | 2.439 | 0.542 |
| 2 weeks | −1.271 | −3.083 | 0.540 | 0.169 |
| Session duration | ||||
| Session | 1.938* | 0.010 | 3.865 | 0.049 |
| Week | 0.070 | −0.433 | 0.572 | 0.785 |
| 2 weeks | 0.026 | −0.168 | 0.221 | 0.792 |
| Training frequency | ||||
| Session | 0.007 | −0.260 | 0.273 | 0.962 |
| Week | −0.018 | −0.084 | 0 .048 | 0.591 |
| 2 weeks | −0.009 | −0.038 | 0.019 | 0.518 |
| Session rating of perceived exertion | ||||
| Session | 9.456 | −8.141 | 27.054 | 0.292 |
| Week | −4.763 | −15.724 | 6.197 | 0.394 |
| 2 weeks | −1.545 | −7.618 | 4.529 | 0.618 |
Data are β coefficient, 95% CI and p value. Negative coefficients suggest that higher training parameters are associated with lower pain intensity.
*p<0.05.
Harms
No adverse events were reported.
Discussion
In individuals with chronic LBP, pain intensity decreased following 6 months of general strength and conditioning but did not reach the minimum clinically meaningful difference of 20 points.20 As hypothesised, pain intensity was negatively associated with time under tension and participant reported RPE and positively associated with training session duration. Additionally, these associations were found when measuring the training parameters over the prior week (for time under tension) and session (for duration and RPE). Pain intensity was not associated with the frequency of training sessions or session-RPE at any time point (sessional, weekly or 2 weekly).
The current study showed that the exercise training variables of time under tension, RPE and training session duration were associated with pain intensity across a 6-month periodised programme of general strength and conditioning. A negative association observed with time under tension indicates that greater weekly volume (measured via time under tension) corresponded to lower pain intensity. For reference, every 60 s increase in weekly time under tension was associated with a lower pain intensity of 1.74 points. Similar results were seen in a study of 352 female office workers with musculoskeletal pain (various non-specific conditions), where total training volume was correlated with pain intensity following 16 weeks of resistance training.28 This suggests that for an exercise programme to be beneficial, a sufficient stimulus must be achieved to facilitate a physiological response to training. Likewise, the negative association between RPE and pain intensity found in the current study suggests that higher participant-reported intensities led to greater reductions in pain intensity. This finding is strengthened by the programme design, which was periodised with heavy and light blocks and progressed in a time-contingent manner irrespective of pain intensity. In other words, training intensity was not increased in response to decreases in pain intensity, which could lead to spurious findings. Similar benefits for high-intensity training have been found in individuals with chronic LBP following a 12-week programme of general strength and conditioning.29 Those completing the programme at a high intensity (100% VO2max and 80% 1RM) reported greater reductions in disability compared with those training at moderate intensity (60% VO2max and 60% 1RM), without any between-group differences in adverse events or adherence. Additionally, a meta-analysis of exercise training studies in individuals with chronic musculoskeletal conditions showed that protocols where participants ‘pushed into pain’ (up to 50 mm on a 100-point VAS) reported greater short-term improvements in pain intensity compared with protocols completed within a pain-free range.30 Combined, these results suggest a higher training intensity and volume may be beneficial for maximising outcomes in individuals with chronic LBP, even when participants report pain during exercise. However, it is unclear where the ceiling of this effect lies for maximising benefit while minimising the risk of adverse events. Future research should seek to identify an upper limit to exercise training volume and intensity that is safe and effective which may be best identified using non-linear modelling.
Despite correlations with other training variables, the current analysis showed that the number of weekly sessions attended over 6 months (training frequency; range: 0–2/week) was not related to improvements in pain intensity. Similar results were seen in the aforementioned study of female office workers with musculoskeletal pain,28 where training attendance (range: 0–3/week) was not correlated with reductions in pain intensity. It is unclear from the current results if the lack of relationship observed between pain intensity and training frequency would differ if participants had access to more than two training sessions per week. For example, when completing stabilisation exercises, 3–5 sessions per week has the greatest impact on improving LBP intensity.13 However, a direct translation between stabilisation exercise and general strength and conditioning is difficult due to the different mechanisms of action (eg, changes to motor control vs strength and capacity). Therefore, future research should explore the dose–response relationship between pain intensity and weekly attendance during a general strength and condition programme in which participants are randomised to low, medium and high training frequencies.
Importantly, the associations between pain intensity and training parameters were observed on a weekly (for time under tension) and sessional (for duration and RPE) basis. While monitoring training parameters over a 2-weekly basis did not provide any additional insight. To our knowledge, this is the first study to explore different time periods over which to measure pain intensity and training parameters. Analysing the response to training parameters measured over sessional, weekly and 2-weekly intervals can help to differentiate between acute and chronic responses to training load and intensity. The current findings suggest that short-term responses following a session or week of exercise training are more indicative of positive outcomes than intermediate responses (ie, 2 weekly). Additionally, measuring session duration alongside volume and training intensity on a short-term basis may prove important in reducing the risk of pain ‘flare-ups’ due to excessive exposure.
Clinical implications
When designing a general strength and conditioning programme for individuals with chronic LBP, training intensity and volume may be important variables to consider, with increased training intensity and volume associated with improvements in pain intensity. Therefore, ensuring the prescribed training load is adequate within each session to provide sufficient stimulus appears necessary to maximise reductions in pain intensity. Additionally, training session duration should be monitored alongside pain intensity to avoid periods of excessive load leading to poorer outcomes. When considering a programme consisting of up to two sessions per week, regular training frequency may not be the most important variable for reducing pain intensity. This information may be beneficial for individuals with limited resources (eg, time and money) to complete more than one training session per week. Additionally, individuals should not be discouraged if they miss a week of exercise training, as they can still achieve positive results from a general strength and conditioning programme.
Strengths and limitations
The current study provides valuable information to guide the delivery of exercise training interventions in individuals with chronic LBP. We used a single-item validated outcome measure to track pain intensity (VAS) every 2 weeks throughout the programme, which allowed us to explore how the accumulation of volume, duration and intensity impacted outcomes across a 2-week period. Additionally, allowing participants to self-select training frequency in the second half of the programme provides a pragmatic foundation to explore how training frequency interacts with recovery. However, the current study is not without limitations. First, pain intensity was the only outcome measure tracked on a 2-weekly basis. It is unclear how training variables relate to other outcomes that may be important in individuals with chronic LBP, such as disability, kinesiophobia, strength and muscular endurance. Training variables such as training frequency may be associated with these additional outcomes and retain importance in programme design. Second, while the single-item pain intensity VAS is a simple measure to administer and track, it does not distinguish between the type of pain experienced (eg, joint pain, neuropathic pain, general soreness). Hence, we could not determine whether pain intensity observed during some 2-week periods was due to an inability of neuromuscular tissue to cope with the imposed loads, an acute response due to delayed onset muscle soreness, a chronic overtraining response or other natural variations in pain. Future studies may benefit from measuring pain intensity more frequently around training sessions (eg, pre-exercise and postexercise session and 24 hours post) in addition to using a specific outcome measure to account for delayed onset muscle soreness. Third, additional training measures (eg, volume-load, weekly physical activity, metabolic equivalent) may have provided further information to identify which specific mode, volume or intensity variables most closely underpin the changes in pain intensity observed. Fourth, training data from the original randomised controlled trial pertaining to the motor control and manual therapy group were not available for analysis due to differences in recording. Fifth, these results are limited to adults aged 25–45 years with non-specific chronic LBP weighing less than 120 kg. Caution should be taken if generalising these findings to the broader public. Finally, although planned, most participants failed to return home-based exercise diaries at 3 and 6 months. Future studies should consider alternative methods of collecting home-based training compliance, such as via digital record keeping or wearable technology.
Conclusion
During a 6-month general strength and conditioning programme, lower pain intensity was associated with higher participant-reported exercise training intensity, greater volume and shorter session duration. When prescribing exercise training for individuals with chronic LBP, monitoring and controlling these variables over a short-term basis is recommended to achieve the best outcomes. Importantly, training frequency did not impact results. Future research should explore the ideal intensity, volume and duration of strength and conditioning programmes in individuals with chronic LBP and include additional exercise training variables to provide further guidance.
Acknowledgments
The authors thank the participants for taking part in the study.
Footnotes
Twitter: @chris_neason, @_clintmiller, @ScottTags, @belavyprof, @LuanaCMain, @PatrickOwenPhD
Contributors: CN contributed to data curation, formal analysis, funding acquisition, visualisation and writing–original draft. CM contributed to conceptualisation, investigation, project administration and supervision. SDT contributed to data curation. DLB contributed to conceptualisation, funding acquisition, investigation, project administration, resources and supervision. LCM contributed to investigation. JF contributed to conceptualisation, investigation and resources. AJH contributed to conceptualisation, investigation, project administration and resources. SJB contributed to formal analysis and validation. PJO (guarantor) contributed to conceptualisation, data curation, investigation, project administration, software, supervision, validation and visualisation. All authors contributed to methodology and writing–review and editing. All authors read and approved the final version of the manuscript, and agreed with the order of presentation of the authors.
Funding: This project was supported by Deakin University under separate internal institutional funding (original study: DLB; analyses: CN).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Deakin University Human Research Ethics Committee on 12 October 2015 (project ID: 2015‐191). Participants gave informed consent to participate in the study before taking part.
References
- 1.Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the global burden of disease study 2015. The Lancet 2016;388:1545–602. 10.1016/S0140-6736(16)31678-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute for Health Metrics and Evaluation . Global health group data exchange. Available: http://ghdx.healthdata.org/gbd-results-tool [Accessed 18 May 2022].
- 3.Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J 2018;27:2791–803. 10.1007/s00586-018-5673-2 [DOI] [PubMed] [Google Scholar]
- 4.Owen PJ, Miller CT, Mundell NL, et al. Which specific modes of exercise training are most effective for treating low back pain? network meta-analysis. Br J Sports Med 2020;54:1279–87. 10.1136/bjsports-2019-100886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cashin AG, Booth J, McAuley JH, et al. Making exercise count: considerations for the role of exercise in back pain treatment. Musculoskeletal Care 2022;20:259–70. 10.1002/msc.1597 [DOI] [PubMed] [Google Scholar]
- 6.Rainville J, Hartigan C, Martinez E, et al. Exercise as a treatment for chronic low back pain. Spine J 2004;4:106–15. 10.1016/s1529-9430(03)00174-8 [DOI] [PubMed] [Google Scholar]
- 7.Feigenbaum MS, Pollock ML. Prescription of resistance training for health and disease. Med Sci Sports Exerc 1999;31:38–45. 10.1097/00005768-199901000-00008 [DOI] [PubMed] [Google Scholar]
- 8.Carpenter DM, Nelson BW. Low back strengthening for the prevention and treatment of low back pain. Med Sci Sports Exerc 1999;31:18–24. 10.1097/00005768-199901000-00005 [DOI] [PubMed] [Google Scholar]
- 9.Ratamess N, Alvar B, Evetoch T, et al. Progression models in resistance training for healthy adults [ACSM position stand]. Med Sci Sports Exerc 2009;41:687–708. 10.1249/MSS.0b013e3181915670 [DOI] [PubMed] [Google Scholar]
- 10.Grgic J, Schoenfeld BJ, Latella C. Resistance training frequency and Skeletal muscle hypertrophy: A review of available evidence. J Sci Med Sport 2019;22:361–70. 10.1016/j.jsams.2018.09.223 [DOI] [PubMed] [Google Scholar]
- 11.Baz-Valle E, Fontes-Villalba M, Santos-Concejero J. Total number of SETS as a training volume Quantification method for muscle hypertrophy: A systematic review. J Strength Cond Res 2021;35:870–8. 10.1519/JSC.0000000000002776 [DOI] [PubMed] [Google Scholar]
- 12.Evans JW. Periodized resistance training for enhancing Skeletal muscle hypertrophy and strength: A mini-review. Front Physiol 2019;10:13. 10.3389/fphys.2019.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mueller J, Niederer D. Dose-response-relationship of stabilisation exercises in patients with chronic non-specific low back pain: a systematic review with meta-regression. Sci Rep 2020;10:16921. 10.1038/s41598-020-73954-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med 2005;142:776–85. 10.7326/0003-4819-142-9-200505030-00014 [DOI] [PubMed] [Google Scholar]
- 15.Steele J, Bruce‐Low S, Smith D. A review of the clinical value of isolated lumbar extension resistance training for chronic low back pain. PM&R 2015;7:169–87. 10.1016/j.pmrj.2014.10.009 [DOI] [PubMed] [Google Scholar]
- 16.Tagliaferri SD, Miller CT, Ford JJ, et al. Randomized trial of general strength and conditioning versus motor control and manual therapy for chronic low back pain on physical and self-report outcomes. J Clin Med 2020;9:1726. 10.3390/jcm9061726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Owen PJ, Miller CT, Rantalainen T, et al. Exercise for the Intervertebral disc: a 6-month randomised controlled trial in chronic low back pain. Eur Spine J 2020;29:1887–99. 10.1007/s00586-020-06379-7 [DOI] [PubMed] [Google Scholar]
- 18.Simson KJ, Miller CT, Ford J, et al. Optimising conservative management of chronic low back pain: study protocol for a randomised controlled trial. Trials 2017;18:184. 10.1186/s13063-017-1913-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shafshak TS, Elnemr R. The visual analogue scale versus numerical rating scale in measuring pain severity and predicting disability in low back pain. J Clin Rheumatol 2021;27:282–5. 10.1097/RHU.0000000000001320 [DOI] [PubMed] [Google Scholar]
- 20.Ostelo RWJG, de Vet HCW. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 2005;19:593–607. 10.1016/j.berh.2005.03.003 [DOI] [PubMed] [Google Scholar]
- 21.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys Ther 2001;81:776–88. 10.1093/ptj/81.2.776 [DOI] [PubMed] [Google Scholar]
- 22.Tagliaferri SD, Miller CT, Owen PJ, et al. Domains of chronic low back pain and assessing treatment effectiveness: A clinical perspective. Pain Pract 2020;20:211–25. 10.1111/papr.12846 [DOI] [PubMed] [Google Scholar]
- 23.Tran QT, Docherty D. Dynamic training volume: a construct of both time under tension and volume load. J Sports Sci Med 2006;5:707–13. [PMC free article] [PubMed] [Google Scholar]
- 24.Haddad M, Stylianides G, Djaoui L, et al. Session-RPE method for training load monitoring: validity, ecological usefulness, and influencing factors. Front Neurosci 2017;11:612. 10.3389/fnins.2017.00612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horton NJ, Kleinman KP. Much Ado about nothing: A comparison of missing data methods and software to fit incomplete data regression models. Am Stat 2007;61:79–90. 10.1198/000313007X172556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boonstra AM, Schiphorst Preuper HR, Balk GA, et al. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014;155:2545–50. 10.1016/j.pain.2014.09.014 [DOI] [PubMed] [Google Scholar]
- 27.Fairbank JCT, Pynsent PB. The Oswestry disability index: spine. Spine 2000;25:2940–53. 10.1097/00007632-200011150-00017 [DOI] [PubMed] [Google Scholar]
- 28.Pedersen MT, Andersen LL, Jørgensen MB, et al. Effect of specific resistance training on musculoskeletal pain symptoms: dose-response relationship. J Strength Cond Res 2013;27:229–35. 10.1519/JSC.0b013e3182541ceb [DOI] [PubMed] [Google Scholar]
- 29.Verbrugghe J, Agten A, Stevens S, et al. Exercise intensity matters in chronic nonspecific low back pain rehabilitation. Med Sci Sports Exerc 2019;51:2434–42. 10.1249/MSS.0000000000002078 [DOI] [PubMed] [Google Scholar]
- 30.Smith BE, Hendrick P, Smith TO, et al. Should exercises be painful in the management of chronic musculoskeletal pain? A systematic review and meta-analysis. Br J Sports Med 2017;51:1679–87. 10.1136/bjsports-2016-097383 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2023-001744supp001.pdf (14.2KB, pdf)
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.