Abstract
To assess the public health impact of the COVID-19 pandemic on mental health, investigators from the National Institutes of Health Environmental influences on Child Health Outcomes (ECHO) research program developed the Pandemic-Related Traumatic Stress Scale (PTSS). Based on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) acute stress disorder symptom criteria, the PTSS is designed for adolescent (13–21 years) and adult self-report and caregiver-report on 3–12-year-olds. To evaluate psychometric properties, we used PTSS data collected between April 2020 and August 2021 from non-pregnant adult caregivers (n = 11,483), pregnant/postpartum individuals (n = 1,656), adolescents (n = 1,795), and caregivers reporting on 3–12-year-olds (n = 2,896). We used Mokken scale analysis to examine unidimensionality and reliability, Pearson correlations to evaluate relationships with other relevant variables, and analyses of variance to identify regional, age, and sex differences. Mokken analysis resulted in a moderately strong, unidimensional scale that retained nine of the original 10 items. We detected small to moderate positive associations with depression, anxiety, and general stress, and negative associations with life satisfaction. Adult caregivers had the highest PTSS scores, followed by adolescents, pregnant/postpartum individuals, and children. Caregivers of younger children, females, and older youth had higher PTSS scores compared to caregivers of older children, males, and younger youth, respectively.
Keywords: COVID-19, traumatic stress, pandemic, survey, Mokken scaling
At the onset of the COVID-19 pandemic, little was known about the effects of the pandemic itself or mitigation efforts, such as quarantines and school closures, on children’s and caregiver’s mental health (Esposito & Principi, 2020; Golberstein et al., 2020; Torales et al., 2020). Concerns about these effects underscored the need for population-level studies to ascertain the public health implications of living through a pandemic (Brooks et al., 2020; Fegert et al., 2020; Sprang & Silman, 2013). Twenty-four prior studies of the psychological impact of quarantine/isolation after exposure to an infectious disease suggest that quarantine is associated with an increased risk of posttraumatic stress disorder (PTSD; Brooks et al., 2020). In adults and children, this risk was reported to be three to four times higher in those who did versus did not experience a quarantine (Brooks et al., 2020). Since half of the people who experience a clinically significant level of acute stress symptoms go on to develop PTSD (American Psychiatric Association, 2022), investigators from the Environmental influences on Child Health Outcomes (ECHO) program designed the Pandemic-Related Traumatic Stress Scale (PTSS; Margolis et al., 2021) to feasibly evaluate youth and caregiver pandemic-related stress symptoms in the national ECHO cohort. The scale was administered as part of a broader COVID-19 survey evaluating family hardships (e.g., job loss), behavior changes (e.g., more/less sleep), and adaptive (e.g., mindfulness practices) or maladaptive (e.g., substances use) coping strategies.
Living during a pandemic may not be viewed as an inciting event in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) definition of acute stress disorder or PTSD (American Psychiatric Association, 2022), but the COVID-19 pandemic did present to many as a life-threatening experience—both real and perceived. The highly infectious and deadly virus has been described as eliciting traumatic stress reactions above and beyond the general psychological distress experienced with pandemic-related disruptions to daily life, such as school and work closures (Bridgland et al., 2021; Horesh & Brown, 2020; Kira, 2021). Since March 2020, COVID-19 has infected nearly 80 million people in the United States, leading to an estimated 900,000 hospitalizations, of which 20% required intensive care unit intervention, and taking the lives of approximately 1 million Americans (Kaiser Family Foundation, 2022). Survivors have a one in three chance of experiencing long-term physical, mental, and cognitive consequences (Logue et al., 2021; Taquet et al., 2021). Thus, fear and experiences of contracting the virus, witnessing or putting a loved one at risk, and suffering severe illness or death reflect the life-threatening nature of the pandemic that can result in traumatic stress reactions (Kira, 2021; Kira et al., 2021).
Although little studied, many populations may be susceptible to pandemic-related traumatic stress. Pregnant and postpartum individuals are at increased risk for severe illness and poor birth outcomes from COVID-19 (Woodworth et al., 2020; Zambrano et al., 2020) and may have heightened fears for their own well-being and that of their infant (Basu et al., 2021; King et al., 2021; Preis et al., 2020). Youth represent another vulnerable population, as the pandemic greatly disrupted their daily life with school closures and lack of social interactions outside the immediate family (Creswell et al., 2021; Hertz et al., 2022; Verlenden et al., 2021). Caregivers also faced potentially traumatic experiences, taking on new roles and responsibilities that often conflicted with each other, such as abrupt shifts to working from home while also trying to manage their children’s care center closures or home-schooling, continuing to work outside the home while arranging and managing alternative childcare, or being unable to work because they needed to care for their children (Calear et al., 2022; Chen et al., 2022; Spinelli et al., 2020).
Initial studies suggest up to 50% of adults could be at risk for pandemic-related posttraumatic stress symptoms (Cooke et al., 2020; Czeisler et al., 2020; Xiong et al., 2020). While many studies measure depression, anxiety, and general stress during the pandemic (Loades et al., 2020; Prati & Mancini, 2021), few focus on traumatic reactions. Additionally, the few studies that have examined traumatic stress demonstrate large inconsistencies in prevalence—anywhere from 1% to 96% in adult samples (Hong et al., 2021) and 11% (Chen et al., 2021) to 86% (Hou et al., 2020) in the few available child studies. Moreover, most studies have been conducted outside the United States and only capture the first 6–10 months of the pandemic. Differentiating depressed mood, overall anxiety, and general stress from traumatic stress reactions fills an important gap in knowledge, given the likelihood of PTSD and related consequences stemming from traumatic stress.
Scales measuring pandemic-related traumatic stress across the lifespan were not readily available at the onset of the COVID-19 pandemic. Those that are now available are for adult samples (Cortez et al., 2020; Taylor et al., 2020). While some parent- and adolescent-report questionnaires include individual items querying COVID-19-related stress (Ladouceur, 2020), incorporate general stress and anxiety scales (Adolescent Brain Cognitive Development, 2020), or evaluate COVID-19-related worries and general mental states (Nikolaidis et al., 2021), reliable and psychometrically valid scales of pandemic-related traumatic stress do not exist for pediatric populations (Tambling et al., 2021). Further, extant adult measures combine stressors (e.g., job loss, financial strain, social distancing) with experienced stress and often confound nontraumatic and traumatic stress in the same measure. For example, the COVID-19 Stress Scales (Taylor et al., 2020) and COVID-19 Stressors Scale (Tambling et al., 2021) include resource-related concerns (e.g., sufficient household/personal supplies), financial concerns (e.g., job loss), social stressors (e.g., changes to work and school), and infection-related stressors (e.g., risk of infection) in addition to their psychological impact. Other scales evaluate COVID-19 fears, anxiety, suspicions, and somatic symptoms (Ahorsu et al., 2022; Feng et al., 2020; Qiu et al., 2020); and yet others rely on existing measures that were developed and validated to assess PTSD outside of this remarkable pandemic context (Bridgland et al., 2021; Pedrozo-Pupo et al., 2020).
Here, we investigated the psychometric properties of the PTSS (Margolis et al., 2021), which was designed to capture information assessed in a clinical interview using the DSM-5 acute stress disorder criteria classification (A and B only), but critically, without the requirement of the symptom occurring within 1 month of the exposure. The PTSS evaluates the five criteria classification domains of intrusion, dissociation, avoidance, arousal regulation problems, and negative mood, only the last of which is captured by general distress indicators (American Psychiatric Association, 2022). We investigated if: (a) responses to the PTSS were characterized by a single underlying latent dimension and (b) the scale had comparable structure across diverse populations, including populations particularly vulnerable to the effects of the COVID-19 pandemic and related mitigation strategies (i.e., pregnant/postpartum individuals, adult caregivers, adolescents, children). To establish validity evidence based on relationships with other variables (American Educational Research Association [AERA], the American Psychological Association, the National Council on Measurement in Education, 2014), we hypothesized that higher ratings of pandemic-related traumatic stress would be associated with higher levels of general perceived stress, anxiety, and depressive symptoms and lower levels of life satisfaction. We also explored group differences, asking: (a) does pandemic-related traumatic stress differ by US region? and hypothesizing: (b) postpartum individuals would have higher PTSS scores compared to pregnant individuals, based on studies finding greater traumatic stress levels in the postpartum period following a natural disaster or pandemic (Basu et al., 2021; Molgora & Accordini, 2020); (c) adult caregivers of younger (<5 years) children would have higher PTSS scores compared to those of older children (5–12 years) and adolescents (13–21 years), given prior work suggesting families with young children are more vulnerable to postdisaster trauma (Baker & Cormier, 2014; Brooks et al., 2020); (d) female adult caregivers would have higher PTSS scores compared to male adult caregivers, given research showing females are more likely to experience psychological distress and PTSD symptoms following traumatic events compared to males (Patel et al., 2022; Wang et al., 2020; Yuan et al., 2021); and (e) older and female children/adolescents would have higher PTSS scores compared to younger and male children/adolescents, respectively, based on emerging evidence that older and female youth experienced greater stress during the pandemic than younger and male youth, respectively (Loades et al., 2020; Magson et al., 2021; Marques de Miranda et al., 2020).
Method
Data were collected as part of the National Institutes of Health ECHO program, a large multicohort research consortium comprising 69 existing pediatric longitudinal observational cohorts with approximately 50,000 children and their caregivers from across the United States and Puerto Rico (Blaisdell et al., 2021; Gillman & Blaisdell, 2018). ECHO’s main objective is to understand the impact of early life environmental exposures (e.g., biological, chemical, built, social) on five primary child outcomes: pre-, peri-, and postnatal outcomes (e.g., small for gestational age, preterm birth); obesity; airways-related outcomes (e.g., asthma); neurodevelopment (e.g., cognition, psychopathology); and positive health (e.g., well-being). Here, we include 47 ECHO cohorts with data on pandemic-related stress. Local cohort and central ECHO institutional review boards (IRBs) reviewed all research methods and procedures, and the work of the ECHO Person Reported Outcome Core was overseen by the Northwestern University IRB.
Participants
Data were divided into four distinct participant samples. The child sample included n = 2,896 caregivers reporting on their 3–12-year-old children from 24 ECHO cohorts; the adolescent sample included n = 1,795 13–21-year-olds from 16 ECHO cohorts; the nonpregnant adult caregiver sample included n = 11,483 adult caregivers from 45 ECHO cohorts; and the pregnant/postpartum sample included n = 1,656 pregnant individuals or individuals who recently gave birth (i.e., gave birth after February 29, 2020, but before completing the PTSS) from 26 ECHO cohorts. The samples were mutually exclusive with respect to PTSS response data given the defining characteristics of such samples (i.e., being a 3–12-year-old child, a 13–21-year-old adolescent; a nonpregnant adult caregiver; or a pregnant/postpartum individual). We note there is some (<25%) family overlap across samples where a participant in one sample was related to another participant in a different sample. Specifically, of the individuals in the adult caregiver sample, 22.4% reported on their 3–12-year-old child, 10.8% had an adolescent in the 13–21-year-old adolescent self-report sample, and n = 11 adult caregivers had both a 3–12-year-old and an adolescent. Of the individuals in the pregnant/postpartum sample, <5% reported on their 3–12-year-old child, <.01% had an adolescent in the 13–21-year-old adolescent self-report sample; and no individual had both a 3–12-year-old and an adolescent.
Measures
Measures were collected between April 2020 and August 2021, except for existing sociodemographic data. Given the structure of ECHO and variability in whether and when cohorts collect specific assessments, not all cohorts administered the measures used to assess relationships with other related variables. Therefore, different subsamples provided data for each measure. We included multiple external measures of the same construct to maximize sample size and enhance validity evidence based on relationships with other variables, noting ≤3% within a subsample completed all external measures. Additionally, external measures were not always completed by participants on the exact same day as the PTSS, and we therefore limited these subsamples to participants who completed measures at the same time as or ±30 days from the PTSS items. Some validation measures used a 7-day recall period, but prior work finds little difference in participant response patterns for a 7- versus 30-day recall (Batterham et al., 2019; Lai et al., 2009), justifying the use of this 30-day window. See Supplemental Tables 2–5, for subsample descriptions by external validation measure.
Pandemic-Related Traumatic Stress was measured using the PTSS, which was developed by the senior author (A.E.M.) and a coauthor (M.A.A.), with contributions from other ECHO investigators (T.B., C.B.,N.R.B.,C.K.B.,J.B.H.,K.Z.L.). The scale was developed with the express purpose of measuring an individual’s response to traumatic stress induced by the COVID-19 pandemic and associated social isolation related to mitigation actions. Items were developed based on the DSM-5 acute stress criteria (American Psychiatric Association, 2022), and the scale was designed to have items map onto each of the five DSM-5 acute stress disorder symptom categories: (a) intrusion (e.g., distressing memories and dreams, flashbacks, catastrophized perceptions of expected events or conditions); (b) negative mood (e.g., anhedonia, anger disproportionate to the situation); (c) dissociation (e.g., feelings of time slowing); (d) avoidance (e.g., purposeful efforts to avoid thinking about the event or actions that are not congruent with required realities of persisting threats); and (e) difficulty regulating arousal (e.g., sleep disturbance, irritability, poor concentration). These concepts were written into survey item format based on examples given in the DSM-5 text, and items were discussed by the research team to reach a consensus on item clarity. One item pertaining to negative mood (“I no longer feel happy or satisfied”) was reframed into a positive statement for clarity (“I feel happy and satisfied with my life”). Parallel versions for the parent-report version for children 3–12 years old and self-report version for adolescents (13–21 years) and adult caregivers (18 years and older) were designed to capture response to traumatic stress across the lifespan from childhood to adulthood. Parent-report items were modified to be less inferential than the self-report version (e.g., instead of “I felt in a daze,” the item was reworded to “My child was in a daze”). Items were reviewed, revised, and finalized by the broader ECHO COVID-19 Working Group, which included experts in clinical and developmental psychology, neuropsychology, pediatrics, acute and posttraumatic stress disorders, epidemiology, and measurement science. Items were asked in the context of, “Since becoming aware of the COVID-19 pandemic,” and a 5-point Likert response scale was used for each item: (1) not at all, (2) rarely, (3) sometimes, (4) often, and (5) very often.
Sociodemographics included adult and child age (continuous), sex (1 = female), race (American Indian or Alaska Native, Asian, Black, Native Hawaiian or other Pacific Islander, White, multiracial, and self- or parent-reported “other race”) and ethnicity (1 = Hispanic); pregnant/postpartum individual or adult caregiver highest educational attainment (less than high school; high school degree or General Educational Development certificate; some college, no degree, or associate’s degree; bachelor’s degree; master’s, professional, or doctorate degree); annual family income (<$30,000, $30–49,999, $50–74,999, $75–99,999, $100–199,999, $200,000 or more); and current/last known state of residence (U.S. 50 states, Washington, DC, and Puerto Rico), which was also aggregated into region of residence, defined as the four U.S. Census regions (West, Midwest, South, and Northeast) and Puerto Rico. Because income is time variant, we restricted data to responses provided within 5 years of the pandemic-related stress items; if multiple responses were provided, the last known income was selected. For participants without residential address information, we used the state of their cohort recruitment site. Sociodemographic variables had acceptable missingness rates <10% (Bennett, 2001), except for caregiver educational attainment and annual family income, where missingness was >20% for some subgroup samples. We did not therefore investigate differences by these variables to avoid biased results.
Measures to Evaluate Relationships With Other Variables
Perceived Stress was measured using the Perceived Stress Scale 10- or four-item (PSS-10, PSS-4; Cohen & Janicki-Deverts, 2012; Kupst et al., 2015; Salsman et al., 2013) for pregnant/postpartum individuals and adult caregivers, which were harmonized by treating the six other items as missing for PSS-4; the PSS-10 (Kupst et al., 2015) or Patient Reported Measurement Information System (PROMIS) Pediatric Psychological Stress Experiences Short Form 4a (PPSE_Ped) for adolescents (Bevans et al.,2018); and the PROMIS Parent Proxy Psychological Stress Experiences Short Form 4a (PPSE_PP) for children (Bevans et al., 2018). All data were scored using the item response theory (IRT) based T-score metric (M = 50, SD = 10). PSS data were available for n = 999 (60.3%) pregnant/postpartum individuals, n = 4,365 (38%) adult caregivers, and n = 210 (11.7%) adolescents. PPSE_Ped data were available for n = 259 (14.4%) adolescents and PPSE_PP for n = 377 (13%) children.
Anxiety was measured using the PROMIS Anxiety Short Form 8a (pregnant/postpartum individuals and adult caregivers; Pilkonis et al., 2011), PROMIS Pediatric Anxiety Short Form 8a (adolescents; Irwin et al., 2010; Quinn et al., 2014), and the PROMIS Parent Proxy Anxiety Short Form 8a (children; Irwin et al., 2012). Instruments were scored using the PROMIS T-score metric (M = 50, SD = 10), and data were available for n = 56 (3.4%) pregnant/postpartum individuals, n = 530 (4.6%) adult caregivers, n = 74 adolescents (4.1%), and n = 297 (10.3%) children. We also used T -scoresfrom the parent-report Child Behavior Checklist–Preschool (CBCL-Pre; 1.5–5 years) or School Age (CBCL-Sch; 6–18 years) DSM-oriented Anxiety subscales (Achenbach & Rescorla, 2000, 2001). For the 3–12-year-old child sample, CBCL-Pre data were available for n = 149 (5.2%) children, and CBCL-Sch data were available for n = 308 (10.6%) children. For the adolescent sample, data on the CBCL-Sch were available for n = 493 (27.3%) adolescents.
Depressive Symptoms were measured with the PROMIS Depression Short Form 8a (pregnant/postpartum individuals and adult caregivers; Pilkonis et al., 2011), PROMIS Pediatric Depressive Symptoms Short Form 8a (adolescents; Irwin et al., 2010; Quinn et al., 2014), and the PROMIS Parent Proxy Depressive Symptoms Short Form 6a (children; Irwin et al., 2012). Instruments were scored using the PROMIS T score metric (M = 50, SD = 10), and data were available for n = 644 (38.9%) pregnant/postpartum individuals, n = 3,715 (32.4%) adult caregivers, n = 553 (30.8%) adolescents, and n = 49 (16.9%) children. We also used the CBCL DSM-oriented Depression subscale T scores (M = 50, SD = 10) for children and adolescents, which included the same sample sizes as described above.
Life Satisfaction was measured with a single-item indicator derived from the PROMIS Life Satisfaction instrument (Forrest et al., 2018). The item asked how often the child/adolescent or participant seemed/felt happy and satisfied with their life since becoming aware of the COVID-19 pandemic. A 5-point Likert scale response option was used, anchored by (1) not at all and (5) very often. The same item was used across all subgroup samples. See Supplemental Materials Methods, for additional details on measures to assess relationships with other variables.
Analytic Procedure
To psychometrically evaluate the PTSS items as a unidimensional scale, we used Mokken scaling, a nonparametric IRT-based method that describes the extent to which a set of items conform to an underlying unidimensional latent trait (Mokken, 2011). Mokken scaling does not make assumptions about item response functions like other factor analytic and parametric methods and can be used in an exploratory manner to identify the optimal set from an item pool that constitutes a monotonic, homogeneous IRT model (Molenaar & Sijtsma, 2000; Sijtsma & Molenaar, 2002). When assumptions hold, Mokken scaling results in an interpretable total score, wherein higher total scores correspond to higher values on the latent trait. We investigated whether there was evidence for the PTSS that followed the monotone homogeneity model (MHM) or the double monotonicity model (DMM) with invariant item ordering (IIO) using Hi and HT to evaluate the extent to which the PTSS fit these models (Sijtsma et al., 2011). We used the automated item selection procedure (AISP) algorithm (Mokken, 2011; Molenaar & Sijtsma, 2000; Sijtsma & Molenaar, 2002). Items were only considered for removal based on theoretical justification and/or if they had significantly lower Hi values compared to other scale items (Crişan et al., 2020; Stochl et al., 2012). A minimum Hi = .3 was chosen as the floor for item scalability based on previous work suggesting the following thresholds: weak (.3–.4); moderate (.4–.5); and strong (.5–.1; Sijtsma & Molenaar, 2002). The same cutoff values were used for HT (Sijtsma & van der Ark, 2017), which pertain to the degree of IIO sufficiency where positive values provide evidence for IIO (Ligtvoet et al., 2011). Cronbach’s α was estimated to investigate internal scale reliability (Cronbach, 1951).
We conducted Mokken scaling using complete cases for each participant sample to identify whether PTSS items performed similarly across these different samples, an indication of scale generalizability across ages, reporters, and subgroup populations (Sijtsma et al., 2011). Differential item functioning (DIF; Zumbo, 1999) was investigated for final scale items within each of the four participant samples by caregiver educational attainment using the ordinal logistic regression function in the lordif R package (Choi et al., 2011). We estimated the magnitude of uniform and nonuniform DIF using McFadden’s pseudo-R2 standard criteria: negligible (< .13), moderate (.13–26), and large (> .26; McFadden, 1974).
To evaluate differences in PTSS scores by region, pregnant versus postpartum, caregiver sex, and child/adolescent age and sex, we conducted known-group differences analyses using one-way analysis of variance (ANOVA). We used η2 to evaluate effect size using standard criteria: small (.01–.05), medium (.06–.14), and large (> .14; Cohen, 1988). We examined associations between PTSS sum scores and external, well-validated measures using Pearson r correlations to evaluate the relations with other variables hypothesized to be measuring constructs related to but not the same as pandemic-related traumatic stress (i.e., general stress, depression, anxiety, life satisfaction; AERA et al., 2014). We evaluated the strength of these correlations using standard criteria for evaluating correlation magnitude: small (.2), moderate (.5), and large (.8; Cohen, 1988).
Procedures to replicate these analyses are available upon request. Aside from the CBCL, all measures used in the analyses are freely available to download from the ECHOchildren.org website. This study—including its design, hypotheses, and analysis plan—was part of the ongoing ECHO program and not preregistered. The ECHO public use data set is available in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Data and Specimen Hub.
Results
Participants
Participants came from all 50 states, Washington, DC, and Puerto Rico (see Supplemental Figure 1, for regional distributions by sample). Participant details including demographics such as age, race, ethnicity, educational attainment, and income, by sample, are provided in Table 1. Briefly, the pregnant/postpartum sample self-identified as White (63.3%), Black (9.2%), American Indian or Alaska Native (4.1%), Asian (2.5%), multiracial (4.8%), and “other race” (2.5%); 18.6% were Hispanic; and 32.8% had some college or less. The adult caregiver sample (98.7% female) self-identified as White (65.2%), Black (14.4%), Asian (4.4%), American Indian or Alaska Native (1.9%), multiracial (3.8%), and “other race” (2.3%); 14.4% were Hispanic; and 40.1% had some college or less. The adolescent sample (53.8% female) was caregiver-identified as White (58%), Black (26.7%), Asian (1.7%), and multiracial (5.1%); 14.1% were Hispanic; and 41.6% had caregivers with some college or less. The child sample (48.6% female) was caregiver-identified as White (75%), Black (6.9%), American Indian or Alaska Native (4.3%), Asian (1.8%), and multiracial (8.2%); 11.8% were Hispanic; and 33.1% had caregivers with some college or less. Compared to the general U.S. population, there were higher proportions of White individuals and lower proportions of Hispanic individuals, higher proportions of individuals with bachelor’s degrees or higher, and slightly lower proportions of individuals with household incomes at or above $100,000 (see Supplemental Tables 6 and 7, for complete demographic comparisons with the general U.S. population).
Table 1.
Participant Sociodemographics by Subgroup Sample
| Sociodemographic characteristics | Pregnant/postpartum |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All (n = 1,656) |
Pregnant (n = 1,036) |
Postpartum (n = 620) |
Adult (n = 11,483) |
Adolescent (n = 1,785) |
Child (n = 2,896) |
|||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
|
| ||||||||||||
| n cohorts | 30 | 27 | 24 | 45 | 11 | 24 | ||||||
| Child age, M (SD) | 7.65 (4.95) | 16.9 (1.89) | 7.45 (2.5) | |||||||||
| Caregiver age, M (SD) | 29.8 (5.36) | 28.12 (5.67) | 30.52 (5.05) | 30.31 | (5.56) | |||||||
| Sex (female) | 1,656 | 100 | 1,036 | 100 | 620 | 100 | 11,191 | 98.7 | 961 | 53.8 | 1,408 | 48.6 |
| Race | ||||||||||||
| American Indian or Alaska Native | 67 | 4.1 | 48 | 4.6 | 19 | 3.1 | 217 | 1.9 | 6 | .3 | 123 | 4.3 |
| Asian | 41 | 2.5 | 31 | 3.0 | 10 | 1.6 | 503 | 4.4 | 31 | 1.7 | 53 | 1.8 |
| Black | 152 | 9.2 | 86 | 8.3 | 66 | 10.7 | 1,657 | 14.4 | 476 | 26.7 | 201 | 6.9 |
| Multiracial | 80 | 4.8 | 49 | 4.7 | 31 | 5.0 | 438 | 3.8 | 91 | 5.1 | 238 | 8.2 |
| Native Hawaiian or Other Pacific Islander | <5 | <5 | <5 | 26 | .2 | <5 | <5 | |||||
| Other race, self-identified | 41 | 2.5 | 29 | 2.8 | 12 | 1.9 | 259 | 2.3 | 12 | .7 | 21 | .7 |
| White | 1,165 | 70.4 | 714 | 68.9 | 451 | 72.7 | 7,487 | 65.2 | 1,033 | 58.0 | 2,172 | 75 |
| Missing | 107 | 6.5 | 78 | 7.5 | 29 | 4.7 | 896 | 7.8 | 135 | 7.6 | 84 | 2.9 |
| Hispanic | 313 | 18.9 | 207 | 20 | 106 | 17.1 | 1,658 | 14.4 | 252 | 14.1 | 343 | 11.8 |
| Missing | <20 | <10 | <15 | 264 | 2.3 | <5 | <30 | |||||
| Caregiver educational attainment | ||||||||||||
| <High School degree | 83 | 5.0 | 50 | 4.8 | 33 | 5.3 | 613 | 5.3 | 136 | 7.6 | 106 | 3.7 |
| High School degree, General Educational | 198 | 12 | 123 | 12 | 75 | 12.1 | 1,248 | 10.9 | 253 | 14.2 | 249 | 8.6 |
| Development certificate, or equivalent | ||||||||||||
| Some college, no degree or associate’s degree or trade school | 386 | 23.3 | 238 | 23 | 148 | 23.9 | 2,748 | 23.9 | 353 | 19.8 | 602 | 20.8 |
| Bachelor’s degree | 474 | 28.6 | 292 | 28.2 | 182 | 29.4 | 2,979 | 25.9 | 357 | 20.0 | 816 | 28.2 |
| Master’s, professional, or doctorate degree | 321 | 19.4 | 189 | 18.2 | 132 | 21.3 | 2,683 | 23.4 | 324 | 18.2 | 602 | 20.8 |
| Missing | 194 | 11.7 | 144 | 13.9 | 50 | 8.1 | 1,212 | 10.6 | 362 | 20.3 | 521 | 18.0 |
| Income | ||||||||||||
| <$30,000 | 298 | 18.0 | 194 | 18.7 | 104 | 16.8 | 1,808 | 15.8 | 378 | 21.2 | 408 | 14.1 |
| $30,000-$49,999 | 140 | 8.5 | 86 | 8.3 | 54 | 8.7 | 1,076 | 9.4 | 174 | 9.8 | 236 | 8.2 |
| $50,000–$74,999 | 197 | 11.9 | 129 | 12.5 | 68 | 11.0 | 1,049 | 9.1 | 153 | 8.6 | 286 | 9.9 |
| $75,000-$99,999 | 231 | 14.0 | 156 | 15.1 | 75 | 12.1 | 956 | 8.3 | 153 | 8.6 | 267 | 9.2 |
| $100,000-$199,999 | 300 | 18.1 | 201 | 19.4 | 99 | 16.0 | 2,069 | 18.0 | 372 | 20.8 | 549 | 19.0 |
| $200,000 or more | 93 | 5.6 | 59 | 5.7 | 34 | 5.5 | 1,095 | 9.5 | 173 | 9.7 | 233 | 8.1 |
| Missing | 397 | 24.0 | 211 | 20.4 | 186 | 30.0 | 3,430 | 29.9 | 382 | 21.4 | 917 | 31.7 |
Note. Race was self- or caregiver-reported.
Mokken Scaling Results
Mokken scaling resulted in moderately strong PTSSs for each of the four participant groups. Table 2 includes the AISP search algorithm results with all original items (Scale 1) and the final Mokken scales (Scale 2) with coefficients across the four groups. For each of the samples, the final scale consisted of nine of the 10 original items. The item, “felt (seemed) happy and satisfied with your (his/her) life” was removed based on psychometric justification (Hij values were much lower than the rest of the items and never exceeded .31) and theoretical justification (the only positively valenced item capturing positive mood, which has been shown to be related but not the exact opposite of the DSM-5 acute stress disorder criteria of negative mood; Blackwell et al., 2022). Each participant subgroup analysis resulted in a nine-item reliable unidimensional scale with Cronbach’s α > .8 (range: .84–.87).
Table 2.
Mokken Scaling Analysis With (Scale 1) and Without (Scale 2) Item 1, by Subgroup Sample
| Pregnant/ postpartum |
Adult |
Adolescent |
Child |
|||||
|---|---|---|---|---|---|---|---|---|
| Items | Scale 1 | Scale 2 | Scale 1 | Scale 2 | Scale 1 | Scale 2 | Scale 1 | Scale 2 |
|
| ||||||||
| 1. Happy and satisfied with lifea | .31 | Did Not Scale | .3 | Did Not Scale | .31 | Did Not Scale | .31 | Did Not Scale |
| 2. Difficulty sleeping | .46 | .44 | .47 | .43 | .45 | .44 | .46 | .48 |
| 3. Startled easily | .49 | .47 | .47 | .43 | DNS | .45 | .45 | .47 |
| 4. Angry outbursts | .47 | .46 | .45 | .42 | .44 | .43 | .45 | .47 |
| 5. Sense of time slowing | .43 | .43 | DNS | .39 | .46 | .45 | .44 | .45 |
| 6. Spaced out or in a daze | .47 | .46 | .46 | .47 | .51 | .50 | .49 | .50 |
| 7. Avoid thoughts and feelings about COVID-19 | .4 | .47 | DNS | .46 | DNS | .49 | .53 | .55 |
| 8. Avoid talking, reading, or watching information related to COVID-19 | DNS | .4 | DNS | .37 | DNS | .42 | .47 | .49 |
| 9. Distressing dreams about COVID-19 | .45 | .46 | .43 | .43 | .42 | .46 | .48 | .50 |
| 10. Distressed when see reminder of COVID-19 | .43 | .44 | .42 | .45 | .42 | .48 | .49 | .51 |
| H values | .46 | .45 | .43 | .43 | .44 | .46 | .46 | .49 |
| HT values of final scales | .41 | .35 | .36 | .21 | ||||
| α | .87 | .85 | .81 | .84 | .81 | .86 | .87 | .88 |
Note. DNS = Did Not Scale; bold values indicate values associated with the final COVID-19-related stress scale for each subgroup; pregnant/postpartum (n = 1,656) and adult (n = 11,483): ≥18 years; adolescent (n = 1,785): 13–21 years; child (n = 2,896): 3–12 years; items used a 5-point Likert response scale: (1) not at all, (2) rarely, (3) sometimes, (4) often, (5) very often; Scale 1 included all 10 original items; Scale 2 included a reduced set of nine negatively valenced items and did not include the one positively valenced item “happy and satisfied with life.” Scale 2 represents the final model.
Item was reverse coded.
There were slight differences in HT values across subgroups. For pregnant/postpartum and adult caregivers, HT = .41 and .35, respectively, suggesting moderate and weak evidence of IIO; the adolescent and child samples both had HT = .28, suggesting insufficient evidence of IIO. These results support the MHM (vs. DMM) for all four subsamples. Thus, within subsamples, pregnant/postpartum individuals, adult caregivers, adolescents, and children can be ordered on the latent trait according to their total scores. Item-level invariance investigations across levels of caregiver education did not reveal nonnegligible DIF (pseudo-R2 between models ≤.01), suggesting no meaningful uniform or nonuniform DIF. See Supplemental Table 8, for item-level descriptive statistics. Overall, the reliability of PTSS scores was consistent across ages, respondents, and other population characteristics.
Adult caregivers reported the highest level of pandemic-related traumatic stress (M = 18.57, SD = 6.46; range: 9–45), followed by adolescents (M = 18.33, SD = 7.16; range: 9–45), pregnant/postpartum individuals (M = 17.4, SD = 6.38; range: 9–45), and children as reported by their caregivers (M = 14.15, SD = 5.62; range: 9–41). All subgroup distributions were slightly positively skewed, and parent-reported child scores had the highest skewness (1.24) and kurtosis (4.24); this was further reflected by 27.6% (n = 800) of 3–12-year-olds having the lowest possible score. Across all samples, only n = 14 individuals had the highest possible score (Figure 1).
Figure 1.
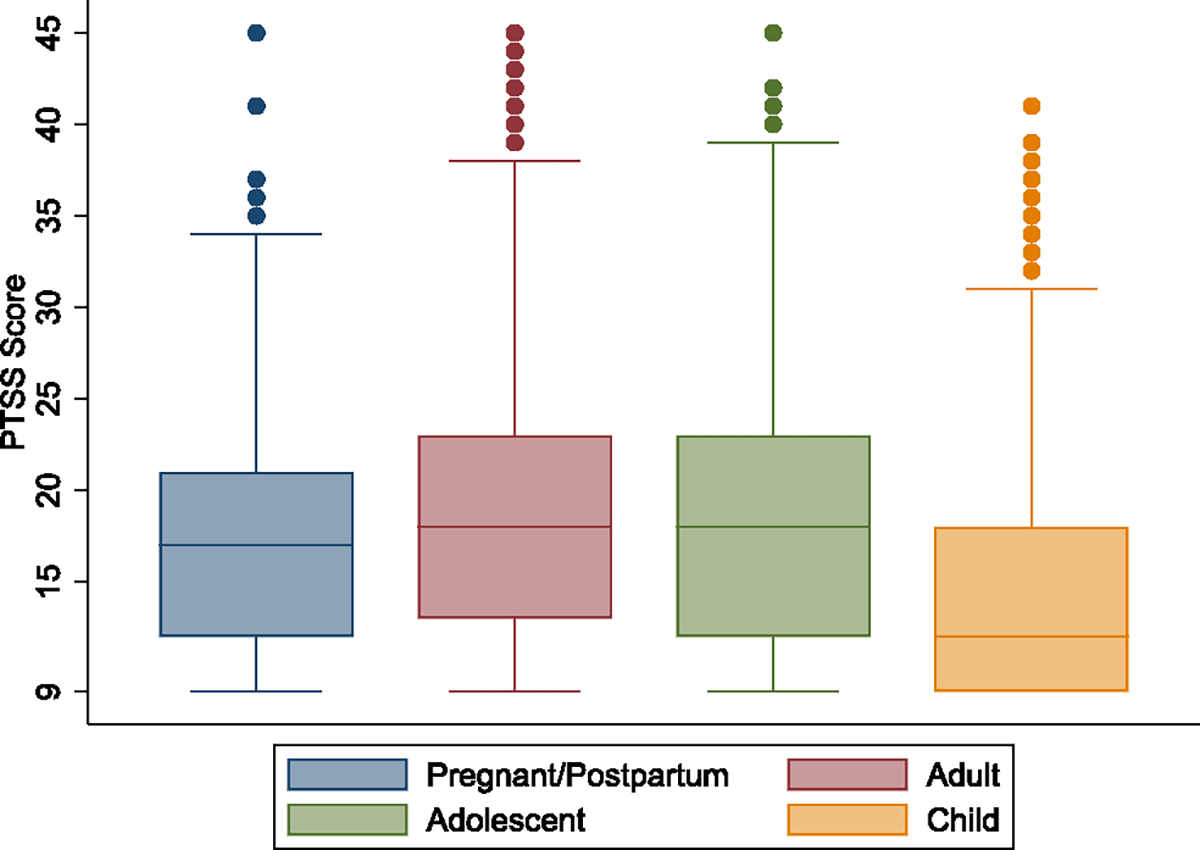
Boxplots of ECHO COVID-19 Pandemic-Related Traumatic Stress Scale Score Distribution, by Subgroup Sample
Note. Pregnant/postpartum (n = 1,656) and adult (n = 11,483): ≥18 years; adolescent (n = 1,785): 13–21 years; child (n = 2,896): 3–12 years. ECHO = Environmental influences on Child Health Outcomes; PTSS = Pandemic-Related Traumatic Stress Scale. See the online article for the color version of this figure.
Individuals within the same family may share COVID-19-related stressors and experiences. For the subsample of adult caregiver–child dyads (n = 2,573) and adult caregiver–adolescent dyads (n = 1,245), correlations of PTSS scores were r = .47 and r = .16, respectively. For the subsample of pregnant/postpartum caregiver–child dyads (n = 82), the correlation was r = .69. No correlation was computed for pregnant/postpartum caregiver–adolescent dyads due to small sample size (n < 10).
Known-Group Differences
One-way ANOVAs revealed significant differences in PTSS scores by region, where individuals in the South and Midwest reported lower traumatic stress (M = 13.5–18.1) and individuals in the Northeast and West reported higher levels (M = 14.3–19.3). Findings were consistent across the four samples (Supplemental Table 9). As hypothesized, postpartum individuals had significantly higher stress compared to those who were pregnant at the time of survey collection, M = 17.87, SD = 6.6 vs. M = 17.1, SD = 6.23; F(1) = 5.34, p = .02, η2 < .01, as did adults of <5-year-olds (M = 19.01, SD = 6.66) compared to adults of 5–12-year-olds (M = 18.91, SD = 6.39) and adolescents, M = 17.88, SD = 6.31; F(2) = 20.66, p < .001, η2 < .01. As hypothesized, female adult caregivers and female adolescents had higher stress compared to adult male caregivers, M = 18.62, SD = 6.46 vs. M = 15.4, SD = 5.68; F(1) = 37.62, p < .001, η2 < .01, and male adolescents, M = 20.23, SD = 7.12 vs. M = 16.1, SD = 6.45; F(1) = 161.47, p < .001, η2 = .08, respectively. Similar trends were found in the child sample, M = 14.36, SD = 5.86 vs. M = 13.95, SD = 5.37; F(1) = 3.77, p = .05, η2 < .01. Finally, confirming hypotheses, pandemic-related traumatic stress increased with age in both the child, F(9) = 10.95, p < .001, η2 = .03, and adolescent, F(8) = 6.32, p < .001, η2 = .03, samples (Supplemental Figure 2).
Relationships With Other Measures
Results showed moderate positive correlations (r =.46–.58) with all perceived stress measures and with PROMIS Anxiety (r = .50–.62) and Depressive Symptoms (r = .30–.48), and moderate negative correlations (r = −.35–−.37) with life satisfaction. Correlations with the CBCL DSM-oriented scales were moderate for the child parent-report sample(r = .28–.35) but slightly lower for the adolescent self-report sample (r = .20–.23), likely due to different respondents across the two measures as prior work shows notable discrepancies between parent and youth report (Upton et al., 2008). Despite being weaker, these correlations were still in the hypothesized positive direction and align with findings on the other external measures for the adolescent sample. See Table 3, for correlations.
Table 3.
Pearson r Correlations Between the PTSS and Other Measures
| Measures | Pregnant/postpartum | Adult | Adolescent | Child |
|---|---|---|---|---|
|
| ||||
| Perceived stress | ||||
| PSS | .46 | .46 | .49 | — |
| PROMIS psychological stress | — | — | .58 | .47 |
| Depression | ||||
| PROMIS depression | .47 | .35 | .48 | .3 |
| CBCL DSM depression | — | — | .23 | Pre: .35; Sch: .28 |
| Anxiety | ||||
| PROMIS anxiety | .5 | .44 | .62 | .54 |
| CBCL DSM anxiety | — | — | .2 | Pre: .35; Sch: .25 |
| Life satisfaction | -.35 | -.33 | -.35 | -.37 |
Note. — = not applicable; PTSS = Pandemic-Related Traumatic Stress Scale; PSS = Perceived Stress Scale; PROMIS = Patient Reported Outcome Measurement System; CBCL = Child Behavior Checklist; DSM = Diagnostic and Statistical Manual of Mental Disorders; Pre = preschool version; Sch = school-age version; pregnant/postpartum (n = 1,656) and adult (n = 11,483): ≥18 years; adolescent (n = 1,785): 13–21 years; child (n = 2,896): 3–12 years.
Discussion
The PTSS scores showed sufficient reliability and validity as measured in a large and geographically, economically, racially, and ethnically diverse U.S. sample. Mokken scaling confirmed unidimensionality of a nine-item version. Small-to-moderate correlations with other variables suggest that PTSS scores capture a related but unique construct other than depressive or anxiety symptoms, general stress, and life satisfaction. Given that many investigations of the psychological impact of the COVID-19 pandemic and related mitigation efforts have primarily focused on anxiety and depression as constructs of pandemic-related distress (e.g., Loades et al., 2020; Prati & Mancini 2021), the PTSS focus on acute stress symptoms provides important additional insight into the psychological impacts of the pandemic. Prior studies show that isolation or quarantine after exposure to a deadly disease is associated with a fourfold increase in risk for posttraumatic stress disorder (Brooks et al., 2020); thus, capturing COVID-19-related traumatic stress symptoms provides an important risk marker of psychopathology. Future work examining the predictive power of the tool above and beyond measures of general distress is warranted.
The PTSS includes items that align with the five symptom categories included in the DSM-5 acute stress disorder criteria. One item querying the negative mood domain did not produce good model fit. The lack of convergence with the other nine items may be a measurement issue related to the positive wording of this item, as all others were negatively valenced (Lindwall et al., 2012). Importantly, the item was conceptually related to the other nine items, suggesting that it does add information above and beyond the four DSM-5 domains covered in the summary score. To capture all five DSM-5 domains, we encourage users to administer all 10 items but consider scoring the one item separately from the other nine. A total sum score for the nine-item PTSS, as done here, can be created if complete data are available. Several alternate scores can also be computed. If individual-level data are missing on some items, we suggest computing an average score, but only for individuals who complete more than 50% of items (i.e., at least five of the nine items; Fairclough & Cella, 1996; Graham, 2009). See Margolis et al.(2021), for additional scoring options, including total symptoms and symptom categories scores.
The primary aim of the PTSS is to identify moderate and high levels of pandemic-related traumatic stress that may signal increased risk for future mental health problems, such as PTSD. Results suggest that the instrument aptly captured variability at higher scores and thus can distinguish between individuals with average versus moderate or severe pandemic-related traumatic stress. While future work is needed to evaluate potential clinical cutoff criteria, general recommendations for patient-reported outcomes like the PTSS are to consider one standard deviation above the mean as moderate and two standard deviations above the mean as severe (Cella et al., 2010). For the adult caregiver sample, for example, “moderate” equates to a score of 25.03 and “severe” equates to a score of 31.49. Conversely, the PTSS was not as good at differentiating among lower scores. For example, a floor effect was observed for the 3–12-year-old sample, where the bottom quartile of children had the lowest possible PTSS score. However, this is not necessarily a meaningful limitation, as individuals with scores below average suggest they are at low risk for developing mental health problems; therefore, understanding individual differences at low scores may not provide additional clinical utility.
Results from ANOVAs exploring regional and known-group differences analyses suggest the instrument differentiates groups as follows: individuals living in the Northeast or West, postpartum individuals, caregivers of younger children, females, older children, and older adolescents had higher levels of pandemic-related traumatic stress compared to individuals living in the Midwest or South, pregnant individuals, caregivers of older children and adolescents, males, younger children, and younger adolescents, respectively. Such findings may reflect differences in pandemic experiences. For example, eight of the top 10 states with the fewest COVID-19 containment strategies were in the South and Midwest (Leatherby & Harris, 2020), both of which had the lowest pandemic-related traumatic stress scores compared to the West and Northeast regions. Additionally, older youth often experienced longer periods of school closures compared to younger youth (Shapiro & Taylor, 2020) and adolescence is a time of peak mental illness onset (Rapee et al., 2019), both of which may explain why older youth experienced greater pandemic-related traumatic stress. However, the magnitude of effect sizes for many of the analyses was negligible (η2 < .01) or “small” (η2 = .01–.05; Cohen, 1988), such that while statistically significant, some of these differences may not be clinically meaningful. One exception was the “medium” effect size of sex in the adolescent age group, highlighting a vulnerability among adolescent females as compared to males. Similar sex differences have been found for adolescent depression and anxiety during the pandemic (Loades et al., 2020; Magson et al., 2021; Marques de Miranda et al., 2020).
Importantly, adolescents in general had the second-highest levels of pandemic-related stress (adults had the highest) and therefore may be particularly vulnerable to the impacts of the pandemic, especially female adolescents. Prior work suggests adolescents had moderate to severe PTSD symptoms, depression, anxiety, and suicidal ideation resulting from the COVID-19 pandemic (Murata et al., 2021), and COVID-19 pandemic-specific distress was reported as a critical contributor to exacerbating existing mental health problems for youth (Magson et al., 2021; Raviv et al., 2021). Targeted interventions specifically addressing COVID-19 pandemic-related traumatic stress in adolescent populations are needed, in addition to further work identifying which adolescents may be at higher risk for developing clinically significant sequelae of experiencing such stress. While the average stress level for 13–21-year-olds was 18.32 out of 45, adolescents also had the most variability in scores, including 12.7% (n = 227) scoring the minimum value. This variability suggests some adolescents had fewer stress reaction symptoms despite the pandemic, whereas others experienced high levels of pandemic-related traumatic stress. Future research to understand what promotes thriving and what exacerbates stress can help guide intervention development.
The psychometric characteristics of the PTSS suggest the scale can be used across childhood, adolescence, and adulthood, an improvement over the few existing pandemic-related stress measures that are only validated in adult samples. While individuals within the same family may experience similar COVID-19 stressors, prior work using the PTSS items finds only small to moderate correlations between caregivers and children (Blackwell et al., 2022). We replicate such findings here, with small-to-moderate correlations found between adult caregiver PTSS score and their reports on their 3–12-year-old’s pandemic-related traumatic stress or their adolescent’s self-reported pandemic-related traumatic stress.
Finally, the utility of the PTSS spans beyond the immediate COVID-19 pandemic context. Unlike previous measures, which were developed to capture traumatic stress reactions to a single inciting event, the PTSS was developed as a tool to evaluate potential traumatic stress reactions to ongoing macrolevel threats without defined time bounds, the long-term impact of which is still unknown. The instrument could therefore be adapted to evaluate reactions to other acute onset stressors with lengthy durations in the future.
Limitations and Future Directions
The PTSS provides researchers and clinicians with a brief, robust questionnaire to assess pandemic-related stress symptoms across the lifespan from childhood through adulthood. However, several study limitations are noted. First, despite the large, nationwide sample, our sample was not representative compared to the general U.S. population and included a higher proportion of White individuals, was higher educated, and had higher income. Of note, the adult caregiver sample was nearly all female. Similarly, regional results should be interpreted with caution given the sociodemographic makeup of the sample by region may not reflect the general U.S. population for that region. Additionally, we had moderate missingness for income and, for certain subsamples, caregiver educational attainment. However, our sample has geographic, economic, racial, and ethnic diversity, which is lacking in prior work (Ahorsu et al., 2022; Bridgland et al., 2021; Feng et al., 2020; Pedrozo-Pupo et al., 2020; Qiu et al., 2020; Tambling et al., 2021; Taylor et al., 2020). The few existing validated instruments were only tested with adult samples, and most were not validated with U.S. participants (Ahorsu et al., 2022; Bridgland et al., 2021; Feng et al., 2020; Kira et al., 2021; Pedrozo-Pupo et al., 2020; Qiu et al., 2020; Tambling et al., 2021; Taylor et al., 2020), which is important given the vast differences in country-level COVID-19 policies and experiences.
Additionally, not all ECHO cohorts administered measures of stress, anxiety, and depression used as comparators for known-group analyses. In some cases, these subsample sizes were relatively small (e.g., n = 56 pregnant/postpartum individuals with PROMIS Anxiety) and not necessarily representative of the larger sample. However, consistent results were found across the pregnant/postpartum, adult caregiver, adolescent, and child samples regardless of sample size or individual measure.
Having all five DSM-5 acute stress disorder domains covered in a single summary score was not feasible with the current items, as the single positively valenced item measuring happiness and satisfaction with life did not fit with the other nine negatively valenced items. Future research can investigate if changing the valence of this item enables a conceptually and psychometrically cohesive scale. Additionally, a second item measuring negative symptoms might help capture this dimension. Relatedly, we did not have clinical diagnoses or clinical measures of acute stress disorder, PTSD, or other mood disorders apart from questionnaire measures of anxiety and depression. While the intent of the instrument was not to be a clinical assessment, future work would benefit from evaluating its clinical validity by coadministering the scale with existing diagnostic tools and in clinically enriched samples.
Finally, the instrument did not measure symptom duration and instead asked participants how often they experienced each item “since becoming aware of the COVID-19 pandemic.” This framing was pertinent during the study period but may become less applicable as time passes. Asking participants to report over a 2- or 3-year period or longer—when their stress experience likely changed at various times—could result in unreliable data. Using a shorter time frame, such as the past month, may prove beneficial to capturing individual’s “current” stress experiences. This revised framing can also be useful for repeated data collection over time. While timing of assessment should not impact score reliability and validity, timing may impact PTSS scores depending on how close/far from becoming aware of the pandemic an individual is, and future studies can track PTSS scores over time to investigate this topic.
Conclusion
As short-term psychosocial impacts of the COVID-19 pandemic emerge in the literature, long-term consequences of living through this unprecedented and protracted time in history have yet to emerge. Building on prior work and integrating current findings, there is potential to inform the design of efforts to identify and ameliorate traumatic stress and associated impacts. Here, we developed and psychometrically validated the PTSS and presented a strategy to quantify COVID-19 pandemic-related traumatic stress in a brief, respondent-sensitive, and scientifically rigorous approach. The age-specific forms measure parallel constructs to enable what has been demonstrated here to be a clinically and psychometrically sound lifespan-coherent measurement.
Supplementary Material
Public Significance Statement.
The PTSS reliably quantifies traumatic stress in the context of the COVID-19 pandemic, enabling researchers and clinicians to differentiate general stress, depression, and anxiety from pandemic-related traumatic stress symptoms. It may help to identify individuals with higher levels of traumatic stress symptoms who may benefit from targeted interventions.
Acknowledgments
See acknowledgments for full listing of Environmental influences on Child Health Outcomes program collaborators.
The authors wish to thank our Environmental influences on Child Health Outcomes (ECHO) colleagues; the medical, nursing, and program staff; and the children and families participating in the ECHO cohorts. They also acknowledge the contribution of the following ECHO program collaborators:
ECHO Components: Coordinating Center: Duke Clinical Research Institute, Durham, North Carolina: Smith PB, Newby KL; Data Analysis Center: Johns Hopkins University Bloomberg School of Public Health, Baltimore, Maryland: Jacobson LP; Research Triangle Institute, Durham, North Carolina: Parker CB; Person Reported Outcomes Core: Northwestern University Feinberg School of Medicine, Chicago, Illinois: Gershon R, Cella D.
ECHO Awardees and Cohorts: Albert Einstein College of Medicine, Bronx, New York: Aschner J, Teitelbaum S; University of Colorado, Aurora, Colorado: Dabelea D; Emory University, Atlanta, Georgia: Dunlop A; Kaiser Permanente Northern California Division of Research, Oakland, California: Ferrara A; University of Wisconsin, Madison, Wisconsin: Gern J; University of California Davis Mind Institute, Sacramento, California: Hertz-Picciotto I; Brigham and Women’s Hospital, Boston, Massachusetts: Weiss S; University of Washington, Department of Environmental and Occupational Health Sciences, Seattle, Washington: Karr C; Pennsylvania State University, University Park, Pennsylvania: Newschaffer C.
Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of The Director, National Institutes of Health, under Awards U2COD023375 (Coordinating Center), U24OD023382 (Data Analysis Center; Aruna Chandran), U24OD023319, with cofunding from the Office of Behavioral and Social Sciences Research (OBSSR; Person Reported Outcomes Core, Courtney K. Blackwell, Phillip Sherlock, Kathryn L. Jackson, David Cella), UH3OD023251 (Akram N. Alshawabkeh), UH3OD023332 (Clancy Blair), UH3OD023287 (Carrie Breton, Tracy Bastain), UH3OD023289 (Lyndsay A. Avalos, Diane R. Gold, Croen, Ferrara), UH3OD023248 (Dabelea), UH3OD023285 (Sean Deoni), UH3OD023328 (Cristiane S. Duarte), UH3OD023318 (Patricia A. Brennan), UH3OD023279 (Amy J. Elliott), UH3OD023282 (Diane R. Gold, Christine Joseph, Anne Marie Singh), UH3OD023290 (Julie B. Herbstman, Molly A. Algermissen, Amy E. Margolis, David Pagliaccio), UH3OD023365 (Hertz-Picciotto), UH3OD023275 (Margaret R. Karagas), UH3OD02371 (W. Alex Mason, Kaja Z. LeWinn, Nicole R. Bush), UH3OD023285 (Kimberly S. McKee), UH3OD023347 (Barry Lester, Elisabeth C. McGowan), UH3OD023389 (Leslie D. Leve, Jody M. Ganiban, Jenae M. Neiderhiser), UH3OD023288 (McEvoy), UH3OD023342 (Rebecca J. Schmidt), UH3OD023349 (Thomas G. O’Connor), UH3OD023286 (Emily Oken), UH3OD023348 (T. Michael O’Shea, Julie A. Hofheimer, Jean A. Frazier), UH3OD023272 (Schantz), UH3OD023249 (Joseph B. Stanford, Elisabeth Conradt, Sheila E. Crowell), UH3OD023305 (Leonardo Trasande), UH3OD02368 (Jessica A. Lasky-Su), and UH3OD023337 (Rosalind J. Wright, Rachel L. Miller, Shaina Collazo, Michelle Bosquet Enlow). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no conflicts of interest to disclose. The authors have no financial relationships relevant to this article to disclose.
Procedures to replicate these analyses are available upon request. Aside from the proprietary Child Behavior Checklist instrument, all measures are freely available to download from the https://ECHOchildren.org website. This study was part of the ongoing ECHO research program and not preregistered. The ECHO public use data set is available in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Data and Specimen Hub.
Courtney K. Blackwell played lead role in conceptualization, writing of original draft and writing of review and editing, supporting role in data curation and formal analysis and equal role in visualization. Phillip Sherlock played lead role in formal analysis and methodology, supporting role in data curation, writing of original draft and writing of review and editing and equal role in conceptualization and visualization. Kathryn L. Jackson played lead role in data curation, supporting role in formal analysis, methodology, writing of original draft and writing of review and editing and equal role in conceptualization. Julie A. Hofheimer played supporting role in visualization and writing of original draft and equal role in investigation and writing of review and editing. David Cella played supporting role in conceptualization and methodology and equal role in writing of review and editing. Molly A. Algermissen played supporting role in writing of review and editing and equal role in conceptualization and investigation. Akram N. Alshawabkeh played equal role in investigation and writing of review and editing. Lyndsay A. Avalos played equal role in investigation and writing of review and editing. Tracy Bastain played equal role in conceptualization and investigation. Clancy Blair played equal role in investigation and writing of review and editing. Michelle Bosquet Enlow played equal role in investigation and writing of review and editing. Patricia A. Brennan played equal role in investigation and writing of review and editing. Carrie Breton played equal role in investigation and writing of review and editing. NicoleR. Bushplayed equal role in conceptualization, investigation and writing of review and editing. Aruna Chandran played equal role in resources and writing of review and editing. Shaina Collazo played equal role in investigation and writing of review and editing. Elisabeth Conradt played equal role in investigation and writing of review and editing. Sheila E. Crowell played equal role in investigation and writing of review and editing. Sean Deoni played equal role in investigation and writing of review and editing. Amy J. Elliott played equal role in investigation and writing of review and editing. Jean A. Frazier played equal role in investigation and writing of review and editing. Jody M. Ganiban played equal role in investigation and writing of review and editing. Diane R. Gold played equal role in investigation and writing of review and editing. Julie B. Herbstman played equal role in investigation and writing of review and editing. Christine Joseph played equal role in investigation and writing of review and editing. Margaret R. Karagas played equal role in investigation and writing of review and editing. Barry Lester played equal role in investigation and writing of review and editing. Jessica A. Lasky-Su played equal role in investigation and writing of review and editing. Leslie D. Leve played equal role in investigation and writing of review and editing. Kaja Z. LeWinn played equal role in investigation and writing of review and editing. W. Alex Mason played equal role in investigation and writing of review and editing. Elisabeth C. McGowan played equal role in investigation and writing of review and editing. Kimberly S. McKee played equal role in investigation and writing of review and editing. Rachel L. Miller played equal role in investigation and writing of review and editing. Jenae M. Neiderhiser played equal role in investigation and writing of review and editing. Thomas G. O’Conner played equal role in investigation and writing of review and editing. Emily Oken played equal role in investigation and writing of review and editing. T. Michael O’Shea played equal role in investigation and writing of review and editing. David Pagliaccio played equal role in conceptualization, investigation and writing of review and editing. Rebecca J. Schmidt played equal role in investigation and writing of review and editing. Anne Marie Singh played equal role in investigation and writing of review and editing. Joseph B. Stanford played equal role in investigation and writing of review and editing. Leonardo Trasande played equal role in investigation and writing of review and editing. Rosalind J. Wright played equal role in investigation and writing of review and editing. Cristiane S. Duarte played equal role in conceptualization, investigation, writing of original draft and writing of review and editing. Amy E. Margolis played lead role in conceptualization and supervision and equal role in investigation, writing of original draft and writing of review and editing.
Supplemental materials: https://doi.org/10.1037/pas0001211.supp
References
- Achenbach TM, & Rescorla LA (2000). Manual for the ASEBA preschool forms & profiles. University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles. University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Adolescent Brain Cognitive Development. (2020). ABCD COVID-19 Questionnaire. https://www.phenxtoolkit.org/toolkit_content/PDF/UCSD_ABCD_Youth.pdf
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, & Pakpour AH (2022). The fear of COVID-19 Scale: Development and initial validation. International Journal of Mental Health and Addiction, 20(3), 1537–1545. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Educational Research Association [AERA], the American Psychological Association, & the National Council on Measurement in Education. (2014). Standards for educational and psychological testing. [Google Scholar]
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (DSM-5-TR) (et al. ed., text revision; ). [Google Scholar]
- Baker LR, & Cormier LA (2014). Disasters and vulnerable populations: Evidence-based practice for the helping professions. Springer Publishing Company. 10.1891/9780826198488 [DOI] [Google Scholar]
- Basu A, Kim HH, Basaldua R, Choi KW, Charron L, Kelsall N, Hernandez-Diaz S, Wyszynski DF, & Koenen KC (2021). A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLOS ONE, 16(4), Article e0249780. 10.1371/journal.pone.0249780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham PJ, Sunderland M, Carragher N, & Calear AL (2019). Psychometric properties of 7- and 30-day versions of the PROMIS emotional distress item banks in an Australian adult sample. Assessment, 26(2), 249–259. 10.1177/1073191116685809 [DOI] [PubMed] [Google Scholar]
- Bennett DA (2001). How can I deal with missing data in my study? Australian and New Zealand Journal of Public Health, 25(5), 464–469. 10.1111/j.1467-842X.2001.tb00294.x [DOI] [PubMed] [Google Scholar]
- Bevans KB, Gardner W, Pajer KA, Becker B, Carle A, Tucker CA, & Forrest CB (2018). Psychometric evaluation of the PROMIS® pediatric psychological and physical stress experiences measures. Journal of Pediatric Psychology, 43(6), 678–692. 10.1093/jpepsy/jsy010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell CK, Mansolf M, Sherlock P, Ganiban J, Hofheimer JA, Barone CJ II, Bekelman TA, Blair C, Cella D, Collazo S, Croen LA, Deoni S, Elliott AJ, Ferrara A, Fry RC, Gershon R, Herbstman JB, Karagas MR, LeWinn KZ, … Wright RJ (2022). Youth well-being during the COVID-19 pandemic. Pediatrics, 149(4), Article e2021054754. 10.1542/peds.2021-054754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaisdell CJ, Park C, Hanspal M, Roary M, Arteaga SS, Laessig S, Luetkemeier E, & Gillman MW (2021). The NIH ECHO program: Investigating how early environmental influences affect child health. Pediatric Research, 92, 1215–1216. 10.1038/s41390-021-01574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridgland VME, Moeck EK, Green DM, Swain TL, Nayda DM, Matson LA, Hutchison NP, & Takarangi MKT (2021). Why the COVID-19 pandemic is a traumatic stressor. PLOS ONE, 16(1), Article e0240146. 10.1371/journal.pone.0240146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calear AL, McCallum S, Morse AR, Banfield M, Gulliver A, Cherbuin N, Farrer LM, Murray K, Rodney Harris RM, & Batterham PJ (2022). Psychosocial impacts of home-schooling on parents and caregivers during the COVID-19 pandemic. BMC Public Health, 22(1), Article 119. 10.1186/s12889-022-12532-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, Devellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai JS, Pilkonis P, Revicki D, … the PROMIS Cooperative Group. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CY-C, Byrne E, & Vélez T (2022). Impact of the 2020 pandemic of COVID-19 on families with school-aged children in the United States: Roles of income level and race. Journal of Family Issues, 43(3), 719–740. 10.1177/0192513X21994153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Zhu Z, Lei F, Lei S, & Chen J (2021). Prevalence and risk factors of post-traumatic stress disorder symptoms in students aged 8–18 in Wuhan, China 6 months after the control of COVID-19. Frontiers in Psychology, 12, Article 740575. 10.3389/fpsyg.2021.740575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi SW, Gibbons LE, & Crane PK (2011). Lordif: An R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and monte carlo simulations. Journal of Statistical Software, 39(8), 1–30. 10.18637/jss.v039.i08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S (1988). Statistical power analysis for the behavioral sciences. Routledge. 10.4324/9780203771587 [DOI] [Google Scholar]
- Cohen S, & Janicki-Deverts D (2012). Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. Journal of Applied Social Psychology, 42(6), 1320–1334. 10.1111/j.1559-1816.2012.00900.x [DOI] [Google Scholar]
- Cooke JE, Eirich R, Racine N, & Madigan S (2020). Prevalence of posttraumatic and general psychological stress during COVID-19: A rapid review and meta-analysis. Psychiatry Research, 292, Article 113347. 10.1016/j.psychres.2020.113347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortez PA, Joseph SJ, Das N, Bhandari SS, & Shoib S (2020). Tools to measure the psychological impact of the COVID-19 pandemic: What do we have in the platter? Asian Journal of Psychiatry, 53, Article 102371. 10.1016/j.ajp.2020.102371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell C, Shum A, Pearcey S, Skripkauskaite S, Patalay P, & Waite P (2021). Young people’s mental health during the COVID-19 pandemic. The Lancet. Child & Adolescent Health, 5(8), 535–537. 10.1016/S2352-4642(21)00177-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crişan DR, Tendeiro JN, & Meijer RR (2020). On the practical consequences of misfit in Mokken scaling. Applied Psychological Measurement, 44(6), 482–496. 10.1177/0146621620920925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronbach LJ (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297–334. 10.1007/BF02310555 [DOI] [Google Scholar]
- Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA, Howard ME, & Rajaratnam SMW (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049–1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito S, & Principi N (2020). School closure during the coronavirus disease 2019 (COVID-19) pandemic: An effective intervention at the global level? JAMA Pediatrics, 174(10), 921–922. 10.1001/jamapediatrics.2020.1892 [DOI] [PubMed] [Google Scholar]
- Fairclough DL, & Cella DF (1996). Functional Assessment of Cancer Therapy (FACT-G): Non-response to individual questions. Quality of Life Research, 5(3), 321–329. 10.1007/BF00433916 [DOI] [PubMed] [Google Scholar]
- Fegert JM, Vitiello B, Plener PL, & Clemens V (2020). Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14(1), Article 20. 10.1186/s13034-020-00329-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng LS, Dong ZJ, Yan RY, Wu XQ, Zhang L, Ma J, & Zeng Y (2020). Psychological distress in the shadow of the COVID-19 pandemic: Preliminary development of an assessment scale. Psychiatry Research, 291, Article 113202. 10.1016/j.psychres.2020.113202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest CB, Devine J, Bevans KB, Becker BD, Carle AC, Teneralli RE, Moon J, Tucker CA, & Ravens-Sieberer U (2018). Development and psychometric evaluation of the PROMIS pediatric life satisfaction item banks, child-report, and parent-proxy editions. Quality of Life Research, 27(1), 217–234. 10.1007/s11136-017-1681-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillman MW, & Blaisdell CJ (2018). Environmental influences on child health outcomes, a research program of the National Institutes of Health. Current Opinion in Pediatrics, 30(2), 260–262. 10.1097/MOP.0000000000000600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E, Wen H, & Miller BF (2020). Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics, 174(9), 819–820. 10.1001/jamapediatrics.2020.1456 [DOI] [PubMed] [Google Scholar]
- Graham JW (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60(1), 549–576. 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Hertz MF, Kilmer G, Verlenden J, Liddon N, Rasberry CN, Barrios LC, & Ethier KA (2022). Adolescent mental health, connectedness, and mode of school instruction during COVID-19. The Journal of Adolescent Health, 70(1), 57–63. 10.1016/j.jadohealth.2021.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong S, Kim H, & Park MK (2021). Impact of COVID-19 on post-traumatic stress symptoms in the general population: An integrative review. International Journal of Mental Health Nursing, 30(4), 834–846. 10.1111/inm.12875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh D, & Brown AD (2020). Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4), 331–335. 10.1037/tra0000592 [DOI] [PubMed] [Google Scholar]
- Hou TY, Mao XF, Dong W, Cai WP, & Deng GH (2020). Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian Journal of Psychiatry, 54, Article 102305. 10.1016/j.ajp.2020.102305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin DE, Gross HE, Stucky BD, Thissen D, DeWitt EM, Lai JS, Amtmann D, Khastou L, Varni JW, & DeWalt DA (2012). Development of six PROMIS pediatrics proxy-report item banks. Health and Quality of Life Outcomes, 10(1), Article 22. 10.1186/1477-7525-10-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin DE, Stucky B, Langer MM, Thissen D, Dewitt EM, Lai JS, Varni JW, Yeatts K, & DeWalt DA (2010). An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Quality of Life Research, 19(4), 595–607. 10.1007/s11136-010-9619-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2022). COVID-19: Metrics by state. https://www.kff.org/coronavirus-covid-19/issue-brief/state-covid-19-data-and-policy-actions/
- King LS, Feddoes DE, Kirshenbaum JS, Humphreys KL, & Gotlib IH (2021). Pregnancy during the pandemic: The impact of COVID-19-related stress on risk for prenatal depression. Psychological Medicine. Advance online publication. 10.1017/S003329172100132X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kira IA (2021). Taxonomy of stressors and traumas: An update of the Development-Based Trauma Framework (DBTF): A life-course perspective on stress and trauma. Traumatology, 28(1), 84–97. 10.1037/trm0000305 [DOI] [Google Scholar]
- Kira IA, Shuwiekh HA, Rice KG, Ashby JS, Elwakeel SA, Sous MSF, Alhuwailah A, Baali SBA, Azdaou C, Oliemat EM, & Jamil HJ (2021). Measuring COVID-19 as traumatic stress: Initial psychometrics and validation. Journal of Loss and Trauma, 26(3), 220–237. 10.1080/15325024.2020.1790160 [DOI] [Google Scholar]
- Kupst MJ, Butt Z, Stoney CM, Griffith JW, Salsman JM, Folkman S, & Cella D (2015). Assessment of stress and self-efficacy for the NIH toolbox for neurological and behavioral function. Anxiety, Stress, and Coping, 28(5), 531–544. 10.1080/10615806.2014.994204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladouceur CD (2020). COVID-19 Adolescent Symptom & Psychological Experience Questionnaire. https://osf.io/py7vg/
- Lai JS, Cook K, Stone A, Beaumont J, & Cella D (2009). Classical test theory and item response theory/Rasch model to assess differences between patient-reported fatigue using 7-day and 4-week recall periods. Journal of Clinical Epidemiology, 62(9), 991–997. 10.1016/j.jclinepi.2008.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leatherby L, & Harris R (2020, November 18). States that imposed few restrictions now have the worst outbreaks. The New York Times. https://www.nytimes.com/interactive/2020/11/18/us/covid-state-restrictions.html [Google Scholar]
- Ligtvoet R, Van der Ark LA, Bergsma WP, & Sijtsma K (2011). Polytomous latent scales for the investigation of the ordering of items. Psychometrika, 76(2), 200–216. 10.1007/s11336-010-9199-8 [DOI] [Google Scholar]
- Lindwall M, Barkoukis V, Grano C, Lucidi F, Raudsepp L, Liukkonen J, & Thøgersen-Ntoumani C (2012). Method effects: The problem with negatively versus positively keyed items. Journal of Personality Assessment, 94(2), 196–204. 10.1080/00223891.2011.645936 [DOI] [PubMed] [Google Scholar]
- Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, Linney C, McManus MN, Borwick C, & Crawley E (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child & Adolescent Psychiatry, 59(11), 1218–1239.e3. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logue JK, Franko NM, McCulloch DJ, McDonald D, Magedson A, Wolf CR, & Chu HY (2021). Sequelae in adults at 6 months after COVID-19 infection. JAMA Network Open, 4(2), Article e210830. 10.1001/jamanetworkopen.2021.0830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson NR, Freeman JYA, Rapee RM, Richardson CE, Oar EL, & Fardouly J (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis A, Algermissen M, Herbstman JB, Bush N, Breton C, Blackwell CK, & Bastain T (2021). Acute stress questions for ECHO COVID-19 survey. PsychArchives. 10.23668/psycharchives.5094 [DOI] [Google Scholar]
- Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, & Simoes-E-Silva AC (2020). How is COVID-19 pandemic impacting mental health of children and adolescents? International Journal of Disaster Risk Reduction, 51, Article 101845. 10.1016/j.ijdrr.2020.101845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFadden D (1974). Conditional logit analysis of qualitative choice behavior. In Zarembka P (Ed.), Frontiers in econometrics (pp. 105–142). Academic Press. [Google Scholar]
- Mokken R (2011). A theory and procedure of scale analysis: With applications in political research. De Gruyter Mouton. 10.1515/9783110813203 [DOI] [Google Scholar]
- Molenaar IW, & Sijtsma K (2000) User’s Manual MSP5 for Windows [Software manual]. IEC ProGAMMA. [Google Scholar]
- Molgora S, & Accordini M (2020). Motherhood in the time of coronavirus: The impact of the pandemic emergency on expectant and postpartum women’s psychological well-being. Frontiers in Psychology, 11, Article 567155. 10.3389/fpsyg.2020.567155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murata S, Rezeppa T, Thoma B, Marengo L, Krancevich K, Chiyka E, Hayes B, Goodfriend E, Deal M, Zhong Y, Brummit B, Coury T, Riston S, Brent DA, & Melhem NM (2021). The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depression and Anxiety, 38(2), 233–246. 10.1002/da.23120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaidis A, Paksarian D, Alexander L, Derosa J, Dunn J, Nielson DM, Droney I, Kang M, Douka I, Bromet E, Milham M, Stringaris A, & Merikangas KR (2021). The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Scientific Reports, 11(1), Article 8139. 10.1038/s41598-021-87270-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel K, Robertson E, Kwong ASF, Griffith GJ, Willan K, Green MJ, Di Gessa G, Huggins CF, McElroy E, Thompson EJ, Maddock J, Niedzwiedz CL, Henderson M, Richards M, Steptoe A, Ploubidis GB, Moltrecht B, Booth C, Fitzsimons E, … Katikireddi SV (2022). Psychological distress before and during the COVID-19 pandemic among adults in the united kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Network Open, 5(4), Article e227629. 10.1001/jamanetworkopen.2022.7629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrozo-Pupo JC, Pedrozo-Cortés MJ, & Campo-Arias A (2020). Perceived stress associated with COVID-19 epidemic in Colombia: An online survey. Cadernos de Saude Publica, 36(5), Article e00090520. [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, & the PROMIS Cooperative Group. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18(3), 263–283. 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G, & Mancini AD (2021). The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. 10.1017/S0033291721000015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis H, Mahaffey B, Heiselman C, & Lobel M (2020). Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Social Science & Medicine, 266, Article 113348. 10.1016/j.socscimed.2020.113348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, & Xu Y (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), Article e100213. 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn H, Thissen D, Liu Y, Magnus B, Lai JS, Amtmann D, Varni JW, Gross HE, & DeWalt DA (2014). Using item response theory to enrich and expand the PROMIS® pediatric self report banks. Health and Quality of Life Outcomes, 12(1), Article 160. 10.1186/s12955-014-0160-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Oar EL, Johnco CJ, Forbes MK, Fardouly J, Magson NR, & Richardson CE (2019). Adolescent development and risk for the onset of social-emotional disorders: A review and conceptual model. Behaviour Research and Therapy, 123, Article 103501. 10.1016/j.brat.2019.103501 [DOI] [PubMed] [Google Scholar]
- Raviv T, Warren CM, Washburn JJ, Kanaley MK, Eihentale L, Goldenthal HJ, Russo J, Martin CP, Lombard LS, Tully J, Fox K, & Gupta R (2021). Caregiver perceptions of children’s psychological well-being during the COVID-19 pandemic. JAMA Network Open, 4(4), Article e2111103. 10.1001/jamanetworkopen.2021.11103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salsman JM, Butt Z, Pilkonis PA, Cyranowski JM, Zill N, Hendrie HC, Kupst MJ, Kelly MA, Bode RK, Choi SW, Lai JS, Griffith JW, Stoney CM, Brouwers P, Knox SS, & Cella D (2013). Emotion assessment using the NIH Toolbox. Neurology, 80(11, Suppl. 3), S76–S86. 10.1212/WNL.0b013e3182872e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro E, & Taylor K (2020, November 30). Why school districts are bringing back younger children first. NewYork Times https://www.nytimes.com/2020/11/30/nyregion/elementary-schools-reopening.html [Google Scholar]
- Sijtsma K, Meijer RR, & Van der Ark LA (2011). Mokken scale analysis as time goes by: An update for scaling practitioners. Personality and Individual Differences, 50(1), 31–37. 10.1016/j.paid.2010.08.016 [DOI] [Google Scholar]
- Sijtsma K, & Molenaar IW (2002). Introduction to nonparametric item response theory (et al. ed.). Sage Publications. 10.4135/9781412984676 [DOI] [Google Scholar]
- Sijtsma K, & van der Ark LA (2017). A tutorial on how to do a Mokken scale analysis on your test and questionnaire data. British Journal of Mathematical & Statistical Psychology, 70(1), 137–158. 10.1111/bmsp.12078 [DOI] [PubMed] [Google Scholar]
- Spinelli M, Lionetti F, Pastore M, & Fasolo M (2020). Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Frontiers in Psychology, 11, Article 1713. 10.3389/fpsyg.2020.01713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G, & Silman M (2013). Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness, 7(1), 105–110. 10.1017/dmp.2013.22 [DOI] [PubMed] [Google Scholar]
- Stochl J, Jones PB, & Croudace TJ (2012). Mokken scale analysis of mental health and well-being questionnaire item responses: A non-parametric IRT method in empirical research for applied health researchers. BMC Medical Research Methodology, 12(1), Article 74. 10.1186/1471-2288-12-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tambling RR, Russell BS, Park CL, Fendrich M, Hutchinson M, Horton AL, & Tomkunas AJ (2021). Measuring cumulative stressfulness: Psychometric properties of the COVID-19 stressors scale. Health Education & Behavior, 48(1), 20–28. 10.1177/1090198120979912 [DOI] [PubMed] [Google Scholar]
- Taquet M, Dercon Q, Luciano S, Geddes JR, Husain M, & Harrison PJ (2021). Incidence, co-occurrence, and evolution of long-COVID features: A 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLOS Medicine, 18(9), Article e1003773. 10.1371/journal.pmed.1003773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, & Asmundson GJG (2020). Development and initial validation of the COVID Stress Scales. Journal of Anxiety Disorders, 72, Article 102232. 10.1016/j.janxdis.2020.102232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales J, O’Higgins M, Castaldelli-Maia JM, & Ventriglio A (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. The International Journal of Social Psychiatry, 66(4), 317–320. 10.1177/0020764020915212 [DOI] [PubMed] [Google Scholar]
- Upton P, Lawford J, & Eiser C (2008). Parent–child agreement across child health-related quality of life instruments: A review of the literature. Quality of Life Research, 17(6), 895–913. 10.1007/s11136-008-9350-5 [DOI] [PubMed] [Google Scholar]
- Verlenden JV, Pampati S, Rasberry CN, Liddon N, Hertz M, Kilmer G, Viox MH, Lee S, Cramer NK, Barrios LC, & Ethier KA (2021). Association of children’s mode of school instruction with child and parent experiences and well-being during the COVID-19 pandemic—COVID experiences survey, United States, October 8–November 13, 2020. Morbidity and Mortality Weekly Report, 70(11), 369–376. 10.15585/mmwr.mm7011a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Kala MP, & Jafar TH (2020). Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLOS ONE, 15(12), Article e0244630. 10.1371/journal.pone.0244630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodworth KR, Olsen EO, Neelam V, Lewis EL, Galang RR, Oduyebo T, Aveni K, Yazdy MM, Harvey E, Longcore ND, Barton J, Fussman C, Siebman S, Lush M, Patrick PH, Halai UA, Valencia-Prado M, Orkis L, Sowunmi S, … the COVID-19 Pregnancy and Infant Linked Outcomes Team (PILOT). (2020). Birth and infant outcomes following laboratory-confirmed sars-cov-2 infection in pregnancy—Set-net, 16 jurisdictions, March 29–October 14, 2020. Morbidity and Mortality Weekly Report, 69(44), 1635–1640. 10.15585/mmwr.mm6944e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, & McIntyre RS (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K, Gong YM, Liu L, Sun YK, Tian SS, Wang YJ, Zhong Y, Zhang AY, Su SZ, Liu XX, Zhang YX, Lin X, Shi L, Yan W, Fazel S, Vitiello MV, Bryant RA, Zhou XY, Ran MS, … Lu L (2021). Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: A meta-analysis and systematic review. Molecular Psychiatry, 26(9), 4982–4998. 10.1038/s41380-021-01036-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrano LD, Ellington S, Strid P, Galang RR, Oduyebo T, Tong VT, Woodworth KR, Nahabedian JF III, Azziz-Baumgartner E, Gilboa SM, Meaney-Delman D, Akosa A, Bennett C, Burkel V, Chang D, Delaney A, Fox C, Griffin I, Hsia J, … the CDC COVID-19 Response Pregnancy and Infant Linked Outcomes Team. (2020). Update: Characteristics of symptomatic women of reproductive age with laboratory-confirmed sars-cov-2 infection by pregnancy status—United States, January 22–October 3, 2020. Morbidity and Mortality Weekly Report, 69(44), 1641–1647. 10.15585/mmwr.mm6944e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zumbo BD (1999). A handbook on the theory and methods of differential item functioning (DIF): Logistic regression modeling as a unitary framework for binary and Likert-type (ordinal) item scores. Directorate of Human Resources Research and Evaluation, Department of National Defense. https://faculty.educ.ubc.ca/zumbo/DIF/handbook.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


