Abstracts
Introduction
Medical disorders complicating pregnancy have recently emerged as the most common cause for maternal morbidity and mortality and it is important to predict mortality risk when they present in moribund state to emergency obstetric care so as to take and timely effective measures to prevent mortality.
Methods
This prospective observational study was conducted over 6 months among pregnant and post-partum women with medical disorders who sought emergency obstetric care at a tertiary care hospital. Severity of morbidity was assessed using SOFA and APACHE II scores at admission.
Results
Of the 128 women, 87.5% were pregnant, and 12.5% were post-partum. Hypertensive disorders, cardiac disorders, neurological disorders and infective disorders were 24.2%, 22.6%, 14% and 9.4%, respectively. The optimal cut-off SOFA score was 2 (AUC = 0.739) with 66% sensitivity and 71% specificity and APACHE II score cut-off was 6 (AUC = 0.732) with a sensitivity of 60% and specificity of 78% in predicting severe maternal morbidity. The median scores of APACHE II and SOFA are 14 and 4, respectively, for non-survivors and for survivors it was 4 and 1.
Conclusion
Hypertensive disorder was the most common medical disorder, but severity was high in cardiac disorder. SOFA and APACHE II scores are good predictors of morbidity and mortality risk.
Keywords: Medical disorders, Emergency obstetric care, APACHE II, SOFA score, Maternal mortality
Introduction
Medical problems may interfere with the physiologic adaptations of pregnancy and cause poor pregnancy outcomes. In the current scenario, pregnant women with medical disorders are increasing, mainly due to demographic, lifestyle factors and most often get referred to tertiary care with complications. The later age of getting married and advanced age at conception are the main factors. Mothers and Babies: Reducing Risk through Audits and Confidential E enquiries (MBRRACE) report in 2011–2013 reported that two-thirds of maternal deaths were in women with medical comorbidities [1]. Identifying and predicting mortality risks will help in providing better care. SOFA (Sequential Organ Failure Assessment) and APACHE II (Acute Physiology And Chronic Health Evaluation II) scores are scores used in critical patients in intensive care unit to predict the acute mortality risk. APACHE II score (range from 0 to 71) was derived from 12 physiologic measurements which includes temperature, blood pressure, heart rate, respiratory rate, arterial pH, oxygenation, serum sodium, potassium and creatinine, haematocrit, white blood cell count and Glasgow coma score, in addition to chronic health status and age of the patient. SOFA score (range from 0 to 24) includes platelet, hepatic, respiratory, renal, cardiovascular and central nervous system functions. The objectives of this study were: (1.) to know the type and proportion of pregnant women with medical disorders seeking emergency care and (2.) to predict mortality risk by using SOFA (Sequential Organ Failure Assessment) and APACHE II (Acute Physiology and Chronic Health Evaluation II) scores. The purpose of predicting mortality risk in these women is to provide effective and timely multidisciplinary care and also to counsel the attendants of the women regarding the seriousness of the condition and take informed consent.
Materials and Methods
This prospective observational study was conducted from April 2021 to September 2021 after obtaining ethical clearance (JIP/IEC/2021/059). All pregnant and post-partum women (up to 6 weeks) with medical disorders who attended Emergency obstetric services at Women and Child Hospital (with dedicated obstetric ICU facility), JIPMER, Puducherry, were included in the study.
Inclusion Criteria
Pregnant women who sought emergency obstetric care with pre-existing medical disorders or medical disorders diagnosed or developed during pregnancy.
Age > 18 years.
Post-partum women (≤ 6 weeks) with medical disorders.
Exclusion Criteria
Pregnant women with only obstetric complications, viz. obstetric haemorrhage, malpresentation in labour, PPROM, rupture uterus, cord prolapse and acute polyhydramnios.
Sampling Population and Sample Size Calculation
We included all pregnant women with medical disorders who came for emergency obstetric care over 6 months and assumed the proportion of pregnant women requiring ICU care with the medical disorder as 3% (based on records from JIPMER). The calculated absolute precision of 3% at 95% CI using the Open-Epi statistical tool number was 125. Subjects included in this study during the 6-month period (April 2021 to September 2021) were 128.
Study Procedure
All women who satisfied the inclusion criteria were enrolled in the study. Patients were initially identified daily after referring to casualty admission register, confinement register, eclampsia room, obstetric ICU register, critical care ICU register and on enquiries from colleagues of all units and staff nurses of various wards. The study procedure was explained to the patients and/or relatives. Informed consent and details were taken from the patient if she is conscious and oriented; otherwise, the same was obtained from the relative. Any referral letter, if present, was obtained from the case record.
A detailed history was taken regarding antenatal care and the reason for morbidity. General physical examination was carried out, and investigation reports were reviewed. The assessment was done using the clinical and laboratory parameters. The nature of complications, their management and organs involved were noted. Type of medical disorder diagnosed as per the system/s involved. The severity of the disease was assessed using mantel’s organ dysfunction criteria [2]. Mortality risk predicted using SOFA [3] and APACHE II [4] scores at the time of admission. Calculation of scores is shown in Appendix 1. All the women were followed until discharge, the maternal and foetal outcomes and the causes of mortality were noted, and the data were entered into the data collection proforma.
Statistical Analysis
All data were computerized and analysed by SPSS software. All the continuous variables were expressed as mean, standard deviation or median with inter-quartile range based on normality of the data. All the categorical variables were expressed as numbers and percentages.
The SOFA score and APACHE II performance in predicting morbidity and mortality risk was determined using receiver operating characteristic (ROC) curves using STATA. The ROC curve was generated, and the cut-off value was determined to evaluate the usefulness of the SOFA score and APACHE II score to predict mortality for obstetric patients. The AUC-ROC curve obtained the power of discrimination, and their specific 95% CIs was used to show the precision of the estimate. Mann–Whitney U test was used to compare scores between the survival group and the non-survival group.
Results
There were a total of 4781 deliveries during this study period of six months. A total of 128 patients with medical disorders who approached for emergency obstetric care in the Department of Obstetrics and Gynaecology, JIPMER, were recruited and analysed.
Table 1 represents the clinicodemographic profile of subjects. The majority of women were in the age group of 20–25 years and mean age of 26.4 ± 4.9 years. BMI was in the normal range in 57% and the mean BMI of 23.0633 ± 0.669 kg/m2. Most of the women (55.46%) were in the upper–lower socio-economic class according to modified Kuppusamy classification and the majority (82%) resided in rural areas. Referral cases constituted 76.56% and they were referred from various hospitals including medical colleges, district hospitals, private hospitals and primary health centres for further management. Pregnant women constituted 87.5% at the time of admission and the rest were post-partum women delivered elsewhere.
Table 1.
Clinicodemographic details of women included in the study
| S. No | Parameter | Number (N = 128) | Percentage (%) |
|---|---|---|---|
| I | Age in years | ||
| A | ≤ 20 | 3 | 2.34 |
| B | 20–25 | 58 | 45.31 |
| C | 26–30 | 47 | 36.72 |
| D | 31–35 | 14 | 10.94 |
| E | 36–40 | 5 | 3.91 |
| F | > 40 | 1 | 0.78 |
| II | BMI (kg/m2) | ||
| A | ≤ 18.5 (underweight) | 15 | 11.7 |
| B | 18.51–25 (normal) | 73 | 57.0 |
| C | 25.01–30 (overweight) | 34 | 26.6 |
| D | 30.01–35 (obese class I) | 5 | 3.9 |
| E | > 35.01 (obese class II) | 1 | 0.8 |
| III | Socioeconomic status (modified Kuppusamy classification*) | ||
| A | Upper (score of 26–29) | 0 | 0 |
| B | Upper middle (score of 16–25) | 13 | 13 (10.16) |
| C | Lower middle (score of 11–15) | 40 | 40 (31.25) |
| D | Upper lower (score of 5–10) | 71 | 71 (55.46) |
| E | Lower (score of < 5) | 4 | 4 (3.13) |
| IV | Area | ||
| A | Rural | 105 | 82.03 |
| B | Urban | 23 | 17.97 |
| V | Referred cases | 98 | 76.56 |
| VI | Obstetric status at admission | ||
| A | Pregnant | 112 | 87.5 |
| B | Post-partum | 16 | 12.5 |
* Includes occupation of head of the family, education of the head of the family and total monthly income of the family
Table 2 presents the obstetric status at admission. Most of the women were multigravidae (56.25%) and 43.75% (49/112) were primigravida. Among pregnant women, 75% (84/112) were in the third trimester, and among them, 75% (63/84) were preterm at the time of presentation. Twenty-one women (18.75%) were discharged after management and continued their pregnancy.
Table 2.
Gestational age of pregnant women and status of post-partum women at the time of admission
| S. No | Obstetric status | Gravidity | Number | Percentage (%) | |
|---|---|---|---|---|---|
| I | Trimester of Pregnancy | Primigravida (N = 49) | Multigravida (N = 63) | 112 | 87.5 |
| a) | First trimester | 1 | 1 | 2 | 1.79 |
| b) | Second trimester | 13 | 13 | 26 | 23.21 |
| II | Third trimester (GA in weeks) | 35 | 49 | 84 | 75 |
| Very preterm (28–31+6 weeks) | 11 | 13 | 24 | 21.43 | |
| Moderate preterm (32–33+6 weeks) | 6 | 8 | 14 | 12.5 | |
| Late preterm (34–36+6 weeks) | 11 | 14 | 25 | 22.32 | |
| Early term (37–38+6 weeks) | 6 | 10 | 16 | 14.29 | |
| Full term (39–40+6 weeks) | 1 | 4 | 5 | 4.46 | |
| Post-term (41 to 42 weeks) | 0 | 0 | 0 | 0 | |
| III | Post-partum | 10 | 6 | 16 | 12.5 |
| a) | Immediate post-partum | 1 | 2 | 3 | 18.75 |
| b) | Within one week | 6 | 3 | 9 | 56.25 |
| c) | More than one week | 3 | 1 | 4 | 25 |
Table 3 shows the type and severity of medical disorders. Hypertensive disorders were the most common (25.7%) medical disorder in this study, followed by cardiovascular disease (22.6%) and neurological disease (12.5%). Regarding the severity, which was assessed using Mantel’s organ dysfunction criteria, majority had cardiac dysfunction (32.21%) followed by liver dysfunction (15.25%), respiratory dysfunction (11.86%) and coagulation dysfunction (11.86%) (Table 4).
Table 3.
Major systems involved in the study population
| S. NO | Major Systems Involved | Pregnancy N = 112 | Post-partum N = 16 | Total N = 128 | Percentage (%) |
|---|---|---|---|---|---|
| I | Hypertensive Disorders of Pregnancy | 25 | 8 | 33 | 25.7 |
| Severe Preeclampsia | 7 | 1 | 8 | ||
| HELLP syndrome | 5 | 1 | 6 | ||
| Eclampsia | 13 | 6 | 17 | ||
| II | Cardiovascular disease | 29 | 0 | 29 | 22.6 |
| Valvular heart disease | 12 | 12 | |||
| Congenital heart disease | 5 | 5 | |||
| Prosthetic heart valve | 5 | 5 | |||
| Pulmonary artery hypertension | 4 | 4 | |||
| Cardiomyopathy | 2 | 2 | |||
| Heart block | 1 | 1 | |||
| II | Neurological Disease | 14 | 2 | 16 | 12.5 |
| Seizure disorder | 7 | 7 | |||
| Intracranial haemorrhage | 0 | 1 | 1 | ||
| Meningoencephalitis | 1 | 1 | |||
| GBS (Guillain–Barre syndrome) | 2 | 2 | |||
| Cerebral venous thrombosis | 1 | 1 | 2 | ||
| Quadriparesis—Barter’s syndrome | 1 | 1 | |||
| Transverse myelitis | 1 | 1 | |||
| Idiopathic intracranial hypertension | 1 | 1 | |||
| IV | Infectious Disease | 9 | 3 | 12 | 9.4 |
| COVID-19 | 5 | 5 | |||
| Dengue | 2 | 2 | |||
| Sepsis | 1 | 3 | 4 | ||
| Cellulitis | 1 | 1 | |||
| V | Haematological Disease | 9 | 2 | 11 | 8.6 |
| Pancytopenia | 4 | 4 | |||
| ITP (Ideopathic Thrombocytopenia) | 3 | 3 | |||
| DIC (Disseminated intravascular Coagulation) | 0 | 2 | 2 | ||
| Severe anaemia | 1 | 1 | |||
| VI | Gastrointestinal disease | 8 | 1 | 9 | 7.1 |
| Chronic liver disease | 2 | 2 | |||
| Non-cirrhotic portal fibrosis | 4 | 4 | |||
| Acute Fatty Liver of Pregnancy (AFLP) | 1 | 1 | 2 | ||
| Pancreatitis | 1 | 1 | |||
| VII | Connective tissue disorder | 7 | 0 | 7 | 5.4 |
| Systemic Lupus Erythematosus | 6 | 6 | |||
| Takayasu arteritis | 1 | 1 | |||
| VIII | Renal disease—CKD | 6 | 0 | 6 | 4.7 |
| IX | Endocrinological disorder | 4 | 0 | 4 | 3.1 |
| Diabetic Ketoacidosis | 2 | 2 | |||
| Hyperthyroidism | 1 | 1 | |||
| Primary adrenal insufficiency | 1 | 1 | |||
| X | Poisoning (oleander seed) | 1 | 0 | 1 | 0.8 |
Table 4.
SAMM as per Mantel’s criteria at admission
| S. no | Mantel’s criteria | Number (N = 59) | Percentage (%) |
|---|---|---|---|
| 1 | Cardiac dysfunction | 19 | 32.21 |
| 2 | Liver dysfunction | 9 | 15.25 |
| 3 | Respiratory dysfunction | 7 | 11.86 |
| 4 | Coagulation dysfunction | 7 | 11.86 |
| 5 | Renal dysfunction | 6 | 10.17 |
| 6 | Cerebral dysfunction | 5 | 8.47 |
| 7 | Immunological dysfunction | 4 | 6.8 |
| 8 | Metabolic dysfunction | 1 | 1.69 |
| 9 | Emergency hysterectomy | 1 | 1.69 |
ROC curve was generated to assess the diagnostic accuracy of the APACHE II score to detect mortality risk. ROC curve was drawn by a nonparametric method using STATA (AUC = 0.7324, 95% CI = 0.64696; 0.81779, p < 0.001). The optimal cut-off was 6 with sensitivity and specificity of 60.27% and 78.18% (Fig. 1).
Fig. 1.
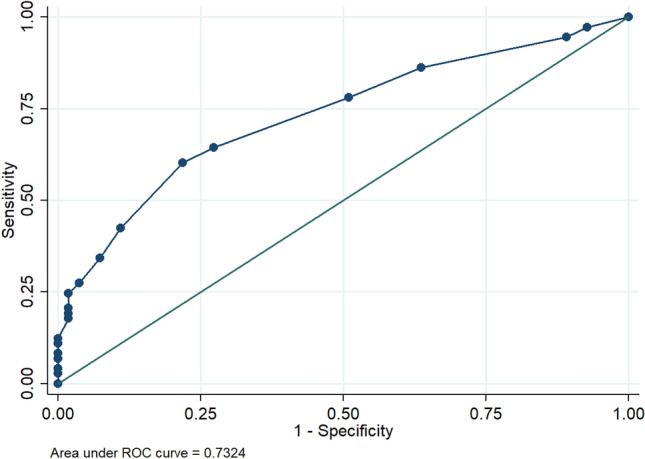
Receiver operating characteristic (ROC) curve of the acute physiology and chronic health evaluation II (APACHE II) score to predict mortality in obstetric patients with medical disorders
ROC curve was generated to assess the diagnostic accuracy of the SOFA score to detect mortality risk. ROC curve was drawn by a nonparametric method using STATA (AUC = 0.7399, 95% CI = 0.65733; 0.82237, p < 0.001). The optimal cut-off was 2 with sensitivity and specificity of 65.75% and 70.91% (Fig. 2).
Fig. 2.

Receiver operating characteristic (ROC) curve of the Sequential Organ Failure Assessment (SOFA) score to predict mortality in obstetric patients with medical disorders
In this study, the median value of APACHE II score and SOFA score were high in the non-survival group when compared to the survival group, which was statistically significant. Hence, APACHE II and SOFA scores are good scores in predicting maternal mortality (Table 5).
Table 5.
Median value of scores in survival and non-survival group
| Score | Non-survival group (N = 9) | Survival group (N = 119) | P-value* |
|---|---|---|---|
| APACHE II (median value) | 14 (IQR 6.5–20.5) | 4 (IQR 2–7) | 0.0002 |
| SOFA score (median value) | 4 (IQR 3–6.5) | 1 (IQR 0–3) | 0.00036 |
*Mann–Whitney U test
SAMM (severe acute maternal morbidity) was 17.53 per 1000 live births. There were 9 maternal deaths (7% of the study population). The maternal morbidity-to-mortality ratio = SAMM/MD = 9.1; Mortality index = MD/SAMM = 10.9%. MMR (maternal mortality rate) was 320.7 per 1,00,000 live births. The perinatal mortality rate was 49.9 per 1000 births.
The causes of maternal mortality were COVID-associated pneumonia and ARDS in 4, intracranial haemorrhage complication of HDP in 2 and eclampsia with cardiac arrest in one women. One women died of meningoencephalitis and another women of recurrent pregnancy loss with severe pulmonary arterial hypertension with thrombotic thrombocytopenic purpura with IVF pregnancy.
Discussion
Due to advancements in the medical field and lifestyle factors, many pregnant women with medical disorders are getting pregnant, and also medical diseases are newly detected during pregnancy. Medical illnesses are emerging as leading causes of maternal morbidity and mortality. It is crucial to predict the risk of mortality to monitor closely and take measures to prevent mortality. This is a prospective observational study in which prediction of mortality was undertaken using APACHE II and SOFA scores.
In this study, hypertensive disorders of pregnancy were the most common (25.7%), followed by the cardiovascular system (22.6%) and central nervous system (12.5%). This is similar to the studies of Demirkiran, Keizer et al. and Vargas et al., in which hypertensive disorder was the most common, viz. 73.6%, 62% and 25%, respectively [5–7].
In the present study, there were 59 (46%) cases who met the criteria of Mantel’s, but in the study by Pattinson et al. there were more cases (423 cases) with organ dysfunction and Parmar et al. showed only 38 cases (60%) with organ dysfunction [8, 9]. We found cardiac dysfunction as the most common organ dysfunction (32.21%), which was comparable with the studies by Pattinson et al. and Rohit Kumar et al., where cardiac dysfunction was 36.8% and 38.6%, respectively [8, 10].
APACHE II and SOFA scoring were employed in various studies to predict the mortality risk. In India, Sodhi et al. in Punjab conducted a prospective study on 48 obstetric patients in non-obstetric ICU from January 2015 to June 2016. The mean APACHE II score for discharged patients was 10.11 ± 5.33 versus 22.60 ± 6.45 of patients who died. The mean SOFA score for discharged patients was 4.81 ± 2.60 versus 12.10 ± 4.25 for patients who died. In the present study, the median APACHE II score of discharged patients was 4 (IQR 2–7) versus 14 (IQR 6.5–20.5) for death patients and the median SOFA score of 1 (IQR 0–3) for discharged patients versus 4 (IQR 3–6.5) for death patients. These values were lower than the study by Sodhi et al. [11]. Fadiloglu et al. conducted a retrospective study in Turkey from 2007 to 2017 among 160 patients and found an AUC of 0.971 for APACHE II with cut-off of 24.5 (sensitivity of 100% and specificity of 95.7%). AUC was 0.901 for the initial SOFA score and the cut-off value for the initial SOFA score was 3.5 (sensitivity of 100% and specificity of 67.4%) [12]. In the present study, AUC for APACHE II and SOFA scores were 0.7324 and 0.7399, respectively.
APACHE II with cut-off ≥ 6 (with a sensitivity of 60.27% and specificity of 78.18%) and SOFA score with cut-off ≥ 2 (sensitivity of 65.7% and specificity of 70.9%) predicted maternal mortality. The cut of values were lower in the present study, but the median scores for non-survivors were high. (APACHE-II was 14, and SOFA score was 4.) In the prospective study by Rohit Kumar et al. which was conducted at New Delhi among 101 obstetric admissions, AUC of SOFA and APACHE II were 0.867 (95% CI = 0.755–0.979) and 0.850 (95% CI = 0.720–0.980), respectively. Mean SOFA score of 7.02 ± 2.96 for survivors and 14.06 ± 4.61 for non-survivors. They reported mean APACHE II of 15.87 ± 4.92 for survivors and 28.94 ± 10.92 for non-survivors [10]. In this study, the cut-off values were higher than our study. Monali Khergade conducted a cohort study in 250 obstetric cases at New Delhi and found AU-ROC of APACHE II was 0.93 (95% CI 0.891–0.958) and cut-off of > 12 had a sensitivity of 93.85% and specificity of 82.16%, whereas the AU-ROC of SOFA score was 0.924 (95% CI 0.884–0.954) with cut-off of > 5 had a sensitivity of 92.31% and specificity of 76.22% [13]. Here also the cut-off values were higher than our study.
The lower cut-off values in the present study may be due to the assessment of scores within 24 h of admission. This was undertaken with the idea that the results/cut-off values of scores would be useful to counsel the future patients about morbidity and mortality risk. The scores should be done every day as once organ dysfunction occurs or becomes severe, the scores differ and the interpretation of morbidity mortality risk changes. Mean SOFA score is calculated over a course based up on SOFA score of each day. SOFA score of 2 points or more is associated with hospital mortality greater than 10% [14]. Some women who had organ dysfunction would have deteriorated later and developed SAMM or mortality as there were 82 women with SAMM at the time of discharge. Another reason for the low cut-off scores is that scores were applied to all women with medical disorders who were admitted through emergency services and not only to those who were morbidly sick. Initially women with COVID-19 were admitted to Ward with fever and respiratory symptoms and diagnosed infectious cause of respiratory system. Moreover, 46% were classified as SAMM as per Mantel’s criteria of organ dysfunction.
Neto et al. conducted a retrospective study in Brazil among 279 women from 2013 to 2015 and found the APACHE II cut-off ≥ 9 with sensitivity 64.6% and specificity of 78% and total SOFA cut-off ≥ 3 with sensitivity of 67.7% and specificity of 88.8%. AUC of APACHE II was 0.779 and SOFA was 0.833 [15]. Total SOFA had a better performance than the others for the prediction of mortality. These values were comparable to our study. Neto et al. also conducted another retrospective study in Brazil from 2002 to 2007 and found 673 cases of severe maternal morbidity were admitted in the ICU. The performance of the total maximum SOFA score for the obstetrical population with severe maternal morbidity was excellent with AUC 0.958 (95% CI: 0.914–1.0). The total maximum SOFA score cut-off 6 showed a sensitivity of 88.9% and specificity of 91.1% in predicting maternal mortality [16]. From this study, they concluded that SOFA score is an effective tool for predicting mortality. SOFA score is simple and easy to calculate than APACHE II score. From the above studies, it seems SOFA score to be an ideal scoring system for obstetric patients in predicting mortality risk.
Obstetric Outcome
Among pregnant women, 18.75% continued their pregnancy and were discharged. There was one ectopic pregnancy and three abortions. MTP was done in two cases for saving maternal life, and the indications were severe aortic stenosis with NYHA class III and another with severe pulmonary artery hypertension with right ventricular dysfunction. Forty pregnant women delivered vaginally, and 42 women underwent caesarean section, and the most common indication for caesarean section was maternal deterioration (35%) followed by pathological CTG (21.43%). Thirty pregnant women were induced for various indications; intrauterine foetal demise was the common indication (16.67%), followed by eclampsia (13.33%). Of total induced, 76.67% delivered vaginally. In the above mentioned studies, obstetric outcomes were not analysed. There were nine maternal deaths in our study population, and the most common cause of maternal death was associated with COVID-associated pneumonia and ARDS (45%).
There were 82 cases of SAMM at the time of discharge on follow-up, and hence, the SAMM ratio was 17.53 per 1000 live births during the study period; this was comparable to 17.8 per 1000 live births in the study by Ps et al. but higher than the study by Norhayati et al. where the ratio was only 2.2 per 1000 live births [17, 18]. This is because our hospital is a tertiary care centre and receives more morbid cases from other hospitals.
The maternal mortality ratio was 320.7 per 1,00,000 live births during this period. The maternal morbidity-to-mortality ratio was 9.1 in this study, which was higher when compared to the studies by Bindal et al. and Siddiqui et al., where the morbidity-to-mortality ratios were 5.4 and 5.8, respectively [19, 20]. Higher morbidity-to-mortality ratio implies a good standard of care. The mortality index was 10.9% in our study was lower than an Indian study by Parmar et al. (28.1%) [9]. The lower the mortality index, the better the standard of care. Maternal mortality in our study (7.03%) is lower than the mortality rates in the studies by Bhadade et al., Jain et al. and Kamal et al., which was 30.3%, 33.3% and 20%, respectively [21–23].
Strengths and Limitations
The strengths of this study are this is a prospective observational study that included women with medical disorders with emergency care conducted in the Department of Obstetrics and Gynaecology in a tertiary care institution in South India, with a dedicated obstetric ICU facility. The limitation of the study was the small sample size over a 6 months period only. The period of study fell during COVID-19 pandemic, and hence, this could have influenced the morbidity and mortality results.
For future research: APACHE II and SOFA scores are good predictors of maternal mortality; large studies required to confirm the same. These scoring systems are meant for general populations. Due to the physiological adaptations during pregnancy, the normal range of various parameters are different in pregnant women. So, some modifications in the APACHE II and SOFA scores may increase the sensitivity and specificity in predicting mortality in pregnant population. These scores may be used for women with organ dysfunction to predict mortality and SOFA score to be done daily to assess prognosis.
Conclusion
Even though hypertensive disorders were the most common medical disorder in our study, severity was more among women the cardiac disorder. APACHE II cut-off ≥ 6 and SOFA score cut-off ≥ 2 predicts maternal mortality risk. Both SOFA and APACHE II scores are good predictors of maternal mortality risk. The SOFA score is simple and easier to calculate when compared to the APACHE II score, as it has fewer variables.
Acknowledgment
The authors thank Dr Simi, Resident in the Department of Preventive and Social Medicine, for her help in statistical analysis.
Papa Dasari
has obtained her MBBS in 1984, DGO in 1987, MD in 1988 from JIPMER, Puducherry, and working as faculty since 1995 in the same Institute. She has teaching experience of 32 years and is examiner for UG, PG and postdoctoral courses in Obstetrics and Gynaecology and Reproductive Medicine of various Universities and for DNB and FNB under National Board of Examinations. She has 10 awards for her scientific contributions and has over 180 publications in national and international journals and also a peer reviwer. Her noteworthy work was innovation of skill certification programmes for UGs and PGs, provision of HPV-DNA test and HPV vaccination, establishing HDU, ART services and introduction of Birth Companion Policy (RMC) as per Govt of India Guidelines at JIPMER.
Appendix 1
Calculation of apache II score: value range from 0 to 71.
APACHE II Score = Acute physiology score (A) + Glasgow coma score (B) + Chronic health points (C).
A. Acute physiology score
| Acute physiology score | Normal range | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Score | 4 | 3 | 2 | 1 | 0 | 1 | 2 | 3 | 4 |
| Rectal temperature (°C) | ≥ 41 | 39–40.9 | – | 38.5–38.9 | 36–38.4 | 34–35.9 | 32–33.9 | 30–31.9 | ≤ 29.9 |
| Mean blood pressure (mmHg) | ≥ 160 | 130–159 | 110–129 | – | 70–109 | – | 50–69 | – | ≤ 49 |
| Heart rate | ≥ 180 | 140–179 | 110–139 | – | 70–109 | – | 55–69 | 45–54 | ≤ 39 |
| Respiratory rate | ≥ 50 | 35–49 | – | 25–34 | 12–24 | 10–11 | 6–9 | – | ≤ 5 |
| Arterial pH | ≥ 7.7 | 7.6–7.69 | – | 7.5 –7.59 | 7.33–7.49 | – | 7.25–7.32 | 7.15–7.24 | ≤ 7.15 |
| Oxygenation, PaO2 | ≥ 500 | 350–499 | 200–349 | – | < 200 > 70 | 61–70 | – | 55–60 | < 55 |
| Serum sodium (mEq/L) | ≥ 180 | 160–179 | 155–159 | 150–154 | 130–149 | – | 120–129 | 111–119 | ≤ 110 |
| Serum potassium (mEq/L) | ≥ 7 | 6–6.9 | – | 5.5–5.9 | 3.5–5.4 | 3–3.4 | 2.5–2.9 | – | < 2.5 |
| Serum creatinine (mg/dL) | ≥ 3.5 | 2–3.4 | 1.5–1.9 | – | 0.6–1.4 | – | < 0.6 | – | – |
| Haematocrit (%) | ≥ 60 | – | 50–59.9 | 46–49.9 | 30–45.9 | – | 20–29.9 | – | < 20 |
| WBC count (103/ml) | ≥ 40 | – | 20–39.9 | 15–19.9 | 3–14.9 | – | 1–2.9 | – | < 1 |
B. Glasgow coma scale
| Eye opening | Verbal non-intubated | Verbal intubated | Motor activity |
|---|---|---|---|
| 4 = spontaneous | 5—Oriented and talks | 5—Seems able to talk | 6—Verbal command |
| 3 = verbal stimuli | 4—Disoriented and talks | 3—Questionable ability to talk | 5—Localizes to pain |
| 2 = painful stimuli | 3—Inappropriate words | 1—Generally unresponsive | 4—Withdraws from pain |
| 1 = no response | 2—Incomprehensible sounds | 3—Decorticate | |
| 1—No response | 2—Decerebrate | ||
| 1—No response |
C. Chronic health points
| History of chronic condition | Score |
|---|---|
| None | 0 |
| If elective post-operative patient with immunocompromise or severe organ insufficiency | 2 |
| Non-operative patient or emergency post-operative patient with immunocompromise or severe organ insufficiency | 5 |
D. Calculation of SOFA score: value range from 0 to 24
| System | Scores | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |
| Respiratory system parameter, PaO2/FiO2 (mmHg) | ≥ 400 | < 400 | < 300 | < 200 | < 100 |
| Coagulation system Platelets *103/µL | > 150 | < 150 | < 100 | < 50 | < 20 |
| Hepatobiliary system parameter Bilirubin, mg/dL | < 1.2 | 1.2–1.9 | 2–5.9 | 6–11.9 | > 12 |
| Cardiovascular parameter | MAP > 70 mmHg | MAP < 70 mmHg | Dopamine < 5 or dobutamine (any dose) | Dopamine 5.1–15 or epinephrine < 0.1 or norepinephrine < 0.1 | Dopamine > 15 or Epinephrine > 0.1 or norepinephrine > 0.1 |
| Central nervous system Glasgow coma scale | 15 | 13–14 | 10–12 | 6–9 | < 6 |
| Renal parameters creatinine, mg/dL | < 1.2 | 1.2–1.9 | 2–3.4 | 3.5–4.9 | > 5 |
| Urine output, ml/day | < 500 | < 200 | |||
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
Declarations
Conflict of interest
The author(s) declared no potential conflict of interest with respect to the research, authorship and/or publication of this article.
Ethical Approval
All data collected after getting approval from institutional ethical committee (JIP/IEC/2021/059).
Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with Helsinki Declaration 1975, as revised in 2008.
Informed Consent of Publications
Informed consent was obtained from all women for being included in the study.
Footnotes
Mecheril Balachandran Divya (MBBS, MS OBG, PDF Obstetric Medicine) is a Former Senior Resident; Papa Dasari (MD, DGO, FICOG, PDCR) is a Senior Professor.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Narayan B, Nelson-Piercy C. Medical problems in pregnancy. Clin Med. 2017;17(3):251. doi: 10.7861/clinmedicine.17-3-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mantel GD, Buchmann E, Rees H, et al. Severe acute maternal morbidity: a pilot study of a definition for a near-miss. BJOG Int J Obstet Gynaecol. 1998;105(9):985–90. doi: 10.1111/j.1471-0528.1998.tb10262.x. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira FL, Bota DP, Bross A, et al. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754–8. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 4.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29. doi: 10.1097/00003246-198510000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Demirkiran O, Dikmen Y, Utku T, et al. Critically ill obstetric patients in the intensive care unit. Int J Obstet Anesth. 2003;12(4):266–70. doi: 10.1016/S0959-289X(02)00197-8. [DOI] [PubMed] [Google Scholar]
- 6.Keizer JL, Zwart JJ, Meerman RH, et al. Obstetric intensive care admissions: a 12-year review in a tertiary care centre. Europ J Obstet Gynecol Reprod Biol. 2006;128(1–2):152–6. doi: 10.1016/j.ejogrb.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 7.Vargas M, Marra A, Buonanno P, et al. Obstetric admissions in ICU in a tertiary care center: a 5-years retrospective study. Indian J Crit Care Med Peer-Rev. 2019;23(5):213. doi: 10.5005/jp-journals-10071-23163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pattinson RC, Buchmann E, Mantel G, et al. Can enquiries into severe acute maternal morbidity act as a surrogate for maternal death enquiries? BJOG Int J Obstet Gynaecol. 2003;110(10):889–93. doi: 10.1111/j.1471-0528.2003.03044.x. [DOI] [PubMed] [Google Scholar]
- 9.Parmar NT, Parmar AG, Mazumdar VS. Incidence of maternal “near-miss” events in a tertiary care hospital of central Gujarat, India. J Obstet Gynecol India. 2016;66(1):315–20. doi: 10.1007/s13224-016-0901-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar R, Gupta A, Suri T, et al. Determinants of maternal mortality in a critical care unit: a prospective analysis. Lung India. 2022;39(1):44–50. doi: 10.4103/lungindia.lungindia_157_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sodhi K, Bansal V, Shrivastava A, et al. Predictors of mortality in critically ill obstetric patients in a tertiary care intensive care unit: a prospective 18 months study. J Obstet Anaesth Crit Care. 2018;8(2):73. doi: 10.4103/joacc.JOACC_57_17. [DOI] [Google Scholar]
- 12.Fadiloglu E, Yuksel ND, Unal C, et al. Characteristics of obstetric admissions to intensive care unit: APACHE II, SOFA and the Glasgow coma scale. J Perinat Med. 2019;47(9):947–57. doi: 10.1515/jpm-2019-0125. [DOI] [PubMed] [Google Scholar]
- 13.Khergade M, Suri J, Bharti R, et al. Obstetric early warning score for prognostication of critically ill obstetric patient. Indian J Crit Care Med Peer-Rev. 2020;24(6):398. doi: 10.5005/jp-journals-10071-23453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Escobar MF, Nasner D, Hurtado CF, et al. Characterization of obstetric patients with sepsis identified by two diagnostic scales at a fourth-level clinic in Colombia. Int J Gynecol Obstet. 2018;143(1):71–6. doi: 10.1002/ijgo.12580. [DOI] [PubMed] [Google Scholar]
- 15.Oliveira-Neto AF, Parpinelli MA, Costa ML, et al. Prediction of severe maternal outcome among pregnant and puerperal women in obstetric ICU. Crit Care Med. 2019;47(2):e136–43. doi: 10.1097/CCM.0000000000003549. [DOI] [PubMed] [Google Scholar]
- 16.Oliveira-Neto A, Parpinelli MA, Cecatti JG, et al. Sequential organ failure assessment score for evaluating organ failure and outcome of severe maternal morbidity in obstetric intensive care. Sci World J. 2012;1:2012. doi: 10.1100/2012/172145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roopa P, Verma S, Rai L, et al. “Nearmiss” obstetric events and maternal deaths in a tertiary care hospital: an audit. J Pregnancy. 2013;2013:393758. doi: 10.1155/2013/393758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Norhayati MN, Hazlina NH, Sulaiman Z, et al. Severe maternal morbidity and near misses in tertiary hospitals, Kelantan, Malaysia: a cross-sectional study. BMC Public Health. 2016;16(1):1–3. doi: 10.1186/s12889-016-2895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Binda J, Solanki G. Clinical and etiological study of maternal near-miss at a tertiary referral hospital of central India. Indian J Obstet Gynaecol Res. 2016;3(1):28–31. doi: 10.5958/2394-2754.2016.00006.0. [DOI] [Google Scholar]
- 20.Siddiqui SA, Soomro N, Hasnain FS. Severe obstetric morbidity and its outcome in patients presenting in a tertiary care hospital of Karachi. JPMA J Pak Med Assoc. 2012;62(3):226. [PubMed] [Google Scholar]
- 21.Bhadade R, de Souza R, More A, et al. Maternal outcomes in critically ill obstetrics patients: a unique challenge. Indian J Crit Care Med Peer-Reviewed Off Publ Indian Soc Crit Care Med. 2012;16(1):8. doi: 10.4103/0972-5229.94416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jain S, Guleria K, Vaid NB, et al. Predictors and outcome of obstetric admissions to intensive care unit: a comparative study. Indian J Public Health. 2016;60(2):15914. doi: 10.4103/0019-557X.184575. [DOI] [PubMed] [Google Scholar]
- 23.Kamal S, Singh V, Singh S. A study of clinical characteristics and outcome of obstetric patients in intensive care and high dependency unit of a tertiary centre of Jharkhand, India. Int J Reprod Contracept Obstet Gynecol. 2020;9:394–9. doi: 10.18203/2320-1770.ijrcog20196054. [DOI] [Google Scholar]


