Abstract
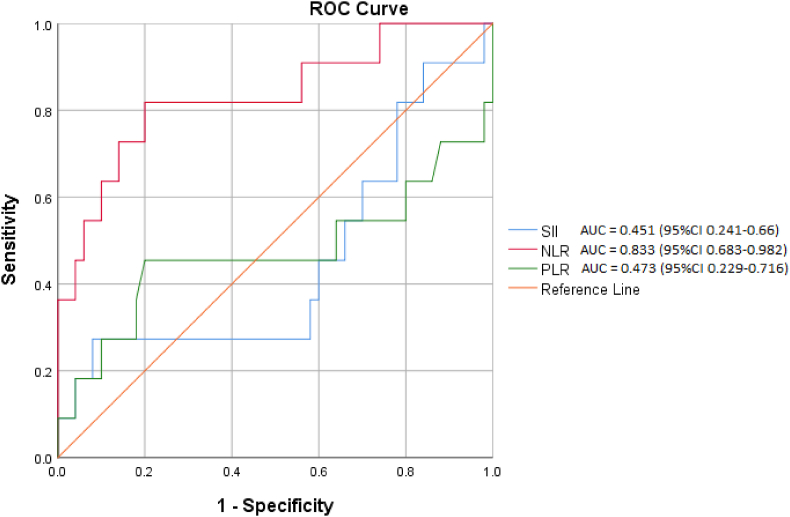
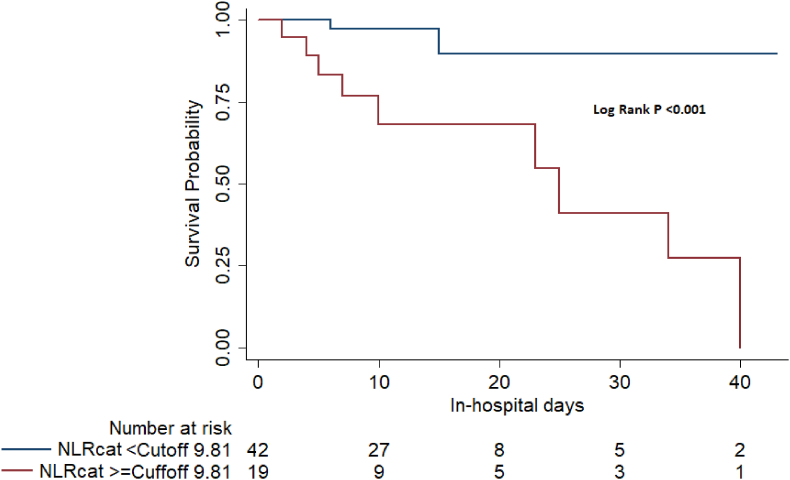
Infective Endocarditis (IE) remains a life-threatening condition and early risk stratification helps us to predict mortality and the need for aggressive treatment. We compared NLR, PLR, and SII, on admission to predict in-hospital mortality. Consecutive IE patients, who met inclusion criteria were analysed. Receiver operating characteristic curve (ROC) analysis was conducted for NLR, PLR, and SII to predict in-hospital mortality. The median value of NLR was 19.6 (10.1–27) in patients with mortality, and 5.4 (3.2–8.5) in alive patients. The median value of PLR and SII were comparable in both groups. The area under the ROC curve of NLR showed a significant value of 0.83 (p = 0.001). A Kaplan Meier survival analysis for patients taking a cut-off value of NLR (9.8) was statistically significant (p < 0.001). In multivariate regression model, only NLR was statistically significant predictor of mortality. So NLR, which is a simple, readily available, and inexpensive parameter has a better association with in-hospital mortality in IE patients.
Keywords: Infective endocarditis, Neutrophil to lymphocyte ratio, In-hospital mortality
1. Introduction
Early risk prediction is important in improving outcomes in Infective endocarditis (IE). Various association studies have focused on identifying widely available and inexpensive inflammatory markers to predict prognosis in IE.1 The platelet-to-lymphocyte ratio (PLR) and neutrophil-to-lymphocyte ratio (NLR) are used as a biomarker to predict the degree of inflammation.2,3 NLR and PLR are found to be independent predictors of worse prognosis in IE.4 Systemic immune-inflammation index (SII), which integrates three types of inflammatory cells (platelet, neutrophil, and lymphocytes), is a promising predictor of adverse events in many immune-related, inflammatory, and infectious diseases.5 Recently two studies have found that high SII levels are independently associated with mortality and embolic events in IE.6,7 NLR has been shown to have a high predictive value for many cardiovascular diseases. However, data are scarce on its predictive value in IE patients. This study aimed to see if the NLR, PLR, and SII, assessed on admission, had any relationship with IE patients and compare how well these indexes could predict mortality.
2. Materials and methods
The IE cases admitted at our centre, who met inclusion criteria were recruited for the study. Patients for whom complete laboratory data available were only enrolled. Patients who did not meet Duke's criteria, age <18 years, patients with inflammatory, autoimmune diseases and cancers were excluded. Haematological tests done on first day of the patient's stay in the hospital were taken. The neutrophil-lymphocyte ratio (NLR) was computed by dividing the absolute neutrophil count by the absolute lymphocyte count. The platelet-to-lymphocyte ratio (PLR) was computed by dividing platelet count by absolute lymphocyte count. The Systemic immune-inflammation index (SII) was calculated as: SII = platelet count × neutrophil count/lymphocyte count. The adverse clinical events in the study endpoints included hospital death, heart failure, embolic events, recurrence and renal failure.
The effects of variables on in-hospital mortality were calculated by bivariate analysis. The variables for which the p-value <0.1 in the bivariate analysis were included in the binary logistic regression model. Chi-square or Fischer exact tests were used to compare categorical variables. Mann–Whitney U test was used to compare quantitative variables with an abnormal distribution, whereas the Student t-test was used to compare the means of two groups with a normal distribution. Receiver operating characteristic curve (ROC) analysis was conducted for NLR, PLR, and SII to predict mortality in terms of sensitivity and specificity and survival analysis was conducted by the Kaplan–Meier curve.
3. Results
A total of 73 patients admitted with IE were screened and 61 patients satisfied the inclusion criteria. The 11 patients who were dead were taken as the study group, and 50 patients who were discharged alive were taken as the control group. Baseline demographic variables were comparable in both groups except for age and atrial fibrillation. The median age of the population with mortality was higher (65 range 57–77) than patients who survived (57 range 49–66). Atrial fibrillation was seen more commonly in patients who had mortality than those alive. Neutrophil counts were significantly higher, and lymphocyte and platelet counts were significantly lower in patients with adverse outcomes. C reactive protein levels were comparable in both groups, while NLR was higher in patients with mortality than in the control group.
The median value of NLR was 6.17 (3.5–10.7), which was 19.6 (10.1–27) in patients with mortality, while 5.4 (3.2–8.5) in patients who survived (Table 1). The median value of PLR was 156.8 (96.1–197.8), and the SII value was 1317.4 (813–2091), which were comparable in both groups. The area under the ROC curve of NLR (Fig. 1) showed a significant value of 0.83 (95 %CI 0.683–0.982, p = 0.001). When we listed the coordinates of the ROC curve of NLR, 9.81 had maximum sensitivity (81.8%, 95%CI 52.3–94.9) and specificity (80%, 95%CI 67–88.8) with a positive predictive value of 47.4% and negative predictive value of 95.2%. ROC analysis made for SII AUC 0.451 (95% CI 0.241–0.66) and PLR AUC 0.473 (95% CI 0.229–0.716) were not significant. A comparison of the ROC curve for NLR, SIII, and PLR is given in Fig. 1.
Table 1.
Comparison of Laboratory variables in IE patients with mortality and no mortality.
| Variable | Total (N = 61) | Mortality |
p-value* | |
|---|---|---|---|---|
| Yes (n = 11) | No (n = 50) | |||
| Hb (g/dL), median (IQR) | 10.2 (9.3–11.3) | 10.8 (8.9–12.3) | 9.8 (9.3–11.0) | 0.493 |
| CRP (mg/L), median (IQR) | 88.6 (41.3–173.9) | 88.6 (16.2–286.1) | 83.7 (42.3–169.3) | 0.871 |
| Urea (mg/dL), median (IQR) | 32.3 (18.7–55.2) | 103 (37–124) | 25 (17.8–46.3) | 0.001 |
| Serum Creatinine (mg/dL), median (IQR) | 1.1 (0.8–1.7) | 1.5 (1.1–3) | 1 (0.73–1.7) | 0.03 |
| PCV (%), median (IQR) | 30.8 (28.2–34.4) | 33.7 (26.0–35.8) | 30.5 (28.3–33.7) | 0.542 |
| TLC (K/μL), median (IQR) | 11.9 (8.1–15.8) | 11.5 (8.5–19.4) | 12.0 (8.0–15.5) | 0.447 |
| Monocyte count(K/μL), median (IQR) | 0.4 (0.2–0.69) | 0.3 (0.2–0.5) | 0.4 (0.28–0.7) | 0.292 |
| Neutrophil count(K/μL), median (IQR) | 9.3 (6.0–12.9) | 10.4 (8.1–15.5) | 9.2 (5.7–12.3) | 0.119 |
| Lymphocyte count (K/μL), median (IQR) | 1.5 (0.89–2.04) | 0.6 (0.5–1.63) | 1.6 (1.2–2.1) | 0.003 |
| Platelet count(K/μL), median (IQR) | 222.0 (159.0–282.5) | 110 (38–165.0) | 229 (177.2–296.7) | 0.001 |
| NLR, median (IQR) | 6.17 (3.5–10.7) | 19.6 (10.1–27.0) | 5.4 (3.2–8.5) | 0.001 |
| PLR, median (IQR) | 156.8 (96.1–197.8) | 127.9 (62.5–235.7) | 156.9 (102.6–192.5) | 0.778 |
| SII (K/μL), median (IQR) | 1317.4 (813.17–2091.6) | 1112.7 (675.0–3234.0) | 1439.4 (843.9–2043.3) | 0.613 |
NLR, Neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio; SII, systemic immune-inflammation index; IQR, interquartile range; CRP, C reactive protein; TLC, total leukocyte count; Hb, haemoglobin; PCV packed cell volume. *p value is between mortality yes and mortality no.
Fig. 1.
The receiver-operating characteristic curve of NLR, PLR and SII for predicting in-hospital mortality in patients with infective endocarditis.
Twenty patients had undergone surgery which was comparable in both groups. Heart failure, renal failure, sepsis, multiple organ dysfunction syndrome (MODS), and peripheral embolism were significantly higher in patients who died than in alive patients. A Kaplan Meier survival analysis was made for patients taking a cut-off value of NLR 9.8 was statistically significant with a log-rank p-value <0.001 (Fig. 2). On bivariate analysis, age, renal failure, diabetes mellitus (DM), and atrial fibrillation (AF) were associated with in-hospital mortality. In the multivariate analysis, only NLR was a statistically significant predictor of mortality (Table 2).
Fig. 2.
Kaplan–Meier curve for in-hospital mortality according to the cut-off value of Neutrophil lymphocyte ratio in patients with infective endocarditis.
Table 2.
Clinical and laboratory predictors of mortality by univariate and multivariate logistic regression analysis.
| Crude OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
|---|---|---|---|---|
| Age≥55 years | 10 (1.2–84.1) | 0.017 | 7.2 (0.5–106.8) | 0.15 |
| Diabetes mellitus | 3.4 (0.9–13.2) | 0.093 | 1.9 (0.1–28.4) | 0.63 |
| Atrial fibrillation | 9 (1.3–62.6) | 0.037 | 1.1 (0–77.1) | 0.977 |
| Dyspnoea | 3.7 (0.9–15.6) | 0.096 | 2.9 (0.2–33.2) | 0.399 |
| Aortic valve vegetation | 3.4 (0.9–13.1) | 0.081 | 10.3 (0.7–162.3) | 0.096 |
| Platelet count <150 K/μL | 12.8 (2.9–57.3) | 0.001 | 8.4 (0.5–130.2) | 0.128 |
| Serum Creatinine >1.3 mg/dL | 4.1 (1–16.1) | 0.079 | 1.7 (0.1–20.1) | 0.676 |
| NLR Cuff off≥9.81 | 18 (3.3–96.7) | <0.001 | 37.5 (2.1–669.3) | 0.014 |
NLR, Neutrophil-to-lymphocyte ratio; OR, odds ratio.
4. Discussion
Our study focused on different inflammatory indexes and their potential to predict mortality in IE patients. Renal failure, heart failure, septic shock, high creatinine, low platelet count, and high NLR were associated with in-hospital mortality. In addition, high NLR and not PLR or SII at admission is a significant predictor of in-hospital mortality in IE patients.
Various inflammatory markers have been studied in IE to predict adverse outcomes. Turak et al8 evaluated 121 patients with IE retrospectively and showed that elevated NLR (NLR > 7.1) is linked to poor prognosis, in-hospital mortality and embolic events. NLR has a stronger predictive value than a stand-alone leukocyte differential count. Bozbay et al9 investigated 171 patients with IE and found that high NLR group has high mortality but NLR showed no predictive indicator of mortality on long-term follow-up. The study by Meshaal et al4 found that NLR is an independent predictor of in-hospital mortality in IE and calculation of NLR at admission may assist in early risk stratification in patients with IE. The study conducted by Chen et al10 found stronger evidence of NLR as a reliable predictor of in-hospital mortality and morbidity.
The predictive power of SII in Infective endocarditis has been studied by Agus et al and found that SII is an independent predictor of mortality in their cohort and performed better than NLR and PLR in predicting mortality in IE patients.3This was in contrast to our study, as NLR was a better mortality predictor than SII and PLR similar to previously mentioned studies.
Our study's fundamental flaws are its retrospective design and limited sample size. The goal of this study was to see if there was a link between inflammatory levels at admission and in-hospital mortality. However, the findings of this study need to be verified in larger prospective cohorts.
5. Conclusion
The present study shows that a high NLR has better association with in-hospital mortality in IE than SII and PLR. NLR is a simple, readily available, and inexpensive parameter that can be used as a predictive marker to identify high-risk patients for mortality in IE.
Funding
This work was supported by the intramural funding from Aster DM Healthcare Ltd., for the year 2021–2022 (Project No. IMRS012).
Contributory statement
SR: Conceptualization, Methodology, Writing and Editing; MC: Methodology, Analysis, Tables and figures, editing and reviewing; AW: Conceptualization, drafting and reviewing; MN: Reviewing and critical analysis; AK: Supervision, drafting, reviewing and critical analysis.
All authors critically revised the article for its intellectual content. All the authors have critically revised and agreed to the article for its contents before submission.
Ethical approval
The study has been approved by the scientific research committee and institutional ethics committee (Ref. AM/EC/203–2021).
Declaration of competing interest
All authors confirm that they have nothing to declare.
References
- 1.Zencir C., Akpek M., Senol S., et al. Association between hematologic parameters and in-hospital mortality in patients with infective endocarditis. Kaohsiung J Med Sci. 2015;31(12):632–638. doi: 10.1016/j.kjms.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Balta S., Ozturk C. The platelet-lymphocyte ratio: a simple, inexpensive, and rapid prognostic marker for cardiovascular events. Platelets. 2015;26(7):680–681. doi: 10.3109/09537104.2014.979340. [DOI] [PubMed] [Google Scholar]
- 3.Erturk M., Cakmak H.A., Surgit O., et al. Predictive value of elevated neutrophil to lymphocyte ratio for long-term cardiovascular mortality in peripheral arterial occlusive disease. J Cardiol. 2014;64(5):371–376. doi: 10.1016/j.jjcc.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 4.Meshaal M.S., Nagi A., Eldamaty A., et al. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as independent predictors of outcome in infective endocarditis (IE) Egypt Heart J. 2019;71(1):1–8. doi: 10.1186/s43044-019-0014-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li C., Tian W., Zhao F., et al. Systemic immune-inflammation index, SII, for prognosis of elderly patients with newly diagnosed tumors. Oncotarget. 2018;9(82):35293–35299. doi: 10.18632/oncotarget.24293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agus H.Z., Kahraman S., Arslan C., et al. Systemic immune-inflammation index predicts mortality in infective endocarditis. J Saudi Heart Assoc. 2020;32(1):58–64. doi: 10.37616/2212-5043.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu W., Su G., Zhu W., et al. Systemic immune-inflammation index predicts embolic events in infective endocarditis. Int Heart J. 2022;63:510–516. doi: 10.1536/ihj.21-627. [DOI] [PubMed] [Google Scholar]
- 8.Turak O., Özcan F., Işleyen A., et al. Usefulness of neutrophil-to-lymphocyte ratio to predict in-hospital outcomes in infective endocarditis. Can J Cardiol. 2013;29(12):1672–1678. doi: 10.1016/j.cjca.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Bozbay M., Ugur M., Uyarel H., et al. Neutrophil-to-lymphocyte ratio as a prognostic marker in infective endocarditis: in-hospital and long-term clinical results. J Heart Valve Dis. 2014;23(5):617–623. [PubMed] [Google Scholar]
- 10.Chen Y., Ye L.J., Wu Y., et al. Neutrophil-lymphocyte ratio in predicting infective endocarditis: a case-control retrospective study. Mediators Inflamm. 2020;27 doi: 10.1155/2020/8586418. [DOI] [PMC free article] [PubMed] [Google Scholar]