Abstract
Objective
This systematic review aimed to investigate the effect of whole-body vibration (WBV) on balance or proprioception for patients with nonspecific chronic low back pain (NSCLBP).
Methods
A comprehensive search was conducted using 5 databases—PubMed, Web of Science, Cochrane Library, Science Direct, and Physiotherapy Evidence Database—from inception to January 2022. Randomized clinical trials that examined the efficacy of WBV on balance or proprioception in patients with NSCLBP were incorporated. The methodological quality of each included study was assessed using the Physiotherapy Evidence Database scale.
Results
Our search strategy yielded 5309 articles, of which 7 published randomized clinical trials (313 patients) met the inclusion criteria. Three of the 4 included studies that investigated balance reported significant improvements after WBV, of which 2 were of high methodological quality. The remaining 3 studies investigating proprioception also showed significant improvements after WBV intervention.
Conclusion
Although some studies seem to provide promising results regarding the efficacy of WBV or WBV combined with exercise in improving balance and proprioception in patients with NSCLBP, at present, no definite conclusions can be drawn due to article heterogeneity and lack of clinical trials.
Key Indexing Terms: Vibration, Postural Balance, Proprioception, Low Back Pain
Introduction
Chronic low back pain (CLBP) is one of the most expensive musculoskeletal conditions having an estimated lifetime prevalence of 60% to 90%.1 It is reported that CLBP in around 90% to 95% of patients has nonspecific causes.2 Studies have shown that low back pain (LBP) lasting for more than 3 months affects around 15% to 45% of the population and is found to be the most common cause of disability in people aged between 45 and 65 years.3 The chronicity of pain may occur due to multiple factors like psychological, emotional, variability in pain thresholds, and neuroplasticity.4 CLBP also presents with multiple related symptoms like reduced lumbar flexibility,5 poor static balance6 and proprioception,7 decreased overall physical fitness, and health-related quality of life.8
CLBP, presenting with a decreased proprioceptive ability might be attributed to the neuromuscular deficits and altered balance in the activation pattern of agonist and antagonist muscles.7 A decrease in proprioception and motor control impairment may also occur due to long-lasting pain, which can interfere with the proprioception inputs to the brain.9 Thus, pain and proprioception may be interrelated, as an increase in proprioception is seen with a reduction in pain.9 Studies have also shown CLBP being associated with static as well as dynamic balance deficits.10 These deficits are difficult to recover from and may persist even after LBP resolves, thus making patients with CLBP vulnerable to injuries.11
According to most clinical trials, multiple therapeutic approaches like taping, bracing, manual therapy, and balance board exercises have been used to improve balance and proprioception.12,13 Recently increasing in popularity, whole-body vibration (WBV) therapy requires a person to stand with flexed knees and barefoot on a platform and provides mechanical oscillatory movements to the whole body.14 The patient assumes a flexed knee posture to help avoid transmissions to the head during the therapy.14 WBV devices can operate at different frequencies and amplitudes. However, it is known that therapeutic effects are seen at lower frequencies, as they induce muscle relaxation and, thus, help reduce LBP by acting on paravertebral muscles.15 Higher frequencies, on the other hand, lead to adverse effects on the body and may increase the risk of back pain16 and its associated problems.
The efficacy of WBV has been examined in those with cerebral palsy,17 osteoporosis,18 fibromyalgia,19 osteoarthritis,20 stroke,21 obesity,22 and anterior cruciate ligament reconstruction.23 In recent years, studies have examined the effects of this intervention on balance and proprioception in patients with nonspecific chronic low back pain (NSCLBP).24, 25, 26, 27, 28, 29, 30, 31, 32 However, ambiguity persists regarding the efficacy of WBV due to the absence of a standard therapeutic protocol in terms of vibration parameters like frequency, amplitude, and duration. To the best of the authors’ knowledge, no prior systematic reviews have been done regarding the efficacy of WBV on balance or proprioception in patients with NSCLBP. Thus, the objective of this study is to perform a systematic review of existing studies to investigate the efficacy of WBV on balance or proprioception in patients with NSCLBP. We hypothesized that WBV would be an effective therapeutic intervention in improving balance and proprioception in patients with NSCLBP.
Methods
Registration Protocol
Our study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) and can be accessed via registration number CRD42021235873. Due to the nature of the study, ethical approval was not required.
Inclusion Criteria
Our systematic review followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.33 The population, intervention, comparison, outcome, and study design (PICOS) system was incorporated for this review. A study must have met the following inclusion criteria to be selected for our research. (1) Type of population: the study population must consist of all participants with NSCLBP (LBP persisting for at least 3 months) irrespective of their age, sex, and ethnicity. Studies that recruited participants having any specific LBP with known pathology (infection, rheumatoid arthritis, ankylosing spondylitis, tumor, fracture, or metabolic disease) were excluded. (2) Type of intervention: intervention must have WBV therapy in which mechanical oscillatory movements on a platform are provided while the patient stands on the platform with knees flexed to avoid vibrations to the brain. The research trials that examined the effect of WBV in combination with other exercise interventions were also included. (3) Type of comparison: there can be various types of comparison interventions without any particular restriction (eg, sham treatment, traditional exercises, stabilization exercises). Studies comparing the effects of WBV in combination with other types of interventions in patients with NSCLBP were also included. (4) Type of outcomes: studies having balance (postural control, postural equilibrium, body posture, balance control, and postural sway), proprioception, or positional sense as primary or secondary outcome measures were included. (5) Type of study design: only randomized clinical trials (parallel, cross-over, or cluster designs) were included.
However, the studies were excluded if (1) outcome measures did not include balance or proprioception; (2) they were non-English-language texts, abstracts, papers, or conference papers from annual meetings; (3) they were done on animal subjects; and (4) they studied locally applied vibration interventions, seated vibration devices, or stochastic resonance WBV (random vibrations applied while the patient stands on 2 separately oscillating platforms).
Data Sources and Searches
A comprehensive search strategy using 5 databases, namely, PubMed, Web of Science, Cochrane Library, Science Direct, and Physiotherapy Evidence Database (PEDro), was conducted from inception to January 2022. Our search strategy located the articles by using a combination of keywords "whole-body vibration OR whole-body vibration therapy OR whole-body vibration training," "balance OR postural control OR postural equilibrium OR balance control," "proprioception OR position sense," and "non-specific chronic low back pain OR chronic low back pain OR low back pain OR back pain." The search strategy was adapted according to different databases (see Supplementary Data).
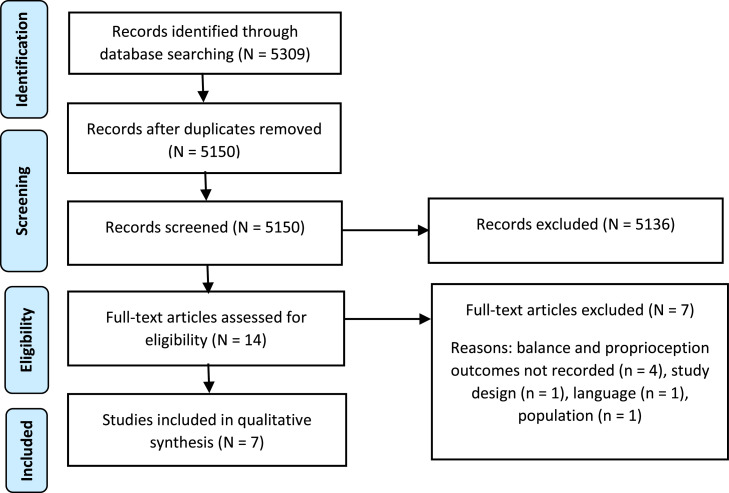
Studies published from inception to January 2022 were included. The process of searching and selecting studies was done independently by 2 researchers (N.T., Z.K.). After exporting all records found on different academic databases to the Mendeley reference manager, the duplicates were removed, and nonrelevant studies were excluded based on the exclusion criteria. The remaining included studies were further screened on the basis of abstract and then closely reviewed for full-text eligibility based on inclusion criteria. Figure 1 shows a flowchart of our search strategy according to PRISMA guidelines.33 Screening strategy was discussed with other independent investigators, and any dispute was settled by discussion.
Fig 1.
Flow diagram for selection of articles based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).33 Systematic screening of articles at different stages of systematic review in which 7 of 5309 articles are selected at the end of our search strategy.
Methodological Quality Assessment
The methodological quality of each included study was conducted using the PEDro scale.34 The total score is calculated up to 11 points. In this, criterion 1 talks about the external validity of the studies, criteria 2 to 9 focus on the internal validity of the trials, and criteria 10 to 11 help to identify whether the studies have enough statistical information to derive interpretable results. The methodological quality increases with the increment in the scores. Rating of the quality is as follows: good quality, 6 to 8; fair quality, 4 to 5; and poor quality, below 4.34
Data Extraction and Analysis
Data were extracted from the selected studies, which included participant characteristics, WBV parameters (type, device, frequency, amplitude, duration), interventions and comparisons, outcome measures, and results. Effect size (Cohen's d) was calculated for post-treatment values of the control group and experimental group to determine significant differences between the groups. Cohen's d is determined as the mean difference of 2 samples divided by the pooled standard deviation. Effect size ≥0.8 was considered to be high, between 0.5 and 0.8 was considered moderate, and effect size <0.5 was regarded as low.35
Results
Search Results
Our comprehensive search resulted in a total of 5309 studies, of which 7 studies were included after thorough screening. Among these 7 included studies, 6 were randomized controlled trials, and 1 was a randomized cross-over trial. Four of the studies compared the efficacy of WBV combined with exercise to exercise alone in patients with NSCLBP. One of the studies examined the effect of WBV compared with no treatment at all. One was the randomized cross-over trial, which examined the immediate effect of WBV, and 1 study compared the effect of 2 types of vibration (horizontal vs vertical) in patients with NSCLBP.
Methodological Quality Assessment of Studies
PEDro criterion of scoring was used to assess the level of evidence of the included studies, as shown in Table 1. Among them, 3 were of good quality,24, 25, 26 3 were fair,27, 28, 29 and 1 of the studies was considered to be of poor-level evidence.30
Table 1.
Methodological Quality of Included Studies
| Study | Physiotherapy Evidence Database Scale |
Final Score | Quality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |||
| del Pozo-Cruz et al, 201124 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | Good |
| Wang et al, 201925 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 | Good |
| Kim et al, 201826 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | Good |
| Yang et al, 201527 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | Fair |
| Wegener et al, 201928 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | Fair |
| Jung et al, 202029 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 5 | Fair |
| Sajadi et al, 201930 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 | Poor |
The Physiotherapy Evidence Database Scale numbers represent the following: (1) eligibility criteria mentioned; (2) random allocation to groups or to treatment order in case of crossover trial; (3) concealed allocation; (4) baseline similarity; (5) blinding of participants; (6) blinding of therapists; (7) blinding of assessors; (8) acceptable follow-up; (9) intention-to-treat analysis; (10) between-group statistics; (11) point measures and measures of variability. “1” represents satisfied criterion and “0” represents unsatisfied criterion. Rating of the quality: good quality, 6-8; fair quality, 4-5; and poor quality, below 4.
Characteristics of Study Sample
The characteristics of included studies are mentioned in Table 2. After the extraction of data, 313 patients (55.2% female, 44.7% male) with NSCLBP were included. The sample size ranged from 24 to 89, with the average age of patients ranging from 18 to 63.9 years. Of all the 7 included studies, 4 studies investigated balance (static balance or postural stability)24,26, 27, 28 and the other 3 studies25,29,30 recorded proprioception as their primary or secondary outcome measures.
Table 2.
Included Studies and Their Characteristics
| Study | Sample Description | Treatment and Comparison | Outcome Measures |
|---|---|---|---|
| del Pozo-Cruz et al, 2011 (randomized controlled trial)24 |
N = 50 (49 followed up for the entire study) patients with NSCLBP (minimum 6 mo of symptoms) Age (y) = 40-70; CG: 59.53 (5.47); WBV group: 58.71 (4.59) BMI = CG: 31.47 (6.41); WBV group: 28.6 (3.84) |
CG: Normal pattern of daily activities were continued for 12 wk. WBV group: WBV was given twice a week with 1-d gap in between the 2 sessions for a total of 12 wk. The participant stood on the platform with knees flexed 120°. |
Postural stability (Biodex balance system; anteroposterior stability index, mediolateral stability index) [0, 12 wk] |
| Wang et al, 2019 (randomized controlled trial)25 |
N = 89 patients with NSCLBP (minimum 3 mo of symptoms) Age (y) = between 18 and 60; CG: 22.02 (4.59); WBV group: 21.64 (3.01) BMI = CG: 21.88 (1.88); WBV group: 22.68 (2.54) |
CG: general exercise program was given. WBV group: exercise program similar to control group was given along with WBV. Both groups had 5-min warm-up followed by 15-min exercise and then 5-min cool down in each session. |
Trunk proprioception (Con-Trex isokinetic dynamometer; joint position sense in flexion and extension) [0, 12 wk] |
| Kim et al, 2018 (randomized controlled trial)26 |
N = 28 patients with NSCLBP (minimum 6 mo of symptoms) Age (y) = HVG: 55.1 ± 11.2; VVG: 53.7 ± 12.1 BMI = NR |
Both HVG and VVG performed exercise for 30 min/d, 3 times a week for overall duration of 12 wk. Both groups had 5-min warm-up, 20-min WBV exercise, and 5-min cool-down session. However, in HVG, horizontal vibrations were given in sagittal axis, and in VVG, vertical vibrations were given in vertical axis. | Standing balance control score (Biodex stability system; anteroposterior stability index, mediolateral stability index) [0, 6, 12, 16 wk] |
| Yang et al, 2015 (randomized controlled trial)27 |
N = 40 patients with NSCLBP (minimum 3 mo of symptoms) Age (y) = CG: 30.95; WBV group: 32.80 BMI = CG: 23.33; WBV group: 24.37 |
CG: lumbar stability training done for 30 min. WBV group: 25 min of lumbar stability training followed by 5 min of WBV. Participant stood with slightly flexed knees and lumbar lordosis on platform. The training in both groups was conducted for 3 times per week for total of 6 wk. |
Static balance (Tetrax; fall index) [0, 6 wk] |
| Wegener et al, 2019 (randomized controlled trial)28 |
N = 65 (33 were followed up for the entire study) patients with nonspecific chronic back pain (minimum 3 mo of symptoms) Age (y) = 61.6 (7.9); CG: 63.9 (6.5); WBV group: 60.9 (8.2) BMI = NR |
CG: classic physiotherapy performed twice a week in 3 blocks of 6 wk each. WBV group: WBV given twice a week in 3 blocks of 6 wk each, in which time and intensity was progressed with each block. Five defined trunk stability exercises were performed by both groups for an overall duration of 18 wk. |
Balance and postural stability (MFT-S3-Check; stability index, sensorimotor index, and symmetry index) [0, 18-24 wk] |
| Jung et al, 2020 (randomized controlled trial)29 |
N = 50 patients with NSCLBP (minimum 3 mo of symptoms) Age (y) = between 10 and 19; CG: 18.04 ± 0.68; WBV group: 18.00 ± 0.65 BMI = NR |
Both WBV and CG performed 5-min warm-up followed by 6 exercises and then 5-min cool down for 25 min/d, 3 times a week for overall duration of 12 wk. In WBV the exercises were performed on the WBV platform, and in CG, without any vibratory platform. Patients stood with knees 30°-45° flexed on the platform. | Trunk proprioception (Dualer IQ digital, repositioning error) [0, 12 wk] |
| Sajadi et al, 2019 (randomized crossover trial)30 |
N = 24 patients with NSCLBP (minimum 3 mo of symptoms) Age (y) = between 20 and 35; 25.2 (2.6) BMI = NR |
Two separate WBV sessions were conducted with a 2-wk washout period in between them. In the first session, half the patients received low-frequency WBV while the other half was given high-frequency WBV. In the second session the order was reversed. Patient stood with 15 flexed knees for five 1-min vibration sets with 1 min rest in between the sets. |
Position sense (Electro goniometer; repositioning error in neutral, 30% and 60% of lumbar flexion) [0, 2 wk] |
Values are represented as mean (standard deviation).
BMI, body mass index; CG, control group; HVG, horizontal vibration group; NR, not reported; NSCLBP, nonspecific chronic low back pain; VVG, vertical vibration group; WBV, whole-body vibration.
WBV Specifications
The WBV device used for intervention in 3 out of 7 studies was Galileo 2000 (Novotec, Pforzheim, Germany) or Galileo plate, and the rest used several different devices (ie, VIB5070, Power Plate Inc, EXXTREAM 1000, and TT2590×7). All the patients stood with flexed knees on the platform to avoid the vibration reaching the head, and some also performed dynamic exercises on the vibrating platform. Frequency in 6 studies was kept low (ie, up to 30 Hz24-29), and in 1 study30 both low- and high-frequency WBV effects were seen in patients. Amplitude was not reported in 4 studies, and the rest used 2 to 5 mm of amplitude. The duration of the overall intervention period was kept at 12 weeks in 4 studies,26, 27, 28,31 and the remaining had kept 6 weeks,29 18 weeks,30 and immediate evaluation32 as their duration. All the studies used vertical vibrations, and only 1 study26 compared horizontal with vertical vibrations to test for better results in patients. WBV specifications and parameters are mentioned in Table 3.
Table 3.
WBV Parameters
| Study | Device | Vibration Type | Frequency (Hz) | Amplitude | Session Duration | Sessions per Week | Total Duration |
|---|---|---|---|---|---|---|---|
| del Pozo-Cruz et al, 201124 | Galileo 2000 | Side-alternating oscillations | 20 | NR | 6-8 min | 2 | 12 wk |
| Wang et al, 201925 |
VIB5070; BODYGREEN, Taiwan | NR | 18 | NR | 15 min | 3 | 12 wk |
| Kim et al, 201826 | HVG: EXXTREAM 1000; AMH International Ltd, Incheon, Korea |
HVG: horizontal vibrations VVG: vertical vibrations |
HVG: 3-5 VVG: 28-34 |
HVG: 1-48 mm VVG: 2.5-5 mm |
20 min | 3 | 12 wk |
| Yang et al, 201527 | Galileo 2000 | NR | 18 | Controlled without restriction | 5 min | 3 | 6 wk |
| Wegener et al, 201928 | Galileo plate (Novotec Medical GmbH, Pforzheim, Germany) | NR | 5-12 12-20 20 |
NR | 1-2 min each of 5 exercises on WBV | 2 | 18 wk |
| Jung et al, 202029 | TT2590×7, TurboSonic Co, Seoul, Korea | NR | 15 | 2 mm | 15 min | 3 | 12 wk |
| Sajadi et al, 201930 | Power Plate Inc, Irvine, California |
NR | High: 50 Low: 30 |
2.5 mm | 5 min | NA | 2 sessions with 2-wk gap in between |
HVG, horizontal vibration group; NA, not applicable; NR, not reported; VVG, vertical vibration group; WBV, whole-body vibration.
Outcome Measures and Their Effects
This review focuses on balance or proprioception as key outcome parameters for assessing the efficacy of WBV. In all the studies, effect size (Cohen's d) was calculated using post-treatment measures of control and experimental groups except in 2 studies where Cohen's d was calculated for pre- and posttreatment values of low-frequency vibration group30 and vertical vibration group.26 This was done to compare the studies on even grounds (Table 4). Balance testing in different studies was performed using various methods. Out of 4 studies24,26, 27, 28 investigating the effects of WBV on balance, 2 studies24, 25, 26 used the Biodex Stability System, which measured the anteroposterior and mediolateral stability index. In contrast, 1 study27 used Tetrax to measure fall index, and 1 study28 MFT-S3-Check, which measured 3 parameters of balance (ie, stability index, sensorimotor index, and symmetry index). Only 1 study30 reported a high effect size in both its balance parameters (1.95; 1.18), and the rest24,27,28 showed low effect size except for mediolateral stability index (0.56) and sensorimotor index in standing (0.5), which fell under moderate effect size. Two studies26,27 found a statistically significant difference in all its parameters of balance (0.000, 0.001; <0.05), and 1 study24 found a statistically significant difference in 1 of its balance parameters (ie, anteroposterior stability index [0.031]). Of the 3 studies that gave statistically significant differences in terms of balance parameters for the WBV group, 2 were of high quality and 1 was regarded as fair.
Table 4.
Outcome Measures
| Study | Outcome Measures | CG Pretreatment | CG Posttreatment | EG Pretreatment | EG Posttreatment | Effect Size (Cohen's d) | P Value |
|---|---|---|---|---|---|---|---|
| del Pozo-Cruz et al, 201124 N = 49 CG = 24 EG = 25 |
Postural stability: Anteroposterior stability index Mediolateral stability index |
0.57 ± 0.40 0.47 ± 0.36 |
0.57 ± 0.40 0.47 ± 0.37 |
0.52 ± 0.22 0.33 ± 0.17 |
0.41 ± 0.95 0.30 ± 0.21 |
0.219518 0.565099 |
.031 .422 |
| Wang et al, 201925 N = 89 CG = 44 EG = 45 |
Trunk proprioception: Joint position sense In flexion In extension |
3.96 (3.22, 4.7) 3.06 (2.37, 3.74) |
3.67 (3.12, 4.21) 2.76 (2.26, 3.26) |
3.55 (2.82, 4.28) 2.96 (2.28, 3.64) |
1.91 (1.36, 2.44) 1.66 (1.17, 2.15) |
-1.14 -0.78 |
.005 .036 |
| Kim et al, 201826 N = 28 HVG =14 VVG =14 |
Standing balance control score: Anteroposterior stability index Mediolateral stability index |
- - |
- - |
VVG: 4.00 ± 0.80 3.89 ± 1.79 |
VVG: 2.52 ± 0.71 2.25 ± 0.79 |
1.956792 1.185391 |
.000 .001 |
| Yang et al, 201527 N = 40 CG = 20 EG = 20 |
Static balance: Fall index |
23.40 ± 12.73 |
21.69 ± 12.68 |
30.59 ± 14.97 |
21.80 ± 10.39 |
0.00949 |
<.05 |
| Wegener et al, 201928 N = 33 CG = 16 EG = 17 |
Balance and postural stability: STI in standing STI in sitting SMI in standing SMI in sitting SI in standing (left) SI in standing (right) SI in sitting (left) SI in sitting (right) |
5.6 ± 1.5 4.9 ± 2.9 5.0 ± 1.5 4.1 ± 2.7 50.7 ± 7.5 49.3 ± 7.5 44.5 ± 15.1 55.5 ± 15.1 |
4.8 ± 1.4 2.6 ± 2.3 4.0 ± 1.2 2.0 ± 1.8 49.3 ± 10.3 50.8 ± 10.3 45.9 ± 17.5 54.1 ± 17.5 |
5.0 ± 1.0 3.9 ± 2.1 4.0 ± 1.2 2.9 ± 1.9 47.8 ± 13.0 52.2 ± 13.0 51.7 ± 22.0 48.3 ± 22.0 |
4.4 ± 1.1 2.9 ± 2.4 3.4 ± 1.2 2.0 ± 1.6 52.2 ± 14.4 47.8 ± 14.4 48.3 ± 21.9 51.7 ± 21.9 |
0.317721 0.127631 0.5 0 0.231648 0.239636 0.121075 0.121075 |
.885 .51 .493 .217 .718 .718 .773 .773 |
| Jung et al, 202029 N = 50 CG = 25 EG = 25 |
Trunk proprioception: Repositioning error |
2.80 ± 1.00 |
2.16 ± 0.99 |
2.72 ± 0.79 |
1.40 ± 0.58 |
0.936738 |
1.20 |
| Sajadi et al, 201930 (randomized crossover trial) N = 24 |
Position sense: Repositioning error In neutral In 30% of lumbar flexion In 60% of lumbar flexion |
- - - |
- - - |
LFG: -2.91 (.57) 13.6 (1.97) 29.7 (3.97) |
LFG: -1.47 (.88) 14.6 (1.47) 28.48 (2.78) |
1.942314 0.57535 0.355992 |
<.001 .05 .004 |
All values extracted are in the form of mean (standard deviation) or mean (95% confidence interval). P values <.05 are considered statistically significant.
CG, control group; EG, experimental group; HFG, high-frequency group; HVG, horizontal vibration group; LFG, low-frequency group; SI, symmetry index; SMI, sensorimotor index; STI, stability index; VVG, vertical vibration group.
The effects of WBV on proprioception were evaluated in 3 of the 7 included studies by different instruments. These studies measured proprioception in the form of repositioning errors at different angles of trunk flexion and extension. Two studies25,29 showed high effect size (-1.14, -0.78; 0.93), and 1 study30 showed high effect size (1.94) in neutral position, moderate (0.57) and low (0.35) effect size in 30% and 60% of lumbar flexion, respectively. Two recent studies25,30 conducted in 2019, where 1 was of good and the other poor methodological quality, showed statistically significant differences (0.005, 0.036; <0.001, 0.05, 0.004) in proprioception after WBV intervention.
Discussion
In the present review, all 3 studies evaluating proprioception reported a significant improvement in the WBV group compared with the controlled condition despite their differing assessment methods. All the studies used an active repositioning test during the evaluation, which may also account for the uniformity of results concerning the positive effects seen in the WBV group. Compared with passive repositioning, active repositioning has a much more significant role in activating muscle receptors.36 WBV enhances muscular activity, leading to increased muscle mechanoreceptor activity and thus improves repositioning accuracy while assessing proprioception actively.36 All 3 studies, however, studied the effects on the younger age group; therefore, the results cannot be generalized to the older age group. Two of the studies25,29 followed a similar protocol of 12-week intervention in which WBV was integrated with exercises and performed for a 15-minute duration with 5 minutes of warm up and cool down. One of the studies,30 however, was a cross-over trial where immediate effects of WBV on proprioception were assessed in different angles of lumbar flexion. With regard to WBV parameters, a low frequency was used in 2 of the studies, and for the cross-over trial, the pre- and postintervention results of only the low-frequency group (ranging up to 30 Hz) were analyzed. An amplitude of 2 to 2.5 mm was used in 2 studies, and 1 study did not report the magnitude. The other parameters like orientation, exercises, posture, and the device used were not uniform. Also, it was noted that the sample population of all 3 had baseline pain intensity within the low to moderate range. Low pain levels may also be associated with better proprioceptive outcomes, as claimed by previous studies that a sensory competition occurs between chronic pain and proprioceptive inputs at the higher centers.9 Therefore, the efficacy of WBV on intense LBP could not be established.
With regard to the balance outcome, not much data was available to confirm a positive effect. Out of 4 studies, 1 study28 reported improvement in the WBV group but not significant enough and could establish no superiority of WBV over classical physiotherapy. In contrast, 2 studies24,26 that used a similar assessment tool to measure balance (Biodex Stability System) reported significant improvement in anteroposterior stability index, and 1 study26 showed improvement in mediolateral stability index as well in the WBV group. Yang et al27 also reported more significant improvements in the WBV group compared with the control group in terms of fall index. The negative findings of Wegener et al28 in comparison with other studies may be attributed to the increased proportion of depressive symptoms seen in its chronic back pain patients and also might be due to different vibration intensity protocols used. The superiority of WBV could not be confirmed due to incomparable protocols used in the groups. The positive effects of WBV training on balance may have occurred due to diminished reaction time of postural muscles and motor unit recruitment thresholds by enhancing muscle spindle sensibility and excitability.37 Of all the 3 studies showing a positive effect on balance, 2 were of good methodological quality and 1 was regarded as fair.
Considering variable patient characteristics in terms of age and body mass index and wide variations in WBV parameters like frequency (5-34 Hz), amplitude, and duration (6-18 weeks), it is not possible to generalize the results to larger populations. Thus, due to different protocols and data heterogeneity, more studies are required to give a conclusive result regarding the impact of WBV on balance and proprioception in NSCLBP.
Correlating With Other Studies
During our thorough search of databases, we came across 1 systematic review published in 2020,38 which evaluated the efficacy of WBV in NSCLBP. However, the outcome parameters assessed (pain and functional ability) in that systematic review differed from our study (balance and proprioception). The effects of WBV have also been reported in the form of systematic reviews and meta-analyses in recent years but in different populations like ACL reconstruction,39 Parkinson disease,40 postmenopausal women,41 older adults,42 peripheral neuropathy,43 stroke,44 and chronic obstructive pulmonary disease.45 The majority of these reviews used the PEDro scale to assess the methodological quality and rated most of their studies from fair to good. Our study also included articles of fair to good quality; however, one of the trials included had a poor methodological quality, but we found its results relevant for this review.
Our study extensively investigated all the parameters involved in WBV training. From assessing all the retrieved articles, much heterogeneity was found among participant characteristics, assessment methods, and WBV parameters (frequency, amplitude, device, duration); thus, a meta-analysis could not be performed from the pooled data. Although heterogeneity was found, data were not excluded because outcome measures are found to interest readers and practitioners.
Limited work is available on therapeutic WBV regarding LBP, but many research trials have been done to study occupational exposure to WBV leading to LBP. Studies show that WBV can have negative as well as positive impacts depending on the duration of application. A systematic review of 2015 depicts that WBV escalates LBP and sciatic symptoms.16 Thus, there is a need to define a standard WBV protocol to differentiate the negative and positive results and for the proper application of WBV in clinical setups.
Strengths and Limitations
In this systematic review, 5 internationally esteemed databases were searched thoroughly, and any disagreement was settled by discussion. Two independent researchers evaluated the methodological quality of studies using the PEDro scale. PRISMA guidelines were followed and PROSPERO registration was done to ensure authenticity. The use of aforementioned methodology contributed to reducing the risk of bias.
However, due to the lack of trials, our study could only assess the effects of WBV on static balance and not on dynamic balance. We were also unable to carry meta-analysis out of the pooled data owing to heterogeneity and the methodological quality of the studies included. Our study lacked the ability to carry out subgroup analyses due to inadequate research trials. Lastly, an exaggeration of the reported results might have occurred due to a lack of blinding of participants and therapists. Thus, the conclusions are still hazy regarding its clinical application in NSCLBP.
Recommendations for Future Studies
More studies are required on the efficacy of WBV, focusing on balance and proprioception as the outcome measures. Future studies should also investigate the effectiveness of WBV on balance under dynamic conditions. Kim et al26 reported improvement after both horizontal and vertical vibration and found no significant difference between their results; thus, studies focusing on the application of horizontal vibrations as a therapeutic intervention should also come up. Furthermore, there is a need for better-designed, long-term, follow-up trials to form a clear view of the effects of different parameters of WBV on balance and proprioception in patients with NSCLBP. More high-quality studies with a larger sample size are needed to form a standard WBV protocol and to establish a clear perspective regarding the efficacy of WBV in comparison with other interventions (general exercises and stability training).
Conclusion
The included studies provide promising results regarding the efficacy of WBV or WBV combined with exercise in improving balance and proprioception in patients with NSCLBP. However, at present, no definite conclusions can be made due to the heterogeneity and lack of clinical trials.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jcm.2023.04.006.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): N.T.
Design (planned the methods to generate the results): N.T.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): Z.K., Z.V.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): N.T., Z.K.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): N.T., Z.K.
Literature search (performed the literature search): N.T.
Writing (responsible for writing a substantive part of the manuscript): N.T.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): Z.K., Z.V.
Practical Applications.
-
•
This review investigated the effect of whole-body vibration on balance or proprioception for patients with nonspecific chronic low back pain.
-
•
Three of the studies reported significant improvements after whole-body vibration.
-
•
Three studies investigated proprioception and showed significant improvements after whole-body vibration intervention.
-
•
Although some studies seem to provide promising results, no definite conclusions can be drawn due to article heterogeneity and lack of clinical trials.
Alt-text: Unlabelled box
Appendix. Supplementary materials
References
- 1.Bell JA, Burnett A. Exercise for the primary, secondary and tertiary prevention of low back pain in the workplace: a systematic review. J Occup Rehabil. 2009;19(1):8–24. doi: 10.1007/s10926-009-9164-5. [DOI] [PubMed] [Google Scholar]
- 2.Bardin LD, King P, Maher CG. Diagnostic triage for low back pain: a practical approach for primary care. Med J Aust. 2017;206:268–273. doi: 10.5694/mja16.00828. [DOI] [PubMed] [Google Scholar]
- 3.Lione KA. Risk factors for chronic low back pain. J Community Med Health Educ. 2013;4(2) [Google Scholar]
- 4.Alleva J, Hudgins T, Belous J, Kristin OA. Chronic low back pain. Dis Mon. 2016;62(9):330–333. doi: 10.1016/j.disamonth.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 5.Shirado O, Ito T, Kaneda K, Strax TE. Flexion-relaxation phenomenon in the back muscles. A comparative study between healthy subjects and patients with chronic low back pain. Am J Phys Med Rehabil. 1995;74(2):139–144. [PubMed] [Google Scholar]
- 6.Alexander KM, LaPier TL. Differences in static balance and weight distribution between normal subjects and subjects with chronic unilateral low back pain. J Orthop Sports Phys Ther. 1998;28(6):378–383. doi: 10.2519/jospt.1998.28.6.378. [DOI] [PubMed] [Google Scholar]
- 7.Gill KP, Callaghan MJ. The measurement of lumbar proprioception in individuals with and without low back pain. Spine. 1998;23(3):371–377. doi: 10.1097/00007632-199802010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Rehn B, Lidstrom J, Skoglund J, Lindstrom B. Effects on leg muscular performance from whole-body vibration exercise: a systematic review. Scand J Med Sci Sports. 2007;17(1):2–11. doi: 10.1111/j.1600-0838.2006.00578.x. [DOI] [PubMed] [Google Scholar]
- 9.Lederman E. Elsevier Health Sciences; 2005. The Science & Practice of Manual Therapy. [Google Scholar]
- 10.Tsigkanos C, Gaskell L, Smirniotou A, Tsigkanos G. Static and dynamic balance deficiencies in chronic low back pain. J Back Musculoskelet Rehabil. 2016;29(4):887–893. doi: 10.3233/BMR-160721. [DOI] [PubMed] [Google Scholar]
- 11.Bouche K, Stevens V, Cambier D, Caemaert J, Danneels L. Comparison of postural control in unilateral stance between healthy controls and lumbar discectomy patients with and without pain. Eur Spine J. 2006;15(4):423–432. doi: 10.1007/s00586-005-1013-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark NC, Röijezon U, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 2: clinical assessment and intervention. Man Ther. 2015;20(3):378–387. doi: 10.1016/j.math.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Arienti C, Lazzarini SG, Pollock A, Negrini S. Rehabilitation interventions for improving balance following stroke: an overview of systematic reviews. PLoS One. 2019;14(7) doi: 10.1371/journal.pone.0219781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cochrane DJ, Stannard SR, Firth EC, Rittweger J. Acute whole-body vibration elicits post-activation potentiation. Eur J Appl Physiol. 2010;108(2):311–319. doi: 10.1007/s00421-009-1215-2. [DOI] [PubMed] [Google Scholar]
- 15.Rittweger J, Mutschelknauss M, Felsenberg D. Acute changes in neuromuscular excitability after exhaustive whole body vibration exercise as compared to exhaustion by squatting exercise. Clin Physiol Funct Imaging. 2003;23(2):81–86. doi: 10.1046/j.1475-097x.2003.00473.x. [DOI] [PubMed] [Google Scholar]
- 16.Burström L, Nilsson T, Wahlström J. Whole-body vibration and the risk of low back pain and sciatica: a systematic review and meta-analysis. Int Arch Occup Environ Health. 2015;88(4):403–418. doi: 10.1007/s00420-014-0971-4. [DOI] [PubMed] [Google Scholar]
- 17.Saquetto M, Carvalho V, Silva C, Conceicao C, Gomes-Neto M. The effects of whole body vibration on mobility and balance in children with cerebral palsy: a systematic review with meta-analysis. J Musculoskelet Neuronal Interact. 2015;15(2):137–144. [PMC free article] [PubMed] [Google Scholar]
- 18.Bouchard C. Prevention of falls, prevention of osteoporosis, or both: what is the best strategy for preventing fractures in older women? Menopause. 2013;20(10):995–996. doi: 10.1097/GME.0b013e3182a49d90. [DOI] [PubMed] [Google Scholar]
- 19.Collado-Mateo D, Adsuar JC, Olivares PR, et al. Effects of whole-body vibration therapy in patients with fibromyalgia: a systematic literature review. Evid Based Complement Alternat Med. 2015;2015 doi: 10.1155/2015/719082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salmon JR, Roper JA, Tillman MD. Does acute whole-body vibration training improve the physical performance of people with knee osteoarthritis? J Strength Cond Res. 2012;26(11):2983–2989. doi: 10.1519/JSC.0b013e318242a4be. [DOI] [PubMed] [Google Scholar]
- 21.Celletti C, Suppa A, Bianchini E, et al. Promoting post-stroke recovery through focal or whole body vibration: criticisms and prospects from a narrative review. Neurol Sci. 2020;41(1):11–24. doi: 10.1007/s10072-019-04047-3. [DOI] [PubMed] [Google Scholar]
- 22.Zago M, Capodaglio P, Ferrario C, Tarabini M, Galli M. Whole-body vibration training in obese subjects: a systematic review. PLoS One. 2018;13(9) doi: 10.1371/journal.pone.0202866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qiu J, Ong MT, Leong HT, He X, Sc Fu, Yung PS. Effects of whole-body vibration therapy on quadriceps function in patients with anterior cruciate ligament reconstruction: a systematic review. Sports Health. 2022;14(2):216–226. doi: 10.1177/19417381211004937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.del Pozo-Cruz B, Hernández Mocholí MA, Adsuar JC, Parraca JA, Muro I, Gusi N. Effects of whole body vibration therapy on main outcome measures for chronic non-specific low back pain: a single-blind randomized controlled trial. J Rehabil Med. 2011;43(8):689–694. doi: 10.2340/16501977-0830. [DOI] [PubMed] [Google Scholar]
- 25.Wang X-Q, Gu W, Chen B-L, et al. Effects of whole-body vibration exercise for non-specific chronic low back pain: an assessor-blind, randomized controlled trial. Clin Rehabil. 2019;33(9):1445–1457. doi: 10.1177/0269215519848076. [DOI] [PubMed] [Google Scholar]
- 26.Kim H, Kwon BS, Park J-W, et al. Effect of whole body horizontal vibration exercise in chronic low back pain patients: vertical versus horizontal vibration exercise. Ann Rehabil Med. 2018;42(6):804–813. doi: 10.5535/arm.2018.42.6.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang J, Seo D. The effects of whole body vibration on static balance, spinal curvature, pain, and disability of patients with low back pain. J Phys Ther Sci. 2015;27(3):805–808. doi: 10.1589/jpts.27.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wegener V, Rarack S, Tiffe T, et al. Effects of whole body vibration therapy and classic physiotherapy on postural stability in people with back pain: a randomized trial. Clin Spine Surg. 2019;32(4):E214–E220. doi: 10.1097/BSD.0000000000000777. [DOI] [PubMed] [Google Scholar]
- 29.Jung K-S, Jung J-H, In T-S, Cho HY. The effectiveness of trunk stabilization exercise combined with vibration for adolescent patients with non-specific low back pain. Int J Environ Res Public Health. 2020;17(19) doi: 10.3390/ijerph17197024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sajadi N, Bagheri R, Amiri A, Maroufi N, Shadmehr A, Pourahmadi M. Effects of different frequencies of whole body vibration on repositioning error in patients with chronic low back pain in different angles of lumbar flexion. J Manipulative Physiol Ther. 2019;42(4):227–236. doi: 10.1016/j.jmpt.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Zheng YL, Wang XF, Chen BL, et al. Effect of 12-week whole-body vibration exercise on lumbopelvic proprioception and pain control in young adults with nonspecific low back pain. Med Sci Monit. 2019;25:443–452. doi: 10.12659/MSM.912047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hojjati Shargh M, Aminian-Far A, Mirmohammadkhani M. Immediate effect of whole body vibration on trunk proprioception in non-specific chronic low back pain. Koomesh. 2020;22(2):282–290. [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG, Group PRISMA. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–133. doi: 10.1016/s0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 35.Cohen J. Routledge Academic; New York, NY: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 36.Proske U, Wise AK, Gregory JE. The role of muscle receptors in the detection of movements. Prog Neurobiol. 2000;60(1):85–96. doi: 10.1016/s0301-0082(99)00022-2. [DOI] [PubMed] [Google Scholar]
- 37.Pollock RD, Woledge RC, Martin FC, Newham DJ. Effects of whole body vibration on motor unit recruitment and threshold. J Appl Physiol. 2012;112(3):388–395. doi: 10.1152/japplphysiol.01223.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang W, Wang S, Lin W, Li X, Andersen LL, Wang Y. Efficacy of whole body vibration therapy on pain and functional ability in people with non-specific low back pain: a systematic review. BMC Complement Med Ther. 2020;20(1):158. doi: 10.1186/s12906-020-02948-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seixas A, Sañudo B, Sá-Caputo D, Taiar R, Bernardo-Filho M. Whole-body vibration for individuals with reconstructed anterior cruciate ligament: a systematic review. Biomed Res Int. 2020;2020 doi: 10.1155/2020/7362069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dincher A, Schwarz M, Wydra G. Analysis of the effects of whole-body vibration in parkinson disease – systematic review and meta-analysis. PM R. 2019;11(6):640–653. doi: 10.1002/pmrj.12094. [DOI] [PubMed] [Google Scholar]
- 41.Rahimi GRM, Smart NA, Liang MTC, et al. The impact of different modes of exercise training on bone mineral density in older post-menopausal women: a systematic review and meta-analysis research. Calcif Tissue Int. 2020;106(6):577–590. doi: 10.1007/s00223-020-00671-w. [DOI] [PubMed] [Google Scholar]
- 42.Alvarez-Barbosa F, Del Pozo-Cruz J, Del Pozo-Cruz B, Garcia-Hermoso A, RM Alfonso-Rosa. Effects of whole-body vibration on functional mobility, balance, gait strength, and quality of life in institutionalized older people: a systematic review and meta-analysis of randomized controlled trials. J Aging Phys Act. 2020;28(2):219–230. doi: 10.1123/japa.2019-0070. [DOI] [PubMed] [Google Scholar]
- 43.Dixit S, Gular K, Asiri F. Effect of diverse physical rehabilitative interventions on static postural control in diabetic peripheral neuropathy: a systematic review. Physiother Theory Pract. 2020;36(6):679–690. doi: 10.1080/09593985.2018.1491078. [DOI] [PubMed] [Google Scholar]
- 44.Yang F, Butler AJ. Efficacy of controlled whole-body vibration training on improving fall risk factors in stroke survivors: a meta-analysis. Neurorehabil Neural Repair. 2020;34(4):275–288. doi: 10.1177/1545968320907073. [DOI] [PubMed] [Google Scholar]
- 45.Dobler CC, Morrow AS, Farah MH, et al. Nonpharmacologic therapies in patients with exacerbation of chronic obstructive pulmonary disease: a systematic review with meta-analysis. Mayo Clin Proc. 2020;95(6):1169–1183. doi: 10.1016/j.mayocp.2020.01.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.