Abstract
We report a case of patient with a single-chamber Hisian pacemaker who developed complete atrioventricular block and significant deterioration of the ventricular threshold and sensing after transcatheter aortic valve replacement. Revision of the implantation was required, with ventricular lead extraction and replacement.
Key Words: aortic stenosis, atrioventricular block, computed tomography, Hisian pacemaker, transcatheter aortic valve implantation, transcatheter heart valve, virtual basal ring
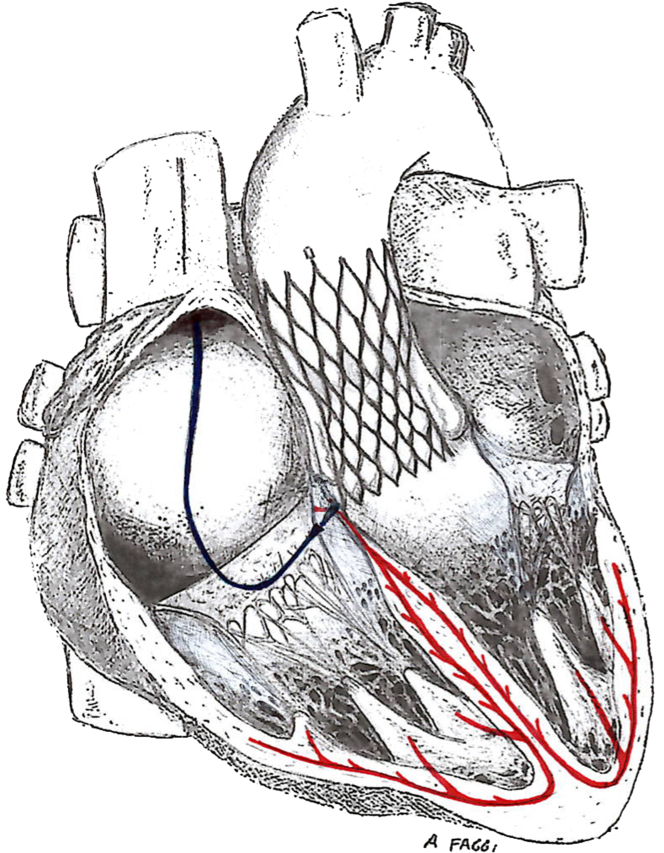
Graphical abstract
History of Presentation
An 81-year-old man was referred to our valve center due to fatigue for common physical activities, worsening dyspnea (NYHA functional class II to III) and over the last months until acute decompensation requiring admission due to heart failure. A systolic heart murmur (grade 4 of 6) was heard in all heart fields. Physical examinations revealed hemoglobin 13.5 g/dL, HT 40,6%, white blood cell count 9.2 × 109 cells/L, platelet count 224 × 109 cells/L, creatinine 0.88 mg/dL, urea 42 mg/dL, no liver function exam alterations.
Learning Objectives
-
•
To recognize the risk of His bundle lead implantation in a patient affected by aortic stenosis with TAVR indication.
-
•
To be able to calculate the best distance from the His bundle lead for the safest TAVR implantation with multimodality imaging.
-
•
To recommend monitoring every Hisian cardiac device carrier before and after TAVR.
Past Medical History
The patient had a previous history of 3-vessel coronary artery bypass grafting and recent (2 months) single-chamber His bundle pacemaker (PM) implantation due to bradycardia in permanent atrial fibrillation previous stroke with cognitive impairment, carotid endarterectomy, bilateral aortofemoral bypass, and stenting of the right common femoral artery.
Investigations
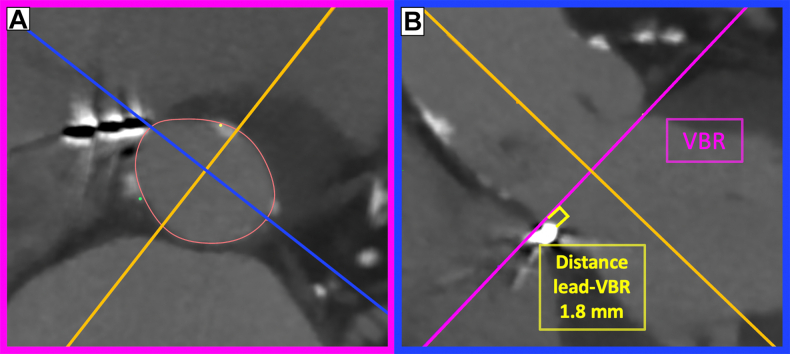
The transthoracic echocardiogram (TTE) showed tricuspid aortic valve stenosis (mean pressure gradient 26 mm Hg, indexed aortic valve area 0.6 cm2/m2, stroke volume 39 mL/m2, ejection fraction 53%) with associated moderate regurgitation and pulmonary hypertension (systolic pulmonary artery pressure 50 mm Hg). Computed tomography revealed a 0.94-cm2 aortic valve area with severe calcific burden, coronary artery bypass grafting patency, and favorable femoral route for TAVR. The calculated virtual basal ring (VBR) area was 583 mm2, with a perimeter of 87 mm. Of note, the PM lead was found pointing sharply into the septum <2 mm below the VBR (Figure 1).
Figure 1.
Pre–Transcatheter Aortic Valve Replacement Computed Tomography
(A) Axial view of the aortic valve virtual basal ring (VBR). The Hisian lead can be observed already at this level between the right and noncoronary cusps. (B) The long axis of the left ventricular outflow tract at the level of contact of the pacemaker into the septum. The pink line is the aortic valve VBR. The distance between the VBR and the pacemaker is 1.8 mm (yellow line).
Management
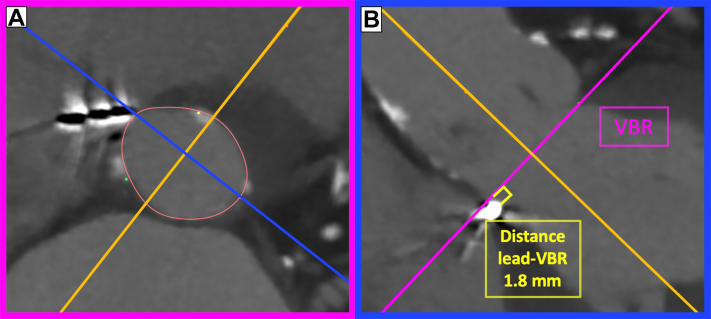
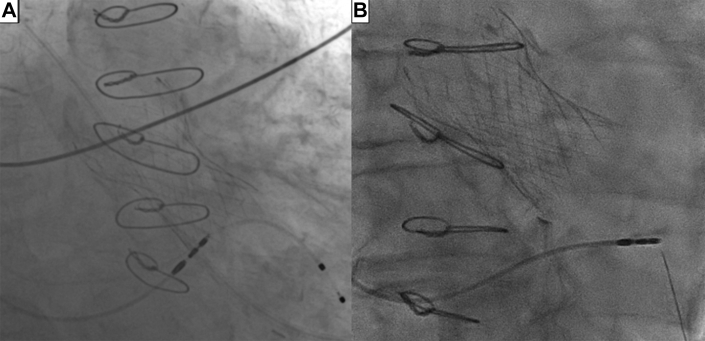
Following heart team discussion, the patient was submitted to TAVR considering the age and the high surgical risk. Given the possible transcatheter heart valve (THV) interference with the Hisian PM,1 a jugular temporary pacing lead was placed into the right ventricle. Based on the VBR size and with the purpose to avoid balloon-induced high radial force pressures on the septum and the lead, direct self-expandable CoreValve Evolut R 34 (Medtronic) implantation was chosen. High implantation technique starting with the Hat marker in the midsection of the pigtail in caudal-right-anterior oblique projection was attempted to try to achieve the highest possible implantation and avoid the Hisian PM (Figure 2, Video 1). Unfortunately, no adequate balance could be found between the position higher than the PM but below the VBR to avoid the risk of embolization, and the decision was taken to implant “low” at the level of the PM (Figures 3A and 4, Video 2). Postdilatation with a 28 mm semicompliant balloon was also required to achieve proper stent expansion and sealing, with final mild residual aortic regurgitation and mean pressure gradient of 3 mm Hg (Video 3). The procedural course was uneventful, and neither bradycardia nor PM malfunction was apparent, but the temporary lead was maintained for safety. After the procedure, PM interrogation was performed, showing a lead malfunction (Figure 5): a steep decreasing in bipolar sensing amplitude and contemporary threshold elevation (bipolar 3 V at 1 ms). The baseline threshold was 1.4 V at 0.4 ms. Lead impedance was stable. PM output was elevated to 7.5 V at 1 ms and intensive electrocardiogram monitoring was established. Five days after the procedure,2 electrical parameters had not recovered; the lead was extracted and a new lead was implanted distally on the interventricular septum (Figures 3B and 6). Of notice, a great part of the proximal third of the septum had unsatisfactory electrical values, probably related to prothesis interference.
Figure 2.
3 Cusp View
Comparison between (A) pre-TAVR computed tomography and (B) the same projection at 3-cusp intraprocedural fluoroscopy.
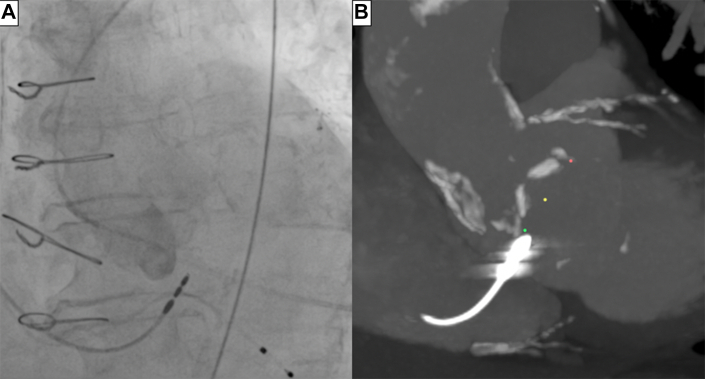
Figure 3.
Hisian Lead and THV Relationships
Fluoroscopic anteroposterior views after transcatheter aortic valve replacement. (A) The transcatheter heart valve stent extends below the pacemaker lead. (B) After extraction of the pacemaker, the near lead is implanted far distally in the septum well below the transcatheter heart valve.
Figure 4.
Hisian Lead and Electrical Conduction System
Drawing representation of the contact between the transcatheter aortic valve replacement valve, His lead (blue), and electrical conduction (red).
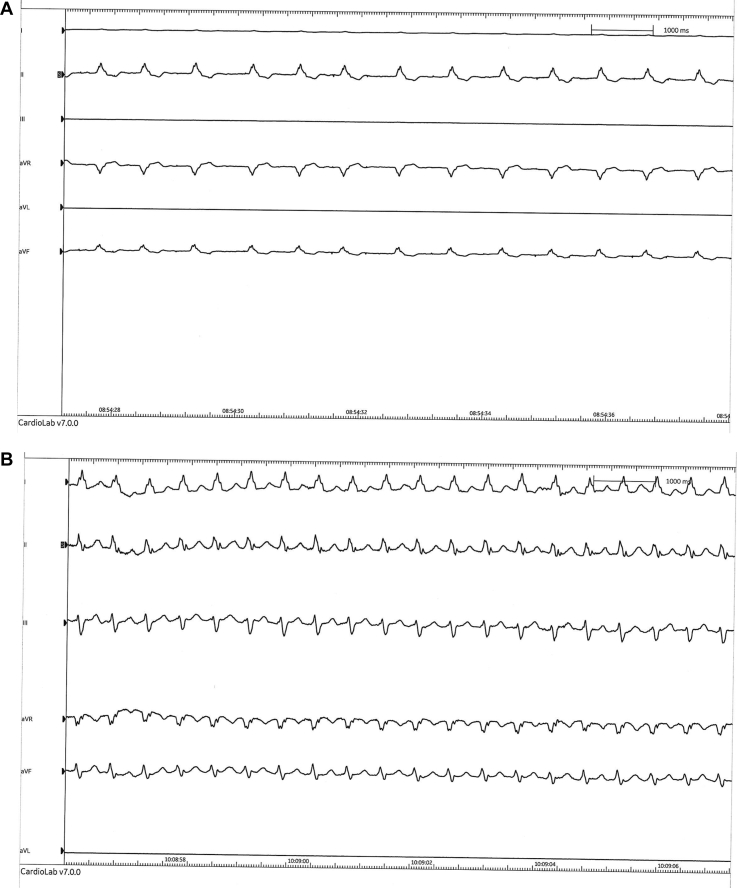
Figure 5.
ECG Pre- and Post-PM Replacement
(A) Electrocardiogram pre–pacemaker replacement. (B) Electrocardiogram post–pacemaker replacement.
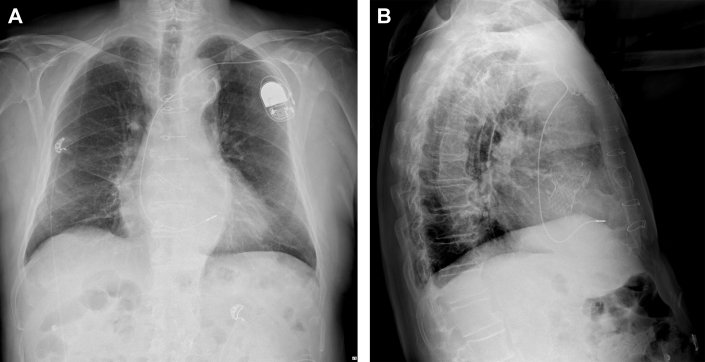
Figure 6.
Final Thoracic X-Ray
(A) Thoracic x-ray film before discharge in anteroposterior view. (B) X-ray film in lateral view.
Discussion
Hisian leads are increasingly used in clinical practice because they allow more physiological and effective conduction of the electric impulse through the ventricles.3 However, their intrinsic position in close anatomical proximity to the subaortic THV landing zone makes them at increased risk of PM malfunction after TAVR. Because TAVR incidence is already high and it will greatly grow in the future, the need to perform TAVR in patients with a His bundle PM will also increase. This currently represents a largely unknown setting, and no data are currently available about its incidence and its best management. The present case offers the opportunity to discuss several aspects:
-
1.
Before TAVR, it is advisable to interrogate a Hisian PM to establish a “baseline” for every electrical parameters.
-
2.
Computed tomography is precious to assess the distance between the VBR and the PM before the procedure. The present case emphasizes that such distance can be so short (1.8 mm) that it becomes impossible to implant the THV safely above the PM and completely avoid it. Indeed, THV implantation that is too high may increase the risk of device embolization. Further experience and CT analysis will be needed to discover how frequently Hisian leads are in such close proximity to the VBR.
-
3.
The His bundle lead consists of a hard metal end that enters the septum with various degrees of angulation. Theoretically, this may warrant some caution when inflating high-pressure balloons in the left ventricular outflow tract due to 2 separate risks (interference/malpositioning/damage of the lead and creation of a ventricular septal defect).3,4 In this case a postdilatation was needed and we cannot be sure of what caused the lead malfunction (THV implantation/balloon inflation). More cases will be needed to clarify the matter.
-
4.
A jugular venous temporary PM is suggested to protect from possible bradyarrhythmic events during the first days after TAVR.3
-
5.
Every Hisian cardiac device carrier should be monitored after TAVR.
-
6.
If a patient is known to be affected by aortic stenosis, the choice between implanting Hisian or a conventional ventricular PM should be carefully considered. If Hisian lead implantation is performed, it should be done as low-far away from the aortic VBR-as possible.
Follow-Up
One year after the intervention, the patient was still alive without severe, persistent heart symptoms and signs: he experiences dyspnea for mild-moderate exercises (NYHA functional class II), no angina, no palpitations, and no ankle swelling. The last PM controls (6 and 12 months from discharge) showed a correct functioning of lead, and the TTE at 1 year confirmed good bioprosthesis functioning (maximum speed 1.98 m/s, mean gradient 8 mmHg, peak of gradient 16 mmHg), with mild regurgitation linked to small anterior and posterior paravalvular leaks and with preserved biventricular motility and function.
Conclusions
Both Hisian PM and TAVR are increasingly common in current clinical practice. Their close anatomical proximity justifies possible PM malfunction following TAVR. To date, no large data are available regarding the proportion of the problem nor its management. Further experience is needed to better understand the anatomical characteristic and the best approach for these patients.
Funding Support and Author Disclosures
Dr Denti has received speaker honoraria from Abbott and Edwards; and served as a consultant for InnovHeart, PiCardia, HRV, and Approxima. Dr Maisano has received grant and/or research institutional support from Abbott, Medtronic, Edwards Lifesciences, Biotronik, Boston Scientific Corporation, NVT, Terumo, and Venus; has received consulting fees and personal and institutional honoraria from Abbott, Medtronic, Edwards Lifesciences, Xeltis, Cardiovalve, Occlufit, Simulands, Mtex, Venus, and Squadra; has received royalty income from and owns IP rights in Edwards Lifesciences; and is a shareholder (including share options) of Cardiogard, Cardiovalve, Magenta, SwissVortex, Transseptalsolutions, 4Tech, and Perifect. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
First THV high implantation attempt in LAO-CAU fluoroscopic view, not accepted due to risk of device embolization.
Second THV implantation attempt in LAO-CAU fluoroscopic view.
Final THV deployment lower into the LVOT at the level of the PM, in LAO-CRA fluoroscopic view.
References
- 1.Mangieri A., Montalto C., Pagnesi M., et al. TAVI and post procedural cardiac conduction abnormalities. Front Cardiovasc Med. 2018;5:85. doi: 10.3389/fcvm.2018.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ng L., Nair R.K., Ali F.M., Pasupati S. Dependence on permanent pacemakers inserted after transcatheter aortic valve implantation: predictive factors in a ten-year retrospective analysis. AsiaIntervention. 2021;7(2):98–102. doi: 10.4244/AIJ-D-21-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vijayaraman P., Dandamudi G., Zanon F., et al. Permanent His bundle pacing: recommendations from a Multicenter His Bundle Pacing Collaborative Working Group for standardization of definitions, implant measurements, and follow-up. Heart Rhythm. 2018;15(3):460–468. doi: 10.1016/j.hrthm.2017.10.039. [DOI] [PubMed] [Google Scholar]
- 4.MacCarthy P., Zaman A., Uren N., et al. Minimising permanent pacemaker implantation (PPI) after TAVI. Br J Cardiol. 2021;28(2):20. doi: 10.5837/bjc.2021.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
First THV high implantation attempt in LAO-CAU fluoroscopic view, not accepted due to risk of device embolization.
Second THV implantation attempt in LAO-CAU fluoroscopic view.
Final THV deployment lower into the LVOT at the level of the PM, in LAO-CRA fluoroscopic view.