Abstract
Among lifestyle habits, the effect of exercise on skin moisturizing function has not been studied. Therefore, we aimed to clarify the effect of regular exercise on skin moisturizing function. The participants were 30-64 years old with no history of skin diseases and no exercise habits at the start of the study. The intervention group (n=9) continued to exercise at least 600 Mets/week for 8 weeks, while the control group (n=28) followed conventional lifestyle habits for 8 weeks. Questionnaires regarding lifestyle habits were administered at the beginning and after 8 weeks, and skin moisturizing function (stratum corneum hydration: SC hydration, Trans-Epidermal Water Loss: TEWL) was measured. Analysis of covariance was performed using sex, age, and measurements at the start of the study as covariates. Analysis of covariance showed that after 8 weeks of “moderate” or “higher” exercise, there was a trend toward higher SC hydration in the intervention group compared to that in the control group (p=0.083, η2=0.10). There was no difference in TEWL after 8 weeks (p=0.864, η2=0.00). These results suggest that regular exercise may help maintain and improve skin moisturizing function.
Key words: skin dryness, dermatitis, moisturizing, exercise
Introduction
Skin dryness increases the risk of developing various skin diseases such as dermatitis and eczema.1 It has been shown that skin dryness is accompanied by a decrease in skin moisturizing function,2,3 and that the skin moisturizing function decreases with age.4,5 To prevent this age-related decline in skin moisturizing function, it is considered important to maintain and promote skin moisturizing function from the onset of skin aging rather than at an older age.
It has been shown that skin aging begins in individuals in their 30s and 40s,6 and skin moisturizing function declines with aging.5 A study examining the percentage of skin dryness by age group reported that skin was dry in approximately 20% of those in their 30s.1 These reports suggest that measures that maintain and improve the skin moisturizing function from around the age of 30 are necessary to prevent skin dryness.
There are both internal and external factors associated with skin moisturizing function.7 Known internal factors include aging,5 race,8 and hormonal balance changes associated with menopause,9,10 while external factors include the surrounding environment and lifestyle habits.5,7 Lifestyle habits can be controlled, and skin functions can be maintained and improved by adjusting our lifestyle habits. Specific lifestyle habits that have been investigated regarding skin moisturizing function include daily moisturizing care,11 bathing habits,11 smoking,12,13 stress,14,15 and sleep quality.16
However, studies examining the relationship between exercise habits and skin moisturizing function are scarce. While some studies have focused on transient changes in the skin caused by exercise, such as the increase in skin blood flow caused by temporary exercise,17 there are no studies that have examined the effects of regular exercise on skin moisturizing function. Since it has been shown that regular exercise changes skin structure,18 it can be inferred that regular exercise has some effect on skin moisturizing function. This study aims to determine how regular exercise affects skin moisturizing function.
Materials and Methods
Study design
This study was a non-randomized controlled trial conducted from November 2020 to May 2021 and November 2021 to May 2022.
Participants
The sample size was estimated using G Power 3.1, requiring 26 participants per group. In the intervention group, participants were recruited from new members of three gyms. It was expected that new gym members would be highly motivated to exercise. In the control group, participants were recruited from two universities. Study participants were recruited on the condition that they did not currently have regular exercise habits.
Exclusion criteria were being pregnant, being 6 months postpartum, having history of chronic skin disease, and smoking.
Data collection
We used a self-administered questionnaire to assess the basic demographics, lifestyle habits, and activity levels of the participants. Skin moisturizing function was assessed by measuring stratum corneum hydration (SC hydration) and Trans-Epidermal Water Loss (TEWL) on the right forearm.
The self-administered questionnaire included questions regarding sex, age groups, medical history, and daily moisturizer use. Lifestyle habit attributes were determined based on the Diagnostic Inventory of Health and Life Habit (DIHAL.2). DIHAL.2 consists of three subscales, including those on exercise, diet, and rest.19 Exercise habits were measured using the International physical activity questionnaire (IPAQ) short version (Japanese). The intensity of exercise was divided into three activity levels according to the responses to IPAQ. Activity levels classification by IPAQ was classified according to the guidelines (The IPAQ group).20 Skin moisturizing functions were evaluated based on SC hydration and TEWL. SC hydration measurements were taken from the center point of each participant’s right forearm (8 cm point on the palm side from the elbow fossa center). SC hydration was measured using Mobile Moisture HP10-N (Courage+Khazaka electronic GmbH, Köln, Germany). TEWL measurements were taken 2 cm elbow side from the SC hydration measurement point. TEWL was measured using VAPO SCAN ASVT100RS (ASCH JAPAN Co., Ltd, Tokyo, Japan). To influence the measurement index, we requested that participants adhere to the following three rules: i) do not apply a body cream or similar substances to the measurement site for at least 12 hours before the study; ii) do not consume caffeinated beverages (e.g., coffee or tea) or smoke for at least three hours before the study; iii) do not engage in strenuous exercise for at least one hour before the study.
Intervention procedures
Definitions
In this study, regular exercise was set at “moderate” or higher on the IPAQ activity level classification for 8 weeks. This amount of exercise is equivalent to more than 600 Mets/week.
Detailed procedures
The study procedures in the intervention group were as follows.
A space in the gym was secured to avoid the influence of airflow, and the room temperature and humidity were checked.
At the beginning of the study, basic information, lifestyle, and activity level of participants were obtained using a questionnaire.
SC hydration and TEWL were measured.
Exercise to meet the criteria for regular exercise was discussed with the participants.
Participants were asked to exercise according to the determined exercise program and to record their daily exercise in an exercise diary.
Once every two weeks, we sent e-mails to participants to confirm their exercise status.
Eight weeks later, participants' lifestyle and activity levels were ascertained through an interview, and SC hydration and TEWL were measured.
The study procedures in the control group were as follows:
A space in the university was secured to avoid the influence of airflow, and the room temperature and humidity were checked.
At the beginning of the study, basic information, lifestyle, and activity level of participants were obtained using a questionnaire.
SC hydration and TEWL were measured.
Participants were asked to maintain their current lifestyle.
Eight weeks later, participants' lifestyle and activity levels were ascertained through an interview, and SC hydration and TEWL were measured.
Ethical consideration
This study was approved by the research ethics committee of Osaka Prefecture University Graduate School of Nursing (Approval No. 2020-29).
Data analysis method
We used analysis of covariance to determine if there was a difference in SC hydration and TEWL after 8 weeks of regular exercise. Covariance analysis was performed with a Full Analysis Set (FAS) and Per Protocol Set (PPS).
Sex, age groups, moisturizing care habits, DIHAL.2 rest score, data collection seasons, and measures of skin moisturizing function at study entry were used as covariates. The data collection season was divided into two study participation periods: November to February and January to May. Before conducting covariance analysis, the normality of the data obtained was checked to ensure that the correlations between the covariates and the objective variable at each measurement level were of equal quality.
In addition, participants were matched for sex, age groups, moisturizing care habits, DIHAL.2 rest score, and data collection seasons, as differences in the number of participants in the intervention and control groups would affect the analysis. For the matched participants, Mann-Whitney U-Test was used to analyze changes in SC water content and TEWL from the start of the study to 8 weeks later. Missing data were processed using multiple assignment methods. All analyses were performed in R ver. 4.0.3.
Results
The first study period was from November 2020 to May 2021, and the second period was from November 2021 to May 2022. In the first period, the intervention group included 6 participants, and 22 participants were in the control group. In the second period, 3 participants were in the intervention group, and the control group included 6 participants. In total, 37 participants (intervention group=9, control group=28) participated in the study. No participants dropped out of the study. However, 3 participants in the intervention group failed to achieve 8 weeks of moderate exercise. The characteristics of the study participants and their skin moisturizing functions at the beginning of the study are shown in Table 1. In terms of sex, the proportion of women in the control group was higher than that in the intervention group. SC hydration was higher in the intervention group than in the control group. Activity levels were low for all study participants in the intervention group, and there were 3 participants in the control group with moderate activity levels.
Changes in stratum corneum hydration due to regular exercise
The changes in SC hydration of study participants in the intervention and control groups are shown in Figure 1. SC hydration after 8 weeks (mean±SD) in the intervention group was 42.4±11.23 and 40.4±9.72 in the control group. FAS analysis of covariance was performed on SC hydration 8 weeks after study participation. The results showed that SC hydration after 8 weeks in the intervention group that exercised regularly tended to be higher than that in the control group, indicating a moderate effect size (p=0.083, η2=0.10). The mean of SC hydration (95% CI) after 8 weeks adjusted for covariates was 44.6 (39.3, 49.9) in the intervention group and 39.4 (36.0, 42.8) in the control group. Next, we conducted an analysis of covariance in the PPS, excluding the 3 participants in the intervention group who did not achieve 8 weeks of exercise and the 3 participants in the control group who had a moderate exercise habit from the beginning. The results showed that the intervention group that exercised regularly had significantly higher SC hydration after 8 weeks than the control group, with a larger effect size (p=0.023, η2=0.26). The intervention and control groups were matched, resulting in 5 matched participants in each group. Mann-Whitney U-Test for change in SC hydration [median (min, max)] from the beginning of the study to 8 weeks later (intervention: 1.7 (-2.7, 16.7); control: -9 (-12.7, -4)] showed a significant difference (p=0.009, r=0.82).
Changes in trans-epidermal water loss due to regular exercise
The changes in TEWL of study participants in the intervention and control groups are shown in Figure 2. TEWL after 8 weeks (mean±SD) in the intervention group was 6.0±2.76 and 6.8±2.68 in the control group. FAS analysis of covariance was performed on TEWL 8 weeks after study participation. The results showed no difference in TEWL values after 8 weeks between regular exercise and no effect size (p=0.864, η2=0.00). The mean of TEWL (95% CI) after 8 weeks adjusted for covariates was 6.62 (4.81, 8.44) in the intervention group and 6.80 (5.57, 8.03) in the control group.
Figure 1.
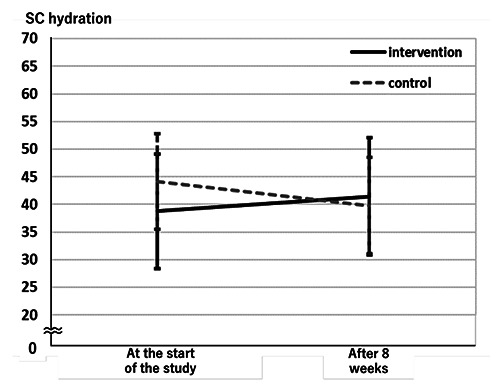
Change in average stratum corneum hydration in each group.
Figure 2.
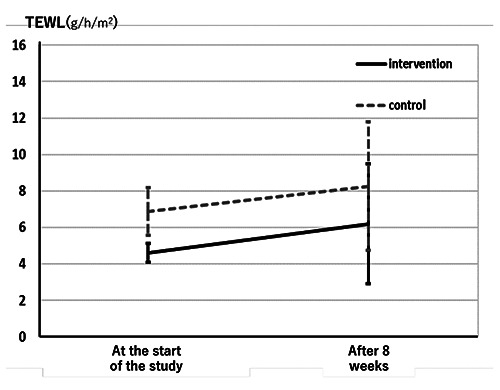
Change in average trans-epidermal water loss in each group.
Table 1.
Study participant characteristics.
| Intervention [n=9] | Control [n=28] | |
|---|---|---|
| Sex, n (%) | ||
| Male | 4(44) | 7(15) |
| Female | 5(56) | 21(75) |
| Age groups, n (%) | ||
| 30s | 3(33) | 11(39) |
| 40s | 1(11) | 8(29) |
| 50s | 5(56) | 8(29) |
| 60s | 0 (0) | 1(3) |
| Daily moisturizer, n (%) | ||
| Use | 3(33) | 9(32) |
| Do not use | 6(67) | 19(68) |
| DIHAL2 rest score, mean±SD | 49.6±9.5 | 45.8±8.1 |
| SC hydration, mean±SD | 39.2±8.1 | 43.1±8.5 |
| TEWL (g/h/m2), mean±SD | 5.2±1.5 | 5.8±1.9 |
| Activity levels, n (%) | ||
| Low | 9(100) | 25(89) |
| Moderate | 0 (0) | 3(11) |
| High | 0 (0) | 0 (0) |
DIHAL2, Diagnostic Inventory of Health and Life Habit 2; SC, stratum corneum; TEWL, trans-epidermal water loss.
Next, we conducted an analysis of covariance in the PPS. The results showed no difference in TEWL values after 8 weeks in the intervention group with regular exercise and almost no effect size (p=0.515, η2=0.02).
Mann-Whitney U-test for change in TEWL [median (min, max)] from the beginning of the study to 8 weeks later [intervention:- 0.1 (-2.3, 6.8); control: 0.2 (-4.4, 5)] showed a no significant difference (p=0.917, r=0.03).
Based on these results, a post-hoc analysis of the power of covariance analysis of SC hydration was performed for each of FAS and PPS: for FAS, the effect size f2=0.33, α=0.05, total sample size=37, number of covariates=7 and a posterior analysis of the test power was performed with power=0.49. For PPS, the effect size f2=0.33, α=0.05, total sample size=37, number of covariates=7 and a posterior analysis of the test power was performed with Power=0.93. Similarly, a post-hoc analysis of power was conducted for TEWL. In the FAS, the effect sizes were small, and post hoc analysis was impossible. For PPS, with effect size f2=0.14, α=0.05, number of samples=37, number of covariates=7, and post-hoc analysis of power, Power=0.13.
Discussion and Conclusions
The purpose of this study was to clarify the effects of regular exercise on skin moisturizing function. To clarify the effect of exercise on skin moisturizing function, we compared the amount of SC hydration and TEWL of the intervention group that exercised regularly for 8 weeks and the control group that lived as before, 8 weeks after the start of the study. The results showed that SC hydration after 8 weeks in the intervention group tended to be higher than that in the control group in the FAS, indicating a moderate effect. In PPS, the SC hydration of the intervention group after 8 weeks was significantly higher than that of the control group, and the effect size was also larger. Conversely, TEWL after 8 weeks did not differ depending on whether participants were exercising regularly or not in both FAS and PPS analyses.
The amount of SC hydration is an indicator of skin dryness.21 It has been shown that when SC hydration decreases, skin functions other than skin moisturizing function, such as a decrease in barrier function and changes in skin appearance, also decrease.2,22 Conversely, it has been reported that an increase in SC hydration also improved indicators such as skin appearance and skin elasticity.23,24 These findings suggest that the change in SC hydration is an important index for evaluating the effect of regular exercise on skin moisturizing function.
On the other hand, regarding TEWL, it has been shown that TEWL, along with SC hydration, decreases with the decline of skin moisturizing function due to aging.5 Therefore, it was hypothesized that both indices would increase when regular physical activity enhanced the retention of skin moisturizing function. However, the results of the present study showed that only SC hydration increased and TEWL did not change, possibly since the study participants were healthy adults and none had extremely irregular lifestyles. Changes in TEWL are caused by factors such as aging, chronic skin diseases, and insomnia.5,16 The current study included healthy adults aged 30-64 years without a history of skin diseases, and none of them had extremely low scores on DIHAL2 rest, which includes information on sleep. Therefore, changes in TEWL due to factors such as aging, skin diseases, and insomnia were considered nonexistent since the study began. Since no factors could change TEWL from the beginning of the study, it is possible that no change in TEWL occurred, even if regular exercise had enhanced the maintenance of skin moisturizing function. In addition, since no relationship between lifestyle and TEWL was found in the author’s previous study,25 TEWL is considered to be an indicator that does not change in healthy adults unless they have extremely irregular lifestyle habits, such as insomnia. In light of these findings, although TEWL did not change, a trend toward increased stratum corneum water content was observed, suggesting that regular exercise can be expected to improve the maintenance of skin moisturizing function.
There were several limitations to this study. The first was that the prevalence of coronavirus disease made it difficult to recruit as many study participants as proposed in the study design. This resulted in a smaller sample size and lower statistical power. However, the results are considered reliable because the analysis with matching still showed statistically significant differences and the post hoc analysis showed high power for changes in SC hydration in the PPS. Second, because the study design was not an RCT, unadjusted and unknown bias between the intervention and control groups cannot be ruled out. Third, we could not determine how long the skin moisturizing function is maintained after exercise. Fourth, it is unclear how much the amount of change in SC hydration and the differences between groups have clinical significance in skin moisturizing function.
Despite these limitations, we were able to show that regular exercise has the potential to maintain and improve skin moisturizing function. In the future, it will be necessary to examine the effects of exercise on skin moisturizing function in more detail by using an RCT design, evaluating the extent to which changes in skin moisturizing function due to exercise are sustained, and evaluating indicators other than skin moisturizing function.
Acknowledgments
The authors greatly appreciate the cooperation of the participants and staff members in this study.
Funding Statement
Funding: this study was funded by Shijonawate-gakuen University Health Science Institute.
References
- 1.Augustin M, Kirsten N, Körber A, et al. Prevalence, predictors, and comorbidity of dry skin in the general population. Eur Acad Deratol Venereol 2019;33:147-50. [DOI] [PubMed] [Google Scholar]
- 2.Verdier-Sévrain S, Bonté F. Skin hydration: a review on its molecular mechanisms. J Cosmet Dermatol 2007;6:75-2. [DOI] [PubMed] [Google Scholar]
- 3.Proksch E, Brandner JM, Jensen JM. The skin: an indispensable barrier. Exp Dermatol 2008;17:1063-72. [DOI] [PubMed] [Google Scholar]
- 4.Tanei R. [Xeroderma in the elderly, Pruritus, Treatment and care of lipid deficient eczema]. Japan Medical Jurnal 2012;4578:67-72. [Article in Japanese]. [Google Scholar]
- 5.Berardesca E, Loden M, Serup J, et al. The revised EEMCO guidance for the in vivo measurement of water in the skin. Skin Res Technol 2018;24:351-8. [DOI] [PubMed] [Google Scholar]
- 6.Krueger N, Luebberding S, Oltmer M, et al. Age-related changes in skin mechanical properties: a quantitative evaluation of 120 female subjects. Skin Res Technol 2011;17:141-8. [DOI] [PubMed] [Google Scholar]
- 7.Farage MA, Miller KW, Elsner P, et al. Intrinsic and extrinsic factors in skin ageing: a review. Int J Cosmet Sci 2008;30:87-95. [DOI] [PubMed] [Google Scholar]
- 8.Robinson MK. Population differences in skin structure and physiology and the susceptibility to irritant and allergic contact dermatitis: implications for skin safety testing and risk assessment. Contact Dermatitis 1999;41:65-79. [DOI] [PubMed] [Google Scholar]
- 9.Thornton M. Estrogens and aging skin. Dermatoendocrinol 2013;5:264-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lephart ED, Naftolin F. Menopause and the skin: old favorites and new innovations in cosmeceuticals for estrogen-deficient skin. Dermatol Ther 2021;11:53-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iizaka S. Skin hydration and lifestyle-related factors in community-dwelling older people. Arch Gerontol Geriatr 2017;72:121-6. [DOI] [PubMed] [Google Scholar]
- 12.Asakura K, Nishiwaki Y, Milojevic A, et al. Lifestyle factors and visible skin aging in a population of Japanese elders. J Epidemiol 2009;19:251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.du Plessis J, Stefaniak A, Eloff F, et al. International guidelines for the in vivo assessment of skin properties in non-clinical settings: Part 2. transepidermal water loss and skin hydration. Skin Res Technol 2013;19:265-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Altemus M, Rao B, Dhabhar FS, et al. Stress-induced changes in skin barrier function in healthy women. J Invest Dermatol 2001;117:309-17. [DOI] [PubMed] [Google Scholar]
- 15.Hunter HJ, Momen SE, Kleyn CE. The impact of psychosocial stress on healthy skin. Clin Exp Dermatol 2015;40:540-6. [DOI] [PubMed] [Google Scholar]
- 16.Yoshizaki T, Kimira Y, Mano H, et al. Association between skin condition and sleep efficiency in Japanese young adults. J Nutr Sci Vitaminol 2017;63:15-20. [DOI] [PubMed] [Google Scholar]
- 17.Rossi M, Santoro G, Maurizio S, Carpi A. Spectral analysis of skin blood flowmotion before and after exercise in healthy trained and in sedentary subjects. Int J Sports Med 2006;27:540-5. [DOI] [PubMed] [Google Scholar]
- 18.Crane JD, MacNeil LG, Lally JS, et al. Exercise-stimulated interleukin-15 is controlled by AMPK and regulates skin metabolism and aging. Aging Cell 2015;1:25-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tokunaga M. [Development of health and life habit inventory (DIHAL.2)]. Health Sci 2005;27:57-70. [Article in Japanese]. [Google Scholar]
- 20.The IPAQ Group. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). Available from: https://sites.google.com/site/theipaq/scoringprotocol. Last accessed November 20, 2022. [Google Scholar]
- 21.White-Chu EF, Reddy M. Dry skin in the elderly: complexities of a common problem. Clin Dermatol 2011;29:37-42. [DOI] [PubMed] [Google Scholar]
- 22.Naik S, Bouladoux N, Wilhelm C, et al. Compartmentalized control of skin immunity by resident commensals. Science 2012;337:1115-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wakeman MP. An open-label forearm-controlled pilot study to assess the effect of a proprietary emollient formulation on objective parameters of skin function of eczema-prone individuals over 14 days. Clin Cosmet Investig Dermatol 2017;10:275-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Draelos ZD, Gunt H, Zeichner J, Levy S. Clinical evaluation of a nature-based Bakuchiol anti-aging moisturizer for sensitive skin. J Drugs Dermatol 2020;19:1181-3. [DOI] [PubMed] [Google Scholar]
- 25.Oizumi R, Sugimoto Y, Aibara H. The association between activity levels and skin moisturising function in adults. Dermatol Rep 2021;13:8811. [DOI] [PMC free article] [PubMed] [Google Scholar]


