Abstract
Objective
Acupuncture is an effective treatment for arrythmias and postoperative symptoms but has not been investigated after cardiac surgery. Acupuncture After Heart Surgery is a prospective, randomized, controlled pilot trial of daily inpatient acupuncture or standard care after valve surgery with the primary end point being feasibility and secondary end points being reduction in postoperative atrial fibrillation incidence and postoperative symptoms.
Methods
A total of 100 patients without a history of atrial fibrillation underwent primary valve surgery via sternotomy and randomized 1:1 to acupuncture (51) or standard care (49). The acupuncture group received daily inpatient sessions starting on postoperative day 1. Postoperative symptoms (pain, nausea, stress, anxiety) were assessed once daily in the standard care group and before/after daily intervention in the acupuncture group. The groups were comparable except for age (acupuncture: 55.6 ± 11.4 years, standard care: 61.0 ± 9.3 years; P = .01).
Results
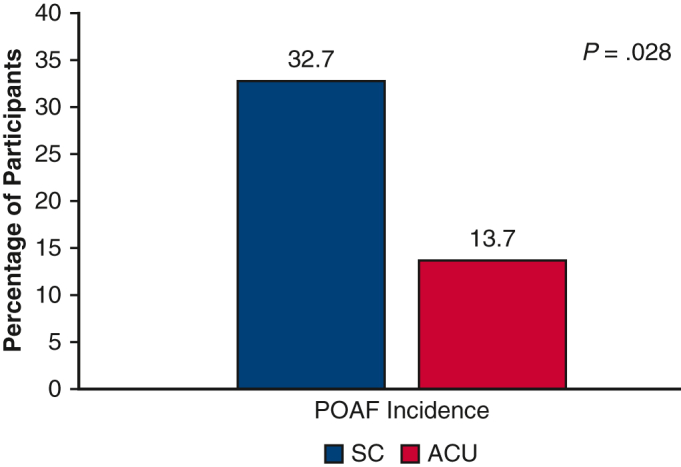
The Acupuncture After Heart Surgery pilot trial met primary and secondary end points. There were no adverse events. An average of 3.8 (±1.1) acupuncture sessions were delivered per patient during a mean hospital stay of 4.6 days (±1.3). Acupuncture was associated with a reduction in pain, nausea, stress, and anxiety after each session (P < .0001), and patients receiving acupuncture had reduced postoperative stress and anxiety across admission compared with standard care (P = .049 and P = .036, respectively). Acupuncture was associated with reduced postoperative atrial fibrillation incidence (acupuncture: 7 [13.7%], standard care: 16 [32.7%]; P = .028), fewer discharges on amiodarone (acupuncture: 5 [9.8%], standard care: 13 [26.5%]; P = .03), and fewer hours in the intensive care unit (acupuncture: 30.3 ± 10.0, standard care: 37.0 ± 22.5; P = .057).
Conclusions
Acupuncture after valve surgery is feasible, is well tolerated, and has clinical benefit. The reduction noted in postoperative atrial fibrillation incidence will inform larger trials designed to further investigate the impact of acupuncture on postoperative atrial fibrillation and medical outcomes.
Key Words: acupuncture, cardiac surgery, clinical trial, postoperative atrial fibrillation, valve surgery
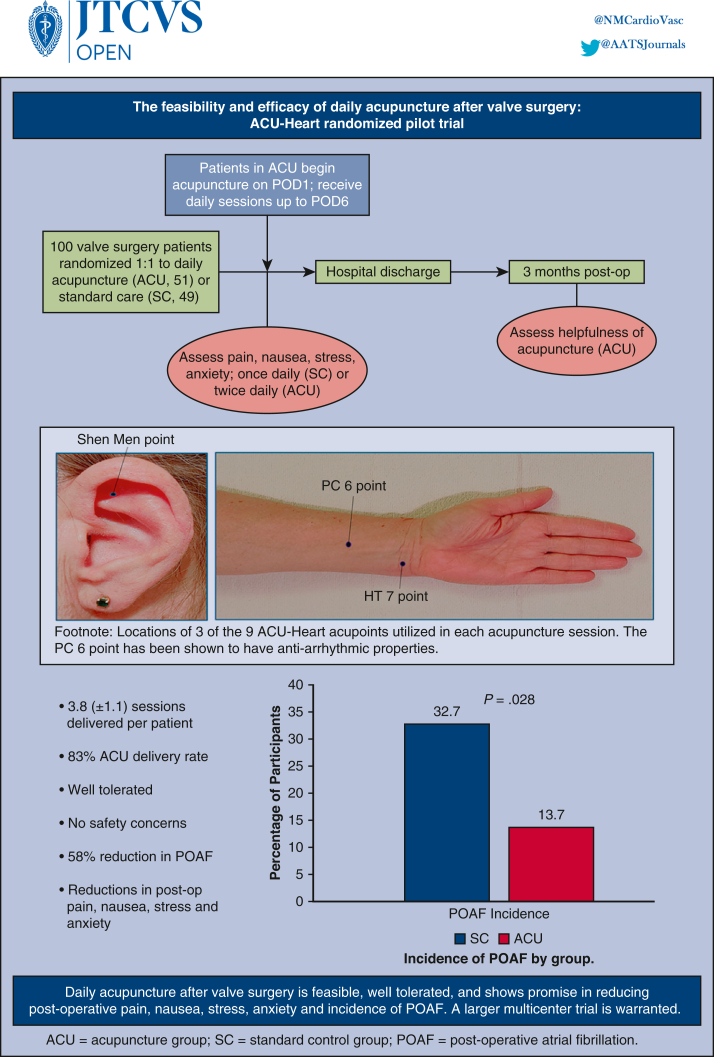
Graphical abstract
Daily inpatient acupuncture was associated with a decreased incidence of in-hospital POAF.
Central Message.
The ACU-Heart pilot trial evaluated daily acupuncture after valve surgery. The primary end point of feasibility was met, as were secondary end points of reduced POAF incidence and postsurgical symptoms.
Perspective.
ACU-Heart is a randomized controlled pilot trial (n = 100) of daily acupuncture or SC after valve surgery that demonstrates the feasibility and potential benefit of postoperative acupuncture in the cardiac surgical setting. Acupuncture was well tolerated, without adverse effects, and positively impacted patients' symptoms. Reduced incidence of POAF is promising.
Postoperative atrial fibrillation (POAF) is one of the most common complications after cardiac surgery, impacting anywhere from 10% to 65% of patients, depending on the type of surgery, surveillance, and patient characteristics, with a higher incidence after valve surgery.1, 2, 3 POAF places considerable burden on the healthcare system, contributing to stroke and increased hospital and late mortality.4,5 Effective therapy to reduce POAF remains elusive but welcome, given its impact on morbidity, mortality, and healthcare costs.
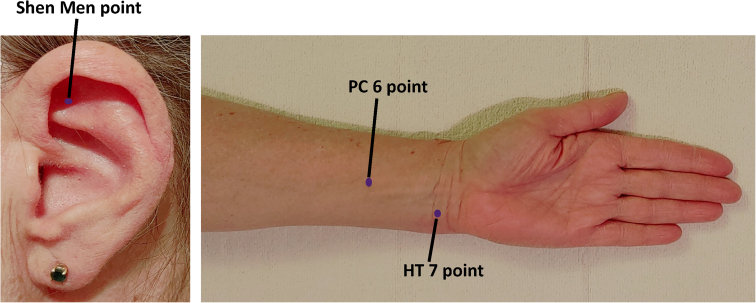
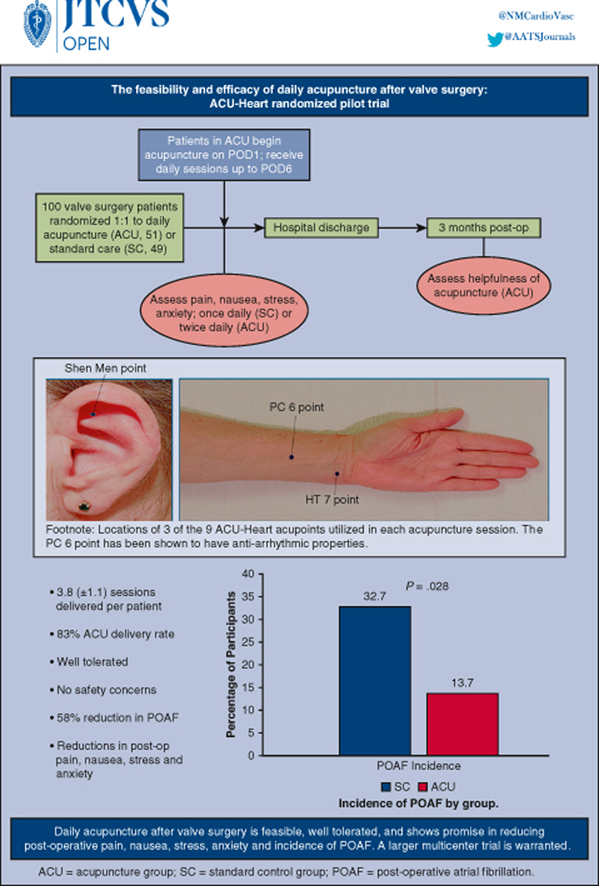
Acupuncture may prove to be a promising prophylactic treatment after heart surgery, with potential to curtail POAF while also reducing surgical side effects, such as pain, nausea, and postoperative anxiety.6, 7, 8, 9, 10 Previous studies have shown that stimulation of the PC 6 point (located on the anterior forearm, Figure 1) has an antiarrhythmic effect in patients with persistent and paroxysmal atrial fibrillation (AF), with acupuncture intervention (ACU) associated with comparable recurrence rates when compared with amiodarone up to 1 year after cardioversion.11,12 In a 2017 systematic review and meta-analysis comprising 13 randomized controlled trials with a total of 797 participants, the authors concluded that acupuncture was as effective as traditional antiarrhythmic medications for treating arrhythmias (risk ratio, 1.18, 95% confidence interval, 0.78-1.79, P = .44), and acupuncture was superior to no treatment (risk ratio, 18.80, 95% confidence interval, 12.68-24.92, P < .001).13 Although daily acupuncture has yet to be examined after cardiac surgery or in the context of POAF, 1-time use of preoperative or intraoperative acupuncture during heart surgery has demonstrated anesthetic, pain mitigating, and antiarrhythmic properties of acupuncture, resulting in decreased pulmonary infection, opioid consumption, postoperative nausea and emesis, and healthcare costs.9,14, 15, 16 Acupuncture for postoperative pain management has proven beneficial across a variety of surgical populations, contributing to decreased pain severity, opioid use, and opioid-related side effects.7,16, 17, 18, 19
Figure 1.
Locations of 3 of the 9 ACU-Heart acupoints used in each acupuncture session. The PC 6 point has been shown to have antiarrhythmic properties. PC, Pericardium meridian; HT, heart meridian.
To our knowledge, the feasibility of daily acupuncture in the hospital setting after open heart surgery has not been established, but acupuncture offers promise in reducing the incidence of POAF and severity of postoperative pain, nausea, and anxiety. We set out to close this gap by devising an acupuncture protocol that has potential to improve postoperative outcomes. The Acupuncture After Heart Surgery (ACU-Heart) pilot trial was designed with the primary end point of feasibility. Secondary end points were incidence of POAF, severity of postoperative pain, nausea, stress, anxiety (PNSA), and medical outcomes. ACU-Heart investigators limited this pilot trial to patients undergoing valve surgery given the traditionally higher incidence of POAF after valve surgery,1 in an attempt to maximize statistical power amidst a smaller sample.
Materials and Methods
Study Design
ACU-Heart was a prospective, 2-arm, randomized, feasibility pilot trial examining the use of daily postoperative acupuncture among patients recovering from valve surgery. Eligible patients were approached during a preoperative clinic visit for nonemergency valve surgery. Patients were assigned randomly (1:1) to ACU or standard care (SC) after informed consent, completion of questionnaires, and a scheduled surgical date. Those randomized to receive ACU were offered daily intervention beginning on postoperative day (POD) 1 and continuing until discharge or POD 6.
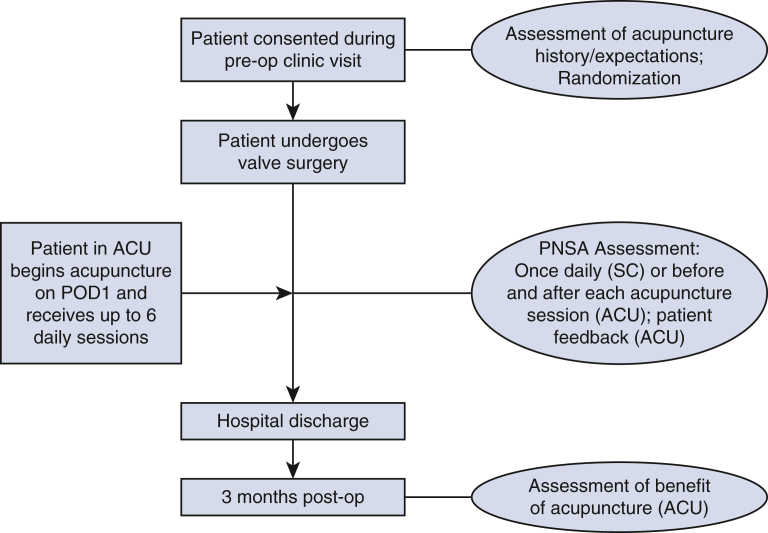
During postoperative hospitalization, patients completed self-report ratings of PNSA, once daily in the SC group and twice daily in the ACU group, immediately before and after intervention to allow for pre–post comparison. PNSA for both groups were completed within the same time window. Participants in the ACU group were queried 3 months postoperatively about the perceived benefit of postoperative acupuncture. Figure E1 shows the study design flow.
Figure E1.
Study design flow. Eligible patients were approached and consented at a preoperative clinic visit, at which time they completed baseline questionnaires. Patients in ACU received daily acupuncture starting on POD 1. Daily assessments of PNSA were completed daily in SC and pre- and postacupuncture in ACU. Patients in ACU completed a questionnaire about the postoperative acupuncture experience at 3 months postoperatively. ACU, Acupuncture intervention; PNSA, pain, nausea, stress, anxiety; POD, postoperative day; SC, standard care.
Recruitment and Eligibility
Eligible patients were aged 18 years or more with valvular disease, scheduled for nonemergency valve surgery via sternotomy after evaluation in the cardiac surgery clinic of a large Midwestern tertiary academic medical center between January 2016 and August 2019. Patients were ineligible to participate if they had a history of AF or flutter, had prior or concomitant cardiac surgery, or presented with presurgical or postsurgical conditions unfavorable for acupuncture. To evaluate the impact of acupuncture on new-onset POAF, participants were excluded if they developed AF intraoperatively or before the start of intervention (afternoon of POD 1).
Ethics and Informed Consent
This study was approved by the Institutional Review Board of Northwestern University (#STU00201408, approved, September 11, 2015). Participants provided written informed consent, which included permission for publication.
Randomization
Patients were randomly assigned (1:1) to ACU or SC via sealed envelopes containing study arm assignment generated by the study statistician who was not involved in enrollment. Participants were notified of randomization status the morning of surgery.
Surgical Protocol
In accordance with Society of Thoracic Surgeons (STS) performance criteria, patients received preoperative beta-blockers. No other AF prophylaxis was performed. Postoperative AF was treated similarly in both groups, according to STS protocol, with amiodarone plus cardioversion as needed. Patients received continuous telemetry monitoring until discharge.
Acupuncture Intervention
The study intervention was a novel application of established acupuncture practice administered in the hospital setting to patients recovering from valve surgery. The ACU-Heart acupuncture protocol consisted of 9 acupoints that were used in each session (5 on the body, 4 on the ear), chosen to target common symptoms after heart surgery, including arrhythmias, mood disturbance, pain, nausea, and stress (Table 1). Each acupuncture session began with a formal assessment consistent with traditional Chinese medicine (TCM). At the start of each intervention, the acupuncturist had the freedom to add additional acupoints from the ACU-Heart supplemental acupoints protocol, in accordance with TCM practice and based on the TCM assessment and patient presentation.
Table 1.
ACU-Heart acupuncture protocol plus supplemental acupoints
| ACU-heart acupuncture protocol: Acupoints used in every ACU session | |||
| Body acupoints and associated targeted symptoms | |||
| PC 6 | Atrial fibrillation, nausea, anxiety, depression | ||
| HT 7 | Atrial fibrillation, anxiety, depression | ||
| LI 4 | Pain, depression | ||
| LIV 3 | Pain, depression | ||
| Yin Tang | Anxiety, depression | ||
| Auricular (ear) acupoints and associated targeted symptoms | |||
| Shen Men | Anxiety, depression, pain, insomnia, inflammation | ||
| Sympathetic | Smooth muscle spasms, anxiety, blood circulation, pain | ||
| Heart (C) | Chest pain, angina, arrhythmia, blood pressure | ||
| Point Zero | Homeostasis, anxiety, depression | ||
| ACU-heart supplemental acupoints: Additional acupoints available for use each session in response to the daily TCM assessment and symptom presentation | |||
| Depression | UB 3 point was added if patient reported depression
|
||
| Anxiety | UB 3 point was added if patient reported anxiety
|
||
| Nausea | ST 36 point was added if patient reported nausea
|
||
| Pain | SP 10 and GB 34 points were added if patient reported pain
|
||
ACU, Acupuncture; PC, pericardium meridian; HT, heart meridian; LI, large intestine meridian; LIV, liver meridian; TCM, traditional Chinese medicine; UB, bladder meridian; LU, lung meridian; DU, governing vessel; ST, stomach meridian; SP, spleen meridian; CV, conception vessel; GB, gallbladder meridian; TW, triple warmer.
Single-use sterile SEIRIN (0.16 × 15 and 0.16 × 30) needles were inserted ¼ to 1 inch, depending on location and underlying anatomy, and no manipulation nor stimulation was delivered. Once in place, needles were retained by the patient for approximately 30 minutes. Weekday acupuncture sessions occurred in the late afternoon/evening, and weekend sessions occurred midday. Nursing staff were notified of the timing in advance. Intervention occurred in the patient's private hospital room, either in bed or in a bedside recliner, depending on patient and nursing preference. Efforts were made to minimize interruptions and maintain a quiet space.
Three licensed acupuncturists trained in TCM provided ACU and are employed by the Osher Center for Integrative Health at the same academic institution. Each had prior experience delivering acupuncture in the medical setting and underwent training to gain familiarity with the postoperative cardiac surgery setting and to ensure consistency across providers and sessions. Acupuncturists were not blinded to treatment condition.
Standard Care
Participants randomized to SC received no intervention.
Data Collection
Outcome measures were as follows.
Feasibility
Feasibility of the intervention was assessed via acceptability and intervention delivery. Acceptability examined enrollment, retention, intervention tolerance, adverse events, and patient feedback. Intervention delivery examined completed, missed, and interrupted sessions.
Postoperative atrial fibrillation
POAF was determined via an adjudication committee consisting of one electrophysiologist and 2 cardiac surgeons who reviewed each patient chart to ascertain the presence of POAF during hospitalization, in accordance with the STS. Raters were blinded to treatment condition and to each other's ratings. Unanimous consensus was required. Discrepancies (2) were discussed until consensus was reached.
Pain, nausea, stress, anxiety
Patients rated current severity of PNSA each on a scale of 0 to 10, once daily in SC and twice daily in ACU, before and after acupuncture. Acupuncturists were blinded to PNSA ratings.
Acupuncture history and expectations
A self-report measure captured history of acupuncture use and expectations related to postoperative acupuncture.
Intervention feedback
Patients rated the helpfulness of each acupuncture session on a scale of 0 to 100. Acupuncturists were blinded to ratings. At 3 months postoperatively, patients were asked, “Overall, did you find acupuncture after heart surgery to be helpful?” with response options ranging from 0 to 4.
Medical information
Preoperative, intraoperative, and postoperative data were pulled directly from our patient population in the STS database. This includes demographics, cardiac disease etiology, comorbidities, risk factors, surgical details, concomitant procedures, complications, and length of stay (LOS) in the intensive care unit (ICU) and hospital.
Statistical Methods
The primary objective of this pilot trial was to evaluate the feasibility of postoperative acupuncture via enrollment, retention, safety, and intervention delivery. A secondary objective was to obtain an initial estimate of the effect size of acupuncture on targeted end points, thus informing the design of a larger and more definitive future clinical trial. Secondary end points included medical outcomes (POAF, LOS, complications) and postsurgical PNSA. Being hypothesis-generating, this pilot trial was not powered to detect specific differences in POAF between groups. However, within each arm, 50 participants was estimated to provide more than 90% power to detect a POAF incidence as low as 4.5% at 0.025 significance level.
Participant enrollment, retention, completed interventions, missed interventions, interrupted interventions, patient feedback, and baseline characteristics were summarized using mean ± standard deviation, median/interquartile range values, or counts/percentages, as appropriate. Surgical outcome measures, including POAF, LOS, complication rates, and use of antiarrhythmic therapies, were summarized and compared using the exact test for binomial proportions, chi-square test, Fisher exact test, or Wilcoxon rank-sum test, depending on data distributions. Longitudinal measures of postoperative symptoms were analyzed via linear mixed effects models and generalized estimating equation. Within-group comparisons of pre- and postacupuncture symptoms were based on paired t tests or Wilcoxon signed-rank test. Statistical significance was declared at 2-sided 5% level, and no adjustments for multiple testing were made. All statistical analyses were performed in SAS Version 9.4 (SAS Institute, Inc).
Results
Table 2 includes demographic and clinical characteristics by study arm. Participants were predominantly male (71%), White (86%), and college educated (71%). Average age was 58.3 (±10.7) years. Participants underwent surgical correction of the mitral valve (68%), aortic valve (35%), or tricuspid valve (4%; Table 3). The 2 groups were well balanced except for age (SC: 61.0 ± 9.3 years, ACU: 55.6 ± 11.4 years, P = .01). A majority of participants (73%) reported no prior acupuncture history. Of those with prior experience (n = 27), 82% had received 5 or fewer sessions, primarily for pain management.
Table 2.
Baseline clinical characteristics
| Variable | N | Entire cohort (N = 100) | ACU (N = 51) | SC (N = 49) | P value |
|---|---|---|---|---|---|
| Age | 100 | 58.3 (±10.7) | 55.6 (±11.4) | 61.0 (±9.3) | .011 |
| Female | 100 | 29 (29%) | 15 (29%) | 14 (29%) | .926 |
| Race—White | 100 | 86 (86%) | 44 (86%) | 42 (86%) | .097 |
| Body mass index | 100 | 27.4 ± 5.2 | 27.0 ± 5.3 | 26.9 ± 5.0 | .332 |
| CHADS2 score | 100 | 0.7 ± 0.8 | 0.6 ± 0.7 | 0.8 ± 0.9 | .198 |
| Creatinine level | 100 | 1.0 (0.9, 1.0) | 1.0 (0.9, 1.1) | 1.0 (0.9, 1.0) | .704 |
| LVEF (%) | 100 | 65.0 (61.5, 69.0) | 65.0 (60.0, 67.0) | 65.9 (63.0, 69.0) | .137 |
| Left atrial size | 100 | 4.0 (3.7, 4.7) | 4.0 (3.9, 4.9) | 4.0 (3.7, 4.6) | .416 |
| Diabetes | 100 | 6 (6.0%) | 1 (2.0%) | 5 (10.2%) | .083 |
| Current smoker | 100 | 3 (3.0%) | 2 (3.9%) | 1 (2.0%) | .582 |
| Renal failure | 100 | 0 (0%) | 0 (0%) | 0 (0%) | |
| Dyslipidemia | 100 | 46 (46%) | 24 (47.1%) | 22 (44.9%) | .828 |
| Hypertension | 100 | 45 (45%) | 22 (43.1%) | 23 (46.9%) | .702 |
| Chronic lung disease | 100 | 0 (0%) | 0 (0%) | 0 (0%) | |
| Peripheral vascular disease | 100 | 0 (0%) | 0 (0%) | 0 (0%) | |
| Cerebrovascular disease | 100 | 0 (0%) | 0 (0%) | 0 (0%) | |
| Prior stroke | 100 | 1 (1%) | 0 (0%) | 1 (2%) | .305 |
| Prior myocardial infarction | 97 | 2 (2.1%) | 0 (0%) | 2 (4.3%) | .132 |
| Congestive heart failure | 100 | 10 (10%) | 4 (7.8%) | 6 (12.2%) | .463 |
| Coronary artery disease | 91 | 6 (6.6%) | 3 (6.5%) | 3 (6.7%) | .978 |
Values are presented as mean ± standard deviation, n (%), or median (interquartile range). ACU, Acupuncture arm; SC, standard care; CHADS2, congestive heart failure, hypertension, age, diabetes, gender; LVEF, left ventricular ejection fraction.
Table 3.
Intraoperative and postoperative outcomes
| Variable | N | Entire cohort (N = 100) | ACU (N = 51) | SC (N = 49) | P value |
|---|---|---|---|---|---|
| MV surgery | 100 | 68 (68%) | 34 (66.7%) | 34 (69.4%) | .771 |
| MV repair | 100 | 65 (65.0%) | 33 (64.7%) | 32 (65.3%) | |
| MV replacement | 100 | 3 (3.0%) | 1 (2.0%) | 2 (4.1%) | |
| AV surgery | 100 | 35 (35%) | 17 (33.3%) | 18 (36.7%) | .721 |
| AV repair | 100 | 2 (2%) | 0 (0%) | 2 (11.1%) | |
| AV replacement | 100 | 33 (33%) | 17 (33.3%) | 16 (32.7%) | |
| Tricuspid valve surgery | 100 | 4 (4.0%) | 2 (3.9%) | 2 (4.1%) | .967 |
| ASD/PFO surgery | 100 | 7 (7.0%) | 3 (5.9%) | 4 (8.2%) | .655 |
| Cardiopulmonary bypass (min) | 100 | 80.7 (±19.1) | 76.9 (±16.8) | 84.7 (±20.7) | .039 |
| Crossclamp time (min) | 100 | 69.1 (±17.4) | 65.9 (15.6) | 72.4 (±18.7) | .061 |
| ICU LOS, h | 100 | 33.6 (±17.5) | 30.3 (±10.0) | 37.0 (±22.5) | .057 |
| Total LOS, d | 100 | 4.6 (±1.3) | 4.7 (±1.5) | 4.5 (±1.0) | .597 |
| Reoperation for bleeding | 100 | 2 (2%) | 0 (0%) | 2 (4.1%) | .145 |
| Postoperative stroke | 100 | 2 (2.0%) | 2 (3.9%) | 0 (0%) | .161 |
| POAF | 100 | 23 (23%) | 7 (13.7%) | 16 (32.7%) | .028 |
| Discharged on amiodarone | 100 | 18 (18%) | 5 (9.8%) | 13 (26.5%) | .030 |
Values are presented as mean ± standard deviation, n (%). ACU, Acupuncture intervention; SC, standard care; MV, mitral valve; AV, aortic valve; ASD, atrial septal defect; PFO, patent foramen ovale; ICU, intensive care unit; LOS, length of stay; POAF, postoperative atrial fibrillation.
Primary Feasibility End Point
Acceptability
Enrollment and retention
A total of 255 consecutive patients were deemed eligible to participate in ACU-Heart during a preoperative clinic visit. A total of 146 patients (57%) provided consent, and 45 patients (17.6%) declined. Reasons for declining included disinterest in research (36%), disinterest in acupuncture (31%), feeling overwhelmed by surgery (22%), and other (11%). Sixty-four patients approached were lost to follow-up, 39 of whom were later determined to be ineligible and 25 of whom retained eligibility but never consented or declined (“passive decliners”). Of the 146 patients who consented to participate, 12 were excluded before randomization for no longer meeting inclusionary criteria and 31 were excluded after randomization for meeting ineligibility during the pre- or perioperative course. The primary reason for postrandomization exclusion was concomitant surgery. Three patients withdrew participation, 2 before intervention and 1 after intervention began. This participant received 2 ACU sessions and withdrew citing pain after returning to the ICU for placement of an implantable cardioverter defibrillator. These 3 participants formally withdrew consent to be included in the study and thus are not retained in the final sample, but are noted for purposes of acceptability. Thus, for purposes of outcomes of this pilot trial, the final sample is composed of 100 participants (51 ACU, 49 SC). Aside from the 1 patient who withdrew after intervention began, 100% who received intervention were retained in the study at hospital discharge and 96% of the ACU group responded to the 3-month follow-up (Figure 2, CONSORT diagram for details).
Figure 2.
Enrollment flow chart. A total of 255 patients were approached for the study, 146 of whom consented to participate. An additional 45 declined and 64 were lost to follow-up. After further exclusion of 12 patients who no longer met study criteria, 134 were randomized 1:1 to SC or daily ACU. A total of 31 patients (17 SC, 14 ACU) were excluded after randomization for meeting exclusionary criteria perioperatively. Three patients withdrew from the study, all in ACU. The final sample consisted of 100 patients (49 SC, 51 ACU). SC, Standard care; ACU, acupuncture intervention.
Participant feedback
Participants rated daily acupuncture as beneficial overall, with an average rating of 69.0 ± 26.6 on a scale of 0 to 100. At follow-up, participants reflected that acupuncture was moderately helpful (35 [74.4%]), with an additional 8 (17.0%) reporting it was extremely helpful and 4 (8.5%) reporting no perceived benefit.
Intervention tolerance and adverse events
Acupuncture was well tolerated, as demonstrated by adherence to the study protocol. All needles were retained for the entirety of the intervention. No adverse events were reported. One event occurred in real-time when a participant felt a pinch on her arm when a blood pressure cuff inflated close to a needle. The needle was repositioned with no further symptom.
Intervention delivery
Delivery of ACU proved logistically feasible in both the cardiac surgery ICU and the step-down unit. In fact, 100% of ACU patients received acupuncture on POD 1 in the cardiac surgery ICU. ACU patients received an average of 3.8 (±1.1) acupuncture sessions across an average LOS of 4.7 (±1.5) days. Missed sessions were uncommon. Of a total of 230 sessions that could have been delivered across the entirety of the study, 192 were completed, an 83% completion rate. The majority of the missed sessions occurred on the day of discharge, which had a 43% completion rate.
Interruptions occurred during 22 sessions (11%) and included nurse entry (11), phone rang (5), visitor entry (2), physician entry (2), hallway noise (1), and bathroom needs (1). Despite interruptions, the intervention was completed according to protocol 100% of the time. Ten sessions were conducted while the TV was on, 1 was conducted with music on, and 1 session was delivered while the patient was wearing a continuous positive airway pressure mask.
Secondary outcomes
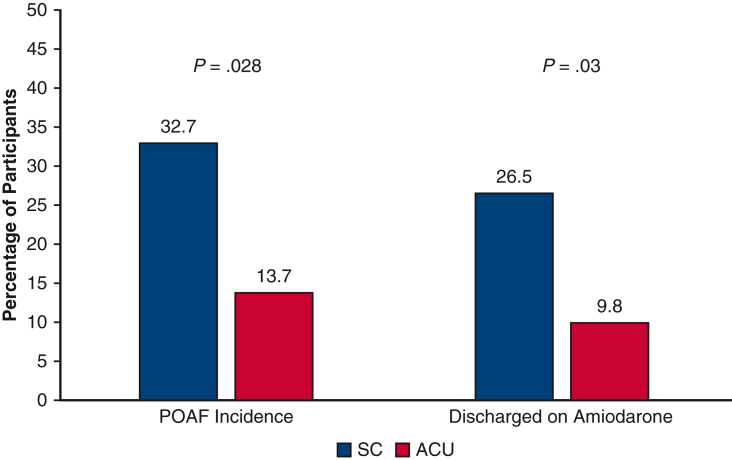
Secondary end point analyses revealed a statistically significant antiarrhythmic effect for acupuncture. As shown in Figure 3, new-onset POAF occurred in 23% of the overall sample, with reduced incidence among those in ACU (7, 13.7%) versus those in SC (16, 32.7%, P = .028). Discharge on amiodarone followed the same pattern, with 5 (9.8%) ACU patients and 13 (26.5%) SC patients discharged on the antiarrhythmic (P = .03). Participants in ACU spent fewer hours in the ICU compared with SC, a trend approaching statistical significance (P = .057), but total LOS was comparable between groups. The groups were comparable regarding other complications. Operative characteristics and outcomes are displayed in Table 3.
Figure 3.
Incidence of POAF and discharge on amiodarone by group. Patients in ACU had a lower incidence of POAF compared with those in SC (13.7% vs 32.7%, P = .028). Fewer patients in ACU were discharged on amiodarone (9.8% vs 26.5%, P = .03). POAF, Postoperative atrial fibrillation; SC, standard care; ACU, acupuncture intervention.
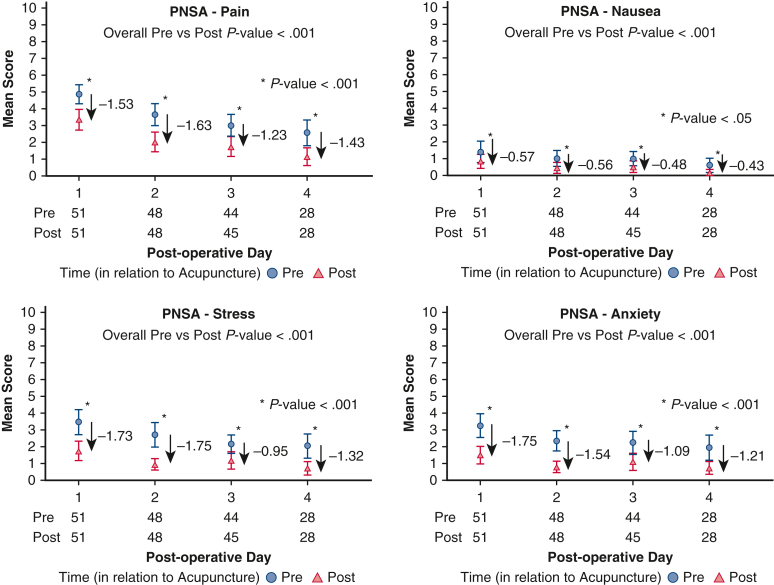
Secondary end point analyses revealed a significant benefit to postoperative PNSA. Daily stress and anxiety levels across hospital admission were more favorable in ACU versus SC (stress: F = 3.91, P = .049; anxiety: F = 4.46, P = .036). Within the ACU group, PNSA severity was significantly reduced after intervention compared with presession levels (P < .0001; Figure 4).
Figure 4.
Severity of postoperative symptoms before and after acupuncture among the ACU participants. PNSA were each reduced after daily ACU, both with each day (P < .001) and collapsed across days (P < .001). PNSA, Pain, nausea, stress, anxiety.
Discussion
The ACU-Heart pilot trial successfully demonstrated that postoperative daily acupuncture in the hospital setting after valve surgery is feasible and efficacious, associated with reduced incidence of POAF, decreased need for amiodarone at discharge, shorter ICU LOS, and reductions in postoperative PNSA (Figure 5).
Figure 5.
The ACU-Heart pilot trial. Postoperative daily acupuncture in the hospital setting after valve surgery is feasible and efficacious, associated with reduced incidence of POAF, shorter ICU LOS, and reductions in postoperative PNSA. ACU, Acupuncture intervention; POD, postoperative day; SC, standard care; POAF, postoperative atrial fibrillation.
The primary end point of feasibility was met. Daily acupuncture after valve surgery was well received by patients and logistically feasible. Retention was high. Three withdrawals occurred, all in the ACU group, implying potential patient hesitation toward acupuncture during surgical recovery. However, the majority of patients (73%) had no prior experience with acupuncture, suggesting that openness to postoperative acupuncture is not dependent on prior history. Acupuncture delivery was feasible in both the ICU and the surgical step-down unit, with 100% of ACU patients receiving intervention on POD 1. Intervention proved more difficult to deliver on the day of discharge, not surprisingly, but maintained a high rate of delivery overall (83%). Patients not only accepted and tolerated acupuncture after valve surgery but also most found it to be a positive experience.
ACU-Heart met secondary end points of improved outcomes, as noted by reductions in incidence of POAF and severity of postoperative PNSA. Those in the ACU group experienced a 58% reduction of incidence of POAF compared with those in the SC group. The antiarrhythmic properties of acupuncture previously found in the outpatient setting among those with persistent and paroxysmal AF11,12 may extend to POAF, offering a safe and noninvasive prophylaxis option for POAF. At a cost of approximately $280 per surgical patient in this trial, acupuncture is a relatively inexpensive adjunct therapy with the potential to reduce healthcare costs. Postoperative symptoms also improved from acupuncture. The benefit to pain control may extend to pulmonary recovery, because acupuncture-mediated pain reduction has been shown to enhance lung functioning after cardiac surgery.15 Together, these findings suggest that acupuncture has a promising future in the cardiac surgery setting.
The postsurgical environment is fast paced, and the feasibility of adding 30 to 45 minutes daily for ACU was unknown. The ACU-Heart trial demonstrated that acupuncture delivery can be well integrated into the cardiac surgery setting. Minor hospital intrusions did not impede intervention delivery. The success of intervention delivery is in part due to the flexibility and support of the acupuncturists and nursing staff. Acupuncturists were available 7 days a week. Nursing staff worked to minimize interruptions. Despite potential for this intervention to feel burdensome to providers, nurses often commented that they observed a positive change in patient disposition after a session. The potential benefit of acupuncture to patients' mood and pain could strengthen staff support and further promote intervention delivery.
The specific mechanisms for acupuncture-mediated rhythm control and pain reduction are not yet well understood, but several physiological pathways may exist, including anti-inflammatory, release of endogenous opioids, and autonomic mechanisms related to vagal or sympathetic neural activity. In a study that found amiodarone plus acupuncture superior to an amiodarone-only control group among patients with persistent AF undergoing pulmonary vein isolation, those who received acupuncture exhibited lower inflammatory markers including tumor necrosis factor-alpha, interleukin-6, C-reactive protein, transforming growth factor-beta1, and matrix metalloproteinase-2.10 Future trials will benefit from incorporating markers of inflammation and sympathetic arousal to better elucidate mechanistic pathways.
Study Limitations
Although the ACU-Heart trial successfully executed a novel approach to postoperative cardiac recovery, it is not without several limitations. First, there was an imbalance in age between groups despite randomization, where those in the SC group were slightly older and spent more minutes on cardiopulmonary bypass, 2 factors that could contribute to increased POAF. These imbalances are not ideal but do not detract from the primary end point of feasibility. Interpretation of secondary end points are preliminary and require a larger trial to understand more definitely the role of acupuncture on surgical outcomes. However, the incidence of POAF in ACU (13.7%) is lower than expected and likely not uniquely reflective of sample characteristics. Second, results may be limited in generalizability due to the narrow inclusion criteria of the study. Several participants became ineligible postrandomization. In retrospect, randomization would have been ideal postsurgery when it was evident that participants still met inclusion criteria. We chose not to perform intent-to-treat analyses with all participants randomized given this would create significant heterogeneity that could undermine meaningful results in this size sample (eg, including those who did not undergo surgery, underwent concomitant surgery). Because this was a pilot trial with the primary end point of feasibility, we were comfortable proceeding with analyses as planned, using those retained in the final sample after all exclusionary criteria were met.
ACU-Heart used chart review limited to the surgical admission for detection of POAF, limiting our understanding of acupuncture's impact on timing and severity of POAF, including postdischarge complications, readmission rates, and later onset or recurrence of POAF.
Acupuncturists and patients were not blinded to randomization, which may have impacted patients' self-report of symptoms. A comparison SC group was chosen given our goal of assessing feasibility. Sham ACUs are largely viewed as suboptimal in the integrative medicine community, with the potential for false-negative results due to incidental factors of sham acupuncture, which is not considered fully inert.20 Adding an attention control arm or sham acupuncture arm may be useful in future studies so long as a SC control can help discern differences due to treatment-related factors (eg, acupuncture) versus incidental factors (eg, uninterrupted time).
ACU-Heart demonstrates the successful integration of a novel ACU into cardiac surgery recovery that benefits surgical outcomes and postoperative symptoms. This trial demonstrates that, with close cooperation with the acupuncture team, postoperative acupuncture is feasible and beneficial. Acupuncture was safe. The important secondary end points demonstrating reduced incidence of POAF, more favorable outcomes, and improved postsurgical symptoms were met. A larger randomized trial of patients undergoing a variety of cardiac operations in multiple medical centers is warranted. In addition to clinical results, examination of potential underlying physiologic mechanisms is warranted.
Conclusions
The increased morbidity, mortality, and healthcare burden imparted by POAF after valve surgery warrants ongoing consideration of alternate treatment strategies. Acupuncture after valve surgery proves to be a feasible and well-tolerated adjunct therapy that shows promise in reducing POAF and postsurgical PNSA. To our knowledge, this was the first study to assess the feasibility and acceptability of daily acupuncture in the hospital setting after heart surgery. A larger multicenter trial targeting a broader surgical population is warranted to evaluate the impact of acupuncture on the severity and timing of POAF, as well as to investigate physiological mechanisms.
Conflict of Interest Statement
K.D.P.: Boston Scientific, consultant. C.J.D.: Edwards Lifesciences, grant support and uncompensated consultant; Abbott, grant support. P.M.M.: AtriCure and Medtronic, honorarium; Abbott, advisory board; Edward Lifesciences, royalties and consulting. All other authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Acknowledgments
ACU-Heart is funded by a philanthropic gift from the Malkin Family Foundation. The support and generosity of the Malkin Family are greatly appreciated.
Footnotes
This pilot study was approved by the Institutional Review Board of Northwestern University (#STU00201408, approved 6/6/17). Participants provided written informed consent, which included permission for publication.
This pilot study was funded by a philanthropic gift from the Malkin Family Foundation, and the sponsor had no participation in the study design, collecting, analyzing, and interpreting the data, writing the report, or deciding whether and where to submit for publication.
Appendix E1
References
- 1.Maisel W.H., Rawn J.D., Stevenson W.G. Atrial fibrillation after cardiac surgery. Ann Intern Med. 2001;135:1061–1073. doi: 10.7326/0003-4819-135-12-200112180-00010. [DOI] [PubMed] [Google Scholar]
- 2.Creswell L.L., Schuessler R.B., Rosenbloom M., Cox J.L. Hazards of postoperative atrial arrhythmias. Ann Thorac Surg. 1993;56:539–549. doi: 10.1016/0003-4975(93)90894-n. [DOI] [PubMed] [Google Scholar]
- 3.Asher C.R., Miller D.P., Grimm R.A., Cosgrove D.M., III, Chung M.K. Analysis of risk factors for development of atrial fibrillation early after cardiac valvular surgery. Am J Cardiol. 1998;82:892–895. doi: 10.1016/s0002-9149(98)00498-6. [DOI] [PubMed] [Google Scholar]
- 4.LaPar D.J., Speir A.M., Crosby I.K., Fonner E., Jr., Brown M., Rich J.B., et al. Postoperative atrial fibrillation significantly increases mortality, hospital readmission, and hospital costs. Ann Thorac Surg. 2014;98:527–533. doi: 10.1016/j.athoracsur.2014.03.039. discussion 533. [DOI] [PubMed] [Google Scholar]
- 5.Arsenault K.A., Yusuf A.M., Crystal E., Healey J.S., Morillo C.A., Nair G.M., et al. Interventions for preventing post-operative atrial fibrillation in patients undergoing heart surgery. Cochrane Database Syst Rev. 2013;1:CD003611. doi: 10.1002/14651858.CD003611.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.VanWormer A.M., Lindquist R., Sendelbach S.E. The effects of acupuncture on cardiac arrhythmias: a literature review. Heart Lung. 2008;37:425–431. doi: 10.1016/j.hrtlng.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Sun Y., Gan T.J., Dubose J.W., Habib A.S. Acupuncture and related techniques for postoperative pain: a systematic review of randomized controlled trials. Br J Anaesth. 2008;101:151–160. doi: 10.1093/bja/aen146. [DOI] [PubMed] [Google Scholar]
- 8.Coura L.E., Manoel C.H., Poffo R., Bedin A., Westphal G.A. Randomised, controlled study of preoperative electroacupuncture for postoperative pain control after cardiac surgery. Acupunct Med. 2011;29:16–20. doi: 10.1136/aim.2010.003251. [DOI] [PubMed] [Google Scholar]
- 9.Korinenko Y., Vincent A., Cutshall S.M., Li Z., Sundt T.M., III Efficacy of acupuncture in prevention of postoperative nausea in cardiac surgery patients. Ann Thorac Surg. 2009;88:537–542. doi: 10.1016/j.athoracsur.2009.04.106. [DOI] [PubMed] [Google Scholar]
- 10.Yin J., Yang M., Yu S., Fu H., Huang H., Yang B., et al. Effect of acupuncture at Neiguan point combined with amiodarone therapy on early recurrence after pulmonary vein electrical isolation in patients with persistent atrial fibrillation. J Cardiovasc Electrophysiol. 2019;30:910–917. doi: 10.1111/jce.13924. [DOI] [PubMed] [Google Scholar]
- 11.Lombardi F., Belletti S., Battezzati P.M., Lomuscio A. Acupuncture for paroxysmal and persistent atrial fibrillation: an effective non-pharmacological tool? World J Cardiol. 2012;4:60–65. doi: 10.4330/wjc.v4.i3.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lomuscio A., Belletti S., Battezzati P.M., Lombardi F. Efficacy of acupuncture in preventing atrial fibrillation recurrences after electrical cardioversion. J Cardiovasc Electrophysiol. 2011;22:241–247. doi: 10.1111/j.1540-8167.2010.01878.x. [DOI] [PubMed] [Google Scholar]
- 13.Li Y., Barajas-Martinez H., Li B., Gao Y., Zhang Z., Shang H., et al. Comparative effectiveness of acupuncture and antiarrhythmic drugs for the prevention of cardiac arrhythmias: a systematic review and meta-analysis of randomized controlled trials. Front Physiol. 2017;8:358. doi: 10.3389/fphys.2017.00358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang F., Yu X., Xiao H. Cardioprotection of electroacupuncture for enhanced recovery after surgery on patients undergoing heart valve replacement with cardiopulmonary bypass: a randomized control clinical trial. Evid Based Complement Alternat Med. 2017;2017:6243630. doi: 10.1155/2017/6243630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maimer A., Remppis A., Sack F.U., Ringes-Lichtenberg S., Greten T., Brazkiewicz F., et al. Objectifying acupuncture effects by lung function and numeric rating scale in patients undergoing heart surgery. Evid Based Complement Alternat Med. 2013;2013:219817. doi: 10.1155/2013/219817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou J., Chi H., Cheng T.O., Chen T.Y., Wu Y.Y., Zhou W.X., et al. Acupuncture anesthesia for open heart surgery in contemporary China. Int J Cardiol. 2011;150:12–16. doi: 10.1016/j.ijcard.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Yoo J.E., Oh D.S. Potential benefits of acupuncture for enhanced recovery in gynaecological surgery. Forsch Komplementmed. 2015;22:111–116. doi: 10.1159/000381360. [DOI] [PubMed] [Google Scholar]
- 18.Mehling W.E., Jacobs B., Acree M., Wilson L., Bostrom A., West J., et al. Symptom management with massage and acupuncture in postoperative cancer patients: a randomized controlled trial. J Pain Symptom Manage. 2007;33:258–266. doi: 10.1016/j.jpainsymman.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Ben-Arye E., Segev Y., Galil G., Marom I., Gressel O., Stein N., et al. Acupuncture during gynecological oncology surgery: a randomized controlled trial assessing the impact of integrative therapies on perioperative pain and anxiety. Cancer. 2023;129:908–919. doi: 10.1002/cncr.34542. [DOI] [PubMed] [Google Scholar]
- 20.Paterson C., Dieppe P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ. 2005;330:1202–1205. doi: 10.1136/bmj.330.7501.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]