Abstract
Volumetric Computed Tomography Dose Index () is an important dose descriptor to reconstruct organ doses for patients combined with the organ dose calculated from computational human phantoms coupled with Monte Carlo transport techniques. can be derived from weighted CTDI () normalized to the tube current-time product (mGy/100mAs), using knowledge of tube current-time product (mAs), tube potential (kVp), type of CTDI phantoms (head or body), and pitch. The normalized is one of the characteristics of CT scanner but not readily available from the literature. In the current study, we established a comprehensive database of normalized values based on multiple data sources: the ImPACT Dose Survey from the United Kingdom, the CT-Expo dose calculation program, and surveys performed by the US Food and Drug Administration (FDA) and the National Lung Screening Trial (NLST). From the sources, the values for a total of 68, 138, 30, and 13 scanner model groups were collected, respectively. The different scanner groups from the four data sources were sorted and merged into 162 scanner groups for 8 manufacturers including General Electric (GE), Siemens, Philips, Toshiba, Elscint, Picker, Shimadzu, and Hitachi. To fill in missing CTDI values, a method based on exponential regression analysis was developed based on the existing data. Once the database was completed, two different analyses of data variability were performed. First, we averaged CTDI values for each scanner in the different data sources and analyzed the variability of the average CTDI values across the different scanner models within a given manufacturer. Among the four major manufacturers, Toshiba and Philips showed the greatest coefficient of variation (COV) (= standard deviation / mean) for the head and body normalized values, 39% and 54%, respectively. Second, the variation across the different data sources was analyzed for CT scanners where more than two data sources were involved. The CTDI values for the scanners from Siemens showed the greatest variation across the data sources, being about 4 times greater than the variation of Toshiba scanners. The established CTDI database will be used for the reconstruction of and then the estimation of individualized organ doses for retrospective patient cohorts in epidemiologic studies.
Keywords: Computed tomography dose index, CT dose survey, dose reconstruction
1. INTRODUCTION
Individualized organ dose estimation is required for epidemiologic studies to accurately analyze the risk of late effects from radiation exposure for patients undergoing computed tomography (CT) examinations. Organ dose is usually calculated from a comprehensive Monte Carlo transport simulation where computational human phantoms and CT scanner models are incorporated. Organ dose varies depending on parameters associated with both patient anatomy and CT scanners. Several studies have revealed that there is considerable variation among CT scanners, demonstrated by the variation of volumetric CT dose index () which represents X-ray output from a CT scanner (Cody et al 2010; Lee et al 2011; Turner et al 2010). It is reported that can be used as a normalization factor to produce scanner-independent organ doses which in turn can be used as a multiplying factor for given CT scanners to readily obtain scanner-specific organ dose. Therefore, is one of the key parameters which have been used in organ dose calculation for epidemiologic studies of patients undergoing CT examinations (Berrington de Gonzalez et al 2009; de González et al 2008; Kim et al 2012; Kim et al 2009; Pearce et al 2012).
The normalized is derived from the measurements of using a 100 mm-long pencil ionization chamber inserted in the central and in the four peripheral holes of cylindrical solid phantoms made of Poly Methyl Methacrylate (PMMA) with diameters of 16 cm and 32 cm representing the head and the body of a patient, respectively (McNitt-Gray 2002). Each dose measurement for a given tube potential (kVp) is conducted for a single axial rotation perpendicular to and at mid-length of the cylinder and ion chamber. The normalized (mGy/100mAs) is calculated using the following formula:
| (1) |
where is the dose measured per 100 mAs at the center of the CTDI phantom and is the average dose per 100 mAs from the four measurements conducted at the periphery of the phantoms.
The volumetric CTDI, (mGy) is then derived from the normalized :
| (2) |
where is tube current (mA) and is a single rotation time (s).
Although is readily obtained from the CT dose sheet or the Digital Imaging and Communication in Medicine (DICOM) header in modern CT examinations, the value is rarely available for patients who received CT scans decades ago, who are commonly the target patient cohort in retrospective cohort-based epidemiologic studies (Pearce et al. 2012). The assessment of is not generally feasible when the CT scanners of interest are no longer available. The must be reconstructed using technical parameters reported in the literature and survey reports. For that purpose, normalized for all CT scanners used in the patient cohort is required together with the values of tube current-time product (mAs), tube potential (kVp), pitch, and CTDI phantom type (head or body) as described in Eq. (2). Whereas other technical parameters vary on a case by case basis, the normalized is one of the scanner-specific characteristics. Although some data is available on scanner manuals and publications, the values or the manuals themselves tend to be scattered and not easy to collect.
The current study compiled the normalized for different scanner models, tube potentials, and CTDI phantoms from several different resources and to establish a comprehensive data matrix which can form the basis of organ dose reconstruction for retrospective epidemiologic studies. Because the CTDI values were not available for all tube potentials, a method to derive missing values was developed through regression analysis based on existing CTDI values. The variation of the normalized across the different scanner models within a given manufacturer as well as across the different data sources was analyzed. Average values over the multiple data sources were calculated for different scanner models from multiple scanner manufacturers with four tube potentials and are presented in table format.
2. MATERIALS AND METHODS
2.1. Sources of normalized data
The normalized values were obtained from four different data sources: the ImPACT Dose Survey, CT-Expo software, and two CT dose surveys performed independently by the US Food and Drug Administration (FDA) and the National Lung Screening Trial (NLST).
The Excel spreadsheet titled “ImPACT Dose Survey CTDI Results, 2000-2004 ImPACT Group” was downloaded from the website (ImPACT Web site Accessed June 20, 2013). The spreadsheet contains , , and normalized by 100 mAs for different tube potentials ranging from 80 to 140 kVp. The dose survey covers a total of 68 CT scanner models from 7 different manufacturers including GE, Philips, Siemens, Toshiba, Elscint, Picker, and Shimadzu. We calculated the normalized (mGy/100 mAs) from and .
Another set of the normalized was calculated from CT-Expo version 2.1 software package (Stamm and Nagel 2002). CT-Expo provides the data collected in the German survey on CT practice in 1999 and provides, among other parameters, when the user selects a category for patient age (baby, child, or adult), gender, scan range, scanner manufacturer and model, and scanner parameters such as mAs, kVp, and pitch. We calculated the normalized for a total of 138 CT scanners from 8 manufacturers (GE, Philips, Siemens, Toshiba, Elscint, Picker, Shimadzu, and Hitachi) by entering the parameters required by the software. The CTDI phantom (head or body) was automatically selected based on the scan coverage in the adult computational phantoms.
The NEXT survey was conducted by the US FDA from 2000 to 2001 across the US (Stern 2007). The report provides the mean normalized and values (mGy/100 mAs) for a total of 30 different CT scanner models from 6 manufacturers (GE, Philips, Siemens, Toshiba, Elscint, and Picker). The CTDI values were measured only using the CTDI head phantom in more than 200 CT scanners across the country for tube potentials between 120 and 140 kVp. The NEXT survey grouped scanner models into the categories based on those provided by the ImPACT Dose Survey. The normalized was calculated from the and .
The medical physics working group of the NLST published the normalized values (mGy/mAs) based on 247 measurements on 96 CT scanners from hospitals involved in the trial during 2002 – 2007 (Cody et al 2010). The normalized values measured only from CTDI body phantom and for the tube potential of 120 kVp are available in the publication for 13 CT scanner models from 4 manufacturers (GE, Philips, Siemens, and Toshiba). The normalized data (mGy/mAs) was entered into our database after multiplying 100 to convert to mGy/100mAs.
From the four data sources, the normalized for the collimation width of 10 mm were collected for four different tube potentials (80, 100, 120, and 140 kVp) and for the eight manufacturers: GE, Philips, Siemens, Toshiba, Elscint, Picker, Shimadzu, and Hitachi. Each survey presented the data by grouping the scanner models differently. The normalized for a total of 68, 138, 30, and 13 scanner model groups were collected from ImPACT dose survey, CT-Expo software, NEXT survey, and NLST survey, respectively.
2.2. Data merging
Once we collected the normalized values for head and body CTDI phantoms for tube potentials ranging from 80 to 140 kVp from the four different data sources, we merged the values to establish a single comprehensive database. The simplest case was that each data source provided a CTDI value for a given CT scanner using the same CT scanner name. For example, the same model group, “GE 9800 Series”, was found in both the ImPACT Dose Survey and the CT-Expo program. Two sets of CTDI values were collected from each data source and average values were calculated for the merged database.
However, in most cases, different data sources do not group CT scanners in the same way. For example, the ImPACT Dose Survey spreadsheet provides one particular set of normalized values for the group of scanner models named “GE HighSpeed FX/i, LX/i” and another set of values for the group of models named “GE HighSpeed ZX/i, NX/i.” The CT-Expo program grouped scanners differently, assigning identical sets of CTDI values to two different categories, “GE HighSpeed DX/i, FX/i, LX/i, ZX/i” and “GE HighSpeed NX/i, -Pro.” The NEXT survey has two different scanner groups, “GE FX/i, LX/i” and “DX/i”. If we kept all scanner groups in the final database, then it would be confusing to assign proper CTDI values when a given scanner is “GE HighSpeed NX/i,” for example, because the model is listed in different groupings of scanners with different CTDI values.
To reduce the problem, the group category in each data source was broken into single scanner model. The CTDI value for each scanner model was collected from different sources. If multiple sources provide different CTDI values, average CTDI was calculated. Then the scanners showing identical CTDI values were regrouped into a new category with a single set of CTDI values in the final database. The merging process is described in Table 1.
Table 1.
An example of the procedure to merge different scanner model groups from different data sources for CT scanners manufactured by GE.
| ImPACT | CT-Expo | NEXT | Break Down | Final Database | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model Group |
CTDI1 | Model Group | CTDI | Model Group |
CTDI | Model | CTDI | Model Group |
CTDI | |||
| ImPACT | CT-Expo | NEXT | Average | |||||||||
| FX/i, LX/i | 18.9 | DX/i, FX/i, LX/i, ZX/i | 15.2 | FX/i, LX/i | 20.9 | FX/i | 18.9 | 15.2 | 20.9 | 18.3 | FX/i, LX/i | 18.3 |
| ZX/i, NX/i | 14.7 | NX/i, -Pro | 15.2 | DX/i | 13.2 | LX/i | 18.9 | 15.2 | 20.9 | 18.3 | ZX/i, NX/i | 14.9 |
| ZX/i | 14.7 | 15.2 | 14.9 | DX/i | 14.2 | |||||||
| NX/i | 14.7 | 15.2 | 14.9 | -Pro | 15.2 | |||||||
| DX/i | 15.2 | 13.2 | 14.2 | |||||||||
| -Pro | 15.2 | 15.2 | ||||||||||
Normalized CTDIw only for head phantom and the tube potential of 120 kVp was included for illustrative purpose.
2.3. Missing values
Since some data sources provided the normalized values for limited tube potentials and only for either the head or body CTDI phantom, exponential regression models were developed between the tube potentials and CTDI values for GE, Philips, Siemens, Toshiba, Shimadzu, and Elscint. The database for the manufacturers, Picker and Hitachi, did not contain any missing values. CTDI values for scanner models where all head and body CTDI values are available for the four tube potentials (80, 100, 120, and 140 kVp) were selected and used in the regression analysis, using MATLAB™. An exponential model as defined by
| (3) |
where is tube potential and is the normalized CTDIw, was fitted to the data by least squares. Based on the analysis, the missing CTDI were calculated using the available values and the tube potentials for the missing values.
2.4. Analysis of CTDI variability
To understand the variability of the normalized values, we analyzed the final database where the merging process and the calculation of missing values were completed. First, we analyzed the variability among scanner models in a single manufacturer. We picked the normalized values for head and body CTDI phantoms for 120 kVp and calculated the mean, standard deviation, and coefficient of variation (COV) across the different scanner models for the four major scanner manufacturers: GE, Philips, Siemens, and Toshiba. Manufacturers such as Picker, Elscint, Shimadzu, and Hitachi, which contributed less than 10 CT scanner models to the final merged data matrix, were excluded from the analysis. Second, we analyzed the variability across the four different data sources. Scanner models with the normalized values for head and body phantoms from more than two sources were included in the analysis to allow the investigation of the inter-source variation. Like the first analysis, only four major manufacturers, GE, Philips, Siemens, and Toshiba, were included in the analysis. The mean, standard deviation, and COV of the normalized values for the head and body CTDI phantoms for 120 kVp were calculated and analyzed.
3. RESULTS AND DISCUSSION
3.1. Data collection
The normalized values were collected or calculated from the four data sources: ImPACT Dose Survey, CT-Expo program, and NEXT and NLST surveys. The number of CT scanner groups abstracted from the four data sources are summarized in Table 2. Through the merging process described in Table 1, a total of 249 original categories were regrouped into 162 categories. CT-Expo program contributed the greatest number of CT scanner groups (n=138) compared to the NLST survey where 13 scanner groups were available. The NEXT and NLST surveys only provided head and body CTDI values, respectively, whereas the ImPACT Dose Survey and CT-Expo program provided both head and body CTDI values.
Table 2.
The number of CT scanner group for eight different manufacturers collected from the four data sources. The number of CT scanner models after data merging is included in the final column.
| Manufacturer | ImPACT | CT-Expo | NEXT | NLST | Merged |
|---|---|---|---|---|---|
| GE | 17 | 27 | 10 | 5 | 27 |
| Philips | 13 | 17 | 2 | 3 | 25 |
| Siemens | 16 | 35 | 3 | 3 | 38 |
| Toshiba | 16 | 34 | 8 | 2 | 42 |
| Elscint | 2 | 7 | 5 | 10 | |
| Picker | 3 | 7 | 2 | 9 | |
| Shimadzu | 1 | 6 | 6 | ||
| Hitachi | 5 | 5 | |||
| Total | 68 | 138 | 30 | 13 | 162 |
3.2. Missing values
To calculate missing CTDI values, an exponential regression model (as in Eq. (3)) was used, applied to the CT scanner groups where the CTDI values are available for all tube potentials considered in this study, namely 80, 100, 120, and 140 kVp. The calculation was only performed for manufacturers apart from Picker and Hitachi that did not contain any missing values. Figure 1 shows an example of the exponential regression analysis for (a) GE LightSpeed VCT and (b) GE Discovery CT HD750 for head/body CTDI phantoms and the tube potential of 80 – 140 kVp. Although the two scanners are from the same manufacturer, the parameter shown in Eq. (3) of the exponential regression curve is significantly different: 1.8 and 1.3 for head phantom in LightSpeed VCT and Discovery CT HD750, respectively. However, the parameter shown in Eq. (3) for the head phantom is identical, 0.0217, and the values for body phantom are very close, 0.0225 and 0.0230. Based on the observation, the average and standard deviation of the parameter for head and body CTDI values were calculated across the different scanner models in six manufacturers to obtain representative values of the parameter . Since at least one CTDI value is available (mostly for 120 kVp), the representative parameter was then used to derive other CTDI values by using Eq. (3) and the available CTDI values for 120 kVp.
Figure 1.

Examples of the exponential regression analysis for (a) GE LightSpeed VCT and (b) GE Discovery CT HD750 scanners.
The mean and standard deviation of the parameter for head and body CTDI values were calculated across the different scanner models in six manufacturers to obtain the representative parameters (Table 3). To investigate if the parameters differ by manufacturer, or by phantom body part (head vs body), we fitted linear models to this data on fitted exponential parameters, in which;
| (4) |
Table 3.
Average and standard deviation of the parameter B of the exponential regression model for of head and body phantoms and for different manufacturers.
| Manufacturer | GE | Philips | Siemens | Toshiba | Elscint | Picker | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | Average | SD | Average | SD | Average | SD | |
| CTDIw Head | 0.0197 | 0.0013 | 0.0216 | 0.0018 | 0.0219 | 0.0022 | 0.0206 | 0.0009 | 0.0199 | 0.0003 | 0.0185 | 0.0015 |
| CTDIw Body | 0.0212 | 0.0013 | 0.0226 | 0.0016 | 0.0230 | 0.0015 | 0.0218 | 0.0007 | 0.0216 | 0.0011 | 0.0196 | 0.0021 |
Analysis of variance was assessed in the standard way using the F-test (Rao 2002). Table 4 demonstrates that all possible comparisons (of manufacturer within each CTDI phantom and across CTDI phantom types, and CTDI phantoms adjusted for manufacturer) were highly statistically significant (p<0.0001). This was also the case when the slope parameters were log-transformed (results not shown). Based on the results, we decided to use a different parameter for each manufacturer and CTDI phantom type.
Table 4.
Analysis of variance decomposition of fitted slope parameters B from model described in Eq. (4).
| Data (phantom body part) | Test for difference by category | p-value (via F-test) |
|---|---|---|
| Head only | Manufacturer | <0.0001 |
| Body only | Manufacturer | <0.0001 |
| Head & body | Manufacturer | <0.0001 |
| Head & body | Manufacturer adjusted for phantom body part | <0.0001 |
| Head & body | Phantom body part adjusted for manufacturer | <0.0001 |
When a given scanner had missing CTDI values, the following equation was used to derive the parameter in Eq. (3).
| (5) |
where is the normalized for 120 kVp (always available), is the reference parameter derived from the average and standard deviation across different scanner models, and 120 kVp is the tube potential for which CTDI value is already available. Once the parameters and were obtained for a given scanner and 120 kVp, missing CTDI values were calculated using the following equation for other tube potentials which is rewritten from Eq. (3):
| (6) |
where is the tube potential for which CTDI values are missing. No calculation was attempted when CTDI values for all tube potentials were not available (e.g., only CTDI head values were available for Philips Tomoscan TX). The approach may be utilized when CTDI values for limited tube potentials are available but the values for additional tube potentials are needed.
3.3. Final database of normalized
After merging data from the four data sources and completing the calculation of missing CTDI values, the final database containing the normalized CTDIw (mGy/100mAs) for 162 scanner groups was established and tabulated in Table 5. The CTDI values for the tube potential of 80, 100, 120, and 140 kVp and for the head and body CTDI phantoms were tabulated. The values in italic and bold were originally missing, but derived using the method described in section 3.2. Standard deviation (SD) is included next to the columns of CTDI values, but not available if data point is only one or the CTDI values are derived. The database spans eight manufacturers: GE, Philips, Siemens, Toshiba, Elscint, Picker, Shimadzu, and Hitachi. The number of CT scanner models covered by the final database is summarized in the final column of Table 2.
Table 5.
Normalized CTDIw (mGy/100mAs) for head and body CTDI phantoms and for the tube potentials of 80, 100, 120, and 140 kVp categorized into manufacturers and models. The values in italic and bold were originally missing, but derived using the fitting equation. Standard deviation (SD) is included next to the columns of CTDI values, but not available if data point is only one or the CTDI values are derived.
| Make | Model | kVp | CTDI H | SD | CTDI B | SD | Make | Scanner Model | kVp | CTDI H | SD | CTDI B | SD | Make | Scanner Model | kVp | CTDI H | SD | CTDI B | SD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GE | 8800, 9000 Series | 80 | 2.82 | 1.79 | HiSpeed DX/I | 80 | 5.08 | 2.27 | LightSpeed VFX Plus, Ultra | 80 | 7.82 | 3.54 | ||||||||
| 100 | 4.19 | 2.73 | 100 | 9.61 | 4.41 | 100 | 13.57 | 6.65 | ||||||||||||
| 120 | 6.21 | 3.51 | 120 | 14.20 | 1.41 | 7.20 | 120 | 20.57 | 10.63 | |||||||||||
| 140 | 9.22 | 6.37 | 140 | 20.42 | 1.03 | 10.35 | 140 | 28.34 | 15.09 | |||||||||||
| 9800 Series | 80 | 6.49 | 2.76 | HiSpeed-Pro | 80 | 5.08 | 2.27 | LightSpeed VFX 16 | 80 | 7.82 | 3.54 | |||||||||
| 100 | 10.14 | 4.31 | 100 | 9.61 | 4.41 | 100 | 13.57 | 6.65 | ||||||||||||
| 120 | 13.57 | 1.81 | 6.22 | 0.03 | 120 | 15.20 | 7.20 | 120 | 20.57 | 10.63 | ||||||||||
| 140 | 18.98 | 1.47 | 8.48 | 0.06 | 140 | 21.15 | 10.35 | 140 | 28.34 | 15.09 | ||||||||||
| BrightSpeed 4, 8, 16 | 80 | 7.82 | 3.54 | LightSpeed 16 | 80 | 7.62 | 0.28 | 3.33 | 0.29 | Max | 80 | 8.00 | 3.33 | |||||||
| 100 | 13.57 | 6.65 | 100 | 13.57 | 0.01 | 6.73 | 0.10 | 100 | 12.50 | 5.21 | ||||||||||
| 120 | 20.57 | 10.63 | 120 | 20.74 | 0.24 | 10.40 | 1.30 | 120 | 18.01 | 0.02 | 7.50 | |||||||||
| 140 | 28.34 | 15.09 | 140 | 28.78 | 0.63 | 15.54 | 0.65 | 140 | 24.50 | 10.21 | ||||||||||
| Discovery CT HD750 | 80 | 7.27 | 3.54 | LightSpeed Pro 16 | 80 | 7.85 | 0.05 | 3.43 | 0.16 | Optima 600 | 80 | 7.50 | 3.50 | |||||||
| 100 | 12.84 | 6.42 | 100 | 13.71 | 0.20 | 6.48 | 0.25 | 100 | 13.24 | 6.34 | ||||||||||
| 120 | 19.59 | 10.04 | 120 | 20.70 | 0.17 | 10.29 | 0.48 | 120 | 20.20 | 9.92 | ||||||||||
| 140 | 26.93 | 14.11 | 140 | 28.50 | 0.24 | 14.60 | 0.69 | 140 | 27.76 | 13.94 | ||||||||||
| HiLight Advantage | 80 | 4.25 | 1.85 | LightSpeed, QX/I, Plus | 80 | 7.64 | 0.25 | 3.40 | 0.19 | Pace, Sytec | 80 | 9.41 | 0.14 | 4.32 | 0.21 | |||||
| 100 | 7.42 | 3.23 | 100 | 13.56 | 0.01 | 6.49 | 0.23 | 100 | 15.53 | 7.30 | ||||||||||
| 120 | 11.59 | 0.16 | 5.10 | 120 | 20.14 | 0.93 | 10.25 | 0.33 | 120 | 22.49 | 1.26 | 10.91 | 0.01 | |||||||
| 140 | 17.24 | 0.06 | 7.50 | 140 | 26.03 | 4.46 | 14.79 | 0.42 | 140 | 32.55 | 0.02 | 15.41 | 0.16 | |||||||
| HiLight, HiSpeed CT/i (no SmartBeam) | 80 | 4.32 | 0.11 | 1.73 | 0.18 | LightSpeed RT | 80 | 7.59 | 0.02 | 3.36 | 0.02 | ProSpeed Series | 80 | 9.64 | 4.04 | |||||
| 100 | 7.84 | 0.60 | 3.42 | 0.26 | 100 | 13.20 | 0.01 | 6.31 | 0.01 | 100 | 15.07 | 6.32 | ||||||||
| 120 | 11.93 | 0.35 | 5.13 | 0.04 | 120 | 19.90 | 0.15 | 9.98 | 0.11 | 120 | 21.94 | 0.37 | 9.43 | 0.47 | ||||||
| 140 | 17.05 | 0.17 | 7.54 | 0.06 | 140 | 28.01 | 0.63 | 14.49 | 0.29 | 140 | 28.82 | 1.25 | 12.88 | 0.69 | ||||||
| HiSpeed CT/e (dual) | 80 | 5.15 | 2.27 | LightSpeed Ultra | 80 | 7.94 | 0.18 | 3.56 | 0.03 | Philips | AcQSim | 80 | 9.16 | 5.34 | ||||||
| 100 | 9.73 | 4.41 | 100 | 14.10 | 0.75 | 6.80 | 0.21 | 100 | 14.12 | 8.40 | ||||||||||
| 120 | 15.40 | 7.20 | 120 | 21.49 | 1.30 | 10.71 | 0.76 | 120 | 17.32 | 9.36 | ||||||||||
| 140 | 21.43 | 10.35 | 140 | 29.75 | 2.00 | 15.50 | 0.58 | 140 | 33.56 | 20.72 | ||||||||||
| HiSpeed FX/i, LX/i | 80 | 6.41 | 1.88 | 2.78 | 0.73 | LightSpeed VCT | 80 | 9.77 | 0.53 | 4.08 | 0.20 | Aura | 80 | 9.84 | 4.35 | |||||
| 100 | 9.61 | 4.41 | 100 | 17.30 | 0.88 | 7.42 | 0.34 | 100 | 16.44 | 7.61 | ||||||||||
| 120 | 18.34 | 2.90 | 7.83 | 0.89 | 120 | 26.30 | 1.45 | 10.68 | 1.53 | 120 | 24.63 | 0.52 | 11.98 | 0.03 | ||||||
| 140 | 22.47 | 2.56 | 11.01 | 0.93 | 140 | 36.14 | 2.02 | 16.18 | 0.92 | 140 | 35.64 | 17.64 | ||||||||
| HiSpeed CT/i (SmartBeam) | 80 | 4.32 | 0.11 | 2.19 | 0.03 | LightSpeed VCT Series (small BF) | 80 | 8.62 | 5.55 | Brilliance 40/64 | 80 | 4.88 | 2.20 | |||||||
| 100 | 7.84 | 0.60 | 4.22 | 0.49 | 100 | 15.34 | 8.47 | 100 | 9.61 | 4.71 | ||||||||||
| 120 | 12.22 | 0.85 | 6.14 | 0.05 | 120 | 23.37 | 1.32 | 10.87 | 120 | 16.18 | 0.38 | 7.86 | 0.75 | |||||||
| 140 | 17.99 | 1.47 | 8.99 | 0.04 | 140 | 32.25 | 19.77 | 140 | 23.72 | 0.60 | 12.51 | 0.07 | ||||||||
| HiSpeed ZX/i, NX/i | 80 | 4.99 | 0.13 | 2.18 | 0.13 | LightSpeed VCT Series (medium BF) | 80 | 10.15 | 4.22 | Brilliance Big Bore | 80 | 3.81 | 1.83 | |||||||
| 100 | 9.61 | 4.41 | 100 | 17.91 | 7.66 | 100 | 7.24 | 3.65 | ||||||||||||
| 120 | 14.94 | 0.36 | 6.91 | 0.41 | 120 | 27.33 | 11.97 | 120 | 11.23 | 0.78 | 5.99 | 0.02 | ||||||||
| 140 | 20.80 | 0.49 | 9.93 | 0.60 | 140 | 37.56 | 16.83 | 140 | 16.32 | 1.20 | 8.71 | 0.11 | ||||||||
| HiSpeed Advantage | 80 | 4.25 | 1.85 | LightSpeed VCT Series (large BF) | 80 | 8.62 | 3.84 | Brilliance iCT SP (adult) | 80 | 5.04 | 2.43 | |||||||||
| 100 | 7.42 | 3.23 | 100 | 15.34 | 7.17 | 100 | 10.06 | 5.19 | ||||||||||||
| 120 | 12.02 | 0.45 | 5.10 | 120 | 23.37 | 1.32 | 11.30 | 0.61 | 120 | 16.82 | 9.05 | |||||||||
| 140 | 17.04 | 0.23 | 7.50 | 140 | 32.25 | 16.03 | 140 | 24.74 | 13.65 | |||||||||||
| Brilliance iCTSP (infant < 18 months) | 80 | 6.34 | Tomoscan 310, 350 (GE2, Cu) | 80 | 6.06 | Somatom AR series | 80 | 7.90 | 4.28 | |||||||||||
| 100 | 12.26 | 100 | 9.34 | 100 | 13.80 | 7.47 | ||||||||||||||
| 120 | 19.93 | 120 | 11.45 | 120 | 21.78 | 11.79 | ||||||||||||||
| 140 | 28.64 | 140 | 22.18 | 140 | 32.01 | 17.33 | ||||||||||||||
| Brilliance iCTSP (trauma/bariatric) | 80 | 8.38 | 5.55 | Tomoscan 310, 350 (GE3, no Cu) | 80 | 4.69 | Somatom Balance, Emotion (> 2000) | 80 | 6.84 | 3.25 | ||||||||||
| 100 | 15.15 | 10.58 | 100 | 7.36 | 100 | 12.62 | 6.29 | |||||||||||||
| 120 | 22.75 | 16.39 | 120 | 8.21 | 120 | 19.98 | 10.31 | |||||||||||||
| 140 | 29.86 | 21.84 | 140 | 18.17 | 140 | 28.40 | 15.02 | |||||||||||||
| MX 16 | 80 | 4.85 | 2.36 | Tomoscan AV Series, LX, SR Series | 80 | 4.50 | 2.33 | 2.85 | 0.07 | Somatom Classic | 80 | 3.93 | 2.15 | |||||||
| 100 | 9.23 | 4.70 | 100 | 9.71 | 0.47 | 4.88 | 0.28 | 100 | 6.43 | 3.68 | ||||||||||
| 120 | 15.02 | 7.74 | 120 | 14.48 | 0.48 | 7.72 | 0.39 | 120 | 9.60 | 5.70 | ||||||||||
| 140 | 21.88 | 11.13 | 140 | 20.46 | 0.84 | 11.05 | 1.00 | 140 | 13.48 | 8.25 | ||||||||||
| MX 4000, MX 6000 | 80 | 3.64 | 1.81 | Tomoscan CX, CX/S | 80 | 7.93 | 3.59 | Somatom CR | 80 | 4.26 | 2.85 | |||||||||
| 100 | 7.00 | 3.63 | 100 | 12.22 | 5.64 | 100 | 7.12 | 4.98 | ||||||||||||
| 120 | 11.50 | 6.10 | 120 | 14.99 | 6.29 | 120 | 10.83 | 7.86 | ||||||||||||
| 140 | 16.88 | 9.02 | 140 | 29.05 | 13.91 | 140 | 15.44 | 11.55 | ||||||||||||
| MX 4000 Dual, MX 6000 Dual | 80 | 3.82 | 1.90 | Tomoscan M/EG | 80 | 14.75 | 9.07 | Somatom Definition 64 (wide BF) | 80 | 6.25 | 2.90 | |||||||||
| 100 | 7.34 | 3.81 | 100 | 24.10 | 15.85 | 100 | 10.91 | 5.07 | ||||||||||||
| 120 | 12.05 | 6.39 | 120 | 38.87 | 4.05 | 27.42 | 3.42 | 120 | 17.21 | 7.99 | ||||||||||
| 140 | 17.68 | 9.45 | 140 | 50.53 | 36.75 | 140 | 25.30 | 11.75 | ||||||||||||
| MX 8000 Dual | 80 | 4.31 | 2.06 | Tomoscan TX | 80 | 2.86 | Somatom Definition 64 (narrow BF) | 80 | 5.53 | 2.36 | ||||||||||
| 100 | 8.29 | 4.12 | 100 | 4.40 | 100 | 9.66 | 4.13 | |||||||||||||
| 120 | 13.62 | 6.91 | 120 | 5.40 | 120 | 15.24 | 6.52 | |||||||||||||
| 140 | 19.99 | 10.22 | 140 | 10.46 | 140 | 22.41 | 9.58 | |||||||||||||
| MX 8000 Quad | 80 | 4.44 | 2.15 | Tomoscan X Series | 80 | 6.15 | 2.90 | Somatom Definition AS | 80 | 4.00 | 0.68 | 1.86 | 0.36 | |||||||
| 100 | 8.54 | 4.30 | 100 | 10.04 | 5.07 | 100 | 7.96 | 1.46 | 3.78 | 0.74 | ||||||||||
| 120 | 14.02 | 7.61 | 120 | 15.00 | 8.00 | 120 | 13.33 | 2.36 | 6.44 | 1.20 | ||||||||||
| 140 | 20.57 | 10.68 | 140 | 21.06 | 11.76 | 140 | 19.54 | 3.52 | 9.56 | 1.77 | ||||||||||
| MX 8000 IDT 6/10, Brilliance 6/10 | 80 | 4.55 | 2.21 | SR4000 | 80 | 6.97 | 3.70 | Somatom Definition DS (tube A) | 80 | 4.82 | 2.15 | |||||||||
| 100 | 8.65 | 4.40 | 100 | 10.74 | 5.81 | 100 | 10.08 | 4.58 | ||||||||||||
| 120 | 14.07 | 7.25 | 120 | 13.18 | 6.48 | 120 | 17.21 | 7.99 | ||||||||||||
| 140 | 20.49 | 10.43 | 140 | 25.53 | 14.33 | 140 | 25.41 | 12.06 | ||||||||||||
| Marconi MX 8000 IDT, Brilliance 16 | 80 | 4.85 | 2.36 | SR 5000 | 80 | 6.67 | 3.60 | Somatom Definition DS (tube A+B) | 80 | 4.55 | 1.95 | |||||||||
| 100 | 9.23 | 4.70 | 100 | 10.29 | 5.66 | 100 | 9.51 | 4.16 | ||||||||||||
| 120 | 15.29 | 0.27 | 9.21 | 2.41 | 120 | 12.62 | 6.31 | 120 | 16.23 | 7.25 | ||||||||||
| 140 | 22.24 | 0.52 | 11.24 | 0.16 | 140 | 24.45 | 13.96 | 140 | 23.95 | 10.95 | ||||||||||
| Secura | 80 | 6.15 | 2.90 | Siemens | DXP | 80 | 5.61 | 3.37 | Somatom Definition DS (cardiac) | 80 | 4.55 | 1.95 | ||||||||
| 100 | 10.04 | 5.07 | 100 | 8.70 | 5.33 | 100 | 9.51 | 4.16 | ||||||||||||
| 120 | 14.63 | 0.53 | 7.79 | 0.29 | 120 | 10.36 | 5.72 | 120 | 16.23 | 7.25 | ||||||||||
| 140 | 20.68 | 0.53 | 11.38 | 0.54 | 140 | 20.93 | 13.35 | 140 | 23.95 | 10.95 | ||||||||||
| Tomoscan 310, 350 (GE2, no Cu) | 80 | 10.77 | Somatom 2 | 80 | 3.48 | 2.33 | Somatom Definition Flash (tube A) | 80 | 5.15 | 2.30 | ||||||||||
| 100 | 16.61 | 100 | 5.81 | 4.06 | 100 | 10.77 | 4.91 | |||||||||||||
| 120 | 20.37 | 120 | 8.83 | 6.41 | 120 | 18.38 | 8.56 | |||||||||||||
| 140 | 39.46 | 140 | 12.59 | 9.43 | 140 | 27.14 | 12.92 | |||||||||||||
| Somatom Definition Flash (tube A+B) | 80 | 5.15 | 2.78 | Somatom Plus | 80 | 3.93 | 2.15 | Somatom Spirit | 80 | 5.29 | 2.24 | |||||||||
| 100 | 10.77 | 5.93 | 100 | 6.43 | 3.68 | 100 | 9.87 | 4.42 | ||||||||||||
| 120 | 18.38 | 10.35 | 120 | 10.03 | 0.39 | 5.71 | 0.02 | 120 | 15.77 | 7.38 | ||||||||||
| 140 | 27.14 | 15.61 | 140 | 13.48 | 8.25 | 140 | 22.59 | 10.93 | ||||||||||||
| Somatom Definition Flash (cardiac) | 80 | 5.15 | 1.89 | Somatom Plus 4 | 80 | 4.12 | 0.01 | 2.41 | 0.09 | Somatom Volume Access | 80 | 7.80 | 0.28 | 2.73 | 0.13 | |||||
| 100 | 10.77 | 4.04 | 100 | 8.71 | 5.00 | 100 | 13.74 | 5.32 | ||||||||||||
| 120 | 18.38 | 7.04 | 120 | 14.32 | 0.46 | 8.10 | 0.28 | 120 | 20.27 | 0.70 | 8.30 | 0.45 | ||||||||
| 140 | 27.14 | 10.62 | 140 | 20.68 | 0.04 | 11.70 | 0.38 | 140 | 28.00 | 0.96 | 12.08 | 0.69 | ||||||||
| Somatom Definition Flash (flash mode) | 80 | 5.15 | 1.89 | Somatom Plus 4 Volume Zoom | 80 | 4.11 | 2.35 | Somatom Volume Zoom | 80 | 7.96 | 0.49 | 2.79 | 0.21 | |||||||
| 100 | 10.77 | 4.04 | 100 | 14.11 | 8.33 | 100 | 14.27 | 5.52 | ||||||||||||
| 120 | 18.38 | 7.04 | 120 | 16.79 | 3.15 | 8.95 | 1.48 | 120 | 20.67 | 1.27 | 8.46 | 0.69 | ||||||||
| 140 | 27.14 | 10.62 | 140 | 24.28 | 11.43 | 140 | 28.55 | 1.74 | 12.33 | 1.03 | ||||||||||
| Somatom DR 1/2/3 | 80 | 3.48 | 2.33 | Somatom Plus-S | 80 | 3.93 | 2.15 | Toshiba | Activion 16 | 80 | 10.01 | 4.61 | ||||||||
| 100 | 5.81 | 4.06 | 100 | 6.43 | 3.68 | 100 | 16.35 | 7.88 | ||||||||||||
| 120 | 8.83 | 6.41 | 120 | 9.98 | 0.54 | 5.71 | 0.02 | 120 | 24.42 | 12.21 | ||||||||||
| 140 | 12.59 | 9.43 | 140 | 13.48 | 8.25 | 140 | 34.28 | 17.67 | ||||||||||||
| Somatom DRG | 80 | 3.65 | 2.42 | Somatom Sensation 4 | 80 | 8.12 | 0.32 | 2.74 | 0.03 | Alexion | 80 | 10.57 | 4.34 | |||||||
| 100 | 6.11 | 4.24 | 100 | 13.55 | 5.12 | 100 | 18.15 | 7.64 | ||||||||||||
| 120 | 9.29 | 6.68 | 120 | 20.55 | 0.08 | 8.34 | 0.06 | 120 | 26.82 | 11.82 | ||||||||||
| 140 | 13.24 | 9.82 | 140 | 28.29 | 0.00 | 12.03 | 0.12 | 140 | 35.59 | 16.72 | ||||||||||
| Somatom DRH | 80 | 4.26 | 2.85 | Somatom Sensation 10 | 80 | 6.85 | 0.90 | 2.31 | 0.30 | Aquilion ONE (small BF) | 80 | 15.33 | 7.27 | |||||||
| 100 | 7.12 | 4.98 | 100 | 12.11 | 1.05 | 4.52 | 0.63 | 100 | 28.11 | 14.02 | ||||||||||
| 120 | 10.83 | 7.86 | 120 | 17.38 | 2.89 | 7.24 | 1.25 | 120 | 44.34 | 22.63 | ||||||||||
| 140 | 15.44 | 11.55 | 140 | 26.83 | 10.49 | 1.64 | 140 | 62.82 | 32.15 | |||||||||||
| Somatom Emotion 16 | 80 | 7.42 | 3.21 | Somatom Sensation 16 | 80 | 7.25 | 1.33 | 2.42 | 0.44 | Aquilion ONE (medium BF) | 80 | 13.94 | 6.62 | |||||||
| 100 | 13.68 | 6.21 | 100 | 13.02 | 1.48 | 4.84 | 0.75 | 100 | 26.28 | 13.07 | ||||||||||
| 120 | 21.67 | 10.18 | 120 | 18.92 | 3.31 | 7.87 | 0.98 | 120 | 41.83 | 21.49 | ||||||||||
| 140 | 30.80 | 14.83 | 140 | 29.36 | 11.20 | 1.97 | 140 | 58.99 | 31.00 | |||||||||||
| Somatom Emotion 6 | 80 | 6.45 | 0.13 | 2.70 | 0.19 | Somatom Sensation 16 Straton | 80 | 6.75 | 2.11 | Aquilion ONE (large BF) | 80 | 13.94 | 7.26 | |||||||
| 100 | 11.72 | 5.48 | 100 | 12.28 | 4.19 | 100 | 26.28 | 14.32 | ||||||||||||
| 120 | 18.57 | 8.98 | 120 | 16.98 | 7.02 | 120 | 41.83 | 23.54 | ||||||||||||
| 140 | 26.38 | 13.08 | 140 | 34.31 | 10.30 | 140 | 58.99 | 33.97 | ||||||||||||
| Somatom Emotion Duo | 80 | 6.08 | 0.03 | 2.58 | 0.00 | Somatom Sensation 40 | 80 | 4.76 | 2.21 | Aquilion 4 | 80 | 8.88 | 0.55 | 4.87 | 0.55 | |||||
| 100 | 11.26 | 4.99 | 100 | 9.94 | 4.72 | 100 | 15.21 | 0.37 | 8.45 | 0.75 | ||||||||||
| 120 | 17.83 | 8.18 | 120 | 16.96 | 8.24 | 120 | 23.11 | 0.59 | 12.71 | 1.04 | ||||||||||
| 140 | 25.33 | 11.92 | 140 | 25.04 | 12.43 | 140 | 33.55 | 20.13 | ||||||||||||
| Somatom Esprit, Balance, Emotion | 80 | 7.67 | 3.87 | Somatom Sensation 64 | 80 | 3.95 | 0.79 | 1.80 | 0.42 | Aquilion 16 | 80 | 9.18 | 0.40 | 5.23 | 0.03 | |||||
| 100 | 14.14 | 7.48 | 100 | 8.31 | 1.57 | 3.92 | 0.78 | 100 | 15.98 | 1.11 | 9.18 | 0.28 | ||||||||
| 120 | 22.39 | 12.27 | 120 | 14.02 | 2.92 | 7.21 | 1.21 | 120 | 24.72 | 1.68 | 13.73 | 0.66 | ||||||||
| 140 | 31.81 | 17.88 | 140 | 23.74 | 10.58 | 1.69 | 140 | 34.07 | 20.13 | |||||||||||
| Somatom HiQ | 80 | 5.13 | 2.64 | Somatom Sensation Open | 80 | 6.27 | 1.22 | 2.91 | 0.76 | Aquilion 8 to 64 | 80 | 8.89 | 5.26 | |||||||
| 100 | 8.56 | 4.61 | 100 | 12.13 | 2.60 | 5.72 | 1.34 | 100 | 15.19 | 8.98 | ||||||||||
| 120 | 13.02 | 7.27 | 120 | 19.55 | 4.86 | 9.40 | 2.35 | 120 | 23.53 | 13.91 | ||||||||||
| 140 | 18.57 | 10.69 | 140 | 33.42 | 14.03 | 3.51 | 140 | 34.07 | 20.13 | |||||||||||
| Aquilion CX, CXL (medium BF) | 80 | 8.01 | 3.63 | Aquilion RX, RXL (medium BF) | 80 | 8.91 | 3.65 | TCT 900S | 80 | 5.79 | ||||||||||
| 100 | 14.80 | 6.71 | 100 | 15.69 | 6.84 | 100 | 8.73 | |||||||||||||
| 120 | 23.61 | 10.71 | 120 | 24.22 | 10.95 | 120 | 11.93 | |||||||||||||
| 140 | 33.94 | 15.39 | 140 | 34.04 | 15.71 | 140 | 19.87 | |||||||||||||
| Aquilion CX, CXL (large BF) | 80 | 9.50 | 4.71 | Aquilion RX, RXL (large BF) | 80 | 10.61 | 4.75 | Xpress GX (after 1998) | 80 | 5.31 | 2.43 | |||||||||
| 100 | 17.54 | 8.70 | 100 | 18.68 | 8.89 | 100 | 8.88 | 4.25 | ||||||||||||
| 120 | 27.99 | 13.87 | 120 | 28.84 | 14.24 | 120 | 13.50 | 6.37 | 0.46 | |||||||||||
| 140 | 40.23 | 19.94 | 140 | 40.54 | 20.42 | 140 | 19.24 | 9.85 | ||||||||||||
| Aquilion CX, CXL (DR filter) | 80 | 4.38 | 2.40 | Aquilion RX, RXL (DR filter) | 80 | 4.79 | 2.44 | Xpress GX (before 1998) | 80 | 7.24 | 2.43 | |||||||||
| 100 | 8.09 | 4.42 | 100 | 8.44 | 4.56 | 100 | 12.10 | 4.25 | ||||||||||||
| 120 | 12.90 | 7.06 | 120 | 13.02 | 7.30 | 120 | 18.14 | 0.42 | 6.70 | |||||||||||
| 140 | 18.54 | 10.15 | 140 | 18.30 | 10.47 | 140 | 26.23 | 9.85 | ||||||||||||
| Aquilion LB | 80 | 6.92 | 4.63 | Asteion | 80 | 6.55 | 3.25 | Xpress HS | 80 | 5.08 | 2.32 | |||||||||
| 100 | 11.57 | 7.90 | 100 | 9.88 | 5.03 | 100 | 8.48 | 4.06 | ||||||||||||
| 120 | 17.59 | 12.24 | 120 | 13.49 | 6.05 | 120 | 12.91 | 0.01 | 6.42 | 0.02 | ||||||||||
| 140 | 25.08 | 17.72 | 140 | 22.48 | 12.06 | 140 | 18.39 | 9.41 | ||||||||||||
| Aquilion Multi | 80 | 8.49 | 4.48 | Asteion Dual | 80 | 13.94 | 6.43 | Xpress HS1 | 80 | 8.03 | 2.61 | |||||||||
| 100 | 14.94 | 7.92 | 100 | 22.78 | 10.98 | 100 | 13.41 | 4.56 | ||||||||||||
| 120 | 22.70 | 12.22 | 120 | 31.55 | 3.49 | 15.98 | 1.45 | 120 | 20.42 | 0.02 | 7.21 | 0.02 | ||||||||
| 140 | 37.81 | 24.38 | 140 | 47.76 | 24.63 | 140 | 29.08 | 10.59 | ||||||||||||
| Aquilion Premium (small BF) | 80 | 15.53 | 7.36 | Asteion 4 (after 2002) | 80 | 11.40 | 4.96 | Xpress SX | 80 | 11.16 | ||||||||||
| 100 | 28.48 | 14.20 | 100 | 18.62 | 8.47 | 100 | 16.84 | |||||||||||||
| 120 | 44.93 | 22.93 | 120 | 27.81 | 13.11 | 120 | 23.00 | |||||||||||||
| 140 | 63.65 | 32.57 | 140 | 39.04 | 18.98 | 140 | 38.32 | |||||||||||||
| Aquilion Premium (medium BF) | 80 | 14.12 | 6.71 | Asteion Multi (CXB-400C tube) | 80 | 11.05 | 0.48 | 4.80 | 0.23 | Xpeed TSX 001A | 80 | 8.80 | ||||||||
| 100 | 26.62 | 13.24 | 100 | 18.51 | 0.15 | 8.81 | 0.49 | 100 | 13.27 | |||||||||||
| 120 | 42.38 | 21.77 | 120 | 27.66 | 0.21 | 13.03 | 0.12 | 120 | 18.13 | |||||||||||
| 140 | 59.76 | 31.41 | 140 | 39.04 | 18.98 | 140 | 30.21 | |||||||||||||
| Aquilion Premium (large BF) | 80 | 14.12 | 7.35 | Asteion Multi (before 2002) | 80 | 14.07 | 1.01 | 6.09 | 0.44 | Xpeed | 80 | 8.38 | 1.67 | |||||||
| 100 | 26.62 | 14.51 | 100 | 23.70 | 0.64 | 11.25 | 0.45 | 100 | 14.00 | 2.92 | ||||||||||
| 120 | 42.38 | 23.85 | 120 | 35.50 | 0.80 | 16.69 | 0.35 | 120 | 19.72 | 2.24 | 4.60 | |||||||||
| 140 | 59.76 | 34.42 | 140 | 50.63 | 24.51 | 140 | 30.36 | 6.76 | ||||||||||||
| Aquilion Prime (small BF) | 80 | 8.88 | 3.59 | Auklet | 80 | 7.20 | 2.36 | Xspeed II | 80 | 8.38 | 1.67 | |||||||||
| 100 | 16.54 | 7.05 | 100 | 12.03 | 4.12 | 100 | 14.00 | 2.92 | ||||||||||||
| 120 | 26.02 | 11.55 | 120 | 18.32 | 0.02 | 6.48 | 0.02 | 120 | 21.29 | 0.02 | 4.62 | 0.04 | ||||||||
| 140 | 36.24 | 16.58 | 140 | 26.09 | 9.56 | 140 | 30.36 | 6.76 | ||||||||||||
| Aquilion Prime (medium BF) | 80 | 8.21 | 3.33 | TCT 500S | 80 | 6.82 | Xvision | 80 | 6.38 | 2.36 | ||||||||||
| 100 | 15.30 | 6.54 | 100 | 10.28 | 100 | 10.65 | 4.12 | |||||||||||||
| 120 | 24.07 | 10.71 | 120 | 14.05 | 120 | 16.19 | 0.02 | 6.52 | 0.03 | |||||||||||
| 140 | 33.53 | 15.39 | 140 | 23.40 | 140 | 23.09 | 9.56 | |||||||||||||
| Aquilion Prime (large BF) | 80 | 8.21 | 3.72 | TCT 600 | 80 | 6.26 | 2.14 | Xvision EX | 80 | 7.85 | 3.52 | |||||||||
| 100 | 15.30 | 7.31 | 100 | 10.45 | 3.74 | 100 | 11.84 | 5.45 | ||||||||||||
| 120 | 24.07 | 11.97 | 120 | 14.57 | 2.28 | 5.92 | 0.03 | 120 | 16.17 | 6.55 | ||||||||||
| 140 | 33.53 | 17.18 | 140 | 22.67 | 8.67 | 140 | 26.94 | 13.06 | ||||||||||||
| Xvision GX | 80 | 9.25 | Picker | 1200SX | 80 | 4.76 | 3.99 | SCT 5000T | 80 | 5.51 | 3.41 | |||||||||
| 100 | 13.95 | 100 | 6.89 | 5.90 | 100 | 9.20 | 5.96 | |||||||||||||
| 120 | 19.06 | 120 | 11.52 | 8.87 | 120 | 14.00 | 9.40 | |||||||||||||
| 140 | 31.75 | 140 | 15.14 | 12.44 | 140 | 19.96 | 13.82 | |||||||||||||
| Elscint | Elite, Elect | 80 | 5.61 | 2.99 | AcQSim | 80 | 7.61 | 4.17 | SCT 6800T | 80 | 7.60 | 3.99 | ||||||||
| 100 | 9.17 | 4.89 | 100 | 11.89 | 6.51 | 100 | 12.69 | 6.97 | ||||||||||||
| 120 | 13.70 | 7.30 | 120 | 17.13 | 9.37 | 120 | 19.30 | 11.00 | ||||||||||||
| 140 | 19.23 | 10.25 | 140 | 23.31 | 12.76 | 140 | 27.51 | 16.17 | ||||||||||||
| Excel 1800 | 80 | 5.63 | IQ Series (Filter 0) | 80 | 6.36 | 4.24 | SCT 7000T | 80 | 7.52 | 4.06 | ||||||||||
| 100 | 8.38 | 100 | 9.94 | 6.63 | 100 | 12.56 | 7.10 | |||||||||||||
| 120 | 12.24 | 120 | 14.31 | 9.54 | 120 | 19.10 | 11.20 | |||||||||||||
| 140 | 18.57 | 140 | 19.48 | 12.99 | 140 | 27.23 | 16.47 | |||||||||||||
| Excel 2400 Elect | 80 | 6.88 | 2.81 | IQ Series (Filter 1) | 80 | 3.90 | 2.35 | SCT 7000TS | 80 | 6.93 | 3.74 | |||||||||
| 100 | 10.23 | 4.32 | 100 | 6.51 | 4.10 | 100 | 11.57 | 6.53 | ||||||||||||
| 120 | 14.95 | 1.21 | 5.31 | 120 | 9.90 | 6.47 | 120 | 17.60 | 10.30 | |||||||||||
| 140 | 22.68 | 7.46 | 140 | 14.11 | 9.51 | 140 | 25.09 | 15.14 | ||||||||||||
| HeliCAT (old BF) | 80 | 5.12 | 2.29 | MX Twin | 80 | 4.63 | Hitachi | Hitachi Eclos 4 | 80 | 7.14 | 2.96 | |||||||||
| 100 | 8.55 | 3.99 | 100 | 6.71 | 100 | 12.20 | 6.05 | |||||||||||||
| 120 | 13.65 | 0.92 | 6.30 | 120 | 11.22 | 120 | 18.54 | 9.72 | ||||||||||||
| 140 | 18.53 | 9.26 | 140 | 14.09 | 140 | 25.98 | 13.13 | |||||||||||||
| HeliCAT (new BF) | 80 | 4.41 | 1.74 | PQ Series (Filter 0) | 80 | 6.36 | 4.24 | Hitachi Eclos OB | 80 | 7.14 | 2.96 | |||||||||
| 100 | 7.36 | 3.04 | 100 | 9.94 | 6.63 | 100 | 12.20 | 6.05 | ||||||||||||
| 120 | 11.20 | 4.80 | 120 | 14.22 | 0.66 | 9.52 | 0.33 | 120 | 18.54 | 9.72 | ||||||||||
| 140 | 15.97 | 7.06 | 140 | 18.82 | 0.94 | 13.25 | 0.47 | 140 | 25.98 | 13.13 | ||||||||||
| MX Twin | 80 | 4.29 | 1.62 | PQ Series (Filter 1) | 80 | 3.90 | 2.35 | Hitachi Eclos 16 | 80 | 7.14 | 2.96 | |||||||||
| 100 | 7.17 | 2.83 | 100 | 6.51 | 4.10 | 100 | 12.20 | 6.05 | ||||||||||||
| 120 | 10.90 | 4.47 | 120 | 9.90 | 6.47 | 120 | 18.54 | 9.72 | ||||||||||||
| 140 | 15.54 | 6.56 | 140 | 14.11 | 9.51 | 140 | 25.98 | 13.13 | ||||||||||||
| SeleCT | 80 | 7.28 | 2.94 | Ultra Z (Filter 0) | 80 | 6.17 | 4.05 | Hitachi Scenaria 64 (small BF) | 80 | 6.85 | 2.77 | |||||||||
| 100 | 12.16 | 5.13 | 100 | 10.02 | 6.61 | 100 | 12.60 | 5.27 | ||||||||||||
| 120 | 18.50 | 8.10 | 120 | 14.16 | 9.57 | 120 | 19.99 | 8.57 | ||||||||||||
| 140 | 26.37 | 11.91 | 140 | 19.10 | 13.10 | 140 | 28.52 | 12.45 | ||||||||||||
| Twin (old BF) | 80 | 5.31 | 2.37 | Ultra Z (Filter 1) | 80 | 3.90 | 2.35 | Hitachi Scenaria 64 (medium BF) | 80 | 6.97 | 3.62 | |||||||||
| 100 | 8.88 | 4.15 | 100 | 6.51 | 4.10 | 100 | 12.83 | 6.88 | ||||||||||||
| 120 | 13.78 | 0.45 | 6.07 | 0.41 | 120 | 9.90 | 6.47 | 120 | 20.36 | 11.17 | ||||||||||
| 140 | 19.24 | 9.62 | 140 | 14.11 | 9.51 | 140 | 29.05 | 16.24 | ||||||||||||
| Twin (new BF) | 80 | 4.29 | 1.62 | Shimadzu | SCT 4500T | 80 | 4.21 | 0.12 | 2.51 | 0.06 | ||||||||||
| 100 | 7.17 | 2.83 | 100 | 7.17 | 4.37 | |||||||||||||||
| 120 | 10.90 | 4.47 | 120 | 10.90 | 6.90 | |||||||||||||||
| 140 | 15.54 | 6.56 | 140 | 14.24 | 1.83 | 9.10 | 0.91 | |||||||||||||
| Twin Flash | 80 | 6.58 | SCT 4800T | 80 | 5.31 | 2.98 | ||||||||||||||
| 100 | 9.79 | 100 | 8.88 | 5.20 | ||||||||||||||||
| 120 | 14.30 | 120 | 13.50 | 8.20 | ||||||||||||||||
| 140 | 21.70 | 140 | 19.24 | 12.06 |
3.4. Variation across the scanner models
The average and standard deviation of the normalized values across different scanner models within a given manufacturer were calculated for the four major manufacturers: GE, Philips, Siemens, and Toshiba. The calculation was performed for the values of head and body CTDI phantoms and for the tube potential of 120 kVp and depicted in Figure 2 (top). To compare the variation across the different manufacturers, COV (%) was calculated for each pair of average and standard deviation as shown in Figure 2 (bottom).
Figure 2.
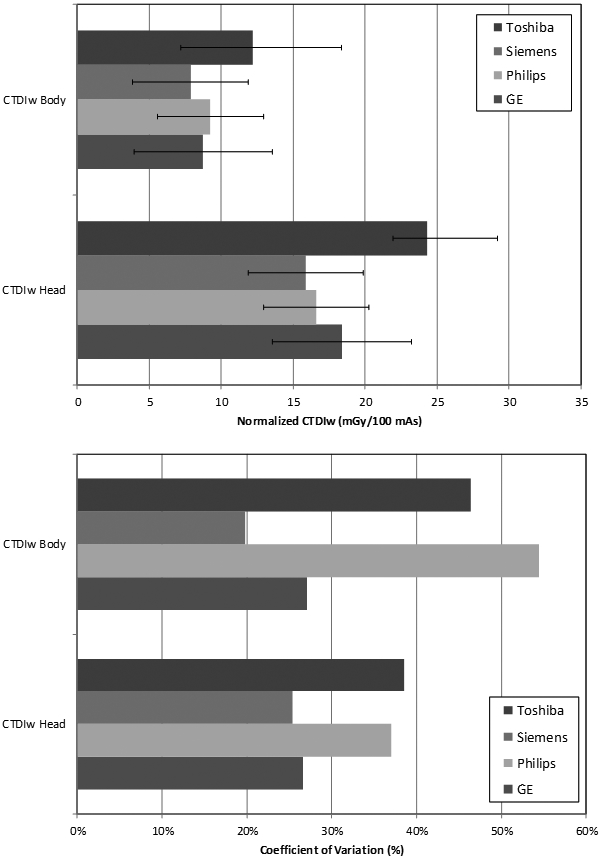
Average and standard deviation (top) and coefficient of variation (COV) (bottom) of the normalized (mGy/100 mAs) for head and body CTDI phantoms and for the tube potential of 120 kVp across different scanner models in four major scanner manufacturers.
It is clear from the graph that Toshiba models have the greatest for both head and body phantoms, 24.3 and 9.4 mGy, respectively. The values are 1.5 times greater than those of Siemens which show the smallest values for both head and body phantoms. As shown in Figure 2 (bottom), Toshiba and Philips show the largest coefficient of variation for head and body measurements, 39% and 54%, respectively. Siemens show the smallest coefficient of variation for both head and body measurements, at 25% for head and 20% for body phantoms. The average coefficient of variation among scanners within each manufacturer was 32% for head measurements and 37% for body measurements.
Since the is linearly proportional to the resulting organ dose in the organ dose calculation and again the is proportional to the normalized assuming identical technical parameters are used (Lee et al 2012; Turner et al 2010), possible misclassification of scanner model in retrospective dose reconstruction may cause significant difference in organ dose even in the same manufacturer category. For example, the normalized body (120 kVp) for Tomoscan M/EG model, 27.4 mGy/100mAs, is about 4 times greater than the value for Tomoscan AV, LX, SR Series, 7.7 mGy/100mAs. Assuming 200 mAs, 120 kVp, and the pitch of 1, the for the two similarly-looking scanner categories would be 54.8 and 15.4 mGy, respectively. The possible dose uncertainty coming from the scanner misclassification could be more severe in Toshiba and Phillips scanners than Siemens and GE based on Figure 2.
3.5. Variation across the data sources
Average, standard deviation, and COV of the normalized values for head and body phantoms only for 120 kVp collected from at least 2 sources were calculated and analyzed. Only four major manufacturers, GE, Philips, Siemens, and Toshiba, were included in the analysis. Figure 3 shows the COV of the normalized for head phantom and 120 kVp.
Figure 3.

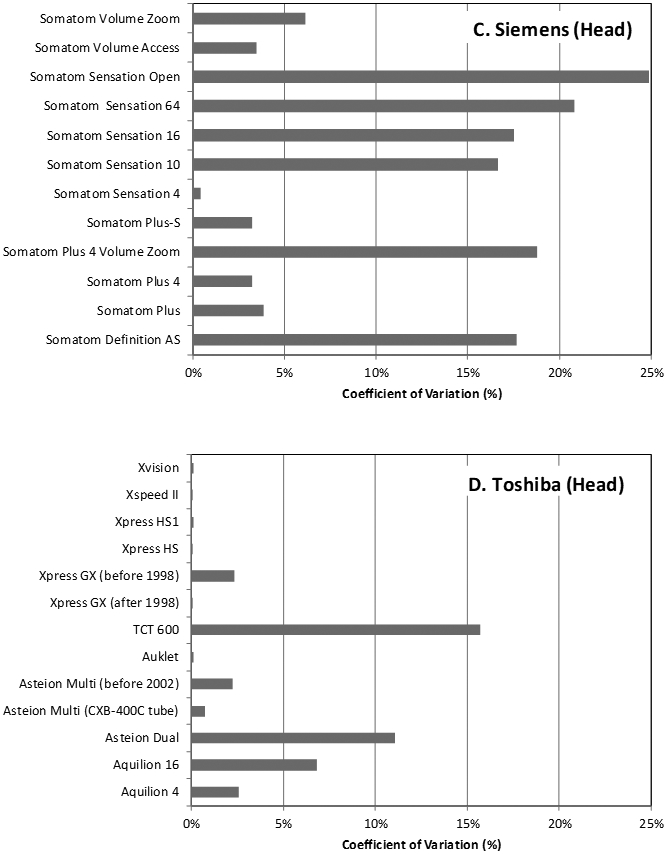
Percent coefficient of variation (COV) of the normalized (mGy/100mAs) for head CTDI phantoms and the tube potential of 120 kVp across different data sources for four major scanner manufacturers: (a) GE, (b) Philips, (c) Siemens, and (d) Toshiba.
The greatest variations were found in HiSpeed FX/i and LX/i, Tomoscan M/EG, Sensation Open, and TCT600 models showing the COVs of 15.8%, 10.4%, 24.9%, and 15.7%, from GE, Philips, Siemens, and Toshiba, respectively. The average of the COVs for CTDI head phantom was 5.6%, 3.8%, 11.4%, and 3.2% for GE, Philips, Siemens, and Toshiba, respectively. The CTDI values for the scanners from Siemens show the greatest variation by data source, which is about 4 times greater than the variation of Toshiba scanners. The COV for the body phantom CTDI values were 4.9%, 8.1%, 10.7%, and 2.7% for GE, Philips, Siemens, and Toshiba scanners, respectively. Siemens shows the greatest variation across different data sources again which is about 4 times greater than the variation in Toshiba scanners. Philips scanners show more than 2 times greater variation in body phantom CTDI values than that of head phantom CTDI values whereas other manufacturers show similar level of variation between head and body phantom CTDI values.
Significant level of variability was already observed even in a single survey such as the NLST. The authors of the NLST dose survey mentioned about two possible factors influencing the variability of the CTDI values: different behavior in one scanner from others even for the same model and possible human error or inconsistency in the measurement or reporting process (Cody et al 2010).
Using the same dose reconstruction algorithm described in the previous section (Lee et al 2012; Turner et al 2010), the resulting organ dose will be significantly different depending on which data source is adopted for a given scanner model. For example, the normalized head (120 kVp) for Siemens Somatom Sensation Open from ImPACT survey is 16.1 mGy/100mAs whereas the value from CT-Expo program is 23.0 mGy/100mAs. Assuming 200 mAs, 120 kVp, and the pitch of 1, the resulting would be 32.2 and 46.0 mGy depending on which data sources are used: ImPACT and CT-Expo, respectively. Kim et al. (Kim et al 2011) also reported the similar dose discrepancy among different computer programs which are based on different normalized database. They observed about 40% higher organ dose using CT-Expo program than CTDosimetry, which is based on ImPACT dose survey. As for the scanner models showing significant variations across the different data sources, we propose using the averaged CTDI values tabulated in Table 5.
3.6. Limitation of the database
When we merged data from the four data sources, we calculated equally weighted average of the CTDI values from the four surveys and tabulated the average in Table 5. We were aware that the CTDI values reported from the surveys are already the average of the multiple measurements and the number of measurements for the same CT scanner model is different across the surveys. However, the original survey data was not accessible and the number of data points is not included in the published report. We are in process of obtaining the original raw data from each survey. Once the data are available, we will be able to derive more accurate CTDI values.
Although a comprehensive database of the normalized is established for different CT scanner models, tube potentials, and CTDI phantoms, it must be noted that the CTDI values are also a function of collimation width, which is missing in our database. The total collimation has more impact on the normalized for multi-detector scanners than single-detector scanners (McNitt-Gray 2002). Unfortunately, the total beam collimation is not available for most retrospective patient cohort in epidemiologic studies. The value has been incorporated into more recent DICOM standard and started to be implemented by the manufacturers (Cody et al 2010). The availability of the total collimation will make calculation of radiation dose more accurate in the future.
4. Conclusion
A comprehensive database of normalized (mGy/100mAs) was established for a total of 162 scanner groups from 8 manufacturers using data from multiple data sources. Different scanner groupings obtained from different data sources were broken up to the single scanner level and regrouped into new scanner groups. An exponential regression model was developed to fill in missing CTDI values. The normalized database developed in the current study will be utilized to reconstruct values for retrospective CT scanners and then individualized organ dose can be calculated from organ dose database independently developed by using computational human phantoms coupled with Monte Carlo radiation transport.
ACKNOWLEDGMENTS
This work was supported by the Intramural Research Program of the National Institutes of Health, the National Cancer Institute, Division of Cancer Epidemiology and Genetics.
5. REFERENCES
- Berrington de Gonzalez A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, and Land C 2009. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Archives of Internal Medicine 169(22) 2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cody DD, Kim HJ, Cagnon CH, Larke FJ, McNitt-Gray MM, Kruger RL, Flynn MJ, Seibert JA, Judy PF, and Wu X 2010. Normalized CT Dose Index of the CT Scanners Used in the National Lung Screening Trial. American Journal of Roentgenology 194(6) 1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de González AB, Kim KP, and Berg CD 2008. Low-dose lung computed tomography screening before age 55: estimates of the mortality reduction required to outweigh the radiation-induced cancer risk. Journal of medical screening 15(3) 153–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ImPACT Web site. [Accessed June 20, 2013]. http://www.impactscan.org/dosesurvey.htm.
- Kim KP, Berrington de Gonzalez A, Pearce MS, Salotti JA, Parker L, McHugh K, Craft AW, and Lee C 2012. Development of a Database of Organ Doses for Paediatric and Young Adult CT Scans in the United Kingdom. Radiation Protection Dosimetry 150(4) 415–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KP, Einstein AJ, and Berrington de Gonzalez A 2009. Coronary artery calcification screening: estimated radiation dose and cancer risk. Archives of Internal Medicine 169(13) 1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KP, Lee J, and Bolch WE 2011. CT dosimetry computer codes: their influence on radiation dose estimates and the necessity for their revision under new ICRP radiation protection standards. Radiation Protection Dosimetry 146(1-3) 252–5 [DOI] [PubMed] [Google Scholar]
- Lee C, Kim K, Long D, Fisher R, Tien C, Simon S, Bouville A, and Bolch W 2011. Organ doses for reference adult male and female undergoing computed tomography estimated by Monte Carlo simulations. Medical Physics 38(3) 1196–1206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C, Kim KP, Long D, and Bolch WE 2012. Organ doses for reference pediatric and adolescent patients undergoing computed tomography estimated by Monte Carlo simulation. Medical Physics 39(4) 2129–2146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNitt-Gray MF 2002. AAPM/RSNA physics tutorial for residents: topics in CT. Radiographics 22(6) 1541. [DOI] [PubMed] [Google Scholar]
- Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, Howe NL, Ronckers CM, Rajaraman P, Craft AW, Parker L, and de González AB 2012. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. The Lancet [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao C 2002. Linear statistical inference and its applications. edition n, editor. Singapore: John Wiley & Sons, Inc. [Google Scholar]
- Stamm G, and Nagel HD 2002. CT-expo--a novel program for dose evaluation in CT. RöFo: Fortschritte auf dem Gebiete der Röntgenstrahlen und der Nuklearmedizin 174(12) 1570. [DOI] [PubMed] [Google Scholar]
- Stern S 2007. National Evaluation of X-Ray Trends (NEXT): Tabulation of Graphical Summary of 2000 Survey of Computed Tomography. Washington, DC: Food and Drug Administration. [Google Scholar]
- Turner AC, Zankl M, DeMarco JJ, Cagnon CH, Zhang D, Angel E, Cody DD, Stevens DM, McCollough CH, and McNitt-Gray MF 2010. The feasibility of a scanner-independent technique to estimate organ dose from MDCT scans: using CTDIvol to account for differences between scanners. Medical Physics 37(4) 1816–25 [DOI] [PMC free article] [PubMed] [Google Scholar]


