Abstract
Objective:
The Coronavirus Disease-19 (COVID-19) pandemic caused a decline in hospitalist wellness. The COVID-19 pandemic has evolved, and new outbreaks (i.e., Mpox) have challenged healthcare systems. The objective of the study was to assess changes in hospitalist wellness and guide interventions.
Methods:
We surveyed hospitalists (physicians and advanced practice providers [APPs]), in May 2021 and September 2022, at a healthcare system’s 16 hospitals in four US states using PROMIS® measures for global well-being, anxiety, social isolation, and emotional support. We compared wellness score between survey periods; in the September 2022 survey, we compared wellness scores between APPs and physicians and evaluated the associations of demographic and hospital characteristics with wellness using logistic (global well-being) and linear (anxiety, social isolation, emotional support) regression models.
Results:
In May 2021 vs. September 2022, respondents showed no statistical difference in top global well-being for mental health (68.4% vs. 57.4%) and social activities and relationships (43.8% vs. 44.3%), anxiety (mean difference:+0.8), social isolation (mean difference:+0.5), and emotional support (mean difference:−1.0) (all, p≥0.05). In September 2022, in logistic regression models, APPs, compared with physicians, had lower odds for top (excellent or very good) global well-being mental health (odds ratio [95% CI], 0.31 [0.13–0.76]; p<0.05). In linear regression models, age <40 vs. ≥40 years was associated with higher anxiety (estimate ± standard error, 2.43±1.05; p<0.05), and concern about contracting COVID-19 at work was associated with higher anxiety (3.74±1.10; p<0.01) and social isolation (3.82±1.21; p<0.01). None of the characteristics showed association with change in emotional support. In September 2022, there was low concern for contracting Mpox in the community (4.6%) or at work (10.0%).
Conclusion:
In hospitalists, concern about contracting COVID-19 at work was associated with higher anxiety and social isolation. The unchanged wellness scores between survey periods identify opportunities for intervention. Mpox had apparently minor impact on wellness.
Keywords: hospitalists, advanced practice providers, COVID-19, wellness, Mpox
Introduction
During the Coronavirus Disease-19 (COVID-19) pandemic, hospitalists (physicians and advanced practice providers [APPs], refer to nurse practitioners and physician assistants) were the leading teams caring for adult patients hospitalized with COVID-19 infection. The objective of the study was to evaluate the wellness of hospitalists and guide wellness interventions.
Several studies have reported the negative impact of the COVID-19 pandemic on the wellness of health care workers in different specialties (e.g., emergency medicine, hospital medicine), professions (e.g., physicians, APPs, nurses), and settings (e.g., clinic, emergency room) and frequently included anxiety, insomnia, and depression [1–11]. Early in the pandemic, we surveyed Internal Medicine hospitalists at our healthcare system’s 16 hospitals in four US states [4]. In our healthcare system, hospitalists refer to physicians and APPs (i.e., nurse practitioners and physician assistants) who provide 24×7 care to adults hospitalized with general medical conditions. Hospitalists triage patients in the emergency department, oversee the hospital course, and coordinate transition in care at hospital discharge. Compared with the pre-pandemic period (March 2020), the early phase of the pandemic (May 2020) was associated with lower global well-being (i.e., mental health [1 question]; social activities and relationships [1 question]), higher mean score for anxiety (8 questions) and social isolation (8 questions), and lower mean score for emotional support (9 questions), assessed using PROMIS® measures [4]. Assessment of wellness in October 2020 and May 2021 showed that hospitalists remained concerned about contracting COVID-19 at work with different patterns of change in anxiety, social isolation, and emotional support [2–4]. Since May 2022, the COVID-19 burden (e.g., incidence rate, volume of hospitalized patients) evolved coincident with the availability of preventive and therapeutic options. During the COVID-19 pandemic, in August 2022, The White House declared Mpox as a national health emergency. Mpox is a rare disease caused by the Mpox virus and transmitted through close, skin-to-skin contact. By August 2022, over 47,000 cases were confirmed in 92 non-endemic countries, with over 17,000 in the US [12]. In the US, by August 2022, the Mpox outbreak had grown exponentially with signs of slowing down. There was concern for an Mpox epidemic, which would have increased strain on healthcare systems. However, the wellness of hospitalists and their perspective on Mpox were not known, thereby limiting the development of wellness interventions and information sessions.
To address these knowledge gaps, we surveyed hospitalists, in September 2022, at our healthcare system’s 16 hospitals in four US states on demographics, wellness, and perspective on Mpox. We compared results by profession (physicians and APPs) and with those from the preceding survey in May 2021 to identify opportunities for wellness interventions.
Methods
The study was conducted by the Hospital Experiences to Advance Goals and Outcomes Network (HEXAGON) team [13] and was deemed ‘Exempt’ by the Mayo Clinic Institutional Review Board.
Survey timeline, sites and respondents
We conducted a COVID-19 wellness study with surveys in May 2020, October 2020, May 2021, and September 2022, as reported [2–4]. The present study is based on May 2021 and September 2022 surveys. The May 2021 survey was conducted from May 10–June 6, 2021 and pertained to wellness from March 15–April 30, 2021. The September 2022 survey was conducted from September 27–November 5, 2022 and pertained to wellness and Mpox from August 1–September 15, 2022.
We surveyed Internal Medicine hospitalists, which included physicians and APPs (i.e., nurse practitioners and physician assistants) from Mayo Clinic in Rochester MN, Jacksonville FL, Phoenix/Scottsdale AZ, and Mayo Clinic Health System (MCHS) hospitals, as reported [4]. The sites were randomly labeled A–D and included academic and community hospitals in urban and rural counties. MCHS included a network of hospitals in Minnesota (Austin/Albert Lea, Cannon Falls, Fairmont, Lake City, Mankato, Owatonna, and Red Wing) and Wisconsin (Barron, Bloomer, Eau Claire, La Crosse, Menomonie, and Osseo).
Survey development and administration
Hospitalists were surveyed on demographics, work hours, and living situation using Research Electronic Data Capture (REDCap®), as listed in Supplement 1 [4,14,15]. Wellness was assessed using Patient-Reported Outcomes Measurement Information System (PROMIS®) surveys (Supplement 1) [4,16]. Global well-being (PROMIS® Scale v1.2–Global Mental 2a) was rated on a 5-point Likert scale (excellent, very good, good, fair, poor) [17]. Global well-being was analyzed as top (excellent or very good) or lower (good, fair, or poor) category. Anxiety (PROMIS® Neuro-QoL Short Form v1.0–Anxiety)[18–20], social isolation (PROMIS® Short Form v2.0–Social Isolation 8a)[21,22], and emotional support (PROMIS® Item Bank v2.0–Emotional Support–Short Form 8a)[23] were assessed using eight questions each (score range 8–40). For emotional support, the study team added one question (“I got emotional support from my colleagues”), which was scored independently and not included in the overall score. Anxiety, social isolation, and emotional support were rated on a 5-point Likert scale (never, rarely, sometimes, usually, always). Each hospitalist received a unique survey link, sent to the work email, with up to two weekly reminders. Survey participation was voluntary.
Data analysis
Mean scores for anxiety, social isolation, and emotional support were calculated as described [20, 21,23]. Respondent demographics and wellness scores were compared between surveys (May 2021 and September 2022).
For the September 2022 survey, demographics and wellness scores were compared between physicians and APPs. We used separate logistic regression models for the outcome of top global well-being and reported the results as odds ratio (95% confidence interval). We used separate linear regression models for anxiety, social isolation, and emotional support, and reported results as estimate (± standard error [SE]). The models included explanatory variables for age group (<40 years; ≥40 years), gender (men; women/other), profession (APPs; physicians), concern about contracting COVID-19 at work (strongly agree or agree; other [neutral, disagree, or strongly disagree]), and survey site (A–D). Data were analyzed using SAS® 9.4 (SAS Institute Inc.) with statistical significance at 2-tailed p<.05.
Results
During both survey periods, COVID-19 mortality was highest in Florida (~350 deaths/week [May 2021] and ~175 deaths/week [October 2022]) compared with Arizona (~50 deaths/week [both periods]), Minnesota (~50 deaths/week [both periods]) and Wisconsin (~30 deaths/week [both periods]) (Figure 1).
Figure 1. Weekly Deaths Attributed to COVID-19 in US states with the study sites.
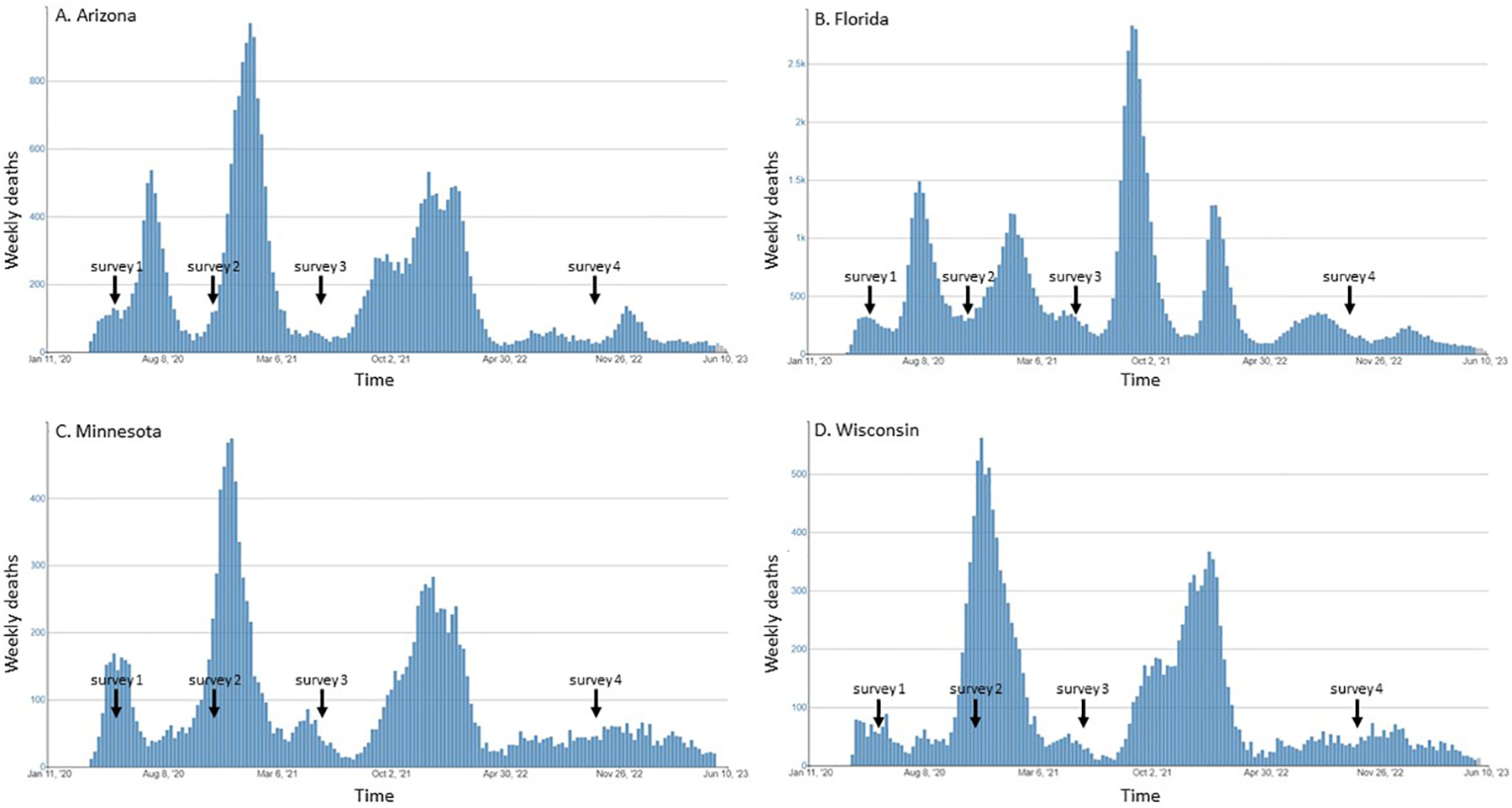
US CDC data on weekly deaths in Arizona (panel A), Florida (panel B), Minnesota (panel C), and Wisconsin (panel D) with overlay of the approximate survey periods. Note the different y-axis scales. Surveys were conducted from May 4–May 25, 2020 (survey 1), October 26–November 9, 2020 (survey 2), May 10–June 6, 2021 (survey 3), and September 27–November 5, 2022 (survey 4). This study was based on results from surveys 3 and 4. Data from US CDC [43].
Respondents to the May 2021 and September 2022 surveys had similar demographic characteristics including proportion of respondents aged <40 years (50.0% vs. 44.3%; p=0.37), men (46.5% vs. 45.8%; p=0.91), and APPs (41.2% vs. 38.9%; p=0.71). In both surveys, most respondents reported caring for patients with known or suspected COVID-19 (80.4% vs. 86.8%; p=0.17), whereas a smaller proportion reported concern about contracting COVID-19 at work (27.2% vs. 29.8%; p=0.66) (Table 1).
Table 1:
Characteristics of respondents, by survey period
| May 2021 (n=114) no. (%) |
September 2022 (n=131) no. (%) |
p value | |
|---|---|---|---|
| Demographics | |||
| Age <40 years | 57 (50.0) | 58 (44.3) | 0.37 |
| Gender | 0.91 | ||
| Men | 53 (46.5) | 60 (45.8) | |
| Women/Othera | 61 (53.5) | 71 (54.2) | |
| Profession | 0.71 | ||
| APPsb | 47 (41.2) | 51 (38.9) | |
| Physicians | 67 (58.8) | 80 (61.1) | |
| Living situation during pandemic | 0.41 | ||
| Lived alone | 14 (12.3) | 10 (7.7) | |
| Lived with 1–4 members | 93 (81.6) | 109 (83.8) | |
| Lived with 5–10 members | 7 (6.1) | 11 (8.5) | |
| People living with you during pandemicc | |||
| Children | 66 (57.9) | 76 (58.0) | 0.98 |
| Parents | 13 (11.4) | 13 (9.9) | 0.71 |
| Spouse, partner, or significant other | 92 (80.7) | 116 (88.5) | 0.09 |
| Worked <4 weeks | 39 (34.2) | 42 (32.3) | 0.75 |
| COVID-19 | |||
| Primary source for COVID-19 information | |||
| News websites | 25 (21.9) | 17 (13.0) | |
| Social medial platforms | 1 (0.9) | 2 (1.5) | |
| Institutional resources | 81 (71.1) | 98 (74.8) | |
| Discussion with family and friends | 0 (0.0) | 2 (1.5) | |
| Other | 7 (6.1) | 12 (9.2) | |
| Cared for patients with known or suspected COVID-19 | 90 (80.4) | 112 (86.8) | 0.17 |
| Concerned about contracting COVID-19 at workd | 31 (27.2) | 39 (29.8) | 0.66 |
| Changed where you lived due to fear of transmitting COVID-19 to family members | 2 (1.8) | 3 (2.3) | |
| Global well-being e | |||
| Mental health | 78 (68.4) | 74 (57.4) | 0.08 |
| Social activities and relationships | 49 (43.8) | 58 (44.3) | 0.93 |
| Mpox | |||
| Concerned about contracting Mpox in communityd | --- | 6 (4.6) | --- |
| Concerned about contracting Mpox at workd | --- | 13 (9.9) | --- |
| Primary source for Mpox information | --- | --- | |
| News websites | 41 (31.3) | ||
| Social medial platforms | 4 (3.1) | ||
| Institutional resources | 74 (56.5) | ||
| Discussion with family and friends | 2 (1.5) | ||
| Other | 10 (7.6) | ||
| Responsibility to provide Mpox informationc | --- | --- | |
| My responsibility | 71 (54.2) | ||
| Hospital Medicine leadership | 64 (48.9) | ||
| Mayo Clinic leadership | 96 (73.3) | ||
| Centers for Disease Control and Prevention | 110 (84.0) | ||
| US Food and Drug Administration | 16 (12.2) | ||
| Helpful for Hospital Medicine leadership to conduct ≥1 Mpox sessiond | --- | 71 (54.2) | --- |
For each survey period, ‘during pandemic’ and questions referred to the preceding six-week period: May 2021 (March 15, 2021–April 30, 2021) and September 2022 (August 1, 2022–September 15, 2022). Percentages may not add to 100 due to rounding.
Mpox questions were asked only in the September 2022 survey.
Other included non-binary/other, prefer not to respond, and missing.
Advanced practice providers (APPs) refer to nurse practitioners and physician assistants.
Respondents could select more than one option.
Agree included strongly agree and agree; other included neutral, disagree, and strongly disagree.
Options were excellent, very good, good, fair, and poor. Top global well-being included excellent and very good.
p value based on chi-square or Fisher test.
Data missing: living situation during pandemic (n=1), worked <4 weeks (n=1), cared for patients with known or suspected COVID-19 (n=4), changed where you lived due to fear of transmitting COVID-19 to family members (n=3), global well-being–mental health (n=2) and global health–social activities and relationship (n=2).
Survey questions listed in Supplement 1.
Abbreviation: COVID-19, Coronavirus disease 2019.
May 2021 vs. September 2022: global well-being
In both surveys, most respondents reported top global well-being for mental health (68.4% vs. 57.4%; p=0.08), whereas a smaller proportion reported top global well-being for social activities and relationships (43.8% vs. 44.3%; p=0.93) (Table 1).
May 2021 vs. September 2022: anxiety, social isolation, and emotional support
The mean difference in raw scores for anxiety, social isolation, and emotional support did not differ significantly between September 2022 and May 2021 surveys (Supplementary Table 1). The mean scores (±SD) for anxiety were 15.7 ± 5.5 (May 2021) and 16.5 ± 6.0 (September 2022) (mean difference: −0.8; p=0.24); for social isolation, the scores were 14.6 ± 5.9 (May 2021) and 15.1 ± 6.3 (September 2022) (mean difference: −0.5; p=0.59), and for emotional support, the scores were 33.7 ± 5.9 (May 2021) and 32.7 ± 7.0 (September 2022) (mean difference: +1.0; p=0.22).
September 2022 demographics
The response rate to the September 2022 survey was 35.2% (n=131/372) and included 38.9% APPs (n=51/131) and 61.1% physicians (n=80/131). There were differences in the proportion of respondents aged <40 years (56.9% of APPs vs. 36.3% of physicians; p=0.02), proportion who lived with children (47.1% of APPs vs. 65.0% of physicians; p=0.04), or with spouse, partner or significant other (80.4% of APPs vs. 93.8% of physicians; p=0.02), and who worked <4 weeks (20.0% of APPs vs. 40.0% of physicians; p=0.02) (Supplementary Table 2). Most respondents cared for patients with known or suspected COVID-19 (92.0% of APPs vs. 83.5% of physicians; p=0.17), and a lower proportion reported concern about contracting COVID-19 at work (25.5% of APPs vs. 32.5% of physicians; p=0.39).
September 2022: global well-being
The proportion of respondents with top global well-being−mental health was higher for physicians (66.7%) compared with APPs (43.1%) (p=0.008). In logistic regression models including age group, gender, profession, concern about contracting COVID-19 at work, and survey site, only profession was associated with top global well-being−mental health: APPs, compared with physicians, had 69% lower odds of top global well-being−mental health (adjusted odds ratio 0.31, 95% CI 0.13–0.76; p<0.05) (Table 2). In contrast, the proportion of respondents with top global well-being−social activities and relationships did not differ between physicians (48.8%) and APPs (37.3%) (p=0.20) and in logistic regression models, none of the characteristics (age group, gender, profession, concern about contracting COVID-19 at work, and survey site) showed association with odds of top global well-being−social activities and relationships.
Table 2:
Characteristics of respondents and self-reported global well-being in the September 2022 survey
| Global well-being–mental health | Global well-being–social activities and relationships | |
|---|---|---|
| Odds ratio (95% confidence interval)a | ||
| Age <40 years vs. ≥40 years | 0.65 (0.30−1.44) | 0.73 (0.34−1.55) |
| Women/Other vs. men | 1.23 (0.53−2.90) | 1.29 (0.58−2.90) |
| APPsb vs. physicians | 0.31 (0.13−0.76)* | 0.56 (0.23−1.32) |
| Concerned about contracting COVID-19 at work | ||
| Strongly agree or agree vs. otherc | 0.80 (0.34−1.86) | 0.81 (0.37−1.79) |
| Survey site | ||
| A vs. D | 0.75 (0.26−2.22) | 0.99 (0.37−2.68) |
| B vs. D | 0.38 (0.12−1.17) | 0.79 (0.27−2.30) |
| C vs. D | 0.56 (0.21−1.51) | 0.63 (0.24−1.63) |
Separate logistic regression models for global well-being–mental health and global well-being–social activities and relationships, adjusted for other listed covariates. Survey sites (Rochester, Mayo Clinic Health System, Arizona, and Florida) were randomly labeled A–D.
Odds ratio for top (excellent or very good) vs. lower (good, fair, or poor) category.
APPs (advanced practice providers) refer to nurse practitioners and physician assistants.
Other included neutral, disagree, or strongly disagree.
p<0.05
Data missing: survey site (n=1).
Survey questions listed in Supplement 1.
Abbreviation: COVID-19, Coronavirus disease 2019.
September 2022: anxiety, social isolation, and emotional support
The mean score (±SD) for anxiety was similar between APPs (17.2 ± 5.2) and physicians (16.1 ± 6.5) (mean difference: −1.1; p=0.33) (Supplementary Table 3). In multivariable linear regression models, higher anxiety was associated with respondents aged <40 years (vs. older) (estimate ± SE, 2.43 ± 1.05; p<0.05) and with concern about contracting COVID-19 at work (estimate ± SE, 3.74 ± 1.10; p<0.01), whereas gender, profession, and survey site showed no independent association (Table 3).
Table 3:
Characteristics of respondents and self-reported anxiety, social isolation, and emotional support in the September 2022 survey
| Anxiety (higher value indicates higher anxiety) | Social isolation (higher value indicates higher isolation) | Emotional support (higher value indicates lower support) | |
|---|---|---|---|
| Estimate (±SE)a | |||
| Intercept | 12.31 | 12.78 | 32.39 |
| Age <40 years vs. ≥40 years | 2.43 (±1.05)* | 0.59 (±1.16) | 2.22 (±1.27) |
| Women/Other vs. men | 0.92 (±1.12) | 0.61 (±1.23) | 1.16 (±1.34) |
| APPsb vs. physicians | 0.88 (±1.19) | 0.64 (±1.31) | 0.73 (±1.43) |
| Concerned about contracting COVID-19 at work | |||
| Strongly agree or agree vs. otherc | 3.74 (±1.10)** | 3.82 (±1.21)** | −1.59 (±1.32) |
| Survey site | |||
| A | 1.31 (±1.40) | −0.48 (±1.54) | −0.03 (±1.68) |
| B | 3.53 (±1.49) | 1.79 (±1.64) | −0.52 (±1.79) |
| C | 1.51 (±1.31) | 0.25 (±1.44) | −4.13 (±1.58) |
| D | ref. | ref. | ref. |
| p value | 0.13 | 0.63 | 0.05 |
Separate linear regression models for anxiety, social isolation, and emotional support, adjusted for other listed covariates.
Survey sites (Rochester, Mayo Clinic Health System, Arizona, and Florida) were randomly labeled A–D.
Compared with reference group (ref.; estimate=0).
Advanced practice providers (APPs) refer to nurse practitioners and physician assistants.
Other included neutral, disagree, or strongly disagree.
p<0.05,
p<0.01
Data missing: survey site (n=1), living situation (n=1).
Survey questions listed in Supplement 1.
Abbreviation: COVID-19, Coronavirus disease 2019; SE, standard error
Similar to anxiety, the mean score (±SD) for social isolation was similar between APPs (15.5 ± 6.8) and physicians (14.8 ± 6.0) (mean difference: −0.7; p=0.57) (Supplementary Table 3). In multivariable linear regression models, higher social isolation was associated with concern about contracting COVID-19 at work (estimate ± SE, 3.82 ± 1.10; p<0.01), whereas other characteristics showed no independent association (Table 3).
Similar to anxiety and social isolation, the mean score (±SD) for emotional support was similar between APPs (33.9 ± 6.0) and physicians (32.0 ± 7.5) (mean difference: −1.9; p=0.12) (Supplementary Table 3). In multivariable linear regression models none of the examined characteristics (age group, gender, profession, concern about contracting COVID-19 at work, and survey site) showed independent association with emotional support scores (Table 3).
September 2022: Mpox
Compared to ~30% of respondents concerned about contracting COVID-19 at work, a smaller proportion was concerned about contracting Mpox at work (~10%) and in the community (~5%) (Table 1). Many respondents relied on institutional resources as the primary source of information on Mpox (68.6% of APPs and 48.8% of physicians) and reported that it was the responsibility of the US Centers for Disease Control and Prevention and the institution to provide information on Mpox.
Discussion
In this study of hospitalists in a healthcare system’s 16 hospitals in four US states, APPs, compared with physicians, had similar odds of top global-wellbeing−social activities and relationships, but 69% lower odds of top global-wellbeing−mental health. Concern about contracting COVID-19 at work was associated with higher anxiety and higher social isolation, independent of profession, demographic and hospital characteristics. Between the September 2022 and May 2021 surveys, there was no change in top global well-being and scores for anxiety, social isolation, and emotional support. To our knowledge, this is the longest running wellness study of physicians and APPs and identifies opportunities for overall and profession-specific wellness interventions.
Based on surveys initiated in May 2020, we reported changes in wellness of physicians and APPs [2–4]. The pre-pandemic top global well-being−mental health was 90% (March 2020), which was higher than in subsequent surveys: 53% (May 2020), 53% (October 2020), 68% (May 2021), and 57% (September 2022) [2,4]. Similarly, pre-pandemic top global well-being−social activities and relationships was 88% (March 2020), which was higher than in subsequent surveys: 24% (May 2020), 32% (October 2020), 44% (May 2021), and 44% (September 2022) [2,4]. Compared with physicians, APPs had 50% lower odds of top global well-being–mental health [2]; this difference in APPs persisted in the present study with 69% lower odds of top global well-being–mental health. Compared with physicians, APPs had 59% lower odds of top global well-being–social activities and relationships [2]; however, in the present study, this difference was eliminated. The improvement in global well-being–social activities and relationships may reflect targeted work programs (e.g., dedicated social rooms, snack breaks, lunch programs) that fostered social interaction, increased non-work social interaction, and reduced travel restriction, among other factors. While institution-specific interventions may be more effective in addressing wellness, a recent study based on 26 US hospitals reported a Best Practices for Hospital Medicine Programs−Checklist, Assessment, Relationship, Evaluation, Safety needs (CARES) model to address wellness in hospital medicine [24]. Suboptimal wellness of physicians and/or APPs affects individuals, their families, hospital medicine team function, and patient care. The lower global well-being–mental health of APPs vs. physicians warrants qualitative studies with APPs to identify individual, organizational, and other factors that affect mental health. Such studies may also generate ideas to design targeted interventions.
In our study, wellness scores in September 2022 were similar to those from May 2021. Between the two survey periods, the prevalence of COVID-19 had declined in all US states with the study sites, COVID-19 vaccines were widely available, and hospital practices were restructured to accommodate practice-related changes in patient volumes [25,26]. In a previous study, we surveyed hospitalists, from December 2020–January 2021, on perceptions of the potential benefit of the COVID vaccine [27]. In that study, physicians and APPs reported that patients and coworkers receiving the COVID-19 vaccine would significantly improve anxiety, social isolation, and emotional support [27]. Despite the availability of COVID-19 vaccines during our survey periods, uptake across US states differed, and the emergence of COVID-19 variants may have had mixed effects on hospitalists’ anxiety. In our study, the proportion of respondents concerned about contracting COVID-19 at work was lower (~27% in May 2021 and September 2022) compared to ~75% in May 2020 and ~55% in October 2020 [2]. Despite this, in September 2022, concern about contracting COVID-19 at work was independently associated with higher anxiety and higher social isolation. These results highlight opportunities to address hospital practice and develop interventions to reduce COVID-19 transmission.
Hospitalists aged <40 years (vs. older) had a higher level of anxiety independent of profession, concern about contracting COVID-19 at work, and other factors. In support, studies have reported higher anxiety in younger adults (e.g., community dwellers, nurses) during the COVID-19 pandemic, attributed to job insecurity, loneliness, and uncertainty about the pandemic [28–30]. Given improvement in the COVID-19 burden, social activities, and travel, anxiety levels may have declined in hospitalists aged <40 years, a topic that will be evaluated in the future.
In our healthcare system, physicians and APPs had access to the same wellness resources, interventions, supports, and profession-based differences may stem from differences in perceived work autonomy, job stability, and ability to maintain social interactions with colleagues, although these possibilities require formal evaluation [31]. Suboptimal wellness of physicians and APPs may have long-term effects on the workforce. In our healthcare system, the number of physicians and APPs increased from 297 (May 2020) to 372 (September 2022) reflecting an expansion of hospital practice and greater need to ensure a healthy workforce. Previous studies have reported the interplay of organizational support, professional factors, and wellness to affect burnout [32–36]. A meta-analysis of 22 studies, from 2014–2019, identified several interventions (e.g., self-care workshop, meditation) to reduce burnout in physicians and nurses, suggesting that a bundled (vs. single intervention) strategy may be more effective in reducing risk of burnout [37]. In support, a study using multimodal interventions (e.g., group meetings, individual coaching) resulted in lower hospitalist burnout (32% in intervention vs. 56% in controls) during the COVID-19 pandemic [38]. The study was based at two hospitals and will require evaluation in other settings [38].
In our study, APPs and physicians were less concerned about contracting Mpox in the community or at work. There was sparse information on health care workers’ perspective on Mpox. In an online survey of 1130 healthcare workers in the Kingdom of Saudi Arabia (from May 27, 2022–June 5, 2022), 56.5% of respondents were more concerned about COVID-19 than Mpox, with concern that Mpox would reach pandemic proportions [39]. Based on CDC data through June 2023, the Mpox burden had declined with no imminent concern for transition to a pandemic [12].
Similar to other survey studies, this study has limitations, as reported [2–4]. The survey response was ~35%, consistent with rates we and others have reported [2–4,41,42]. However, the wellness scores and potential benefit of interventions in non-respondents is not known. We examined several demographic and hospital characteristics; however, the role of other potentially confounding factors (e.g., family illness) or factors unavailable for analysis (e.g., individual income, household income, immunization status) is not known. This study has strengths. It is the longest running study on wellness of hospitalists and guides wellness interventions. The survey sites are within the same healthcare system; however, the heterogeneity in state burden of COVID-19, patients, hospitalists, and other hospital workers, increases generalizability to other healthcare systems [4,27].
Conclusion
In this assessment of hospitalists, in September 2022, concern about contracting COVID-19 at work was independently associated with higher anxiety and social isolation. Global well-being remained below pre-pandemic levels despite significant reduction in the prevalence of COVID-19. The similar scores, for global well-being, anxiety, social isolation, and emotional support, compared with 16 months prior (May 2021), highlight opportunities for targeted interventions to achieve pre-pandemic levels of wellness.
Supplementary Material
Declaration of funding
S.B.D. was supported by the National Institutes of Health/National Institute on Minority Health and Health Disparities (NIH K23 MD016230) and the Robert and Elizabeth Strickland Career Development Award, Mayo Clinic, Rochester, MN, USA. The study was made possible by the Mayo Clinic CTSA through grant number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health. The study was supported by the Mayo Clinic Department of Medicine Research Hub and Division of Hospital Internal Medicine. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data analysis and interpretation; in writing of the report; and in the decision to submit the manuscript for publication. The findings do not necessarily represent the views of the funders.
Declaration of financial/other relationships
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- 1.Aymerich C, Pedruzo B, Pérez JL, et al. COVID-19 pandemic effects on health worker’s mental health: Systematic review and meta-analysis. Eur Psychiatry. 2022;65(1):e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dugani SB, Fischer KM, Schroeder DR, et al. Wellness of hospitalists and hospital medicine advanced practice providers during the COVID-19 pandemic, 2020–2021. J Hosp Med. 2022;17(4):259–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dugani SB, Fischer KM, Geyer HL, et al. Psychologic wellness of PA, NP, and physician hospitalists during the COVID-19 pandemic. JAAPA. 2022;35(5):45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dugani SB, Geyer HL, Maniaci MJ, et al. Psychological wellness of internal medicine hospitalists during the COVID-19 pandemic. Hosp Pract (1995). 2021;49(1):47–55. [DOI] [PubMed] [Google Scholar]
- 5.Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Sousa GM, Tavares VDO, de Meiroz Grilo MLP, et al. Mental health in COVID-19 pandemic: A meta-review of prevalence meta-analyses. Front Psychol. 2021;12:703838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dragioti E, Tsartsalis D, Mentis M, et al. Impact of the COVID-19 pandemic on the mental health of hospital staff: An umbrella review of 44 meta-analyses. Int J Nurs Stud. 2022;131:104272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phiri P, Ramakrishnan R, Rathod S, et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: A systematic review and meta-analysis. EClinicalMedicine. 2021;34:100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keniston A, Patel V, McBeth L, et al. The impact of surge adaptations on hospitalist care teams during the COVID-19 pandemic utilizing a rapid qualitative analysis approach. Arch Public Health. 2022;80(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shanafelt TD, West CP, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic. Mayo Clin Proc. 2022;97(12):2248–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Linker AS, Kulkarni SA, Astik GJ, et al. Bracing for the Wave: A multi-institutional survey analysis of inpatient workforce adaptations in the first phase of COVID-19. J Gen Intern Med. 2021;36(11):3456–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CDC. Mpox 2022 Outbreak Cases and Data 2023. [cited 2023 June 18, 2023]. Available from: https://www.cdc.gov/poxvirus/mpox/index.html
- 13.HEXAGON. HEXAGON 2020. [cited 2022 November 18]. Available from: https://www.mayo.edu/research/centers-programs/hospital-experiences-advance-goals-outcomes-network/about
- 14.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.HealthMeasures 2020. Available from: https://www.healthmeasures.net/
- 17.Hays RD, Schalet BD, Spritzer KL, et al. Two-item PROMIS(R) global physical and mental health scales. J Patient Rep Outcomes. 2017;1(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): depression, anxiety, and anger. Assessment. 2011;18(3):263–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pilkonis PA, Yu L, Dodds NE, et al. Validation of the depression item bank from the Patient-Reported Outcomes Measurement Information System (PROMIS®) in a three-month observational study. Journal of Psychiatric Research. 2014; 112–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.PROMIS. Anxiety 2019. [cited 2020 September 25]. Available from: https://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Anxiety_Scoring_Manual.pdf
- 21.PROMIS. Social Isolation 2015. [cited 2020 September 25]. Available from: http://www.healthmeasures.net/administrator/components/com_instruments/uploads/15-09-01_16-44-48_PROMISSocialIsolationScoringManual.pdf
- 22.Hahn EA, DeWalt DA, Bode RK, et al. New English and Spanish social health measures will facilitate evaluating health determinants. Health Psychol; 2014;490–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.PROMIS. Emotional Support 2020. [cited 2020 September 25]. Available from: http://www.healthmeasures.net/images/promis/manuals/PROMIS_Emotional_Support_Scoring_Manual.pdf
- 24.Murphy E, Chokshi K, Niranjan-Azadi A, et al. Looking back while thinking forward: Institutional best practices to address hospitalist well-being during COVID-19. J Gen Intern Med. 2023;38(5):1326–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CDC. COVID Data Tracker 2023. [cited 2023 March 5, 2023]. Available from: https://covid.cdc.gov/covid-data-tracker/#datatracker-home
- 26.CDC. How Do I Find a COVID-19 Vaccine or Booster? 2022. [cited 2023 March 5, 2023]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/How-Do-I-Get-a-COVID-19-Vaccine.html?s_cid=10500:new%20covid%20vaccine%20availability:sem.ga:p:RG:GM:gen:PTN:FY21
- 27.Dugani SB, Geyer HL, Maniaci MJ, et al. Hospitalist perspectives on barriers to recommend and potential benefit of the COVID-19 vaccine. Hosp Pract (1995). 2021;21:1–7. [DOI] [PubMed] [Google Scholar]
- 28.Adams SH, Schaub JP, Nagata JM, et al. Young adult anxiety or depressive symptoms and mental health service utilization during the COVID-19 pandemic. J Adolesc Health. 2022;70(6):985–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alzahrani NS, Almarwani AM, Asiri SA, et al. Factors influencing hospital anxiety and depression among emergency department nurses during the COVID-19 pandemic: A multi-center cross-sectional study. Front Psychiatry. 2022;13:912157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Croghan IT, Chesak SS, Adusumalli J, et al. Stress, resilience, and coping of healthcare workers during the COVID-19 pandemic. J Prim Care Community Health. 2021;12:21501327211008448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klein CJ, Dalstrom MD, Weinzimmer LG, et al. Strategies of advanced practice providers to reduce stress at work. Workplace Health Saf. 2020;68(9):432–42. [DOI] [PubMed] [Google Scholar]
- 32.Capone V, Borrelli R, Marino L, et al. Mental well-being and job satisfaction of hospital physicians during COVID-19: Relationships with efficacy beliefs, organizational support, and organizational non-technical skills. Int J Environ Res Public Health. 2022;19(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou AY, Hann M, Panagioti M, et al. Cross-sectional study exploring the association between stressors and burnout in junior doctors during the COVID-19 pandemic in the United Kingdom. J Occup Health. 2022;64(1):e12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Faderani R, Monks M, Peprah D, et al. Improving wellbeing among UK doctors redeployed during the COVID-19 pandemic. Future Healthc J. 2020;7(3):e71–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morgantini LA, Naha U, Wang H, et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS One. 2020;15(9):e0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Melnikow J, Padovani A, Miller M. Frontline physician burnout during the COVID-19 pandemic: National survey findings. BMC Health Serv Res. 2022;22(1):365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang XJ, Song Y, Jiang T, et al. Interventions to reduce burnout of physicians and nurses: An overview of systematic reviews and meta-analyses. Medicine (Baltimore). 2020;99(26):e20992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.James TT, Hudon R, Merrick T, et al. Creating a comprehensive pandemic response to decrease hospitalist burnout during COVID-19: Intervention vs control results in 2 comparable hospitals (HOSP-CPR). J Gen Intern Med. 2023;10:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ajman F, Alenezi S, Alhasan K, et al. Healthcare workers’ worries and monkeypox vaccine advocacy during the first month of the WHO monkeypox alert: Cross-sectional survey in Saudi Arabia. Vaccines (Basel). 2022;10(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.ASPR. Renewal of Determination that A Public Health Emergency Exists. 2022. [cited 2023 March 6, 2023]. Available from: https://aspr.hhs.gov/legal/PHE/Pages/mpx-renewal-2Nov2022.aspx
- 41.Cunningham CT, Quan H, Hemmelgarn B, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol. 2015;15:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barnhart BJ, Reddy SG, Arnold GK. Remind me again: Physician response to web surveys: The effect of email reminders across 11 opinion survey efforts at the American Board of Internal Medicine from 2017 to 2019. Eval Health Prof. 2021;44(3):245–59. [DOI] [PubMed] [Google Scholar]
- 43.CDC. Trends in United States COVID-19 hospitalizations, deaths, emergency visits, and test positivity by geographic area 2023. [cited 2023 June 18, 2023]. Available from: https://covid.cdc.gov/covid-data-tracker/#trends_weeklyhospitaladmissions_select_00
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


