Opening Vignette
Aaron, an 18-month-old boy, was brought by his parents to your clinic for his 5-in-1 booster vaccination and developmental screen. His childcare teachers had raised concerns that he was ‘slower’ in his speech and language development as compared to his peers. His parents reported that he is able to use the words ‘papa’ and ‘mama’ specifically but say only two other single words. He can point and use gestures to indicate his wants. You assessed his receptive language to be age appropriate. He has no hearing problems or behavioural concerns suggestive of autism spectrum disorder. In general, he has been in good health and has no significant past medical problems of note. Your clinical examination of him was unremarkable. Aaron’s parents appeared anxious and were concerned that he will be at a disadvantage as compared to his peers when he grows up.
WHAT IS SPEECH AND LANGUAGE?
Speech and language are often mistaken to be synonymous. Speech is the articulation and production of speech sounds within the mouth, whereas language encompasses comprehension, processing and production of communication. Expressive language refers to the ability to communicate and convey meaning to others. Typically, this output is speech, but may be in the form of signs, gestures and written language. Receptive language refers to the ability to understand the communication of others, and encompasses auditory and visual skills. Apart from expressive and receptive language, other pertinent components of language development are necessary for children to develop effective communication. These include joint attention, play and social-pragmatic language (which refers to the way in which language is comprehended and applied in a social context).
The acquisition of normal speech and language skills is a key developmental milestone that most parents eagerly anticipate. Naturally, there are parental concerns and anxiety when there are deviations from parental expectations or perceived norms. Hence, the understanding of normal patterns of speech and language development and identification of delays is crucial in primary care.
The prevalence of isolated speech and language delays and disorders was estimated to be between 5% and 12% (median 6%) among children between 2 and 5 years of age in the United States.[1] Preschool children with untreated speech and language delay may be at a higher risk of learning disabilities. This may be exhibited in the form of diminished reading skills in grade school, poor verbal and spelling skills, behaviour problems and impaired psychosocial adjustment.[1] Consequently, this may constitute an overall academic underachievement[2] and may eventually lead to an impact on employment and even mental health.[3] As such, early identification of delays through developmental surveillance and screening, followed by prompt evaluation and intervention, is critical.
HOW RELEVANT IS THIS TO MY PRACTICE?
A local study on the profiles and outcomes of children who were referred to KK Women’s and Children’s Hospital Department of Child Development between 2003 and 2004 noted that the most common presenting concern was speech and language delay, and more than half the cohort was recommended for speech and language therapy after review by the paediatrician. Most of the children were around 2–4 years of age, consistent with the time at which speech and language delays may begin to appear more evident due to their impact on communication and social interaction.[4] In Singapore, structured childhood developmental screening is conducted at regular intervals in the primary care setting for all children aged 4 weeks to around 4–6 years. As part of preventive care, the primary care physician is also encouraged to use every encounter as an opportunity for developmental surveillance. Moreover, many children of this age group may not be enrolled in any formal education system, placing the primary care physician in a central role in identifying delays. Therefore, it is essential for them to have the knowledge and skills to assess speech and language appropriately and to provide appropriate counselling to caregivers on any issues identified.
WHAT ARE THE NORMAL DEVELOPMENTAL MILESTONES?
Development of speech and language arises from a complex interplay between genetic factors and environmental stimulation. In the first year of life, infants develop significant foundations that underpin speech and language development, and much of the language that they acquire is through listening and interacting with people around them. Within the first 3 years of life, children understand a lot more than they can express. Normal speech progresses through stages of cooing, babbling, words and forming different combinations of words. In language development, children go through stages of understanding and expressing more complex concepts. Table 1 describes the normal developmental milestones for speech and language in children.[5]
Table 1.
Receptive and expressive language milestones.[5]
| Milestone type | Skill | Mean age (mth) | Normal range (mth) |
|---|---|---|---|
| Receptive | Alerts to sound | Newborn | N/A |
|
| |||
| Orients to sound/turns to voice | 4 | 3–6 | |
|
| |||
| Responds to name | 4 | 4–9 | |
|
| |||
| Understands ‘no’ | 10 | 9–18 | |
|
| |||
| Follows one-step command with gesture | 12 | 10–16 | |
|
| |||
| Follows one-step command without gesture | 15 | 12–20 | |
|
| |||
| Points to several body parts | 18 | 12–24 | |
|
| |||
| Follows two-step command with gesture | 24 | 22–30 | |
|
| |||
| Understands basic spatial terms (e.g. in, on, under) | 28 | 27–30 | |
|
| |||
| Follows three-step, unrelated directions | 34 | 33–36 | |
|
| |||
| Expressive | Cooing (vowel sounds) | 3 | 1–4 |
|
| |||
| Laughs | 4 | 3–6 | |
|
| |||
| Babbling (consonants added to vowel sounds) | 6 | 5–9 | |
|
| |||
| Dada/mama non-specifically | 8 | 6–10 | |
|
| |||
| Dada/mama specifically | 10 | 9–14 | |
|
| |||
| 3–5-word vocabulary | 12 | – | |
|
| |||
| Immature jargoning (i.e. gibberish with inflection) | 13 | 10–18 | |
|
| |||
| Mature jargoning (i.e. gibberish with the occasional word) | 18 | 16–24 | |
|
| |||
| 10–25-word vocabulary | 18 | – | |
|
| |||
| ≥50-word vocabulary (50–300 words) | 24 (minimum) | – | |
|
| |||
| Two-word phrases | 24 | 20–30 | |
|
| |||
| Uses pronouns indiscriminately | 24 | 22–30 | |
|
| |||
| States first name | 34 | 30–40 | |
|
| |||
| Uses pronouns appropriately (i.e. I, you, we, me, they) | 36 | 30–42 | |
|
| |||
| >200-word vocabulary (200–1000 words) | 3 years | – | |
|
| |||
| 75% of speech intelligible to strangers | 3 years | – | |
|
| |||
| Three-word sentences | 3 years | – | |
WHAT CAUSES SPEECH AND LANGUAGE DELAY?
There is a range of acquisition of normal language milestones, and a delay may be detected if the development falls outside of what is expected. A delay can be significant, especially if it persists into school age, limits communication and learning and/or impairs social development. Speech and language delay may be idiopathic or may occur as a facet of an underlying medical condition or a social–environmental problem. Examples of these causes are listed in Box 1.[5]
Box 1.
Causes of delayed speech and language development and red flags.[5]
| Causes of delayed speech and language development |
| 1. Hearing impairment |
| 2. Perinatal risk factors resulting in hearing impairment |
| 3. Disorders of central nervous system processing: |
| (a) Global developmental delay |
| (b) Intellectual disability |
| (c) Autism spectrum disorder |
| 4. Developmental language disorders |
| 5. Disorders of speech production: |
| (a) Articulation disorder |
| (b) Dysarthria |
| (c) Verbal apraxia |
| 6. Presence of anatomic abnormalities (e.g. cleft lip, cleft palate) |
| 7. Environmental deprivation |
| Red flags in speech and language development |
| 1. Inconsistent or lack of response to auditory stimuli at any age |
| 2. Regression in language or social skills at any age |
| 3. No babbling by age 9 months |
| 4. No pointing or gesturing by age 12 months |
| 5. No intelligible single words by age 16 months |
| 6. No joint attention (i.e. following the eye gaze of others) by age 15 months |
| 7. No two-word spontaneous phrases by age 24 months |
| 8. Inability to respond to simple directions or commands (e.g. ‘sit down’, ‘come here’) by age 24 months |
| 9. Speech predominantly unintelligible at age 36 months |
| 10. Hypernasality at any age |
| 11. Inappropriate vocal quality, pitch or intensity at any age |
Decreased hearing acuity, whether bilateral or unilateral, can significantly impact speech and language development in early childhood. The earlier hearing loss occurs in a child’s life, the bigger the impact on the child’s development. When the problem is identified as early as possible, this negative impact can be reduced. Hence, the Joint Committee on Infant Hearing endorses early detection of hearing loss and intervention for infants with hearing loss and recommends that infants confirmed to have hearing loss should receive appropriate interventions by 6 months of age.[6] It is crucial to note that hearing loss may be progressive, and hence, may not be identified upon newborn screening. In addition, hearing loss may be acquired due to causes such as persistent otitis media with effusion, bacterial meningitis, exposure to ototoxic medications or severe hyperbilirubinaemia. As such, primary care physicians must be vigilant to identify parental concerns; children suspected to have hearing impairment and/or significant speech and language delay should be referred for a formal hearing assessment.
It is also pertinent to look out for features of autism spectrum disorder (ASD) in children who present with speech and language delay. Although most significant delays will be noted in language and social–emotional domains, delays may also be present in other domains of development. Caregivers may raise associated behavioural concerns that involve problems with social–emotional reciprocity, non-verbal communication and difficulty developing, maintaining and understanding relationships.[7] For example, children with ASD often have difficulty maintaining eye contact and using gestures to express their intentions. They may appear socially insensitive and are often focused on their own topics of interest, rather than the interests of others. Other features include repetitive and stereotypic motor movements, need for sameness and routines, fixed interests of abnormal intensity or focus, as well as increased or decreased reactivity to sensory input.[7] For example, they may often have an obsession for sameness in household routines and be resistant to change. Children with ASD may also develop strong interests in certain topics such as letters and numbers. Though some may be able to read as early as 2 years of age, they have difficulties in communicating with others and understanding what they read. These features, where present, should prompt primary care physicians to refer the child to a developmental paediatrician.
Environmental deprivation may also be a contributing factor to speech and language delay. This includes less-than-desirable circumstances such as poverty, parents with limited knowledge of child development, victims of child neglect or abuse, and lack of warm and nurturing parent–child interactions.
WHEN SHOULD I REFER TO A SPECIALIST?
The prognosis for children with speech and language delays depends on the nature and severity of the underlying cause, and the supports and interventions they received. Children identified to have speech and language delays in the context of global developmental delay, cognitive delay or ASD should be referred promptly to the appropriate medical or allied health professionals for evaluation and early intervention services.
‘Red flags’ are noted at ages where 90% of typically developing children have achieved a developmental milestone. A useful resource would be the developmental checklist in the health booklet, which is based on the Denver Developmental Screening Test-Singapore (DDST-Singapore).[8] This is currently the only tool that is standardised for the local population. The cut-offs on DDST-Singapore indicate 90th percentile norms of the population at the stated age (an item would be scored as ‘Delay’ when a child older than the 90th percentile passing age failed the item). Importantly, red flags [Box 1] may point towards an underlying cause of the child’s speech and language delay.[5] Knowing these can guide the primary care physician to initiate prompt and appropriate referrals to medical or allied health professionals in the tertiary institutions.
WHAT CAN I DO IN MY PRACTICE?
Early identification and appropriate management of developmental delays are essential and can positively alter the child’s developmental trajectory.[9] Parental concerns about developmental delays (be it perceived or true delays) should be addressed and promptly acted upon. Among all the developmental domains, speech and/or language concerns make up the most common presenting concern of parents, both locally and globally. This may be a result of concerns raised by childcare or preschool teachers and may arise from parents’ own observation of their children and comparison with other children, including the child’s siblings. Although it is pertinent for primary care physicians to be able to identify delays and make appropriate referrals where warranted, it is equally important for them to provide reassurance and allay parental anxiety in the absence of red flags.
Educating parents to make use of the health booklet’s developmental checklist is key as a first step towards early identification.[10] Apart from early identification, parents may also be taught to use the checklist as a guide to work towards the next milestone. Through developmental surveillance, parents must be encouraged to raise any concerns during each well-child visit.
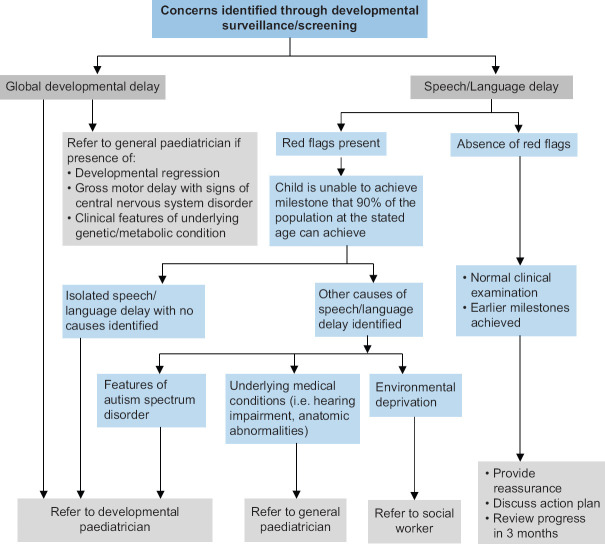
As highlighted earlier, red flags identified through developmental surveillance and developmental screening should prompt an early specialist review. Some children may have a mild speech and/or language delay (but still remain within the 90th percentile based on DDST-Singapore). In such cases, in the absence of red flags and with a normal clinical examination, parents can be counselled on the acceptable norm and appropriate stimulation activities [Box 2].[11,12] Together, the primary care physician and parents can work on an action plan [Box 3] and decide on goals which can be reviewed at the next follow-up visit. Figure 1 illustrates a framework for this process.[13]
Box 2.
| 1. When your child starts an interaction through talking, gesture or behaviour, respond to it. Assume your child is talking back to you even if he/she makes sounds, babbles or simply paying attention to you. |
| 2. Pause and give your child the opportunity to initiate or take his/her turn in the interaction. |
| 3. Repeat what your child has said and expand on them. For example, if your child says ‘car’, you can say ‘blue car’ or ‘Daddy is in the car’. |
| 4. Use opportunities in the daily routines. For example, teach body parts during bath time, teach colours/quantity of food during meals. |
| 5. Talk about things as they happen (e.g. when you change your child, watch television, go to a shop) or whatever your child is interested in. |
| 6. Expose your child to lots of different words in lots of different contexts (e.g. this is your cup, this is mummy’s cup, mummy’s cup is big, your cup is small). |
| 7. Give choices (e.g. ‘Do you want to wear shoes or sandals?’). |
| 8. Read and share books with your child from birth. Talk about the pictures and point to the words as you read them. Make it a daily routine if you can. |
| 9. Sing songs and nursery rhymes, paired with actions as much as possible. |
Box 3.
Parental counselling: a proposed action plan.
| 1. Educate |
| (a) Inform parents about normal speech and language development. |
| (b) Emphasise the potential red flags to look out for. |
| (c) Share on communication skills, which form the foundation for learning, play, social interaction and building relationships with others. |
| 2. Empower and equip |
| (a) Equip parents with general strategies to promote speech and language development and communication. |
| (b) Identify specific issue for the child, that is, receptive/expressive language or speech, and tailor advice towards it. |
| (c) Introduce stimulation activities and learning games. |
| 3. Encourage exposure |
| (a) Work on the milestone that the child had not been able to achieve. |
| (b) Work towards the next milestone based on the Denver developmental screening test. |
| 4. Evaluate |
| (a) Arrange for follow-up visit in 3 months to review progress. |
| (b) Counsel parents that the child may need a specialist referral if there are red flags or if concerns of speech and language delay persist despite exposure. |
Figure 1.
A framework for management of speech and language delay in the primary care setting.[13]
Concerns with speech and language delay inevitably lead to parental anxiety, and these must be adequately addressed. In cases where a referral is indicated, parents can still be counselled on appropriate stimulation activities. In such situations, the primary care physician should also counsel the parents on the potential evaluation and intervention that may take place in the tertiary setting. For example, this would usually include a hearing assessment and review by a general paediatrician and a speech and language therapist. In certain cases, a direct referral to a developmental paediatrician may be necessary.
In Singapore, many families speak more than one language at home. Evidence indicates that bilingualism does not result in language delays, but is associated with increased cognitive control such as improved executive function skills and mental flexibility.[14] The home language should be preserved wherever possible; an option would be the one person–one language model, where each parent is encouraged to use his or her own language with their child. This enables parents to connect with their children in their own native language and allows the child to hear and speak both languages too. When there are significant concerns of speech and language delay in a bilingual child, a specialist referral should be made. Each family is unique. Hence, a case-by-case approach is frequently taken, with consideration given to the family setup as well as the caregivers’ degree of confidence and proficiency in the spoken languages.
Last but not least, primary care physicians should actively reinforce recommendations on the use of digital media in early childhood. Studies show associations between excessive screen time in early childhood and cognitive, language and social–emotional delays that are likely secondary to reduced opportunities for parent–child interaction. As per the latest American Academy of Pediatrics guidelines,[15] children below 18 months of age should avoid use of screen media other than video chatting. For those between aged 18 months and 2 years, any media should be of high quality, and parents should watch these programmes with their children to help them understand the content. For children aged 2–5 years, screen usage should be limited to an hour of high-quality programmes per day, with adult supervision. In the primary care setting, it is also crucial to promote healthy habits within families with regard to the use of digital media.[15] Some examples include the following:
Avoid the use of digital media for both parents and children during mealtimes, before bedtime and during parent–child playtime.
Avoid the use of digital media as the only means of calming children down.
Switch off televisions and other devices when not in use.
Most importantly, digital media must not replace parent–child interaction. Caregivers should take every opportunity to interact, connect and communicate with their children.
TAKE HOME MESSAGES
Speech is the verbal production of language, whereas language encompasses the understanding, processing and production of communication.
Speech and language delay may be idiopathic or may occur as a facet of an underlying medical condition or a social–environmental problem.
Primary care physicians play a crucial role in early identification of speech and language delay, and specialist referrals should be initiated when red flags are present.
In instances where speech and language delay is mild with no red flags, the primary care physician should provide reassurance, discuss an action plan and monitor the child’s progress.
Parental counselling on the anticipated evaluation and intervention should be provided when specialist referrals are warranted.
Primary care physicians should actively counsel caregivers on the use of stimulation activities and strategies to promote speech and language development for their children.
Closing Vignette
You performed a full developmental assessment for Aaron. Aside from mild expressive language delay, you assessed that the rest of his developmental domains were age appropriate. Aaron had been meeting all his developmental milestones during the previous touchpoints of developmental screening. No red flags were identified thus far. You reassured his parents and allayed their anxiety. You educated them on normal speech and language development and the red flags they should look out for. Together with them, you worked on an action plan and provided them with strategies to improve Aaron’s language and communication skills. You arranged a follow-up visit in 3 months to review his speech and language development.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We wish to acknowledge Dr Sylvia Choo Henn Tean (Senior Consultant, Department of Child Development, KK Women’s and Children’s Hospital, Singapore) and Ms Goh Siew Li (Head, Speech Language Therapy Service, KK Women’s and Children’s Hospital, Singapore) for their invaluable input and feedback in the writing of this article.
SMC CATEGORY 3B CME PROGRAMME
Online Quiz: https://www.sma.org.sg/cme-programme
Deadline for submission: 6 pm, 05 January 2024
| Question | True | False |
|---|---|---|
| 1. Speech and language concerns are the most common presenting developmental concerns from parents. | ||
|
| ||
| 2. The use of signs and gesturing for communication is a form of expressive language. | ||
|
| ||
| 3. Preschool children with untreated speech and language delay may be at higher risk of behavioural problems. | ||
|
| ||
| 4. Speech and language development arises only from environmental stimulation. | ||
|
| ||
| 5. Within the first 3 years of life, children express a lot more than they can understand. | ||
|
| ||
| 6. Speech and language delay may occur as part of an underlying medical condition or social–environmental problem. | ||
|
| ||
| 7. Unilateral hearing impairment can significantly affect speech development. | ||
|
| ||
| 8. Infants with hearing loss should receive early intervention by 2 years of age. | ||
|
| ||
| 9. A normal newborn hearing screen indicates that speech and language delay is not secondary to hearing impairment. | ||
|
| ||
| 10. Autism spectrum disorder presents with delays in language and social domains only. | ||
|
| ||
| 11. A social history should be taken for children with speech and language delays as environmental deprivation can be a contributing factor. | ||
|
| ||
| 12. Children identified to have global developmental delay should be immediately referred for specialist review. | ||
|
| ||
| 13. Children unable to achieve a milestone that 90% of the population at the stated age can achieve should be followed up again in 3 months for review and referred for specialist evaluation if the delay persists. | ||
|
| ||
| 14. In cases where children are referred to a specialist for further evaluation of speech and language delay, parents should be advised to await specialist review before attempting stimulation activities at home. | ||
|
| ||
| 15. Following commands is a form of receptive language development. | ||
|
| ||
| 16. The average age range for children to respond to their name is 9–12 months. | ||
|
| ||
| 17. The development of appropriate use of pronouns occurs at a mean age of 3 years. | ||
|
| ||
| 18. The average age range for children to say their first name is 30–40 months. | ||
|
| ||
| 19. Inconsistent or lack of response to auditory stimuli is a red flag at age 6 months and above. | ||
|
| ||
| 20. No babbling by age 6 months is a red flag in speech and language development. | ||
REFERENCES
- 1.Wallace IF, Berkman ND, Watson LR, Coyne-Beasley T, Wood CT, Cullen K, et al. Screening for speech and language delay in children 5 years old and younger: A systematic review. Pediatrics. 2015;136:e448–62. doi: 10.1542/peds.2014-3889. [DOI] [PubMed] [Google Scholar]
- 2.Stern LM, Connell TM, Lee M, Greenwood G. The Adelaide preschool language unit: Results of follow-up. J Paediatr Child Health. 1995;31:207–12. doi: 10.1111/j.1440-1754.1995.tb00787.x. [DOI] [PubMed] [Google Scholar]
- 3.Snowling MJ, Adams JW, Bishop DV, Stothard SE. Educational attainments of school leavers with a preschool history of speech-language impairments. Int J Lang Commun Disord. 2001;36:173–83. doi: 10.1080/13682820010019892. [DOI] [PubMed] [Google Scholar]
- 4.Wee BL, Ho SKY, Choo SHT, Shah VA, Chan DWL, Yeo CL, et al. Children with developmental and behavioural concerns in Singapore. Singapore Med J. 2012;53:439. [PubMed] [Google Scholar]
- 5.Berkowitz, Carol D. Berkowitz's Pediatrics: A Primary Care Approach. Sixth revised edition. American Academy of Pediatrics; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120:898–921. doi: 10.1542/peds.2007-2333. [DOI] [PubMed] [Google Scholar]
- 7.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) American Psychiatric Pub; 2013. May 22, [Google Scholar]
- 8.Lim HC, Chan T, Yoong T. Standardisation and adaptation of the Denver Developmental Screening Test (DDST) and Denver II for use in Singapore children. Singapore Med J. 1994;35:156–60. [PubMed] [Google Scholar]
- 9.Choo YY, Agarwal P, How CH, Yeleswarapu SP. Developmental delay: Identification and management at primary care level. Singapore Med J. 2019;60:119–23. doi: 10.11622/smedj.2019025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choo YY, Yeleswarapu SP, How CH, Agarwal P. Developmental assessment: Practice tips for primary care physicians. Singapore Med J. 2019;60:57–62. doi: 10.11622/smedj.2019016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Speech-Language-Hearing Association (ASHA). (n.d.) Activities to Encourage Speech and Language Development. ASHA. [[Last accessed on 2022 Feb 12]]. Available from: https://www.asha.org/public/speech/development/activities-to-encourage-speech-and-language-development/
- 12.Families for Life. (n.d.) Talking with babies and toddlers: Why it's important. [[Last accessed on 2022 Feb 12]]. Available from: https://familiesforlife.sg/parenting/Toddlers/Pages/ToddlersDevelopment/ToddlersLanguage_Development/Toddlers_Importance_Talking.aspx .
- 13.Ministry of Health, Singapore. Circular 183/2020. Guidance on childhood development screening. [[Last accessed on 2022 Feb 12]]. Available from: https://www.cfps.org.sg/assets/1-Circular-for-GPs/5-MOH-Cir-No-183-2020-13Jul20-CDS-Guidance-Drs.pdf .
- 14.Bialystok E, Craik FI, Luk G. Bilingualism: Consequences for mind and brain. Trends Cogn Sci. 2012;16:240–50. doi: 10.1016/j.tics.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hill D, Ameenuddin N, Reid Chassiakos YL, Cross C, Hutchinson J, Levine A, et al. Media and young minds. Pediatrics. 2016;138:e20162591. doi: 10.1542/peds.2016-2591. [DOI] [PubMed] [Google Scholar]