Abstract
Adnexal torsion is an emergency commonly presenting in women of reproductive age. Timely diagnosis and management are needed to preserve the ovary. Recurrence is more uncommon. This article presents a case of recurrent torsion, and reviews the literature to highlight the significance of early diagnosis and management. The case is presented of a nulliparous 31-year-old woman who presented on five occasions with symptoms of acute pain and vomiting. Adnexal torsion was suspected on clinical assessment and ultrasound scan. She was found to have left-sided isolated fallopian tube torsion twice, and tubo-ovarian torsion on two occasions. Detorsion was performed four times. Bilateral oophoropexy was performed during an emergency laparoscopy on the fourth presentation. The left ovary was conserved, but viability was doubted. She presented four weeks later with similar symptoms. An intraoperative finding was of an auto-amputated left ovary with no attachment to infudibulopelvic ligament. This ovary was removed. Operative management was performed promptly, but planned oophoropexy was delayed, and an earlier procedure may have resulted in conservation of the ovary. There is no standardised management for prevention of recurrent ovarian torsion. The benefits of oophoropexy to prevent further torsion versus risks lack evidence. There is also debate as to the method by which oophoropexy is done. There is no consensus or guideline regarding the best management approach for recurrent adnexal torsion. Further research is needed to obtain evidence to support clinicians in discussing management options with their patients.
Keywords: Ovarian torsion, Fallopian tube torsion, Recurrent torsion, Oophoropexy, Case report
Highlights
-
•
Recurrent ovarian torsion and isolated fallopian tube torsion are rare.
-
•
Unlike ovarian torsion, there are no classical clinical characteristics or investigations for the diagnosis of isolated fallopian tube torsion.
-
•
Oophoropexy is an option to manage recurrent ovarian torsion, with various techniques used, but with a lack of evidence regarding the best approach.
1. Introduction
Ovarian torsion accounts for up to 7.4% of gynaecological emergencies [1]. This occurs when the ovary and occasionally the fallopian tube twists around its supporting tissue and vascular supply [2]. It most commonly presents in women of reproductive age [1,3]. Timely diagnosis and management are needed to prevent necrosis and preserve the ovary and therefore fertility [1,3]. Recurrent torsion is more uncommon. However, those with torsion in the absence of an adnexal mass may have a higher risk of recurrence than those with an adnexal mass [4,5]. This article discusses a patient who presented on multiple occasions with acute pelvic pain. She was diagnosed and surgically managed for recurrent left-adnexal torsion. Bilateral oophoropexy was performed as an emergency to prevent further torsion. The article discusses this case in detail, the risk factors and diagnosis recurrent torsion, isolated fallopian tube torsion, and the merits and methods of oophoropexy.
2. Case Presentation
A nulliparous 31-year-old woman presented on five occasions over three years with symptoms of acute pelvic pain and vomiting. Adnexal torsion was suspected on clinical assessment and ultrasound scan at each visit. She had a history of polycystic ovaries. No adnexal masses were found on ultrasonography, and the ovaries were not enlarged. In total she was found to have left-sided isolated fallopian tube torsion twice and tubo-ovarian torsion on a further two occasions. Laparoscopic detorsion was performed four times. She was found to have absent left mesosalpinx and bilateral elongated fallopian tubes. She was placed on a waiting list for elective oophoropexy after the second episode, with the aim of preventing recurrence of torsion. This was unfortunately cancelled on more than one occasion due to constraints on elective theatre lists during the COVID-19 pandemic. Bilateral oophoropexy was performed during emergency laparoscopy (on the patient's fourth presentation) for another episode of torsion involving the left fallopian tube and ovary [Fig. 1]. Detorsion was performed and the ovary was conserved. The viability of the ovary was however doubtful both on pre-operative ultrasound assessment and at laparoscopy. She presented four weeks following oophoropexy with symptoms of acute right iliac fossa pain. An ultrasound scan showed an avascular ovary on colour Doppler [Fig. 2]. The suspicion of torsion was low; however, she was taken for laparoscopy given her previous history. An intraoperative finding at this time was of a necrosed left ovary that had auto-amputated, with no attachment to infudibulopelvic ligament [Fig. 3]. This ovary was removed. The contralateral tube and ovary were healthy.
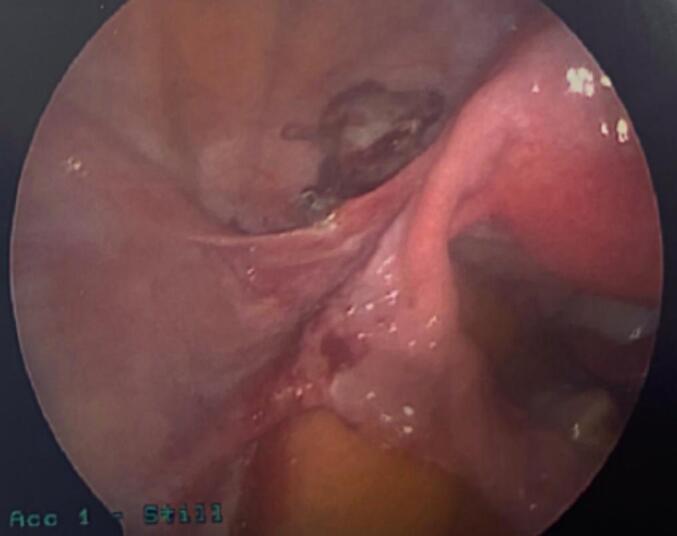
Fig. 1.

Laparoscopic image showing torted left fallopian tube and oedematous/congested left ovary.
Fig. 2.

This ultrasound image of the patient shows a small avascular left ovary.
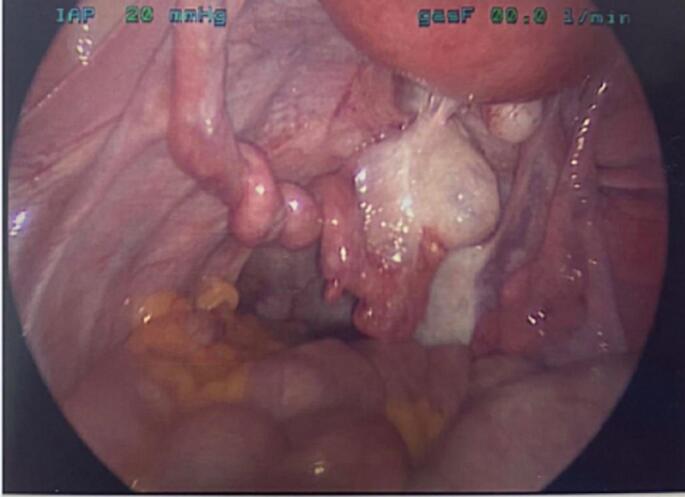
Fig. 3.
A necrotic left ovary is seen, attached to oophoropexy suture on the round ligament, but detached from the infundibulopelvic ligament.
2.1. Outcome and Follow-Up
The patient presented once more following her final laparoscopy with similar pelvic pain. However, on ultrasound no signs of torsion were seen. She was reassured and safety-netting advice was given. The patient was understandably cautious due to her previous multiple operations, and had concerns regarding fertility given she now had one ovary. No outpatient follow-up was arranged but it was made clear to the patient that a swift review and scan would be offered should she have any further acute pain. She later had successful oocyte cryopreservation privately due to her keen wish to ensure fertility.
3. Discussion
Torsion causes disruption of the blood supply to the ovary, which can lead to necrosis. Therefore, early diagnosis is of paramount importance in conserving the adnexa [1,3]. This patient had classic symptoms of unilateral pain and vomiting at each presentation. Prompt clinical assessment and ultrasound by senior members of the team that showed typical features of torsion allowed timely surgical intervention during her visits. Diagnosis of ovarian torsion is made following comprehensive clinical history and examination in combination with ultrasound [1]. Clinical history usually includes acute-onset severe pelvic pain [1,2]. This is often severe and unilateral, and in up to 85% is accompanied by nausea and vomiting [1,2,6]. However, many patients present with milder, non-specific pelvic pain [1,2,6]. There may be a history of risk factors for torsion. This may include ovarian cyst or mass, polycystic ovaries, or recent induction of ovulation due to treatments for infertility [[1], [2], [3]]. The patient may present with tachycardia and low-grade fever [1]. On examination, generalised or localised tenderness may be found on palpation of the abdomen [1,2]. On digital examination of the vagina, tenderness in the adnexa, cervical excitation, and adnexal masses may be palpated [1,2]. This patient presented on each occasion with acute-onset generalised pelvic pain and tenderness. She had some nausea on each occasion and vomiting on one occasion.
Ultrasonographic features of ovarian torsion include tender examination, unilateral enlarged ovary, peripherally displaced follicles, presence of an ovarian mass, thickened ovarian tissue due to oedema, follicular ring sign, twisted pedicle ‘target sign’ (Fig. 4), and free fluid in the pelvis [7,8]. There may also be an absence of venous or arterial blood flow to the ovary [9]. Many of these features were seen on ultrasonography of this patient. This included unilateral oedematous ovary, target sign, and lack of vascularity to the ovary and follicular ring sign. However, despite these features which may be seen on ultrasound there is up to a 27.9% false negative rate in ultrasonographic diagnosis of torsion [10].
Fig. 4.
Ultrasound image of the patient demonstrating target sign to the left of the uterus indicating a twisted pedicle.
Ovarian torsion is more common on the right-hand side, [3,11]. This patient however had left-sided torsion on all four occasions. She had isolated fallopian tube torsion on the left on two occasions. The congenital absence of mesosalpinx, and bilateral elongated fallopian tubes may have been the contributing factors to her having recurrent adnexal torsion that involved ovary on two occasions, and finally resulted in loss of the ovary. She also had polycystic ovaries, which are a risk factor for ovarian torsion [2,3]. Other risk factors for ovarian torsion include large ovarian cysts (over 5 cm) [1], ovarian cancers [11], and ovarian enlargement following induction of ovulation [10]. There is some evidence that those who have ovarian torsion without ovarian masses or enlargement are at higher risk of recurrence of torsion [4,5]. This was the case in this patient.
Isolated fallopian tube torsion is rare [[12], [13], [14]]. Risk factors include hydro- or haematosalpinx, elongated fallopian tubes, absence of mesosalpinx, and tubal masses [13,14]. Unlike ovarian torsion, there are no clear classical clinical characteristics or investigations for the diagnosis of a tube torsion [12,13]. There is therefore unfortunately more often a delay in diagnosis and intervention, and therefore an increased risk of harm to the tube which is irreversible [12]. Ultrasonographic features may demonstrate a thickened or dilated fallopian tube, haematosalpinx, or absent blood flow on colour Doppler with normal appearance of the ovary [12,13]. Definitive diagnosis is however usually made at diagnostic laparoscopy [13]. There have been very few studies, but the literature states that there may only be up to 29.6% of isolated fallopian tube torsion correctly diagnosed by ultrasound [15], with the remaining having a false negative ultrasound result. On the two occasions when this patient presented with isolated left fallopian tube torsion, she did so with acute-onset left-sided lower abdominal pain. Her left fallopian tube was long and she also had an absent mesosalpinx on this side (Fig. 5). This was likely the cause of her isolated fallopian tube torsion. There was tenderness on examination, and dilatation of fallopian tube seen on ultrasonography leading to suspicion of fallopian tube torsion. The diagnosis was confirmed at the time of laparoscopy.
Fig. 5.
Laparoscpic image of the patient showing isolated left fallopian tube torsion, elongated tube, absent mesosalpinx and normal ovary.
Recurrent ovarian torsion is rare. Up to 80% of those presenting with ovarian torsion have an ovarian mass. Only 8.7% of these present with recurrent torsion [4]. However, it is more common in those with torsion and an adnexa without an ovarian mass [4]. This has a rate of recurrence of up to 63% [4]. There is no standardised management for prevention of recurrence. Oophoropexy is a commonly used surgical technique to manage and prevent recurrent ovarian torsion. Oophoropexy has several techniques. These include plication of the ovarian ligament, fixation of the ovary to the lateral pelvic wall, rear of the uterus, or posterior abdominal wall, or utero-ovarian ligament shortening [3,16]. Plication of the utero-ovarian ligament may be associated with minimum disruption of the anatomical relationship between the tube and the ovary, therefore possibly having less effect fertility. The benefits of oophoropexy to prevent further torsion versus theoretical risks lack in evidence. The literature states that the risks of oophoropexy may include disruption of blood supply to the fallopian tube, and disruption of physiological relationship between fallopian tube and ovary [3]. There may also be a risk of detachment from the infundubulopelvic ligament. In this case, it is unclear whether detachment of the ovary following oophoropexy happened as a result of oophoropexy or if the ovary was already non-viable. It was strongly suspected to be non-viable pre- and intraoperatively. It was unfortunate in this case that planned oophoropexy was delayed. An earlier procedure may have resulted in conservation of the left ovary. There is some evidence that interval oophoropexy may be more successful than performing this as an emergency procedure at the time of detorsion, [17]. This may be due to concerns about fragile and ischaemic tissue causing instability of sutures when oophoropexy is performed at the time of diagnosis [3,17]. This was the reasoning in this case for not initially performing oophoropexy during the emergency procedure.
4. Conclusion
-
•
It is imperative that patients with suspected torsion are scanned or have laparoscopy to diagnose and manage torsion promptly in order to aim to restore blood supply and save the ovary.
-
•
Diagnosis via ultrasound may be difficult in up to 30% of cases of ovarian torsion, and 70% of cases of isolated fallopian tube torsion. Therefore, if there is a strong clinical suspicion, a diagnostic laparoscopy should not be delayed [10,15].
-
•
There is a lack of robust evidence and no guideline regarding the best management approach for recurrent ovarian or fallopian tube torsion, including timing and method of oophoropexy.
Acknowledgments
Patient perspective
I was grateful for the quick diagnosis and management I received from the team. I have been very concerned regarding my fertility, but now feel reassured as I have had no pain episodes for almost 1 year, and now that I have frozen some eggs.
Contributors
Lili Ellison contributed to acquiring and interpreting the data, drafting the manuscript, undertaking the literature review and revising the article critically for important intellectual content.
Katherine Sinclair contributed to acquiring and interpreting the data, drafting the manuscript, and revising the article critically for important intellectual content.
Yasmin Sana contributed to conception of the case report, provided images, and revised the article critically for important intellectual content.
All authors contributed to patient care. All authors approved the final version of the case report.
Funding
The authors received no funding from an external source.
Patient consent
Written consent was obtained from the patient to publish this case and accompanying images.
Provenance and peer review
This article was not commissioned and was peer reviewed. Peer review was directed by Professor Margaret Rees, Editor in Chief, and Dr. Dudley Robinson, an editor of Case Reports in Women's Health and member of the same institution as the authors, was blinded to the process.
Acknowledgments
Conflict of interest statement
The authors declare that they have no conflict of interest regarding the publication of this case report.
References
- 1.Iatrikes E.D.P., Johns J. An update on the diagnosis and management of ovarian torsion. Obstet. Gynaecol. 2012;14:229–236. [Google Scholar]
- 2.White M., Stella J. Ovarian torsion: 10-year perspective. Emerg. Med. Aust. 2005;17:231–237. doi: 10.1111/j.1742-6723.2005.00728.x. [DOI] [PubMed] [Google Scholar]
- 3.Hartley J., et al. Oophoropexy for Recurrent Ovarian Torsion. 2018. https://www.hindawi.com/journals/criog/2018/8784958/ Case reports in Obstetrics and Gyanecology. [DOI] [PMC free article] [PubMed]
- 4.Pansky M., et al. Torsion of normal adnexa in postmenarchal women and risk of occurrence. Obstet. Gynaecol. 2007;109:355–359. doi: 10.1097/01.AOG.0000250969.15438.17. [DOI] [PubMed] [Google Scholar]
- 5.Hyttel T.E.W., et al. Re-torsion of the ovaries. Acta Obstet. Gynecol. Scand. 2014;94(3):236–244. doi: 10.1111/aogs.12542. [DOI] [PubMed] [Google Scholar]
- 6.Jain N., et al. Adnexal torsion-symptoms, diagnosis and management: a review of literature. Int. J. Reproduct. Concept. Obstet. Gyanecol. 2016;5:1276–1284. [Google Scholar]
- 7.Duigenan S., et al. Ovarian torsion: diagnostic features on CT and MRI with pathologic correlation. Am. J. Roentgenol. 2012;198:122–131. doi: 10.2214/AJR.10.7293. [DOI] [PubMed] [Google Scholar]
- 8.Pearls and Pitfalls in Diagnosis of Ovarian Torsion, Chang H., et al. Pearls and pitfalls in diagnosis of ovarian torsion. RadioGraphics. 2008;28:1355–1368. doi: 10.1148/rg.285075130. [DOI] [PubMed] [Google Scholar]
- 9.Sibal M. Follicular ring sign. J. Ultrasound Med. 2012;31:1803–1809. doi: 10.7863/jum.2012.31.11.1803. (Accessed on 29/4/21) [DOI] [PubMed] [Google Scholar]
- 10.Rostamzadeh A., et al. Diagnostic efficacy of sonography for diagnosis of ovarian torsion. Pakistan J. Med. Sci. 2014;30(2):413–416. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3999021/ (Accessed on 31/1/2022) [PMC free article] [PubMed] [Google Scholar]
- 11.Weitzman V.N., et al. Prevention of recurrent adnexal torsion. Fertil. Steril. 2008;90:5. doi: 10.1016/j.fertnstert.2008.02.144. [DOI] [PubMed] [Google Scholar]
- 12.Bora S.A., et al. Isolated fallopian tube torsion: an unusual cause of acute abdominal pain. BMJ Case Rep. 2011 doi: 10.1136/bcr.05.2011.4183. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3171034/ bcr0520114183 (Accessed on 29/4/21) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kardakis S., et al. Isolated Fallopian Tube Torsion. 2013. https://www.hindawi.com/journals/criog/2013/479698/ Case Reports in Obstetrics and Gynaecology. [DOI] [PMC free article] [PubMed]
- 14.Gross M., et al. Isolated fallopian tube torsion: a rare twist on a common theme. Am. J. Roentgenol. 2005;185:1590–1592. doi: 10.2214/AJR.04.1646. [DOI] [PubMed] [Google Scholar]
- 15.Raban O., et al. Isolated fallopian tube torsion: a unique ultrasound identity or a serial copycat? J. Ultrasound Med. 2018;37(10):2387–2393. doi: 10.1002/jum.14595. https://pubmed.ncbi.nlm.nih.gov/29573346/ (Accessed on 31/1/2022) [DOI] [PubMed] [Google Scholar]
- 16.Hosny T.A. Oophoropexy for ovarian torsion: a new easier technique. Gynaecol. Surg. 2017;14:7. doi: 10.1186/s10397-017-1001-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fee E.K., et al. Recurrent ovarian torsion in an adolescent after oophoropexy. J Pediatr Surg Case Rep. 2017;19:22–24. [Google Scholar]



