Abstract
Herlyn-Werner-Wunderlich (HWW) syndrome is a rare and complex congenital anomaly of the genitourinary system characterized by uterus didelphys, an obstructed hemivagina, and ipsilateral renal agenesis. It is the result of the maldevelopment of both the Mullerian and Wolffian ducts. Clinical manifestations of dysmenorrhea, dysuria, and urinary retention appear after menarche due to the accumulation of menstrual blood and distention of the obstructed hemivagina. Diagnosis of this anomaly is often delayed, and the obstructive nature of the condition is missed due to cyclic menstruation from the one canalized hemivagina. This case report represents a typical form of HWW syndrome to highlight the importance of considering this rare entity in an adolescent girl presenting with signs of dysmenorrhea and urinary complaints. A 13-year-old patient was presented at the obstetrics and gynecology clinic due to low abdominal pain and urinary retention on the fifth day of menstruation. For the last 6 months, the patient suffered progressive cyclic low abdominal pain associated with menstruation. Inspection of the external genitalia was unremarkable, and the hymenal membrane had a normal oval opening. An ultrasound examination revealed the sonographic features of the didelphys uterus and was suggestive of a right obstructed hemivagina with hematocolpos. Magnetic resonance imaging and computed tomography urography showed evidence of didelphys uterus, right blind obstructed hemivagina associated with huge hematocolpos, and ipsilateral renal agenesis. The diagnosis of HWW syndrome was established. Surgical resection of the vaginal septum was undertaken without delay, and the patient was discharged the following days.
Keywords: Embryonic development, Mullerian ducts, Hematocolpos, Dysmenorrhea, Magnetic resonance imaging
Introduction
Herlyn-Werner-Wunderlich (HWW) syndrome is a rare and complex congenital anomaly of the genitourinary system characterized by uterus didelphys, an obstructed hemivagina, and ipsilateral renal agenesis [1]. The exact etiology is yet to be determined; however, results from recent studies suggest a potential cause can be a specific group of genes that simultaneously are responsible for the agenesis of the kidneys. With a rare incidence of approximately 0.1%-3.5% of all Mullerian anomalies, the diagnosis of this condition is often missed and delayed even when the first and very nonspecific symptoms appear [2].
Clinical manifestations of severe dysmenorrhea and urinary retention are related to the onset of menarche, worsening in following cycles due to the accumulation of blood in the obstructed hemivagina. Nonetheless, diagnosis of HWW syndrome is challenging. It has an exceptionally rare incidence and is often overlooked because menstruation occurs from the normally canalized hemivagina. These factors may lead to the wrong exclusion of an obstructive anomaly, leading to a delayed diagnosis. Although uncommon, this syndrome can cause severe complications, so it mustn't be overlooked. An early diagnosis can best be reached by imaging diagnostic procedures such as an ultrasonographic examination, while magnetic resonance imaging (MRI) is the gold standard for diagnosis [3]. Surgical intervention utilizing a vaginal septum resection is necessary and should be performed without delay in order to drain the accumulated blood, subside the symptoms, and prevent further complications.
Case presentation
A 13-year-old patient was presented at the obstetrics and gynecology clinic due to severe lower abdominal pain and urinary retention on the fifth day of menstruation. Based on the patient's history, menarche occurred at the age of 12, and for the last 6 months, the patient suffered progressive cyclic lower abdominal pain associated with menstruation and dysuria. The patient's family and personal history were without remarkable medical or surgical conditions. She had made several checkups at the family doctor and was incorrectly diagnosed with dysmenorrhea, for which she was prescribed NSAID and later contraceptives. Her menstrual cycle was 28 days, with menstruation lasting an average of 5-6 days. The lower abdominal pain was described as related to her menstruation, lasting usually 4-5 days after menstruation began. On examination, the female patient, 158 centimeters, weighing 53 kg, had normally developed secondary sexual characteristics. On palpation, the lower abdomen was firm and sensitive. By inspection, the external genitalia were normally developed, and the hymenal membrane had a normal oval opening through which menstrual blood was seen to be flowing. Using a vaginoscope, the vagina was examined and appeared to be normally canalized and of normal length. Laboratory analysis, including blood count number, C-reactive protein, and sedimentation rate, were nonremarkable. A transabdominal pelvic ultrasound was performed, and the patient was observed to have 2 divergent uterine horns, 2 endometrial stripes, each 3 mm thick, and 2 cervixes. The ultrasound examination revealed features correlating to uterus didelphys. Below the right uterine horn, a large fluid-filled echogenic structure measuring 100 × 60 mm was observed (Fig. 1).
Fig. 1.
Transabdominal ultrasonographic imaging of uterus didelphys and a large fluid-filled structure suggesting hematocolpos.
The right kidney couldn't be visualized during the ultrasound examination, suggesting ectopic or renal agenesis as possibilities. An MRI scan of the pelvis and abdomen was performed to confirm a diagnosis. The MRI imaging revealed clear evidence of uterus didelphys, as shown in Fig. 2.
Fig. 2.
MRI of the pelvis. The MRI imaging demonstrates uterus didelphys and both hemivaginas; the left hemivagina collapsed, and the right one distended.
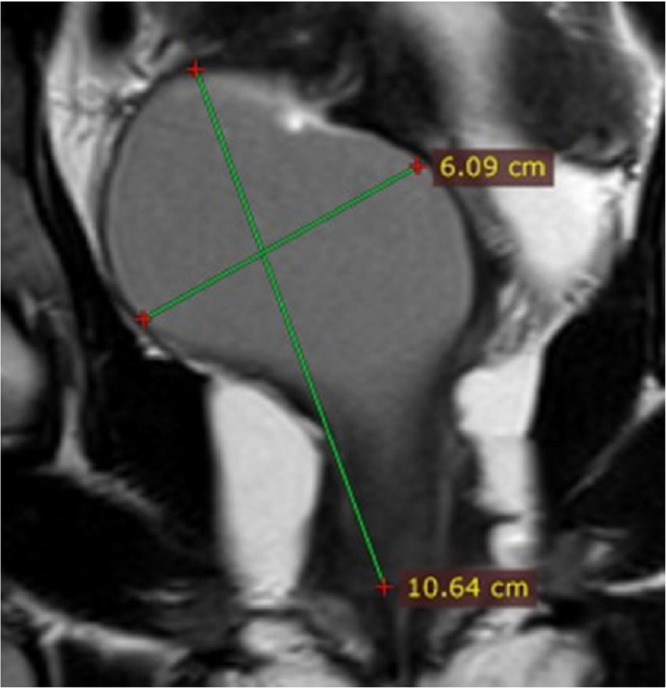
The left uterine horn continued normally through the left cervix into the collapsed left hemivagina, and the right uterine horn passed through the right cervix into the right hemivagina, which was distended with fluid content with dimensions of 10.6 × 6.0 centimeters, suggesting hematocolpos (Fig. 3).
Fig. 3.
MRI of the pelvis. MRI showed a markedly distended vagina measuring 10.64 × 6.09 cm.
A CT urography was also performed, confirming the absence of the right kidney, while the left kidney was hypertrophic and had a dilated pylon (Figs. 4A and B).
Fig. 4.
CT urography (A) CT urography showing absent right kidney (B) excretory phase showing hypertrophic left kidney.
With the ultrasonography, MRI, and CT examination, a diagnosis of HWW syndrome was established.
Following preoperative preparation, the patient was placed under spinal anesthesia, and surgical intervention was undertaken. Per vaginam, the vaginal septum was resected until the right cervix was visible. Approximately 800 mL of blood was drained from the right obstructed hemivagina. To prevent closure, the edges of the resected septum were sutured with 3.0 vicryl absorbent sutures to the anterior/posterior vaginal walls. A postoperation ultrasound confirmed that the hematocolpos was treated, and all blood was drained successfully.
After 3 days of close monitoring, no complications arose, and the patient was discharged with no complaints.
Discussion
Herlyn-Werner-Wunderlich syndrome is a complex and rare congenital genitourinary anomaly characterized by uterus didelphys, obstructed hemivagina, and ipsilateral renal agenesis. It was first reported in 1971 when Herlyn and Werner described the association of renal agenesis with ipsilateral blind hemivagina and added to in 1976 by Wunderlich, who described a uterus anomaly named bicornuate uterus, which completed the triad of this syndrome [4].
The estimated overall prevalence of Mullerian duct anomalies is 2%-3% of women in the general population, while the exact incidence of HWW syndrome is unknown. According to the literature, it represents approximately 0.1%-3.5% of Mullerian anomalies [2]. In most reported cases, renal anomalies are ipsilateral or on the same side as the obstructed hemivagina, and the anomaly is more commonly on the right side, as in the presented case [5], [6], [7].
Pathogenesis of HWW syndrome is very complex, involving the maldevelopment of both Mullerian and Wolfian ducts in genetically female-determined embryos [8,9]. In female embryos, the Mullerian ducts have the essential role of developing the internal female genitalia, including the fallopian tubes, uterus, cervix, and two-thirds of the upper portion of the vagina. The Wolfian ducts, on the other hand, play a role in the differentiation of the Mullerian ducts and initial renal embryogenesis. During the seventh to eighth week of embryogenesis, the Mullerian ducts lie between the Wolfian ducts and adjacent to the urogenital septum. During this period, specific teratogen agents are believed to cause embryological arrest affecting both the Mullerian and Wolfian ducts, resulting in HWW syndrome [10]. Different studies suggest that this embryological arrest may be caused by several different genetic, environmental, or endocrine factors [11]. A recent study conducted by Li et al. [12], which involved 12 patients with HWW syndrome, demonstrated that the same genes causing renal agenesis, such as CHD1L, TRIM32, RET, and WNT4, are potentially associated with the pathogenesis of HWW syndrome. This study set a good foundation; however, more in-depth studies with larger patient groups are required to explore the exact genetic pathogenesis of HWW syndrome.
HWW syndrome often remains asymptomatic and undetected until adolescence. With the onset of menarche, menstrual blood flows from the unobstructed hemivagina. However, in the obstructed hemivagina, blood accumulates, causing hematocolpos and, in some cases, accumulating in the uterus, fallopian tubes, and even the peritoneal cavity. Symptoms develop and worsen with every following menstrual cycle, causing lower abdominal pain, dysuria, and urinary retention. As menstruation occurs normally, lower abdominal pain continues, leading to the patient often being misdiagnosed with dysmenorrhea and treated as such. This doesn't treat the symptoms and can lead to further complications such as endometriosis and subfertility. Correctly diagnosing HWW syndrome is primarily done by means of radiological imaging. A sonographic examination of the pelvic area is often the initial diagnostic measure taken; however, it allows only the uterus didelphys, hematocolpos, and the absent kidney to be recognized. MRI stands as the gold standard for a complete diagnosis as it provides much more detailed information regarding the uterus didelphys, the collapsed and distended hemivagina, and the longitudinal vaginal septum. Altogether, it provides a better picture of the patient's condition, allowing for a better-planned surgical intervention. Treatment of HWW syndrome consists of surgical removal of the vaginal septum enabling the menstrual blood from both uteruses to be drained into the patent vagina, relieving the patient of the symptoms of hematocolpos and preventing its development in the future [13].
Conclusion
Although HWW syndrome is a rare anomaly of the urogenital system, it must not be overlooked when diagnosing adolescent females experiencing dysmenorrhea. Cooperation between gynecologists and radiologists is vital as radiological imaging, either by ultrasound or MRI scan, is the modality of choice for diagnosing HWW. Treatment consists of surgical resection of the vaginal septum and draining of any accumulated blood. An early diagnosis and following surgical treatment are essential to alleviating the symptoms and preventing the complications caused by HWW syndrome.
Patient consent
Written consent was obtained from the patient's legal guardian, for publication of this case and any accompanying images. A copy of the consent can be available upon request of the Editor-in-Chief of this journal.
Authorship contributions
Concept: V.A.I., Design: V.A.I., G.H. Data Collection: V.A.I., G.H.,B.D.E., Analysis: V.A.I., G.H., B.D.E., Literature Search: V.A.I, G.H., B.D.E., Writing: V.A.I, G.H., B.D.E. All the authors have read and approved the final version of the manuscript.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Orazi C, Lucchetti MC, Schingo PM, Marchetti P, Ferro F. Herlyn-Werner-Wunderlich syndrome: uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol. 2007;37(7):657–665. doi: 10.1007/s00247-007-0497-y. [DOI] [PubMed] [Google Scholar]
- 2.Lewis P, Zarariya A, Daver R, Choudhary S, Kale K. An interesting case report on Herlyn-WernerWunderlich syndrome with hematocolpos and communicating blind duplex ureters. Int J Interdisc Multidisc Stud (IJIMS) 2015;2:163–167. https://www.researchgate.net/publication/285220046 [Google Scholar]
- 3.Del Vescovo R, Battisti S, Di Paola V, Piccolo CL, Cazzato RL, Sansoni I, et al. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging. 2012;12:4. doi: 10.1186/1471-2342-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu L, Chen N, Tong JL, Wang W, Zhang L, Lang JH. New classification of Herlyn-Werner-Wunderlich syndrome. Chin Med J (Engl) 2015;128(2):222–225. doi: 10.4103/0366-6999.149208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vercellini P, Daguati R, Somigliana E, Viganò P, Lanzani A, Fedele L. Asymmetric lateral distribution of obstructed hemivagina and renal agenesis in women with uterus didelphys: institutional case series and a systematic literature review. Fertil Steril. 2007;87(4):719–724. doi: 10.1016/j.fertnstert.2007.01.173. [DOI] [PubMed] [Google Scholar]
- 6.Prada Arias M, Muguerza Vellibre R, Montero Sánchez M, Vázquez Castelo JL, Arias González M, Rodríguez Costa A. Uterus didelphys with obstructed hemivagina and multicystic dysplastic kidney. Eur J Pediatr Surg. 2005;15(6):441–445. doi: 10.1055/s-2005-872926. [DOI] [PubMed] [Google Scholar]
- 7.Paz JJ, Gaitán LF, Acosta MA. Síndrome de OHVIRA, a propósito de un caso. Univ Salud. 2020;22(3):288–291. [Google Scholar]
- 8.Rechberger T, Kulik-Rechberger B. Congenital anomalies of the female reproductive tract–diagnosis and management. Ginekol Pol. 2011;82:137–145. [PubMed] [Google Scholar]
- 9.Leanza V, Incognito G, Gulisano M, Incognito D, Correnti S.G, Palumbo M. Herlyn-Werner-Wunderlich syndrome and central placenta previa in a COVID-19 positive pregnant woman: a case report. Italian J Gynaecol Obstet. 2023;35(2):136–141. doi: 10.36129/jog.2022.54. [DOI] [Google Scholar]
- 10.Cunha GR, Robboy SJ, Kurita T, Isaacson D, Shen J, Cao M, et al. Development of the human female reproductive tract. Differentiation. 2018;103:46–65. doi: 10.1016/j.diff.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma R, Mishra P, Seth S, Agarwal N. OHVIRA syndrome—diagnostic dilemmas and review of literature. J South Asian Feder Obst Gynae. 2020;12(6):421–426. [Google Scholar]
- 12.Li L, Chu C, Li S, Lu D, Zheng P, Sheng J, et al. Renal agenesis-related genes are associated with Herlyn-Werner-Wunderlich syndrome. Fertil Steril. 2021;116(5):1360–1369. doi: 10.1016/j.fertnstert.2021.06.033. [DOI] [PubMed] [Google Scholar]
- 13.Khaladkar SM, Kamal V, Kamal A, Kondapavuluri SK. The Herlyn-Werner-Wunderlich syndrome - a case report with radiological review. Pol J Radiol. 2016;81:395–400. doi: 10.12659/PJR.897228. [DOI] [PMC free article] [PubMed] [Google Scholar]