Abstract
Background and Objective
Breast reconstruction in patients with obesity presents numerous challenges, both in terms of surgical technique and post-operative complication management. As breast reconstruction techniques continue to evolve, the armamentarium of reconstructive options for patients with obesity has vastly expanded. Options now include immediate or delayed, implant-based, autologous, or hybrid reconstruction. Determining the optimal breast reconstruction in this complex population requires nuanced and experienced decision-making.
Methods
A literature search was conducted to identify studies assessing breast reconstruction considerations in patients with obesity. The search was performed on PubMed and was limited to English language studies published between 1990 and 2023. Primary studies, case reports, chart reviews, and qualitative studies were included. Additional articles were identified for inclusion based on a review of references, as well as a web-based search, to identify additional studies that were not captured with the primary search strategy.
Key Content and Findings
This narrative review article summarizes the current literature available to guide surgeons in breast reconstruction in patients with obesity.
Conclusions
The advancements in oncologic surgery and breast reconstruction techniques have expanded available surgical options, including immediate or delayed implant-based, autologous, or hybrid breast reconstruction. Each approach has its unique advantages, disadvantages, and surgical considerations. Despite the challenges, patients with obesity can achieve favorable aesthetic outcomes through careful assessment of comorbidities and expectation management.
Keywords: Breast reconstruction, body mass index (BMI), obesity
Introduction
Obesity presents an ongoing health crisis in the United States (1). Standard categories for obesity are based on the World Health Organization (WHO) classification, with an overweight body mass index (BMI) defined as 25–29.9 kg/m2, Class I obesity 30–34.9 kg/m2, Class II obesity 35–39.9 kg/m2, and Class III obesity >40 kg/m2. In the United States, a staggering 42% of women have Class I obesity and 12% have Class II. These numbers are only expected to increase (2). Concurrently, while the current lifetime risk of breast cancer is 13%, breast cancer diagnoses continue to rise, especially at younger ages (3-5). Furthermore, there is an increased risk of breast cancer among patients with a higher BMI (6). Therefore, it is likely that the proportion of obesity among patients seeking breast reconstruction will continue to rise.
Patients with breast cancer seeking breast reconstruction following mastectomy have the opportunity to decide between various reconstructive options, including immediate or delayed reconstruction and implant-based reconstruction versus autologous reconstruction (or a combination of methods). In patients with obesity, breast reconstruction is challenging as they frequently require longer operations, hospital stays and have a higher risk for complications (7). Patients with Class III obesity that undergo any form of breast reconstruction have an increased risk of perioperative complications, major surgical complications, medical complications, respiratory complications, venous thromboembolism, and wound complications compared to non-obese patients (8,9). While significant obesity has historically been considered a contraindication in breast reconstruction, recent recommendations dictate that patients should be carefully counseled regarding an increased risk of complications (10).
This review provides a summary of general approaches, outcomes, reconstructive techniques, and technical pearls for breast reconstruction following mastectomy in patients with obesity. We present this article in accordance with the Narrative Review reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1599/rc).
Methods
A literature search was conducted to identify studies assessing breast reconstruction considerations in patients with obesity (Table 1). The search was performed on PubMed and was limited to English language studies published between 1990 and 2023 (search was done in April 2023). Key words included were: obesity, breast reconstruction, autologous, implant, prosthesis, obese, complications, BMI, DIEP, TRAM, MS-TRAM, mesh, patient satisfaction. Primary studies, case reports, chart reviews, and qualitative studies were included. Additional articles were identified for inclusion based on a review of references, as well as a web-based search, to identify additional studies that were not captured with the primary search strategy.
Table 1. Sources used for this narrative review.
| Items | Specification |
|---|---|
| Date of search | April 1, 2023 |
| Databases and other sources searched | PubMed, Google |
| Search terms used | “Obesity”, “Breast Reconstruction”, “BMI”, “Autologous”, “Implant”, “Prosthesis”, “Obese”, “Complications”, “DIEP”, “TRAM”, “MS-TRAM”, “Mesh”, “Patient Satisfaction” |
| Timeframe | 1990–2023 |
| Inclusion criteria | English language, primary studies, case reports, chart reviews, qualitative studies |
| Selection process | Authors Cevallos P, Berry C |
Managing the skin flap
The optimization of outcomes of breast reconstruction in patients with obesity builds upon the mastectomy techniques employed by surgical oncology. In contrast to radical mastectomies, skin sparing and nipple sparing mastectomies allow for enhanced preservation of mastectomy flap perfusion and viability. When considering the skin envelope, the hypodermis contains adipocytes and the subdermal vascular supply to the overlying mastectomy skin. Careful dissection between the hypodermis and mammary glands, minimization of trauma to the hypodermis, and preservation of intercostal artery perforators at the lateral border of the sternum are integral to maintaining skin flap viability. Additional consideration for skin flap perfusion must be given due to the increased grade of breast ptosis in patients with obesity (11).
Mammary hypertrophy is common in patients with obesity. Surgically, this results in redundancy of the mastectomy skin flap and longer operative times for both the mastectomy and reconstruction. As they have a significant degree of ptosis, they should be counseled about the higher risk of nipple and mastectomy flap necrosis (11). Redundancy of the mastectomy flap can be managed with a skin reducing mastectomy (12), most commonly utilizing an inverted T incision (Wise Pattern) that allows for reduction of skin in both horizontal and vertical vectors and minimization of the amount of dysvascular tissue retained (13). These incision patterns require a close discussion and coordination with the oncologic breast surgeon.
While the obese population may have more abundant skin, its quality can be compromised in the presence of radiation. Radiation-induced skin fibrosis has deleterious effects on skin elasticity and wound healing ability, leading to increased complication rates for all patients with a history of radiation in the reconstructive surgical field. Although not unique to the obese population, a delayed reconstruction with autologous tissue is recommended to reduce complication rates and increase patient satisfaction. The reason for this is that critical structures or foreign body exposure resulting from suboptimal wound healing are more concerning than wound dehiscence along a well-vascularized flap or abdominal flap site suture line (11).
Pocket control is critical for reducing the risk of seroma and improving the aesthetic outcome of the reconstruction. Further pocket control may be required to adequately address the tendency of both the lateral subcutaneous tissue to settle towards the posterior axillary line and the cephalad subcutaneous tissue to retract further along the vertical axis after mastectomy.
Goldilocks mastectomy technique
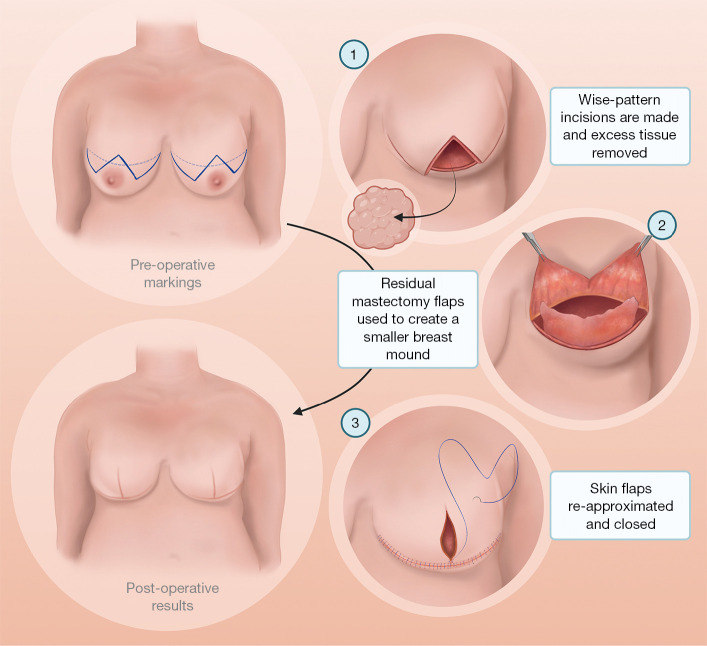
The Goldilocks mastectomy technique, originally described by Richardson in 2012, was developed with the goal of creating a technique which would allow a safe breast reconstruction alternative for patients with significant comorbidities, particularly elevated BMI (14). This technique utilizes redundant mastectomy flap tissue to reconstruct a breast mound (Figure 1). Specifically, de-epithelized redundant inferior dermal flaps are used for lower pole coverage, soft tissue support and auto-augmentation, while the superior medial and lateral flaps portion of the inferior dermal flap is folded over to create a reconstructed breast mound. It takes advantage of a vascularized inferior dermal flap and addresses both redundant mastectomy skin while also diminishing the resulting extensive dead space in the prepectoral space following mastectomy (12). These inferior dermal flaps and the mastectomy skin flaps provide a substrate for future serial fat grafting to further augment the reconstruction to create the breast mound. The Goldilocks technique offers shorter operating time, shorter recovery, greater cost-effectiveness, and requires no additional donor site (15). In this manner, this technique minimizes the complications of both implant- based and abdominally based autologous reconstruction, however may still be used in the setting of implant or autologous reconstruction. When used alone, there is no risk of implant infection, capsular contraction, implant rupture, and decreased risk of fat necrosis, superficial skin loss, and abdominal bulge or hernia (15). This technique has been shown to be a favorable option for patients with obesity, especially for patients who desire a smaller breast and do not want to undergo a full reconstruction (15,16). Further, it is often necessary in the setting of revision after adjuvant radiation (15).
Figure 1.
Visual depiction of the Goldilocks mastectomy technique utilizing redundant mastectomy flap tissue to reconstruct a breast mound.
It should be noted that the technique has several inherent disadvantages. The wise pattern or goldilocks technique has a higher rate of wound complications compared to a simple horizontal incision, given the T point inset. Additionally, the size of the breast mound is limited by the pre-mastectomy breast size and thickness of the mastectomy skin flaps. This technique may result in a lack of final projection of the reconstructed breast tissue and offers less control of shape and volume (17). Revision may be required which could include secondary implant placement, fat grafting, or addition of an autologous tissue flap (18). A meta-analysis of obese patients who had undergone reconstruction with the Goldilocks technique found that approximately one third of patients ultimately undergo secondary surgery, most frequently for implant placement or latissimus flap reconstruction (15).
A summary of general techniques in managing the skin envelope, flap redundancy, and pocket control for breast reconstruction in patients with obesity can be found in Table 2.
Table 2. General techniques in managing the skin envelope, flap redundancy, and pocket control for breast reconstruction in patients with obesity.
| Category | Pearl/technique | Advantages | Limitations |
|---|---|---|---|
| Skin envelope | Work with general surgeons to minimize aggressive mastectomies | Preservation of mastectomy flap perfusion and viability (most commonly skin sparing or nipple sparing mastectomy) | May not be possible if radical mastectomy is indicated |
| Dissection at junction of hypodermis and mammary glands to preserve hypodermis | Contains blood supply to mastectomy skin, crucial for flap viability | Contributes to thicker mastectomy flap | |
| • Perioperative flap perfusion assessment •(indocyanine green angiography) | |||
| • Low threshold for skin debridement due to compromised perfusion | |||
| Flap redundancy | Skin reducing mastectomy —commonly Wise Pattern closure |
Indications for Wise Pattern closure: Grade 3 ptosis, breasts with extensive stretch marks, require implant >800 cc, desires smaller breasts | Can result in inadequate volume of tissue to support prosthesis |
| Preservation of and utilization of de-epithelized inferior dermal mastectomy skin flap to auto-augment the breast (Goldilocks technique) |
• Incisional approach can vary (most commonly inverted T or anchor) | • May require augmentation with fat grafting or revision | |
| • Can be used in nipple reconstruction | • Decreased projection of breast, offers less control of shape and volume | ||
| • With or without immediate reconstruction (DTI or 2-stage) with or without ADM | |||
| • Can be used for salvage after implant-based reconstruction | |||
| • Alternative for patients who are poor candidates for traditional reconstruction or prefer 1-stage reconstruction | |||
| Pocket control | Reposition displaced subcutaneous tissue (lateral tissue towards anterior axillary line, cephalad tissue more caudally) | Eliminate dead space, decrease risk of seroma, improved aesthetics | – |
DTI, direct-to-implant; ADM, acellular dermal matrix.
Complications
Obesity is a well-established risk factor for minor and major surgical complications, a finding that is reflected in studies of surgical outcomes of both implant and autologous breast reconstruction in the setting of obesity (7,19-23). Obesity is also highly associated with conditions known to increase surgical complications, such as higher American Society of Anesthesiologists (ASA) physical status score, longer operative time, and increased length of hospital stay (9).
The risk of infection is perhaps the most well-established complication associated with obesity following breast reconstruction. Patients with obesity have an increased rate of both superficial and deep wound infections (7,9,20), as well as increased rates of infection outside of the incision site, including organ space infection, pneumonia, and sepsis (9). Several studies have named delayed wound healing and dehiscence as the complication most increased by obesity in the setting of breast reconstruction (7,9,20). The risk of seroma following breast reconstruction is also substantially increased by obesity, potentially due to the effect of shearing stress associated with increased use of upper body muscles by obese individuals to lift oneself up, and increased dead space following mastectomy (7,20,23). There are conflicting reports on the rates of hematoma after breast reconstruction in patients with obesity. One study suggests there may be a procoagulative effect that is protective against hematoma development (24), while other studies find increased (20) or no differences (7) in rates of hematomas. While current literature generally shares the consensus that obesity is an increased risk factor for the development of fat necrosis following breast reconstruction, the degree to which this occurs is debated (7,20,23). Obesity has further been associated with higher rates of reoperation after breast reconstruction (7,9,20). Obesity is associated with a high rate of comorbidities, which can increase the risk of perioperative complications and need for reoperation. Additionally, obesity can affect the aesthetic outcome of breast reconstruction, as achieving symmetry and aesthetic results is more difficult given larger tissue requirements.
A large 2016 retrospective study by Huo et al. found that obese breast reconstruction patients ultimately incur a higher complication cost, averaging $4,684 for non-obese patients, $6,250 for patients with Class I obesity, and $7,868 for patients with Class II and III obesity (P<0.001) (25). The discrepancy between these costs was found to be fueled higher infection rates as well as higher wound and perfusion complications (25).
Although the evidence clearly indicates increased risk of complications in the setting of obesity, there is support for existence of the “obesity paradox” in breast reconstruction: obesity is associated with improved survival following surgical breast reconstruction (19). Most frequently discussed in the context of joint arthroplasty, this concept describes the paradoxical relationship observed among patients with obesity experiencing higher complication rates yet lower mortality compared to patients without obesity undergoing the same operation (26). The leading hypothesis for this phenomenon is that a frailty phenotype is predictive of mortality, with body mass and weight acts as a protective measure for patients at risk of mortality. Additionally, some have theorized that the obese populations studied may have higher cardiorespiratory fitness than their non-obese counterparts, accounting for the paradoxical findings (26).
Patient reported outcomes
Studies indicate that patient reported outcome measures are improved across all BREAST-Q measures in the obese population following breast reconstruction, except for physical well-being of the abdomen in the case of abdominally based autologous reconstruction, a finding which only becomes evident 2 years postoperatively in patients with obesity (27). A retrospective study of 460 patients who had undergone breast reconstruction found that overall patient satisfaction was not significantly different between patients with and without obesity who underwent implant-based breast reconstruction. However, for patients who underwent breast reconstruction with a free or pedicled TRAM flap, overall satisfaction rates were lower (70%) for obese individuals compared to patients of normal weight (76%) (28).
Srinivasa et al. published a 2020 study of BREAST-Q results from 1444 patients,examining the differences in patient responses between patients with and without obesity who underwent implant-based reconstruction (29). They found that overall satisfaction decreased as BMI increased, from 65.7% in patients who were underweight or normal weight to 58.6% in patients with obesity (29). However, this study also reported that patients with Class II and III obesity experienced a greater increase in psychological and sexual well-being 2 years postoperatively compared to patients with normal or underweight BMIs (29). Atisha et al. showed that patients with obesity who pursued an implant-based reconstruction are significantly less satisfied with the ultimate aesthetic outcome compared to those who underwent an autologous reconstruction (28). This may be due to the limitation of implant volumes when attempting to match the mastectomy volume, leading to greater long-term satisfaction with autologous reconstruction compared to implants (30). Another study considering BREAST-Q results from 404 patients found that patient-reported physical well-being of the abdomen was lower in patients with obesity compared to non-obese patients 3 years following autologous breast reconstruction with abdominal free-tissue transfer (P<0.05) (27). Authors hypothesized that this finding could be accounted for by differences in flap types between the two groups, as patients with obesity were less likely to receive perforator flaps and therefore were more likely to sacrifice muscle at the donor site (27).
Autologous breast reconstruction
Autologous breast reconstruction uses a patient’s own tissue, typically from the abdomen, buttocks or back, to recreate a new breast. This is generally accomplished using a pedicled or free flap but may also take advantage of de-epithelized inferior dermal mastectomy skin. Common flaps utilized in autologous breast reconstruction in patients with obesity include muscle-sparing transverse rectus abdominis musculocutaneous (MS-TRAM) and the deep inferior epigastric perforator (DIEP) free flaps.
Advantages to autologous flap reconstruction
Several studies demonstrate that autologous reconstruction in the obese population is less likely to result in mastectomy skin flap necrosis, seroma, hematoma, and infection when compared to implant-based reconstruction (11,31,32). Another study found that while autologous reconstruction in patients with Class II and III obesity was associated complication rates triple those of normal weight, implant-based reconstruction was still more likely to result in reconstructive failure (29). There is no clear prohibitive BMI to performing autologous flap reconstruction given the heterogeneity in the literature, which ranges from a cut-off threshold of BMI >35 to 39.9 kg/m2 (33).
Overall, evidence suggests that women who undergo autologous breast reconstruction are more likely to achieve reconstruction completion compared to those who undergo implant-based reconstruction (11). One study of 352 reconstructions in patients with obesity found that >98% of autologous reconstructions had successfully resulted in a breast mound 2 years postoperatively, while only 76.8% of implant-based reconstructions had this outcome (P<0.001) (11). Interestingly, another study found that women who underwent autologous breast reconstruction were more likely to complete nipple areolar reconstruction than those who underwent implant-based reconstruction (11).
In terms of patient-reported outcomes, a study by Klement et al. conducted a retrospective review of BREAST-Q data which demonstrated improved satisfaction following autologous reconstruction compared to implant reconstruction (31). Higher satisfaction with breasts (P<0.0001), satisfaction with outcome (P<0.01), psychosocial well-being (P<0.007), and sexual well-being (P<0.006) was reported for patients undergoing autologous reconstruction versus implant-based reconstruction (31). Another study by Liu et al. recapitulated these results at later timepoints, indicating that even at 10 years of follow-up, patients who underwent abdominal-based autologous reconstruction reported elevated satisfaction scores in chest physical well-being and abdominal physical well-being (34).
Complication rates and outcomes aside, autologous flap reconstruction has several advantages over implant-based reconstruction. First, the use of autologous tissue results in a reconstruction that closely matches the shape, firmness, mobility, and warmth of the natural female breast anatomical structure. Autologous flap reconstruction in the obese population also comes with the advantage of abundant tissue availability, which allows for accommodation of the increased reconstructive volume required in patients with larger body habitus (31). The reconstruction may also be augmented with fat grafting to optimize the final result and improve the volume.
Disadvantages to autologous reconstruction
Autologous flap reconstruction comes with the disadvantages of increased operative time, additional donor site wounds and dissections, and complications such as fat necrosis and flap failure (31). When autologous breast reconstruction is performed in the obese population, delayed healing and donor-site infection are the most common donor-site complications reported (31,32). Panayi et al.’s meta-analysis found that obesity was associated with a relative risk of 1.6 for partial flap failure and 1.97 for total flap failure in breast reconstruction (P<0.05) (7). Another meta-analysis found that 1.3% of non-obese patients experienced partial flap failure and 1.0% experienced total flap failure, compared to 3.9% (P<0.002) and 2.2% (P<0.05), respectively, for patients with obesity (23). A study of 179 flap reconstructions found that increasing weight of the flap significantly correlated with increased occurrence of fat necrosis. In single perforator flaps weighing more than 1,000 grams, more than 42.9% of flaps developed fat necrosis. This number decreased to 14.3% in flaps of the same weight with multiple perforators (35). In the obese population, increased flap weight may require careful surgical planning to include multiple perforators supplying the flap so as to minimize risk of fat necrosis.
Muscle sparing TRAM & DIEP flaps
Patients with obesity undergoing microsurgical breast reconstruction using abdominal tissue have a higher rate of abdominal donor site complications, but the class of obesity does not increase this risk (36). Additionally, the detrimental effects of chemotherapy may further hinder wound healing in this population (37). Increased flap weight resected has not been associated with increased flap complications, however, it is associated with increased rate of donor site would healing issues (38).
Compared to DIEP flap reconstruction, free MS-TRAM reconstruction provides an increased number of perforators which may serve a function in optimizing flap perfusion, minimizing fat necrosis, and improving venous drainage. This technique also offers the ability to more easily capture multiple perforators down to their pedicle on the external iliac artery, compared to the more laborious intramuscular dissection with DIEP flap reconstruction. Mindful positioning of the patient avoids over-harvesting of abdominal tissue in the vertical dimension, allowing for a more tension-free closure (36).
Varying degrees of remaining fascia, scarring, and innervation to the rectus abdominis impact donor site morbidity and functionality. Abdominal based reconstruction particularly predisposes patients with obesity to abdominal hernia/bulge or seroma (37). The literature remains unclear whether the use of mesh in patients with obesity increases (39) or decreases the risk of abdominal hernia in either DIEP or MS-TRAM flaps, with many conflicting reports (37,40-47). Additionally, the trade-off of decreased donor site morbidity in DIEP flaps comes at the expense of increased rates of partial flap necrosis and fat necrosis (48,49).
A summary of general considerations with autologous breast reconstruction in patients with obesity can be found in Table 3.
Table 3. General considerations with autologous breast reconstruction in patients with obesity.
| Category | Pearl/technique | Advantage | Limitation |
|---|---|---|---|
| Flap perfusion | Use of indocyanine green angiography to selectively trim the flap of areas of diminished perfusion to decrease chance of fat necrosis | Lowers rate of fat necrosis | Not readily available at some hospitals |
| Donor-site | Low threshold for liberal use of mesh, especially in setting of increased harvested fascia | – | – |
Implant-based breast reconstruction
General considerations in implant-based reconstruction
Prior recommendations for implant-based breast reconstruction in the obese included pursuing delayed first-stage reconstruction with fat grafting aimed at elevation of central mastectomy scarring (50). Subpectoral prosthetic placement was traditionally favored, with prepectoral placement considered in select patients with no history of radiation therapy and no other associated comorbidities. However, continued surgical experience has loosened contraindications for prepectoral placement in patients with obesity (51). Unlike in subpectoral reconstruction, prepectoral placement necessitates use of acellular dermal matrix (ADM). The reliance of ADM in prepectoral reconstruction, while largely advantageous (52-54), raises concerns for ADM non-integration when used in larger quantities, as well as increased risk of complications such as seroma (30,51,55). Prepectoral breast reconstruction has been shown to have the same rate of skin necrosis (3.5%), wound dehiscence (5.9%), seroma rate (4.7%), and failure rate (1.2%) in patients with obesity compared to nonobese patients (56). Nguyen et al. determined that every one-point increase of BMI raised the odds of complications and explantation following implant-based breast reconstruction by 3.4% for prepectoral implants and by 8.6% for subpectoral implants (22). While patients with Class II or Class III obesity may experience increased implant failure after prepectoral reconstruction, it has also been shown that the presence of associated comorbidities (e.g., diabetes mellitus, smoking) is more predictive of the risk of complication than BMI alone (57). This calls into question the utility of BMI alone as a continuous predictor of implant-based breast reconstruction complications (57,58).
Restoration of breast volume in prosthetic reconstruction largely depends on the available catalog of implant volumes offered by industry. Currently, the largest available implant volume on the market is 800 mL with a maximum recommended fill volume of 960 mL. Given that the average weight of mastectomy for patients with obesity is greater than 1,000 g (59), surgeons may be limited in their ability to adequately restore breast volume with implants alone. The ATHENA trial is currently evaluating the safety and effectiveness of the Mentor Large Size MemoryGel Ultra High-Profile breast implant with a fill volume up to 1,445 mL (60).
In patients who desire a greater breast volume than achievable by implant-based reconstruction alone, a hybrid approach using both an adjustable implant and autologous tissue may be pursued (61). This approach may be considered in patients who have a prior history of radiotherapy, which is a relative contraindication to implant-based reconstruction. The use of a flap, traditionally a latissimus dorsi myocutaneous flap, in conjunction with an implant, may further obviate the need for additional revision procedures. However, combination of the latissimus dorsi flap with an implant may have an increased likelihood of short- and long-term risk of infection and necessity for future exchange (31,62,63). Although there have been conflicting reports (64).
Advantages to implant-based reconstruction
Despite the higher risk of complication with prosthetic breast reconstruction compared to autologous reconstruction (8,11,29,32), implant-based reconstruction remains the most commonly technique utilized. Prosthetic reconstruction may be pursued immediately at the time of mastectomy or in a delayed fashion depending on the patient's clinical characteristics. The procedure is of shorter duration compared to autologous reconstruction, without the additional risk of donor site morbidity.
Disadvantages to implant-based reconstruction
Implant-based breast reconstruction has a higher complication rate compared to autologous reconstruction among patients with obesity (8,11,29,32). Implant-based breast reconstruction results in a higher rate of skin necrosis, postoperative seroma, hematoma, infection, expander extrusion, and failure, and often requires multiple operations (31). In a report of 700 patients with obesity, Garvey et al. showed a breast reconstruction failure in patients of 15.8% for those with an implant-based reconstruction compared to a 1.5% failure rate for those undergoing an autologous reconstruction (32). Optimal cutoff values for prosthetic reconstruction have been suggested, ranging from a BMI of 30 kg/m2 (58) to 34 kg/m2 (32). However, given conflicting reports of the utility of BMI as a continuous predictor of postoperative complications (57), attention to the comprehensive health of an individual patient and presence of comorbidities should guide the ultimate reconstruction pursued (32,58).
Timing of implant-based reconstruction
Immediate reconstruction may allow for better control of the mastectomy skin envelope and scar location compared to delayed reconstruction (56). However, delayed implant-based reconstruction may be preferred for patients with obesity and/or additional comorbidities, such as post-mastectomy radiation. In patients who have undergone a Goldilocks reconstruction, a revision or augmentation of the breast mound may be indicated, most commonly with an implant (59%) (15). Even in patients with a BMI between 37–50 kg/m2, Goldilocks mastectomy technique with delayed implant reconstruction allowed for improvements in aesthetic outcome with no implant related complications over a 9-month follow-up period (65).
Outcomes in implant-based reconstruction
Concern for infection after implant-based reconstruction warrants aggressive action to salvage the implant and avoid explantation. This usually involves a hospital admission with a combination of intravenous antibiotic treatment, possible operative washout, excision of areas of concern, implant exchange, or removal. The result of an implant infection is costly, taxing, and devastating for patients (11).
A summary of general considerations with implant-based breast reconstruction in patients with obesity can be found in Table 4.
Table 4. General considerations with implant-based breast reconstruction in patients with obesity.
| Category | Pearl/technique | Advantage | Limitation |
|---|---|---|---|
| ADM | – | • Allows for single stage reconstruction | • Costly |
| • Improved aesthetic outcome | • Increased risk of complications with larger amounts of ADM | ||
| • Decreased risk of capsular contracture | |||
| Autoderm | Uses patient’s own de-epithelialized mastectomy flap for lower pole coverage of an implant (65) | • Vascularized dermis provides robust barrier for implant | Limitations with nipple-sparing mastectomy |
| • With or without ADM for upper pole coverage if in prepectoral plane | |||
| • Similar complication rate to ADM | |||
| • More affordable compared to ADM | |||
| Plane | Prepectoral vs. subpectoral placement | • Similar outcomes to subpectoral | Higher risk of complications compared to subpectoral |
| • No protective benefit of a subpectoral placement | |||
| • Muscle-sparing technique diminishes pain, risk of animation deformity, risk of long-term concavity of rib cage | |||
| Tissue expansion/implant | • Intraoperative expansion with air & underinflation of tissue expander for vulnerable flaps | • Reduces pressure on the overlying mastectomy flap | Full volume restoration restricted to manufacturer catalog of available implants |
| • Overinflation of implant to achieve final volume | • Implants may be overinflated beyond fill volume up to the maximum recommended volume |
ADM, acellular dermal matrix.
Conclusions
This article summarizes the general approaches and outcomes of breast reconstruction following mastectomy in patients with obesity. Steady advancements in oncologic surgery and breast reconstruction techniques has expanded reconstructive options for patients with obesity. Multiple options for breast reconstruction in this challenging patient population have been described in the literature, each with unique advantages, disadvantages, and surgical pearls. These include immediate or delayed implant-based, autologous, or hybrid breast reconstruction. Given the evolving landscape of breast reconstruction, patients with obesity can achieve a great aesthetic outcome. Choosing which type of reconstruction is optimal for patients ultimately requires a careful assessment of comorbidities and expectation management.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Translational Medicine for the series “Breast Reconstruction”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1599/rc
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1599/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1599/coif). The series “Breast Reconstruction” was commissioned by the editorial office without any funding or sponsorship. O.J.M. served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Translational Medicine from July 2022 to June 2024. The authors have no other conflicts of interest to declare.
References
- 1.Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA 2016;315:2284-91. 10.1001/jama.2016.6458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Y, Beydoun MA, Min J, et al. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol 2020;49:810-23. 10.1093/ije/dyz273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Cancer Society. Breast Cancer Facts & Figures 2022-2024. Atlanta: American Cancer Society, Inc.; 2022. [Google Scholar]
- 4.Manrique OJ, Banuelos J, Abu-Ghname A, et al. Surgical Outcomes of Prepectoral Versus Subpectoral Implant-based Breast Reconstruction in Young Women. Plast Reconstr Surg Glob Open 2019;7:e2119. 10.1097/GOX.0000000000002119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manrique OJ, Charafeddine A, Abu-Ghname A, et al. Two-Staged Implant-Based Breast Reconstruction: A Long-Term Outcome Study in a Young Population. Medicina (Kaunas) 2019;55:481. 10.3390/medicina55080481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Picon-Ruiz M, Morata-Tarifa C, Valle-Goffin JJ, et al. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA Cancer J Clin 2017;67:378-97. 10.3322/caac.21405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panayi AC, Agha RA, Sieber BA, et al. Impact of Obesity on Outcomes in Breast Reconstruction: A Systematic Review and Meta-Analysis. J Reconstr Microsurg 2018;34:363-75. 10.1055/s-0038-1627449 [DOI] [PubMed] [Google Scholar]
- 8.Fischer JP, Cleveland EC, Nelson JA, et al. Breast reconstruction in the morbidly obese patient: assessment of 30-day complications using the 2005 to 2010 National Surgical Quality Improvement Program data sets. Plast Reconstr Surg 2013;132:750-61. 10.1097/PRS.0b013e31829fe33c [DOI] [PubMed] [Google Scholar]
- 9.Fischer JP, Nelson JA, Kovach SJ, et al. Impact of obesity on outcomes in breast reconstruction: analysis of 15,937 patients from the ACS-NSQIP datasets. J Am Coll Surg 2013;217:656-64. 10.1016/j.jamcollsurg.2013.03.031 [DOI] [PubMed] [Google Scholar]
- 10.Chang EI. Latest Advancements in Autologous Breast Reconstruction. Plast Reconstr Surg 2021;147:111e-22e. 10.1097/PRS.0000000000007480 [DOI] [PubMed] [Google Scholar]
- 11.Velazquez C, Siska RC, Pestana IA. Breast Reconstruction Completion in the Obese: Does Reconstruction Technique Make a Difference in Its Achievement? J Reconstr Microsurg 2021;37:720-7. 10.1055/s-0041-1726031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Becker H, Vazquez OA, Komberg J. Goldilocks Procedure without a Vertical Incision and a Comprehensive Literature Review. Plast Reconstr Surg Glob Open 2021;9:e3786. 10.1097/GOX.0000000000003786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathew J. Direct to implant reconstruction with adjustable permanent Becker implant expanders with ADM following de-epithelised skin reducing mastectomy in high-risk overweight and obese patients with severe ptosis. Surgeon 2023;21:54-9. 10.1016/j.surge.2022.02.002 [DOI] [PubMed] [Google Scholar]
- 14.Richardson H, Ma G. The Goldilocks mastectomy. Int J Surg 2012;10:522-6. 10.1016/j.ijsu.2012.08.003 [DOI] [PubMed] [Google Scholar]
- 15.Ghanouni A, Thompson P, Losken A. "Outcomes of the Goldilocks technique in High-risk Breast Reconstruction Patients.". Plast Reconstr Surg 2023;152:35S-40S. 10.1097/PRS.0000000000010354 [DOI] [PubMed] [Google Scholar]
- 16.Chaudhry A, Oliver JD, Vyas KS, et al. Outcomes analysis of Goldilocks mastectomy and breast reconstruction: A single institution experience of 96 cases. J Surg Oncol 2019;119:1047-52. 10.1002/jso.25465 [DOI] [PubMed] [Google Scholar]
- 17.Bustos SS, Nguyen MD, Harless CA, et al. The Goldilocks Procedure with and without Implant-Based Immediate Breast Reconstruction in Obese Patients: The Mayo Clinic Experience. Plast Reconstr Surg 2021;148:703-16. 10.1097/PRS.0000000000008362 [DOI] [PubMed] [Google Scholar]
- 18.Manrique OJ, Kuruoglu D, Yan M, et al. Immediate Breast Reconstruction Using the Goldilocks Procedure: A Balance between More Surgery and Patient Satisfaction. Plast Reconstr Surg 2022;149:801-9. 10.1097/PRS.0000000000008895 [DOI] [PubMed] [Google Scholar]
- 19.Tjeertes EK, Hoeks SE, Beks SB, et al. Obesity--a risk factor for postoperative complications in general surgery? BMC Anesthesiol 2015;15:112. 10.1186/s12871-015-0096-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen CL, Shore AD, Johns R, et al. The impact of obesity on breast surgery complications. Plast Reconstr Surg 2011;128:395e-402e. 10.1097/PRS.0b013e3182284c05 [DOI] [PubMed] [Google Scholar]
- 21.Ogilvie WA, Shakir Z, Whinery LD, et al. Effect of obesity on outcomes after breast reconstruction surgery, an analysis of national surgical quality improvement program. J Plast Reconstr Aesthet Surg 2022;75:4496-512. 10.1016/j.bjps.2022.10.009 [DOI] [PubMed] [Google Scholar]
- 22.Nguyen KT, Hanwright PJ, Smetona JT, et al. Body mass index as a continuous predictor of outcomes after expander-implant breast reconstruction. Ann Plast Surg 2014;73:19-24. 10.1097/SAP.0b013e318276d91d [DOI] [PubMed] [Google Scholar]
- 23.Schaverien MV, Mcculley SJ. Effect of obesity on outcomes of free autologous breast reconstruction: a meta-analysis. Microsurgery 2014;34:484-97. 10.1002/micr.22244 [DOI] [PubMed] [Google Scholar]
- 24.Lee KT, Lee H, Jeon BJ, et al. Impact of overweight/obesity on the development of hematoma following tissue expander-based breast reconstruction. J Plast Reconstr Aesthet Surg 2020. [Epub ahead of print]. doi: . 10.1016/j.bjps.2020.08.105 [DOI] [PubMed] [Google Scholar]
- 25.Huo J, Smith BD, Giordano SH, et al. Post-mastectomy breast reconstruction and its subsequent complications: a comparison between obese and non-obese women with breast cancer. Breast Cancer Res Treat 2016;157:373-83. 10.1007/s10549-016-3832-x [DOI] [PubMed] [Google Scholar]
- 26.Kunutsor SK, Whitehouse MR, Blom AW. Obesity paradox in joint replacement for osteoarthritis - truth or paradox? Geroscience 2022;44:651-9. 10.1007/s11357-021-00442-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nelson JA, Sobti N, Patel A, et al. The Impact of Obesity on Patient-Reported Outcomes Following Autologous Breast Reconstruction. Ann Surg Oncol 2020;27:1877-88. 10.1245/s10434-019-08073-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Atisha DM, Alderman AK, Kuhn LE, et al. The impact of obesity on patient satisfaction with breast reconstruction. Plast Reconstr Surg 2008;121:1893-9. 10.1097/PRS.0b013e3181715198 [DOI] [PubMed] [Google Scholar]
- 29.Srinivasa DR, Clemens MW, Qi J, et al. Obesity and Breast Reconstruction: Complications and Patient-Reported Outcomes in a Multicenter, Prospective Study. Plast Reconstr Surg 2020;145:481e-90e. 10.1097/PRS.0000000000006543 [DOI] [PubMed] [Google Scholar]
- 30.Roubaud MS, Carey JN, Vartanian E, et al. Breast reconstruction in the high-risk population: current review of the literature and practice guidelines. Gland Surg 2021;10:479-86. 10.21037/gs-2020-nfbr-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klement KA, Hijjawi JB, LoGiudice JA, et al. Microsurgical Breast Reconstruction in the Obese: A Better Option Than Tissue Expander/Implant Reconstruction? Plast Reconstr Surg 2019;144:539-46. 10.1097/PRS.0000000000005897 [DOI] [PubMed] [Google Scholar]
- 32.Garvey PB, Villa MT, Rozanski AT, et al. The advantages of free abdominal-based flaps over implants for breast reconstruction in obese patients. Plast Reconstr Surg 2012;130:991-1000. 10.1097/PRS.0b013e318267efc5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taghioff SM, Slavin BR, Mehra S, et al. Risk stratification of surgical-site outcomes by BMI and flap type in autologous breast reconstruction. J Plast Reconstr Aesthet Surg 2023;80:115-25. 10.1016/j.bjps.2023.01.042 [DOI] [PubMed] [Google Scholar]
- 34.Liu T, Freijs C, Klein HJ, et al. Patients with abdominal-based free flap breast reconstruction a decade after surgery: A comprehensive long-term follow-up study. J Plast Reconstr Aesthet Surg 2018;71:1301-9. 10.1016/j.bjps.2018.06.009 [DOI] [PubMed] [Google Scholar]
- 35.Mulvey CL, Cooney CM, Daily FF, et al. Increased Flap Weight and Decreased Perforator Number Predict Fat Necrosis in DIEP Breast Reconstruction. Plast Reconstr Surg Glob Open 2013;1:1-7. 10.1097/GOX.0b013e318294e41d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spitz JA, Bradford PS, Aguilar F, et al. How Big is Too Big: Pushing the Obesity Limits in Microsurgical Breast Reconstruction. Ann Plast Surg 2018;80:137-40. 10.1097/SAP.0000000000001284 [DOI] [PubMed] [Google Scholar]
- 37.Zhong T, Novak CB, Bagher S, et al. Using propensity score analysis to compare major complications between DIEP and free muscle-sparing TRAM flap breast reconstructions. Plast Reconstr Surg 2014;133:774-82. 10.1097/PRS.0000000000000024 [DOI] [PubMed] [Google Scholar]
- 38.Lam G, Weichman KE, Reavey PL, et al. Analysis of Flap Weight and Postoperative Complications Based on Flap Weight in Patients Undergoing Microsurgical Breast Reconstruction. J Reconstr Microsurg 2017;33:186-93. 10.1055/s-0036-1594298 [DOI] [PubMed] [Google Scholar]
- 39.Fischer JP, Nelson JA, Sieber B, et al. Free tissue transfer in the obese patient: an outcome and cost analysis in 1258 consecutive abdominally based reconstructions. Plast Reconstr Surg 2013;131:681e-92e. 10.1097/PRS.0b013e31828e2159 [DOI] [PubMed] [Google Scholar]
- 40.Ochoa O, Chrysopoulo M, Nastala C, et al. Abdominal wall stability and flap complications after deep inferior epigastric perforator flap breast reconstruction: does body mass index make a difference? Analysis of 418 patients and 639 flaps. Plast Reconstr Surg 2012;130:21e-33e. 10.1097/PRS.0b013e3182547d09 [DOI] [PubMed] [Google Scholar]
- 41.Hofer SO, Damen TH, Mureau MA, et al. A critical review of perioperative complications in 175 free deep inferior epigastric perforator flap breast reconstructions. Ann Plast Surg 2007;59:137-42. 10.1097/01.sap.0000253326.85829.45 [DOI] [PubMed] [Google Scholar]
- 42.Garvey PB, Buchel EW, Pockaj BA, et al. The deep inferior epigastric perforator flap for breast reconstruction in overweight and obese patients. Plast Reconstr Surg 2005;115:447-57. 10.1097/01.prs.0000149588.09148.53 [DOI] [PubMed] [Google Scholar]
- 43.Bajaj AK, Chevray PM, Chang DW. Comparison of donor-site complications and functional outcomes in free muscle-sparing TRAM flap and free DIEP flap breast reconstruction. Plast Reconstr Surg 2006;117:737-46; discussion 747-50. 10.1097/01.prs.0000200062.97265.fb [DOI] [PubMed] [Google Scholar]
- 44.Chen CM, Halvorson EG, Disa JJ, et al. Immediate postoperative complications in DIEP versus free/muscle-sparing TRAM flaps. Plast Reconstr Surg 2007;120:1477-82. 10.1097/01.prs.0000288014.76151.f7 [DOI] [PubMed] [Google Scholar]
- 45.Nahabedian MY, Tsangaris T, Momen B. Breast reconstruction with the DIEP flap or the muscle-sparing (MS-2) free TRAM flap: is there a difference? Plast Reconstr Surg 2005;115:436-44; discussion 445-6. 10.1097/01.prs.0000149404.57087.8e [DOI] [PubMed] [Google Scholar]
- 46.Garvey PB, Salavati S, Feng L, et al. Perfusion-related complications are similar for DIEP and muscle-sparing free TRAM flaps harvested on medial or lateral deep inferior epigastric Artery branch perforators for breast reconstruction. Plast Reconstr Surg 2011;128:581e-9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nelson JA, Guo Y, Sonnad SS, et al. A Comparison between DIEP and muscle-sparing free TRAM flaps in breast reconstruction: a single surgeon's recent experience. Plast Reconstr Surg 2010;126:1428-35. 10.1097/PRS.0b013e3181ef8b20 [DOI] [PubMed] [Google Scholar]
- 48.Nahabedian MY, Momen B, Galdino G, et al. Breast Reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg 2002;110:466-75; discussion 476-7. 10.1097/00006534-200208000-00015 [DOI] [PubMed] [Google Scholar]
- 49.Kroll SS. Fat necrosis in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg 2000;106:576-83. 10.1097/00006534-200009030-00008 [DOI] [PubMed] [Google Scholar]
- 50.Sigalove S, Maxwell GP, Sigalove NM, et al. Prepectoral Implant-Based Breast Reconstruction: Rationale, Indications, and Preliminary Results. Plast Reconstr Surg 2017;139:287-94. 10.1097/PRS.0000000000002950 [DOI] [PubMed] [Google Scholar]
- 51.Sbitany H. Discussion: Should Obesity Be Considered a Contraindication for Prepectoral Breast Reconstruction? Plast Reconstr Surg 2020;145:628-9. 10.1097/PRS.0000000000006541 [DOI] [PubMed] [Google Scholar]
- 52.Leong M, Basu CB, Hicks MJ. Further evidence that human acellular dermal matrix decreases inflammatory markers of capsule formation in implant-based breast reconstruction. Aesthet Surg J 2015;35:40-7. 10.1093/asj/sju014 [DOI] [PubMed] [Google Scholar]
- 53.Forsberg CG, Kelly DA, Wood BC, et al. Aesthetic outcomes of acellular dermal matrix in tissue expander/implant-based breast reconstruction. Ann Plast Surg 2014;72:S116-20. 10.1097/SAP.0000000000000098 [DOI] [PubMed] [Google Scholar]
- 54.Ibrahim AM, Koolen PG, Ganor O, et al. Does acellular dermal matrix really improve aesthetic outcome in tissue expander/implant-based breast reconstruction? Aesthetic Plast Surg 2015;39:359-68. 10.1007/s00266-015-0484-x [DOI] [PubMed] [Google Scholar]
- 55.Krishnan NM, Chatterjee A, Van Vliet MM, et al. A comparison of acellular dermal matrix to autologous dermal flaps in single-stage, implant-based immediate breast reconstruction: a cost-effectiveness analysis. Plast Reconstr Surg 2013;131:953-61. 10.1097/PRS.0b013e3182865a24 [DOI] [PubMed] [Google Scholar]
- 56.Gabriel A, Storm-Dickerson TL, Chan V, et al. Prepectoral Breast Reconstruction in Morbidly Obese Patients. Plast Reconstr Surg Glob Open 2022;10:e4261. 10.1097/GOX.0000000000004261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gabriel A, Sigalove S, Sigalove NM, et al. Effect of Body Mass Index on Outcomes after Prepectoral Breast Reconstruction. Plast Reconstr Surg 2019;144:550-8. 10.1097/PRS.0000000000005901 [DOI] [PubMed] [Google Scholar]
- 58.Rudolph M, Moore C, Pestana IA. Operative risk stratification in the obese female undergoing implant-based breast reconstruction. Breast J 2019;25:1182-6. 10.1111/tbj.13434 [DOI] [PubMed] [Google Scholar]
- 59.Kachare MD, Kachare SD, Vivace BJ, et al. Restoring Breast Volume in High BMI Patients: A Single-Center Review of Breast Reconstruction Using Hyperinflated Saline Implants. Eplasty 2022;22:e30. [PMC free article] [PubMed] [Google Scholar]
- 60.A Study of the Safety and Effectiveness of the Mentor Larger Size MemoryGel Ultra High Profile Breast Implants in Subjects Who Are Undergoing Primary Breast Reconstruction or Revision Reconstruction (Athena) ClinicalTrials.gov: U.S. National Library of Medicine; 2023 (Identifier: NCT02724371). Available online: https://clinicaltrials.gov/ct2/show/NCT02724371
- 61.Yesantharao PS, Nguyen DH. Hybrid breast reconstruction: a systematic review of current trends and future directions. Ann Breast Surg 2021;6:17. [Google Scholar]
- 62.Demiri EC, Dionyssiou DD, Tsimponis A, et al. Outcomes of Fat-Augmented Latissimus Dorsi (FALD) Flap Versus Implant-Based Latissimus Dorsi Flap for Delayed Post-radiation Breast Reconstruction. Aesthetic Plast Surg 2018;42:692-701. 10.1007/s00266-018-1081-6 [DOI] [PubMed] [Google Scholar]
- 63.Escandón JM, Escandón L, Ahmed A, et al. Breast reconstruction using the Latissimus Dorsi Flap and Immediate Fat Transfer (LIFT): A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg 2022;75:4106-16. 10.1016/j.bjps.2022.08.025 [DOI] [PubMed] [Google Scholar]
- 64.Palve J, Luukkaala T, Kääriäinen M. Comparison of Different Techniques in Latissimus Dorsi Breast Reconstruction: Plain, Immediately Lipofilled, and Implant Enhanced. Ann Plast Surg 2022;88:20-4. 10.1097/SAP.0000000000002798 [DOI] [PubMed] [Google Scholar]
- 65.Schwartz JC. Goldilocks Mastectomy: A Safe Bridge to Implant-Based Breast Reconstruction in the Morbidly Obese. Plast Reconstr Surg Glob Open 2017;5:e1398. 10.1097/GOX.0000000000001398 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as