Abstract
Background:
The medial patellofemoral ligament (MPFL) is the primary soft tissue restraint to lateral patellar translation and is often disrupted by lateral patellar dislocation. Surgical management for recurrent patellar instability focuses on restoring the MPFL function with repair or reconstruction techniques. Recent studies have favored reconstruction over repair; however, long-term comparative studies are limited.
Purpose:
To compare long-term clinical outcomes, complications, and recurrence rates of isolated MPFL reconstruction and MPFL repair for recurrent lateral patellar instability.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A total of 55 patients (n = 58 knees) with recurrent lateral patellar instability were treated between 2005 and 2012 with either MPFL repair or MPFL reconstruction. The exclusion criteria were previous or concomitant tibial tubercle osteotomy or trochleoplasty and follow-up of <8 years. Pre- and postoperative descriptive, surgical, imaging, and clinical data were recorded for each patient.
Results:
MPFL repair was performed on 26 patients (n = 29 knees; 14 women, 15 men), with a mean age of 18.4 years. MPFL reconstruction was performed on 29 patients (n = 29 knees; 18 women, 11 men), with a mean age of 18.2 years. At a mean follow-up of 12 years (range, 8.3-18.9 years), the reconstruction group had a significantly lower rate of recurrent dislocation compared with the repair group (14% vs 41%; P = .019). There were no differences in the number of preoperative dislocations or tibial tubercle–trochlear groove distance. The reconstruction group had significantly more time from initial injury to surgery compared with the repair group (median, 1460 days vs 627 days; P = .007). There were no differences in postoperative Tegner, Lysholm, or Kujala scores at the final follow-up. In addition, no statistically significant differences were detected in return to sport (RTS) rates (repair [81%] vs reconstruction [75%]; P = .610) or reoperation rates for recurrent instability (repair [21%] vs reconstruction [7%]; P = .13).
Conclusion:
MPFL repair resulted in a nearly 3-fold higher rate of recurrent patellar dislocation (41% vs 14%) at the long-term follow-up compared with MPFL reconstruction. Given this disparate rate, the authors recommend MPFL reconstruction over repair because of the lower failure rate and similar, if not superior, clinical outcomes and RTS.
Keywords: dislocation, instability, medial patellofemoral ligament, patella, reconstruction, repair
Lateral patellar dislocation is a common injury—particularly among young athletes. 27 An acute dislocation often leads to partial or complete disruption of the medial patellofemoral ligament (MPFL)—the primary restraint to lateral patellar subluxation.5,8,15 Historically, the standard of care for most patients with a first-time dislocation is nonoperative treatment, while patients with recurrent instability are generally treated with surgery.30,32 Patellar instability is a complex problem and requires a multifactorial approach. In addition to disruption of the MPFL, other factors contributing to instability include trochlear dysplasia, lateralized tibial tubercle, patella alta, limb rotation, limb alignment, and patellar tilt.16,24 In the absence of dysplasia or malalignment, focus is placed on the MPFL.
Multiple techniques have been described to repair or reconstruct the MPFL to restore its function.7,19,20 Additionally, surgical technique remains an important factor in patient outcomes and complications. Recent trends favor MPFL reconstruction because of the reported higher rates of failure, defined as recurrent subluxation and/or dislocation after repair,1,3,22 and favorable outcomes after reconstruction.10-12 MPFL reconstruction has also shown favorable results with regard to rates of return to sport (RTS). 23
There is a paucity of literature comparing MPFL repair versus reconstruction with follow-up greater than the mean of 10 years (minimum, 8 years). Therefore, this study aimed to compare long-term clinical outcomes, complications, and recurrence rates of isolated MPFL reconstruction and MPFL repair for the treatment of recurrent lateral patellar instability. We hypothesized that similar rates of RTS but a higher rate of dislocation would be observed in the repair versus reconstruction group.
Methods
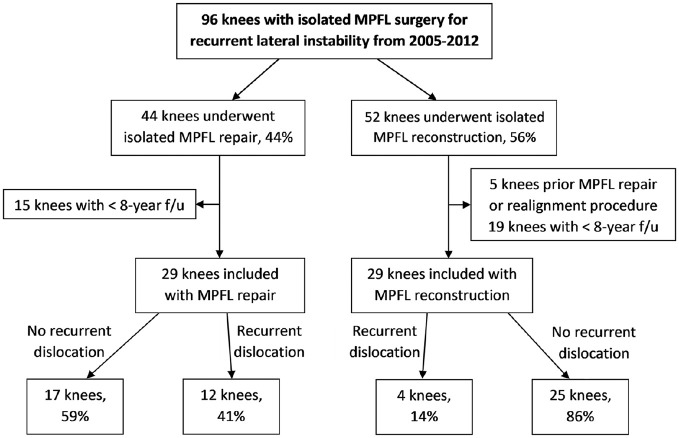
After receiving institutional review board approval, a retrospective review identified all patients who underwent MPFL reconstruction or MPFL repair at our institution between 2005 and 2012 for recurrent lateral patellar instability (n = 96 knees). Patients provided informed consent. Medical records were reviewed to confirm a diagnosis of recurrent instability with history, clinical examination, and advanced imaging characteristics—that is, MPFL injury on magnetic resonance imaging (MRI). The inclusion criteria were patients who had >1 episode of confirmed patellar dislocation or subluxation, had undergone either MPFL reconstruction or MPFL repair, and had a minimum follow-up of 8 years. The exclusion criteria were previous or concomitant tibial tubercle osteotomy or trochleoplasty. A total of 34 patients were excluded because they had a follow-up time of <8 years. Attempts were made to contact these patients via telephone and email but were unsuccessful. Thus, 58 knees were included in the study; 29 in 26 patients underwent MPFL repair, and 29 in 29 patients underwent MPFL reconstruction (Figure 1).
Figure 1.
Flowchart demonstrating patient inclusion and exclusion in the present study. MPFL, medial patellofemoral ligament.
Surgical Technique and Indication
All operations were performed at our institution between 2005 and 2012. Indications for revision surgery included an osteochondral loose body, symptomatic recurrent instability, or instability significantly impairing daily activities or sports. While the decision to repair or reconstruct the MPFL was made by the individual surgeon, the specific indication for one or the other is unknown. However, MPFL reconstruction was not commonly performed during the early years of the study period. Improved surgical techniques resulted in a shift from repair to reconstruction over time.
MPFL Reconstruction
MPFL reconstruction operations were performed by 6 surgeons at our institution—including the senior authors (M.J.S. and A.J.K). The mean time from initial injury to surgery was 4 years (range, 0.4-15.4 years). After diagnostic arthroscopy, dissection was performed in the plane between layers 2 and 3 in the anteromedial knee to allow for graft passage. 25 Graft fixation to the patella was achieved by either two 3.5-mm sockets using bioabsorbable interference screws (Arthrex) or a subperiosteal trough using 2 suture anchors (Arthrex). The knee was then placed at 90° of flexion, and the Schöttle point was identified on the medial aspect of the knee on true lateral fluoroscopic views.14,29 A small secondary incision was then made, and a guide pin was placed on the Schöttle point with fluoroscopic guidance. The graft was shuttled between layers 2 and 3 of the medial incision. Isometry was confirmed throughout an arc of motion. Subsequently, No. 2 nonabsorbable suture (FiberWire or FiberLoop; Arthrex) whipstitches were placed at the end of the hamstring graft for approximately 20 mm. A 6- to 7-mm socket corresponding to the graft diameter was reamed over the guide pin. The graft was inserted into the femoral socket with the knee at 30° of flexion and fixed using a bioabsorbable interference screw (Arthrex). The knee was then examined to ensure full extension, flexion, appropriate patellar tracking, and lateral patellar glide. The arthroscope was then reintroduced into the knee to ensure the patellar tracked well through the arc of motion and engaged the trochlear at about 30° of knee flexion.
Reconstruction Rehabilitation
The postoperative rehabilitation protocol in the early part of the study included partial weightbearing for the first 6 weeks with a knee immobilizer and crutches. Patients focused on active flexion and passive extension knee range of motion, quadriceps sets, and straight-leg raises. After 6 weeks, patients transitioned out of the knee immobilizer and crutches and started with progressive quadriceps strengthening exercises. Later in the study, patients were made weightbearing as tolerated immediately after surgery. Passive, active assisted, and active range of motion were initiated immediately postoperatively, with active range of motion limited to 90° of flexion. From weeks 2 to 6, the active range of motion progressed from 120° of flexion for the first 2 weeks postoperatively to full range of motion at 4 weeks postoperatively. During this time, quadriceps strength and endurance progressed with open kinetic chain body weight extensions and closed kinetic chain strengthening from 0° to 45° of flexion. From weeks 6 to 12, patients initiated resisted open kinetic chain exercises. The jogging program, as well as low-intensity plyometric and agility training, was started at 12 weeks if cleared by the surgeon. From months 4 to 6 after surgery, patients progressed in strength, endurance, and intensity of functional training. At 6 months, patients continued to progress with functional strengthening, began sport-specific training, and gradually returned to sport. Full RTS was allowed after functional assessment and evaluation by the supervising physician. At the time of this study, there was no standardized or consistent RTS criteria. However, all surgeons performed a physical examination and reviewed isokinetic strength testing results.
MPFL Repair
All MPFL repair surgeries were performed by 2 surgeons at our institution—including a senior author (M.J.S). The mean time from initial injury to the date of surgery was 1.7 years (range, 37-8.1 years). After diagnostic arthroscopy, a 4- to 7-cm incision—depending on the patient's anatomy and need for adequate visualization—was made over the medial border of the patella. Dissection was performed in a subperiosteal manner along the proximal two-thirds of the medial patella down to the interval between layer 2 (MPFL) and layer 3 (capsule). The interval between the 2 layers was then dissected toward the medial femoral epicondyle. After identifying the MPFL, a No. 2 nonabsorbable, locking whipstitch suture (FiberWire [Arthrex] or Ethibond [Ethicon]) was placed in the patellar end of the MPFL with suture anchors (FASTak [Arthrex], Corkscrew FT [Arthrex], or GII [DePuy Synthes]), and the ligament was tensioned to test the integrity of the ligament and femoral attachment. If the femoral attachment was not intact, 2 suture anchors were placed into the MPFL origin. A secondary incision was made over the MPFL femoral origin for femoral-sided repair when deemed necessary. If the patellar insertion was not intact, 2 suture anchors were placed at the patellar attachment of the MPFL. The locking whipstitch suture was then tied in a pants-over-vest fashion with the knee in 30° of flexion. Tension was applied until the patient's native translation, measured by the contralateral extremity, if not pathologic, was achieved. Otherwise, approximately 1 quadrant of lateral patellar translation was restored. The medial retinaculum was then repaired with No. 0 absorbable sutures. (FiberWire [Arthrex] or Ethibond [Ethicon]). After repair, an additional arthroscopic examination was performed to evaluate the joint and patellar tracking.
Repair Rehabilitation
The postoperative rehabilitation during the first 6 weeks after repair consisted of partial weightbearing using a knee immobilizer and crutches, active flexion, and passive extension knee range of motion, quadriceps sets, and straight leg-raise exercises. After 6 weeks, the crutches and immobilizer were discontinued, and patients began progressive resistance quadriceps strengthening exercises. Over time, these rehabilitation protocols evolved, and currently, at our institution, there is no difference in the protocol between MPFL repair and reconstruction.
Evaluation
Patient history, clinical examination data, radiographs, computed tomography (CT) scans, MRI, and surgical reports were reviewed retrospectively. Clinical data included descriptive information, such as age, sex, and body mass index, as well as a detailed history, including number of instability episodes (dislocation or subluxation), date of injuries, mechanism of injury, sports participation, type of reduction (spontaneous or requiring manual reduction), and any prior surgeries. All patients underwent pre- and postoperative physical examinations. The physical examination included hip and knee range of motion, generalized ligamentous laxity, patellofemoral crepitus, areas of tenderness to palpation, patellar apprehension, patellar glide, and lateral patellar tilt. Functional outcome measurements included preoperative Tegner scores and postoperative Tegner, Kujala, and Lysholm scores. A failure was defined as a repeat lateral patellar dislocation at any time after surgical treatment. Radiographic measurements were performed on CT images as previously described 4 and first interpreted by a musculoskeletal-trained radiologist, and confirmation was made by a board-certified orthopaedic surgeon .
Statistical Analysis
Data were collected and stored in Microsoft Excel (Version 2010; Microsoft Corp). After analyzing data for parametric/nonparametric assumptions, continuous variables were compared between age groups utilizing Student t tests or Wilcoxon rank-sum tests, and categorical variables were compared using chi-square analysis or the Fisher exact test when comparing descriptive and clinical data, failure rates, RTS rates, and outcome scores between MPFL repair and reconstruction groups. For multivariable analysis using significant or clinically important risk factors, we used multivariable logistic regression models and reported odds ratios (ORs) with 95% CIs. We reported relative risk (RR) with 95% CI for univariate analysis. Tests were 2-sided, and statistical significance was defined as P < .05. All analyses were performed using BlueSky Statistics (BlueSky Statistics LLC).
Results
Descriptive, Clinical, and Imaging Data
The mean postoperative follow-up period for the study patients was 12 years (range, 8.3-18.9 years). Descriptive data details according to the study group can be found in Table 1. Four patients in the MPFL repair group and 10 patients in the MPFL reconstruction group were radiographically diagnosed with trochlear dysplasia. Arthroscopic examination revealed 46 knees (79.3%) with patellofemoral chondromalacia (1 with grade 1, 26 with grade 2, 15 with grade 3, and 4 with grade 4) and 3 knees (5%) had osteochondral fractures. Medial patellar facet chondromalacia was noted in 22 of 29 patients in the reconstruction group. No patients in the reconstruction group were reported to have lateral patellar facet cartilage pathology. In the repair group, 22 of 29 patients had medial patellar facet chondromalacia, and 1 of 29 had lateral patellar facet chondromalacia. Chondral lesions were treated with debridement (24 knees [41.4%]), microfracture (4 knees [6.9%]), or open excision (1 knee [1.7%]), which was done for a firmly adherent displaced osteochondral fragment. In addition to patellofemoral pathology, lateral femoral condyle chondromalacia was noted in 8 knees (1 with grade 2, 2 with grade 3, and 5 with grade 4). Loose body removal was required in 24% of knees.
Table 1.
Demographic and Baseline Imaging Characteristics for the MPFL Repair and Reconstruction Groups a
| Characteristic | MPFL Repair (n = 29 Knees) | MPFL Reconstruction (n = 29 Knees) | P |
|---|---|---|---|
| Age at surgery, y | 18.4 (11.2-32.1) | 18.2 (10.3-31.7) | .84 |
| Age at initial injury, y | 16.7 (11-30.1) | 14.1 (6.4-24.9) | .02 |
| Sex, female, No. of knees | 14 | 18 | .29 |
| Preoperative dislocations (≥3) | 17 (59) | 21 (72) | .27 |
| Generalized laxity | 1 (3) | 13 (45) | .01 |
| Sport participation | 25 (86) | 27 (93) | .23 |
| Time from injury to surgery, d | 627 (37-2946) | 1460 (151-5635) | .01 |
| TT-TG distance, mm | 13.7 ± 4.2 | 13.4 ± 3.9 | .884 |
| Follow-up, y | 14.4 ± 2.4 | 9.7 ± 1 | .01 |
Data are reported as mean (range), mean ± SD, or n (%) unless otherwise indicated. Boldface P values indicate statistically significant differences between groups (P < .05). MPFL, medial patellofemoral ligament; TT-TG, tibial tubercle–trochlear groove.
Reconstruction graft choice included autograft semitendinosus (n = 13), autograft gracilis (n = 15), and autograft quadriceps tendon (n = 1). Five patients had previous MPFL surgery or concomitant distal realignment procedure during MPFL repair or reconstruction. There were no significant differences in demographic variables between the repair and reconstruction groups, including sex, number of preoperative dislocations, or sports participation (Table 1). However, preoperative generalized laxity was observed in 45% of the patients in the reconstruction group compared with 3% in the repair group (P = .01). The median number of days from the initial instability event to surgery was 1460 days in those who eventually went on to MPFL reconstruction, while the patients in the repair group had 627 days from injury to surgery (P = .01). The mean tibial tubercle–trochlear groove (TT-TG) distance was 13.7 mm in the repair group and 13.4 mm in the reconstruction group (P = .884) (Table 1).
Surgical Outcomes
Twelve knees (41%) experienced a redislocation after MPFL repair compared with 4 knees (14%) after MPFL reconstruction at the final follow-up (P = .019). There was no significant difference between reoperation rates in the 2 groups (repair, 21% vs reconstruction, 14%; P = .487). Postoperative Tegner, Lysholm, and Kujala scores showed no significant difference between the groups at the final follow-up (Table 2). RTS rates were 81% after MPFL repair and 75% after MPFL reconstruction (P = .610).
Table 2.
Comparison of Outcomes After MPFL Repair and Reconstruction a
| Outcome | MPFL Repair (n = 29 Knees) | MPFL Reconstruction (n = 29 Knees) | P |
|---|---|---|---|
| Tegner score | 5.3 ± 1.7 | 4.9 ± 1.6 | .39 |
| Median (IQR) | 6 (4.5-7.5) | 4 (2.5-6.5) | |
| Lysholm score | 80.5 ± 20.5 | 87.6 ± 9.5 | .54 |
| Kujala score | 86.7 ± 19.1 | 88.1 ± 10.8 | .75 |
| RTS | 21 (81) | 21 (75) | .61 |
| Failure | 12 (41) | 4 (14) | .02 |
| Reoperation | 6 (21) | 4 (14) | .49 |
| Instability | 6 (21) | 2 (7) | .13 |
| Complication | 15 (52) | 9 (31) | .11 |
Data are reported as mean ± SD or No. of knees (%) unless otherwise indicated. The boldface P value indicates a statistically significant difference between groups (P < .05). IQR, interquartile range; MPFL, medial patellofemoral ligament; RTS, return to sport.
The complication rate was 52% in the repair group and 31% in the reconstruction group (P = .11) (Table 2). Complications included 14 recurrent subluxations and 1 knee with patellofemoral pain in the repair group and 7 recurrent subluxations, 1 stitch abscess, and 1 wound complication in the reconstruction group. Six reoperations were performed in the repair group for recurrent instability; 1 knee underwent revision MPFL repair, and the other 5 underwent MPFL reconstructions. In the reconstruction group, 4 reoperations were performed with 2 reoperations for recurrent instability; revision MPFL reconstruction was performed in these 2 cases. The 2 other reoperations included 1 irrigation and debridement for a superficial infection and 1 scar revision (Table 2).
Risk Factors for Failure
Univariate analysis revealed no significant differences in age at initial injury, sex, presence of generalized laxity, sports participation, time from injury to surgery, preoperative TT-TG, or preoperative Blackburne-Peel ratio between patients with and without repeat patellar dislocation after surgery. However, there were significant differences in the age at surgery (19.1 ± 4.6 vs 16.1 ± 4.7 years; P = .03). Univariate analysis also identified MPFL reconstruction as a factor to decrease the risk of failure (RR, 0.33; P = .02) (Table 3).
Table 3.
Results of Univariate Analysis of Risk for Failure After MPFL Surgery a
| RR (95% CI) | P | |
|---|---|---|
| Male sex | 1.58 (0.68-3.67) | .280 |
| Ligamentous laxity | 2.10 (0.94-4.68) | .114 |
| ≥3 preoperative dislocations | 1.58 (0.58-4.26) | .348 |
| Reconstruction | 0.33 (0.12-0.91) | .019 |
The boldface P value indicates statistical significance (P < .05). MPFL, medial patellofemoral ligament; RR, relative risk.
Additional multivariate analysis identified MPFL reconstruction (OR, 0.23; P = .02) and age at surgery (OR, 0.83 per year; P = .04) as factors to potentially decrease the risk of failure when controlling for surgical technique, including age at surgery and initial injury, sex, ligamentous laxity, number of preoperative dislocations (≥ 3), time from injury to surgery, preoperative TT-TG, and preoperative Blackburne-Peel ratio (Table 4).
Table 4.
Potential Risk Factors for Failure After MPFL Surgery a
| OR (95% CI) | P | |
|---|---|---|
| Reconstruction | 0.23 (0.06-0.82) | .024 |
| Male sex | 1.89 (0.59-6.06) | .284 |
| Age at surgery | 0.83 (0.69-0.99) | .043 |
| Age at initial instability | 0.92 (0.79-1.07) | .269 |
| Ligamentous laxity | 3.56 (0.69-18.28) | .129 |
| ≥3 preoperative dislocations | 1.85 (0.51-6.72) | .352 |
| Time from injury to surgery | 1.00 (0.99-1.0002) | .115 |
| TT-TG | 1.03 (0.80-1.32) | .833 |
| Blackburne-Peel ratio | 1 (0.92-1.08) | .992 |
Boldface P values indicate statistical significance (P < .05). MPFL, medial patellofemoral ligament; OR, odds ratio; TT-TG, tibial tubercle–trochlear groove.
Discussion
The most important finding of the present study is that the failure rate after isolated MPFL repairs was nearly 3-fold higher (41%) compared with MPFL reconstruction (14%) at a mean of 12 years after surgery. Surgical technique (ie, MPFL reconstruction) and increased age at the time of surgery were shown to decrease failure risk. However, there were no significant differences in postoperative outcomes scores, complication rates, reoperation rates, or RTS between the 2 groups at the final follow-up. These findings are clinically relevant because they highlight satisfactory patient-reported outcomes of MPFL reconstruction compared with repair while also demonstrating the lower rate of failure observed with reconstruction at the long-term follow-up. Importantly, given the OR of 0.23 with a 95% CI of 0.06 to 0.82 for failure after MPFL surgery, this finding is clinically meaningful and statistically robust.
The failure rate in the MPFL repair group was 41% compared with 14% in the MPFL reconstruction group at the final follow-up. It is important to consider the definition of failure when comparing studies in the literature. The present study defined failure as a recurrent dislocation. The literature has consistently shown that isolated MPFL reconstruction has a lower failure rate compared with repair, particularly with short- and midterm follow-up studies. MPFL reconstruction failure rates, defined as recurrent dislocation, range from 0% to 6%, with a follow-up of between 3.5 and 6 years.2,9,13,26 Failure rates after MPFL repair have demonstrated greater variability compared with MPFL reconstruction. Camp et al 3 reported a 28% repair failure rate at a mean follow-up of 4 years and Puzzitiello et al 26 reported a 37% failure rate at a mean follow-up of 5 years. In contrast, Dragoo et al 9 had 1 repair failure out of 16 (6%) at a mean follow-up of 4 years. The present study further demonstrates the higher failure rate after isolated MPFL repair compared with isolated MPFL reconstruction in patients with recurrent patellar instability.
Despite the differences in failure, the present study showed no significant differences in postoperative Tegner, Lysholm, and Kujala scores at the final follow-up. RTS rates were also similar between the repair and reconstructions groups. These findings are consistent with previous studies comparing MPFL repair and reconstruction with short- to midterm follow-ups.9,26 Erickson et al 13 reported on patients with isolated MPFL reconstruction with RTS rates of 90% and 88% at 1 and 2 years, respectively. Another study found similar RTS rates at a mean follow-up of 4.5 years. 23 Time to RTS and the level of RTS were beyond the scope of this study; however, the literature has reported times of RTS after reconstruction of 8.8 to 10.4 months. 13 Less is known regarding the level at which athletes can expect to RTS. Still, limited data suggest up to 67% of patients return to the same level of competition after MPFL reconstruction. Based on the current literature and present study, athletes can expect good outcomes after MPFL repair or reconstruction,3,9,26 but there remains a paucity of data regarding the level of RTS and time to RTS. 21
When accounting for demographic, clinic, and imaging factors, MPFL reconstruction and older age at the time of surgery were protective against recurrent dislocations. 18 These findings are corroborated by numerous studies, including a recent meta-analysis by Hurley et al. 18 Although this study did not identify additional risk factors, factors predicting MPFL repair and reconstruction failure have been described, including a Caton-Deschamps Index ≥1.3 and a preoperative positive J-sign for failure of repair, 28 trochlear dysplasia, patella alta, preoperative J-sign, and femoral tunnel malposition for failure of reconstruction. 6 However, several notable demographic and clinical differences existed between the reconstruction and repair groups. The reconstruction group was observed to have significantly higher generalized laxity. Additionally, the time from initial injury to surgery was significantly longer for the reconstruction group as compared with the repair. These differences may be explained by surgeon selection bias, as chronic injuries and poor tissue quality due to ligamentous laxity may be less amenable to repair, with recent evidence suggesting that even acute injuries with good tissue quality have inferior outcomes with repair compared with reconstruction. 17 In either case, these factors can make stabilizing the patellofemoral joint more challenging. Despite these potential disadvantages in the reconstruction group, the failure rates were much lower. This further highlights the success of reconstruction versus repair for patellar instability.
Limitations
This study is not without limitations. First, this is a retrospective review of patients at a single institution treated with isolated MPFL surgery and with loss to follow-up. Thus, there is potential for bias in patient treatment selection and follow-up. Second, patients were treated by multiple surgeons over a 7-year span, which resulted in multiple surgical techniques, variations in rehabilitation protocols, and no specific definition of “laxity.” Third, the repair technique may not have adequately addressed the site of MPFL injury (midsubstance, femoral attachment of multiple locations). Fourth, as trochlear dysplasia becomes increasingly understood, there is evidence that isolated MPFL reconstruction may not be sufficient. 31 Last, the relatively small numbers may have resulted in the inability to detect differences between the outcomes of the 2 groups.
Conclusion
MPFL repair resulted in a nearly 3-fold higher rate of recurrent patellar dislocation (41% vs 14%) at long-term follow-ups compared with MPFL reconstruction. Given this disparate rate, the authors recommend MPFL reconstruction over repair because of the lower failure rate and similar, if not superior, clinical outcomes and RTS.
Footnotes
Final revision submitted June 1, 2023; accepted July 31, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.L.C. has received research support from Major League Baseball; education payments from Arthrex; consulting fees from Arthrex; nonconsulting fees from Arthrex, Zimmer Biomet Holdings, and Gemini Mountain Medical; and royalties from Arthrex. D.B.F.S. has received research support from JRF Ortho and consulting fees from NewClip. A.J.K. has received research support from Aesculap, Arthrex, Arthritis Foundation, Ceterix, and Histogenics; grants from DJO and Exactech; consulting fees from Arthrex, JRF Ortho, Vericel, and Responsive Arthroscopy; nonconsulting fees from Arthrex; royalties from Arthrex, JRF Ortho, and Responsive Arthroscopy; honoraria from MTF Biologics, JRF Ortho, and Responsive Arthroscopy; and hospitality payments from Gemini Mountain Medical and Smith & Nephew and serves on the medical board of trustees for MTF Biologics. M.J.S. has received research support from Stryker; education payments from Arthrex; consulting fees from Arthrex; nonconsulting fees from Arthrex; and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Mayo Clinic (ref No. PR15-000601-09).
References
- 1. Arendt EA, Moeller A, Agel J. Clinical outcomes of medial patellofemoral ligament repair in recurrent (chronic) lateral patella dislocations. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1909-1914. [DOI] [PubMed] [Google Scholar]
- 2. Basso M, Arnaldi E, Tamini J, Bruno AAM. Medial patellofemoral ligament reconstruction with autologous gracilis tendon: clinical and radiological outcomes at a mean 6 years of follow up. Knee. 2021;33:252-259. [DOI] [PubMed] [Google Scholar]
- 3. Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38(11):2248-2254. [DOI] [PubMed] [Google Scholar]
- 4. Camp CL, Stuart MJ, Krych AJ, et al. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41(8):1835-1840. [DOI] [PubMed] [Google Scholar]
- 5. Conlan T, Garth WP, Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682-693. [DOI] [PubMed] [Google Scholar]
- 6. Cregar WM, Huddleston HP, Wong SE, Farr J, Yanke AB. Inconsistencies in reporting risk factors for medial patellofemoral ligament reconstruction failure: a systematic review. Am J Sports Med. 2022;50(3):867-877. [DOI] [PubMed] [Google Scholar]
- 7. Desai VS, Tagliero AJ, Parkes CW, et al. Systematic review of medial patellofemoral ligament reconstruction techniques: comparison of patellar bone socket and cortical surface fixation techniques. Arthroscopy. 2019;35(5):1618-1628. [DOI] [PubMed] [Google Scholar]
- 8. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65. [DOI] [PubMed] [Google Scholar]
- 9. Dragoo JL, Nguyen M, Gatewood CT, Taunton JD, Young S. Medial patellofemoral ligament repair versus reconstruction for recurrent patellar instability: two-year results of an algorithm-based approach. Orthop J Sports Med. 2017;5(3):2325967116689465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Drez D, Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17(3):298-306. [DOI] [PubMed] [Google Scholar]
- 11. Ellera Gomes JL. Medial patellofemoral ligament reconstruction for recurrent dislocation of the patella: a preliminary report. Arthroscopy. 1992;8(3):335-340. [DOI] [PubMed] [Google Scholar]
- 12. Ellera Gomes JL, Stigler Marczyk LR, Cesar de Cesar P, Jungblut CF. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy. 2004;20(2):147-151. [DOI] [PubMed] [Google Scholar]
- 13. Erickson BJ, Nguyen J, Gasik K, et al. Isolated medial patellofemoral ligament reconstruction for patellar instability regardless of tibial tubercle-trochlear groove distance and patellar height: outcomes at 1 and 2 years. Am J Sports Med. 2019;47(6):1331-1337. [DOI] [PubMed] [Google Scholar]
- 14. Featherall J, Metz AK, Froerer DL, et al. The Schöttle point is consistently located distal to the medial femoral physis in pediatric patients: a digitally reconstructed radiographic study. Am J Sports Med. 2022;50(13):3565-3570. [DOI] [PubMed] [Google Scholar]
- 15. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114-1121. [DOI] [PubMed] [Google Scholar]
- 16. Hevesi M, Heidenreich MJ, Camp CL, et al. The recurrent instability of the patella score: a statistically based model for prediction of long-term recurrence risk after first-time dislocation. Arthroscopy. 2019;35(2):537-543. [DOI] [PubMed] [Google Scholar]
- 17. Hiemstra LA, Kerslake S, Kupfer N, Lafave M. Patellofemoral stabilization: postoperative redislocation and risk factors following surgery. Orthop J Sports Med. 2019;7(6):2325967119852627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hurley ET, Colasanti CA, Anil U, et al. Management of patellar instability: a network meta-analysis of randomized control trials. Am J Sports Med. 2022;50(9):2561-2567. [DOI] [PubMed] [Google Scholar]
- 19. Husen M, Milbrandt TA, Shah V, et al. Medial patellofemoral ligament reconstruction using allografts in skeletally immature patients. Am J Sports Med. 2023;51(6):1513-1524. [DOI] [PubMed] [Google Scholar]
- 20. Kay J, Memon M, Ayeni OR, Peterson D. Medial patellofemoral ligament reconstruction techniques and outcomes: a scoping review. Curr Rev Musculoskelet Med. 2021;14(6):321-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lampros RE, Tanaka MJ. Return to play considerations after patellar instability. Curr Rev Musculoskelet Med. 2022;15(6):597-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Matic GT, Magnussen RA, Kolovich GP, Flanigan DC. Return to activity after medial patellofemoral ligament repair or reconstruction. Arthroscopy. 2014;30(8):1018-1025. [DOI] [PubMed] [Google Scholar]
- 23. Meynard P, Malatray M, Sappey-Marinier E, et al. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation allows a good rate to return to sport. Knee Surg Sports Traumatol Arthrosc. 2022;30(6):1865-1870. doi: 10.1007/s00167-021-06815-1 [DOI] [PubMed] [Google Scholar]
- 24. Parikh SN, Lykissas MG, Gkiatas I. Predicting risk of recurrent patellar dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Parvaresh K, Huddleston HP, Yanke AB. Medial patellofemoral ligament reconstruction with concomitant lateral patellofemoral reconstruction for patellar instability. Arthrosc Tech. 2021;10(9):e2099-e2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Puzzitiello RN, Waterman B, Agarwalla A, et al. Primary medial patellofemoral ligament repair versus reconstruction: rates and risk factors for instability recurrence in a young, active patient population. Arthroscopy. 2019;35(10):2909-2915. [DOI] [PubMed] [Google Scholar]
- 27. Sanders TL, Pareek A, Hewett TE, et al. Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health. 2018;10(2):146-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sappey-Marinier E, Sonnery-Cottet B, O’Loughlin P, et al. Clinical outcomes and predictive factors for failure with isolated MPFL reconstruction for recurrent patellar instability: a series of 211 reconstructions with a minimum follow-up of 3 years. Am J Sports Med. 2019;47(6):1323-1330. [DOI] [PubMed] [Google Scholar]
- 29. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801-804. [DOI] [PubMed] [Google Scholar]
- 30. Shubin Stein BE, Gruber S, Brady JM. MPFL in first-time dislocators. Curr Rev Musculoskelet Med. 2018;11(2):182-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Vinod AV, Hollenberg AM, Kluczynski MA, Marzo JM. Ability of medial patellofemoral ligament reconstruction to overcome lateral patellar motion in the presence of trochlear flattening: a cadaveric biomechanical study. Am J Sports Med. 2021;49(13):3569-3574. [DOI] [PubMed] [Google Scholar]
- 32. Zheng X, Hu Y, Xie P, et al. Surgical medial patellofemoral ligament reconstruction versus non-surgical treatment of acute primary patellar dislocation: a prospective controlled trial. Int Orthop. 2019;43(6):1495-1501. [DOI] [PubMed] [Google Scholar]