Abstract
Introduction
During the COVID-19 outbreak, China applied a unique volunteerism system in which nurses and physicians traveled to the epicenter to care for patients. During the same period, another group, nurse and physician nonvolunteers, stayed at their home hospitals outside of the epicenter and cared for patients without COVID-19. Yet only one Chinese study examined psychological responses comparing these groups.
Objective
To explore whether relationships among compassion satisfaction, general health, attitude toward life, satisfaction with life, perceived stress, and posttraumatic stress disorder (PTSD) symptomatology differ between volunteers and nonvolunteers. Attitude toward life is examined for the first time in COVID-19 research.
Methods
A cross-sectional study was conducted (259 nurse and physician volunteers, 330 nurse and physician nonvolunteers). Online survey data were analyzed using multisample path analysis.
Results
There was no significant difference between volunteer and nonvolunteer models. In the volunteer model, paths significantly related to PTSD symptomatology included compassion satisfaction (total effect, β = −0.12), general health (total effect, β = −0.09), attitude toward life (direct effect, β = −0.30; total effect, β = −0.30), and perceived stress (direct effect, β = 0.30; total effect, β = 0.30), and in nonvolunteers included general health (direct effect, β = −0.11; total effect, β = −0.11) and attitude toward life (direct effect, β = −0.47; total effect, β = −0.47).
Conclusion
No significant difference between models means both groups could benefit from psychological intervention. Within each model, significant paths were identified. For volunteers, counselors might focus on compassion satisfaction and perceived stress and, for both volunteers and nonvolunteers, on health and attitude toward life. Delivering counseling based on key indicators in China may help prevent or mitigate PTSD. Globally, researchers could identify factors to target and determine to whom long-term counseling might be directed. Findings about attitude toward life lay the groundwork for future research.
Keywords: attitude toward life, path analysis, COVID-19
Introduction/Background
China experienced the first wave of coronavirus disease (COVID-19) between January and March 2020 and 40,000 health care volunteers (VOL) traveled across China to Hubei Province, the epicenter, to provide direct care to COVID-19 patients (China Youth On Line, 2020; Leung et al., 2020; The State Council The People's Republic of China, 2020a). Due to China's unique volunteerism system, Chinese nurses and physicians responded immediately to a national call to service, even with the uncertainty surrounding COVID-19, due to a sense of duty and patriotism to remedy a major health care deficit, a lack of frontline health care personnel (People's Daily, 2020). During this disaster, the threat of COVID-19 infection and overwhelmingly heavy workloads jeopardized the psychological well-being of health care providers (De Kock et al., 2021; National Administration of Disease Prevention and Control, 2020).
During this crisis at the epicenter, the National Health Commission of the People's Republic of China issued principles for emergency psychological intervention to help health care VOL cope and provided brief on-the-spot telephone counseling (Kang et al., 2020; National Administration of Disease Prevention and Control, 2020). Although it may have addressed satisfaction with life and perceived stress in crisis mode, this brief intervention might not have been sufficient to address more pathological sequelae such as posttraumatic stress disorder (PTSD) after health care providers returned to their home hospitals.
Now that three years have passed since the outbreak, countries such as the United States (U.S.), the United Kingdom, and China are becoming more aware of the severity of aftereffects and are calling for intensive, large-scale, and longer-term psychological interventions for health care providers internationally to mitigate the COVID-19-related psychological burden and improve psychological well-being (Organisation for Economic Co-operation and Development, 2021; The State Council The People's Republic of China, 2020b; Tri-Council for Nursing, 2021; Türközer & Öngür, 2020; Vostanis & Bell, 2020). Questions remain as to whom these extensive interventions might be directed and what psychological variables should be targeted.
Review of Literature
The overarching framework used in the current study is the HOPE model that reflects the content, context, and essence of disaster nursing (Hugelius & Adolfsson, 2019). Although the HOPE model was developed before the COVID-19 crisis, it can be applied to the personal, professional, and environmental situations surrounding this crisis because its core elements are highly applicable today: Holistic health assessment and promotion, Organization and management of immediate response, Professional adaptation, and Endurance and recovery (Hugelius & Adolfsson, 2019). This study focuses mainly on the final element, endurance and recovery. According to this model, disasters are characterized by being unpredictable, unplanned, unexpected, and uncertain; they result in a substantial amount of human suffering. Disasters result in serious disruption with shock, feeling overwhelmed, and frustration with not being able to make immediate changes to improve the situation. Losses and influences that are material, human, environment, and economic occur.
The HOPE model emphasizes how disasters dramatically change what is referred to as (a) personal borders such as comfort zone and moral obligation, (b) professional borders such as changing roles and new competencies demanded, and (c) environmental borders such as performance of duties outside of usual practice settings and safety concerns. The process of disaster nursing at the epicenter included being hit by reality, adapting to the conditions, providing aid, relief, and caring. Then recovering, remembering, and growing occur. The model also displays time across the event. During a crisis, short-term counseling is provided, but in the current context where the pandemic continues with varying degrees of outbreaks across countries, the concern now is getting long-term counseling to enhance psychological well-being of large numbers of people. Modeling first-wave conditions can help in decision-making about long-term counseling as it depicts the degree of challenges at hand.
The research based on psychological variables examined in health care providers at the epicenter is fragmented and limited. For example, one related study found moderate to high compassion satisfaction in frontline nurses (Jiang et al., 2021). Studies more generally on those psychological variables important to health care providers used one-group study designs. This was the case for perceived stress (Leng et al., 2021; Mo et al., 2020; Mo et al., 2021; Zhan et al., 2020; Zhang et al., 2020) and PTSD (Leng et al., 2021). Moreover, research on perceived stress in frontline VOL in China used various stress scales and cutoff scores.
Liao et al. (2021), a Chinese researcher, published initial work at the epicenter and studied groups of health care providers to determine who might need long-term psychological counseling in China. Specifically, the VOL were frontline health care VOL who traveled to Hubei Province and worked directly with COVID-19 patients. In contrast, the nonvolunteers (NV) were health care providers outside of Hubei Province who had no contact with COVID-19 patients. On the face of it, one might predict that frontline health care providers should be given psychological counseling first and need it the most. However, this premise may or may not be the case. First, there are few studies that serve as a research base to support or refute this idea. Second, Liao et al. (2021) found in a large sample that perceived stress was lower in the VOL than in NV. This is an interesting finding that deserves further study.
No research was found that examined general health in the COVID-19 literature, yet people have reported specific symptoms (Ren et al., 2021; Zhou et al., 2021). More research on general health using advanced modeling techniques is warranted.
One psychological response not yet examined in the COVID-19-related literature is the novel measure, attitude toward life. This measure encompasses the elements of evaluation of ordinary life and connectedness, evaluation of individual efforts, and the futility of life. Attitude toward life already has established importance in a previous earthquake disaster situation in Asia (Uchida et al., 2014) as well as in qualitative studies in which health care providers described rethinking their life situation because of the COVID-19 crisis (Liu et al., 2020; Sun et al., 2020). Quantitative studies are needed on attitude toward life within a COVID-19 context.
The purpose of the current study is to extend the work of Liao et al. (2021) and, in addition, include a novel psychological measure, attitude toward life. We explored, using multisample path analysis, whether the models of relationships among compassion satisfaction, general health, attitude toward life, satisfaction with life, perceived stress, and PTSD symptomatology differ between contrasting groups: frontline health care VOL in Hubei Province and a health care nonvolunteer group outside Hubei Province with no COVID-19 patient contact. For the purpose of this paper, compassion satisfaction is defined as the pleasure derived from work (Professional Quality of Life, 2021). General health refers to individuals’ perceptions about their health status (Centers for Disease Control and Prevention [CDC], 2018). Attitude toward life reflects the meaning of life (Uchida et al., 2014). Satisfaction with life is defined as how much a person likes his/her life (Veenhoven, 1996). Perceived stress refers to the feelings or thoughts that an individual has about how much stress they are under at a given point in time or over a given time period (Phillips, 2016). Posttraumatic stress disorder refers to an anxiety problem that develops after extremely traumatic events, such as a natural disaster (American Psychological Association [APA], 2022) with PTSD symptomatology comprised of four clusters of symptoms: reexperiencing the event, alterations in arousal, avoidance, and negative alterations in cognition and mood (APA, 2013). These specific constructs were chosen to examine in the current analyses based on a review of the previous literature pertaining to experiences of health care providers during the pandemic (He et al., 2021; Liu et al., 2020; Sun et al., 2020) as well as their important health and quality of life implications for health care providers. Due to the exploratory nature of the analyses, no a priori hypothesis was made regarding whether relationships among psychological and health variables differ between VOL and NV groups.
Methods
Design
The current study used a cross-sectional design. Reporting was done following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (Equator Network, 2021).
Research Question
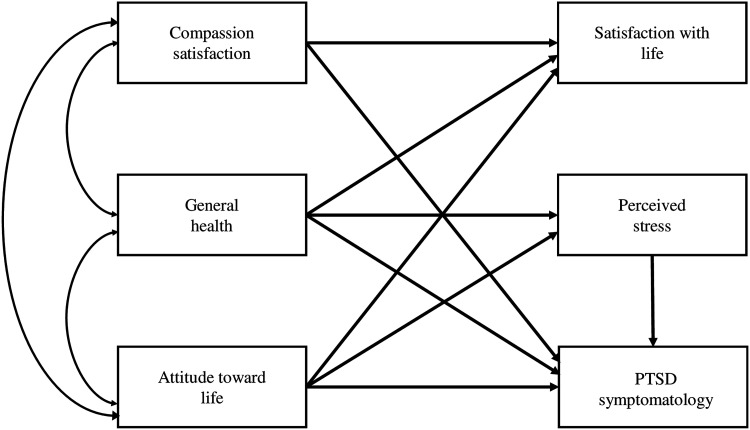
The research question is: Using multisample path analysis, do the models of relationships among compassion satisfaction, general health, attitude toward life, satisfaction with life, perceived stress, and PTSD symptomatology differ between frontline health care VOL in Hubei Province and health care NV outside Hubei Province with no COVID-19 patient contact? A hypothesized model that is used in path analysis is presented in Figure 1. This model was built upon previous psychological research (Guo et al., 2014; Haber et al., 2013; Jacobowitz et al., 2015; Samios, 2018; Schiff & Lane, 2019; Tirgari et al., 2019) and COVID-19-related research (González-Pando et al., 2022; Kader et al., 2021; Leng et al., 2021; Rogowska et al., 2020; Zheng et al., 2020), illustrating a framework that depicts relationships among psychological and health variables.
Figure 1.
The hypothesized model.
Sample
Convenience sampling was used in the current study. A nurse researcher recruited participants by inviting nurse directors, chief physicians, and team leaders from eight provinces in Central, Southern, Eastern, and Western China to send a clickable online survey invitation to eligible health care providers on their lists. Although the clinical leaders had lists of potential participants, it was not administratively possible to have them do random sampling.
Inclusion/Exclusion Criteria
Inclusion criteria for VOL were nurses or physicians >18 years of age; signed up as VOL, traveled, had direct contact with patients with COVID-19 in Hubei Province; and returned to their home hospitals outside of Hubei Province; and volunteered to participate in the study. Inclusion criteria for NV were nurses or physicians >18 years of age; worked at home hospitals outside of Hubei Province during COVID-19; had no contact with COVID-19 patients; and volunteered to participate in the study. An exclusion criterion was a lack of internet access. Sample size was determined for multivariate analysis using a rule of thumb recommending 10 respondents for each of the 49 items (Tabachnick & Fidell, 2007).
Ethical Considerations
The current study complied with the Declaration of Helsinki. Individuals participated in the study anonymously and voluntarily. Ethical approvals were obtained from Institutional Review Boards at a U.S. university (approval number: 275305) and a Chinese hospital (approval number: 2020LWKY022). A digital consent was obtained from each participant. Permissions were obtained for the use of research instruments.
Study Instruments
Compassion satisfaction was measured using a subscale of the Professional Quality of Life Scale Version 5 (Stamm, 2010). This is a 10-item subscale that measures the pleasure derived from being able to do work well. It uses a 5-point, Likert-type scale (never to very often). A sample item is: I get satisfaction from being able to help people. A total score ≤22 indicates low, between 23 and 41 indicates moderate, and ≥42 indicates high compassion satisfaction. Cronbach's alpha was 0.82 (Zheng et al., 2013). In the current study, Cronbach's alpha was 0.94 in VOL and 0.95 in NV.
General health was measured using the General Health item from the Healthy Days core questions (CDC, 2018). It uses a 5-point, Likert-type scale (scored 1–5, poor to excellent). The item is: After the experience of COVID-19, would you say that in general your health was poor, fair, good, very good, or excellent?
Attitude toward life was measured using the total score of a Japanese Attitude Toward Life Scale (Uchida et al., 2011). This 10-item scale assesses how individuals’ attitude toward life is changed after a disaster; one item, conceptually nontranslatable to Chinese culture, was eliminated. The first item measured the degree of change in attitude toward life after the experience of COVID-19 using a 5-point, Likert-type scale (not changed at all to changed a lot). Only participants who choose changed somewhat or changed a lot are automatically directed to the rest of the scale, which uses a 7-point Likert-type scale (strongly disagree to strongly agree). The scale has three factors: evaluation of ordinary life and connectedness, evaluation of individual efforts, and the futility of life (Uchida et al., 2014). Sample items listed by factor are: (a) evaluation of ordinary life and connectedness (I began to feel that normal everyday living is important and makes me happy. I started wanting to place a higher value on the connection with my local community); (b) evaluation of individual efforts (I started wanting to place a higher value on the sense of fulfillment I get from work or academics); and (c) the futility of life (I began to feel that no matter how hard I try, it's all in vain). Cronbach's alpha ranged from 0.89 to 0.97 (Uchida et al., 2014). In the current study, Cronbach's alpha was 0.66 in VOL and 0.69 in NV.
Satisfaction with life was measured using the total score of the Satisfaction with Life Scale, a 5-item scale assessing global cognitive judgments of satisfaction with one's life (Diener et al., 1985). It uses a 7-point Likert-type scale (strongly disagree to strongly agree; Diener, 2017). A sample item is: If I could live my life over, I would change almost nothing. Cronbach's alpha was 0.88 (Bai et al., 2011). In the current study, Cronbach's alpha was 0.87 in both VOL and NV.
Perceived stress was measured using the total score of the Perceived Stress Scale; this 4-item scale examines experiencing stress in various life situations (Carnegie Mellon University Laboratory for the Study of Stress, Immunity and Disease, 2015). It uses a 5-point, Likert-type scale (scored 0–4, never to very often). A sample item is: How often did you feel difficulties were piling up so high that you could not overcome them? Cronbach's alpha was 0.67 (Leung et al., 2010). In the current study, Cronbach's alpha was 0.62 in VOL and 0.56 in NV.
Posttraumatic stress disorder symptomatology was measured using the total score of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a 20-item scale designed to assess the severity of 20 DSM-5 symptoms of PTSD (U.S. Department of Veterans Affairs PTSD, 2022). It uses a 5-point, Likert-type scale (scored 0–4, not at all to extreme). A sample item is: Taking too many risks or doing things that could cause you harm. Consistent with clinical guidance, the current study used a cutoff score ≥31 for probable PTSD (National Center for PTSD, 2021). Cronbach's alpha was 0.95 (Fung et al., 2019). In the current study, Cronbach's alpha was 0.96 in VOL and 0.97 in NV.
Data Collection Procedure
A survey by invitation only was administered using a Chinese online web-based platform (www.wjx.cn). It had 17 questions about demographic and clinical information and 49 about psychological and health responses. Questions were distributed on 11 pages with 6 questions per page. Usability and technical functionality of the online survey were thoroughly pilot tested. By clicking on the online survey invitation, participants were granted access to the survey between October 22 and November 20, 2020. The Chinese platform required participants to fill in all items. The surveys were completed anonymously to reduce response bias and minimize risk. No incentive was offered. Data entry was web-based and data were captured automatically. Data were exported from www.wjx.cn and stored in a password-protected computer that was only accessible to researchers.
Statistical Analysis
All completed surveys were analyzed. In the one case of a duplicate IP address, the first of the two completed surveys was retained. To compare VOL and the NV groups in terms of demographic, psychological, and health variables, independent sample t-tests, and chi-square tests were used. Bivariate correlation was utilized to examine relationships among psychological and health variables in VOL and NV groups. Path analysis was applied to monitor the influence and total effect of compassion satisfaction, general health, and attitude toward life on satisfaction with life, perceived stress, and PTSD symptomatology in VOL and NV. To investigate this influence, the hypothesized model was applied to both the VOL and the NV groups. The hypothesized model was used to examine the group differences between VOL and NV by using the total sample. In order to examine the model of VOL being different from the model of NV, unconstrained and constrained model analyses were obtained, and a chi-square difference test was computed to examine if the constrained model was statistically different from the unconstrained model. The constrained model was the model with all parameters constrained to be equal between VOL and NV. The unconstrained model was the model with all parameters freely estimated.
After checking for VOL and NV model differences, each model's goodness of fit and modification indices were used to obtain the reported VOL and NV models. To check the model's goodness of fit for both groups, chi-square and goodness-of-fit indices, including comparative fit index (CFI) and Root Mean Square Error of Approximation (RMSEA), were used. A CFI value, ranging from 0 to 1 with recommending values >0.90, indicates a good fit. Typically, there is a good fit when RMSEA is <0.05 (Kline, 2016). Descriptive analyses were conducted using SPSS Statistics 26 and the path analysis was conducted using AMOS 26.
Results
Sample Characteristics
Data from 589 participants were analyzed, including 259 participants (229 nurses, 30 physicians; male = 65, female = 194) in VOL and 330 (313 nurses, 17 physicians; male = 18, female = 312) in NV. There were more males (p < .001) and more physicians (p = .004) in VOL than NV. Mean age in VOL (33.86 ± 5.52 years, range 23–51) was higher than in NV (30.58 ± 6.67 years, range 20–50; p < .001). The duration of work experience was longer in VOL (11.68 ± 5.93 years) than NV (8.88 ± 7.26 years; p < .001). In VOL, the duration of caring for COVID-19 patients was 48.70 ± 14.81 days. Additionally, the VOL group had significantly higher compassion satisfaction and satisfaction with life as well as significantly lower perceived stress compared to the NV group (Table 1). A higher percentage of nurses and physicians in the VOL group (80.69%) experienced at least somewhat of an attitude toward life change compared to the NV group (60.91%; p < .001). Tables 2 and 3 showed bivariate correlations among psychological and health variables in VOL and NV groups.
Table 1.
Psychological and Health Variables in Volunteers (VOL) and Nonvolunteers (NV).
| Variables | VOL (n = 259) | NV (n = 330) | p value | |
|---|---|---|---|---|
| Compassion satisfaction (Mean ± SD) | 35.78 ± 6.43 | 32.20 ± 6.92 | <.001 | |
| General health | 2.81 ± 0.84 | 2.80 ± 0.81 | .796 | |
| Attitude toward life a (Mean ± SD) | 10.31 ± 10.26 | 10.79 ± 11.75 | .656 | |
| Satisfaction with life (Mean ± SD) | 20.61 ± 6.06 | 19.34 ± 5.81 | .010 | |
| Perceived stress (Mean ± SD) | 7.27 ± 1.66 | 7.62 ± 1.53 | .008 | |
| PTSD symptomatology (Mean ± SD) | 10.79 ± 11.06 | 10.69 ± 11.78 | .912 | |
| Have probable PTSD (%) | 7.72 | 10.00 | .338 | |
PTSD = posttraumatic stress disorder.
Have probable PTSD = PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders score ≥31.
Because of the scoring requirements of the Attitude Toward Life Scale, for this variable, 209 participants were in the VOL group and 201 participants were in the NV group.
Table 2.
Bivariate Correlations Among Psychological and Health Variables in Volunteers (VOL; n = 259).
| Variable | Compassion satisfaction | General health | Attitude toward life | Satisfaction with life | Perceived stress | PTSD symptomatology |
|---|---|---|---|---|---|---|
| Compassion satisfaction | 1.00 | |||||
| General health | 0.29* | 1.00 | ||||
| Attitude toward life a | 0.51* | 0.32* | 1.00 | |||
| Satisfaction with life | 0.51* | 0.52* | 0.30* | 1.00 | ||
| Perceived stress | −0.48* | −0.42* | −0.37* | −0.55* | 1.00 | |
| PTSD symptomatology | −0.31* | −0.25* | −0.39* | −0.29* | 0.41* | 1.00 |
Because of the scoring requirements of the Attitude Toward Life Scale, for correlations involving attitude toward life, data from 209 participants were analyzed in the VOL group.
*p < .001.
Table 3.
Bivariate Correlations Among Psychological and Health Variables in Nonvolunteers (NV; n = 330).
| Variable | Compassion satisfaction | General health | Attitude toward life | Satisfaction with life | Perceived stress | PTSD symptomatology |
|---|---|---|---|---|---|---|
| Compassion satisfaction | 1.00 | |||||
| General health | 0.36** | 1.00 | ||||
| Attitude toward life a | 0.47** | 0.18* | 1.00 | |||
| Satisfaction with life | 0.50** | 0.39** | 0.27** | 1.00 | ||
| Perceived stress | −0.46** | −0.34** | −0.30** | −0.51** | 1.00 | |
| PTSD symptomatology | −0.28** | −0.21** | −0.49** | −0.23** | 0.30** | 1.00 |
Because of the scoring requirements of the Attitude Toward Life Scale, for correlations involving attitude toward life, data from 201 participants were analyzed in the NV group.
*p < .05, **p < .001.
Multisample Path Analysis Results
The constrained model, with all parameters set to be equal between VOL and NV, had goodness-of-fit values of χ2 (15) = 62.16, p < .05, CFI = 0.94, RMSEA = 0.07. The unconstrained model with all parameters freely estimated had goodness-of-fit values of χ2 (6) = 52.13, p < .05, CFI = 0.95, RMSEA = 0.11. A chi-square difference test indicated that the constrained and the unconstrained models were not significantly different, χ2dif = 10.03, df = 9, p = .348. Therefore, the VOL model was not significantly different from the NV model.
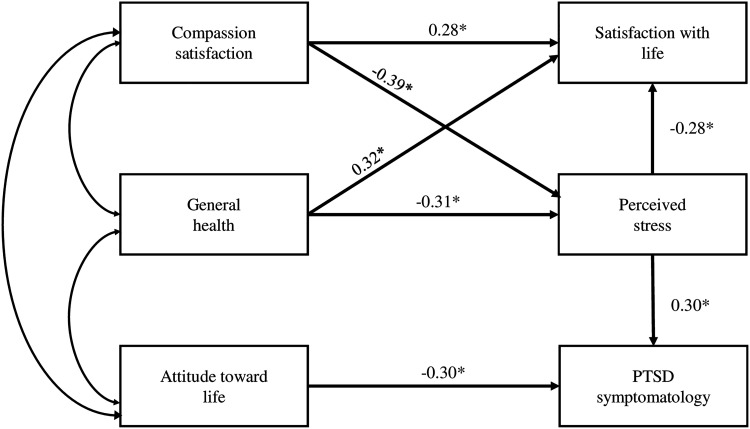
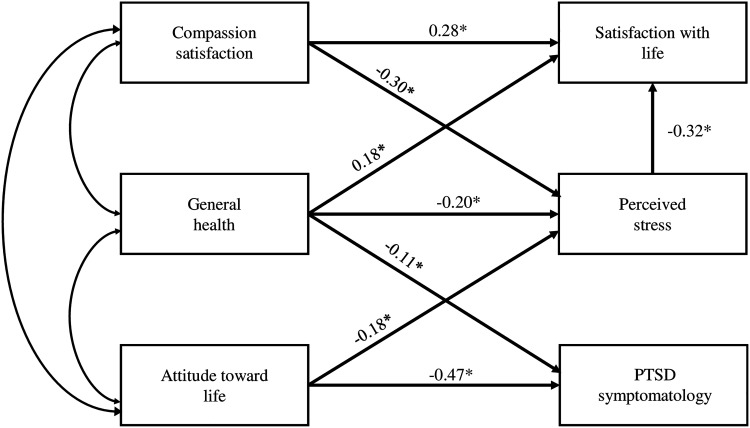
After checking the goodness of fit of the hypothesized model (Figure 1) for both groups and applying necessary modifications to ensure model fit, the models for VOL and NV groups were obtained (Figures 2 and 3). Volunteers data had a χ2 (5) = 4.84, p = .44, CFI >0.95, RMSEA < 0.05. Nonvolunteers data had a χ2 (4) = 6.15, p = .19, CFI >0.95, RMSEA < 0.05.
Figure 2.
Path analysis model for volunteers.
Figure 3.
Path analysis model for nonvolunteers *p < .05.
In the VOL group (Figure 2), compassion satisfaction and general health (r = 0.29), compassion satisfaction and attitude toward life (r = 0.55), and general health and attitude toward life (r = 0.30) were significantly correlated. In the NV group (Figure 3), compassion satisfaction and general health (r = 0.36), compassion satisfaction and attitude toward life (r = 0.53), and general health and attitude toward life (r = 0.22) were significantly correlated.
Table 4 shows standardized path coefficients for direct and total effects in the VOL and NV models. For example, in the VOL model, significant paths related to PTSD symptomatology included: (a) compassion satisfaction and PTSD symptomatology (total effect, β = −0.12); (b) general health and PTSD symptomatology (total effect, β = −0.09); (c) attitude toward life and PTSD symptomatology (direct effect, β = −0.30; total effect, β = −0.30); and (d) perceived stress and PTSD symptomatology (direct effect, β = 0.30; total effect, β = 0.30). In the NV model, significant paths related to PTSD symptomatology included: (a) general health and PTSD symptomatology (direct effect, β = −0.11; total effect, β = −0.11) and (b) attitude toward life and PTSD symptomatology (direct effect, β = −0.47; total effect, β = −0.47).
Table 4.
Standardized Path Coefficients in Models for Volunteers (VOL) and Nonvolunteers (NV).
| Paths | VOL (n = 259) | NV (n = 330) | ||||
|---|---|---|---|---|---|---|
| Direct effects | Total effects | Direct effects | Total effects | |||
| Satisfaction with life | ||||||
| Compassion satisfaction → satisfaction with life | 0.28* | 0.39 | 0.28* | 0.38 | ||
| General health → satisfaction with life | 0.32* | 0.40 | 0.18* | 0.24 | ||
| Attitude toward life → satisfaction with life | – | – | – | 0.06 | ||
| Perceived stress → satisfaction with life | −0.28* | −0.28 | −0.32* | −0.32 | ||
| Perceived stress | ||||||
| Compassion satisfaction → perceived stress | −0.39* | −0.39 | −0.30* | −0.30 | ||
| General health → perceived stress | −0.31* | −0.31 | −0.20* | −0.20 | ||
| Attitude toward life → perceived stress | – | – | −0.18* | −0.18 | ||
| PTSD symptomatology | ||||||
| Compassion satisfaction → PTSD symptomatology | – | −0.12 | – | – | ||
| General health → PTSD symptomatology | – | −0.09 | −0.11* | −0.11 | ||
| Attitude toward life → PTSD symptomatology | −0.30* | −0.30 | −0.47* | −0.47 | ||
| Perceived stress → PTSD symptomatology | 0.30* | 0.30 | – | – | ||
PTSD = posttraumatic stress disorder.
*p < .05.
Discussion
This study extends previous research (Liao et al., 2021) by incorporating a wider variety of relevant psychological and health variables from the literature; the measure of attitude toward life in the current study is novel. Compared to the NV group, a significantly higher percentage of health care providers in the VOL group experienced at least somewhat of an attitude toward life change, reflecting that they reevaluated their life situations when directly facing a disaster (Uchida et al., 2014). This difference might be due to the strong powerlessness that frontline health care VOL experienced when facing the unknown future at the epicenter (He et al., 2021). Compared to NV, VOL might be more likely to reassess what things were meaningful to their lives after returning from the epicenter. In the pandemic context, the Attitude Toward Life Scale had content validity, had items that resonated with health care providers, and was feasible in an online survey setting. Future research is warranted to study the scale with diverse populations.
Like Liao et al. (2021), in the current study, perceived stress was lower in the volunteer group than the nonvolunteer group. The reason for the lower perceived stress in the volunteer group may be due to receiving COVID-19-related training, psychological support, and living accommodations that the NV did not receive (Liao et al., 2021). Although no differences were found between VOL and NV models, the volunteer group reported lower perceived stress than the nonvolunteer group. This is unexpected and should be the focus of future research.
This study also extends previous research (Liao et al., 2021) by successfully utilizing a high-level statistical modeling technique, multisample path analysis. Due to the exploratory nature of the current study, there is no evidence base to explain why VOL and NV models were not significantly different. This lack of difference between the models indicates that both groups could benefit from psychological counseling. One such therapy is cognitive processing therapy, a specific type of cognitive behavioral therapy developed to reduce symptoms of PTSD occurring after a variety of traumatic events including natural disasters (APA, 2017). It has been recommended by international practice guidelines as a frontline intervention to target PTSD (Haagen et al., 2015). Future studies are needed, especially large-scale randomized controlled trials with diverse samples, to determine the effectiveness of cognitive processing therapy on PTSD in nurses and physicians within the current COVID-19 context in China.
An advantage of the multisample path analysis technique used in the current study is that we can use those paths with a significant total effect on PTSD symptomatology to identify potential key early indicators to prevent PTSD and inflection points for intervention to mitigate PTSD for VOL and NV groups. In the VOL group, potential key early indicators to prevent PTSD and inflection points for intervention to mitigate PTSD are compassion satisfaction, general health, attitude toward life, and perceived stress. This means that improving compassion satisfaction or improving general health would be associated with reducing perceived stress and consequently associated with reducing the severity of PTSD symptomatology. Improving attitude toward life or reducing perceived stress would be associated with reducing the severity of PTSD symptomatology. In the current study, compassion satisfaction was most frequently at a moderate level, general health only good or fair, and mean attitude toward life low in the VOL group; therefore, counseling to focus on these variables in the VOL group may have beneficial effects.
The research base underlying the significant paths we discovered through path analysis is minimal. In the current study, in the VOL model, compassion satisfaction was negatively correlated with perceived stress, and perceived stress was positively correlated with PTSD symptomatology. These two relationships were consistent with findings during the pandemic in one-group studies on frontline nurses in Spain (González-Pando et al., 2022) and frontline nurse VOL in China (Leng et al., 2021).
In the NV group, potential key early indicators to prevent PTSD and inflection points for intervention to mitigate PTSD are general health and attitude toward life. This means that enhancing general health or improving attitude toward life would be associated with reducing the severity of PTSD symptomatology. In the current study, general health was only good or fair, and mean attitude toward life was low in the NV group; counseling to emphasize these variables in the NV group may have beneficial effects. Overall, future studies need to be done to determine (a) if VOL would benefit from cognitive processing therapy with emphasis on compassion satisfaction, general health, attitude toward life, and perceived stress and (b) if NV would benefit from cognitive processing therapy with emphasis on general health and attitude toward life.
Strengths and Limitations
The study has major strengths. This is the first study to use the Attitude Toward Life Scale (Uchida et al., 2014) during COVID-19 and explore the relationships between attitude toward life and other psychological responses. Additionally, the design incorporating a multisample approach with advanced modeling techniques was more rigorous than that found in other studies in the literature. A limitation of the current study is the use of self-report measures, which could have resulted in overestimation or underestimation of psychological burden. Additionally, due to the cross-sectional design, causality cannot be inferred from the results; the path analytical approach provides probabilistic causality (Kline, 2016). Although the sampling technique is nonrandom, which reduces the representativeness, recruiting participants across China allows for a greater generalizability of study findings. The Attitude Toward Life Scale and the 4-item Perceived Stress Scale should undergo further testing by Chinese health care providers. Data on availability of psychological supporting resources were not available and, therefore, could not be examined in the current study. Furthermore, analysis was not conducted by sex due to a large difference in male and female sample sizes. Finally, generalization of these findings outside of China should be done with caution.
Implications for Practice
The current findings support the importance of assessing attitude toward life. With future research, could this instrument be used for nurse managers to learn to identify early signs of colleagues’ attitude toward life deteriorating? In this way, could nurses and physicians facilitate early intervention and help avert psychological sequelae such as PTSD? Future research on the relationships of attitude toward life, PTSD symptomatology, and counseling outcomes is warranted.
Researchers should consider studying indicators that directly impact patient outcomes, as well as procedures that support health care providers’ well-being and enhance workforce capacity, which may improve patient care (National Academies, 2022). The holistic approach of the HOPE model takes both aspects, outcomes and supports, into consideration (Hugelius & Adolfsson, 2019). According to the HOPE model, health care providers in disasters go through a phase of recovery to move beyond the disaster mode or scene (Enduring and recovery). However, a difference now is, due to the long-term nature and uncertainties of the pandemic, the recovery process and emphasizing concern and support must continue to be extended into the future. Administrators should continue to support personnel by developing initiatives to mitigate stress in working environments to facilitate recovery and prevent triggering negative psychological issues, such as PTSD (Buchan et al., 2022).
According to the pandemic disaster guideline developed by the Tri-Council for Nursing in 2021, mental health and well-being during the pandemic is an important area that provides critical lessons and future opportunities for transforming health care (Tri-Council for Nursing, 2021). The Tri-Council guideline recommends providing free and easy access to mental health resources. Additionally, similar to current high priorities regarding physical health, the status of psychological well-being should be elevated as an equally important outcome measure of success (Tri-Council for Nursing, 2021).
A concern remains about the education of nursing students and their facilitation in uncertain times (Tri-Council for Nursing, 2021). Students tend not to recognize or prioritize mental health. Furthermore, textbooks and curricula are deficient related to students’ resilience and well-being particularly during crisis situations. The guideline recommends redesigning curricula to better incorporate mental health content and skills about stress self-assessment and coping strategies during disasters to improve clinical practice and enhance students’ ability to promote mental health in the workplace (Robinson et al., 2023; Tri-Council for Nursing, 2021).
According to Sustain and Retain in 2022 and Beyond the Global Nursing Workforce and the COVID-19 Pandemic, a document issued by the International Council of Nurses (Buchan et al., 2022), the pandemic has greatly disrupted nurse retention and staffing and consequently has reduced patient care quality and increased hospital costs. Our finding about the associations between general health and PTSD in health care providers, regardless of COVID-19 patient contact, lends credence to the vital role of ensuring health in the health care workforce. Ensuring that nurses and physicians globally have priority access to full vaccinations (Buchan et al., 2022) is an essential and universal approach to improve general health and retention.
Globally, countries are recognizing that they need to prepare to administer long-term psychological interventions for health care providers (Organisation for Economic Co-operation and Development, 2021; The State Council The People's Republic of China, 2020b; Tri-Council for Nursing, 2021; Türközer & Öngür, 2020; Vostanis & Bell, 2020). Findings of the current study have national applications in China, specifically pointing out to whom extensive interventions might be directed and psychological and health variables targeted.
Conclusions
Our pioneering work using advanced modeling techniques suggests that psychological therapy in China should be delivered to both volunteer and nonvolunteer health care providers. We found significant paths that identified potential key early indicators that could be targeted within each group to prevent or mitigate PTSD. Although this is the first study of its kind, the findings do suggest that, for VOL, counselors might focus on compassion satisfaction and perceived stress and, for both VOL and NV, they might focus on general health and attitude toward life. Delivering counseling based on these key indicators may reduce COVID-19's aftereffects. Given that this is the first study to use attitude toward life in COVID-related research, this novel measure requires future study.
Supplemental Material
Supplemental material, sj-docx-1-son-10.1177_23779608231215580 for A Multisample Path Analysis Including a Novel Psychological Indicator, Attitude Toward Life, After the First Wave of COVID-19 by Fan Li, Haiping Gu, Umit Tokac, Kimberly Werner, Anne F. Fish and Qingqing Lou in SAGE Open Nursing
Acknowledgments
The authors thank all nurses and physicians who spent their time and effort to participate in the study.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Considerations: The current study complied with the Helsinki Declaration. Prior approval of using and revising research instruments was obtained from creators of research instruments. Individuals participated in the study anonymously and voluntarily. The study was approved by the Institutional Review Board at the University of Missouri – St. Louis (approval number: 275305) and the Institutional Review Board at the Affiliated Hospital of Integrated Traditional Chinese and Western Medicine, Nanjing University of Chinese Medicine (approval number: 2020LWKY022). Digital consent was obtained from each participant.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Qingqing Lou https://orcid.org/0000-0002-4743-0900
Supplemental Material: Supplemental material for this article is available online.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. [Google Scholar]
- American Psychological Association (2017, July 31). Cognitive processing therapy. https://www.apa.org/ptsd-guideline/treatments/cognitive-processing-therapy .
- American Psychological Association (2022, September). Post traumatic stress disorder. https://www.apa.org/pubs/highlights/ptsd#:∼:text=Posttraumatic%20Stress%20Disorder%20(PTSD)%20is,from%20APA%20Publishing%20about%20PTSD.
- Bai X., Wu C., Zheng R., Ren X. (2011). The psychometric evaluation of the satisfaction with life scale using a nationally representative sample of China. Journal of Happiness Studies, 12(2), 183–197. 10.1007/s10902-010-9186-x [DOI] [Google Scholar]
- Buchan J., Catton H., Shaffer F. A. (2022, January). Sustain and retain in 2022 and beyond: The global nursing workforce and the COVID-19 pandemic. International Council of Nurses. https://www.icn.ch/system/files/2022-01/Sustain%20 and%20Retain%20in%202022%20and%20Beyond-%20The%20global%20nursing%20workforce%20and%20the%20COVID-19%20pandemic.pdf.
- Carnegie Mellon University Laboratory for the Study of Stress, Immunity, and Disease (2015, February 19). Dr. Cohen’s scales. https://www.cmu.edu/dietrich/ psychology/stress-immunity-disease-lab/scales/index.html.
- Centers for Disease Control and Prevention (2018, October 31). CDC HRQOL-14 “Healthy Days Measure”. https://www.cdc.gov/hrqol/hrqol14_measure.htm .
- China Youth On Line (2020, March 17). From health care volunteers arrived in Hubei Province to their leave: A timeline to record how China did it. http://news.cyol. com/content/2020-03/17/content_18519149.htm.
- De Kock J. H., Latham H. A., Leslie S. J., Grindle M., Munoz S. A., Ellis L., Polson R., O'Malley C. M. (2021). A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health, 21(1), 1–18. 10.1186/s12889-020-10070-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E. (2017, September 9). Satisfaction With Life Scale (SWLS). https://eddiener. com/scales/7.
- Diener E., Emmons R. A., Larsen R. J., Griffin S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- Equator Network (2021, April 13). The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. https://www.equator-network.org/reporting-guidelines/strobe/ . [DOI] [PMC free article] [PubMed]
- Fung H. W., Chan C., Lee C. Y., Ross C. A. (2019). Using the post-traumatic stress disorder (PTSD) checklist for DSM-5 to screen for PTSD in the Chinese context: A pilot study in a psychiatric sample. Journal of Evidence-Based Social Work, 16(6), 643–651. 10.1080/26408066.2019.1676858 [DOI] [PubMed] [Google Scholar]
- González-Pando D., González-Nuevo C., González-Menéndez A., Alonso-Pérez F., Cuesta M. (2022). The role of nurses’ professional values during the COVID-19 crisis. Nursing Ethics, 29(2), 293–303. 10.1177/09697330211034250 [DOI] [PubMed] [Google Scholar]
- Guo J., Wu P., Tian D., Wang X., Zhang W., Zhang X., Qu Z. (2014). Post-traumatic stress disorder among adult survivors of the Wenchuan earthquake in China: A repeated cross-sectional study. Journal of Anxiety Disorders, 28(1), 75–82. 10.1016/j.janxdis.2013.12.001 [DOI] [PubMed] [Google Scholar]
- Haagen J. F., Smid G. E., Knipscheer J. W., Kleber R. J. (2015). The efficacy of recommended treatments for veterans with PTSD: A metaregression analysis. Clinical Psychology Review, 40, 184–194. 10.1016/j.cpr.2015.06.008 [DOI] [PubMed] [Google Scholar]
- Haber Y., Palgi Y., Hamama-Raz Y., Shrira A., Ben-Ezra M. (2013). Predictors of professional quality of life among physicians in a conflict setting: The role of risk and protective factors. The Israel Journal of Psychiatry and Related Sciences, 50(2), 174–181. [PubMed] [Google Scholar]
- He Q., Li T., Su Y., Luan Y. (2021). Instructive messages and lessons from Chinese countermarching nurses of caring for COVID-19 patients: A qualitative study. Journal of Transcultural Nursing, 32(2), 96–102. 10.1177/1043659620950447 [DOI] [PubMed] [Google Scholar]
- Hugelius K., Adolfsson A. (2019). The HOPE model for disaster nursing—a systematic literature review. International Emergency Nursing, 45, 1–9. 10.1016/j.ienj.2019.03.007 [DOI] [PubMed] [Google Scholar]
- Jacobowitz W., Moran C., Best C., Mensah L. (2015). Post-traumatic stress, trauma-informed care, and compassion fatigue in psychiatric hospital staff: A correlational study. Issues in Mental Health Nursing, 36(11), 890–899. 10.3109/01612840.2015.1055020 [DOI] [PubMed] [Google Scholar]
- Jiang W., Zhao X., Jiang J., Zhou Q., Yang J., Chen Y., Goldsamt L., Williams A. B., Li X. (2021). Hospital ethical climate associated with the professional quality of life among nurses during the early stage of COVID-19 pandemic in Wuhan, China: A cross-sectional study. International Journal of Nursing Sciences, 8(3), 310–317. 10.1016/j.ijnss.2021.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kader N., Elhusein B., Chandrappa N. S. K., Nashwan A. J., Chandra P., Khan A. W., Alabdulla M. (2021). Perceived stress and post-traumatic stress disorder symptoms among intensive care unit staff caring for severely ill coronavirus disease 2019 patients during the pandemic: A national study. Annals of General Psychiatry, 20(1), 38–46. 10.1186/s12991-021-00363-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B., Wang Y., Hu J., Lai J., Ma X., Chen J., Guan L., Wang G., Ma H., Liu Z. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry, 7(3), e14. 10.1016/S2215-0366(20)30047-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R. B. (2016). Principles and practice of structural equation modeling (4th ed). Guilford Press. [Google Scholar]
- Leng M., Wei L., Shi X., Cao G., Wei Y., Xu H., Zhang X., Zhang W., Xing S., Wei H. (2021). Mental distress and influencing factors in nurses caring for patients with COVID-19. Nursing in Critical Care, 26(2), 94–101. 10.1111/nicc.12528 [DOI] [PubMed] [Google Scholar]
- Leung D. Y., Lam T. H., Chan S. S. (2010). Three versions of perceived stress scale: Validation in a sample of Chinese cardiac patients who smoke. BMC Public Health, 10, 1–7. https://doi.org/1010.1186/1471-2458-10-513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung K., Wu J. T., Liu D., Leung G. M. (2020). First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: A modelling impact assessment. The Lancet, 395(10233), 1382–1393. 10.1016/S0140-6736(20)30746-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao C., Guo L., Zhang C., Zhang M., Jiang W., Zhong Y., Lin Q., Liu Y. (2021). Emergency stress management among nurses: A lesson from the COVID-19 outbreak in China–a cross-sectional study. Journal of Clinical Nursing, 30(3-4), 433–442. 10.1111/jocn.15553 [DOI] [PubMed] [Google Scholar]
- Liu Q., Luo D., Haase J. E., Guo Q., Wang X. Q., Liu S., Xia L., Liu Z., Yang J., Yang B. X. (2020). The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. The Lancet Global Health, 8(6), e790–e798. https://doi.org/0.1016/S2214-109X(20)30204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo Y., Deng L., Zhang L., Lang Q., Liao C., Wang N., Qin M., Huang H. (2020). Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. Journal of Nursing Management, 28(5), 1002–1009. 10.1111/jonm.13014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo Y., Deng L., Zhang L., Lang Q., Pang H., Liao C., Wang N., Tao P., Huang H. (2021). Anxiety of nurses to support Wuhan in fighting against COVID-19 epidemic and its correlation with work stress and self-efficacy. Journal of Clinical Nursing, 30(3-4), 397–405. 10.1111/jocn.15549 [DOI] [PubMed] [Google Scholar]
- National Academies (2022). National plan for health workforce well-being. https://nap.nationalacademies.org/catalog/26744/national-plan-for-health-workforce-well-being.
- National Administration of Disease Prevention and Control (2020, January 27). A notification: Recommendations for urgent psychological interventions to cope with COVID-19 crisis. http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467.shtml .
- National Center for PTSD. (2021). Using the PTSD Checklist for DSM-5 (PCL-5). https://www. ptsd.va.gov/professional/assessment/documents/using-PCL5.pdf.
- Organisation for Economic Co-operation and Development (2021, May 12). OECD policy responses to coronavirus (COVID-19)-Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response. https://www.oecd.org/coronavirus/policy-responses/tackling-the-mental-health-impact-of-the-covid-19-crisis-an-integrated-whole-of-society-response-0ccafa0b .
- People’s Daily (2020, January 24). Medical teams across China volunteered to come to Wuhan. https://wap.peopleapp.com/article/5071825/4966282 .
- Phillips A. C. (2016). Perceived stress. In Encyclopedia of behavioral medicine (pp. 1453–1454). Springer. [Google Scholar]
- Professional Quality of Life (2021, July 14). The ProQOL 5 self-score. https://img1. wsimg.com/blobby/go/dfc1e1a0-a1db-4456-9391-18746725179b/down loads/ProQOL_5_English_Self-Score.pdf?ver=1622777390411.
- Ren H., Luo X., Wang Y., Guo X., Hou H., Zhang Y., Yang P., Zhu F., Hu C., Wang R., Sun Y., Du Y., Yin Q., Xu G., Zuo H., Hu Q., Wang Y. (2021). Psychological responses among nurses caring for patients with COVID-19: A comparative study in China. Translational Psychiatry, 11(1), 1–9. 10.1038/s41398-020-00993-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson K. R., Gierach M., Bartelt S., Wolles B., McClellan C., Hodge J., Lovro J. (2023). Battle of COVID-19: Frontline nurses feel abandoned during the pandemic. American Nurse Journal, 18(3), 12–16. 10.51256/ANJ032312 [DOI] [Google Scholar]
- Rogowska A. M., Kuśnierz C., Bokszczanin A. (2020). Examining anxiety, life satisfaction, general health, stress and coping styles during COVID-19 pandemic in Polish sample of university students. Psychology Research and Behavior Management, 13, 797–811. 10.2147/PRBM.S266511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samios C. (2018). Burnout and psychological adjustment in mental health workers in rural Australia: The roles of mindfulness and compassion satisfaction. Mindfulness, 9(4), 1088–1099. 10.1007/s12671-017-0844-5 [DOI] [Google Scholar]
- Schiff J. W., Lane A. M. (2019). PTSD Symptoms, vicarious traumatization, and burnout in front line workers in the homeless sector. Community Mental Health Journal, 55(3), 454–462. 10.1007/s10597-018-00364-7 [DOI] [PubMed] [Google Scholar]
- Stamm B. H. (2010). The concise ProQOL manual. 2nd ed. https://img1.wsimg.com/blobby/go/dfc1e1a0-a1db-4456-9391-18746725179b/downloads/ProQOL% 20Manual.pdf?ver=1622839353725.
- The State Council The People’s Republic of China (2020a, May 13). Nurses accounted for almost 70% of health care volunteers who travelled to Hubei Province to fight against COVID-19. http://www.gov.cn/xinwen/2020-05/13/content_5511104.htm .
- The State Council The People’s Republic of China (2020b, March 19). A notification: plans for psychological interventions relevant to COVID-19. http://www.gov.cn/xinwen/2020-03/19/content_5493051.htm .
- Sun N., Wei L., Shi S., Jiao D., Song R., Ma L., Wang H., Wang C., Wang Z., You Y., Liu S., Wang H. (2020). A qualitative study on the psychological experience of caregivers of COVID-19 patients. American Journal of Infection Control, 48(6), 592–598. 10.1016/j.ajic.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B. G., Fidell L. S. (2007). Using multivariate statistics (5th ed.). Allyn & Bacon/Pearson Education. [Google Scholar]
- Tirgari B., Azizzadeh Forouzi M., Ebrahimpour M. (2019). Relationship between posttraumatic stress disorder and compassion satisfaction, compassion fatigue, and burnout in Iranian psychiatric nurses. Journal of Psychosocial Nursing and Mental Health Services, 57(3), 39–47. 10.3928/02793695-20181023-02 [DOI] [PubMed] [Google Scholar]
- Tri-Council for Nursing (2021, May). Transforming together: Implications and opportunities from the COVID-19 pandemic for nursing education, practice, and regulation. https://calhospital.org/wp-content/uploads/2021/05/Tri-Council-COVID-19-Report-5-2021.pdf .
- Türközer H. B., Öngür D. (2020). A projection for psychiatry in the post-COVID-19 era: Potential trends, challenges, and directions. Molecular Psychiatry, 25(10), 2214–2219. 10.1038/s41380-020-0841-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs National Center for PTSD (2022, November 10). PTSD checklist for DSM-5 (PCL-5). https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp.
- Uchida Y., Takahashi Y., Kawahara K. (2011, December). Behavior and well-being of young Japanese after the Great East Japan Earthquake. Economic and Social Research Institute, Cabinet Office. https://warp.da.ndl.go.jp/info:ndljp/pid/ 11539153/www.esri.go.jp/jp/archive/new_wp/new_wp030/new_wp024.pdf.
- Uchida Y., Takahashi Y., Kawahara K. (2014). Changes in hedonic and eudaimonic well-being after a severe nationwide disaster: The case of the great East Japan earthquake. Journal of Happiness Studies, 15, 207–221. 10.1007/s10902-013-9463-6 [DOI] [Google Scholar]
- Veenhoven R. (1996). The study of life-satisfaction. In Saris W. E., Veenhoven R., Scherpenzeel A. C., Bunting B. (Eds.), A comparative study of satisfaction with life in Europe (pp. 11–48). Eötvös University Press. [Google Scholar]
- Vostanis P., Bell C. A. (2020). Counseling and psychotherapy post-COVID-19. Counselling and Psychotherapy Research, 20(3), 389–393. 10.1002/capr.12325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhan Y., Ma S., Jian X., Cao Y., Zhan X. (2020). The current situation and influencing factors of job stress among frontline nurses assisting in Wuhan in fighting COVID-19. Frontiers in Public Health, 8, 1–6. 10.3389/fpubh.2020.579866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Peng D., Lv L., Zhuo K., Yu K., Shen T., Xu Y., Wang Z. (2020). Individual perceived stress mediates psychological distress in medical workers during COVID-19 epidemic outbreak in Wuhan. Neuropsychiatric Disease and Treatment, 16, 2529–2537. 10.2147/NDT.S266151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng L., Miao M., Gan Y. (2020). Perceived control buffers the effects of the COVID-19 pandemic on general health and life satisfaction: The mediating role of psychological distance. Applied Psychology: Health and Well-Being, 12(4), 1095–1114. 10.1111/aphw.12232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X., Yang M., Gao W., Chen F. (2013). The Chinese version professional quality of life scale: Testing of reliability and validity in nurses. Journal of Nursing Science, 28(5), 13–15. [Google Scholar]
- Zhou X. J., Dang Y. Y., Wang X., Yang W. Z., Lu W., Zhang J. H. (2021). Factors influencing nurses’ work interruption in Wuhan isolation wards during the COVID-19 pandemic. Medical Science Monitor, 27, e929851-1–e929851-8. https://doi.org/0.12659/MSM.92985 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-son-10.1177_23779608231215580 for A Multisample Path Analysis Including a Novel Psychological Indicator, Attitude Toward Life, After the First Wave of COVID-19 by Fan Li, Haiping Gu, Umit Tokac, Kimberly Werner, Anne F. Fish and Qingqing Lou in SAGE Open Nursing