Abstract
CMV infection is still a matter of concern in IBD patients, especially regarding the disease’s relapse management. Why IBD patients, particularly those affected by ulcerative colitis, are more susceptible to CMV reactivation is not totally explained, although a weakened immune system could be the reason. Various techniques, ranging from serology to histology, can be employed to detect intestinal CMV infection; however, there is currently disagreement in the literature regarding the most effective diagnostic test. Furthermore, CMV involvement in steroid resistance has been broadly discussed, but whether CMV infection is a cause or consequence of the disease severity and, consequently, steroid refractoriness is still debated. Its potential contribution to the lack of response to advanced therapy and small molecules must be more valued and wholly explored. In this review, we look at the actual literature on CMV in IBD patients, and we suggest a pragmatic algorithm for clinical practice management of CMV infection.
Keywords: infections, CMV, IBD, Crohn’s, ulcerative colitis
1. CMV Incidence and Prevalence in IBD Patients: The Size of the Problem
Cytomegalovirus (CMV) is a member of the herpes-virus family, which causes a broad spectrum of human illnesses depending on the host, but most commonly an asymptomatic viral infection (only detectable by serology or viral DNA). Clinically apparent infections (CMV disease) usually present as a mononucleosis-like syndrome but can affect potentially any organ of the human body [1,2].
The epidemiology of CMV infection and colitis varies according to the definition used to diagnose the infection due to the lack of a gold standard definition of clinically relevant CMV infection and CMV intestinal disease, to the severity of colitis, to the studied population, including immunological status, and to the geographical distribution. The highest prevalence of CMV disease is found in studies that used the positive serum polymerase chain reaction (PCR), followed by studies using antigenemia, where the definition of CMV infection is serum CMV replication.
The proportion of individuals with evidence of prior exposure to CMV varies worldwide, with seroprevalence rates in the adult population ranging between 40% in highly industrialized areas and 100% in developing countries [3]. Additionally, some studies indicate that the prevalence of CMV-specific antibodies rises with age, with rates ranging from 47% in children aged 10–12 to 81% in young adults aged 36–60. It also differs based on race, ethnicity, and other variables, such as female sex, foreign birthplace, low family income, overcrowding in the family, and low family education [4,5].
Regarding patients affected by inflammatory bowel disease (IBD), a recent meta-analysis showed no difference in latent CMV infection between IBD and healthy controls (69.6% vs. 51.8%, odds ratio [OR] = 1.36, 95% confidence interval [CI] = 0.45–4.14, p = 0.59). However, the authors found a significant difference between the two groups regarding the CMV IgM (5.5% vs. 0.59%, OR 7.14, 95% CI = 1.58–32.25, p = 0.01), with higher rates among IBD patients. Similarly, there was a significantly increased risk in IBD patients of serum CMV replication, as evidenced by CMV antigenemia (40.4% vs. 6.6%, OR 7.4) and the level of blood CMV DNA (42.5% vs. 26.4%, OR 4.99) [6,7]. These data agree with previous studies showing that subclinical reactivation of CMV during immunomodulator, steroid or biological therapy is common in IBD patients, but it is nearly always asymptomatic and self-limiting even if therapy is continued [7,8,9].
There are very few data on CMV detection in stool, and those available focus on IBD patient cohorts. However, a Scandinavian study in a cohort of IBD patients with active UC (n = 75) using quantitative stool-PCR found a prevalence of CMV of 40.4% compared to 21.3% determined via tissue immune histochemistry (IHC) [10].
When considering intestinal CMV infection, the association between IBD and CMV colitis has been recognized for 50 years [11]. However, data on the incidence and prevalence of CMV colitis among IBD patients still need to be clarified, mainly due to selection bias and heterogeneity in the methods used to diagnose CMV infection. The highest prevalence of CMV infection has been seen in studies that used tissue PCR greater than 10 copies/mg tissue. In an observational study, the CMV genome was detected using PCR on intestinal tissue samples in 32.9% of the IBD patients and only 2.4% of the controls, patients who underwent colonoscopy for other reasons such as anemia or non-IBD [12]. Studies regarding patients with inactive or mild-to-moderate ulcerative colitis (UC) have not shown an increased risk of CMV colitis, as diagnosed with hematoxylin and eosin (H&E) and IHC. Most of the literature, however, focuses on severe and/or steroid-refractory UC, terms used interchangeably and often not clearly defined. Therefore, the results are difficult to interpret [13].
The prevalence of CMV colitis diagnosed with H&E or IHC varies considerably between UC patients [14,15], ranging from 4.5% in new onset UC [16] to 16.6% in acute severe UC [17,18], and up to 36% in patients with acute severe colitis resistant to intravenous steroids [19]. The highest values were found in patients who needed an urgent colectomy, where the prevalence ranged between 11.5% and 27% [13].
Interestingly, a large observational study by Bontà et al. revealed a prevalence of 1.37% of CMV disease diagnosed with IHC in a cohort of 1023 consecutive IBD patients. All the patients who developed CMV colitis were receiving immunosuppressive medication, such as steroids, azathioprine, or infliximab, most frequently in combination, or had HIV infection (n = 1). None of the diagnosed cases was treated with infliximab as monotherapy [20]. Similarly, other research indicates that anti-TNFalpha has no effect on the CMV infection’s clinical course [21,22]. In particular, a previous prospective study found that infliximab was not associated with progression from CMV infection to disease [22]. Additionally, in another study, the authors even suggested treating colitis flare-ups associated with CMV reactivation with infliximab or adalimumab [21].
Contrary to UC, most studies have not shown an increased prevalence of CMV colitis diagnosed via IHC in patients with Crohn’s disease (CD). Some theories have been proposed to explain the different prevalence of CMV colitis among CD and UC patients. However, these results were obtained from small studies and should be carefully interpreted. One explanation suggests that in patients with IBD, tumor necrosis factor-alpha (TNF-α) might be associated with CMV infection or reactivation. At the same time, interferon-γ (IFNγ), produced by CD4+ T cells, might suppress CMV reactivation. According to some authors, in CD, the Th1-type inflammatory process could be enhanced with high expression of IFNγ, thereby explaining the lower prevalence of CMV colitis [13].
Factors that have been associated in previous studies with an increased risk of CMV reactivation in IBD patients include the female sex, pancolitis, advanced age (age > 30 years) [23,24,25], immunosuppressive therapy (steroids and azathioprine) [23] (OR 6.7), disease duration less than 60 months [OR 7.7], and blood leukocytes count less than 11/nl (OR 4.49) [23].
2. Clinical Implications
2.1. Clinical Presentation
Primary CMV infection is frequently asymptomatic but sometimes may present as a mononucleosis-like syndrome accompanied by systemic symptoms such as fever, leucopenia, splenomegaly, and lymphadenopathy [26]. Moreover, although uncommon, involvement of other organs is possible even in patients with IBD [27]. CMV colitis occurs with symptoms such as increased stool frequency, rectal bleeding, and tenesmus. For this reason, it may be difficult to distinguish it from an underlying flare of disease [26]. However, IBD patients seem to be more vulnerable to CMV reactivation, especially those with UC, probably because of an impaired immune reaction to the virus [28].
Following the initial phase of infection, CMV can move into a latent state in a variety of cell types, including cells of colonic mucosa. During this time, the immune system, in particular natural killer (NK) cells, maintains a control on the virus.
In IBD patients, there is an impaired immune system (NK and T cells) and an increase in inflammatory cytokines, especially TNF-α, which would encourage CMV reactivation. Indeed, TNF-alpha could trigger infected monocytes to differentiate into macrophages, which would enable the reactivated CMV to infect surrounding cells (interstitial, vascular endothelial, and epithelial cells) [29]. This would increase the production of IL-6 and trigger a vicious cycle with worsening colitis [30].
2.2. CMV Infection, Steroid Resistance and Outcomes
To date, differentiating a UC relapse from CMV colitis represents a major challenge in clinical practice. Furthermore, the clinical implications of CMV colitis, such as possible steroid refractoriness, must be evaluated with a view to treatment.
Regarding the correlation between the endoscopic severity of UC and CMV, there are contradictory results. While some research indicates that patients with CMV antigenemia show a higher prevalence of endoscopically severe UC than patients without antigenemia (p = 0.016) [31], other studies did not find a statistically significant association between the Mayo endoscopic score and the detection of CMV DNA in intestinal tissue [32]. Furthermore, specific endoscopic findings in patients with UC complicated by CMV infection were identified, such as pounced-out ulcers, wide mucosal defects and irregular ulcerations. In a study, the sensitivity of irregular ulceration for positive CMV was 100%; meanwhile, mucosal defects showed a specificity of 95% [33]. Similarly, a higher proportion of punched-out ulcers were observed among the patients with CMV colitis compared to the non-CMV control group (52.0% versus 20.0%, p-value = 0.04), with a sensitivity of 52.0% and a specificity of 77% [34].
However, Iida et al. revealed that punched-out ulcers were among the colonoscopic findings that were similar in CMV (+) and CMV (−) individuals [35]. Importantly, steroid-refractory illness had a much higher prevalence of these ulcers. These results point away from CMV infection and toward the possibility that perforated ulceration is a sign of disease severity, specifically of steroid refractoriness.
An increasing amount of evidence supports the notion that patients with acute severe colitis and CMV infection are more resistant to corticosteroid treatment than individuals without the infection.
Specifically, several meta-analyses suggest that CMV infection in IBD patients is associated with a two- to four-fold higher risk of steroid resistance [6,36,37].
Similarly, in a pediatric multicenter retrospective study [38], the authors demonstrated that, compared to CMV-negative patients, a higher proportion of CMV (+) patients were resistant to intravenous corticosteroid administration (p = 0.009).
Nevertheless, it is still completely unknown what leads to steroid resistance in IBD patients during CMV infection and if CMV infection is a cause or consequence of the disease severity and steroid refractoriness. A recent work by Wang et al. attempted to explain this mechanism [39]. It is commonly known that glucocorticoids, when bound to glucocorticoid α (GRα) receptors, have anti-inflammatory and immunosuppressive properties; conversely, glucocorticoid β (GRβ) binding has no effect. As demonstrated, the GRβ/α ratio significantly increases during the lytic phase of CMV reactivation.
Consequently, the refractory response to steroid treatment may be explained by these changes in receptors [28].
However, the influence of CMV on the response to therapies other than steroids, including the most recent biological and advanced one, has been poorly investigated.
Moreover, several studies have shown worse long-term outcomes in patients with CMV infection [40,41,42].
In a retrospective study, Zagorowicz et al. found that UC patients with CMV infection and high counts of CMV-positive cells on biopsy (defined as ≥5 CMV IHC-positive cells per section) had significantly lower colectomy-free survival than patients with less or no IHC-positive cells (1.9 vs. 3.2 years, respectively, p = 0.014) [40]. Schenk et al. found similar results in patients whose colonic biopsies revealed CMV-DNA positivity [41]. In fact, they reported that, over a median follow-up of nearly four years (52 months), patients with positive detection of CMV-DNA in biopsy had a higher rate of proctocolectomy (33.3% vs. 11.9%, p < 0.005). In order to assess the outcomes of CMV infection, a recent study examined 254,839 pediatric hospitalizations connected to IBD, including both CD and UC. As a result, they observed that CMV infection was associated with 3.5 times higher odds of in-hospital mortality (OR: 3.58; CI: 1.85 to 6.93, p < 0.001) and severe IBD (OR: 3.31; CI: 2.54 to 4.32, p < 0.001), which in turn contributed to a longer hospital stay (in fact, CMV infection increased the length of stay by 9 days) [42].
On the contrary, Delvicourt et al., in a case-control (n = 26) retrospective study, found no differences in terms of the length of hospital stay and 3-month colectomy rate [43]. They attempted to evaluate the impact of CMV reactivation on hospitalized patients experiencing an IBD flare and the effect of antiviral therapy on IBD flare. They found 8.7 days vs. 9.7 days (p = 0.42) and a colectomy rate of 15.4% vs. 23.1% (p = 0.48) for CMV+ and CMV patients, respectively. Similar results were obtained from a small pediatric case-control study where CMV positivity was not statistically associated with an increased risk of colectomy at 12 months (p = 0.429) [44].
3. Methods for Diagnosis of CMV Infection
The diagnostic challenge in this complex clinical picture is to distinguish CMV colitis from IBD exacerbations, as both conditions can present with similar clinical features. Serology, histology, and PCR for CMV DNA in the blood, stool or intestinal tissue are the techniques that can be used to identify intestinal CMV infection.
3.1. Serology
Serological diagnosis of CMV infection relies on detecting specific antibodies the host produces in response to the virus. IgM serology has a sensitivity of between 15 and 60% in detecting CMV in a 2004 study of a cohort of 64 IBD patients, including 10 with CMV infection [24]. Enzyme-Linked Immunosorbent Assay (ELISA) is the most common serological method used to detect CMV antibodies. In ELISA, viral antigens are immobilized on a solid phase, and patient serum is applied. If specific anti-CMV antibodies are present, they bind to the antigens. Subsequent enzymatic reactions generate a color change, which is quantified to determine the antibody levels [45].
Another essential serological technique is the Immunofluorescence Assay (IFA), which uses fluorescent antibodies to detect CMV-specific immunoglobulins in patient samples [46]. This method is beneficial for confirming positive ELISA results and distinguishing between IgM and IgG antibodies.
Blood serology for CMV has limited diagnostic value for CMV colitis due to the high adult seroprevalence of the virus, as previously mentioned [47].
Therefore, serology has limited utility in diagnosing CMV reactivation in individuals with IBD, only allowing doctors to rule out CMV infection in patients who are negative for anti-CMV antibodies [48].
3.2. Mucosal Biopsies: Immunohistochemistry and PCR
Histological examination of colonic mucosa biopsies is a critical tool for diagnosing CMV infection in IBD patients. Histological assessment of CMV infection in colonic mucosa biopsies involves the examination of tissue samples obtained via endoscopy or surgical procedures [49]. Quality colonoscopy is essential for the diagnostic algorithm of patients with suspected CMV infection, and it must be performed under conditions of adequate bowel preparation. This can be achieved either using oral solutions or using enemas, especially in cases of severe acute ulcerative colitis where rectoscopy allows us to perform sampling for CMV search and rapid endoscopic Mayo score evaluation [50]. The characteristic features of CMV infection in these samples include cytomegalic cells, intranuclear inclusions, and characteristic nuclear and cytoplasmic inclusions [49].
Cytomegalic cells are enlarged cells with characteristic nuclear and cytoplasmic changes. These cells often have large, basophilic intranuclear inclusions indicative of CMV infection. In the cytoplasm, there may be granular or eosinophilic inclusions. The presence of these cytomegalic cells in colonic mucosa biopsies is highly suggestive of CMV infection [51].
Several staining methods can be used to confirm the diagnosis. H&E staining is a standard histological method highlighting the characteristic cellular changes [52]. However, IHC can be even more specific, using antibodies against CMV antigens to identify the virus within infected cells. High specificity [92–100%] can be achieved with H&E staining, while the sensitivity ranges from 10% to 87% [53].
In 2013, Mills et al. showed that CMV-PCR on formalin-fixed, paraffin-embedded (FFPE) tissue gastrointestinal biopsies complements IHC [54]. In fact, in a total of 102 FFPE gastrointestinal biopsy specimens from 74 patients, CMV DNA was detected via PCR in 90.9% of IHC-positive and 14.5% of IHC-negative tissues. Meanwhile, Kandiel et al. have demonstrated that staining the colonic CMV histology with a particular IHC that is specific to one of the immediate early antigens increases the diagnostic sensitivity [78–93%] and specificity (92–100%) of the examination [27].
Kim et al. identified active gastrointestinal (GI) CMV illness, defined as histological detection of intranuclear inclusion bodies or positive IHC and clinical improvement on ganciclovir treatment, using both interferon γ-releasing assays [IGRA] for CMV and CMV PCR. For predicting gastrointestinal CMV illness, the sensitivity and specificity of the CMV replication in biopsy tissue (positive IHC staining) and low CMV IGRA results were 92% (95% CI = 62–100) and 100% (95% CI = 74–100), respectively [15].
Either way, PCR on GI biopsy tissue is the diagnostic method recommended by the European Crohn’s and Colitis Organization (ECCO) for diagnosing CMV colitis in IBD patients [55].
Real-time PCR increases the sensitivity to identify CMV in FFPE tissue of GI biopsies, as demonstrated by McCoy et al. [47]. In their study, qPCR analysis showed positive results in 88 out of the 91 CMV-positive samples that were histologically confirmed, obtaining a sensitivity of 96.7%. In addition, 78 out of the 79 negative controls tested negative via qPCR, yielding a specificity of 98.7%.
Furthermore, in a study published in 2015, Zidar et al. compared immunohistochemistry and qPCR in resected bowel samples from 12 IBD patients [56]. Tissue samples were obtained from different sites of the resected colonic samples. The highest densities of CMV-positive cells were found in samples from the base of ulcers or the edge of ulcers, regardless of the test used and underling the fact that the number of sampled biopsies and/or the number of investigated levels is more important than the choice of diagnostic method [56].
Distinguishing CMV infection from other inflammatory changes in IBD is crucial. Patients with IBD often exhibit histological signs of inflammation in the colon, such as increased numbers of inflammatory cells, architectural distortion, and crypt abscesses. Therefore, these inflammatory changes in colonic mucosa biopsies must be carefully evaluated in the context of CMV diagnosis. A comprehensive assessment should consider the overall clinical presentation and the results of other diagnostic tests, such as PCR-based assays for CMV DNA in blood or tissue.
3.3. Serum and Fecal PCR
PCR-based assays can also detect CMV DNA in blood or other body fluids, providing direct evidence of active viral replication. This approach is highly sensitive and is often used with serological tests for a comprehensive diagnosis.
A prospective study was conducted in 2023 on 117 patients with clinical suspicion of CMV colitis. Compared to colonoscopy and histology, plasma CMV-PCR had a 94.7% specificity and a 66.7% sensitivity [57].
However, according to the ECCO statement regarding IBD patients, this high sensitivity of the PCR assay may lead to inadequate specificity when diagnosing an active CMV infection since it may be able to identify tiny amounts of CMV that are not harmful to the colonic mucosa or the latent form of the virus [58]. To get around this drawback, PCR primers that identify CMV in its reactivated state, but not in its latent form, must be chosen.
A pilot study conducted in 2010 investigated the use of stool PCR in 21 patients with IBD flare-ups unresponsive to steroids. It demonstrated that in comparison to PCR-based CMV detection in mucosal biopsies, the sensitivity, specificity, and accuracy of the stool test for CMV DNA detection were 83, 93, and 90%, respectively [59].
Ganzenmueller et al. examined 66 patients’ lower intestinal tract biopsies and fecal samples using quantitative CMV PCR. They showed that stool PCR had a good specificity of 96% but a poor sensitivity (67%) for diagnosing CMV intestinal disease [60].
This study highlights how fecal PCR analysis can be a useful diagnostic tool for CMV intestinal disease by avoiding an endoscopic examination for a positive result, even though it does not help rule out CMV infection in case of a negative result [60]. In contrast, a more recent study in 2020 that included patients with ulcerative colitis revealed that the stool-CMV PCR had a sensitivity of 84.7% and a specificity of 71.4% [10].
In conclusion, more studies regarding PCR on stool still need to be conducted to determine the true place of this test in the diagnostic algorithm of CMV-related colitis.
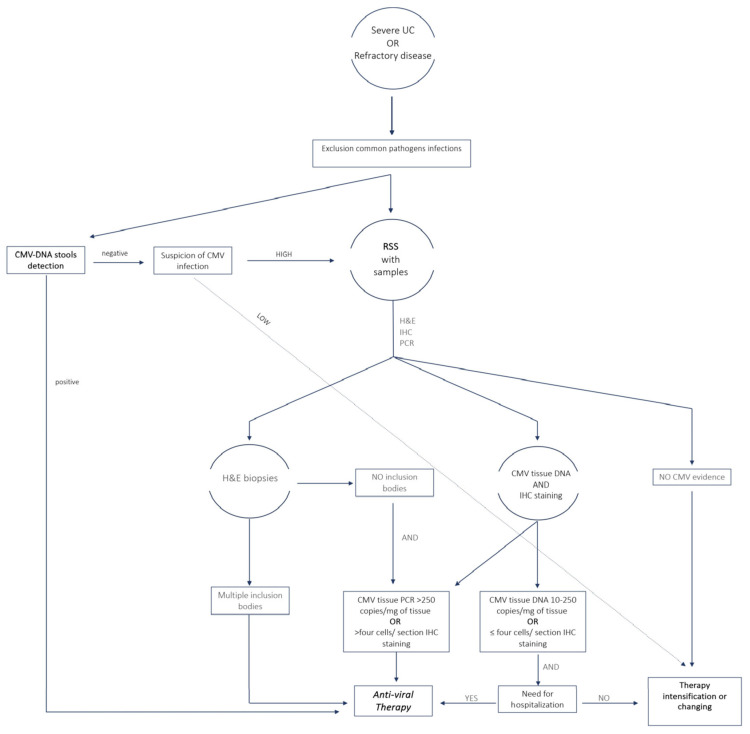
The sensitivity, specificity and strengths of the main diagnostic methods are shown in Table 1. In Figure 1 we propose an algorithm that from the diagnosis can direct physicians in selecting patients for treatment.
Table 1.
Sensitivity, specificity and accuracy of diagnostic methods.
| Test | Sens | Spec | Pro |
|---|---|---|---|
| Serology | 15–60% | 96–99% | Easily accessible, fast |
| Serum PCR | 66.7% | 94.7% | Easily accessible, fast |
| Histology w/IHC | 78–93% | 92–100% | Proves intestinal disease |
| Tissue PCR | 96.7% | 98.7% | Proves intestinal disease |
| Fecal PCR | 83–96% | 67–93% | Less invasive |
PCR, polymerase chain reaction; IHC, immune histochemistry.
Figure 1.
Algorithm for the diagnosis of CMV infection and selection of patients to treat for clinical practice. UC, ulcerative colitis; H&E, hematoxylin and eosin; IHC, immune histochemistry; PCR, polymerase chain reaction; RSS, rectosigmoidoscopy.
4. Treatment
4.1. When to Treat? Indications for Specific Antiviral Therapy
The development of CMV colitis is associated with an increased risk of poor outcomes, including toxic megacolon, colectomy, need for rescue therapy and increased rates of disease flares [38,41,61,62,63,64]. Therefore, it is crucial to maintain a high level of clinical suspicion of CMV infection/reactivation in UC patients presenting with a worsening of their gastrointestinal symptoms, regardless of their immunosuppression status. A delay in diagnosis and subsequent management may be associated with unfavorable outcomes, including increased colectomy rates.
Previous studies showed that in steroid-dependent or steroid-refractory UC patients, those receiving antiviral treatment experienced a significantly higher clinical remission rate at 12 months compared to those who did not receive such treatment [65].
It is interesting to note that conflicting findings about the risk of colectomy following antiviral therapy for CMV were found in two separate meta-analyses involving 176 and 333 UC patients with CMV, respectively [66,67]. Indeed, the first study found that patients who had received antiviral therapy had a higher risk of a 30-day colectomy [66]. In contrast, the second study found that antiviral therapy may be helpful concerning he colectomy risk in a subgroup of UC patients refractory to corticosteroids (OR, 0.20; 95% CI = 0.08–0.49) [67]. Furthermore, in these patients, the authors observed a lower rate of colectomy in those for whom the diagnosis was made using histological criteria (H&E and/or IHC) rather than with tissue PCR [67]. To some extent, the discordance of these results may derive from differences in the CMV burden and in the methods used to perform the diagnosis in each study.
Thus, antiviral therapy may be required by only a subset of IBD patients with CMV disease. However, to date, only limited information is available in the literature concerning the relationship between the tissue viral load, measured by viral inclusion in IHC [40,68] or CMV-DNA copies [32], and the UC outcome.
Jones A. et al. showed that patients with low-grade CMV colitis (<5 viral inclusions on IHC) were significantly more likely to undergo surgery than those with high-grade colitis (HR 2.13, 95% CI = 0.85–5.33). Interestingly, compared to patients with high-grade colitis who received treatment, patients with low-grade CMV colitis who did not receive anti-viral therapy had a nearly five-fold higher likelihood of undergoing surgery within a year (HR 4.81, 95% CI = 1.60–14.48). However, Nguyen et al. demonstrated that anti-viral treatment did not change the colectomy rates in UC patients with low-grade disease but did change the outcomes in those with high-grade disease (44% if treated and 83% if untreated) [69].
Similarly, Roblin et al. revealed that most patients with a higher colonic viral load (CMV DNA load above 250 copies/mg of tissue) responded to anti-viral therapy despite failing three consecutive lines of immunosuppressant therapy [32]. However, quantitative RT-PCR is only sometimes available in clinical settings; hence, clinicians often assess CMV DNA-positivity only qualitatively.
In a recent retrospective case-control study, Wang et al. showed that in UC patients with positive colonic CMV virocytes diagnosed via H&E and/or IHC, the anti-viral therapy significantly improved the surgery-free survival within 30 days, with a difference sustained for 70 months [70]. Okahura et al. demonstrated that patients with a high tissue viral load of CMV may respond to anti-viral treatment alone without additional therapy for UC, whereas patients with a low viral load (<5500 copies/μg DNA) might benefit from intensified UC therapy [25]. On the other side, a small study involving 20 patients suggested that the absence of endoscopically visible large ulcers (>5 mm) in patients with active UC and a positive CMV DNA via mucosal PCR assay are signs of a latent CMV infection, therefore not requiring an anti-viral therapy and likely to respond to conventional immunosuppressive therapy [71]. Conversely, patients with large ulcers poorly responded even when they were given the combined therapy [71].
Whether CMV reactivation exacerbates the progression of IBD is still unknown. However, in patients with low CMV burdens, the underlying IBD colitis is likely the primary cause of gut inflammation, and CMV is just “an innocent bystander”. On the other hand, in patients with high CMV burdens, the virus appears to be an active pathogen; in these cases, UC-induced inflammation may not have a principal impact on gut inflammation.
Hence, despite the lack of controlled trial data, there are sufficient pieces of evidence to support anti-viral therapy only in patients with steroid-dependent/refractory moderate-to-severe colitis and high-grade colonic CMV reactivation diagnosed via H&E staining with IHC and/or CMV tissue PCR (CMV DNA load above 250 copies/mg of tissue [32] or ≥five viral inclusions evident on IHC in each biopsy specimen) [40,68]. However, while some algorithms have been proposed [72,73], an exact threshold to determine which patients might benefit from anti-viral therapy is still to be defined.
Pillet and colleagues presented a treatment algorithm that categorized patients according to the density of CMV in colon samples: individuals with high-grade CMV density, individuals with low-grade CMV density, or individuals without CMV. Specifically, they stated that patients with high-grade CMV (defined as CMV tissue DNA > 250 copies/mg or >four inclusions on IHC) would require anti-viral and anti-TNF therapy; meanwhile, patients with low-grade CMV (CMV tissue DNA 10–250 copies/mg or ≤4 inclusions on IHC) would need only anti-viral therapy in case of severe disease (defined as large colic ulcers [>5 mm] at colonoscopy or need to hospitalization).
On the other hand, individuals lacking CMV would need to treat the underlying UC with a more intense immunosuppressive regime [72].
Recently, Mourad et al., in a comprehensive review, suggested the administration of anti-viral treatment in two circumstances: firstly, in patients with acute severe colitis and multiple inclusion bodies on colonic samples, regardless of the CMV tissue PCR or positive IHC strains; and secondly, in patients with negative inclusion bodies but high CMV tissue PCR (>250 copies/mg of tissue) or high IHC staining (>four cells/section) [28].
4.2. Comparison of Guidelines: IBD Guidelines vs. Infectious Disease Guidelines
The remission rate of UC patients after antiviral therapy for CMV colitis is high (67% to 100%) [17,19,74]. The preferred antiviral agent for treating CMV colitis is intravenous ganciclovir at 5–7.5 mg/kg twice daily for two weeks [53,75,76]. Due to the drug’s renal excretion, the dosage and frequency should be adjusted in patients with renal dysfunction [77], and strict monitoring of patients’ renal function and electrolytes during the treatment is recommended [78].
Prolonged intravenous antiviral therapy (2–3 weeks) usually requires hospitalization [79]. However, ganciclovir may be replaced with oral valganciclovir (1 g 3 times daily) in those treated as outpatients.
Despite low-quality evidence, the British Society guidelines recommend for hospitalized patients the intravenous administration of ganciclovir (5 mg/kg twice daily) while maintaining conventional therapy with corticosteroids or rescue medications with infliximab or cyclosporine [80].
The 2014 ECCO guidelines recommended the administration of intravenous ganciclovir (5 mg/kg twice daily) for 3–5 days. Depending on the clinical course and expert advice, switching to oral valganciclovir (900 mg twice daily) for the remaining 2–3 weeks could be considered [55].
More recently, however, the ECCO has extended the period of intravenous ganciclovir 5 mg/kg twice daily to 5–10 days, with the possibility of an earlier switch to oral therapy depending on clinical response [78].
Foscarnet, administrated intravenously (90 mg/kg) twice daily for 2–3 weeks, has been proposed as an alternative treatment in cases of resistance or intolerance (e.g., myelotoxicity) to ganciclovir. In case of severe adverse events, such as severe neutropenia and thrombocytopenia, consulting an infectious disease specialist is strongly recommended [55,78].
In rare cases of systemic CMV reactivation causing meningoencephalitis, pneumonitis, hepatitis, or esophagitis, all the guidelines recommend immediate discontinuation of the immunosuppressive agents and prompt treatment of the CMV infection with antivirals according to the indications of infectious disease specialists, since this regimen is associated with clinical improvement and decreased mortality [55,78,80]
4.3. Implications of Immunosuppressant and Advanced Therapies
Immunosuppressive conditions are known to frequently result in CMV infection or reactivation. In IBD, the use of immunosuppressants and treatment with biologics may result in an alteration in the immune system, thus favoring CMV reactivation. While the British Society guidelines recommend to continue conventional immunosuppressive therapy during antiviral therapy [80], the ECCO guidelines suggest considering the cessation of all immunomodulatory therapies, including steroids, until the CMV symptoms are controlled (evidence level 5, experts’ opinion) [55].
Several therapeutic schedules have been proposed for the treatment of steroid-dependent/resistant colitis with CMV reactivation, including a rapid steroid tapering and discontinuation [38,81,82].
On the other hand, previous studies suggested that any already initiated IBD treatment, including conventional steroid therapy, should be continued during antiviral therapy for CMV colitis, and medical rescue therapy should be prescribed when necessary [76,77]. Accordingly, a retrospective multicenter study involving 110 hospitalized patients with refractory UC, associated with CMV disease, demonstrated that administration of infliximab or cyclosporine together with ganciclovir did not cause a worse outcome (colectomy rate at 1, 3 and 12 months) compared with ganciclovir alone [83].
It has been demonstrated that thiopurines interfere with the function of natural killer cells and T lymphocytes specific to CMV. Shukla et al. recently conducted a meta-analysis that included 16 observational studies and found that exposure to thiopurines was associated with a higher risk of CMV reactivation (1273 patients, OR 1.56, 95% CI = 1.01–2.39) [84]. When the analysis was restricted to hospitalized patients, the thiopurine results remained consistent. In addition, there was no significant link between exposure to TNF-alpha antagonists and risk of CMV reactivation (OR 1.44, 95% CI = 0.93–2.24) [84].
Similarly, Pillet et al. try to assess the relationship between CMV colitis and UC therapy with anti-TNF-alpha (adalimumab or infliximab) or azathioprine (AZA) in 109 disease flare-ups (anti-TNF-alpha = 69 and AZA = 40) [21]. The percentage of CMV reactivation was similar in the two groups (35% vs. 38% in patients receiving anti-TNF and AZA, respectively). In a sub-analysis of patients who required optimization of the anti-TNF therapy, the clinical response (defined as partial Mayo score < 3) was not significantly different in patients exhibiting or not a detectable CMV DNA load in colonic tissue just before optimization (p = 0.52) [21]. Since the authors found no evidence of a reciprocal negative relationship between anti-TNF medications and CMV infection, their findings imply that these medications may be used to treat flare-ups brought on by CMV reactivation.
Accordingly, the study by Lavagna et al. showed that administration of infliximab in CMV-seropositive patients with refractory CD did not cause the reactivation of CMV, since no patient was positive on blood CMV PCR during the three sessions of infliximab therapy [7].
Treatment with anti-TNF alpha does not adversely affect the outcome of patients with CMV reactivation [21,85].
Moreover, previous studies suggested that by lowering the TNF-α levels and the macrophage differentiation in the colon tissue, anti-TNF agents inhibit CMV reactivation and reduce the incidence of CMV colitis, thereby being preferable to other immunosuppressant therapies used to treat CMV reactivation-associated flare-ups in UC patients [79].
Finally, in a multicenter retrospective study, the authors found no additional risk of colectomy in CMV-positive patients associated with exposure to infliximab (IFX) or cyclosporine [83].
Cyclosporine A (CyA) selectively suppresses T lymphocyte-mediated immune responses by altering the calcineurin–calmodulin interaction. A small Japanese study examines the effects of an ongoing CMV infection after treating steroid-refractory UC with Cya [86]. They included 23 patients treated with intravenous CyA. None of the patients had an active CMV infection prior to receiving CyA treatment. Out of the 23 UC patients treated with CyA, 18 developed a CMV infection. Following CyA treatment, the CMV infection started to manifest, on average, 8.5 days later (range: 4–20 days). Uncontrolled, severe, deteriorating colitis necessitated surgical treatment in 15 out of the 18 patients (83.3%) with CMV infection. Of the 18 patients with CMV infection, 15 (83.3%) required surgery due to severe and rapidly worsening colitis.
Vedolizumab is an anti-α4β7 integrinmonoclonal antibody that inhibits leucocyte trafficking in the gut. Typically, it has very limited systemic effects [87].
Even though several works have reported the safety of vedolizumab and focused on its risk of infection [88], a recent case report described a case of CMV colitis in a patient undergoing monotherapy with the anti-integrin, indicating that it might be a risk factor for UC CMV colitis. In addition, vedolizumab may even be useful in treating CMV colitis as showed in two case reports [89].
The available data on the other advanced therapies are still scarce.
Only two cases of CMV colitis in patients receiving ustekinumab as maintenance were reported in the UNIFI study [90]. To the best of our knowledge, the OCTAVE Induction 2 study contains the only information on small molecules. In this study, a single patient receiving tofacitinib 10 mg twice daily developed CMV colitis [91].
Actually, despite the theoretical risk of worsening the outcome of CMV colitis, immunosuppressants are maintained in most of the cases for the control of disease activity [1,20,38,43,62,81,83,92,93,94,95,96] since, especially in patients with low viral loads and a low number of IHC-positive cells in the colon, CMV clearance may be parallel to the achievement of remission induced by immunosuppressants, even in patients who did not receive antivirals [93].
Therefore, the correct therapeutic schedule for corticosteroid and immunosuppressive agents during CMV reactivation in refractory IBD is still to be determined. Additional studies are required to explore the effects of immunomodulators in the treatment of IBD complicated by CMV colitis.
Most evidence suggests direct rectosigmoidoscopy with biopsy in patients at high risk of CMV. However, considering the non-invasiveness, relatively low cost and diagnostic accuracy, a suggested alternative approach, particularly for outpatients, might be first to determine the presence of CMV-DNA in the stools and to only perform RSS in negative patients with a high suspicion of CMV infection. There is a no universally accepted cut-off for defining PCR positivity in stools.
Further studies are needed to confirm the diagnostic accuracy and to define the correct cut-off and the cost-effectiveness of this strategy in a clinical setting.
See the text for more details.
5. Conclusions
CMV colitis could have a major impact on the IBD course, particularly during UC flares. Even if its role in reducing the clinical response during steroid therapy is well established, practical approaches to the infection largely vary in clinical practice due to the different implemented diagnostic methods, with consequent variable diagnostic accuracy and different thresholds for treatment reported in the literature. Furthermore, the role of CMV colitis as a possible determinant of a lack of response to new biological drugs and small molecules has not been systematically investigated in the literature, thus it could be largely underestimated. Further studies are required to investigate the potential role of CMV during new advanced therapies and its optimal management in this setting to improve response to therapy.
Acknowledgments
The authors thank Fondazione Roma.
Author Contributions
Conceptualization, R.M., S.V., M.A.Z. and L.L.; methodology, R.M., S.V., F.D.V. and L.L.; validation, M.E.A., A.P., F.S., A.G. and M.C.G.; writing—original draft preparation, R.M., S.V. and F.D.V.; writing—review and editing, R.M., S.V., F.D.V., I.M., M.A.Z. and L.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Landolfo S., Gariglio M., Gribaudo G., Lembo D. The Human Cytomegalovirus. Pharmacol. Ther. 2003;98:269–297. doi: 10.1016/S0163-7258(03)00034-2. [DOI] [PubMed] [Google Scholar]
- 2.Antretter H., Höfer D., Hangler H., Larcher C., Pölzl G., Hörmann C., Margreiter J., Margreiter R., Laufer G., Bonatti H. Is It Possible to Reduce CMV-Infections after Heart Transplantation with a Three-Month Antiviral Prophylaxis? 7 Years Experience with Ganciclovir. Wien. Klin. Wochenschr. 2004;116:542–551. doi: 10.1007/BF03217708. [DOI] [PubMed] [Google Scholar]
- 3.Krech U. Complement-Fixing Antibodies against Cytomegalovirus in Different Parts of the World. Bull. World Health Organ. 1973;49:103. [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis Bate S., Dollard S.C., Cannon M.J. Cytomegalovirus Seroprevalence in the United States: The National Health and Nutrition Examination Surveys, 1988-2004. Clin. Infect. Dis. 2010;50:1439–1447. doi: 10.1086/652438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klemola E., Kääriäinen L. Cytomegalovirus as a Possible Cause of a Disease Resembling Infectious Mononucleosis. Br. Med. J. 1965;2:1099–1102. doi: 10.1136/bmj.2.5470.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lv Y.L., Han F.F., Jia Y.J., Wan Z.R., Gong L.L., Liu H., Liu L.H. Is Cytomegalovirus Infection Related to Inflammatory Bowel Disease, Especially Steroid-Resistant Inflammatory Bowel Disease? A Meta-Analysis. Infect. Drug Resist. 2017;10:511–519. doi: 10.2147/IDR.S149784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lavagna A., Bergallo M., Daperno M., Sostegni R., Costa C., Leto R., Crocellà L., Molinaro G., Rocca R., Cavallo R., et al. Infliximab and the Risk of Latent Viruses Reactivation in Active Crohn’s Disease. Inflamm. Bowel Dis. 2007;13:896–902. doi: 10.1002/ibd.20131. [DOI] [PubMed] [Google Scholar]
- 8.Matsuoka K., Iwao Y., Mori T., Sakuraba A., Yajima T., Hisamatsu T., Okamoto S., Morohoshi Y., Izumiya M., Ichikawa H., et al. Cytomegalovirus Is Frequently Reactivated and Disappears without Antiviral Agents in Ulcerative Colitis Patients. Am. J. Gastroenterol. 2007;102:331–337. doi: 10.1111/j.1572-0241.2006.00989.x. [DOI] [PubMed] [Google Scholar]
- 9.Nakase H., Chiba T. TNF-Alpha Is an Important Pathogenic Factor Contributing to Reactivation of Cytomegalovirus in Inflamed Mucosa of Colon in Patients with Ulcerative Colitis: Lesson from Clinical Experience. Inflamm. Bowel Dis. 2010;16:550–551. doi: 10.1002/ibd.21047. [DOI] [PubMed] [Google Scholar]
- 10.Magdziak A., Szlak J., Mróz A., Wieszczy P., Zagórowicz E. A Stool Test in Patients with Active Ulcerative Colitis Helps Exclude Cytomegalovirus Disease. Scand. J. Gastroenterol. 2020;55:664–670. doi: 10.1080/00365521.2020.1771760. [DOI] [PubMed] [Google Scholar]
- 11.Powell R.D., Warner N.E., Levine R.S., Kirsner J.B. Cytomegalic Inclusion Disease and Ulcerative Colitis; Report of a Case in a Young Adult. Am. J. Med. 1961;30:334–340. doi: 10.1016/0002-9343(61)90105-X. [DOI] [PubMed] [Google Scholar]
- 12.Dimitroulia E., Spanakis N., Konstantinidou A.E., Legakis N.J., Tsakris A. Frequent Detection of Cytomegalovirus in the Intestine of Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2006;12:879–884. doi: 10.1097/01.mib.0000231576.11678.57. [DOI] [PubMed] [Google Scholar]
- 13.Garrido E., Carrera E., Manzano R., Lopez-Sanroman A. Clinical Significance of Cytomegalovirus Infection in Patients with Inflammatory Bowel Disease. World J. Gastroenterol. 2013;19:17–25. doi: 10.3748/wjg.v19.i1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Domènech E., Vega R., Ojanguren I., Hernández Á., Garcia-Planella E., Bernal I., Rosinach M., Boix J., Cabré E., Gassull M.A. Cytomegalovirus Infection in Ulcerative Colitis: A Prospective, Comparative Study on Prevalence and Diagnostic Strategy. Inflamm. Bowel Dis. 2008;14:1373–1379. doi: 10.1002/ibd.20498. [DOI] [PubMed] [Google Scholar]
- 15.Kim S.H., Lee H.S., Lee H.J., Kim S.M., Shin S., Park S.H., Kim K.J., Kim Y.H., Sung H., Lee S.O., et al. Clinical Applications of Interferon-γ Releasing Assays for Cytomegalovirus to Differentiate Cytomegalovirus Disease from Bystander Activation: A Pilot Proof-of-Concept Study. Korean J. Intern. Med. 2017;32:900. doi: 10.3904/kjim.2015.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim J.J., Simpson N., Klipfel N., Debose R., Barr N., Laine L. Cytomegalovirus Infection in Patients with Active Inflammatory Bowel Disease. Dig. Dis. Sci. 2010;55:1059–1065. doi: 10.1007/s10620-010-1126-4. [DOI] [PubMed] [Google Scholar]
- 17.Criscuoli V., Casà A., Orlando A., Pecoraro G., Oliva L., Traina M., Rizzo A., Cottone M. Severe Acute Colitis Associated with CMV: A Prevalence Study. Dig. Liver Dis. 2004;36:818–820. doi: 10.1016/j.dld.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Yoshino T., Nakase H., Ueno S., Uza N., Inoue S., Mikami S., Matsuura M., Ohmori K., Sakurai T., Nagayama S., et al. Usefulness of Quantitative Real-Time PCR Assay for Early Detection of Cytomegalovirus Infection in Patients with Ulcerative Colitis Refractory to Immunosuppressive Therapies. Inflamm. Bowel Dis. 2007;13:1516–1521. doi: 10.1002/ibd.20253. [DOI] [PubMed] [Google Scholar]
- 19.Cottone M., Pietrosi G., Martorana G., Casa A., Pecoraro G., Oliva L., Orlando A., Rosselli M., Rizzo A., Pagliaro L. Prevalence of Cytomegalovirus Infection in Severe Refractory Ulcerative and Crohn’s Colitis. Am. J. Gastroenterol. 2001;96:773–775. doi: 10.1111/j.1572-0241.2001.03620.x. [DOI] [PubMed] [Google Scholar]
- 20.Bontà J., Zeitz J., Frei P., Biedermann L., Sulz M.C., Vavricka S.R., Scharl S., Fried M., Rogler G., Scharl M. Cytomegalovirus Disease in Inflammatory Bowel Disease: Epidemiology and Disease Characteristics in a Large Single-Centre Experience. Eur. J. Gastroenterol. Hepatol. 2016;28:1329–1334. doi: 10.1097/MEG.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 21.Pillet S., Jarlot C., Courault M., Del Tedesco E., Chardon R., Saint-Sardos P., Presles E., Phelip J.M., Berthelot P., Pozzetto B., et al. Infliximab Does Not Worsen Outcomes During Flare-Ups Associated with Cytomegalovirus Infection in Patients with Ulcerative Colitis. Inflamm. Bowel Dis. 2015;21:1580–1586. doi: 10.1097/MIB.0000000000000412. [DOI] [PubMed] [Google Scholar]
- 22.D’Ovidio V., Vernia P., Gentile G., Capobianchi A., Marcheggiano A., Viscido A., Martino P., Caprilli R. Cytomegalovirus Infection in Inflammatory Bowel Disease Patients Undergoing Anti-TNFalpha Therapy. J. Clin. Virol. 2008;43:180–183. doi: 10.1016/j.jcv.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Gauss A., Rosenstiel S., Schnitzler P., Hinz U., Rehlen T., Kadmon M., Ehehalt R., Stremmel W., Zawierucha A. Intestinal Cytomegalovirus Infection in Patients Hospitalized for Exacerbation of Inflammatory Bowel Disease: A 10-Year Tertiary Referral Center Experience. Eur. J. Gastroenterol. Hepatol. 2015;27:712–720. doi: 10.1097/MEG.0000000000000361. [DOI] [PubMed] [Google Scholar]
- 24.Kishore J., Ghoshal U., Ghoshal U.C., Krishnani N., Kumar S., Singh M., Ayyagari A. Infection with Cytomegalovirus in Patients with Inflammatory Bowel Disease: Prevalence, Clinical Significance and Outcome. J. Med. Microbiol. 2004;53:1155–1160. doi: 10.1099/jmm.0.45629-0. [DOI] [PubMed] [Google Scholar]
- 25.Okahara K., Nagata N., Shimada T., Joya A., Hayashida T., Gatanaga H., Oka S., Sakurai T., Uemura N., Akiyama J. Colonic Cytomegalovirus Detection by Mucosal PCR and Antiviral Therapy in Ulcerative Colitis. PLoS ONE. 2017;12:e0183951. doi: 10.1371/journal.pone.0183951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gilmore R.B., Taylor K.M., Morrissey C.O., Gardiner B.J. Cytomegalovirus in Inflammatory Bowel Disease: A Clinical Approach. Intern. Med. J. 2022;52:365–368. doi: 10.1111/imj.15085. [DOI] [PubMed] [Google Scholar]
- 27.Kandiel A., Lashner B. Cytomegalovirus Colitis Complicating Inflammatory Bowel Disease. Am. J. Gastroenterol. 2006;101:2857–2865. doi: 10.1111/j.1572-0241.2006.00869.x. [DOI] [PubMed] [Google Scholar]
- 28.Mourad F.H., Hashash J.G., Kariyawasam V.C., Leong R.W. Ulcerative Colitis and Cytomegalovirus Infection: From A to Z. J. Crohns Colitis. 2020;14:1162–1171. doi: 10.1093/ecco-jcc/jjaa036. [DOI] [PubMed] [Google Scholar]
- 29.Goodgame R.W. Gastrointestinal Cytomegalovirus Disease. Ann. Intern. Med. 1993;119:924–935. doi: 10.7326/0003-4819-119-9-199311010-00010. [DOI] [PubMed] [Google Scholar]
- 30.Rahbar A., Boström L., Lagerstedt U., Magnusson I., Södergerg-Naucler C., Sundqvist V.A. Evidence of Active Cytomegalovirus Infection and Increased Production of IL-6 in Tissue Specimens Obtained from Patients with Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2003;9:154–161. doi: 10.1097/00054725-200305000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Wada Y., Matsui T., Matake H., Sakurai T., Yamamoto J., Kikuchi Y., Yorioka M., Tsuda S., Yao T., Yao S., et al. Intractable Ulcerative Colitis Caused by Cytomegalovirus Infection: A Prospective Study on Prevalence, Diagnosis, and Treatment. Dis. Colon Rectum. 2003;46:S59–S65. doi: 10.1097/01.DCR.0000087486.21981.C6. [DOI] [PubMed] [Google Scholar]
- 32.Roblin X., Pillet S., Oussalah A., Berthelot P., Del Tedesco E., Phelip J.M., Chambonnière M.L., Garraud O., Peyrin-Biroulet L., Pozzetto B. Cytomegalovirus Load in Inflamed Intestinal Tissue Is Predictive of Resistance to Immunosuppressive Therapy in Ulcerative Colitis. Am. J. Gastroenterol. 2011;106:2001–2008. doi: 10.1038/ajg.2011.202. [DOI] [PubMed] [Google Scholar]
- 33.Suzuki H., Kato J., Kuriyama M., Hiraoka S., Kuwaki K., Yamamoto K. Specific Endoscopic Features of Ulcerative Colitis Complicated by Cytomegalovirus Infection. World J. Gastroenterol. WJG. 2010;16:1245. doi: 10.3748/wjg.v16.i10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang H., Zhou W., Lv H., Wu D., Feng Y., Shu H., Jin M., Hu L., Wang Q., Wu D., et al. The Association Between CMV Viremia or Endoscopic Features and Histopathological Characteristics of CMV Colitis in Patients with Underlying Ulcerative Colitis. Inflamm. Bowel Dis. 2017;23:814–821. doi: 10.1097/MIB.0000000000001095. [DOI] [PubMed] [Google Scholar]
- 35.Iida T., Ikeya K., Watanabe F., Abe J., Maruyama Y., Ohata A., Teruyuki S., Sugimoto K., Hanai H. Looking for Endoscopic Features of Cytomegalovirus Colitis: A Study of 187 Patients with Active Ulcerative Colitis, Positive and Negative for Cytomegalovirus. Inflamm. Bowel Dis. 2013;19:1156–1163. doi: 10.1097/MIB.0b013e31828075ce. [DOI] [PubMed] [Google Scholar]
- 36.Wu X.W., Wu L., Ji H.Z., Wang F.Y. Relationship Between Cytomegalovirus Infection and Steroid Resistance in Inflammatory Bowel Disease: A Meta-Analysis. Dig. Dis. Sci. 2015;60:3203. doi: 10.1007/s10620-015-3733-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu C.C., Ji S., Ding Y., Zhou L., Liu X., Li W. Cytomegalovirus Infection and Steroid-Refractory Inflammatory Bowel Disease: Possible Relationship from an Updated Meta-Analysis. Ir. J. Med. Sci. 2018;187:935–942. doi: 10.1007/s11845-018-1752-y. [DOI] [PubMed] [Google Scholar]
- 38.Cohen S., Martinez-Vinson C., Aloi M., Turner D., Assa A., De Ridder L., Wolters V.M., De Meij T., Alvisi P., Bronsky J., et al. Cytomegalovirus Infection in Pediatric Severe Ulcerative Colitis-A Multicenter Study from the Pediatric Inflammatory Bowel Disease Porto Group of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition. Pediatr. Infect. Dis. J. 2018;37:197–201. doi: 10.1097/INF.0000000000001724. [DOI] [PubMed] [Google Scholar]
- 39.Wang S., Dou Y., Yang H., Ni A., Zhang R., Qian J. Alteration of Glucocorticoid Receptors and Exacerbation of Inflammation during Lytic Cytomegalovirus Infection in THP-1 Cells. FEBS Open Bio. 2017;7:1924–1931. doi: 10.1002/2211-5463.12334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zagórowicz E., Bugajski M., Wieszczy P., Pietrzak A., Magdziak A., Mróz A. Cytomegalovirus Infection in Ulcerative Colitis Is Related to Severe Inflammation and a High Count of Cytomegalovirus-Positive Cells in Biopsy Is a Risk Factor for Colectomy. J. Crohns Colitis. 2016;10:1205–1211. doi: 10.1093/ecco-jcc/jjw071. [DOI] [PubMed] [Google Scholar]
- 41.Schenk W., Klugmann T., Borkenhagen A., Klecker C., Dietel P., Kirschner R., Schneider E., Bruns T., Stallmach A., Teich N. The Detection of the Cytomegalovirus DNA in the Colonic Mucosa of Patients with Ulcerative Colitis Is Associated with Increased Long-Term Risk of Proctocolectomy: Results from an Outpatient IBD Clinic. Int. J. Colorectal Dis. 2019;34:393–400. doi: 10.1007/s00384-018-3210-8. [DOI] [PubMed] [Google Scholar]
- 42.Thavamani A., Umapathi K.K., Sferra T.J., Sankararaman S. Cytomegalovirus Infection Is Associated With Adverse Outcomes Among Hospitalized Pediatric Patients with Inflammatory Bowel Disease. Gastroenterol. Res. 2023;16:1–8. doi: 10.14740/gr1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Delvincourt M., Lopez A., Pillet S., Bourrier A., Seksik P., Cosnes J., Carrat F., Gozlan J., Beaugerie L., Roblin X., et al. The Impact of Cytomegalovirus Reactivation and Its Treatment on the Course of Inflammatory Bowel Disease. Aliment. Pharmacol. Ther. 2014;39:712–720. doi: 10.1111/apt.12650. [DOI] [PubMed] [Google Scholar]
- 44.Temtem T., Whitworth J., Zhang J., Bagga B. Cytomegalovirus in Pediatric Inflammatory Bowel Disease Patients with Acute Severe Colitis. Clin. Res. Hepatol. Gastroenterol. 2021;45:101625. doi: 10.1016/j.clinre.2021.101625. [DOI] [PubMed] [Google Scholar]
- 45.Vainionpää R., Leinikki P. Encyclopedia of Virology. 3rd ed. Elsevier Ltd.; Amsterdam, The Netherlands: 2008. Diagnostic Techniques: Serological and Molecular Approaches; pp. 29–37. [DOI] [Google Scholar]
- 46.Hekker A.C., Brand-Saathof B., Vis J., Meijers R.C. Indirect Immunofluorescence Test for Detection of IgM Antibodies to Cytomegalovirus. J. Infect. Dis. 1979;140:596–600. doi: 10.1093/infdis/140.4.596. [DOI] [PubMed] [Google Scholar]
- 47.McCoy M.H., Post K., Sen J.D., Chang H.Y., Zhao Z., Fan R., Chen S., Leland D., Cheng L., Lin J. QPCR Increases Sensitivity to Detect Cytomegalovirus in Formalin-Fixed, Paraffin-Embedded Tissue of Gastrointestinal Biopsies. Hum. Pathol. 2014;45:48–53. doi: 10.1016/j.humpath.2013.07.040. [DOI] [PubMed] [Google Scholar]
- 48.De la Hoz R.E., Stephens G., Sherlock C. Diagnosis and Treatment Approaches to CMV Infections in Adult Patients. J. Clin. Virol. 2002;25:1–12. doi: 10.1016/S1386-6532(02)00091-4. [DOI] [PubMed] [Google Scholar]
- 49.Azer S.A., Limaiem F. Cytomegalovirus Colitis. StatPearls [Internet] StatPearls Publishing; Treasure Island, FL, USA: 2023. [PubMed] [Google Scholar]
- 50.Gravina A.G., Pellegrino R., Romeo M., Palladino G., Cipullo M., Iadanza G., Olivieri S., Zagaria G., De Gennaro N., Santonastaso A., et al. Quality of Bowel Preparation in Patients with Inflammatory Bowel Disease Undergoing Colonoscopy: What Factors to Consider? World J. Gastrointest. Endosc. 2023;15:133–145. doi: 10.4253/wjge.v15.i3.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu G.-D., Shintaku I., Chien K., Geller S. A Comparison of Routine Light Microscopy, Immunohistochemistry, and in Situ Hybridization for the Detection of Cytomegalovirus in Gastrointestinal Biopsies. Am. J. Gastroenterol. 1989;84:1517–1520. [PubMed] [Google Scholar]
- 52.Cornaggia M., Leutner M., Mescoli C., Sturniolo G.C., Gullotta R. Chronic Idiopathic Inflammatory Bowel Diseases: The Histology Report. Dig. Liver Dis. 2011;43((Suppl. S4)):S293–S303. doi: 10.1016/S1590-8658(11)60585-9. [DOI] [PubMed] [Google Scholar]
- 53.Lawlor G., Moss A.C. Cytomegalovirus in Inflammatory Bowel Disease: Pathogen or Innocent Bystander? Inflamm. Bowel Dis. 2010;16:1620–1627. doi: 10.1002/ibd.21275. [DOI] [PubMed] [Google Scholar]
- 54.Mills A.M., Guo F.P., Copland A.P., Pai R.K., Pinsky B.A. A Comparison of CMV Detection in Gastrointestinal Mucosal Biopsies Using Immunohistochemistry and PCR Performed on Formalin-Fixed, Paraffin-Embedded Tissue. Am. J. Surg. Pathol. 2013;37:995–1000. doi: 10.1097/PAS.0b013e31827fcc33. [DOI] [PubMed] [Google Scholar]
- 55.Rahier J.F., Magro F., Abreu C., Armuzzi A., Ben-Horin S., Chowers Y., Cottone M., de Ridder L., Doherty G., Ehehalt R., et al. Second European Evidence-Based Consensus on the Prevention, Diagnosis and Management of Opportunistic Infections in Inflammatory Bowel Disease. J. Crohns Colitis. 2014;8:443–468. doi: 10.1016/j.crohns.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 56.Zidar N., Ferkolj I., Tepeš K., Štabuc B., Kojc N., Uršič T., Petrovec M. Diagnosing Cytomegalovirus in Patients with Inflammatory Bowel Disease--by Immunohistochemistry or Polymerase Chain Reaction? Virchows Arch. 2015;466:533–539. doi: 10.1007/s00428-015-1741-8. [DOI] [PubMed] [Google Scholar]
- 57.Sattayalertyanyong O., Limsrivilai J., Phaophu P., Subdee N., Horthongkham N., Pongpaibul A., Angkathunyakul N., Chayakulkeeree M., Pausawasdi N., Charatcharoenwitthaya P. Performance of Cytomegalovirus Real-Time Polymerase Chain Reaction Assays of Fecal and Plasma Specimens for Diagnosing Cytomegalovirus Colitis. Clin. Transl. Gastroenterol. 2023;14:e00574. doi: 10.14309/ctg.0000000000000574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nakase H., Matsumura K., Yoshino T., Chiba T. Systematic Review: Cytomegalovirus Infection in Inflammatory Bowel Disease. J. Gastroenterol. 2008;43:735–740. doi: 10.1007/s00535-008-2246-x. [DOI] [PubMed] [Google Scholar]
- 59.Herfarth H.H., Long M.D., Rubinas T.C., Sandridge M., Miller M.B. Evaluation of a Non-Invasive Method to Detect Cytomegalovirus (CMV)-DNA in Stool Samples of Patients with Inflammatory Bowel Disease (IBD): A Pilot Study. Dig. Dis. Sci. 2010;55:1053–1058. doi: 10.1007/s10620-010-1146-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ganzenmueller T., Kluba J., Becker J.U., Bachmann O., Heim A. Detection of Cytomegalovirus (CMV) by Real-Time PCR in Fecal Samples for the Non-Invasive Diagnosis of CMV Intestinal Disease. J. Clin. Virol. 2014;61:517–522. doi: 10.1016/j.jcv.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 61.Kim Y.S., Kim Y.H., Kim J.S., Jeong S.Y., Park S.J., Hee Cheon J., Ye B.D., Jung S.A., Park Y.S., Choi C.H., et al. Long-Term Outcomes of Cytomegalovirus Reactivation in Patients with Moderate to Severe Ulcerative Colitis: A Multicenter Study. Gut Liver. 2014;8:643–647. doi: 10.5009/gnl13427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee H.S., Park S.H., Kim S.H., Kim J., Choi J., Lee H.J., Kim W.S., Lee J.M., Kwak M.S., Hwang S.W., et al. Risk Factors and Clinical Outcomes Associated with Cytomegalovirus Colitis in Patients with Acute Severe Ulcerative Colitis. Inflamm. Bowel Dis. 2016;22:912–918. doi: 10.1097/MIB.0000000000000675. [DOI] [PubMed] [Google Scholar]
- 63.Criscuoli V., Rizzuto M.R., Gallo E., Orlando A., Cottone M. Toxic Megacolon and Human Cytomegalovirus in a Series of Severe Ulcerative Colitis Patients. J. Clin. Virol. 2015;66:103–106. doi: 10.1016/j.jcv.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 64.Matsumoto S., Yoshida Y. What Are the Factors That Affect Hospitalization and Surgery for Aggravation of Ulcerative Colitis? Eur. J. Gastroenterol. Hepatol. 2014;26:282–287. doi: 10.1097/MEG.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 65.Maconi G., Lombardini M., Furfaro F., Bezzio C., Zerbi P., Ardizzone S. Long-Term Outcome of Inflammatory Bowel Diseases with Cytomegalovirus Colitis: Effect of Antiviral Treatment. Eur. J. Gastroenterol. Hepatol. 2014;26:1146–1151. doi: 10.1097/MEG.0000000000000175. [DOI] [PubMed] [Google Scholar]
- 66.Kopylov U., Eliakim-Raz N., Szilagy A., Seidman E., Ben-Horin S., Katz L. Antiviral Therapy in Cytomegalovirus-Positive Ulcerative Colitis: A Systematic Review and Meta-Analysis. World J. Gastroenterol. 2014;20:2695–2703. doi: 10.3748/wjg.v20.i10.2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shukla T., Singh S., Loftus E.V., Bruining D.H., McCurdy J.D. Antiviral Therapy in Steroid-Refractory Ulcerative Colitis with Cytomegalovirus: Systematic Review and Meta-Analysis. Inflamm. Bowel Dis. 2015;21:2718–2725. doi: 10.1097/MIB.0000000000000489. [DOI] [PubMed] [Google Scholar]
- 68.Jones A., McCurdy J.D., Loftus E.V., Bruining D.H., Enders F.T., Killian J.M., Smyrk T.C. Effects of Antiviral Therapy for Patients with Inflammatory Bowel Disease and a Positive Intestinal Biopsy for Cytomegalovirus. Clin. Gastroenterol. Hepatol. 2015;13:949–955. doi: 10.1016/j.cgh.2014.09.042. [DOI] [PubMed] [Google Scholar]
- 69.Nguyen M., Bradford K., Zhang X., Shih D.Q. Cytomegalovirus Reactivation in Ulcerative Colitis Patients. Ulcers. 2011;2011:282507. doi: 10.1155/2011/282507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang Y., Aggarwal P., Liu X., Lu H., Lian L., Wu X., Guo S., Aggarwal N., Lashner B., Shen B. Antiviral Treatment for Colonic Cytomegalovirus Infection in Ulcerative Colitis Patients Significantly Improved Their Surgery Free Survival. J. Clin. Gastroenterol. 2018;52:e27–e31. doi: 10.1097/MCG.0000000000000759. [DOI] [PubMed] [Google Scholar]
- 71.Omiya M., Matsushita M., Tanaka T., Kawamata S., Okazaki K. The Absence of Large Ulcer Predicts Latent Cytomegalovirus Infection in Ulcerative Colitis with Positive Mucosal Viral Assay. Intern. Med. 2010;49:2277–2282. doi: 10.2169/internalmedicine.49.3657. [DOI] [PubMed] [Google Scholar]
- 72.Pillet S., Pozzetto B., Roblin X. Cytomegalovirus and Ulcerative Colitis: Place of Antiviral Therapy. World J. Gastroenterol. 2016;22:2030–2045. doi: 10.3748/wjg.v22.i6.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beswick L., Ye B., Van Langenberg D.R. Toward an Algorithm for the Diagnosis and Management of CMV in Patients with Colitis. Inflamm. Bowel Dis. 2016;22:2966–2976. doi: 10.1097/MIB.0000000000000958. [DOI] [PubMed] [Google Scholar]
- 74.Papadakis K.A., Tung J.K., Binder S.W., Kam L.Y., Abreu M.T., Targan S.R., Vasiliauskas E.A. Outcome of Cytomegalovirus Infections in Patients with Inflammatory Bowel Disease. Am. J. Gastroenterol. 2001;96:2137–2142. doi: 10.1111/j.1572-0241.2001.03949.x. [DOI] [PubMed] [Google Scholar]
- 75.Hommes D.W., Sterringa G., van Deventer S.J.H., Tytgat G.N.J., Weel J. The Pathogenicity of Cytomegalovirus in Inflammatory Bowel Disease: A Systematic Review and Evidence-Based Recommendations for Future Research. Inflamm. Bowel Dis. 2004;10:245–250. doi: 10.1097/00054725-200405000-00011. [DOI] [PubMed] [Google Scholar]
- 76.Sager K., Alam S., Bond A., Chinnappan L., Probert C.S. Review Article: Cytomegalovirus and Inflammatory Bowel Disease. Aliment. Pharmacol. Ther. 2015;41:725–733. doi: 10.1111/apt.13124. [DOI] [PubMed] [Google Scholar]
- 77.Landsman M.J., Sultan M., Stevens M., Charabaty A., Mattar M.C. Diagnosis and Management of Common Gastrointestinal Tract Infectious Diseases in Ulcerative Colitis and Crohn’s Disease Patients. Inflamm. Bowel Dis. 2014;20:2503–2510. doi: 10.1097/MIB.0000000000000140. [DOI] [PubMed] [Google Scholar]
- 78.Kucharzik T., Ellul P., Greuter T., Rahier J.F., Verstockt B., Abreu C., Albuquerque A., Allocca M., Esteve M., Farraye F.A., et al. ECCO Guidelines on the Prevention, Diagnosis, and Management of Infections in Inflammatory Bowel Disease. J. Crohns Colitis. 2021;15:879–913. doi: 10.1093/ecco-jcc/jjab052. [DOI] [PubMed] [Google Scholar]
- 79.Park S.C., Jeen Y.M., Jeen Y.T. Approach to Cytomegalovirus Infections in Patients with Ulcerative Colitis. Korean J. Intern. Med. 2017;32:383–392. doi: 10.3904/kjim.2017.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lamb C.A., Kennedy N.A., Raine T., Hendy P.A., Smith P.J., Limdi J.K., Hayee B., Lomer M.C.E., Parkes G.C., Selinger C., et al. British Society of Gastroenterology Consensus Guidelines on the Management of Inflammatory Bowel Disease in Adults. Gut. 2019;68:s1–s106. doi: 10.1136/gutjnl-2019-318484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Inokuchi T., Kato J., Hiraoka S., Suzuki H., Nakarai A., Hirakawa T., Akita M., Takahashi S., Harada K., Okada H., et al. Long-Term Follow-up of Ulcerative Colitis Patients Treated on the Basis of Their Cytomegalovirus Antigen Status. World J. Gastroenterol. WJG. 2014;20:509. doi: 10.3748/wjg.v20.i2.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ciccocioppo R. Letter: Cytomegalovirus Infection in Inflammatory Bowel Disease. Aliment. Pharmacol. Ther. 2015;42:127–129. doi: 10.1111/apt.13234. [DOI] [PubMed] [Google Scholar]
- 83.Kopylov U., Papamichael K., Katsanos K., Waterman M., Bar-Gil Shitrit A., Boysen T., Portela F., Peixoto A., Szilagyi A., Silva M., et al. Impact of Infliximab and Cyclosporine on the Risk of Colectomy in Hospitalized Patients with Ulcerative Colitis Complicated by Cytomegalovirus-A Multicenter Retrospective Study. Inflamm. Bowel Dis. 2017;23:1605–1613. doi: 10.1097/MIB.0000000000001160. [DOI] [PubMed] [Google Scholar]
- 84.Shukla T., Singh S., Tandon P., McCurdy J.D. Corticosteroids and Thiopurines, But Not Tumor Necrosis Factor Antagonists, Are Associated With Cytomegalovirus Reactivation in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. J. Clin. Gastroenterol. 2017;51:394–401. doi: 10.1097/MCG.0000000000000758. [DOI] [PubMed] [Google Scholar]
- 85.Tun G.S.Z., Raza M., Hale M.F., Lobo A.J. Polymerase Chain Reaction for Detection of Mucosal Cytomegalovirus Infection in Patients with Acute Ulcerative Colitis. Ann. Gastroenterol. 2019;32:81–87. doi: 10.20524/aog.2018.0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liu J., Farmer J.D., Lane W.S., Friedman J., Weissman I., Schreiber S.L. Calcineurin Is a Common Target of Cyclophilin-Cyclosporin A and FKBP-FK506 Complexes. Cell. 1991;66:807–815. doi: 10.1016/0092-8674(91)90124-H. [DOI] [PubMed] [Google Scholar]
- 87.Wyant T., Fedyk E., Abhyankar B. An Overview of the Mechanism of Action of the Monoclonal Antibody Vedolizumab. J. Crohns Colitis. 2016;10:1437–1444. doi: 10.1093/ecco-jcc/jjw092. [DOI] [PubMed] [Google Scholar]
- 88.Meserve J., Aniwan S., Koliani-Pace J.L., Shashi P., Weiss A., Faleck D., Winters A., Chablaney S., Kochhar G., Boland B.S., et al. Retrospective Analysis of Safety of Vedolizumab in Patients With Inflammatory Bowel Diseases. Clin. Gastroenterol. Hepatol. 2019;17:1533–1540.e2. doi: 10.1016/j.cgh.2018.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jentzer A., Veyrard P., Roblin X., Saint-Sardos P., Rochereau N., Paul S., Bourlet T., Pozzetto B., Pillet S. Cytomegalovirus and Inflammatory Bowel Diseases (IBD) with a Special Focus on the Link with Ulcerative Colitis (UC) Microorganisms. 2020;8:1078. doi: 10.3390/microorganisms8071078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sands B.E., Sandborn W.J., Panaccione R., O’Brien C.D., Zhang H., Johanns J., Adedokun O.J., Li K., Peyrin-Biroulet L., Van Assche G., et al. Ustekinumab as Induction and Maintenance Therapy for Ulcerative Colitis. N. Engl. J. Med. 2019;381:1201–1214. doi: 10.1056/NEJMoa1900750. [DOI] [PubMed] [Google Scholar]
- 91.Sandborn W.J., Su C., Sands B.E., D’Haens G.R., Vermeire S., Schreiber S., Danese S., Feagan B.G., Reinisch W., Niezychowski W., et al. Tofacitinib as Induction and Maintenance Therapy for Ulcerative Colitis. N. Engl. J. Med. 2017;376:1723–1736. doi: 10.1056/NEJMoa1606910. [DOI] [PubMed] [Google Scholar]
- 92.Ciccocioppo R., Racca F., Paolucci S., Campanini G., Pozzi L., Betti E., Riboni R., Vanoli A., Baldanti F., Corazza G.R. Human Cytomegalovirus and Epstein-Barr Virus Infection in Inflammatory Bowel Disease: Need for Mucosal Viral Load Measurement. World J. Gastroenterol. WJG. 2015;21:1915. doi: 10.3748/wjg.v21.i6.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Clos-Parals A., Rodríguez-Martínez P., Cañete F., Mañosa M., Ruiz-Cerulla A., Paúles M.J., Llaó J., Gordillo J., Fumagalli C., Garcia-Planella E., et al. Prognostic Value of the Burden of Cytomegalovirus Colonic Reactivation Evaluated by Immunohistochemical Staining in Patients with Active Ulcerative Colitis. J. Crohns Colitis. 2019;13:385–388. doi: 10.1093/ecco-jcc/jjy173. [DOI] [PubMed] [Google Scholar]
- 94.Do Carmo A.M., Santos F.M., Ortiz-Agostinho C.L., Nishitokukado I., Frota C.S., Gomes F.U., De Arruda Leite A.Z., Pannuti C.S., Boas L.S.V., Teixeira M.G., et al. Cytomegalovirus Infection in Inflammatory Bowel Disease Is Not Associated with Worsening of Intestinal Inflammatory Activity. PLoS ONE. 2014;9:e111574. doi: 10.1371/journal.pone.0111574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hirayama Y., Ando T., Hirooka Y., Watanabe O., Miyahara R., Nakamura M., Yamamura T., Goto H. Characteristic Endoscopic Findings and Risk Factors for Cytomegalovirus-Associated Colitis in Patients with Active Ulcerative Colitis. World J. Gastrointest. Endosc. 2016;8:301. doi: 10.4253/wjge.v8.i6.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Johnson J., Affolter K., Boynton K., Chen X., Valentine J., Peterson K. CMV Disease in IBD: Comparison of Diagnostic Tests and Correlation with Disease Outcome. Inflamm. Bowel Dis. 2018;24:1539–1546. doi: 10.1093/ibd/izy045. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.