Abstract
Introduction: Basal cardiovascular risk assessment in cardio-oncology is essential. Integrating clinical information, ECG and transthoracic echocardiogram can identify concealed inherited cardiomyopathies (ICMPs) with potential added risk of cardiotoxicity. We aimed to evaluate the impact of our Cardio-Oncology Unit design in detecting concealed ICMPs. Methods: We carried out a retrospective study of all consecutive breast cancer patients referred to the Cardio-Oncology Unit for cardiac evaluation (2020–2022). ICMPs diagnosis was provided according to ESC guidelines and underwent genetic testing. ICMPs prevalence in this cohort was compared to the highest and lowest frequency reported in the general population. Results: Among 591 breast cancer patients, we identified eight patients with ICMPs: one arrhythmogenic cardiomyopathy (ACM), three familial non-ischemic dilated cardiomyopathy (DCM), three hypertrophic cardiomyopathy (HCM) and one left ventricular non-compaction cardiomyopathy (LVNC), which has now been reclassified as non-dilated left ventricular cardiomyopathy. The number of ICMPs identified was within the expected range (neither overdiagnosed nor overlooked): ACM 0.0017 vs. 0.0002–0.001 (p 0.01–0.593); DCM 0.0051 vs. 0.002–0.0051 (p 0.094–0.676); HCM 0.005 vs. 0.0002–0.002 (p < 0.001–0.099); LVCN 0.0017 vs. 0.00014–0.013 (p 0.011–0.015). Genetic testing identified a pathogenic FLNC variant and two pathogenic TTN variants. Conclusion: Opportunistic screening of ICMPs during basal cardiovascular risk assessment can identify high-risk cancer patients who benefit from personalized medicine and enables extension of prevention strategies to all available relatives at concealed high cardiovascular risk.
Keywords: cardio-oncology, cardiomyopathy, genetics
1. Introduction
Over the past few decades, given encouraging improvement in cancer-related mortality [1], cardiovascular (CV) disease (CVD) and complications have become a major concern in cancer patients. Some very useful known cancer treatments, including anthracycline chemotherapy (AC) and anti-HER2 targeted therapies, have been associated with induced cardiomyopathy, left ventricular ejection fraction (LVEF) dysfunction and heart failure (HF) [2,3]. Apart from that, the number of cancer patients who already have pre-existing CVD or CV risk factors (CVRF) is also increasing. As a result, cancer treatments with potential CV toxicity require specific cardiac surveillance protocols. In this challenging scenario, cardio-oncology has emerged as a new discipline to improve the management of patients with both cancer and CVD [2,3,4,5].
Cardio-oncology multidisciplinary teams arise with the main goal of helping the management of cancer patients, planning their best possible cancer treatments while trying to safely minimize their CV complications [5]. In this regard, in 2022, the European Society of Cardiology (ESC) published the very first guidelines on cardio-oncology [3], a major breakthrough in the field. Accordantly, all cancer patients should undergo a baseline CV risk stratification before starting any potentially cardiotoxic anticancer therapy [2,4,5,6,7,8,9] (class I, level B [3]). This baseline evaluation should include, at least, personal history of pre-existing CVD or previous cardiotoxic cancer treatment and CVRF assessment (including smoking, diabetes mellitus (DM), hypertension (HTN) or dyslipidemia (DL), lifestyle, etc.) [5]. Moreover, basal electrocardiogram (ECG) is recommended (class I, level C) in all patients [3]. Further choice of additional CV tests should be individualized [3]. In this sense, cardiac imaging plays a central role in cardiotoxicity risk evaluation of many patients [10]. For instance, baseline transthoracic echocardiography (TTE) is recommended in all patients before anti-HER2 or AC (class I, level B) [5,11,12,13,14,15].
However, in the era of precision medicine, we believe that basal CV assessment should go beyond classical CVRF and LVEF evaluation [10]. In this regard, identifying inherited cardiomyopathies (ICMPs) in CV basal screening could be of utmost importance [16]. In fact, recent 2023 ESC guidelines encourage clinicians to use a ‘cardiomyopathy mindset’ to identify these patients with genetic cardiomyopathies at every clinical phase, from subclinical (or concealed) to overt and/or at end stage [17].
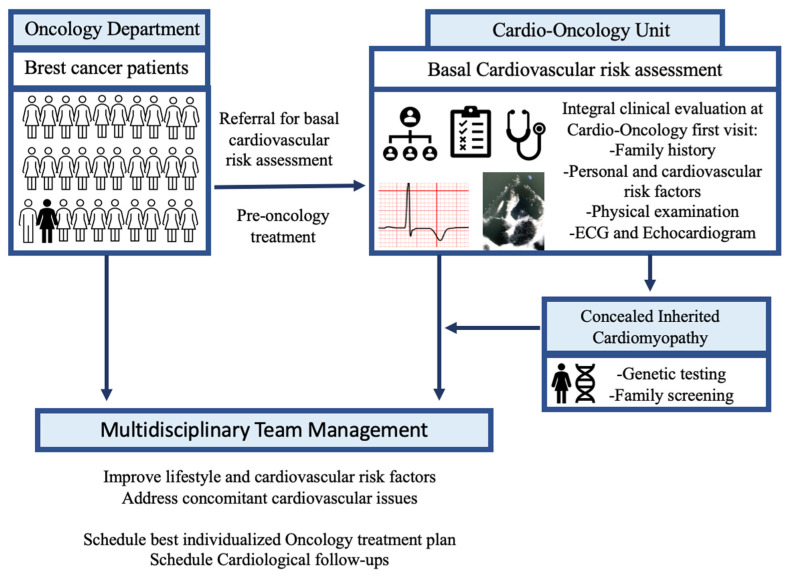
In this study, we aimed to evaluate the impact of integral CV assessment at our Cardio-Oncology Unit in detecting concealed ICMPs. Our Cardio-Oncology Unit was designed in the COVID-19 pandemic scenario to minimize hospital visits [18]. As a result, all cancer patients who needed basal TTE underwent on the same first visit an integral basal CV assessment including global clinical evaluation plus CV risk stratification, ECG and TTE [18].
2. Materials and Methods
2.1. Patients
In this retrospective study, we reviewed all consecutive breast cancer patients who were referred to the Cardio-Oncology Unit for cardiac evaluation during three consecutive years (2020–2022). The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee (CEImPA 2023.264).
Their first cardiological evaluation at the Cardio-Oncology Unit was performed by the same cardiologist, a specialist in cardio-oncology and ICMPs. Basal integral CV assessment at the Cardio-Oncology Unit included: (1) basal ECG; (2) history and physical examination: review of clinical history (both family and personal history, including planned and prior oncological treatment), anamnesis and physical examination; (3) TTE (Figure 1). All cardiological visits took place in the same clinical practice with the same electrocardiograph and echocardiogram (Philips—Affinity 50 Ultrasound System). This study was approved by the local Institutional Ethical Committee (CEImPA 2023.264).
Figure 1.
Clinical diagnostic workflow. All breast cancer patients are referred for basal cardiovascular risk assessment. Thanks to integral clinical evaluation at Cardio-Oncology Unit, patients with concealed inherited cardiomyopathies can be identified. All patients undergo multidisciplinary team management. ECG, electrocardiogram.
We identified those cancer patients with a new ICMPs final diagnosis at cardio-oncology evaluation (Figure 1): hypertrophic cardiomyopathy (HCM), familial non-ischemic dilated cardiomyopathy (DCM) or arrhythmogenic cardiomyopathy (ACM), according to ESC guidelines [6,19,20]. Borderline phenotypes, or those who presented alternative explaining conditions [6,17,19,20], were not included. Only patients previously labeled as left ventricular non-compaction cardiomyopathy (LVNC) who met current criteria for non-dilated left ventricular cardiomyopathy (NDLVC) were reclassified as NDLVC [17]. Although, for the purpose of this study, patients with arrhythmogenic cardiomyopathy are presented as so, some of the patients with “left ACM” would now be reclassified as NDLVC or DCM [17].
Cardiological follow-up, evaluation and treatment, including implantable cardioverter device (ICD) implantations, were also performed according to ESC guidelines [6,19,20]. Clinical data from ECG, TTE and cardiac magnetic resonance (CMR), when available, as well as medical treatment, gender, age, oncological treatment and CVRF, including HTN, smoking history, DM, DL and the presence of familial or personal history for premature CVD or sudden cardiac death (SCD), were collected.
2.2. Genetic Study and Variant Classification
Genetic testing was offered according to guidelines [6,19,21]. All patients who agreed to participate signed the informed consent for genetic testing (local Institutional Ethical Committee approval, CEImPA 2022.254). DNA was obtained from peripheral blood, and NGS analysis was performed, as reported elsewhere [22,23,24,25,26]. The NGS cardiovascular panel provided in our institution was designed with the aim of optimizing economic resources, attempting to be both time effective and cost effective. Therefore, our last version of the NGS cardiovascular panel [27] analyzes more than 200 genes and includes all minimum genes related to inherited cardiac conditions [6,19,21]. As a result, all patients with inherited cardiovascular conditions undergo the same NGS cardiovascular panel, irrespective of the cardiovascular phenotype. Complete information about the NGS cardiovascular panel can be consulted in Supplementary Table S1.
Interpretation of genetic variants with an allele frequency < 0.01 was based on the American College of Medical Genetics and Genomics (ACMG-AMP) 2015 Standards and Guidelines criteria [28]. Selected variants were evaluated by a cardiologist and a biologist specialized in inherited CV conditions. According to ACMG criteria, all variants were considered as pathogenic/likely pathogenic (P/LP), variants of uncertain significance (VUS) or benign/likely benign. All genetic rare variants identified in those genes with definitive or strong evidence for pathogenicity for each inherited cardiac condition were evaluated and classified according to ACM Criteria [28], initially regardless of the patient’s phenotype. Sanger sequencing of the corresponding PCR fragments was used to confirm the presence of VUS, LP and P variants. Afterwards, to achieve the final classification of VUS, LP and P variants, clinical data of all carriers were carefully reviewed before concluding with the final genetic report. Incidental or secondary findings (results that are not related to the indication for ordering the sequencing but that may nonetheless be of medical value or utility to the ordering physician and the patient) were reported according to ACMG recommendations. Finally, in this study, only P/LP variants associated with the cardiological phenotype are reported in the results section.
2.3. Statistical Analysis
Statistical analyses were performed with SPSS v.19. Descriptive data for continuous variables are presented as mean ± SD and as frequencies or percentages for categorical variables. ICMPs prevalence in this cohort was compared to the highest and lowest frequency reported in the general population. DCM has an estimated prevalence of 1 in 250–500; HCM ranges between 1 in 500 and 1 in 5000 and ACM between 1 in 1000 and 1 in 5000 persons [16,19]. Real prevalence of LVNC is unknown. Reported prevalence varies from 0.014 to 1.3% [29,30,31,32,33,34,35]. Differences frequencies were evaluated with the Chi-square test, and continuous variables were compared with the Student’s t-test. Differences were considered to be significant if the p value was below 0.05.
3. Results
From 2020 to 2022, 591 breast cancer patients were referred to the Cardio-Oncology Unit for cardiological evaluation. Seven patients had a prior history of LVEF deterioration under oncology treatment before 2020, and another two were referred with a severe reduced LVEF due to prior ischemic coronary artery disease.
Mean age at the first Cardio-Oncology visit was 57.5 (±12.9 SD), and most breast cancer patients were women (99.5%). General clinical characteristics of the cohort are shown in Table 1.
Table 1.
Clinical characteristics of breast cancer patients evaluated at the Cardio-Oncology Unit from 2020 to 2022.
| Breast Cancer Patients (n = 591) | |
|---|---|
| HER2 positive | 36.04% (213) |
| Cancer stage IV | 16.75% (99) |
| Family history of cardiovascular disease | |
| None | 94.25% (557) |
| Sudden death * | 1.52% (9) |
| Cardiomyopathies | 0.68% (4) |
| Premature coronary artery disease | 1.52% (9) |
| Others | 0.17% (1) |
| Second-degree relatives or at an older age | 1.69% (10) |
| Personal history of cardiovascular disease | |
| None | 93.57% (553) |
| Arrythmias | 2.54% (15) |
| Coronary artery disease | 1.86% (11) |
| Valvular heart diseases | 0.68% (4) |
| Prior cardiac dysfunction due to chemotherapy | 1.18% (7) |
| Cardiovascular risk factors | |
| Tabaco consumption | 47.04% (278) |
| Hypertension | 24.03% (142) |
| Diabetes | 7.78% (46) |
| Dyslipidemia | 25.55% (151) |
| Body mass index (kg/m2) | 27.4 (±6.1) |
| Mean of available echocardiogram parameters † |
Basal/Final |
| LVMWT (mm) | 1 ± 0.2/1 ± 0.2 |
| LVTDV (mL) | 46.7 ± 19.4/1 ± 0.2 |
| LVEF | 62 ± 6/61.45 ± 5.8 |
| E/A | 1 ± 0.6/1 ± 0.4 |
| E/e’ | 7.2 ± 2.75/7.2 ± 2.8 |
| GLS † | −20% ± 3.4/−20% ± 0.4 |
| % of patients with significant LVEF reduction in follow-up |
3.7% (22) 7.2% in HER2 positive vs. 1.3% in HER2 negative (p < 0.001) |
| TAPSE | 2.3 ± 0.5/2.23 ± 0.3 |
* Sudden death was considered positive in first-degree relatives and those < 60 years old, to include inherited cardiomyopathies and premature coronary artery disease. LVMWT: left ventricular maximum wall thickness; LVTDV: left ventricular tele-diastolic volume; LVEF: left ventricular ejection fraction (mm); † LVEF evaluation by 3D was unavailable and GLS only in some patients.
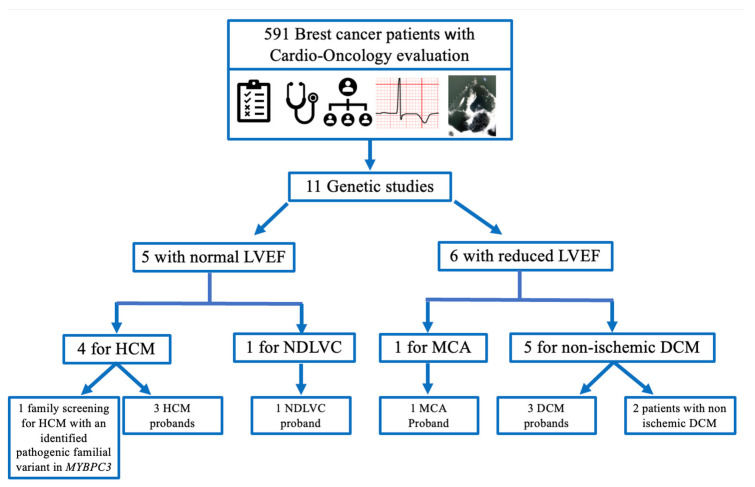
Based on cardio-oncology evaluation, genetic testing was indicated in 11 patients (Figure 2), 5 of them with normal LVEF. For instance, genetic screening was indicated in one patient due to family history of HCM. Sanger sequencing revealed that she was not carrier of the familial pathogenic MYBPC G263*. Four other patients were sequenced due to HCM diagnosis or NDLVC (with fibrosis and hypertrabeculation on CRM, previously classified as LVNC).
Figure 2.
Flowchart of breast cancer patients with genetic testing. Cardio-oncology evaluation (cardiovascular risk stratification including cardiotoxic cancer treatment, physical examination, family history of cardiovascular disease).
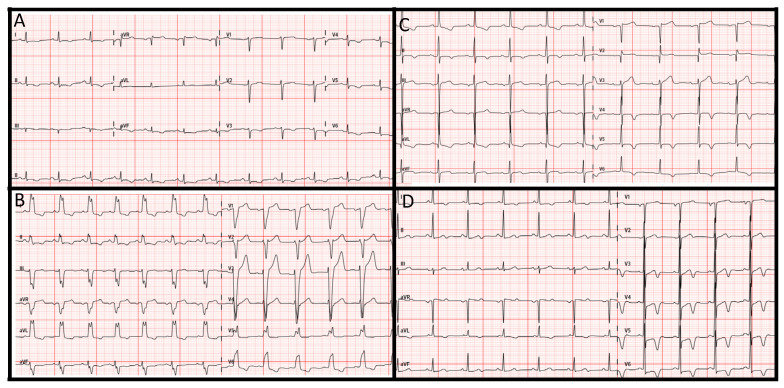
On the other hand, the other six patients who underwent genetic testing did present reduced LVEF. Clinical characteristics and genetic findings are shown in Table 2. Suspicion of ICMP was based on ECG findings (Figure 3) and family history, considering cardiotoxic cancer treatment. For instance, patient 1 was one of the seven patients with an LVEF deterioration under oncology treatment before 2020. When she was referred to the new Cardio-Oncology Unit in 2020, her last LVEF was 48%. Despite it was thought that the decrease in LVEF was secondary to anthracycline chemotherapy; her ECG with negative T waves at inferior leads, I and from v3 to v6, suggested otherwise (Figure 3A). CMR confirmed ICMP suspicion, and genetic testing revealed she was carrier of the pathogenic truncating variant in FLNC p.Tyr1042Ter, leading to the final diagnosis of left ACM (now it should also be reclassified as NDLVC). As none of her parents was carriers of the variant, it was considered de novo.
Table 2.
Clinical characteristics and genetic variants identified by NGS gene sequencing in the 8 patients with final definitive diagnosis of inherited cardiomyopathy.
| Patient | Cardiomyopathy | Genetic Results | Birth Date | ECG | LVEF |
|---|---|---|---|---|---|
| 1 | NDLVC (reclassified from ACM) | FLNC c.82060_82061del (p.Tyr1042Ter) | 11 May 1975 | Abnormal | 48% |
| 2 | DCM | TTN c.82060_82061del (p.Lys27354ValfsTer7) | 23 June 1962 | Abnormal | Fluctuant |
| 3 | DCM |
TTN c.28074 + 1G > T (IVS112 + 1G > T) |
13 May 1963 | Normal | 45% |
| 4 | DCM | Negative | 10 January 1963 | Abnormal | 35% |
| 5 | HCM | Negative | 20 September 1949 | Abnormal | >55% |
| 6 | HCM | Negative | 18 December 1956 | Abnormal | >55% |
| 7 | Apical HCM | Negative | 11 July 1948 | Abnormal | >55% |
| 8 | NDLVC (reclassified from LVNC) |
Negative | 10 May 1974 | Abnormal | >55% |
LVEF: left ventricular ejection fraction; DCM: familial dilated cardiomyopathy; HCM: hypertrophic cardiomyopathy; ACM: arrhythmogenic cardiomyopathy; NDLVC, non-dilated left ventricular cardiomyopathy; LVNC: left ventricular non-compaction cardiomyopathy.
Figure 3.
Electrocardiograms. (A) Patient 1 with arrhythmogenic cardiomyopathy; (B) patient 4 with dilated cardiomyopathy; (C) patient 6 with hypertrophic cardiomyopathy and apical aneurism; (D) patient 7 with apical hypertrophic cardiomyopathy.
At basal evaluation, only one patient (patient 4, Table 2) presented concealed DCM, with asymptomatic severely reduced LVEF and abnormal ECG (Figure 3B). From the 22 patients whose LVEF deteriorated during follow-up, only 5 patients (22.7%) were considered for genetic testing due clinical suspicion of ICMP. Genetic testing identified an underlying cause in three of these five cases (60%) (Table 2). In the absence of other supporting data, the two patients with ICMP suspicion but negative genetic results were not considered as conclusively having ICMP (only “non-ischemic” DCM), and, subsequently, are not presented as so in this study. However, further information about clinical family screening could provide more insights about their disease.
Thus, we performed a new diagnosis of ICMP in eight patients (one ACM, three DCM, three HCM and one NDLVC with hypertrabeculation) and could rule out one familial HCM. The number of ICMPs identified in the 591 consecutive breast cancer patients was a bit higher considering the lowest frequencies reported in a random population but within the expected range of the highest reported ones [16,19,29,30,31,32,33,34,35] (Table 3).
Table 3.
| Prevalence | Breast Cancer Cohort | General Population (Lowest) |
p Value | Breast Cancer Cohort | p Value |
|---|---|---|---|---|---|
| ACM | 0.0017 | 0.0002 | 0.010 * | 0.0017 | 0.593 |
| DCM | 0.0051 | 0.002 | 0.094 | 0.0051 | 0.676 |
| HCM | 0.005 | 0.0002 | <0.001 * | 0.005 | 0.099 |
| LVNC | 0.0017 | 0.00014 | 0.011 * | 0.0017 | 0.015 |
DCM: familial non-ischemic dilated cardiomyopathy; HCM: hypertrophic cardiomyopathy; ACM: arrhythmogenic cardiomyopathy; LVNC: left ventricular non-compaction cardiomyopathy. * p < 0.05.
SCD risk stratification was carefully evaluated in all patients diagnosed with ICMP and their relatives. Cancer treatment was scheduled with close cardiological follow-up, and all patients successfully completed planned cancer treatment. In all HCM patients, LVEF remained normal.
4. Discussion
The frequency of ICMPs in a cancer population should be the same as in the general healthy population. Consequently, in our cohort, thanks to the integral cardiovascular basal evaluation performed at the Cardio-Oncology Unit, we were able to identify the expected numbers of ICMPs (Table 3) that otherwise may have been overlooked. This means that ICMPs were neither overdiagnosed nor overlooked in this cancer cohort.
To date, very few studies have evaluated the prevalence of ICMP at baseline CV assessment in cancer populations. Most studies have focused on evaluating the role of genetic predisposition in those patients who develop HF or LVEF dysfunction during/after cancer treatment. For instance, pathogenic variants and rare variants in TTN and MYH7 genes have been reported in patients with chemotherapy-induced cardiomyopathy [36,37,38,39,40,41]. However, to the best of our knowledge, this is the first study to evaluate the impact of cardio-oncology CV basal screening in detection of ICMPs. In this regard, we would like to reinforce the importance of CV basal risk evaluation, including ECG and family history investigation.
The emergence of the cardio-oncology discipline and recent ESC guidelines have provided important insights that have substantially helped improve cancer patients management in many challenging scenarios [2,3,4]. The previous cardiotoxicity surveillance of many studies and oncology trials during anticancer therapies just focused on LVEF measurements. Therefore, some physicians may only focus their cardiotoxicity awareness on evaluation of this single parameter [10]. However, TTE has an important role beyond LVEF changes recognition. TTE can also reveal subclinical unknown CVD [5,10,42], including ICMPs. Moreover, basal CV risk stratification, including ECG, is also essential and recommended in all cancer patients [3]. In this regard, the CARDIOTOX registry [9] is one of the most important studies that has illustrated the importance of baseline CV risk assessment. Basal SCORE [43] results could predict severe cardiotoxicity and all-cause mortality during follow-up [9].
In the present ESC guidelines, the recommendation for cardiological referral is limited to those patients whose baseline CV toxicity risk assessment presents abnormal findings, those who have pre-existing CVD or ECG abnormalities or those who are at high or very high risk (class I, level C) [3]. Although not explicitly taken into account in the scores, excluding family history of cardiomyopathy and ruling out that the patient is carrier of a pathogenic gene variant associated with a known familiar cardiomyopathy is also required to consider the patient as “low risk” [3,9,10,43]. In this regard, planning protocols for cancer treatments with potential CV toxicity provides unique opportunities to comprehensively assess CV health before initiation of cancer treatment [5]. However, basal risk assessment can be challenging. Our Cardio-Oncology Unit began in 2020, coinciding with the rise of the COVID-19 pandemic [18]. Therefore, to minimize hospital visits, we took advantage of the possibility to integrate the TTE evaluation with a general cardiac evaluation, including personal and family history, physical examination, anamnesis and global CV risk assessment, including ECG, at the same visit. As a result, considering that all breast cancer patients scheduled for AC or anti-HER therapies will need a pre-treatment basal TTE [3], we specifically designed a breast cancer patient flow chart. The primary objective was to avoid waiting lists to prevent cancer treatment delays in the pandemic scenario.
Given the presented data, we encourage clinicians to invest a little more time to gather information about family history of suspected ICMP and SCD at a young age and carefully look for ECG abnormalities. Moreover, we also hypothesize that, in those patients whose TTE is mandatory, scheduling a basal cardiology consult in the same visit, including both TTE plus clinical evaluation and CV risk assessment (including family history and ECG), could be of value and, perhaps, cost effective.
On the other hand, identifying concealed ICMPs in cancer patients is of utmost importance as they can represent a potentially very-high-risk population for cardiotoxicity. In our cohort, cancer treatment was discussed by the Cardio-Oncology team to plan the best possible cancer treatment while trying to safely minimize its CV complications. Multidisciplinary work, properly scheduling cardiological and cancer treatment, was the goal so that all our patients could successfully complete their planned treatment. In this regard, in patient 4, ICD-TRC implantation was delayed until radiotherapy and optimal medical treatment were completed. Afterwards, both LVEF and the severe mitral regurgitation, as well as HF symptoms, significantly improved. In addition, genetic data can provide very valuable information for personalized medicine, including planning targeted therapeutic options and properly scheduling the timing for follow-up appointments and future exams [17]. For instance, patients with TTN truncating variants (such as patients 2 and 3) are associated with recovery of LVEF with standard HF treatment [6,17].
In addition, risk stratification for SCD should also be carefully evaluated in all ICMP patients, considering the estimated life expectancy. Identifying a pathogenic variant in any patient with ICMP not only provides clinical prognostic information but also may contribute to the indications for device implantation [6]. However, little information is available about possible additional risk provided by the cardiotoxic drugs in SCD risk stratification. To date, identifying those DCM patients who are at a high arrhythmogenic risk, even in the absence of cardiotoxic therapies still remains a real clinical challenge. In this regard, genetic information can be crucial. For instance, in patient 1, who presented left ventricular dysfunction, a pathogenic truncating variant in FLNC was identified. Pathogenic variants in certain DCM genes, like FLNC, have been reported in highly arrhythmogenic phenotypes with minimal or subtle structural defects [44]. Therefore, in current ESC guidelines, ICD implantation in primary prevention should be considered in those with a high-risk genetic background for SCD even if their LVEF is higher than 35%. Moreover, in relatives who are carriers of a causative genetic variant associated with increased risk of SCD, like FLNC, complete phenotypical evaluation with CMR, even with normal LVEF by TTE, is recommended [17].
Apart from that, if a pathogenic variant is identified in the proband, this information is also very useful for the family. Genetic information enables family counseling and identifying at-risk carriers of the familial pathogenic variant through the proven cost-effective cascade screening [21,45].
5. Limitations
We present the results of a single-center study on the experience of breast cancer patients and, consequently, mostly women. We do not believe that general CV risk assessment by Cardio-Oncology Units should be extended to all cancer patients. We strongly believe that CV risk stratification assessment (including family history and ECG) should continue to be performed by the treating oncology or hematology team to identify the patients who really benefit from referring. It is of utmost importance that Cardio-Oncology Units are able to provide specific evaluations without delay, but only in selected patients. If all patients were referred indefinitely, these units would not be able to respond in time to those who really need them. Our approach was only intended for those patients who were already programmed for mandatory basal TTE.
6. Conclusions
The 2022 ESC cardio-oncology guidelines recommend a comprehensive baseline assessment of CV toxicity risk before cardiotoxic therapies. Opportunistic screening of concealed ICMPs using clinical history, ECG and TTE provides important information to re-stratify the baseline CV toxicity risk and to optimize preventive strategies and cancer treatment monitoring. It also allows for cascade family testing and the extension of preventive strategies to all available relatives with concealed high cardiovascular risk.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13010002/s1, Table S1: NGS-Cardiovascular gene panel sequenced for all inherited cardiovascular conditions at our institution.
Author Contributions
Conceptualization, R.L.; methodology, R.A.-V. and J.G.; software, R.A.-V. and J.G.; validation, R.A.-V. and J.G.; formal analysis, M.F. and R.A.-V.; investigation, R.L., M.F., S.C., M.M., M.I., Y.F. and E.E.; resources, S.C., M.M., M.I., Y.F. and E.E.; data curation, M.F.; writing—original draft preparation, R.L.; writing—review and editing, I.P. and T.L.-F.; visualization I.P.; supervision, P.A. and T.L.-F.; project administration, P.A. and T.L.-F.; funding acquisition, P.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee (CEImPA 2023.264).
Informed Consent Statement
All patients who underwent genetic testing signed a written informed consent form for genetic testing and investigational purposes (CEImPA 2023.254).
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by Instituto de Salud Carlos III (ISCIII) (grant number PI22/00705).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Herrmann J., Lerman A., Sandhu N.P., Villarraga H.R., Mulvagh S.L., Kohli M. Evaluation and management of patients with heart disease and cancer: Cardio-oncology. Mayo Clin. Proc. 2014;89:1287–1306. doi: 10.1016/j.mayocp.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zamorano J.L., Lancellotti P., Rodriguez Muñoz D., Aboyans V., Asteggiano R., Galderisi M., Habib G., Lenihan D.J., Lip G.Y.H., Lyon A.R., et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC) Eur. Heart J. 2016;37:2768–2801. doi: 10.1093/eurheartj/ehw211. [DOI] [PubMed] [Google Scholar]
- 3.Lyon A.R., López-Fernández T., Couch L.S., Asteggiano R., Aznar M.C., Bergler-Klein J., Boriani G., Cardinale D., Cordoba R., Cosyns B., et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS) Eur. Heart J. 2022;43:4229–4361. doi: 10.1093/eurheartj/ehac244. [DOI] [PubMed] [Google Scholar]
- 4.Lancellotti P., Suter T.M., López-Fernández T., Galderisi M., Lyon A.R., Van der Meer P., Cohen Solal A., Zamorano J.-L., Jerusalem G., Moonen M., et al. Cardio-Oncology Services: Rationale, organization, and implementation. Eur. Heart J. 2019;40:1756–1763. doi: 10.1093/eurheartj/ehy453. [DOI] [PubMed] [Google Scholar]
- 5.Lyon A.R., Dent S., Stanway S., Earl H., Brezden-Masley C., Cohen-Solal A., Tocchetti C.G., Moslehi J.J., Groarke J.D., Bergler-Klein J., et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: A position statement and new risk assessment tools from the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society. Eur. J. Heart Fail. 2020;22:1945–1960. doi: 10.1002/ejhf.1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDonagh T.A., Metra M., Adamo M., Gardner R.S., Baumbach A., Böhm M., Burri H., Butler J., Čelutkienė J., Chioncel O., et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021;42:3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 7.Visseren F.L.J., Mach F., Smulders Y.M., Carballo D., Koskinas K.C., Bäck M., Benetos A., Biffi A., Boavida J.-M., Capodanno D., et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021;42:3227–3337. doi: 10.1093/eurheartj/ehab484. [DOI] [PubMed] [Google Scholar]
- 8.Curigliano G., Lenihan D., Fradley M., Ganatra S., Barac A., Blaes A., Herrmann J., Porter C., Lyon A.R., Lancellotti P., et al. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2020;31:171–190. doi: 10.1016/j.annonc.2019.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caro-Codón J., López-Fernández T., Álvarez-Ortega C., Zamora Auñón P., Rodríguez I.R., Gómez Prieto P., Buño Soto A., Canales Albendea M., Albaladejo A., Mediavilla G., et al. Cardiovascular risk factors during cancer treatment. Prevalence and prognostic relevance: Insights from the CARDIOTOX registry. Eur. J. Prev. Cardiol. 2022;29:859–868. doi: 10.1093/eurjpc/zwaa034. [DOI] [PubMed] [Google Scholar]
- 10.Čelutkienė J., Pudil R., López-Fernández T., Grapsa J., Nihoyannopoulos P., Bergler-Klein J., Cohen-Solal A., Farmakis D., Tocchetti C.G., von Haehling S., et al. Role of cardiovascular imaging in cancer patients receiving cardiotoxic therapies: A position statement on behalf of the Heart Failure Association (HFA), the European Association of Cardiovascular Imaging (EACVI) and the Cardio-Oncology Council of the European Society of Cardiology (ESC) Eur. J. Heart Fail. 2020;22:1504–1524. doi: 10.1002/ejhf.1957. [DOI] [PubMed] [Google Scholar]
- 11.Romond E.H., Jeong J.H., Rastogi P., Swain S.M., Geyer C.E., Ewer M.S., Rathi V., Fehrenbacher L., Brufsky A., Azar C.A., et al. Seven-year follow-up assessment of cardiac function in NSABP B-31, a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel (ACP) with ACP plus trastuzumab as adjuvant therapy for patients with node-positive, human epidermal growth factor receptor 2-positive breast cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2012;30:3792–3799. doi: 10.1200/JCO.2011.40.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cardinale D., Colombo A., Bacchiani G., Tedeschi I., Meroni C.A., Veglia F., Civelli M., Lamantia G., Colombo N., Curigliano G., et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131:1981–1988. doi: 10.1161/CIRCULATIONAHA.114.013777. [DOI] [PubMed] [Google Scholar]
- 13.Wang L., Tan T.C., Halpern E.F., Neilan T.G., Francis S.A., Picard M.H., Fei H., Hochberg E.P., Abramson J.S., Weyman A.E., et al. Major Cardiac Events and the Value of Echocardiographic Evaluation in Patients Receiving Anthracycline-Based Chemotherapy. Am. J. Cardiol. 2015;116:442–446. doi: 10.1016/j.amjcard.2015.04.064. [DOI] [PubMed] [Google Scholar]
- 14.Abu-Khalaf M.M., Safonov A., Stratton J., Wang S., Hatzis C., Park E., Pusztai L., Gross C.P., Russell R. Examining the cost-effectiveness of baseline left ventricular function assessment among breast cancer patients undergoing anthracycline-based therapy. Breast Cancer Res. Treat. 2019;176:261–270. doi: 10.1007/s10549-019-05178-z. [DOI] [PubMed] [Google Scholar]
- 15.Cameron D., Piccart-Gebhart M.J., Gelber R.D., Procter M., Goldhirsch A., de Azambuja E., Castro G., Untch M., Smith I., Gianni L., et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: Final analysis of the HERceptin Adjuvant (HERA) trial. Lancet Lond. Engl. 2017;389:1195–1205. doi: 10.1016/S0140-6736(16)32616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seferović P.M., Polovina M., Bauersachs J., Arad M., Ben Gal T., Lund L.H., Felix S.B., Arbustini E., Caforio A.L.P., Farmakis D., et al. Heart failure in cardiomyopathies: A position paper from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2019;21:553–576. doi: 10.1002/ejhf.1461. [DOI] [PubMed] [Google Scholar]
- 17.Arbelo E., Protonotarios A., Gimeno J.R., Arbustini E., Barriales-Villa R., Basso C., Bezzina C.R., Biagini E., Blom N.A., de Boer R.A., et al. 2023 ESC Guidelines for the management of cardiomyopathies. Eur. Heart J. 2023:ehad194. doi: 10.1093/eurheartj/ehad194. [DOI] [PubMed] [Google Scholar]
- 18.Lorca R., López Triviño R., Morís C. Cardio-onco-hematology patients’ management in the context of the current COVID-19 pandemic. Rev. Espanola Cardiol. Engl. Ed. 2020;73:694–695. doi: 10.1016/j.recesp.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Authors/Task Force Members. Elliott P.M., Anastasakis A., Borger M.A., Borggrefe M., Cecchi F., Charron P., Hagege A.A., Lafont A., Limongelli G., et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC) Eur. Heart J. 2014;35:2733–2779. doi: 10.1093/eurheartj/ehu284. [DOI] [PubMed] [Google Scholar]
- 20.Towbin J.A., McKenna W.J., Abrams D.J., Ackerman M.J., Calkins H., Darrieux F.C.C., Daubert J.P., de Chillou C., DePasquale E.C., Desai M.Y., et al. 2019 HRS expert consensus statement on evaluation, risk stratification, and management of arrhythmogenic cardiomyopathy: Executive summary. Heart Rhythm. 2019;16:e373–e407. doi: 10.1016/j.hrthm.2019.09.019. [DOI] [PubMed] [Google Scholar]
- 21.Wilde A.A.M., Semsarian C., Márquez M.F., Sepehri Shamloo A., Ackerman M.J., Ashley E.A., Sternick Eduardo B., Barajas-Martinez H., Behr E.R., Bezzina C.R., et al. European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society (LAHRS) Expert Consensus Statement on the state of genetic testing for cardiac diseases. J. Arrhythmia. 2022;38:491–553. doi: 10.1002/joa3.12717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cuesta-Llavona E., Lorca R., Díaz-Molina B., Lambert-Rodríguez J.L., Reguero J.R., Iglesias S., Alonso B., Junco-Vicente A., Alonso V., Coto E., et al. Genetic Screening of a Large Panel of Genes Associated with Cardiac Disease in a Spanish Heart Transplanted Cohort. Cardiogenetics. 2022;12:198–205. doi: 10.3390/cardiogenetics12020018. [DOI] [Google Scholar]
- 23.Gómez J., Reguero J.R., Morís C., Martín M., Alvarez V., Alonso B., Iglesias S., Coto E. Mutation Analysis of the Main Hypertrophic Cardiomyopathy Genes Using Multiplex Amplification and Semiconductor Next-Generation Sequencing. Circ. J. 2014;78:2963–2971. doi: 10.1253/circj.CJ-14-0628. [DOI] [PubMed] [Google Scholar]
- 24.Gómez J., Lorca R., Reguero J.R., Morís C., Martín M., Tranche S., Alonso B., Iglesias S., Alvarez V., Díaz-Molina B., et al. Screening of the Filamin C Gene in a Large Cohort of Hypertrophic Cardiomyopathy Patients. Circ. Cardiovasc. Genet. 2017;10:e001584. doi: 10.1161/CIRCGENETICS.116.001584. [DOI] [PubMed] [Google Scholar]
- 25.Lorca R., Aparicio A., Cuesta-Llavona E., Pascual I., Junco A., Hevia S., Villazón F., Hernandez-Vaquero D., Rodríguez Reguero J.J., Moris C., et al. Familial Hypercholesterolemia in Premature Acute Coronary Syndrome. Insights from CholeSTEMI Registry. J. Clin. Med. 2020;9:E3489. doi: 10.3390/jcm9113489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lorca R., Junco-Vicente A., Pérez-Pérez A., Pascual I., Persia-Paulino Y.R., González-Urbistondo F., Cuesta-Llavona E., Fernández-Barrio B.C., Morís C., Rubín J.M., et al. KCNH2 p.Gly262AlafsTer98: A New Threatening Variant Associated with Long QT Syndrome in a Spanish Cohort. Life. 2022;12:556. doi: 10.3390/life12040556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cuesta-Llavona E., Lorca R., Salgado M., García-Lago C., Rodríguez-Reguero J., Rodríguez-López R., Escribano-Hernández V., Peña-Cabia A., Vázquez-Coto D., Pascual I., et al. Retrospective variant reclassification and resequencing in hypertrophic cardiomyopathy: A Reference Unit Centre Experience. Eur. J. Prev. Cardiol. 2023:zwad325. doi: 10.1093/eurjpc/zwad325. [DOI] [PubMed] [Google Scholar]
- 28.Richards S., Aziz N., Bale S., Bick D., Das S., Gastier-Foster J., Grody W.W., Hegde M., Lyon E., Spector E., et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. Off. J. Am. Coll. Med. Genet. 2015;17:405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aras D., Tufekcioglu O., Ergun K., Ozeke O., Yildiz A., Topaloglu S., Deveci B., Sahin O., Kisacik H.L., Korkmaz S. Clinical features of isolated ventricular noncompaction in adults long-term clinical course, echocardiographic properties, and predictors of left ventricular failure. J. Card. Fail. 2006;12:726–733. doi: 10.1016/j.cardfail.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 30.André F., Burger A., Loßnitzer D., Buss S.J., Abdel-Aty H., Gianntisis E., Steen H., Katus H.A. Reference values for left and right ventricular trabeculation and non-compacted myocardium. Int. J. Cardiol. 2015;185:240–247. doi: 10.1016/j.ijcard.2015.03.065. [DOI] [PubMed] [Google Scholar]
- 31.Stähli B.E., Gebhard C., Biaggi P., Klaassen S., Valsangiacomo Buechel E., Attenhofer Jost C.H., Jenni R., Tanner F.C., Greutmann M. Left ventricular non-compaction: Prevalence in congenital heart disease. Int. J. Cardiol. 2013;167:2477–2481. doi: 10.1016/j.ijcard.2012.05.095. [DOI] [PubMed] [Google Scholar]
- 32.Oechslin E., Jenni R. Left ventricular non-compaction revisited: A distinct phenotype with genetic heterogeneity? Eur. Heart J. 2011;32:1446–1456. doi: 10.1093/eurheartj/ehq508. [DOI] [PubMed] [Google Scholar]
- 33.Pignatelli R.H., McMahon C.J., Dreyer W.J., Denfield S.W., Price J., Belmont J.W., Craigen W.J., Wu J., El Said H., Bezold L.I., et al. Clinical characterization of left ventricular noncompaction in children: A relatively common form of cardiomyopathy. Circulation. 2003;108:2672–2678. doi: 10.1161/01.CIR.0000100664.10777.B8. [DOI] [PubMed] [Google Scholar]
- 34.Stanton C., Bruce C., Connolly H., Brady P., Syed I., Hodge D., Asirvatham S., Friedman P. Isolated left ventricular noncompaction syndrome. Am. J. Cardiol. 2009;104:1135–1138. doi: 10.1016/j.amjcard.2009.05.062. [DOI] [PubMed] [Google Scholar]
- 35.Lorca R., Martín M., Pascual I., Astudillo A., Díaz Molina B., Cigarrán H., Cuesta-Llavona E., Avanzas P., Rodríguez Reguero J.J., Coto E., et al. Characterization of Left Ventricular Non-Compaction Cardiomyopathy. J. Clin. Med. 2020;9:2524. doi: 10.3390/jcm9082524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Linschoten M., Teske A.J., Baas A.F., Vink A., Dooijes D., Baars H.F., Asselbergs F.W. Truncating Titin (TTN) Variants in Chemotherapy-Induced Cardiomyopathy. J. Card. Fail. 2017;23:476–479. doi: 10.1016/j.cardfail.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 37.van den Berg M.P., van Spaendonck-Zwarts K.Y., van Veldhuisen D.J., Gietema J.A., Postma A., van Tintelen J.P. Familial dilated cardiomyopathy: Another risk factor for anthracycline-induced cardiotoxicity? Eur. J. Heart Fail. 2010;12:1297–1299. doi: 10.1093/eurjhf/hfq175. [DOI] [PubMed] [Google Scholar]
- 38.Shipman K.E., Arnold I. Case of epirubicin-induced cardiomyopathy in familial cardiomyopathy. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2011;29:e537–e538. doi: 10.1200/JCO.2011.34.8052. [DOI] [PubMed] [Google Scholar]
- 39.Wasielewski M., van Spaendonck-Zwarts K.Y., Westerink N.D.L., Jongbloed J.D.H., Postma A., Gietema J.A., van Tintelen J.P., van den Berg M.P. Potential genetic predisposition for anthracycline-associated cardiomyopathy in families with dilated cardiomyopathy. Open Heart. 2014;1:e000116. doi: 10.1136/openhrt-2014-000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Garcia-Pavia P., Kim Y., Restrepo-Cordoba M.A., Lunde I.G., Wakimoto H., Smith A.M., Toepfer C.N., Getz K., Gorham J., Patel P., et al. Genetic Variants Associated With Cancer Therapy-Induced Cardiomyopathy. Circulation. 2019;140:31–41. doi: 10.1161/CIRCULATIONAHA.118.037934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moghadasi S., Fijn R., Beeres S.L.M.A., Bikker H., Jongbloed J.D.H., Josephus Jitta D., Kroep J.R., Lekanne Deprez R.H., Vos Y.J., de Vreede M.J.M., et al. Case series, chemotherapy-induced cardiomyopathy: Mind the family history! Eur. Heart J. Case Rep. 2021;5:ytab333. doi: 10.1093/ehjcr/ytab333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Plana J.C., Thavendiranathan P., Bucciarelli-Ducci C., Lancellotti P. Multi-Modality Imaging in the Assessment of Cardiovascular Toxicity in the Cancer Patient. JACC Cardiovasc. Imaging. 2018;11:1173–1186. doi: 10.1016/j.jcmg.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 43.Conroy R.M., Pyörälä K., Fitzgerald A.P., Sans S., Menotti A., De Backer G., De Bacquer D., Ducimetière P., Jousilahti P., Keil U., et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003;24:987–1003. doi: 10.1016/S0195-668X(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 44.Peters S., Kumar S., Elliott P., Kalman J.M., Fatkin D. Arrhythmic Genotypes in Familial Dilated Cardiomyopathy: Implications for Genetic Testing and Clinical Management. Heart Lung Circ. 2019;28:31–38. doi: 10.1016/j.hlc.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 45.Wordsworth S., Leal J., Blair E., Legood R., Thomson K., Seller A., Taylor J., Watkins H. DNA testing for hypertrophic cardiomyopathy: A cost-effectiveness model. Eur. Heart J. 2010;31:926–935. doi: 10.1093/eurheartj/ehq067. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.