Abstract
Vertex epidural hematomas are very uncommon complications of traumatic head injury. Besides the volume of the epidural bleeding, compression of the superior sagittal sinus may be source for added elevated intracranial pressure. Clinical presentation of such lesions is heterogenous and symptoms can develop in an acute to a chronic frame. Radiological diagnosis can sometimes be challenging. Due to its rarity, such lesions have been only reported on case reports and small series and the management remain controversial. Hereby we report 3 cases of surgically managed post traumatic acute epidural hematomas of the vertex. Wen also went through a literature-based discussion of clinical, radiological and therapeutic features related to this condition.
Keywords: Cranial epidural hematoma, Brain trauma, Neurosurgery, Vertex
INTRODUCTION
Vertex epidural hematomas (VEHs) are uncommon complications of traumatic head injuries that account for 18% of traumatic epidural hematomas.1,2,3) The clinical presentation of such lesions is heterogeneous, symptoms can develop from an acute to chronic, and radiological diagnosis can be challenging.11) Due to the rarity of VEH, such lesions have only been described in case reports and small series, and their management remains controversial, with most authors preferring a conservative approach. Herein, we report 3 cases of surgically managed post-traumatic acute VEHs. The ensuing literature-based discussion addresses the clinical, radiological, and therapeutic features related to this condition.
CASE REPORT
Three cases of VEH that were surgically managed in the Department of Neurosurgery of the Center for Traumatology and Major Burns, Ben Arous(Tunis, Tunisia) are described.
Case 1
A 39-year-old male with no medical records was struck by a motor vehicle while riding a motorcycle, causing brain, thoracic, and peripheral trauma. Early neurological examination revealed a normal state of consciousness, with a Glasgow Coma Scale score of 15/15 and no neurological signs of localization.
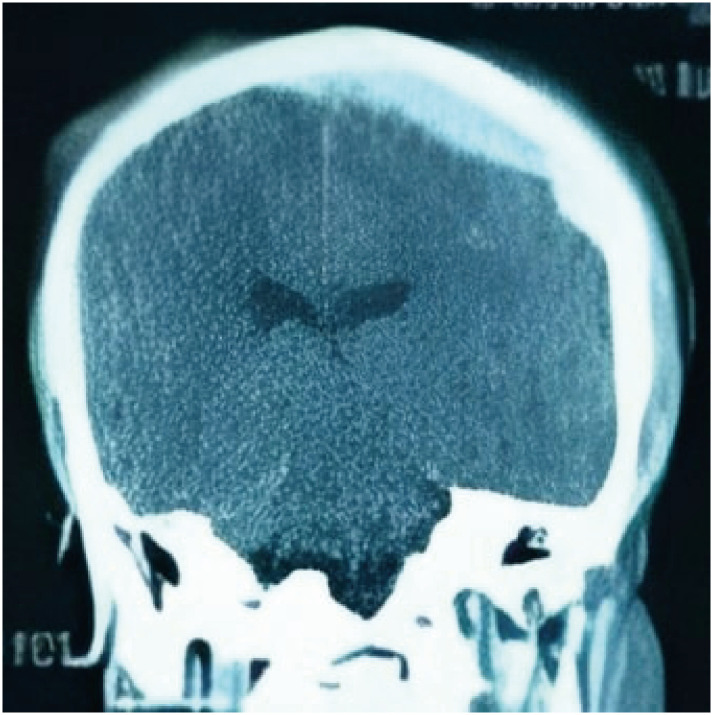
Brain computed tomography (CT) revealed an acute frontoparietal epidural hematoma of the vertex with a nondisplaced fracture of the midline. The main site of the epidural bleeding was on the left side (FIGURE 1). Several hours later, the patient experienced intense headache, although control CT did not reveal any obvious changes. It was decided to evacuate the hematoma through unilateral left craniotomy (FIGURE 2). The bleeding appeared to be related to wide detachment of the dura mater because it was diffuse without any obvious specific source of hemorrhage. Both the peripheral and central dural suspensions were prepared. Postoperative follow-up was uneventful, the patient improved clinically, and was discharged with no complications on day 5 after the trauma.
FIGURE 1. Coronal section of a brain computed tomography scan showing an epidural hematoma of the vertex mainly located on the left side of the sinus.
FIGURE 2. 3D reconstruction of a postoperative computed tomography scan on bony windows showing the location of the performed craniotomy.
Case 2
A 35-year-old male with no medical records experienced a domestic accident as he slipped on stairs, causing isolated head trauma with an occipitoparietal impact. Early neurological examination of the trauma revealed a normal state of consciousness, with a Glasgow Coma Scale score of 15/15 and no neurological deficits. He reported headache with horizontal diplopia, suggesting increased intracranial pressure syndrome. Brain CT (FIGURE 3) revealed a VEH with a fracture and midline diastasis, suggesting a superior sagittal sinus (SSS) wound. It was decided to perform surgery due to progressively increasing intracranial pressure syndrome. Two craniotomies were performed bilaterally, leaving an osseous bridge at the midline to protect the SSS (FIGURE 4). The epicenter of the hematoma appeared to be on the edge of the SSS; however, it was decided to stay clear of the coagulated blood in contact with the sinus to avoid rebleeding. Peripheral suspension of the dura was performed on the edges of both craniotomies. The hematoma was then completely removed. Postoperative follow up was uneventful and postoperative CT (FIGURE 5) revealed subtotal removal of the hematoma; the patient was discharged on day 3 after admission.
FIGURE 3. Axial (A), sagittal (B) and coronal (C) sections of a brain computed tomography scan showing an epidural hematoma of the vertex. 3D reconstruction on bony sections of the same scan (D) showed a fracture located towards the skull midline.
FIGURE 4. Peroperative picture showing the location of the craniotomies leaving a bony bridge between them.
FIGURE 5. Postoperative computed tomography scan showing a subtotal removal of the hematoma.
Case 3
A 23-year-old male was the victim of a traffic accident as he was struck by a motor vehicle while trying to cross the street, causing both head and thoracic injuries. On initial examination, the patient was drowsy, with a Glasgow Coma Scale score of 14/15. The remaining clinical examinations revealed no abnormalities. A body scan revealed pulmonary contusions and a vertex parietal epidural hematoma (FIGURE 6), an indication for emergent surgical evacuation due to neurological deterioration. The patient underwent surgery using the same technique described in Case 2. Postoperatively, the patient recovered to an ideal state of consciousness, and further follow-up was uneventful. Postoperative CT (FIGURE 7) revealed subtotal hematoma removal. The patient was discharged 5 days after surgery.
FIGURE 6. Axial (A), coronal (B) and sagittal sections (C) of a brain computed tomography scan showing an epidural hematoma of the vertex. 3D reconstruction on bony sections of the same scan (D) showed a fracture of the parietal bone crossing the midline.
FIGURE 7. Postoperative computed tomography scan showing a total removal of the hematoma as well as the epidural drain.
DISCUSSION
VEH is a specific presentation of epidural hematoma, mostly due to traumatic injury. On reviewing the literature, we found that this pathology has only been described in case reports or small series due to its rarity.11)
Wylen and Nanda12) reported that VEH accounted for 1.3%–8.2% of all traumatic intracranial hematomas. Ramesh 11) reported that the incidence of VEH was 0.024% for head injuries and 0.47% for epidural hematomas.
The pathophysiological mechanisms associated with vertex localization of epidural hematomas vary. Most cases are related to trauma, such as tears of the SSS, bleeding from a skull fracture, or dural laceration of the inner table of the skull.11) In some cases, non-traumatic conditions may facilitate bleeding after a head injury (Paget’s disease or arteriovenous fistula of the meningeal artery). Spontaneous VEH have also been reported.11)
VEH is a particular type of epidural hematoma with a misleading clinical presentation and neuroradiological features. Diagnosis can sometimes be delayed due to difficulties in visualizing bleeding on axial CT, with clinical signs of increased intracranial pressure.4,10) This problem is more important in patients with chronic VEH because it may spontaneously expand and pose additional harm.2)
The clinical presentation of VEH varies. In some cases (such as Cases 1 and 3), the onset of symptoms is acute and directly attributable to trauma; in other cases, the presentation is more progressive or delayed.9) Pain is the most common symptom.5) Headaches are secondary to different factors, such as direct dural irritation caused by detachment along the SSS, considering that the dura in this area is richly innervated by sensory fibers. Increased intracranial pressure secondary to both the added volume and compression of the SSS and venous system is also an important source of headaches.5,11)
In some cases, patients may present with a lower limb deficit, which can be unilateral or bilateral, secondary to the direct pressure of the VEH on one or both motor cortices. Paraparesis due to bilateral compression can lead to a spinal cord injury.7)
Radiological diagnosis of VEH in the pre-CT era was challenging. When suspected, venous angiography can yield in a positive diagnosis because it reveals an avascular lesion detaching a narrowed SSS from the inner table of the skull.1,9)
Multiplanar imaging makes the diagnosis much easier because the diagnosis of VEH on axial CT may sometimes be challenging.5) In fact, many investigators have noticed that acute VEH may be overlooked on classic CT because of a blind spot near the top of the calvaria.9) Coronal and sagittal sections are mandatory for diagnosis when vague hyperdense collections are visualized on the highest sections of axial CT with the coexistence of a fracture running across the vault of the skull or diastasis of the sagittal or coronal suture.11)
The management of VEH should be considered on a case-to-case basis.8) In our experience, we tend to operate on symptomatic epidural hematomas; no exception has been adopted for those of the vertex. None of our patients experienced any complications and were rapidly discharged, avoiding the unpredictable complications of hematoma and multifactorial elevated intracranial pressure, as well as repetitive CT scans. To our knowledge, no studies have directly addressed VEH. However, with advances in monitoring technologies, there is an increasing tendency to manage epidural hematomas conservatively, with surgery indicated only in cases with evidence of imminent decompensation of elevated intracranial pressure.11)
Technical approaches are diverse; some authors have proposed a midline craniotomy that exposes the SSS to control any bleeding originating from it. Generally, even when bleeding originates from the SSS, it should already be blocked by the hematoma stopping bleeding from the dural tear when surgery is performed. For this reason, it is recommended to leave some of the hematoma on the sinus to avoid recurrence of bleeding. Others prefer bilateral craniotomies separated by a bony bridge that protects the sinus and enables an easier and more efficient dural suspension. When bleeding is lateralized to one side, a unilateral craniotomy can also be performed, leaving a small volume of blood above the sinus and on the contralateral side.1,3,4,8)
During follow-up, patients must be monitored clinically and radiologically to detect thrombosis of the SSS, which may occur due to sinus compression by the hematoma.6) In this case, anticoagulation must be proposed with monitoring for any eventual rebleeding.
CONCLUSION
VEH is a rare form of epidural hematoma. The clinical and radiological features described herein may lead to misdiagnosis. Diagnosis must be confirmed through coronal section imaging using CT to avoid serious complications that may harm the functional and vital prognosis. There is no consensus regarding either a management or technical approach.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.Ben-Israel D, Isaacs AM, Morrish W, Gallagher NC. Acute vertex epidural hematoma. Surg Neurol Int. 2017;8:219. doi: 10.4103/sni.sni_218_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonilha L, Mattos JP, Borges WA, Fernandes YB, Andrioli MS, Borges G. Chronic epidural hematoma of the vertex. Clin Neurol Neurosurg. 2003;106:69–73. doi: 10.1016/j.clineuro.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Fernandes-Cabral DT, Kooshkabadi A, Panesar SS, Celtikci E, Borghei-Razavi H, Celtikci P, et al. Surgical management of vertex epidural hematoma: technical case report and literature review. World Neurosurg. 2017;103:475–483. doi: 10.1016/j.wneu.2017.04.040. [DOI] [PubMed] [Google Scholar]
- 4.Harbury OL, Provenzale JM, Barboriak DP. Vertex epidural hematomas: imaging findings and diagnostic pitfalls. Eur J Radiol. 2000;36:150–157. doi: 10.1016/s0720-048x(00)00175-3. [DOI] [PubMed] [Google Scholar]
- 5.Klepinowski T, Kawalec P, Larysz M, Sagan L. Acute-on-chronic vertex epidural hematoma with diastasis of the sagittal suture in an adult. World Neurosurg. 2020;139:245–249. doi: 10.1016/j.wneu.2020.04.088. [DOI] [PubMed] [Google Scholar]
- 6.Kumar J, Prakash A, Harsh V, Kumar A. Vertex extradural hematoma: a diagnostic dilemma. Asian J Neurosurg. 2017;12:718–720. doi: 10.4103/1793-5482.215758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Messori A, Pauri F, Rychlicki F, Veronesi V, Salvolini U. Acute posttraumatic paraplegia caused by epidural hematoma at the vertex. AJNR Am J Neuroradiol. 2001;22:1748–1749. [PMC free article] [PubMed] [Google Scholar]
- 8.Miller DJ, Steinmetz M, McCutcheon IE. Vertex epidural hematoma: surgical versus conservative management: two case reports and review of the literature. Neurosurgery. 1999;45:621–624. doi: 10.1097/00006123-199909000-00036. [DOI] [PubMed] [Google Scholar]
- 9.Navarro JN, Alves RV. Vertex epidural hematoma: a rare cause of post-traumatic headache and a diagnostic challenge. Surg Neurol Int. 2016;7(Suppl 10):S276–S278. doi: 10.4103/2152-7806.181982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pomeranz S, Wald U, Zagzag D, Gomori M, Shalit M. Chronic epidural hematoma of the vertex: problems in detection with computed tomography. Surg Neurol. 1984;22:409–411. doi: 10.1016/0090-3019(84)90148-4. [DOI] [PubMed] [Google Scholar]
- 11.Ramesh VG. Vertex extradural hematoma. Neurol India. 2012;60:369. doi: 10.4103/0028-3886.98552. [DOI] [PubMed] [Google Scholar]
- 12.Wylen EL, Nanda A. Vertex epidural hematoma with coronal suture diastasis presenting with paraplegia. J Trauma. 1998;45:413–415. doi: 10.1097/00005373-199808000-00042. [DOI] [PubMed] [Google Scholar]