Abstract
Background
Diabetic peripheral neuropathy (DPN) is a frequent complication in people living with type 1 or type 2 diabetes. There is currently no effective treatment for DPN. Although alpha‐lipoic acid (ALA, also known as thioctic acid) is widely used, there is no consensus about its benefits and harms.
Objectives
To assess the effects of alpha‐lipoic acid as a disease‐modifying agent in people with diabetic peripheral neuropathy.
Search methods
On 11 September 2022, we searched the Cochrane Neuromuscular Specialised Register, CENTRAL, MEDLINE, Embase, and two clinical trials registers. We also searched the reference lists of the included studies and relevant review articles for additional references not identified by the electronic searches.
Selection criteria
We included randomised clinical trials (RCTs) that compared ALA with placebo in adults (aged 18 years or older) and that applied the study interventions for at least six months. There were no language restrictions.
Data collection and analysis
We used standard methods expected by Cochrane. The primary outcome was change in neuropathy symptoms expressed as changes in the Total Symptom Score (TSS) at six months after randomisation. Secondary outcomes were change in neuropathy symptoms at six to 12 months and at 12 to 24 months, change in impairment, change in any validated quality of life total score, complications of DPN, and adverse events. We assessed the certainty of the evidence using GRADE.
Main results
Our analysis incorporated three trials involving 816 participants. Two studies included people with type 1 or type 2 diabetes, while one study included only people with type 2 diabetes. The duration of treatment was between six months and 48 months. We judged all studies at high risk of overall bias due to attrition.
ALA compared with placebo probably has little or no effect on neuropathy symptoms measured by TSS (lower score is better) after six months (mean difference (MD) −0.16 points, 95% confidence interval (CI) −0.83 to 0.51; 1 study, 330 participants; moderate‐certainty evidence). The CI of this effect estimate did not contain the minimal clinically important difference (MCID) of 0.97 points. ALA compared with placebo may have little or no effect on impairment measured by the Neuropathy Impairment Score‐Lower Limbs (NIS‐LL; lower score is better) after six months (MD −1.02 points, 95% CI −2.93 to 0.89; 1 study, 245 participants; low‐certainty evidence). However, we cannot rule out a significant benefit, because the lower limit of the CI surpassed the MCID of 2 points. There is probably little or no difference between ALA and placebo in terms of adverse events leading to cessation of treatment within six months (risk ratio (RR) 1.48, 95% CI 0.50 to 4.35; 3 studies, 1090 participants; moderate‐certainty evidence).
No studies reported quality of life or complications associated with DPN.
Authors' conclusions
Our analysis suggests that ALA probably has little or no effect on neuropathy symptoms or adverse events at six months, and may have little or no effect on impairment at six months. All the studies were at high risk of attrition bias. Therefore, future RCTs should ensure complete follow‐up and transparent reporting of any participants missing from the analyses.
Keywords: Adult; Humans; Diabetes Mellitus, Type 2; Diabetes Mellitus, Type 2/complications; Diabetes Mellitus, Type 2/drug therapy; Diabetic Neuropathies; Diabetic Neuropathies/drug therapy; Lower Extremity; MEDLINE; Thioctic Acid; Thioctic Acid/adverse effects
Plain language summary
Is alpha‐lipoic acid (a natural antioxidant) better than no treatment or dummy treatment for nerve damage in people with diabetes?
Key messages
• We found that alpha‐lipoic acid treatment compared with placebo (dummy treatment) probably has little or no effect on the symptoms of nerve damage and may have little or no effect on impairment after six months of treatment. • There is probably little or no difference between alpha‐lipoic acid and placebo in the occurrence of unwanted effects that cause people to stop using treatment. • We found no studies to help us answer whether alpha‐lipoic acid treatment can improve quality of life or complications of nerve damage (ulceration, amputation, or both) in people with diabetes.
What is diabetic peripheral neuropathy?
People with diabetes have too much sugar in their blood because their pancreas cannot make any insulin (type 1 diabetes) or cannot make enough insulin (type 2 diabetes). Diabetes is one of the most common non‐communicable diseases (diseases not spread by infection), and it is becoming more common every year. People with both type 1 and type 2 diabetes develop complications.
High blood sugar can decrease blood flow in the blood vessels that supply the nerves, resulting in nerve damage (diabetic peripheral neuropathy). The main symptom of this condition is pain. Other symptoms include tingling, a burning sensation, numbness, shooting or sharp aches, and even extreme sensitivity to clothes touching the skin. These symptoms are caused by direct nerve damage, which is different from typical pain caused by injury or tissue damage. For this reason, usual painkiller medicines do not alleviate pain caused by peripheral neuropathy. People with this condition can also experience weakness, loss of reflexes, or loss of sensation (together known as impairment), which can disrupt normal functions such as walking.
How is diabetic peripheral neuropathy treated?
Medicines used to treat depression or epilepsy may improve symptoms of diabetic peripheral neuropathy. Some studies have suggested that alpha‐lipoic acid (an antioxidant made naturally in the body) may help because of its presumed anti‐inflammatory effects.
What did we want to find out?
We wanted to find out if alpha‐lipoic acid was better than no treatment or placebo (dummy treatment) for improving symptoms of diabetic peripheral neuropathy, impairment, quality of life, and complications of diabetic peripheral neuropathy (ulceration, amputation, or both) in people with type 1 or type 2 diabetes. We also wanted to know if alpha‐lipoic acid had any unwanted effects.
What did we do?
We searched for studies that investigated alpha‐lipoic acid treatment compared to no treatment or placebo for at least six months. We analysed and summarised the results of the trials and rated our confidence in the findings.
What did we find?
We found three studies that analysed 816 adults with type 1 and type 2 diabetes. The participants received either alpha‐lipoic acid or placebo. The dose of alpha‐lipoic acid ranged from 600 mg/day to 1800 mg/day.
Alpha‐lipoic acid compared to placebo probably has little or no effect on symptoms of diabetic peripheral neuropathy and may have little or no effect on impairment after six months of treatment. There is probably little or no difference between alpha‐lipoic acid and placebo in terms of unwanted effects that cause people to stop treatment.
No studies measured the effect of alpha‐lipoic acid treatment on quality of life or complications of peripheral neuropathy.
Until alpha‐lipoic acid is proven effective, there is no rationale for comparing it with active treatments.
What are the limitations of the evidence?
We are moderately confident in the evidence on symptoms and unwanted effects because in all three studies, the investigators lost contact with many participants before the end of treatment (loss to follow‐up). We have little confidence in the evidence on impairment, because of loss to follow‐up and because the result was very imprecise.
How up‐to‐date is this evidence?
The evidence is current to 11 September 2022.
Summary of findings
Summary of findings 1. Alpha‐lipoic acid compared to placebo for diabetic peripheral neuropathy.
| Alpha‐lipoic acid compared to placebo for diabetic peripheral neuropathy | ||||||
| Patient or population: people with DPN Setting: outpatients Intervention: ALA Comparison: placebo | ||||||
| Outcomes | Number of participants (studies) | Certainty of the evidence (GRADE) | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | Comments | |
| Risk with placebo | Risk difference with ALA | |||||
| Change in neuropathy symptoms Assessed with: TSS (0 to 14.64, lower is better) Follow‐up: 6 months | 330 (1 RCT) | ⊕⊕⊕⊝ Moderatea | — | The mean change was 3.78 points lower | MD 0.16 points lower (0.83 lower to 0.51 higher) | ALA compared to placebo probably has little or no effect on neuropathy symptoms after 6 months. The 95% CI did not contain the MCID of 0.97 points (Bastyr 2005). |
| Change in impairment Assessed with: NIS‐LL (0 to 88, lower is better) Follow‐up: 6 months | 245 (1 RCT) | ⊕⊕⊝⊝ Lowb | — | The mean change was 3.37 points lower | MD 1.02 points lower (2.93 lower to 0.89 higher) | ALA compared to placebo may have little or no effect on impairment after 6 months. However, the lower 95% CI limit surpasses the MCID of 2 points (Dyck 1991; Peripheral Nerve Society 1995), so we cannot rule out a beneficial effect. |
| Change in any validated quality of life score | — | — | — | — | — | No studies reported this outcome. |
| Complications of DPN | — | — | — | — | — | No studies reported this outcome. |
| Adverse events leading to cessation of treatment Follow‐up: 6 months | 1090 (3 RCTs) | ⊕⊕⊕⊝ Moderatec | RR 1.48 (0.50 to 4.35) | Study population | There is probably little or no difference between alpha‐lipoic acid and placebo probably results in little or no difference in adverse events at 6 months. | |
| 2 per 1000 | 1 more per 1000 (1 fewer to 7 more) | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ALA: alpha‐lipoic acid; CI: confidence interval; DPN: diabetic peripheral neuropathy; MCID: minimal clinically important difference; MD: mean difference; NIS‐LL: Neuropathy Impairment Score‐Lower Limbs RCT: randomised clinical trial; RR: risk ratio; TSS: Total Symptom Score. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded once for risk of bias (attrition bias). bDowngraded once for risk of bias (attrition bias) and once for imprecision (95% CI contains the MCID). cDowngraded once for risk of bias (attrition bias).
Background
Description of the condition
Epidemiology of diabetes mellitus and diabetic polyneuropathy
Diabetes mellitus is one of the most common non‐communicable diseases and a leading public health concern. Chronic hyperglycaemia arises from two main conditions: insufficient insulin production, known as type 1 diabetes (previously insulin‐dependent diabetes); and insulin resistance, known as type 2 diabetes (previously non‐insulin dependent diabetes; WHO 1999). As reported in the 9th edition of the International Diabetes Federation Diabetes Atlas, nearly half a billion people worldwide were living with diabetes in 2019. Projections estimate a 25% increase in prevalence by 2030 and a 51% increase by 2045 (Saeedi 2019). People with both types of diabetes can develop multisystem chronic complications, with diabetic neuropathies being the most frequent (IDF 2021; WHO 2016). These are classified clinically as either diffuse or atypical (e.g. mononeuropathies, radiculopathies, or polyradiculopathies; Pop‐Busui 2017). Both the sensorimotor and autonomic nervous systems can be affected by diffuse disease. Sensorimotor polyneuropathy disease can involve either large or small nerve fibres, is usually predominantly sensory, and is often painful (Edwards 2008).
Across the spectrum of nervous system involvement, distal symmetric polyneuropathy (referred to as diabetic peripheral neuropathy (DPN) in this review) is the most common form, accounting for up to 75% of diabetic neuropathies (Bansal 2006). The estimated prevalence in the diabetic population ranges from 8% to 54% (Feldman 2019), and the four‐year cumulative incidence ranges from 66% to 74%, increasing with age and disease duration (Pop‐Busui 2013).
DPN is a major cause of morbidity and is the primary cause of non‐traumatic amputations. It is also associated with considerable physical disability, altered quality of life, and increased mortality (Boulton 2005; Tesfaye 2011).
Regular screening for DPN signs and symptoms is crucial to identify the disease in its earliest stages and intervene promptly, preventing the development of complications (Pop‐Busui 2017).
Clinical manifestations of diabetic polyneuropathy
From a clinical perspective, DPN is defined as "the presence of symptoms and/or signs of peripheral nerve dysfunction in people with diabetes after the exclusion of other causes" (Bansal 2006; Boulton 1998). DPN may be asymptomatic and insidious at onset. It may be sensory or motor and may affect small or large fibres, or both (Bansal 2006).
The most common symptom of DPN is neuropathic pain caused by involvement of small fibres, which occurs in up to 50% of people with DPN and is the most frequent reason for seeking medical care (Bredfeldt 2015; Tesfaye 2011). Painful symptoms are varied and include tingling, burning sensations, paraesthesia, shooting or lancinating pains, aching, and allodynia, defined as pain elicited by normally innocuous stimuli, such as contact with clothing (Tesfaye 2011). Involvement of large fibres manifests as painless paraesthesia with vibration impairment, touch and pressure sensations, and loss of ankle reflex, with the possibility of sensory ataxia in advanced stages (Bansal 2006).
DPN complications are also a major threat to the general well‐being and quality of life of people with diabetes. Sensory loss, along with retinopathy and vestibular dysfunction, increases the risk of falls two‐ to three‐fold in people with versus people without DPN (Agrawal 2010). People with DPN are also seven times more likely to develop foot ulcerations (Amin 2016). This further predisposed them to active or passive soft tissue infection, which can progress to bone infection and subsequent lower extremity amputation (Kim 2013). DPN, peripheral vascular disease, and soft tissue and bone deformity are serious complications that make diabetes the leading cause of lower extremity amputation (Callaghan 2012a).
DPN symptoms are usually assessed using patient‐reported outcome measures that quantify discomfort, sleep disturbances, and quality of life (Bredfeldt 2015).
Pathophysiology of diabetic polyneuropathy
DPN primarily involves sensory and autonomic axons, and to a lesser extent, motor axons (Feldman 2019). Substantial experimental data support the idea that DPN affects the entire neuron, from the perikaryon to the distal terminals (Feldman 2019). However, the pathophysiology of DPN is not fully understood and is likely multifactorial, encompassing genetic, environmental, behavioural, metabolic, neurotrophic, and vascular factors (Chen 2013; Xu 2013). Oxidative stress, whether it arises from an overproduction of free radicals, a deficiency in antioxidant protection, or both, is believed to play a crucial role in the disease's pathogenesis (Low 1997). While good glycaemic control can lower the risk of DPN development, it is not always possible to achieve and is typically insufficient to halt the progression of DPN (Chen 2013; DCCT 1993; Duckworth 2009; Tesfaye 2011).
The pathophysiology of DPN can primarily be described as a neural dysfunction resulting from the interplay of reduced blood flow to nerves (due to hyperglycaemia) and increased oxidative stress, which induces local inflammatory reactions through reactive oxygen species (ROS; Brownlee 2005). Prolonged hyperglycaemia can activate multiple pathways simultaneously, leading to:
activation of polyol and protein kinase pathways, which leads to reduced nicotinamide adenine dinucleotide phosphate (NADPH) and subsequent depletion of glutathione and nitric oxide (Feldman 1997; Uehara 2004);
stimulation of angiogenesis via the vascular endothelial growth factor pathway;
induction of basement membrane thickening and endothelial proliferation (through transforming growth factor‐beta (TGF‐β) and nuclear factor‐kappa B (NFkB)), which cause altered capillary permeability and local hypoxia;
activation of the hexosamine pathway and diversion of fructose‐6‐phosphate from the glycolytic pathway; and
modification of gene expression for glucose transporters and glucokinase (Kolm‐Litty 1998).
Generation of ROS and advanced glycosylation end‐products activate the same NFkB pathway, which increases oxidative stress and further depletes NADPH. Oxidative stress also induces the activation of poly(adenosine diphosphate‐ribose) polymerase, resulting in further nicotinamide adenine dinucleotide depletion, a positive feedback loop activation of the protein kinase pathway, and increased inflammation (Vinik 2004). All these pathways promote mitochondrial dysfunction, leading to apoptosis, axonal degeneration, and eventual axonal death. Local proinflammatory cytokines, induced by oxidative stress, promote macrophage recruitment, leading to subsequent glial failure, myelin breakdown, and impaired nerve regeneration (Wang 2006). The overpowered antioxidant response allows the progression of a vast injury cascade initiated by ROS, which is accentuated by loss of adenosine triphosphate (ATP) production and neuronal dysfunction (Fernyhough 2015). Neuronal oxidative/nitrosative stress can also stimulate numerous downstream kinases and transcriptional factors, triggering a feed‐forward loop of injury (Stavniichuk 2014) and the release of cytokines and chemokines (Feldman 2017). Existing inflammation and immune responses are further stimulated, enhancing cellular oxidative/nitrosative stress, and leading to increased neuronal injury (Vincent 2013). These pathways primarily affect axons, while Schwann cells, exhibiting a much stronger innate antioxidant response, are at least partially protected against ROS damage (Feldman 2017).
The clinical consequences of this hyperglycaemia‐induced inflammatory and oxidative state include axonal dystrophy, decreased nerve conduction velocity, diminished neurovascular flow, and, ultimately, small and large fibre neuropathy (Edwards 2008; Feldman 2017).
Management of diabetic polyneuropathy
For the current management of DPN, there are three major treatment strategies: causal therapy (which includes lifestyle changes, intensive glucose and metabolic syndrome control, and overall cardiovascular risk reduction; DCCT 1995; Elafros 2022), pathogenesis‐oriented therapy, and symptomatic‐directed therapy (Ziegler 2021a).
DPN guidelines issued by the American Diabetes Association (Pop‐Busui 2017), International Diabetes Foundation (Ibrahim 2017), American Academy of Neurology (Price 2022), and German Diabetes Association (Ziegler 2021b) all recommend the use of tricyclic antidepressants (Lunn 2014; Saarto 2007), serotonin‐noradrenaline reuptake inhibitors (e.g. duloxetine or venlafaxine; Allen 2014), and anticonvulsants (e.g. gabapentin or pregabalin) as first‐ or second‐line treatments for painful DPN. Opioids and opioid‐like drugs (e.g. tramadol) are recommended as second‐ or third‐line treatments (Snedecor 2014; Tesfaye 2011; Ziegler 2006).
Regarding pathogenesis‐oriented therapy, recommendations are less consistent across the guidelines, primarily due to a lack of sufficient high‐quality clinical data supporting the use of medications that target the inflammatory and oxidative stress mechanisms involved in the polyol, hexosamine, protein kinase C, and advanced glycation end product pathways (Ziegler 2022). Two guidelines mention the use of alpha‐lipoic acid (ALA) to target the inflammatory pathways in DPN (Allen 2014; Ibrahim 2017; Ziegler 2021b), while others do not (Pop‐Busui 2017; Price 2022).
Description of the intervention
ALA, or thioctic acid, is a natural thiol often used as a dietary supplement. It is believed to have potent antioxidant properties and metal‐chelating functions, with capacity to regenerate endogenous antioxidants and stimulate glucose uptake (Rochette 2015). The therapeutic use of ALA has been explored in various clinical scenarios, including cardiovascular diseases and diabetic complications such as DPN. Clinical trials have used different methods of administration (intravenous or oral), different doses (from 200 mg/day to 1800 mg/day), and different durations of treatment. Recommendations for maintenance therapy indicate a daily oral dose of 600 mg (Ziegler 2022).
How the intervention might work
ALA, acting as a scavenger of ROS, possesses antioxidant properties that could potentially interrupt the oxidative stress‐inflammation pathways triggered in DPN. Thus, it could prove beneficial for both the prevention and treatment of DPN (Rochette 2015).
Early in‐vitro studies indicated that both ALA and its reduced form, dihydrolipoic acid (DHLA), are capable of scavenging ROS, including hydroxyl radicals, hypochlorous acid, and singlet oxygen (Packer 1995). In vivo studies have also suggested that ALA can mitigate oxidative stress (Marangon 1999), contribute to the restoration of endogenous cellular antioxidant levels, decrease proinflammatory pathways (Petersen 2008), and potentially facilitate the regeneration of vitamins C and E (Rochette 2015).
The potential benefits of ALA for individuals with diabetes may extend beyond its antioxidant and anti‐inflammatory effects. It might also be instrumental in restoring glucose availability, enhancing insulin‐stimulated glucose transport, and increasing non‐oxidative and oxidative glucose metabolism in insulin‐resistant muscle cells (Khanna 1999; Streeper 1997).
Why it is important to do this review
As DPN is highly prevalent among people with diabetes and is associated with considerable morbidity and quality of life impairment, it is critical to prevent and treat this condition effectively and promptly. Although ALA is frequently used for DPN, there is currently no established universal consensus on its usage (Ziegler 2022). Several published Cochrane reviews have assessed the effects of other treatments for DPN, such as aldose reductase inhibitors (Chalk 2007), Chinese herbal medicine (Chen 2013), enhanced glucose control (Callaghan 2012b), and acetyl‐L‐carnitine (Rolim 2019), but none have synthesised the evidence on ALA. If proven to be effective and safe, this drug could serve as a cost‐effective component in the long‐term management of DPN.
Objectives
To assess the effects of alpha‐lipoic acid as a disease‐modifying agent in people with diabetic peripheral neuropathy.
Methods
Criteria for considering studies for this review
Types of studies
Randomised clinical trials (RCTs) and quasi‐RCTs that compared ALA with placebo or no treatment for a minimum duration of six months were eligible for inclusion in this review. There were no restrictions on publication status or language.
Types of participants
We included studies involving adults (aged 18 years and older) with type 1 or type 2 diabetes mellitus and established DPN, regardless of participant sex or study setting. For this Cochrane review, we defined DPN as the "presence of symptoms and/or signs of peripheral nerve dysfunction in people with diabetes after excluding other causes" (Boulton 1998). DPN typically presents as a length‐dependent and symmetrical sensorimotor polyneuropathy (Tesfaye 2010). Asymptomatic neuropathy may be detected through abnormal nerve conduction tests, which provide an objective – albeit indirect – semi‐quantitative indication of the condition (Tesfaye 2010). Therefore, we included studies that used clinical or electrophysiological criteria (or both) for DPN diagnosis.
Where studies included people younger and older than 18 years, and we were unable to obtain separate data for eligible participants, we included all participants, under the assumption that age would not influence the effect of ALA on DPN.
Types of interventions
We included studies that administered ALA orally or intravenously, at any dose, for at least six months. Eligible comparators were placebo or no treatment. Studies that used co‐interventions were eligible if these interventions were equally applied across all groups.
Types of outcome measures
We included studies that measured at least one of the following outcomes.
Primary outcomes
Change in neuropathy symptoms, expressed as change in Total Symptom Score (TSS) or other validated symptom score at six months after randomisation.
Secondary outcomes
Change in neuropathy symptoms, expressed as change in TSS or other validated symptom score at six to 12 months and at 12 to 24 months after randomisation.
Change in impairment, as measured by validated metrics, at six months, six to 12 months, and 12 to 24 months after randomisation. Validated scores include the Medical Research Council (MRC) sum score, the Neuropathy Impairment Score (NIS), the Neuropathy Disability Score (NDS; an impairment score), and the Inflammatory Neuropathy Cause and Treatment (INCAT) Sensory Sum Score.
Change in any validated quality of life total score at six months after randomisation
Complications of DPN, including the number of participants with foot ulceration, amputation, or both at any stage after treatment
-
Adverse events, categorised as follows
Any adverse event
Adverse events leading to cessation of treatment
Serious adverse events (i.e. any event that was life‐threatening or required prolonged hospitalisation)
Search methods for identification of studies
Electronic searches
On 12 March 2018 and 11 September 2022, the Information Specialist of Cochrane Neuromuscular searched the following databases.
Cochrane Neuromuscular Specialised Register via the Cochrane Register of Studies (CRS‐Web; Appendix 1)
Cochrane Central Register of Controlled Trials (CENTRAL) via CRS‐Web (Issue 1, 2018 for the first search, and Issue 3, 2022 for the updated search; Appendix 2)
MEDLINE via Ovid SP (1946 to 11 September 2022; Appendix 3)
Embase via Ovid SP (1974 to Week 37 2022; Appendix 4)
In March 2018 and September 2022, we also searched the following trial registries.
US National Institutes of Health Ongoing Trials Registry ClinicalTrials.gov (clinicaltrials.gov; Appendix 5)
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; trialsearch.who.int; Appendix 6)
There were no restrictions on language, date, or status of publication.
Searching other resources
We conducted a thorough literature search by reviewing the reference lists of all included primary studies, as well as those of pertinent review articles. This was to ensure that we captured any additional references that might have been overlooked in the electronic searches. Given the comprehensiveness of our search strategy, we considered it unnecessary to reach out to individuals or organisations for further information.
Data collection and analysis
Selection of studies
Two review authors (CB and CD) independently reviewed the titles and abstracts of references identified through electronic searches (minus duplicates). We retrieved the full‐text articles of all potentially suitable studies, and another two review authors (AP and FF) independently assessed them using a standardised inclusion form. We resolved any disagreements regarding study relevance through discussion or by consulting a third review author (CB), if necessary. To avoid duplication of data, we consolidated multiple reports of the same study, ensuring that each unique study was the unit of interest. For transparency and thoroughness, we compiled a Characteristics of excluded studies table and created a PRISMA diagram (Moher 2009).
Data extraction and management
Two review authors (AP and FF) independently extracted pertinent information concerning the study design and setting, population, interventions, outcomes, sources of funding, and any declared conflicts of interest of the trial investigators, using Covidence software (Covidence). The two review authors compared their findings and resolved any disagreements through discussion. As a testament to the consistency of our process, there was no need to involve a third review author. We contacted the authors of two included studies for additional clarifications, but we received no response.
Assessment of risk of bias in included studies
Two review authors (AP and FF) independently evaluated the risk of bias of the included studies using the Cochrane risk of bias tool RoB 1, which covers the following domains (Higgins 2017).
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessors
Incomplete outcome data
Selective outcome reporting
Other potential sources of bias
For the last domain, we determined whether studies were conducted in a single centre or by a single investigator (Mallik 2014). We classified each study at low, high, or unclear risk of bias in each domain, and we populated a risk of bias table with our findings. We then provided a narrative description of the overall risk of bias for each study, based on whether any of the domains were deemed to have a high risk of bias.
Measures of treatment effect
In our analysis, we calculated mean differences (MDs) with 95% confidence intervals (CIs) for homogeneous continuous outcome measures. Where studies used different scales to measure the same outcome, we calculated the standardised mean difference (SMD) with its 95% CI. For our dichotomous outcomes (adverse events), we used risk ratios (RRs) with 95% CIs. The scales used in our analysis all had the same directional interpretation: a lower score indicated less severity of symptoms or impairment. Thus, a negative change was indicative of an improvement in symptoms or impairment.
Unit of analysis issues
All included studies were parallel‐group randomised trials.
Two trials had three arms. We combined the sample sizes, means and standard deviations (SDs) across the two treatment arms of Reljanovic 1999 using the method described in section 6.5.2.10 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022). We did not include one arm of Ziegler 1999 in any meta‐analysis, because the participants received both intravenous ALA (for the first three weeks) and oral placebo (for the remaining six months), and we could not categorise the intervention as either treatment or placebo (due to the possible residual effect of the intravenous ALA).
Had we included any studies that used no treatment as a control, we would have combined data from comparisons with placebo and no treatment groups in a single analysis.
Dealing with missing data
We recorded dropout rates and included them in the risk of bias table. For continuous data, we performed an available case analysis. When interpreting the results of the review, we considered the potential impact of missing data (Higgins 2017). If SDs were missing, we calculated them from other measures such as P values, standard errors (SEs), and the limits of CIs. This procedure ensures that all available data are utilised effectively while also accounting for the potential bias introduced by missing data.
Assessment of heterogeneity
First, we examined the trials to determine whether there were clinical reasons for heterogeneity. For assessing statistical heterogeneity across trials, we used the Chi2 test and I2 statistic. We evaluated heterogeneity in meta‐analyses with at least three studies.
Assessment of reporting biases
Had we included at least 10 studies in any meta‐analysis, we would have evaluated publication bias by creating a funnel plot and performing the Egger test (Egger 1997). We searched for unpublished trials on trial registration databases.
Data synthesis
We calculated the pooled treatment effects using the Cochrane software Review Manager 5 (RevMan 2014). We used a fixed‐effect model and performed a sensitivity analysis with the random‐effects model.
Subgroup analysis and investigation of heterogeneity
We hypothesised that response to treatment might differ according to disease duration (long‐standing DPN less likely to improve), age (older participants less likely to improve), severity of the disease, types of diabetes (as their pathogenesis is different), and the presence of pain. We also expected that the route of administration may influence bioavailability and lead to different effects.
However, we could not perform any subgroup analyses because the sample sizes were small, and the information from the included studies was insufficient.
Sensitivity analysis
We did not perform any sensitivity analysis according to risk of bias because all the studies were at high risk of bias. We did not perform a sensitivity analysis with the random‐effects model because either the outcomes included only one study, or there was no heterogeneity.
Summary of findings and assessment of the certainty of the evidence
We assessed the certainty of the evidence using the five GRADE considerations (risk of bias, inconsistency, indirectness, imprecision, and publication bias) as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022). We downgraded the certainty rating by one or two levels for limitations related to each consideration, up to a maximum of three levels for all considerations. Three review authors independently assessed the certainty of the evidence and resolved differences in opinion through discussion.
We included the following outcome measures in the summary of findings table.
Change in neuropathy symptoms at six months after randomisation
Change in impairment at six months after randomisation
Change in any validated quality of life total score at six months after randomisation
Complications of DPN
Adverse events leading to cessation of treatment
Results
Description of studies
Results of the search
Our searches identified 517 references, of which 230 were duplicates. Of the remaining 287 references, we excluded 282 based on their titles and abstracts (not RCTs or quasi‐RCTS, treatment duration shorter than six months, or control intervention other than placebo or no treatment). We assessed five full‐text articles, excluding one (Medvedeva 2006). For one of the four remaining studies, we found some discrepancies between the content of a conference abstract and the later full‐text article (El Nahas 2020). We were unable to obtain the trial data from the trialists, so we decided to list this study as awaiting classification. We included three studies in our qualitative and quantitative synthesis (Reljanovic 1999; Ziegler 1999; Ziegler 2011).
Figure 1 illustrates the study selection process in a PRISMA diagram.
1.
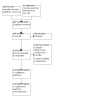
Study flow diagram.
Included studies
All three included studies were placebo‐controlled, parallel‐group RCTs. Two studies had three arms (Reljanovic 1999; Ziegler 1999), and one study had two arms (Ziegler 2011).
Two studies had two phases of treatment (Reljanovic 1999; Ziegler 1999). In Reljanovic 1999, participants in the two ALA groups (600 mg/day and 1200 mg/day) received intravenous ALA for five days and then oral ALA for 24 months. The three arms in Ziegler 1999 were intravenous ALA 600 mg/day for three weeks followed by oral ALA 1800 mg/day for six months, intravenous ALA 600 mg/day for three weeks followed by oral placebo for six months, and intravenous placebo for three weeks followed by oral placebo for six months. We did not consider data from the second arm because the treatment with ALA lasted less than six months. In Ziegler 2011, participants were randomised to oral ALA 600 mg/day or oral placebo for four years.
From the three studies, we analysed a total of 816 adults who received either ALA or placebo for at least six months. Two studies included people with type 1 or type 2 diabetes (Reljanovic 1999; Ziegler 2011), while one study included only people with type 2 diabetes (Ziegler 1999). All trial participants had symptomatic DPN as determined by clinical and electrophysiological examinations.
The age range at trial inclusion was 18 to 60 years in Reljanovic 1999, 18 to 65 years in Ziegler 1999, and 18 to 64 years in Ziegler 2011. The participants' mean age was 57.8 (SD 9.7) years in Reljanovic 1999, 56.9 (SD 6.3) years in Ziegler 1999, and 53.6 (SD 7.9 years) in Ziegler 2011.
Reljanovic 1999 had mostly female participants (56.9%), Ziegler 2011 had mostly male participants (66.5%), and the distribution of the sexes was equal in Ziegler 1999.
Two studies assessed change in symptoms, both using the TSS (Ziegler 1999; Ziegler 2011). The TSS scale ranges from 0 to 14.64 points, with higher scores indicating worse symptoms. The minimal clinically important difference (MCID) is 0.97 points (Bastyr 2005).
All studies assessed change in impairment. Ziegler 1999 and Ziegler 2011 used the NIS and the Lower Limbs subscale of the NIS (NIS‐LL), while Reljanovic 1999 used the NDS, developed by Young and colleagues (Young 1993). We decided to analyse the NIS‐LL data from Ziegler 1999 and Ziegler 2011, for three reasons. First, DPN predominantly impacts the lower limbs. Second, we combined data from Ziegler 2011 (which used the NIS/NIS‐LL) and Reljanovic 1999 (which used the NDS) in Analysis 1.4, and since the NDS focusses on the lower limbs, it is more similar to the NIS‐LL than to the NIS. Third, the intervention effects were similar for the NIS and the NIS‐LL, suggesting these scales may be interchangeable in this context. The NIS‐LL scale ranges from 0 to 88 points, with higher scores indicating more significant impairment; the MCID is considered to be 2 points (Dyck 1991; Peripheral Nerve Society 1995). The NDS ranges from 0 to 10 points, with higher scores representing worse impairment. In the analysis that combined different scales, we calculated the SMD. By distribution‐based statistical methods, the MCID is universally equivalent to 0.5 × SD (Norman 2003), which implies that 0.5 is the MCID of outcomes expressed as SMDs.
1.4. Analysis.

Comparison 1: Alpha‐lipoic acid (ALA) versus placebo, Outcome 4: Change in impairment score at 24 months
All three studies assessed adverse events.
In addition, the included studies measured nerve conduction velocities, nerve or compound muscle action potentials, the Neuropathy Symptoms and Change score, the cooling detection threshold, or the heat pain response slope.
Two studies reported glycosylated haemoglobin levels (Reljanovic 1999; Ziegler 1999).
The Characteristics of included studies table provides details of all included studies.
Excluded studies
We excluded one study during full‐text review because the duration of treatment was shorter than six months (Medvedeva 2006; see the Characteristics of excluded studies table).
Studies awaiting classification
El Nahas 2020 compared oral ALA 600 mg twice daily with placebo over six months in people with type 2 diabetes.
Risk of bias in included studies
The overall risk of bias was high for all three studies because of attrition rates ranging from 25% to 43% (Figure 2).
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All studies were multicentric and used a central computerised randomisation list. Only Ziegler 2011 specified that "a randomization list was generated by the biostatistics department of the manufacturer of the study drug, at distance of the centers the study took place", and "the random allocation was balanced using an undisclosed block size of six". Still, using the current tools, we considered all the studies at low risk of bias regarding allocation.
Blinding
We assessed the risk of bias related to blinding for each outcome separately. We considered all three studies at low risk of performance bias because they used a placebo, and because the publications indicated that participants and investigators were blinded. The level of detail on randomisation and blinding procedures in these studies is consistent with the standards of that period.
We judged all three studies at low risk of detection bias, as all investigators were blinded to treatment allocation. Ziegler 2011 clearly stated that assessors were blinded, and procedures were in place to decode the individual blinded treatment if necessary. In Ziegler 1999, specific additives in the placebo made it similar in appearance to the active medication.
Although all studies had symptom‐based scores as the primary outcome, they were probably assessed objectively.
Incomplete outcome data
We judged all three studies at high risk of attrition bias.
In Reljanovic 1999, although the study initially included 299 participants in an intention‐to‐treat (ITT) analysis as stated in the protocol, a high attrition rate of 43% (130 participants) was allowed. Furthermore, many participants with outlying electrophysiological results were excluded from the analysis, so that only 65 participants' results were presented.
In Ziegler 1999, although data were presented for the primary outcome (change in TSS) at seven months in an ITT analysis for 503/516 randomised participants, the study authors mentioned a 25% withdrawal rate across all groups and provided no explanation regarding the handling of missing data. Additionally, for the secondary outcomes, data were analysed for only a subset of participants (364 for NIS and 368 for NIS‐LL) without any explanation.
In Ziegler 2011, while only 6/460 randomised participants were excluded from the analysis, there were high discontinuation rates of 41% in the treatment arm and 42% in the placebo arm over the four‐year study period. The publication did not mention how many outcome measurements were based on the last observation carried forward (LOCF) method ("mean of weeks 191 and 192 or last available value after randomization"). Even in the best‐case scenario of conducting an ITT analysis with complete outcome data, the high attrition rates would have likely diluted the potential benefits of ALA, resulting in insufficient statistical power to detect any effect.
Selective reporting
We judged all three studies at low risk of reporting bias.
Reljanovic 1999 aimed to investigate changes in various outcomes related to neuropathy. The publication reported all specified outcomes at the designated time points. Ziegler 1999 focused on measuring changes in TSS and NIS at specific time intervals. Results for these outcomes were reported as initially proposed. Although we could not access the protocols for Reljanovic 1999 or Ziegler 1999, the reported outcomes in these studies align with those typically examined in DPN treatment studies.
Ziegler 2011 had a registered study protocol and reported the results of all prespecified outcomes at both the two‐ and four‐year time points. The publication reported some additional outcomes that were not prespecified in the study protocol, but none were included in our review.
Other potential sources of bias
We found no other sources of bias for any study. Pharmaceutical companies sponsored all studies, but we did not consider this a source of bias. All studies were multicentric and had multiple investigators.
Effects of interventions
See: Table 1
Alpha‐lipoic acid versus placebo
Primary outcome
Change in neuropathy symptoms at six months
Only Ziegler 1999 reported change in neuropathy symptoms at six months. ALA compared with placebo probably has little or no effect on neuropathy symptoms as assessed by TSS at six months (MD −0.16 points, 95% CI −0.83 to 0.51; 330 participants; moderate‐certainty evidence; Analysis 1.1). The 95% CI was narrow and did not contain the MCID. We downgraded the certainty of the evidence by one level for attrition bias.
1.1. Analysis.

Comparison 1: Alpha‐lipoic acid (ALA) versus placebo, Outcome 1: Change in validated symptom score at 6 months
Secondary outcomes
Change in neuropathy symptoms at six to 12 months and 12 to 24 months
Only Ziegler 2011 reported change in neuropathy symptoms beyond six months (at 24 months). ALA compared with placebo probably has little or no effect on neuropathy symptoms as assessed by TSS at 24 months (MD −0.23 points, 95% CI −0.67 to 0.21; 421 participants; moderate‐certainty evidence; Analysis 1.2). The 95% CI was narrow and did not contain the MCID. We downgraded the certainty of the evidence by one level for attrition bias.
1.2. Analysis.

Comparison 1: Alpha‐lipoic acid (ALA) versus placebo, Outcome 2: Change in validated symptom score at 24 months
Change in impairment at six months, six to 12 months, and 12 to 24 months
One study assessed impairment at six months using the NIS‐LL (Ziegler 1999). Two studies assessed impairment at 24 months; Reljanovic 1999 used the NDS and Ziegler 2011 used the NIS‐LL.
ALA compared with placebo may have little or no effect on impairment as measured by the NIS‐LL at six months (MD −1.02 points, 95% CI −2.93 to 0.89 points; 1 study, 245 participants; low‐certainty evidence; Analysis 1.3). We downgraded the certainty of the evidence by one level for attrition bias and by one level for imprecision. The lower limit of the 95% CI surpasses the MCID (2 points), so we cannot rule out a beneficial effect.
1.3. Analysis.

Comparison 1: Alpha‐lipoic acid (ALA) versus placebo, Outcome 3: Change in impairment score at 6 months
ALA compared with placebo probably has little or no effect on impairment at 24 months (SMD −0.07 SDs, 95% CI −0.24 to 0.11; I2 = 0%, P = 0.39; 2 studies, 486 participants; moderate‐certainty evidence; Analysis 1.4). We downgraded the certainty of the evidence by one level for attrition bias. The 95% CIs did not include the statistical MCID (0.5), which means the possibility of a clinically significant difference is very low.
Change in any validated quality of life total score at six months
No studies reported quality of life.
Complications of diabetic peripheral neuropathy
No studies reported complications of DPN.
Adverse events
All three studies reported adverse events leading to cessation of treatment. There is probably little or no difference between ALA and placebo in the risk of adverse events leading to cessation of treatment (RR 1.48, 95% CI 0.50 to 4.35; I2 = 0, P = 0.69; 3 studies, 1090 participants; moderate‐certainty evidence; Analysis 1.5). The number of participants forReljanovic 1999 should have been the 169 participants who completed the 24 months of follow‐up rather than the 65 analysed for the other outcomes. However, the whole cohort was included in the adverse events analysis. We downgraded the certainty of the evidence by one level for attrition bias.
1.5. Analysis.

Comparison 1: Alpha‐lipoic acid (ALA) versus placebo, Outcome 5: Adverse events leading to cessation of treatment
No studies recorded all types of adverse event or serious adverse events.
Discussion
Summary of main results
This review included three studies with a total of 1089 participants. From the three studies, we analysed 816 adults who received either ALA or placebo for at least six months.
All three studies were prospective, double‐blind, placebo‐controlled RCTs with parallel‐group design. Two studies (395 participants) had a three‐arm protocol, and one study (421 participants) had two arms. The studies used different doses of ALA; the minimum dose was 600 mg once daily. Two studies had an initial intravenous regimen of ALA versus placebo for up to three weeks, followed by an oral regimen of ALA versus placebo for up to 24 months. Two studies included both type 1 and type 2 diabetes, and one study included only type 2 diabetes.
ALA 600 mg three times daily compared to placebo probably has little or no effect on neuropathy symptoms after six months, and ALA 600 mg once daily compared to placebo probably has little or no effect on neuropathy symptoms after 24 months. We identified only one study for each time frame. The certainty of the evidence for both outcomes was moderate (downgraded for attrition bias).
ALA 600 mg once daily compared to placebo may have little or no effect on impairment after six months; however, the 95% CI was wide and included the MCID of the NIS‐LL. Only one study reported this outcome. The certainty of the evidence was low (downgraded for attrition bias and imprecision).
Two studies assessed impairment at 24 months using different scales: the NIS‐LL and the NDS. Neither study found a clinically significant improvement with ALA. The certainty of the evidence was moderate (downgraded for attrition bias).
We planned to evaluate the impact of ALA treatment on quality of life and the progression of DPN to foot ulceration, amputation, or both. However, no studies reported these outcomes.
All three studies reported adverse events. Data from 1090 participants indicated little or no difference between ALA and placebo in adverse events leading to the cessation of treatment at six months after randomisation. The certainty of the evidence was moderate (downgraded for attrition bias).
Overall completeness and applicability of evidence
We included only three studies assessing the benefits and harms of long‐term treatment (more than six months) of DPN with ALA compared to placebo, because most existing studies have a much shorter treatment time. Although all the studies were randomised and double‐blinded and included people of both sexes with a wide age interval (18 to 65 years) from multiple centres, different outcomes of interest were reported in only one or two studies.
We found data for symptom improvement, impairment, and adverse events. We did not assess the impact of ALA treatment on quality of life because no studies used a validated quality of life tool. In addition, no studies reported the occurrence of complications (foot ulceration, amputation, or both).
A notable limitation arises from the inconsistent reporting of outcomes across studies, as well as the different time frames the study authors selected for their analysis. This may have reduced the robustness of our conclusions. Only one study reported our primary outcome (change in neuropathy symptoms at six months), while another study reported change in neuropathy symptoms at 24 months. Similarly, one study reported our secondary outcome change in impairment at six months (using the NIS‐LL), while two studies reported change in impairment at 24 months (using the NIS‐LL and NDS). Concerning harm, the studies only provided data for adverse events leading to treatment cessation, but not all types of adverse events or serious adverse events.
The doses of ALA varied from 600 mg per day to 1800 mg per day, and the route of administration was either oral or intravenous followed by oral. We were unable to perform any subgroup analyses to determine whether the response to treatment varied according to factors like type of diabetes, duration or severity of the disease, age, or route of administration.
Quality of the evidence
Using the GRADE approach, we rated the certainty of evidence as moderate for the primary outcome (change in symptoms at six months) and for all secondary outcomes except change in impairment at six months, which we rated as low.
We downgraded the certainty of evidence for all outcomes because of attrition bias. Ziegler 1999 had an attrition rate of 25%. Ziegler 2011 mentions an attrition rate of 41% for the treatment group and 42% for the placebo groups during the four‐year study period; the study authors performed an ITT analysis at 24 months, but did not report the discontinuation status at that time. Reljanovic 1999 started with 299 participants but presented results for only 65 participants.
We also downgraded the certainty of the evidence for change in impairment because of imprecision, because the CI was very wide and contained the MCID.
Overall, we assume that the quality of the included studies limits the robustness of our conclusions.
Potential biases in the review process
This review is the first to cover ALA in diabetic neuropathy for a more extended period (at least six months). The review team is mixed, with three members new to the Cochrane review methodology and two experienced members. We received help with the search strategy from a Cochrane expert. This should, in our opinion, minimise selection risk.
We consider that the review questions are clearly stated and should not induce bias in the study selection process. They were predefined in the published Cochrane protocol and presented following the Cochrane Handbook for Systematic Reviews of Interventions and PRISMA. All predefined outcomes from the review protocol are discussed in the review.
We selected outcomes that answer patient‐relevant questions following PICO recommendations. We included subjective, patient‐reported outcomes (symptom scores) influencing the quality of life. No studies reported objective outcomes like complications (ulcerations or amputations, or both), and this could lead to potential bias in study synthesis.
The selection criteria excluded many trials, mainly because of their duration (a few weeks in most cases). We consider that this selection process induces no bias since outcomes of DPN should focus on the long‐term evolution to be clinically meaningful, and the agreement between the review authors concerning the selection of the studies was high.
We identified one study that had identical results to a previous conference paper except for the stated time of development of the study (El Nahas 2020). We contacted the study authors and the publisher for clarification, but the study authors refused to share the study data, so we listed the study as awaiting classification. We felt that this action would not induce any bias.
As with all reviews that include few trials, ours could lack sensitivity for events with infrequent occurrence, such as adverse events.
Agreements and disagreements with other studies or reviews
We identified several published systematic reviews reporting the effect of ALA on DPN.
Han 2012 conducted a similar meta‐analysis that included studies from Chinese biological medicine alongside CENTRAL, MEDLINE, and Embase. The intervention was intravenous ALA. Their primary outcomes were 'benefit', median motor and sensory conduction velocities, and peroneal nerve sensory and motor conduction velocities. Secondary outcomes included the occurrence of adverse events. Of 138 studies screened, the authors of Han 2012 retrieved 24 full‐text articles (18 in Chinese and six in English) and included 15 studies (all in Chinese). The intervention in all 15 studies was ALA combined with another treatment (methylcobalamin in eight studies, prostaglandins in four, vitamin B1 in one, cilostazol in one, and gingko leaves injection in one). The duration of the intervention ranged from 14 days to 28 days, with a mean of 21 days. There was significant heterogeneity for each of the outcomes presented. The stated limitations were related to the overall poor methodology of the included trials, most of which did not provide details of the study design, randomisation, or allocation. Although the authors of Han 2012 stated that rigorous studies are needed, they concluded that short‐term ALA treatment is generally safe and can improve both symptoms and nerve conduction speeds. No studies included in Han 2012 met our inclusion criteria because of the short duration of the interventions.
Another published review evaluated intravenous ALA treatment (minimum three weeks) and included only studies from the German VIATRIS repository (Ziegler 2004). Like Han 2012, Ziegler 2004 concluded that intravenous ALA is effective for improving symptoms and nerve conduction speeds.
We identified only one systematic review published since 2020 that evaluated ALA for DPN (Abubaker 2022). Secondary outcomes included adverse effects of the interventions. There were no inclusion criteria regarding length of treatment, but the included studies had to evaluate standalone ALA treatment and report pain or symptom scores. Eight studies were included, totalling 1500 participants. Two of the included studies were also in our review (Reljanovic 1999; Ziegler 1999), and one was the study we listed as awaiting classification (El Nahas 2020). Of the four remaining studies, one evaluated ALA in fibromyalgia and not in DPN (Gilron 2021). The authors of Abubaker 2022 considered all the studies to be of "high quality", stating as their risk of bias assessment tool the Critical Appraisal Skills Programme (CASP) appraisal tool. They concluded that ALA is safe and tolerable and may reduce symptoms, but that there is limited evidence to support its efficacy. The results of our review also suggest that ALA is safe, but we found no convincing evidence of a beneficial effect. In addition, we considered the studies included in our review to be at high overall risk of bias.
Authors' conclusions
Implications for practice.
For patients
Treatment with alpha‐lipoic acid (ALA) probably has little or no effect on neuropathy symptoms after six months of therapy or on functional impairment after 24 months of therapy in people with diabetic peripheral neuropathy (DPN). ALA may have little or no effect on functional impairment after six months of therapy. ALA probably has no adverse effects that would lead to treatment cessation within six months.
We found no studies assessing the impact of ALA treatment on quality of life or on the complications of DPN (foot ulceration, amputation, or both).
For clinicians
There was moderate‐certainty evidence from one study that ALA treatment has little or no effect on DPN symptoms (Total Symptom Score; TSS) after six months of treatment, and moderate‐certainty evidence from another study that ALA treatment has little or no effect on DPN symptoms (TSS) after 24 months of treatment.
There was low‐certainty evidence from one study that ALA treatment compared with placebo has little or no effect on impairment assessed by the Neuropathy Impairment Score‐Lower Limbs (NIS‐LL) after six months of treatment. There was moderate‐certainty evidence from two studies using different scales (NIS‐LL and Neuropathy Disability Score) that ALA treatment compared with placebo has little or no effect on impairment after 24 months of treatment.
There were no data on the impact of ALA treatment on quality of life or DPN complications (foot ulceration, amputation, or both).
There was moderate‐certainty evidence from three studies of little or no difference between ALA and placebo in terms of adverse events that would lead to cessation of treatment after six months.
For policymakers and funders
There is moderate‐certainty data that ALA has little or no effect on symptoms of DPN.
There is low‐ and moderate‐certainty data that ALA has little or no effect on impairment.
There are no data on the effect of ALA on quality of life or DPN complications.
Implications for research.
We found only three randomised clinical trials assessing the efficacy of long‐term treatment (more than six months) of DPN with ALA compared to placebo. All were at high risk of attrition bias; therefore, future RCTs should ensure complete follow‐up and transparent reporting of any participants missing in the analyses. Studies should also measure symptoms, impairment, and quality of life using validated scales. Other important outcomes are complications of DPN (foot ulceration, amputation, or both) and adverse effects.
Intensive glycaemic control is considered the primary approach for preventing DPN, and haemoglobin A1C (HbA1C) is widely recognised as the most reliable biomarker for assessing glycaemic control. It is important to note that ALA is not expected to directly affect HbA1C levels, and only limited evidence suggests its potential as an insulin sensitiser. In the included studies, no significant variation was observed in HbA1C levels between baseline and end of follow‐up in the intervention or control groups. However, future studies may assess the role of glycaemic control as a modifier of the potential effect of ALA.
Until ALA is proven effective, there is no rationale for comparing it with active treatments.
History
Protocol first published: Issue 2, 2018
Acknowledgements
The Information Specialist of Cochrane Neuromuscular, Angela Gunn, developed the search strategy in consultation with the review authors, while Farhad Shokraneh performed the latest search.
The Methods section of the review protocol is based on a template developed by Cochrane Neuromuscular from an original created by the Cochrane Airways Group (Baicus 2018).
This project was supported by the UK National Institute for Health and Care Research (NIHR) via Cochrane Infrastructure funding to Cochrane Neuromuscular until 31 March 2023. The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the Evidence Synthesis Programme, the NIHR, the UK National Health Service (NHS), or the Department of Health and Social Care. Cochrane Neuromuscular was also supported by the MRC Centre for Neuromuscular Disease.
Editorial and peer‐reviewer contributions
The following people conducted the editorial process for this article.
Sign‐off Editor (final editorial decision): Colin Chalk, Department of Neurology & Neurosurgery, McGill University, Montreal, Canada
Managing Editor (selected peer reviewers, provided editorial guidance to authors, edited the article): Luisa M Fernandez Mauleffinch, Cochrane Central Editorial Service
Editorial Assistant (conducted editorial policy checks, collated peer‐reviewer comments and supported editorial team): Lisa Wydrzynski, Cochrane Central Editorial Service
Copy Editor (copy editing and production): Julia Turner, Cochrane Central Production Service
Peer‐reviewers (provided comments and recommended an editorial decision): Jennifer Hilgart, Cochrane (methods); Douglas M Salzwedel, Information Specialist, Cochrane Hypertension (search); Robert Wyllie (consumer); Professor Richard Hughes, King's College London (clinical). Two additional peer reviewers provided clinical peer review but chose not to be publicly acknowledged.
Appendices
Appendix 1. Cochrane Neuromuscular Specialised Register (CRS‐Web) search strategy
1 MESH DESCRIPTOR Diabetes Mellitus EXPLODE ALL AND INREGISTER 798
2 (diabet*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 1524
3 #1 OR #2 1524
4 MESH DESCRIPTOR Peripheral Nervous System Diseases EXPLODE ALL AND INREGISTER 2070
5 (neuropath* or polyneuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 2489
6 #4 OR #5 3466
7 #3 AND #6 1292
8 MESH DESCRIPTOR Thioctic Acid EXPLODE ALL AND INREGISTER 53
9 ("lipoic acid" or "alpha lipoic" or thioctic):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 62
10 #8 OR #9 87
11 #7 AND #10 49
Appendix 2. Cochrane Central Register of Controlled Trials (CRS‐Web) search strategy
1 MESH DESCRIPTOR Diabetes Mellitus EXPLODE ALL AND CENTRAL:TARGET 35204
2 (diabet*):AB,EH,EMT,KW,KY,MH,TI AND CENTRAL:TARGET 103341
3 #1 OR #2 103631
4 MESH DESCRIPTOR Peripheral Nervous System Diseases EXPLODE ALL AND CENTRAL:TARGET 6098
5 (neuropath* or polyneuropath*):AB,EH,EMT,KW,KY,MH,TI AND CENTRAL:TARGET 16341
6 #4 OR #5 19187
7 #3 AND #6 5026
8 MESH DESCRIPTOR Thioctic Acid EXPLODE ALL AND CENTRAL:TARGET 2278
9 ("lipoic acid" or "alpha lipoic" or thioctic):AB,EH,EMT,KW,KY,MH,TI AND CENTRAL:TARGET 832
10 #8 OR #9 2756
11 #7 AND #10 155
12 12/03/2018_TO_27/03/2022:CRSINCENTRAL AND CENTRAL:TARGET 815714
13 #11 AND #12 62
Appendix 3. MEDLINE (Ovid SP) search strategy
Database: Ovid MEDLINE(R) ALL <1946 to March 25, 2022>
1 ((Randomized Controlled Trial or Controlled Clinical Trial).pt. or (Randomi?ed or Placebo or Randomly or Trial or Groups).ab. or Drug Therapy.fs.) not (exp Animals/ not Humans.sh.) (4628636)
2 ((exp Diabetes Mellitus/ or diabet*.mp.) and (exp Peripheral Nervous System Diseases/ or (neuropath* or polyneuropath*).mp.)) or Diabetic Neuropathies/ (31081)
3 Thioctic Acid/ or (lipoic acid or alpha lipoic or thioctic).mp. (6501)
4 1 and 2 and 3 (222)
5 limit 4 to ed=20180309‐20221231 (31)
6 limit 4 to dt=20180309‐20221231 (40)
7 5 or 6 (45)
Appendix 4. Embase (Ovid SP) search strategy
Database: Embase <1974 to 2022 Week 12>
1 ((crossover‐procedure or double‐blind procedure or single‐blind procedure or randomized controlled trial).sh. or (random* or crossover* or cross over* or placebo* or (doubl* adj blind*) or allocat*).tw,ot. or trial.ti. or controlled clinical trial/) not ((exp animal/ or exp invertebrate/ or animal.hw. or non human/ or nonhuman/) not (human/ or human cell/ or human tissue/ or normal human/)) (2125573)
2 limit 1 to (conference abstracts or embase) (1782354)
3 (exp diabetes mellitus/ or diabet*.mp.) and (peripheral neuropathy/ or (neuropath* or polyneuropath*).mp.) (57802)
4 thioctic acid/ or (lipoic acid or alpha lipoic or thioctic).mp. (10191)
5 2 and 3 and 4 (180)
6 limit 5 to dc=20180310‐20221231 (40)
Appendix 5. ClinicalTrials.gov search strategy
Condition or disease: Diabetic Neuropathy OR Diabetic Polyneuropathy OR Diabetic Peripheral Neuropathy OR Diabetic Peripheral Polyneuropathy
Study type: Interventional Studies (Clinical Trials)
Intervention/treatment: Thioctic OR Lipoic
13 Studies found
Appendix 6. WHO ICTRP
(Diabetic Neuropathy OR Diabetic Polyneuropathy OR Diabetic Peripheral Neuropathy OR Diabetic Peripheral Polyneuropathy) AND (Thioctic OR Lipoic)
19 records for 19 trials
Data and analyses
Comparison 1. Alpha‐lipoic acid (ALA) versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Change in validated symptom score at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2 Change in validated symptom score at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3 Change in impairment score at 6 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.4 Change in impairment score at 24 months | 2 | 486 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.24, 0.11] |
| 1.5 Adverse events leading to cessation of treatment | 3 | 1090 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.50, 4.35] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Reljanovic 1999.
| Study characteristics | ||
| Methods | Prospective, double‐blind, multicentre, 3‐arm parallel‐group, randomised study | |
| Participants |
Number: 299 randomised, 65 analysed Age: mean 57.8 (SD 9.7) years Sex: 56.9% women Inclusion criteria
|
|
| Interventions |
EG1: ALA 600 mg/day, IV administration (with trometamol salt solution) for 5 days followed by oral administration for a total of 24 months EG2: ALA 1200 mg/day, IV administration (with trometamol salt solution) for 5 days followed by oral administration for a total of 24 months CG: placebo |
|
| Outcomes |
Primary outcomes
Secondary outcomes
|
|
| Funding | Grants from ASTA Medica AG, Frankfurt am Main, Germany | |
| Conflicts of interest | ALA tablets (Thioctacid®) were manufactured by ASTA Medica AG, Frankfurt am Main, Germany. | |
| Notes | 299 people were recruited from 32 outpatient centres, but 130 participants were lost for different reasons. From the 169 participants who completed the 24 months' follow‐up, another 104 were excluded because of flaws in the electrophysiological assessment, so the analysis included only 65 participants. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "... patients with symptomatic polyneuropathy were randomly assigned to TA 1200, TA 600 or PLA according to their entry sequence following a central computerized randomization list." |
| Allocation concealment (selection bias) | Low risk | Quote: "... patients with symptomatic polyneuropathy were randomly assigned to TA 1200, TA 600 or PLA according to their entry sequence following a central computerized randomization list." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Both PLA tablets and solutions contained ingredients identical with those containing TA except for the latter. In order to achieve a color similar to the active drug ferrooxide (E 172) was added to the tablets and 0.03 mg of riboflavin to the ampoules." Comment: trial described as double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Trial described as double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | High risk | As treated analysis with substantial departure from randomisation: 299 patients included, 64 analysed. |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the published report includes all expected outcomes. |
| Other bias | Low risk | We found no other sources of bias. |
Ziegler 1999.
| Study characteristics | ||
| Methods | Prospective, double‐blind, placebo‐controlled, multicentre, 3‐arm parallel‐group, randomised study | |
| Participants |
Number: 516 randomised, 503 analysed in the 3 groups (330 participants analysed in the 2 groups of interest, comparing ALA with placebo) Age: 56.9 (SD 6.3) years Sex: 52.1% women Inclusion criteria
|
|
| Interventions |
EG1: ALA 600 mg IV once daily for 3 weeks followed by ALA 1800 mg daily (3 600‐mg tablets) for 6 months EG2: ALA 600 mg IV once daily for 3 weeks followed by oral placebo 3 times daily for 6 months (we did not include this group in our review, as it did not fulfil the inclusion criteria concerning duration of treatment) CG: placebo IV administration once daily for 3 weeks followed by oral placebo 3 times daily for 6 months |
|
| Outcomes |
Primary outcomes
Secondary outcomes
|
|
| Funding | "This study was supported by ASTA Medica AG, Frankfurt am Main, Germany" | |
| Conflicts of interest | The trometamol salt solution and the tablets containing 600 mg of ALA were manufactured by ASTA Medica AG, Frankfurt am Main, Germany. | |
| Notes | Of the 516 randomised participants, 7 participants from 1 centre were not exposed to treatment, and no efficacy data were available for 6 other participants. Therefore 503 participants were included in the ITT analysis. 34 participants dropped out during the IV treatment period because of lack of efficacy (2; EG1/EG2/CG: 1/1/0), drug intolerance (2: 0/0/2), intercurrent disease (6: 1/1/4), exclusion criteria (19: 7/7/5), noncompliance (5: 1/4/0) and other reasons (7: 2/3/2). 92 participants dropped out during the oral treatment period because of lack of efficacy (24: 8/11/5), drug intolerance (9: 4/1/4), intercurrent disease (15: 4/5/6), exclusion criteria (11: 3/6/2), noncompliance (28: 8/11/9) and other reasons (17: 9/5/3). The total rate of withdrawal was 25% throughout the trial, without significant differences between the 3 studied groups. There were 24 protocol violations. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Each patient was randomized according to his or her entry sequence following a central computerized randomization list." |
| Allocation concealment (selection bias) | Low risk | Quote: "Each patient was randomized according to his or her entry sequence following a central computerized randomization list." Comment: the measures for concealment are not fully described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "During the oral phase, tablets containing 600 mg a‐lipoic acid or placebo of identical size, appearance, and taste were used. All investigators and participants were blinded to the randomization of the study drug assignments." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "During the oral phase, tablets containing 600 mg a‐lipoic acid or placebo of identical size, appearance, and taste were used. All investigators and participants were blinded to the randomization of the study drug assignments." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition and exclusions reported in each interventional group; total withdrawal rate of 25% during the trial, equal in the 3 arms of the study. For the primary outcome (change in TSS), 503/516 participants were included in the ITT analysis, but there was no mention of missing data or how the study authors dealt with them. For the secondary outcomes (change in NIS and NIS‐LL) the study authors analysed data of only 364 participants (NIS) and 368 participants (NIS‐LL), without any explanation. Therefore, we consider a high risk of attrition bias for NIS and NIS‐LL and an unclear risk of attrition bias for TSS. |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the published report includes all expected outcomes. |
| Other bias | Low risk | We found no other sources of bias. |
Ziegler 2011.
| Study characteristics | ||
| Methods | Prospective, double‐blind, placebo‐controlled, multicentre, 2‐arm 1:1 allocation ratio, parallel‐group, randomised study | |
| Participants |
Number: 460 randomised, 421 analysed Age: 53.6 (SD 7.9) years Sex: 33.5% women Inclusion criteria
|
|
| Interventions |
EG: oral administration once daily of ALA 600 mg (film‐coated tablets) for 4 years CG: oral placebo tablets once daily for 4 years "The trial consisted of a 2‐week screening phase, 6‐week placebo run‐in phase, 4‐year double‐blind phase, and 4‐week washout phase." |
|
| Outcomes |
Primary outcomes
Secondary outcomes
|
|
| Funding | No funding source is mentioned. However, MEDA Pharma produced the medication, its Biostatistics department generated the randomisation list, 5 study authors received honoraria/grants from MEDA Pharma, and the other 3 authors were employees of MEDA Pharma. | |
| Conflicts of interest | 5 study authors received honoraria or grants from, and 3 authors were employees of the manufacturer of the study drug. | |
| Notes | 879 people were assessed for eligibility, of whom 419 were excluded (353 did not meet the inclusion criteria and 91 met the exclusion criteria). 460 participants were randomised: 233 were randomised to ALA (of whom 231 received ALA) and 227 were randomised to placebo, (of whom 225 received placebo). More than 40% of the participants from each group discontinued treatment/placebo. Results for all outcomes at 2 years from randomisation were reported for 421 participants (214 in the ALA group and 207 in the placebo group). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a randomization list was generated by the biostatistics department of the manufacturer of the study drug ..." |
| Allocation concealment (selection bias) | Low risk | Quote: "a randomization list was generated by the biostatistics department of the manufacturer of the study drug, at distance of the centers the study took place"; "the random allocation was balanced using an undisclosed block size of six." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "... matching placebo tablets with increased amounts of cellulose and lactose that were identical in
appearance." Comment: trial described as double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The investigators and the monitor received sealed envelopes to enable decoding the individual blinded treatment in case of emergency." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 40% of participants discontinued intervention in both groups during the 4‐year study. We do not know how many participants were lost before the outcomes at 2 years (our outcome of interest), and how many after the first 2 years. Most participants (454/460) were included in the ITT analysis, but the study authors did not report for how many they managed to measure the outcome, and for how many they used the last observation carried forward ("mean of weeks 191 and 192 or last available value after randomization"). Apparently, the proportion of dropouts and the causes of dropout were equally distributed among the 2 groups. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported (ClinicalTrials.gov ID NCT00977483). The publication also reported outcomes that were not prespecified, which were the only outcomes with statistically significant results. However, these added outcomes were not among the outcomes of our systematic review. |
| Other bias | Low risk | We identified no other sources of bias. |
ALA: alpha‐lipoic acid; CG: control group; DPN: diabetic peripheral neuropathy; EG: experimental group; ITT: intention‐to‐treat; IV: intravenous; NDS: Neuropathy Disability Score; NIS: Neuropathy Impairment Score; NIS‐LL: Neuropathy Impairment Score‐Lower Limbs; SD: standard deviation; TSS: Total Symptom Score.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Medvedeva 2006 | The duration of the intervention and follow‐up was 10 days, not compatible with our inclusion criteria. |
Characteristics of studies awaiting classification [ordered by study ID]
El Nahas 2020.
| Methods | Prospective, double‐blind, placebo‐controlled, double‐arm randomised study |
| Participants | 200 people with type 2 diabetes and symptomatic peripheral neuropathy |
| Interventions |
EG: ALA 600 mg twice daily for 6 months CG: placebo for 6 months |
| Outcomes |
Primary outcomes
Secondary outcomes
|
| Notes |
ALA: alpha‐lipoic acid; CG: control group; EG: experimental group; NDS: Neuropathy Disability Score; VAS: visual analogue scale.
Differences between protocol and review
See Baicus 2018 (protocol).
For consistency with other outcomes, we changed the label of the primary outcome from 'Improvement in neuropathy symptoms' to 'Change in neuropathy symptoms'.
For the secondary outcome 'Change in impairment', one validated scale mentioned in the protocol was the Neuropathy Impairment Score (NIS; Baicus 2018). Two included studies used both the NIS and its subscale Neuropathy Impairment Score‐Lower Limbs (NIS‐LL; Ziegler 1999; Ziegler 2011), and we chose to use NIS‐LL because: 1) diabetic peripheral neuropathy mainly affects lower limbs; 2) for Analysis 1.4, we meta‐analysed NIS‐LL score with another impairment score, the Neuropathy Disability Score (NDS; Young 1993), which also refers only to lower limbs; and 3) the effects of interventions were similar for both NIS and NIS‐LL (Ziegler 1999; Ziegler 2011).
In the summary of findings table, we included 'Adverse events leading to cessation of treatment' instead of 'Any adverse event' because the included studies reported the more specific harms outcome.
We were unable to perform the planned subgroup analysis, because the sample sizes were small, and the information from the included studies was insufficient.
Contributions of authors
CB, CD, FF, AP and EvE conceived the review. CB, CD, FF, AP and EvE designed the review. CB and EvE co‐ordinated the review. CB and CD collected the data for the review. CD and CB screened the search results. AP and FF performed the full‐text review and CB resolved any discrepancies. CD and CB extracted data from papers. CB wrote to the authors of the papers for additional information. CD obtained and screened data on unpublished studies. CB managed data for the review. CB, CD, FF, and AP entered data into RevMan. CB performed the data analysis. CB, EvE, and FF interpreted the data. FF and AP evaluated the risk of bias, and CB and EvE resolved discrepancies. CB and EvE provided a methodological perspective. CB, CD, FF, and AP provided a clinical perspective. CB, CD, FF, and AP wrote the review. EvE provided general advice on the review. CB, CD, FF, AP, and EvE created the protocol on which the current review is based.
Sources of support
Internal sources
-
None, Other
None
External sources
-
None, Other
None
Declarations of interest
CB: none known. AP: none known. EvE: none known. CD: none known. FLF: none known.
New
References
References to studies included in this review
Reljanovic 1999 {published data only}
- Reljanovic M, Reichel G, Rett K, Lobisch M, Schuette K, Moller W, et al. Treatment of diabetic polyneuropathy with the antioxidant thioctic acid (alpha-lipoic acid): a two year multicenter randomized double-blind placebo-controlled trial (ALADIN II). Free Radical Research 1999;31(3):171-9. [DOI: 10.1080/10715769900300721] [DOI] [PubMed] [Google Scholar]
Ziegler 1999 {published data only}
- Ziegler D, Hanefeld M, Ruhnau KJ, Hasche H, Lobisch M, Schütte K, et al. Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a 7-month multicenter randomized controlled trial (ALADIN III Study). ALADIN III Study Group. Alpha-Lipoic Acid in Diabetic Neuropathy. Diabetes Care 1999;22(8):1296-301. [DOI: 10.2337/diacare.22.8.1296] [DOI] [PubMed] [Google Scholar]
Ziegler 2011 {published data only}
- Ziegler D, Low PA, Litchy WJ, Boulton AJ, Vinik AI, Freeman R, et al. Efficacy and safety of antioxidant treatment with α-lipoic acid over 4 years in diabetic polyneuropathy: the NATHAN 1 trial. Diabetes Care 2011;34(9):2054-60. [DOI: 10.2337/dc11-0503] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Medvedeva 2006 {published data only}
- Medvedeva LA, Gnezdilov AV, Zagorul'ko OI, Syrovegin AV, Samoilova NV, Slashchuk IuI. Neurometabolic therapy of diabetic neuropathy. Zhurnal nevrologii i psikhiatrii imeni S.S. Korsakova / Ministerstvo zdravookhraneniia i meditsinskoi promyshlennosti Rossiiskoi Federatsii, Vserossiiskoe obshchestvo nevrologov [i] Vserossiiskoe obshchestvo psikhiatrov 2006;203:71-3. [PubMed] [Google Scholar]
References to studies awaiting assessment
El Nahas 2020 {published data only}
- El-Nahas MR, El Kannishy G, Abdelhafez H, Taher I, El Sehrawy A. Oral alpha-lipoic acid adjunctive treatment for symptomatic diabetic peripheral neuropathy: a prospective, double blind, placebo controlled study. 53rd Annual Meeting of the European Association for the Study of Diabetes, 2017, Lisbon. www.easd.org/media-centre/home.html#!resources/oral-alpha-lipoic-acid-adjunctive-treatment-for-symptomatic-diabetic-peripheral-neuropathy-a-prospective-double-blind-placebo-controlled-study (accessed 20 December 2023).
- El-Nahas MR, Elkannishy G, Abdelhafez H, Elkhamisy ET, El-Sehrawy AA. Oral alpha lipoic acid treatment for symptomatic diabetic peripheral neuropathy: a randomized double-blinded placebo-controlled study. Endocrine, Metabolic and Immune Disorders Drug Targets 2020;20(9):1531-4. [DOI: 10.2174/1871530320666200506081407] [DOI] [PubMed] [Google Scholar]
Additional references
Abubaker 2022
- Abubaker SA, Alonazy AM, Abdulrahman A. Effect of alpha-lipoic acid in the treatment of diabetic neuropathy: a systematic review. Cureus 2022;14(6):e25750. [DOI] [PMC free article] [PubMed] [Google Scholar]
Agrawal 2010
- Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Diabetes, vestibular dysfunction, and falls: analyses from the National Health and Nutrition Examination Survey. Otology & Neurotology 2010;31(9):1445-50. [DOI: 10.1097/MAO.0b013e3181f2f035.] [DOI] [PubMed] [Google Scholar]
Allen 2014
- Allen R, Sharma U, Barlas S. Clinical experience with desvenlafaxine in treatment of pain associated with diabetic peripheral neuropathy. Journal of Pain Research 2014;7:339-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Amin 2016
- Amin N, Doupis J. Diabetic foot disease: from the evaluation of the "foot at risk" to the novel diabetic ulcer treatment modalities. World Journal of Diabetes 2016;7(7):153-64. [DOI: 10.4239/wjd.v7.i7.153.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bansal 2006
- Bansal V, Kalita J, Misra UK. Diabetic neuropathy. Postgraduate Medical Journal 2006 Feb;82(964):95-100. [DOI: 10.1136/pgmj.2005.036137] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bastyr 2005
- Bastyr EJ 3rd, Price KL, Bril V, MBBQ Study Group. Development and validity testing of the neuropathy total symptom score-6: questionnaire for the study of sensory symptoms of diabetic peripheral neuropathy. Clinical Therapeutics 2005;27(8):1278-94. [DOI] [PubMed] [Google Scholar]
Boulton 1998
- Boulton AJ, Gries FA, Jervell JA. Guidelines for the diagnosis and outpatient management diabetic peripheral neuropathy. Diabetic Medicine 1998;15(6):508-14. [DOI] [PubMed] [Google Scholar]
Boulton 2005
- Boulton AJ, Vinik AI, Arezzo JC, Bril V, Feldman EL, Freeman R, et al. American Diabetes Association. Diabetic neuropathies: a statement by the American Diabetes Association. Diabetes Care 2005;28(4):956-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bredfeldt 2015
- Bredfeldt C, Altschuler A, Adams AS, Ports J, Bayliss E. Patient reported outcomes for diabetic peripheral neuropathy. Journal of Diabetes and Its Complications 2015;29(8):1112-8. [DOI] [PubMed] [Google Scholar]
Brownlee 2005
- Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes 2005;54(6):1615–25. [DOI] [PubMed] [Google Scholar]
Callaghan 2012a
- Callaghan BC, Cheng HT, Stables CL, Smith AL, Feldman EL. Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurology 2012;11(6):521-34. [DOI: 10.1016/S1474-4422(12)70065-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Callaghan 2012b
- BC, Little AA, Feldman EL, Hughes RA. Enhanced glucose control for preventing and treating diabetic neuropathy. Cochrane Database of Systematic Reviews 2012, Issue 6. Art. No: CD007543. [DOI: 10.1002/14651858.CD007543.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chalk 2007
- Chalk C, Benstead TJ, Moore F. Aldose reductase inhibitors for the treatment of diabetic polyneuropathy. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD004572. [DOI: 10.1002/14651858.CD004572.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2013
- Chen W, Zhang Y, Li X, Yang G, Liu JP. Chinese herbal medicine for diabetic peripheral neuropathy. Cochrane Database of Systematic Reviews 2013, Issue 10. Art. No: CD007796. [DOI: 10.1002/14651858.CD007796.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Covidence [Computer program]
- Covidence. Version accessed 1 May 2018. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
DCCT 1993
- Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine 1993;329(14):977-86. [DOI] [PubMed] [Google Scholar]
DCCT 1995
- DCCT Research Group. Effect of intensive diabetes treatment on nerve conduction in the Diabetes Control and Complications Trial. Annals of Neurology 1995;38(6):869-80. [DOI: 10.1002/ana.410380607] [DOI] [PubMed] [Google Scholar]
Duckworth 2009
- Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. New England Journal of Medicine 2009;360(2):129-39. [DOI] [PubMed] [Google Scholar]
Dyck 1991
- Dyck PJ, Kratz KM, Lehman KA, Karnes JL, Melton LJ 3rd, O'Brien PC, et al. The Rochester Diabetic Neuropathy Study: design, criteria for types of neuropathy, selection bias, and reproducibility of neuropathic tests. Neurology 1991;41(6):799-807. [DOI] [PubMed] [Google Scholar]
Edwards 2008
- Edwards JL, Vincent AM, Cheng HT, Feldman EL. Diabetic neuropathy: mechanisms to management. Pharmacology & Therapeutics 2008;120(1):1-34. [DOI: 10.1016/j.pharmthera.2008.05.005] [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elafros 2022
- Elafros MA, Andersen H, Bennett DL, Savelieff MG, Viswanathan V, Callaghan BC, et al. Towards prevention of diabetic peripheral neuropathy: clinical presentation, pathogenesis, and new treatments. Lancet Neurology 2022;21(10):922-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feldman 1997
- Feldman EL, Stevens MJ, Greene DA. Pathogenesis of diabetic neuropathy. Clinical Neuroscience 1997;4(6):365-70. [PubMed] [Google Scholar]
Feldman 2017
- Feldman EL, Bennett DL, Nave KA, Jensen TS. New horizons in diabetic neuropathy: mechanisms, bioenergetics, and pain. Neuron 2017;93(6):1296-313. [DOI: 10.1016/j.neuron.2017.02.005] [DOI] [PMC free article] [PubMed] [Google Scholar]
Feldman 2019
- Feldman EL, Callaghan BC, Pop-Busui R, Zochodne DW, Wright DE, Bennett DL, et al. Diabetic neuropathy. Nature Reviews Disease Primers 2019;5(1):41. [DOI: 10.1038/s41572-019-0092-1] [DOI] [PubMed] [Google Scholar]
Fernyhough 2015
- Fernyhough P. Mitochondrial dysfunction in diabetic neuropathy: a series of unfortunate metabolic events. Current Diabetes Reports 2015;15(11):89. [DOI: 10.1007/s11892-015-0671-9] [DOI] [PubMed] [Google Scholar]
Gilron 2021
- Gilron I, Robb S, Tu D, Holden R, Towheed T, Ziegler D, et al. Double-blind, randomized, placebo-controlled crossover trial of alpha-lipoic acid for the treatment of fibromyalgia pain: the IMPALA trial. Pain 2021;162(2):561-8. [DOI] [PubMed] [Google Scholar]
Han 2012
- Han T, Bai J, Liu W, Hu Y. A systematic review and meta-analysis of α-lipoic acid in the treatment of diabetic peripheral neuropathy. European Journal of Endocrinology 2012;167(4):465-71. [DOI] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In Higgins JP, Altman DG, Sterne JA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). Cochrane 2017. Available from www.training.cochrane.org/handbook/archive/v5.2.
Higgins 2022
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook/archive/v6.3. [DOI] [PMC free article] [PubMed]
Ibrahim 2017
- Ibrahim A. IDF Clinical Practice Recommendation on the Diabetic Foot: a guide for healthcare professionals. Diabetes Research and Clinical Practice 2017;127:285-7. [DOI: 10.1016/j.diabres.2017.04.013] [DOI] [PubMed] [Google Scholar]
IDF 2021
- International Diabetes Federation. IDF Diabetes Atlas. 10th edition. Brussels: International Diabetes Federation, 2021. [Google Scholar]
Khanna 1999
- Khanna S, Roy S, Packer L, Sen CK. Cytokine-induced glucose uptake in skeletal muscle: redox regulation and the role of alpha-lipoic acid. American Journal of Physiology 1999;276(5 Pt 2):R1327-33. [DOI] [PubMed] [Google Scholar]
Kim 2013
- Kim PJ, Steinberg JS. Complications of the diabetic foot. Endocrinology and Metabolism Clinics of North America 2013;42(4):833-47. [DOI: 10.1016/j.ecl.2013.08.002] [DOI] [PubMed] [Google Scholar]
Kolm‐Litty 1998
- Kolm-Litty V, Sauer U, Nerlich A, Lehmann R, Schleicher ED. High glucose-induced transforming growth factor beta1 production is mediated by the hexosamine pathway in porcine glomerular mesangial cells. Journal of Clinical Investigation 1998;101(1):160-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Low 1997
- Low PA, Nickander KK, Tritschler HJ. The roles of oxidative stress and antioxidant treatment in experimental diabetic neuropathy. Diabetes 1997;46(Suppl 2):S38-42. [DOI] [PubMed] [Google Scholar]
Lunn 2014
- Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database of Systematic Reviews 2014, Issue 1. Art. No: CD007115. [DOI: 10.1002/14651858.CD007115.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mallik 2014
- Mallik S, Kallis C, Lunn MPT, Smith AG. Gangliosides for the treatment of diabetic peripheral neuropathy. Cochrane Database of Systematic Reviews 2014, Issue 3. Art. No: CD011028. [DOI: 10.1002/14651858.CD011028] [DOI] [Google Scholar]
Marangon 1999
- Marangon K, Devaraj S, Tirosh O, Packer L, Jialal I. Comparison of the effect of alpha-lipoic acid and alpha-tocopherol supplementation on measures of oxidative stress. Free Radical Biology & Medicine 1999;27(9-10):1114-21. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norman 2003
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health‐related quality of life: the remarkable universality of half a standard deviation. Medical Care 2003;41(5):582-92. [DOI] [PubMed] [Google Scholar]
Packer 1995
- Packer L, Witt EH, Tritschler HJ. Alpha-lipoic acid as a biological antioxidant. Free Radical Biology & Medicine 1995;19(2):227-50. [DOI] [PubMed] [Google Scholar]
Peripheral Nerve Society 1995
- Peripheral Nerve Society. Diabetic polyneuropathy clinical trials: consensus in controlled report of the peripheral nerve society. Annals of Neurology 1995;38(3):478-82. [DOI] [PubMed] [Google Scholar]
Petersen 2008
- Petersen Shay K, Moreau RF, Smith EJ, Hagen TM. Is alpha-lipoic acid a scavenger of reactive oxygen species in vivo? Evidence for its initiation of stress signaling pathways that promote endogenous antioxidant capacity. IUBMB Life 2008;60(6):362-7. [DOI: 10.1002/iub.40] [DOI] [PubMed] [Google Scholar]
Pop‐Busui 2013
- Pop-Busui R, Lu J, Mori Brooks M, Albert S, Althouse AD, Escobedo J, et al. Impact of glycemic control strategies on the progression of diabetic peripheral neuropathy in the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) Cohort. Diabetes Care 2013;36(10):32-15. [DOI: 10.2337/dc13-0012] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pop‐Busui 2017
- Pop-Busui R, Boulton AJ, Feldman EL, Bril V, Freeman R, Malik RA, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care 2017;40(1):136-54. [DOI: 10.2337/dc16-2042] [DOI] [PMC free article] [PubMed] [Google Scholar]
Price 2022
- Price R, Smith D, Franklin G, Gronseth G, Pignone M, David WS, et al. Oral and topical treatment of painful diabetic polyneuropathy: practice guideline update summary. Report of the AAN Guideline Subcommittee. Neurology 2022;98(1):31-43. [DOI: 10.1212/WNL.0000000000013038] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rochette 2015
- Rochette L, Ghibu S, Muresan A, Vergely C. Alpha-lipoic acid: molecular mechanisms and therapeutic potential in diabetes. Canadian Journal of Physiology and Pharmacology 2015;93(12):1021-7. [DOI] [PubMed] [Google Scholar]
Rolim 2019
- Rolim LC, da Silva EM, Flumignan RL, Abreu MM, Dib SA. Acetyl-L-carnitine for the treatment of diabetic peripheral neuropathy. Cochrane Database of Systematic Reviews 2019, Issue 6. Art. No: CD011265. [DOI: 10.1002/14651858.CD011265.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saarto 2007
- Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD005454. [DOI: 10.1002/14651858.CD005454.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saeedi 2019
- Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Research and Clinical Practice 2019;157:107843. [DOI: 10.1016/j.diabres.2019.107843] [DOI] [PubMed] [Google Scholar]
Snedecor 2014
- Snedecor SJ, Sudharshan L, Cappelleri JC, Sadosky A, Mehta S, Botteman M. Systematic review and meta-analysis of pharmacological therapies for painful diabetic peripheral neuropathy. Pain Practice 2014;14(2):167-84. [DOI] [PubMed] [Google Scholar]
Stavniichuk 2014
- Stavniichuk R, Shevalye H, Lupachyk S, Obrosov A, Groves JT, Obrosova IG, et al. Peroxynitrite and protein nitration in the pathogenesis of diabetic peripheral neuropathy. Diabetes Metabolism Research and Reviews 2014;30(8):669-78. [DOI: 10.1002/dmrr.2549] [DOI] [PMC free article] [PubMed] [Google Scholar]
Streeper 1997
- Streeper RS, Henriksen EJ, Jacob S, Hokama JY, Fogt DL, Tritschler HJ. Differential effects of lipoic acid stereoisomers on glucose metabolism in insulin-resistant skeletal muscle. American Journal of Physiology 1997;273(1 Pt 1):E185-91. [DOI] [PubMed] [Google Scholar]
Tesfaye 2010
- Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 2010;33(10):2285-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tesfaye 2011
- Tesfaye S, Vileikyte L, Rayman G, Sindrup SH, Perkins BA, Baconja M, et al. Painful diabetic peripheral neuropathy: consensus recommendations on diagnosis, assessment and management. Diabetes/Metabolism Research and Reviews 2011;27(7):629-38. [DOI: 10.1007/BF00400697] [DOI] [PubMed] [Google Scholar]
Uehara 2004
- Uehara K, Yamagishi S, Otsuki S, Chin S, Yagihashi S. Effects of polyol pathway hyperactivity on protein kinase C activity, nociceptive peptide expression, and neuronal structure in dorsal root ganglia in diabetic mice. Diabetes 2004;53(12):3239-47. [DOI] [PubMed] [Google Scholar]
Vincent 2013
- Vincent AM, Calabek B, Roberts L, Feldman EL. Biology of diabetic neuropathy. Handbook of Clinical Neurology 2013;115:591-606. [DOI: 10.1016/B978-0-444-52902-2.00034-5] [DOI] [PubMed] [Google Scholar]
Vinik 2004
- Vinik AI, Mehrabyan A. Diabetic neuropathies. Medical Clinics of North America 2004;88(4):947-99. [DOI] [PubMed] [Google Scholar]
Wang 2006
- Wang Y, Schmeichel AM, Iida H, Schmelzer JD, Low PA. Enhanced inflammatory response via activation of NF-kappaB in acute experimental diabetic neuropathy subjected to ischemia reperfusion injury. Journal of the Neurological Sciences 2006;247(1):47-52. [DOI] [PubMed] [Google Scholar]
WHO 1999
- World Health Organization. Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications. Part 1: Diagnosis and Classification of Diabetes Mellitus (WHO/NCD/NCS/99.2). Geneva: World Health Organization. apps.who.int/iris/bitstream/10665/66040/1/WHO_NCD_NCS_99.2.pdf 1999.
WHO 2016
- World Health Organization. Global Report on Diabetes. 2016. www.who.int/diabetes/global-report/en/ (accessed 22 May 2017).
Xu 2013
- Xu Q, Pan J, Yu J, Liu X, Liu L, Zuo X, et al. Meta-analysis of methylcobalamin alone and in combination with lipoic acid in patients with diabetic peripheral neuropathy. Diabetes Research and Clinical Practice 2013;101(2):99-105. [DOI: 10.1016/j.diabres.2013.03.033] [DOI] [PubMed] [Google Scholar]
Young 1993
- Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia 1993;36(2):150-4. [DOI] [PubMed] [Google Scholar]
Ziegler 2004
- Ziegler D, Nowak H, Kempler P, Vargha P, Low PA. Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a meta-analysis. Diabetic Medicine 2004;21(2):114-21. [DOI] [PubMed] [Google Scholar]
Ziegler 2006
- Ziegler D. Treatment of diabetic polyneuropathy: update. 2006. Annals of the New York Academy of Sciences 2006;1084:250-66. [DOI] [PubMed] [Google Scholar]
Ziegler 2021a
- Ziegler D, Papanas N, Schnell O, Nguyen BD, Nguyen KT, Kulkantrakorn K, et al. Current concepts in the management of diabetic polyneuropathy. Journal of Diabetes Investigation 2021;12(4):464-75. [DOI: 10.1111/jdi.13401] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ziegler 2021b
- Ziegler D, Keller J, Maier C, Pannek J. Diabetic neuropathy. Experimental and Clinical Endocrinology and Diabetes 2021;129(S 01):S70-S81. [DOI: 10.1055/a-1284-6245] [DOI] [PubMed] [Google Scholar]
Ziegler 2022
- Ziegler D, Tesfaye S, Spallone V, Gurieva I, Al Kaabi J, Mankovsky B, et al. Screening, diagnosis and management of diabetic sensorimotor polyneuropathy in clinical practice: international expert consensus recommendations. Diabetes Research and Clinical Practice 2022;186:109063. [DOI: 10.1016/j.diabres.2021.109063] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Baicus 2018
- Baicus C, Purcarea A, Elm E, Delcea C, Furtunescu F. Alpha‐lipoic acid for diabetic peripheral neuropathy. Cochrane Database of Systematic Reviews 2018, Issue 2. Art. No: CD012967. [DOI: 10.1002/14651858.CD012967] [DOI] [PMC free article] [PubMed] [Google Scholar]


