Abstract
Introduction and importance:
A primary congenital splenic epidermoid cyst is an immensely rare pathology with mostly unknown epidemiological parameters. Misdiagnosis can easily happen and this results in life-threatening ramifications for patients. Considering this pathology as a potential differential diagnosis allows for the required surgical intervention to be timely accomplished. In this case, the authors are documenting this pathology and presenting how it was successfully managed via proper and informed preoperative analysis and meticulous intraoperative technique.
Case presentation:
Hereby, we portray the exceptionally rare case of a 7-year-old male who presented to our surgical clinic complaining of a sudden left hypochondriac pain with early satiety for 1 month’s duration. The preoperative radiological assessment displayed numerous splenic cystic lesions throughout the splenic parenchyma.
Clinical discussion:
Resection of the cysts was accomplished via total splenectomy. The ensuing histopathological analysis via Hematoxylin and Eosin of the resected specimens established the diagnosis of a congested hemorrhagic spleen with multiple primary congenital splenic epidermoid cysts.
Conclusion:
Primary congenital splenic epidermoid cysts are an extremely rare type of splenic pathology. There is profound scarcity amidst the published literature regarding it. This merits in-depth study and apt documentation to raise awareness regarding this pathology as a potential differential diagnosis in cases of abdominal pain. Documentation allows us to set up proper and innovative clinical and surgical protocols for these patients. Based on our conclusive review of the published literature, the authors conclude that ours is the first ever documented case from our country of a primary congenital splenic epidermoid cyst.
Keywords: abdominal surgery, case report, epidermoid cyst, primary congenital splenic epidermoid cyst, splenic cyst, total splenectomy
Introduction
Highlights
A primary congenital splenic epidermoid cyst is a profoundly rare pathology with an unknown incidence rate. Many epidemiological parameters are still yet unclear and this further magnifies the rarity and relevance of our findings.
The significance of primary splenic epidermoid cysts is that they are the rarest of all true splenic cysts. Nevertheless, they must be borne in mind as a potential differential diagnosis to avoid their potential complications and to facilitate timely surgical interventions.
In principle, cystic lesions of the spleen are classically diagnosed in the 2nd and 3rd decades of life and have a notable female-to-male predominance.
Curative treatment is primarily in the form of splenectomy where all the cysts are thoroughly resected. This highly limits recurrence and lessens the potential risks of cystic hemorrhage, rupture, and ensuing infections.
The definitive diagnosis can only be reached via meticulous histopathological analysis of the cystic lesions. This highlights the vitality of microscopic examination of the resected specimens.
Splenic cysts are an enormously rare entity to be diagnosed in the everyday surgical practice. Their real incidence rate remains unspecified, but according to a study written by Robbins et al., they concluded an incidence rate of 0.07% amongst 42 327 autopsies1,2. Cystic lesions of the spleen are either parasitic or nonparasitic in origin. The latter are rarer to occur and are classified into primary cysts that are characterized by having either an epithelial lining (i.e. Mesothelial, epidermoid, and dermoid) or an endothelial lining (i.e. Hemangioma and lymphangioma), and secondary cysts (i.e. Pseudocysts) that are principally a result of trauma3,4. Among these splenic pathologies, primary splenic epidermoid cysts are contemplated to account for ~10% of cases and are chiefly seen in the pediatric and young age groups5. To diagnose this type of splenic cysts, multiple radiological imaging methods have been proposed to demonstrate the relevant cystic features. However, the definitive diagnosis can solely be accomplished after conducting meticulous histopathological analysis on the specimens6. Treatment approaches for splenic cysts of nonparasitic origin remains a subject of discussion in the contemporary surgical practice. Nevertheless, partial splenectomy, when applicable, has proven to be the most efficient form of treatment to both treat the condition while preserving a degree of splenic function and to avoid any possible recurrence7. Based on our in-depth review of the available published literature, we conclude that our case is the first ever case from our country of a primary congenital splenic epidermoid cyst. The work has been reported in line with the SCARE criteria and the revised 2020 SCARE guidelines8.
Presentation of case
Patient information
We herein demonstrate the rare case of a previously healthy 7-year-old Middle Eastern male who introduced to our surgical outpatient clinic with the chief complaint of left hypochondriac pain with early satiety. The onset of his symptoms was reported to begin 1 month prior to his clinical presentation. The pain was localized in the left hypochondriac region, sudden in onset, vague in nature, did not radiate to any other regions, associated with early satiety, had no triggering factors, was partially relieved by over-the-counter analgesic medications, and estimated to measure 05/10 on the patient’s numerical pain scale. It is worth noting that the patient did not experience any nausea, emesis, jaundice, or any alternations in bowel habits. The remaining review of systems was unremarkable. He further denied any history of physical trauma, contact with animals, eating any contaminated or not properly cleaned food, tussis, or chest pain. Moreover, our patient denied experiencing any of the cardinal B-Symptoms, such as fever, chills, cold and night sweats, or unintended changes in his body weight. His previous medical, surgical, allergic, drug, and psychosocial histories are all uneventful. Furthermore, his family history is negative for such an occurrence and overall unremarkable. It is vital to note that he denied experiencing any previous similar symptoms in the past as this is the first time encountering them. His growth parameters in terms of weight for age and weight for length were within normal.
Clinical findings
We commenced our physical evaluation by recording the patient’s vital signs and they were within normal values. Upon abdominal inspection, it moved symmetrically with respiration, the umbilicus was central, and no distention or skin discolorations were seen (i.e. Caput medusa, spider naevi, jaundice, or hypo-/hyperpigmentation). We noticed localized guarding and marked tenderness upon abdominal palpation and percussion of the left hypochondriac region. However, no vital organs (i.e. The spleen) were palpable during the examination. Nonetheless, deep palpation was not feasible due to the patient’s frank discomfort and elicited pain and tenderness. The findings of the abdominal auscultation were unremarkable. The remaining physical examination did not yield any other findings. Based on the previous patient history and physical examination, the following differential diagnoses were taken into consideration: Hydatid cysts, splenic abscesses, splenic neoplastic pathologies (i.e. Epidermoid cysts, lymphangiomas, and hemangiomas), metastases, and hamartoma of the spleen.
Diagnostic assessment
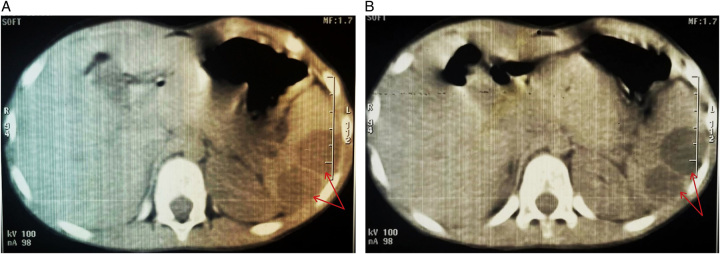
We instigated our preoperative radiological assessment by performing a detailed abdominal ultrasound. It revealed a spleen with normal echogenicity but markedly enlarged as it measured approximately (10 cm) and was seen containing multiple anechoic thin-walled cystic lesions where the largest of which was estimated to measure around (2.8 cm). No free fluid was seen in the abdomen or pelvis. Further in-depth radiological analysis was completed, to further understand the findings and to rule-out any intrathoracic common lesions like hydatid cysts or potential metastasis in the possible case of a neoplastic formation, via performing a high-resolution Multi-Slice Computed Tomography (MSCT) scan of the chest, abdomen, and pelvis. Findings included splenomegaly where the spleen measured around (12 cm) with multiple splenic lesions within its parenchyma without calcifications. The largest of said lesions measured approximately (2.5 cm) (Fig. 1 A, B). No further abnormalities (i.e. Hepatomegaly, ascites, lymphadenopathy, or other masses) were seen and the lung field was clear. A complete laboratory workup was also done and the values of which were all within normal. Additionally, we opted to conduct an indirect hemagglutination test and Enzyme-Linked Immunosorbent Assay to detect any possible parasitic infection (i.e. Echinococcus Granulosus) and the results of which were negative. After taking the previous elements into careful consideration, we admitted our patient and our multidisciplinary team reached the decision to perform a curative surgical intervention in the form of open surgery. To prepare the patient for surgery, he was administered the proper vaccines for patients who will have undergo a splenectomy, we assigned him to a nil-per-mouth status and set up 2 large-bore intravenous cannulas to administer the proper fluids and antibiotics alike. We do not report encountering any particular challenges or encumbrances throughout any of the perioperative phases.
Figure 1.
(A, B): MSCT cross-sectional images of the abdomen and pelvis. Findings include splenomegaly where the spleen measured around (12 cm) with multiple splenic lesions within its parenchyma without calcifications (Identified in both images by the Red Arrows). The largest of said lesions measured approximately (2.5 cm).
Therapeutic intervention
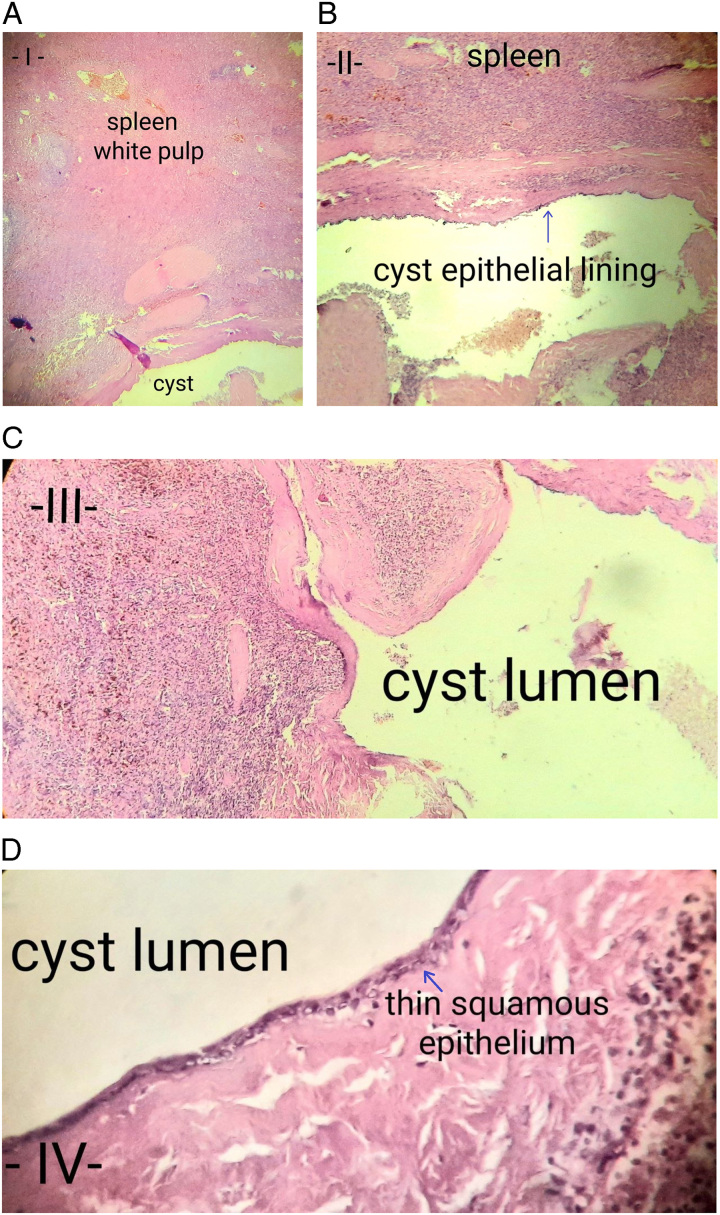
The surgical team elected to implement the open surgical approach to minimize the perioperative complications based on the clinical and radiological assessments. Our tertiary hospital is where our operation successfully took place on the 2nd day after patient admission and once all the preoperative preparatory proceedings have taken place. The surgical intervention was achieved via a left subcostal incision to provide adequate field of vision and limit the possible complications. The surgical intervention was inducted under general anesthesia with no marked perioperative complications. The operation was directly supervised by our General Surgery professor who has 35 years of previous experience. He was assisted by two senior surgical assistants, the first with 11 and the other with 8 years of experience, respectively. An architecturally sound but enlarged spleen with a hemorrhagic appearance was seen. We found several splenic cystic formations occupying most of the splenic parenchyma and near the splenic hilum. Therefore, a total splenectomy was deemed necessary as the spleen could not be spared. The spleen was carefully isolated and dissected to avoid any hemorrhage or rupturing of the cysts. The spleen was then completely removed along with the cysts. Careful exploration of the abdomen was completed and no further findings were seen. On the same day of surgery, the resected specimens were directly sent to a specialized histopathology laboratory to undergo meticulous microscopic analysis to determine a definitive diagnosis. Overall and microscopic analyses were overall concluded within 48 h of surgery. Grossly, it described a congested hemorrhagic spleen measuring (12×8×6 cm) with five congenital epidermoid cysts where the largest of which measured (6 cm). Furthermore, microscopic analysis of the resected specimens via Hematoxylin and Eosin (H&E) revealed the presence of a well-preserved splenic architecture, large lymphoid follicles with large congested vessels, and severe interstitial hemorrhage. The cysts were lined with squamous epithelial lining and surrounded by a dense fibrotic wall (Fig. 2 A–D). No evidence of hydatid and/or parasitic cysts, granuloma, malignancy or atypia was demonstrated. Kindly note, that all the provided histology images are equipped within with annotations and arrows to help identify the discussed structures. Postoperatively, we ensured the successful early ambulation of our patient as early as the same day of surgery. Moreover, we provided him with the appropriate postoperative antibiotics and intravenous fluids in addition to applying daily sterile wound dressings to avoid any potential postoperative infections. He was then discharged from the hospital to the outpatient settings on the 2nd postoperative day as his general state was good and his vital signs were optimal. Hence, he was clinically followed up for 13 weeks thus far. In his regularly scheduled clinical visits, he underwent physical, radiological, and laboratory examinations. The results of these evaluations were all normal.
Figure 2.
A: Microscopic image of the histopathological analysis of the resected specimens. Via H&E staining, we can demonstrate the spleen’s native histological tissue characterized by the white pulp. B: Microscopic image of the histopathological analysis of the resected specimens. Via H&E staining, we can see the splenic histological structure while depicting the cyst’s epithelial lining identified by the Blue Arrow. C: Microscopic image of the histopathological analysis of the resected specimens. Via H&E staining, we can clearly visualize the cystic lumen. D: Microscopic image of the histopathological analysis of the resected specimens. Via H&E staining, we can clearly visualize the cystic lumen along with the thin squamous epithelial lining identified by the Blue Arrow.
Discussion
In 1958, Martin proposed the core classification of splenic cysts that assigned them into two chief categories; primary cysts that are characterized by having an epithelial cell lining, and secondary cysts that lack an epithelial cell lining. The former can be further subtyped into nonparasitic and parasitic cysts according to their etiological factors9. Our topic which is epidermoid splenic cysts are classified as primary nonparasitic congenital splenic cysts that are highlighted by an epithelial cell lining on the contrary to secondary cysts that are mainly made up of fibrous soft tissue10,11. Tracking the historical elements of splenic cysts, it is established that Andral G.12 was the pioneer who first depicted a case of dermoid cyst of the spleen during an autopsy in 1829. The pathophysiological origin of primary splenic cysts remains a subject of controversy. However, it is hypothesized that they arise as a result of peritoneal mesothelial cells entrapment within the parenchyma of the spleen during the phases of fetal embryogenesis13. The significance of primary splenic epidermoid cysts is that they are the rarest of all true splenic cysts14. In principle, cystic lesions of the spleen are classically diagnosed in the 2nd and 3rd decades of life. Nonetheless, they are also found in pediatrics15. With regard to gender predominance, splenic cysts are found to have a female-to-male predominance16. Primary splenic epidermoid cysts are conformant with this and are considered chiefly occur in the pediatric and young age groups5. In terms of clinical presentation, the majority of patients have an asymptomatic clinical course. Moreover, patients do not usually complain of any characteristic or pathognomonic symptoms, especially if the cyst’s size is small. However, large cysts result in the development of nonspecific abdominal complaints, such as discomfort, nausea, pain, or detecting a palpable mass formation situated mainly in the left hypochondriac region11,17. Nevertheless, a small percentage of patients initially present with disease-related complications, such as infections, cystic hemorrhage, or rupture18,19. Patients could also present with an unexplained thrombocytopenia, but this seldom occurs20,21. Additionally, patients could sometimes also present with the chief complaint of a persistent tussis and pleuritic pain22. In the context of diagnostic radiological imaging, splenic epidermoid cysts can manifest as well-demarcated solitary cystic lesions with a varied number of septations11. Diagnostic ultrasonography scan is the ideal initial noninvasive imaging modality to screen for and demonstrate the presence of a cystic lesion23. Via ultrasonography, we can distinguish between the solid and cystic nature of a lesion in the majority of cases24. Epidermoid splenic cysts manifest on ultrasonography scan as anechoic mass formations with thin walls and septic formations. In instances where the cysts are structurally complex, foci of calcifications could be demonstrated. These are particularly beneficial to distinguish the different etiological factors of the occurring splenomegaly22,25,26. On the other hand, more complex diagnostic methods include Computed Tomography scanning. On Computed Tomography imaging, we can properly visualize calcifications and septations of a cystic lesion when they are present11. Primary congenital epidermoid splenic cysts appear typically as anechoic lesions with thin walls on ultrasound scanning with no calcific foci on Computed Tomography5. In terms of differential diagnoses that must be taken into consideration when presented with similar cases, we should mention hydatid cysts, splenic abscesses, splenic neoplastic pathologies (i.e. Dermoid cysts, lymphangiomas, and hemangiomas), metastases, inflammatory pseudotumors, and hamartoma of the spleen. However, it is worth noting that epidermoid splenic cysts are the rarest of the true splenic cysts14,27. To establish a definitive diagnosis, microscopic analysis of the resected spleen via histopathology is the gold standard method. Primary splenic epidermoid cysts are typically solitary in occurrence. To a much lesser extent, they are multiple, and some cases of multiple cysts have been documented in the literature.28,29. Via histopathological analysis, we can note that primary splenic cysts of nonparasitic origin possess an inner lining of stratified squamous epithelium. Nevertheless, this cellular lining may be lost, simply becomes flattened, or show transitional cell lining (i.e. Squamous, columnar, cuboidal, unilayered, or multilayered). Furthermore, primary splenic epidermoid cysts classically show stratified Squamous epithelial lining in addition to a fibrocollagenous wall3,20. Therapeutic approaches in the form of a curative surgical intervention is the modality of choice in splenic cysts that exert symptoms and for those that are greater in size than (5 cm). It is worth noting that attempting to take a biopsy via radiological-guided needle aspiration is not a suitable option because of its high risks and potential devastating complications, such as cystic leakage, rupture, bleeding, and infections5,10,11. Removing said splenic cystic lesions via surgery requires several crucial factors to be first taken into consideration (i.e., Size, site, and depth). When proposing total splenectomy as a therapeutic choice, factors that support that approach include the presence of several cysts, cysts located in the splenic hilum, splenic cysts that are totally engulfed by the parenchyma of the spleen, and as mentioned above; cysts larger than (5 cm)30–32. Other treatment options come in the form of fenestration or marsupialization. Yet, those are applicable for in the cases where the splenic cysts are superficial. Nevertheless, these methods come with the risk of post-treatment cystic recurrence11,33. Another therapeutic modality is the percutaneous drainage of the splenic cysts. However, this matter remains a subject of debate. Some experts consider it an efficient, safe, and cost-friendly method that aids in a fast recovery, whereas other experts consider this method to yield in high rates of cystic recurrence30,31. To sum up, our case’s significance stems from multiple elements. First it is documented in a male rather than a female. Second, it depicts multiple splenic epidermoid cysts rather than a solitary cyst. Third, it is arising in an atypical age group. Fourth, it is the first documented case of its kind from our country.
Conclusion
A congenital splenic epidermoid cyst is an extremely rare splenic pathology. The subsequent splenic congestion and hemorrhagic changes in addition to the complications of an untreated splenic epidermoid cyst can yield life-threatening complications for the affected patients. This pathology warrants further investigation, evaluation, and documentation to raise awareness regarding this disease as a differential diagnosis in in the clinical and surgical settings. Therefore, we must document these cases to help set up proper and innovative clinical, surgical, and surveillance protocols for these patients. Based on our careful review of the available literature, we conclude that ours is the first ever documented case from our country of a congenital splenic epidermoid cyst.
Ethical approval and consent to participate
Institutional review board approval is not required for deidentified single case reports or histories based on institutional policies.
Consent
Written informed consent was obtained from the patient’s parents/legal guardian for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
N/A.
Author contribution
O.A.: Conceptualization, resources, methodology, data curation, investigation, who wrote, original drafted, edited, visualized, validated, literature reviewed the manuscript, and the corresponding author who submitted the paper for publication.
R.S.: Data curation, resources, validation, visualization, writing, and reviewing the manuscript.
A.Al., M.A.: General Surgery PhD students and specialists who performed and supervised the operation, in addition to supervision, project administration, and review of the manuscript.
M.B.: General Surgery professor who supervised the operation, in addition to supervision, project administration, and review of the manuscript.
All authors read and approved the final manuscript.
Conflicts of interest disclosure
The authors declare that there are no conflicts of interest.
Research registration unique identifying number (UIN)
N/A.
Guarantor
Omar Al Laham.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available because the data were obtained from the hospital computer-based in-house system. Data are available from the corresponding author upon reasonable request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
Dr Lina Haffar’s Histopathology and Immunohistochemistry Laboratory, Damascus, (The) Syrian Arab Republic.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 2 December 2023
Contributor Information
Omar Al Laham, Email: 3omar92@gmail.com.
Rahaf Sharaf Aldeen, Email: rahaf.n.sharaf.aldeen@gmail.com.
M Fadi Al Kurdi, Email: DrMuhammadFadiAlkurdi@gmail.com.
Ali Alshiekh, Email: alialshiekh5@gmail.com.
Maher Bozo, Email: drmaherbozo62@gmail.com.
References
- 1.Khan Z, Chetty R. A review of the cysts of the spleen. Diagnostic Histopathol 2016;22:479–484. [Google Scholar]
- 2.Robbins FG, Yellin AE, Lingua RW, et al. Splenic epidermoid cysts. Ann Surg 1978;187:231–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reddi VR, Reddy MK, Srinivas B, et al. Mesothelial splenic cyst--a case report. Ann Acad Med Singap 1998;27:880–882. [PubMed] [Google Scholar]
- 4.Verma M, Vashist MG, Dalal S, et al. Epidermoid cyst of the spleen. IJRRMS 2013;3:47–48. [Google Scholar]
- 5.Rana AP, Kaur M, Singh P, et al. Splenic epidermoid cyst - a rare entity. J Clin Diagn Res 2014;8:175–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soo WT, Lau KS, Yong SG, et al. Giant epithelial nonparasitic splenic cyst a pre-operative diagnosis dilemma: a case report. Med J Malaysia 2021;76:597–599. [PubMed] [Google Scholar]
- 7.Garza-Serna U, Ovalle-Chao C, Martinez D, et al. Laparoscopic partial splenectomy for congenital splenic cyst in a pediatric patient: case report and review of literature. Int J Surg Case Rep 2017;33:44–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agha RA, Franchi T, Sohrabi C, et al. SCARE Group . The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 2020;84:226–230. [DOI] [PubMed] [Google Scholar]
- 9.MARTIN JW. Congenital splenic cysts. Am J Surg 1958;96:302–308. [DOI] [PubMed] [Google Scholar]
- 10.Cianci P, Tartaglia N, Altamura A, et al. A recurrent epidermoid cyst of the spleen: report of a case and literature review. World J Surg Oncol 2016;14:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vo QD, Monnard E, Hoogewoud HM. Epidermoid cyst of the spleen. BMJ Case Rep 2013;2013:bcr2013009707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andral G. Précis d'anatomie pathologique. Gabon; 1829.
- 13.Algino SE, Sorrentino S, Luyimbazi DT, et al. Epidermoid cysts in a wandering spleen: an unusual enigma. Case Rep Surg 2019;2019:1581736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marjanović ZO, Djordjević IM. Epidermoid splenic cysts in children and adolescents. Acta Chir Iugosl 2008;55:63–67; Serbian. [DOI] [PubMed] [Google Scholar]
- 15.Sakamoto Y, Yunotani S, Edakuni G, et al. Laparoscopic splenectomy for a giant splenic epidermoid cyst: report of a case. Surg Today 1999;29:1268–1272. [DOI] [PubMed] [Google Scholar]
- 16.Karia N, Lakhoo K. Complicated congenital splenic cyst: saved by a splenunculus. Afr J Paediatr Surg 2011;8:98–100. [DOI] [PubMed] [Google Scholar]
- 17.Mathur SK, Sangwan M, Singh R, et al. An unusual case of epidermoid-splenic cyst. Trop Gastroenterol 2014;35:62–64. [PubMed] [Google Scholar]
- 18.Pastore V, Bartoli F. A report of a giant epidermoid splenic cyst. Afr J Paediatr Surg 2014;11:67–70. [DOI] [PubMed] [Google Scholar]
- 19.Okuno M, Yuasa N, Takeuchi E, et al. A case of ruptured splenic cyst with elevated serum levels of CEA treated by laparoscopic unroofing. Clin J Gastroenterol 2019;12:642–649. [DOI] [PubMed] [Google Scholar]
- 20.Ingle SB, Hinge CR, Jatal SN. An interesting case of primary epithelial cyst of spleen. Indian J Pathol Microbiol 2013;56:181–182. [DOI] [PubMed] [Google Scholar]
- 21.Tsakraklides V, Hadley TW. Epidermoid cysts of the spleen. A report of five cases. Arch Pathol 1973;96:251–254. [PubMed] [Google Scholar]
- 22.Labruzzo C, Haritopoulos KN, El Tayar AR, et al. Posttraumatic cyst of the spleen: a case report and review of the literature. Int Surg 2002;87:152–156. [PubMed] [Google Scholar]
- 23.Garg M, Kataria SP, Sethi D, et al. Epidermoid cyst of spleen mimicking splenic lymphangioma. Adv Biomed Res 2013;2:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siniluoto TM, Päivänsalo MJ, Lähde ST, et al. Nonparasitic splenic cysts. Ultrasonographic features and follow-up. Acta Radiol 1994;35:447–451. [PubMed] [Google Scholar]
- 25.Robertson F, Leander P, Ekberg O. Radiology of the spleen. Eur Radiol 2001;11:80–95. [DOI] [PubMed] [Google Scholar]
- 26.Hansen MB, Moller AC. Splenic cysts. Surg Laparosc Endosc Percutan Tech 2004;14:316–322. [DOI] [PubMed] [Google Scholar]
- 27.Morgenstern L. Nonparasitic splenic cysts: pathogenesis, classification, and treatment. J Am Coll Surg 2002;194:306–314. [DOI] [PubMed] [Google Scholar]
- 28.Morohoshi T, Hamamoto T, Kunimura T, et al. Epidermoid cyst derived from an accessory spleen in the pancreas. A case report with literature survey. Acta Pathol Jpn 1991;41:916–921. [DOI] [PubMed] [Google Scholar]
- 29.Tateyama H, Tada T, Murase T, et al. Lymphoepithelial cyst and epidermoid cyst of the accessory spleen in the pancreas. Mod Pathol 1998;11:1171–1177. [PubMed] [Google Scholar]
- 30.Karfis EA, Roustanis E, Tsimoyiannis EC. Surgical management of nonparasitic splenic cysts. JSLS 2009;13:207–212. [PMC free article] [PubMed] [Google Scholar]
- 31.Smith ST, Scott DJ, Burdick JS, et al. Laparoscopic marsupialization and hemisplenectomy for splenic cysts. J Laparoendosc Adv Surg Tech A 2001;11:243–249. [DOI] [PubMed] [Google Scholar]
- 32.Macheras A, Misiakos EP, Liakakos T, et al. Non-parasitic splenic cysts: a report of three cases. World J Gastroenterol 2005;11:6884–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen YY, Shyr YM, Wang SE. Epidermoid cyst of the spleen. J Gastrointest Surg 2013;17:555–561. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available because the data were obtained from the hospital computer-based in-house system. Data are available from the corresponding author upon reasonable request.