To the Editor: Herpes vegetans (HV) is a rare manifestation of herpes simplex virus (HSV) seen in patients with immunodeficiency, most commonly in the setting of acquired immunodeficiency syndrome (AIDS),1 but also in other states of severe immunocompromise such as malignancy and congenital immunodeficiencies.2 HV classically presents in the anogenital region, but there are few reports in the literature documenting lesions in other areas, including the tongue and eyelids.2,3 Similarly, HV in immunocompetent patients living with human immunodeficiency virus (HIV) with undetectable viral load (VL) has not been well-documented. Hill et al4 reports a case of anogenital HV mimicking condyloma acuminata in a well-controlled HIV and renal transplant patient on multiple immunosuppressive agents. We present our case to highlight another instance of HV in a person living with HIV (PLWH) but in the setting of undetectable VL, with lesions in an atypical location, mimicking a neoplastic or infectious process.
A 51-year-old woman with a past medical history of asthma and gastroesophageal reflux disease presented to the emergency department with a 4-week history of a rapidly progressive, ulcerating nodule on the right nasal ala. The patient is a PLWH, well-controlled on bictegravir/emtricitabine/tenofovir alafenamide. The patient’s VL was undetectable; her CD4+ cell count was 382 cells/μL. She reported adherence to antiretroviral therapy with no lapses in care. Physical examination was significant for a round, exophytic plaque abutting the right nasal opening, extending medially to the columella and inferiorly to the upper lip (Fig 1). Based on the patient’s clinical presentation, a diagnosis of HV was suspected; other differential diagnoses included squamous cell carcinoma, blastomycosis, and other atypical infections.
Fig 1.
Herpes vegetans (HV) presenting as a large, round, exophytic plaque abutting the right nasal opening.
A lesional punch biopsy revealed impetiginized, purulent scale crust and markedly inflamed granulation tissue with rare multinucleated cells, features suggestive of HSV infection; the immunohistochemical stain confirmed HSV-2 infection (Fig 2). The patient failed to respond adequately to high-dose oral valacyclovir, but topical imiquimod reduced the lesion’s size by 50%. The patient is pending surgical evaluation, hoping to remove the residual plaque.
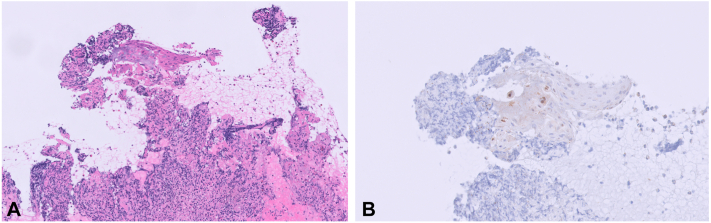
Fig 2.
A, A 10× magnification. Hematoxylin & Eosin (H&E) stained sections show markedly inflamed granulation tissue and overlying multinucleated epithelial cells. B, A 20× magnification. An immunohistochemical stain for HSV is positive in the epithelial cells.
The first-line treatment for HV is acyclovir, valacyclovir, or famciclovir. Imiquimod, foscarnet, cidofovir, and vidarabine, administered either topically or intravenously, are alternative options in the case of unresponsiveness to initial antivirals, and surgical excision offers another alternative treatment for patients with single or a few small lesions.5 In our case, the patient responded poorly to valacyclovir and incompletely to imiquimod, necessitating referral for surgical intervention.
We present this case to emphasize that despite HV classically presenting in the anogenital region of severely immunocompromised patients, clinicians must consider HV on the differential for PLWH presenting with a verrucous plaque, irrespective of the lesion location or the patient’s VL. HV may mimic neoplastic or atypical infections, and prompt identification of the correct diagnosis is essential for proper treatment and favorable outcomes.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
Patient consent: Consent for the publication of all patient photographs and medical information was provided by the authors at the time of article submission to the journal stating that all patients gave consent for their photographs and medical information to be published in print and online and with the understanding that this information may be publicly available.
References
- 1.Ronkainen S.D., Rothenberger M. Herpes vegetans: an unusual and acyclovir-resistant form of HSV. J Gen Intern Med. 2018;33(3):393. doi: 10.1007/s11606-017-4256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yen-Fen Y., Yu-Hung W. Herpes vegetans. Dermatol Sin. 2013;31(3):163–164. doi: 10.1016/j.dsi.2012.12.001. [DOI] [Google Scholar]
- 3.Frey C., Dinkins J., Suah S., Merkel K. Herpetic pseudotumor of the nostril: a report of facial herpes vegetans in a patient with chronic lymphocytic leukemia. Cureus. 2023;15(5) doi: 10.7759/cureus.38702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hill M.S., Jampel R.M. Verrucous herpes treated as condyloma acuminata: a case of cognitive bias. JAAD Case Rep. 2021;17:81–83. doi: 10.1016/j.jdcr.2021.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Charles J.E.M., Weis S.E., Hosler G.A. Acyclovir-resistant anogenital herpes simplex virus in an HIV patient with pseudoepitheliomatous hyperplasia resembling squamous cell carcinoma. HCA Healthc J Med. 2022;3(4):247–252. doi: 10.36518/2689-0216.1301. [DOI] [PMC free article] [PubMed] [Google Scholar]